Abstract
Objective:
Cannabis use disorder diagnoses are increasing among U.S. adults and are more prevalent among people with comorbid psychiatric disorders. Recent changes in cannabis laws, increasing cannabis availability, and higher-potency cannabis may have placed people with cannabis use and psychiatric disorders at disproportionately increasing risk for cannabis use disorder. The authors used Veterans Health Administration (VHA) data to examine whether trends in cannabis use disorder prevalence among VHA patients differ by whether they have psychiatric disorders.
Methods:
VHA electronic health records from 2005 to 2019 (N range, 4,332,165–5,657,277) were used to identify overall and age-group-specific (<35, 35–64, and ≥65 years) trends in prevalence of cannabis use disorder diagnoses among patients with depressive, anxiety, posttraumatic stress, bipolar, or psychotic spectrum disorders and to compare these to corresponding trends among patients without any of these disorders. Given transitions in ICD coding, differences in trends were tested within two periods: 2005–2014 (ICD-9-CM) and 2016–2019 (ICD-10-CM).
Results:
Greater increases in prevalence of cannabis use disorder diagnoses were observed among patients with psychiatric disorders compared to those without (difference in prevalence change, 2005–2014: 1.91%, 95% CI=1.87–1.96; 2016–2019: 0.34%, 95% CI=0.29–0.38). Disproportionate increases in cannabis use disorder prevalence among patients with psychiatric disorders were greatest among those under age 35 between 2005 and 2014, and among those age 65 or older between 2016 and 2019. Among patients with psychiatric disorders, the greatest increases in cannabis use disorder prevalences were observed among those with bipolar and psychotic spectrum disorders.
Conclusions:
The findings highlight disproportionately increasing disparities in risk of cannabis use disorder among VHA patients with common psychiatric disorders. Greater public health and clinical efforts are needed to monitor, prevent, and treat cannabis use disorder in this population.
Many individuals use cannabis without evident harm. However, people with regular or heavy use are at increased risk of numerous cannabis-related health consequences (1–3), including an estimated 20%–33% of individuals with cannabis use who develop cannabis use disorder (4). Cannabis use disorder is associated with impaired functioning, psychosocial impairments, and health problems (5, 6). Over the past two decades, nonmedical use of cannabis has increased (7, 8), and the prevalence of cannabis use disorder has increased among adults in the U.S. general population (9, 10), in national samples of clinical populations (11, 12), and among U.S. veterans (13, 14). Identifying characteristics that are associated with disproportionately increased risk for medically recognized cannabis use disorder over time is an important public health priority. Numerous studies point to associations between cannabis use disorder and psychiatric disorders (6, 15–17). Several etiological models are used to explain mechanisms that underlie these complex relationships. These include shared vulnerabilities (e.g., genetic factors) (18–20) and secondary psychiatric illnesses (21, 22), including substance use disorders as a risk factor for psychiatric disorders. In addition, psychiatric disorders increase the risk for substance use disorders (21, 23), primarily as a result of substance use to cope with or self-medicate negative internal experiences that are related to mental health conditions (24). Findings from a growing number of studies, including cannabis studies (25–27), provide support for psychiatric disorders increasing risk for cannabis use and subsequent cannabis use disorder (28).
In a survey of U.S. adults, nearly half believed that cannabis use is beneficial for stress, anxiety, or depression (29), consistent with self-reported reasons for use (30). However, reviews and meta-analyses (31, 32) suggest that using cannabinoids to treat psychiatric conditions increases the risk for adverse events while not providing significant benefits for depression, most anxiety conditions, posttraumatic stress disorder (PTSD), or psychotic disorders. Nevertheless, states that have legalized medical cannabis use generally permit its use for psychiatric conditions. Given the rapidly evolving U.S. cannabis landscape, including increasingly permissive attitudes and laws, increasing availability, and increasingly potent cannabis products (33, 34), people with psychiatric disorders may be a group whose risk for cannabis use disorder is increasing disproportionately over time. If so, greater public health and clinical efforts should be focused on identifying, preventing, and treating cannabis use disorder among individuals with psychiatric disorders.
Cannabis use and cannabis use disorder are prevalent among veterans, a population that is disproportionally affected by many health conditions, including psychiatric disorders such as PTSD and depressive disorders (35, 36). Among veterans, medical and nonmedical cannabis use as well as cannabis use disorder are associated with numerous negative health outcomes, including other substance use, psychiatric disorders, self-harm and suicidality, and physical conditions (37–39) such as chronic pain (40). Among veterans receiving health care within the Veterans Health Administration (VHA), rates of cannabis use disorder diagnoses have increased considerably since 2005 (13, 14). However, information regarding differences in cannabis use disorder trends between veterans with and without psychiatric disorders is currently lacking.
To date, few sources of data have been available on trends over time in cannabis use disorder that also provide detailed information on diagnoses of specific psychiatric disorders. The VHA is the largest integrated health care system in the United States, and its electronic health record (EHR) database can be leveraged to compare trends in diagnoses of cannabis use disorder between patients with and without comorbid psychiatric disorders. Using yearly VHA EHR data from 2005 to 2019, we compared cannabis use disorder trends among patients with and without common psychiatric disorders, including depressive, anxiety, posttraumatic stress, bipolar, and psychotic spectrum disorders. Because of known age differences in the risk of cannabis use disorder (6, 17), we also examined trends in cannabis use disorder diagnoses across these psychiatric disorders by age group (<35, 35–64, and ≥65 years).
METHODS
Sample
Data from January 1, 2005, to December 31, 2019, were obtained through the Veterans Affairs (VA) Corporate Data Warehouse, a data repository for all care provided at VHA facilities or paid for by the VHA. Veterans at least 18 years of age with at least one VHA primary care, emergency department, or mental health visit in a given calendar year were included in the study populations, except those in hospice or palliative care or residing outside the 50 states or Washington, DC. Fourteen study populations were created, one for each year from 2005 to 2014 (N range, 4,332,165–5,383,712) and from 2016 to 2019 (N range, 5,508,670–5,657,277). Because of the 2015 transition from ICD-9-CM to ICD-10-CM and methodological effects on rates across this transition, as described in detail elsewhere (14, 41), we excluded that year. Study approvals and waivers of or exemptions from informed consent were granted by the institutional review boards of New York State Psychiatric Institute, the VA Puget Sound Health Care System, and the VA New York Harbor Healthcare System.
Measures
Cannabis use disorder diagnoses.
The primary outcome was a cannabis use disorder diagnosis made by a provider during at least one outpatient or inpatient encounter within a calendar year. We used ICD-9-CM for the period from 2005 to 2014 (305.2X, abuse; 304.3X, dependence) and ICD-10-CM for the period from 2016 to 2019 (F12.1X, abuse; F12.2X, dependence). We combined abuse and dependence because their criteria are unidimensional. As was done previously (14, 41), remission and unspecified cannabis use disorder diagnoses were excluded.
Psychiatric disorders.
ICD-9-CM or ICD-10-CM psychiatric disorder diagnoses indicated disorders in five categories: depressive disorders, anxiety disorders, PTSD, bipolar disorders, and psychotic spectrum disorders (for ICD codes, see Table S1 in the online supplement). All codes indicating disorders in remission were excluded. The five categories were selected because they include the most common psychiatric disorders recorded in the VHA EHR. For each category, a dichotomous variable was created indicating whether patients were diagnosed with any of the disorders within that category in a given year. These categories were not mutually exclusive, so patients could be included in more than one category if they met criteria for multiple conditions. These five dichotomous variables were used to create a binary summary variable indicating whether patients were positive for at least one of the five categories within each year (hereafter termed “any psychiatric disorder”). To explore the sensitivity of the findings to comorbidity, we also created five analogous psychiatric disorder categories that were mutually exclusive, with each category including only the subset of patients who were diagnosed with a disorder in that category and not diagnosed with disorders in any of the other four categories.
Covariates.
Covariates included sex (male, female), age group (<35, 35–64, and ≥65 years), and race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other/multiple races, and unknown).
Statistical Analysis
Following our previous work (14), analyses were performed on the overall sample and then stratified by age group (<35, 35–64, and ≥65 years). Demographic characteristics, unadjusted prevalence of cannabis use disorder, and unadjusted prevalence of any psychiatric disorder and the five psychiatric disorder categories are presented for the overall sample and stratified by age group for study years 2005, 2014, 2016, and 2019. As noted above, given the methodological issues created by the 2015 mid-year transition from ICD-9-CM to ICD-10-CM, we excluded that year and examined adjusted trends in cannabis use disorder within two periods: 2005–2014 (ICD-9-CM) and 2016–2019 (ICD-10-CM). To test for changes in cannabis use disorder over time by any psychiatric disorder, multivariable logistic regression models were used that included categorical study year, any psychiatric disorder (yes, no), and an interaction term for any psychiatric disorder and study year, adjusted for sex, race/ethnicity, and age in three categories, as above. Separate multivariable logistic regression models were then run, stratified by age group, adjusting for sex, race/ethnicity, and continuous age. The predicted diagnostic prevalence of cannabis use disorder diagnoses (i.e., adjusted proportions) in each year, the change in prevalence, the difference in those trends between patients with and without any psychiatric disorder and the associated 95% confidence intervals were obtained from the margins command in Stata for the fitted logistic regression model. Confidence intervals were based on standard statistical methods that assume normal sampling distributions. While full-census data such as VHA EHR data do not necessarily require uncertainty estimates, we present them to indicate the precision of our prevalence estimates.
Trends in cannabis use disorder prevalence between the 2005–2014 and 2016–2019 periods were then examined within each of the five diagnostic categories using logistic regression models including study year, adjusted for demographic covariates. Each model was limited to patients diagnosed with the specific condition to examine within-group trends. These diagnostic categories were not exclusive, such that patients were included in more than one category if they met criteria for multiple diagnoses. Then, to check the robustness of the findings to potential influences of comorbidity, similar models were run for each of the five categories, using the variables indicating patients with diagnoses only in the specific category and no other categories. Stata, version 17, was used for all analyses.
RESULTS
Psychiatric Disorders and Demographic Characteristics
Prevalences (in 2005 and 2019) of any psychiatric disorder and each of the five specific disorder categories are presented for the overall sample and by age category in Table S2A in the online supplement. From 2005 to 2019, the prevalence of any psychiatric disorder increased from 19.0% to 29.2%. The most common diagnoses were depressive disorders (2005: 10.5%; 2019: 16.1%) and PTSD (2005: 6.2%; 2019: 14.8%). Overall and age-stratified demographic characteristics (in 2005 and 2019) are presented for the entire sample and for patients with and without psychiatric disorders in Table S2B in the online supplement. In the overall sample, patients were primarily male (2005: 95.0%; 2019: 90.8%) and non-Hispanic White (2005: 78.7%; 2019: 70.3%). About half were age 65 or older (2005: 49.2%; 2019: 51.9%). In both periods, patients with and without psychiatric disorders were primarily male (2005: 92.2% and 95.7%, respectively; 2019: 85.6% and 93.0%, respectively), and non-Hispanic White (2005: 75.9% and 79.3%, respectively; 2019: 65.2% and 72.5%, respectively).
Cannabis Use Disorder
In the overall sample, the adjusted prevalence of ICD-9-CM cannabis use disorder diagnoses increased twofold, from 0.85% in 2005 to 1.87% in 2014. As described and discussed in detail previously (14, 41), the ICD-9-CM to ICD-10-CM transition led to an artifactual decrease in cannabis use disorder prevalence in 2016 as a result of provider coding practices and EHR procedures. Between 2016 and 2019, the adjusted prevalence of ICD-10-CM cannabis use disorder increased from 1.62% to 1.92%.
Overall Trends in Prevalence of Cannabis Use Disorder Among Veterans With and Without Any Psychiatric Disorder
2005–2014.
In 2005, the prevalence of ICD-9-CM cannabis use disorder was greater among patients with any psychiatric disorder than among patients without any psychiatric disorder (2.48% and 0.35%, respectively) (Table 1, Figure 1). Over time, the adjusted overall prevalence of cannabis use disorder diagnoses increased among patients with and without any psychiatric disorder. Among patients with any psychiatric disorder, the prevalence of ICD-9-CM cannabis use disorder diagnoses increased by 2.22%, reaching 4.70% in 2014. Among patients without any psychiatric disorder, the prevalence of ICD-9-CM cannabis use disorder diagnoses increased by 0.31%, reaching 0.66% in 2014. The increase in ICD-9-CM cannabis use disorder diagnoses among patients with any psychiatric disorder was significantly greater than for patients without these disorders (difference in prevalence change, 1.91%, 95% CI=1.87–1.96).
Table 1.
Overall and Age-Stratified Change in the Diagnostic Prevalence of CUD by Any Psychiatric Disordera in VA patients, 2005–2019
| Adjusted Prevalenceb | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ICD-9-CM CUD diagnoses | ICD-10-CM CUD diagnoses | |||||||||||
| 2005 | 2014 | Change | 95% CI | 2016 | 2019 | Change | 95% CI | |||||
| Any Psychiatric Disorder | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | ||||
| Overall | ||||||||||||
| No | 0.35 | 0.34–0.35 | 0.66 | 0.65–0.66 | 0.31 | 0.30–0.32 | 0.51 | 0.50–0.51 | 0.57 | 0.56–0.58 | 0.06 | 0.05–0.07 |
| Yes | 2.48 | 2.45–2.51 | 4.70 | 4.67–4.74 | 2.22 | 2.18–2.27 | 4.28 | 4.25–4.31 | 4.68 | 4.65–4.71 | 0.40 | 0.36–0.44 |
| Difference in prevalence | 2.13 | 2.10–2.16 | 4.05 | 4.02–4.08 | 1.91 | 1.87–1.96 | 3.77 | 3.74–3.81 | 4.11 | 4.08–4.14 | 0.34 | 0.29–0.38 |
| Age Groups | ||||||||||||
| <35 | ||||||||||||
| No | 0.57 | 0.53–0.61 | 1.01 | 0.98–1.05 | 0.44 | 0.39–0.50 | 0.89 | 0.86–0.93 | 0.93 | 0.89–0.96 | 0.04 | −0.01–0.08 |
| Yes | 5.56 | 5.53–5.80 | 9.67 | 9.54–9.81 | 4.11 | 3.84–4.38 | 9.28 | 9.15–9.41 | 9.75 | 9.62–9.88 | 0.47 | 0.29–0.65 |
| Difference in prevalence | 4.99 | 4.76–5.23 | 8.66 | 8.52–8.80 | 3.66 | 3.39–3.94 | 8.39 | 8.25–8.52 | 8.82 | 8.69–8.96 | 0.43 | 0.24–0.62 |
| 35–64 | ||||||||||||
| No | 0.69 | 0.67–0.70 | 1.13 | 1.11–1.15 | 0.44 | 0.42–0.46 | 0.82 | 0.80–0.83 | 0.81 | 0.79–0.82 | −0.01 | −0.03–0.01 |
| Yes | 4.14 | 4.08–4.19 | 6.99 | 6.93–7.05 | 2.85 | 2.78–2.93 | 6.04 | 5.99–6.10 | 6.39 | 6.34–6.44 | 0.35 | 0.27–0.43 |
| Difference in prevalence | 3.45 | 3.39–3.50 | 5.86 | 5.80–5.92 | 2.41 | 2.33–2.49 | 5.23 | 5.17–5.28 | 5.59 | 5.53–5.64 | 0.36 | 0.28–0.44 |
| >65 | ||||||||||||
| No | 0.02 | 0.02–0.02 | 0.19 | 0.18–0.19 | 0.17 | 0.16–0.17 | 0.17 | 0.17–0.18 | 0.30 | 0.29–0.31 | 0.13 | 0.12–0.14 |
| Yes | 0.16 | 0.15–0.18 | 1.16 | 1.14–1.18 | 0.99 | 0.96–1.02 | 1.27 | 1.24–1.29 | 2.04 | 2.00–2.07 | 0.77 | 0.73–0.81 |
| Difference in prevalence | 0.14 | 0.13–0.16 | 0.97 | 0.95–1.00 | 0.83 | 0.80–0.86 | 1.10 | 1.07–1.12 | 1.74 | 1.70–1.77 | 0.64 | 0.60–0.68 |
Dichotomous psychiatric summary variable indicating if patients were positive for any disorder from one or more of the 5 categories (depressive disorders, anxiety disorders, PTSD, bipolar disorders, psychotic-spectrum disorders) each year, 2005–2014 and 2016–2019.
Models include year, mental health condition, year X mental health condition, sex, race/ethnicity, continuous age.
Note: Bolded values indicate statistically significant differences between those with psychiatric disorders versus those without psychiatric disorders.
Figure 1.
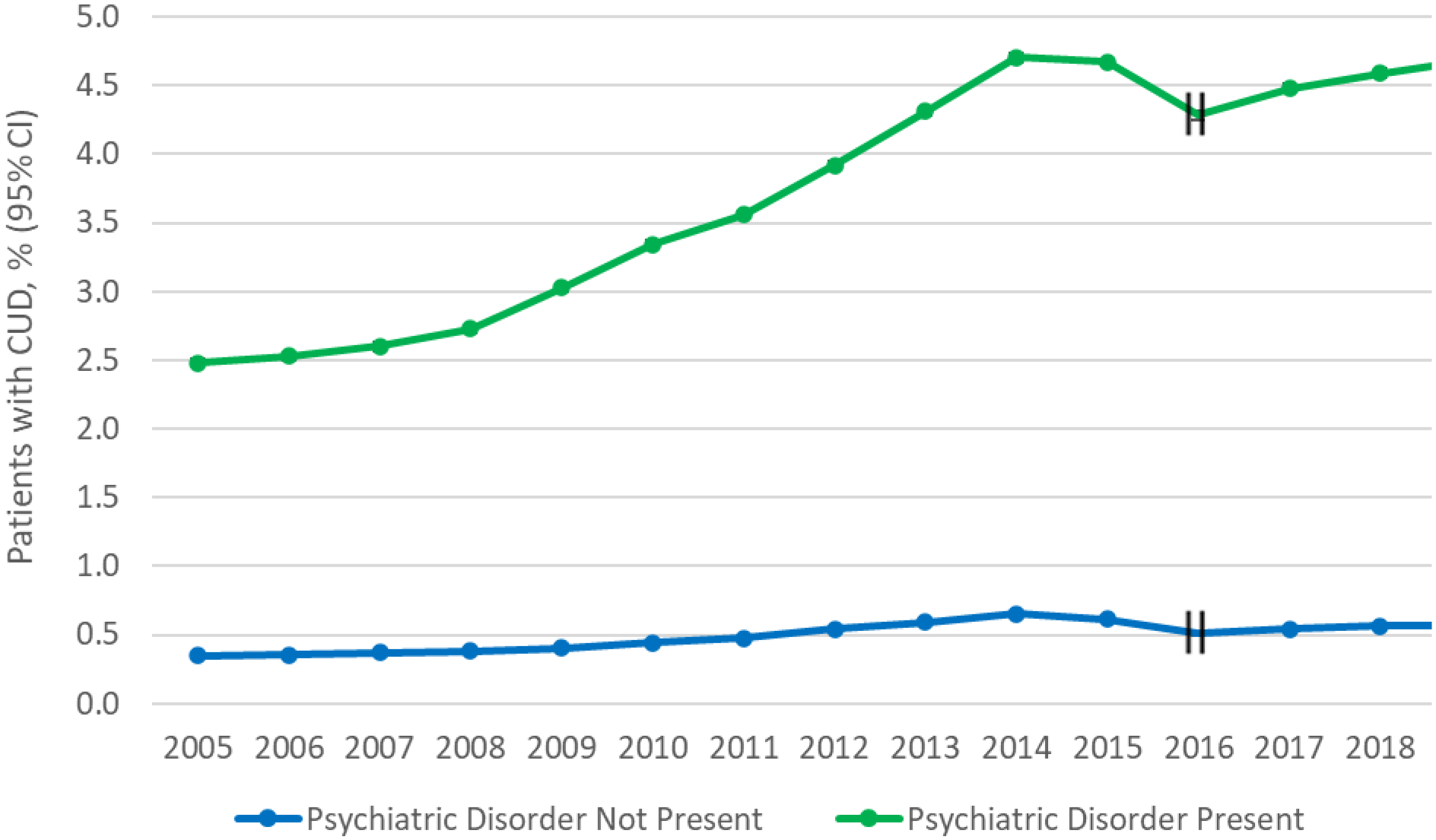
Overall Trends in Prevalence of CUD by Any Psychiatric Disordera in VA Patients, 2005–2019
aDichotomous psychiatric summary variable indicating if patients were positive for any disorder from ≥1 of the 5 categories (depressive disorders, anxiety disorders, PTSD, bipolar disorders, psychotic-spectrum disorders) each year, 2005–2014 and 2016–2019.
Error bars indicate 95% confidence intervals (95% CI). In cases of narrow 95% CI, error bars may be difficult to visualize.
Hash marks at 2015 indicate that this year was not included in models due to a change in ICD coding.
2016–2019.
In 2016, the prevalence of ICD-10-CM cannabis use disorder was greater among patients with any psychiatric disorder than among patients without any psychiatric disorder (4.28% and 0.51%, respectively) (Table 1, Figure 1). Over time, the adjusted overall prevalence of ICD-10-CM cannabis use disorder diagnoses increased among patients with and without any psychiatric disorder. Among patients with any psychiatric disorder, the prevalence of ICD-10-CM cannabis use disorder diagnoses increased by 0.40%, reaching 4.68% in 2019. Among patients without any psychiatric disorder, the prevalence of ICD-10-CM cannabis use disorder diagnoses increased by 0.06%, reaching 0.57% in 2019. The increase in ICD-9-CM cannabis use disorder diagnoses among patients with any psychiatric disorder was significantly greater than for patients without these disorders (difference in prevalence change, 0.34% (95% CI=0.29–0.38).
Age-Stratified Trends in Prevalence of Cannabis Use Disorder Among Veterans With and Without Any Psychiatric Disorder
2005–2014.
Across all age groups, patients with any psychiatric disorder had significantly greater increases in prevalence of cannabis use disorder diagnoses than patients without any psychiatric disorders (Table 1; see also Figure S1A–C in the online supplement). Between 2005 and 2014, the greatest absolute increases among patients with any psychiatric disorder occurred among those under age 35 (difference in prevalence change=3.66%, 95% CI=3.39–3.94), followed by those ages 35–64 (difference in prevalence change=2.41%, 95% CI=2.33–2.49) and those age 65 or older (difference in prevalence change=0.83%, 95% CI=0.80–0.86).
2016–2019.
The greatest differences in absolute increases in percent change in prevalence of cannabis use disorder diagnoses between patients with and without any psychiatric disorder occurred among those age 65 or older (difference in prevalence change=0.64%, 95% CI=0.60–0.68), followed by those under age 35 (difference in prevalence change=0.43%, 95% CI=0.24–0.62) and those ages 35–64 (difference in prevalence change=0.36%, 95% CI=0.28–0.44) (Table 1; see also Figure S1A–C in the online supplement).
Trends in Prevalence of Cannabis Use Disorder Among Veterans With Specific Psychiatric Disorders
2005–2014.
Within the five psychiatric disorder categories that were not mutually exclusive (i.e., with comorbidity between the categories permitted), the prevalence of ICD-9-CM cannabis use disorder ranged considerably (Table 2A, Figure 2A), with the lowest prevalences among patients in the depressive disorder category (2005: 3.16%; 2014: 5.74%) and the highest prevalences in the bipolar disorder (2005: 6.65%; 2014: 12.31%) and psychotic spectrum disorder categories (2005: 5.07%; 2014: 11.08%). The increases in ICD-9-CM cannabis use disorder diagnosis prevalence between 2005 and 2014 were significant within all five of the categories, with the smallest increase among patients with depressive disorders (2.58%, 95% CI=2.51–2.65), followed by those with PTSD (2.93%, 95% CI=2.84–3.02) and those with anxiety disorders (3.49%, 95% CI=3.38–3.60). The increases in cannabis use disorder prevalence were greater among those with bipolar disorders (5.66%, 95% CI=5.40–5.91) or psychotic spectrum disorders (6.01%, 95% CI=5.79–6.23).
Table 2.
Change in the Predicted Diagnostic Prevalence of CUD by 5 Categories of Psychiatric Disorders in VA patients, 2005–2019
| 2a. Categories not mutually exclusive; comorbid cases included | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predicted Prevalence of ICD-9-CM CUD diagnoses, 2005–2014a | Predicted Prevalence of ICD-10-CM CUD diagnoses, 2016–2019a | |||||||||||
| 2005 | 2014 | Change | 95% CI | 2016 | 2019 | Change | 95% CI | |||||
| Disorder categories | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | ||||
| Depressive disorders | 3.16 | 3.11–3.21 | 5.74 | 5.69–5.79 | 2.58 | 2.51–2.65 | 5.42 | 5.37–5.48 | 5.87 | 5.82–5.92 | 0.44 | 0.37–0.51 |
| Anxiety disorders | 2.76 | 2.68–2.84 | 6.25 | 6.18–6.33 | 3.49 | 3.38–3.60 | 6.14 | 6.06–6.21 | 6.71 | 6.65–6.78 | 0.58 | 0.48–0.67 |
| PTSD | 3.19 | 3.13–3.26 | 6.12 | 6.06–6.18 | 2.93 | 2.84–3.02 | 5.66 | 5.61–5.72 | 6.33 | 6.27–6.38 | 0.66 | 0.59–0.74 |
| Bipolar disorders | 6.65 | 6.47–6.83 | 12.31 | 12.13–12.49 | 5.66 | 5.40–5.91 | 12.18 | 12.00–12.37 | 14.38 | 14.19–14.57 | 2.20 | 1.93–2.46 |
| Psychotic-spectrum disorders | 5.07 | 4.94–5.20 | 11.08 | 10.90–11.26 | 6.01 | 5.79–6.23 | 11.21 | 11.02–11.40 | 14.23 | 14.01–14.44 | 3.01 | 2.72–3.30 |
| 2b. Categories mutually exclusive; comorbid cases excludedb | ||||||||||||
| Depressive disorders | 2.52 | 2.47–2.58 | 4.24 | 4.17–4.30 | 1.71 | 1.62–1.80 | 3.72 | 3.65–3.78 | 3.80 | 3.73–3.87 | 0.08 | −0.01–0.18 |
| Anxiety disorders | 1.05 | 0.97–1.13 | 2.51 | 2.43–2.60 | 1.46 | 1.34–1.58 | 2.16 | 2.08–2.24 | 2.20 | 2.13–2.27 | 0.04 | −0.07–0.15 |
| PTSD | 1.92 | 1.85–1.99 | 3.08 | 3.01–3.15 | 1.16 | 1.06–1.27 | 2.65 | 2.59–2.71 | 2.81 | 2.75–2.86 | 0.15 | 0.07–0.24 |
| Bipolar disorders | 5.16 | 4.96–5.37 | 8.26 | 8.02–8.49 | 3.09 | 2.79–3.40 | 7.24 | 7.01–7.47 | 8.53 | 8.28–8.79 | 1.29 | 0.95–1.64 |
| Psychotic-spectrum disorders | 3.22 | 3.09–3.35 | 5.93 | 5.73–6.14 | 2.71 | 2.47–2.95 | 5.29 | 5.09–5.49 | 7.06 | 6.81–7.31 | 1.77 | 1.45–2.09 |
Models include year, psychiatric disorder-only variables, sex, race/ethnicity, and categorical age.
Only each of the other four disorder categories.
Note: Bolded values indicate statistically significant change in prevalence of CUD from 2005 to 2014 and 2016–2019.
Figure 2a.
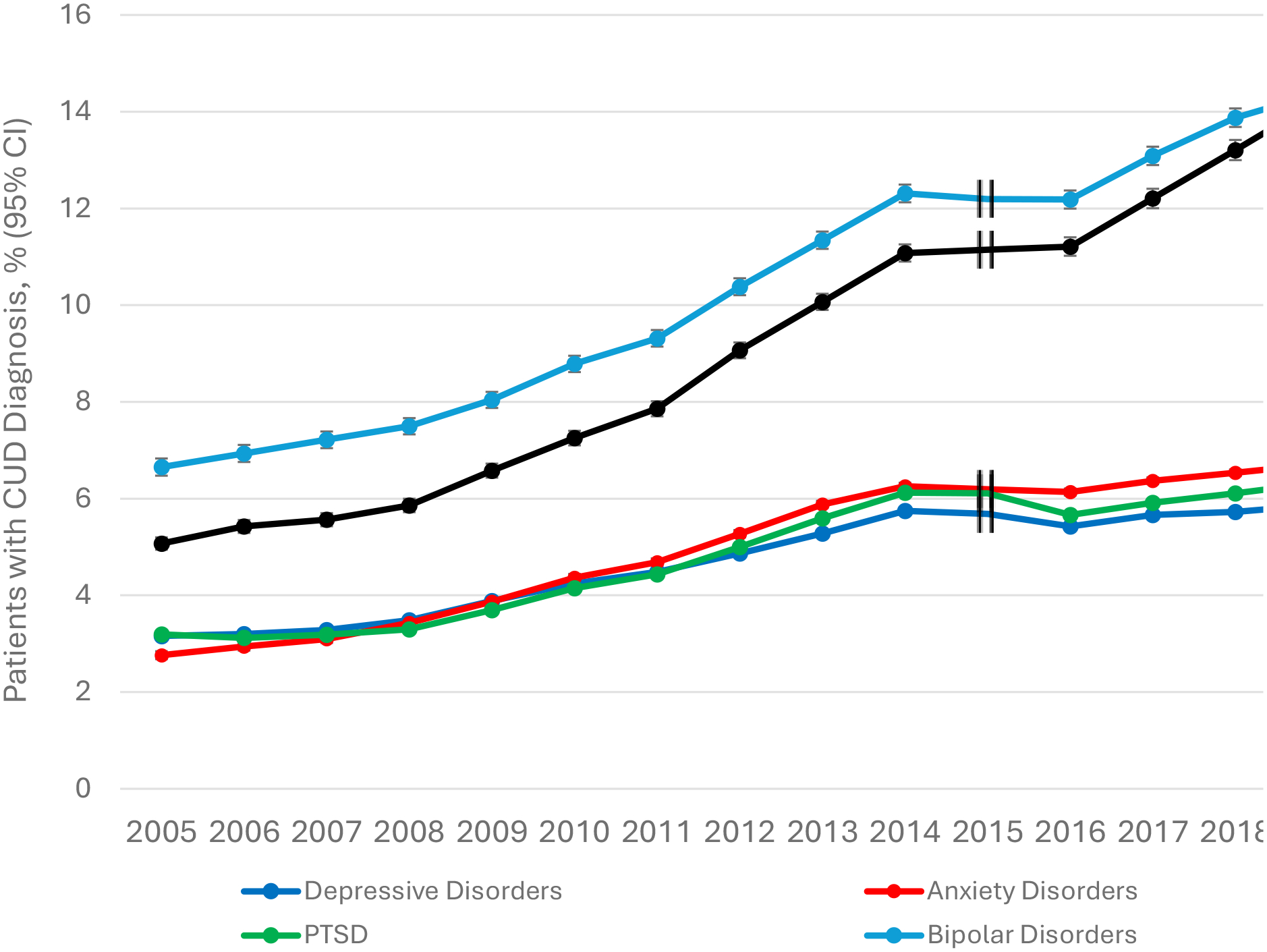
Overall Trends in Prevalence of CUD by 5 Categories of Psychiatric Disorders that are not mutually exclusive (comorbid cases included) in VA patients, 2005–2019.
Error bars indicate 95% confidence intervals (95% CI). In cases of narrow 95% CI, error bars may be difficult to visualize.
Hash marks at 2015 indicate that this year was not included in models due to a change in ICD coding.
Using the five psychiatric disorder categories that were mutually exclusive (indicating only the subset of patients in each category who had no comorbidity with the other four categories) (Table 2B, Figure 2B), the overall prevalences of ICD-9-CM and ICD-10-CM cannabis use disorder were lower than when the comorbid cases were included. However, cannabis use disorder prevalence increased significantly among patients within each of the five specific non-comorbid-disorder categories.
2016–2019.
Within the five psychiatric disorder categories defined as non–mutually exclusive (i.e., with comorbidity between the categories permitted), the prevalence of ICD-10-CM cannabis use disorder ranged considerably (Table 2A, Figure 2A), although the ranking of cannabis use disorder prevalence by disorder categories was similar to the 2005–2014 period. The lowest prevalence of ICD-10-CM cannabis use disorder was among patients in the depressive disorder category (2016: 5.42%; 2019: 5.87%). The highest prevalences were in the bipolar disorder (2016: 12.18%; 2019: 14.38%) and psychotic spectrum disorder categories (2016: 11.21%; 2019: 14.23%). Increases in ICD-10-CM cannabis use disorder prevalence between 2016 and 2019 were smallest among patients with depressive disorders (0.44%, 95% CI=0.37–0.51), followed by anxiety disorders (0.58%, 95% CI=0.48–0.67) and PTSD (0.66%, 95% CI=0.59–0.74). Increases in cannabis use disorder prevalence were greatest among patients with bipolar disorders (2.20%, 95% CI=1.93–2.46) and psychotic spectrum disorders (3.01%, 95% CI=2.72–3.30).
When the five psychiatric disorder categories that were mutually exclusive were used, increases in ICD-10-CM cannabis use disorder prevalence among patients with depressive or anxiety disorders were slight and not significantly different from zero (Table 2B, Figure 2B). However, the prevalence of ICD-10-CM cannabis use disorder increased significantly among patients with PTSD, bipolar disorders, and psychotic spectrum disorders.
Age-Stratified Trends in Prevalence of Cannabis Use Disorder Among Veterans by Specific Disorder Categories
2005–2014.
Cannabis use disorder prevalence among patients with each of the disorder categories increased across age categories, with the greatest increases observed among patients under age 35, followed by those ages 35–64 and those age 65 or older (see Table S3 and Figure S2A–C in the online supplement).
2016–2019.
Cannabis use disorder prevalence among patients with depressive disorders and anxiety disorders increased among those ages 35–64 and those age 65 or older, but not among those under age 35 (see Table S3 and Figure S2A–C in the online supplement). Cannabis use disorder prevalence among patients with PTSD, bipolar disorders, and psychotic spectrum disorders increased among patients across all age groups.
DISCUSSION
We used VHA EHR data to examine overall and age-specific differences in time trends in the annual prevalence of cannabis use disorder among VHA patients with and without psychiatric disorders over two periods (2005–2014 and 2016–2019). Cannabis use disorder rates more than doubled among all VHA patients from 2005 to 2019, with disproportionately greater increases among patients with psychiatric disorders compared to those without. Among patients with psychiatric disorders, the greatest disparities were observed among those with bipolar and psychotic spectrum disorders. Trends also varied by age group: disparities in cannabis use disorder rates between patients with and without psychiatric disorders were greatest among veterans under age 35 between 2005 and 2014 but greatest among those age 65 or older between 2016 and 2019. Altogether, our findings show changes over time in the vulnerability of certain cannabis-using populations to cannabis use disorder—namely, individuals with psychiatric disorders—and identify age groups at higher risk that need to be closely monitored for cannabis use disorder.
The increasing prevalence of cannabis use disorder in the overall VHA patient population reported in this study generally supports previous analyses of VHA samples (14) and some nationally representative U.S. survey reports (9, 42–44). Our finding that increasing prevalence of cannabis use disorder was disproportionately greater among veterans with psychiatric disorders compared to other patients contributes novel findings to a small literature that has limitations, including analysis of cannabis use without cannabis use disorder (45–48); a focus mainly on mood, anxiety (45–47), and psychotic disorders (48) but not PTSD or bipolar disorders; and rarely reporting estimated changes in prevalence of cannabis use disorder among individuals with psychiatric conditions.
In the analyses in which comorbidity between the examined psychiatric disorder categories was permitted, the prevalence of cannabis use disorder diagnoses increased disproportionately among patients diagnosed with each of the five psychiatric disorder categories during both study periods compared to patients without psychiatric disorders. When only non-comorbid cases were examined, results showed similar trends, albeit with a few exceptions. Notably, the disproportionate increases in the prevalence of cannabis use disorder diagnoses were particularly striking among individuals with what may be the most severe conditions—bipolar and psychotic spectrum disorders. Our results on disproportionate increases in comorbidity of cannabis use disorder and psychotic spectrum disorders are consistent with previous findings from a study of self-reported psychotic diagnoses in the general population (48). However, our finding on patients with bipolar disorders is, to our knowledge, the first reported time trend for comorbidity of cannabis use disorder with these disorders. With greater legalization of recreational cannabis use and increased availability, patients with bipolar or psychotic spectrum disorders may be using cannabis in an attempt to self-medicate, even though evidence suggests that this is inadvisable (31, 32).
From 2005 to 2014, differences in cannabis use disorder rates between patients with and without psychiatric disorders were greatest among veterans under age 35. However, from 2016 to 2019, these trends shifted, with the greatest differences in cannabis use disorder rates observed among veterans age 65 or older. This may be partly driven by the dramatic rise in recent years in cannabis use among U.S. adults age 65 or older compared to younger age groups (49, 50). Additionally, many Vietnam-era veterans, now older adults, continue to experience high rates of psychiatric disorders, including PTSD (51), which is now a legally authorized indication for treatment with cannabis in many U.S. states and for which self-medication with cannabis is common (52). Future studies need to examine whether changing state cannabis laws are differentially influencing patients with and without psychiatric disorders overall, as well as those with specific psychiatric diagnoses.
Our study has several limitations. First, VHA patients are largely White middle-aged males with high rates of medical disorders (53). Our findings may not be generalizable to veterans receiving care outside the VHA, to women, or to the general population, although our trend results are largely consistent with other general population findings (45–47). Additionally, as with other studies using EHR data, diagnoses were based on patient-encounter ICD codes entered by VHA providers rather than on research assessments. Therefore, these diagnoses may include some degree of error relative to structured research diagnostic assessments. While providers may be more likely to note diagnoses of more severe or conspicuous conditions, diagnostic disparities could have arisen based on the presence or absence of psychiatric disorders, or the severity of any psychiatric disorders. Second, the transition from ICD-9-CM to ICD-10-CM necessitated our examining trends within two periods: 2005–2014 and 2016–2019. Recording practices for some diagnoses are likely to have affected the prevalence estimates of cannabis use disorder (14, 41) as well as of some psychiatric disorders. Additionally, the statistical models employed may not have fully addressed nonindependence between data points, as patients could have been included in more than one year. This could potentially have an impact on precision estimates, for example, confidence intervals. However, in this study, our utilization of full-census data rendered confidence intervals unnecessary. Third, some psychiatric disorders may be of interest (e.g., attention deficit hyperactivity disorder) but were outside the scope of the present study. Fourth, while results from these analyses suggest possible increased vulnerability to cannabis use disorder among veterans with psychiatric disorders, our models were not designed to account for temporality. Considering the complex and potentially bidirectional relationship between cannabis use disorder and psychiatric disorders, additional retrospective and prospective cohort studies are needed that can account for temporality. Finally, the VHA EHR does not include measures of cannabis use such as frequency, route of administration, and motive for use (recreational vs. medical); therefore, we cannot assess whether these factors affected the observed trends.
CONCLUSIONS
During a period of increasing cannabis use and cannabis use disorder in the United States, the prevalence of cannabis use disorder was disproportionally increased among VHA patients with psychiatric disorders, especially among those with more severe psychiatric disorders. Despite evidence of potential harms from cannabis use, U.S. adults have become increasingly likely to perceive cannabis use as harmless (54, 55) and useful for treating conditions such as stress, anxiety, and depression (29). However, individuals with comorbid cannabis use disorder and psychiatric disorders are at increased risk of functional impairments and other harms (4–6).
Consequently, greater public health and clinical efforts are needed to systematically monitor risky cannabis use and cannabis use disorder and to develop preventive and harm reduction strategies in these cannabis-using populations.
Supplementary Material
Figure 2b.
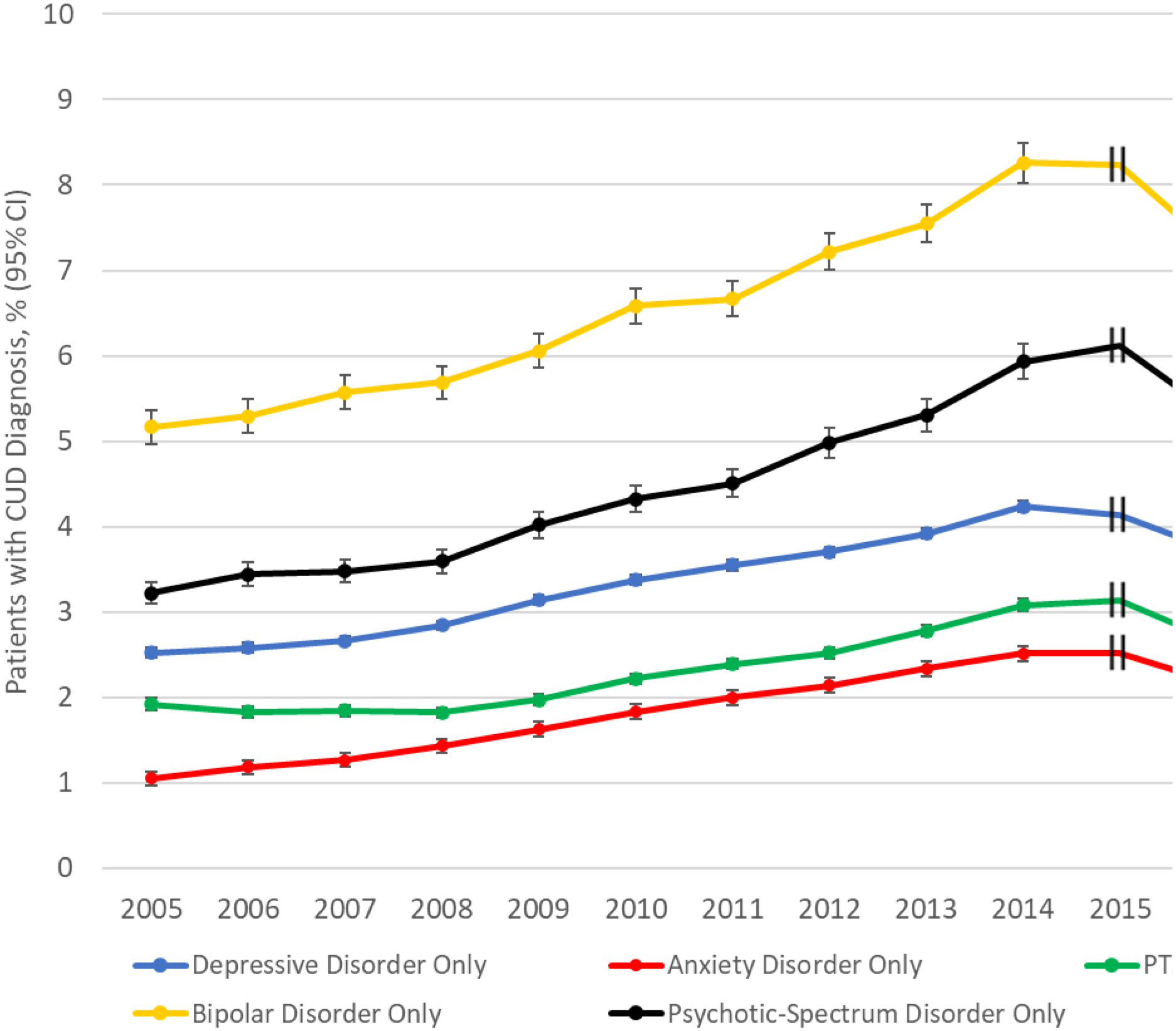
Overall Trends in Prevalence of CUD by 5 Categories of Psychiatric Disorders that are mutually exclusive (comorbid cases excluded) in VA patients, 2005–2019
Error bars indicate 95% confidence intervals (95% CI). In cases of narrow 95% CI, error bars may be difficult to visualize.
Hash marks at 2015 indicate that this year was not included in models due to a change in ICD coding.
Acknowledgments
Supported by NIDA grant R01DA048860 (principal investigator, Dr. Hasin), NIDA grant K23DA057417 (principal investigator, Dr. Livne), New York State Psychiatric Institute, and the Veterans Administration Center for Excellence in Substance Addiction Treatment and Education.
Dr. Saxon receives royalties from UpToDate. Dr. Hasin has received support from Syneos Health.The other authors report no financial relationships with commercial interests.
REFERENCES
- 1.Hall W, Degenhardt L: Adverse health effects of non-medical cannabis use. Lancet 2009; 374:1383–1391 [DOI] [PubMed] [Google Scholar]
- 2.Volkow ND, Baler RD, Compton WM, et al. : Adverse health effects of marijuana use. N Engl J Med 2014; 370:2219–2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Memedovich KA, Dowsett LE, Spackman E, et al. : The adverse health effects and harms related to marijuana use: an overview review. CMAJ Open 2018; 6:E339–E346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leung J, Chan GCK, Hides L, et al. : What is the prevalence and risk of cannabis use disorders among people who use cannabis? A systematic review and meta-analysis. Addict Behav 2020; 109: 106479. [DOI] [PubMed] [Google Scholar]
- 5.Gutkind S, Fink DS, Shmulewitz D, et al. : Psychosocial and health problems associated with alcohol use disorder and cannabis use disorder in US adults. Drug Alcohol Depend 2021; 229:109137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hasin DS, Kerridge BT, Saha TD, et al. : Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: findings from the National Epidemiologic Survey on Alcohol and Related Conditions–III. Am J Psychiatry 2016; 173:588–599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Compton WM, Han B, Jones CM, et al. : Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry 2016; 3:954–964 [DOI] [PubMed] [Google Scholar]
- 8.Center for Behavioral Health Statistics and Quality Results from the 2020 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2021. https://www.samhsa.gov/data/ [Google Scholar]
- 9.Hasin DS, Saha TD, Kerridge BT, et al. : Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry 2015; 72:1235–1242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Compton WM, Han B, Jones CM, et al. : Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend 2019; 204:107468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charilaou P, Agnihotri K, Garcia P, et al. : Trends of cannabis use disorder in the inpatient: 2002 to 2011. Am J Med 2017; 130:678–687 [DOI] [PubMed] [Google Scholar]
- 12.Shi Y: Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend 2017; 173: 144–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonn-Miller MO, Harris AHS, Trafton JA: Prevalence of cannabis use disorder diagnoses among veterans in 2002, 2008, and 2009. Psychol Serv 2012; 9:404–416 [DOI] [PubMed] [Google Scholar]
- 14.Hasin DS, Saxon AJ, Malte C, et al. : Trends in cannabis use disorder diagnoses in the US Veterans Health Administration, 2005–2019. Am J Psychiatry 2022; 179:748–757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasin D, Walsh C: Cannabis use, cannabis use disorder, and comorbid psychiatric illness: a narrative review. J Clin Med 2020; 10:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Compton WM, Thomas YF, Stinson FS, et al. : Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2007; 64:566–576 [DOI] [PubMed] [Google Scholar]
- 17.Stinson FS, Ruan WJ, Pickering R, et al. : Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychol Med 2006; 36:1447–1460 [DOI] [PubMed] [Google Scholar]
- 18.Kendler KS, Prescott CA, Myers J, et al. : The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry 2003; 60: 929–937 [DOI] [PubMed] [Google Scholar]
- 19.María-Ríos CE, Morrow JD: Mechanisms of shared vulnerability to post-traumatic stress disorder and substance use disorders. Front Behav Neurosci 2020; 14:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsuang MT, Lyons MJ, Meyer JM, et al. : Co-occurrence of abuse of different drugs in men: the role of drug-specific and shared vulnerabilities. Arch Gen Psychiatry 1998; 55:967–972 [DOI] [PubMed] [Google Scholar]
- 21.Otasowie J: Co-occurring mental disorder and substance use disorder in young people: aetiology, assessment and treatment. BJPsych Adv 2021; 27:272–281 [Google Scholar]
- 22.Mueser KT, Drake RE, Wallach MA: Dual diagnosis: a review of etiological theories. Addict Behav 1998; 23:717–734 [PubMed] [Google Scholar]
- 23.Khantzian EJ: The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry 1997; 4:231–244 [DOI] [PubMed] [Google Scholar]
- 24.Hawn SE, Cusack SE, Amstadter AB: A systematic review of the self-medication hypothesis in the context of posttraumatic stress disorder and comorbid problematic alcohol use. J Trauma Stress 2020; 33:699–708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jefsen OH, Erlangsen A, Nordentoft M, et al. : Cannabis use disorder and subsequent risk of psychotic and nonpsychotic unipolar depression and bipolar disorder. JAMA Psychiatry 2023; 80:803–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonn-Miller MO, Zvolensky MJ, Bernstein A: Marijuana use motives: concurrent relations to frequency of past 30-day use and anxiety sensitivity among young adult marijuana smokers. Addict Behav 2007; 32:49–62 [DOI] [PubMed] [Google Scholar]
- 27.Brodbeck J, Matter M, Page J, et al. : Motives for cannabis use as a moderator variable of distress among young adults. Addict Behav 2007; 32:1537–1545 [DOI] [PubMed] [Google Scholar]
- 28.Wallis D, Coatsworth JD, Mennis J, et al. : Predicting self-medication with cannabis in young adults with hazardous cannabis use. Int J Environ Res Public Health 2022; 19:1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steigerwald S, Cohen BE, Vali M, et al. : Differences in opinions about marijuana use and prevalence of use by state legalization status. J Addict Med 2020; 14:337–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Azcarate PM, Zhang AJ, Keyhani S, et al. : Medical reasons for marijuana use, forms of use, and patient perception of physician attitudes among the US population. J Gen Intern Med 2020; 35: 1979–1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whiting PF, Wolff RF, Deshpande S, et al. : Cannabinoids for medical use: a systematic review and meta-analysis. JAMA 2015; 313: 2456–2473 [DOI] [PubMed] [Google Scholar]
- 32.Stanciu CN, Brunette MF, Teja N, et al. : Evidence for use of cannabinoids in mood disorders, anxiety disorders, and PTSD: a systematic review. Psychiatr Serv 2021; 72:429–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spindle TR, Bonn-Miller MO, Vandrey R: Changing landscape of cannabis: novel products, formulations, and methods of administration. Curr Opin Psychol 2019; 30:98–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mueller RL, Ellingson JM, Bidwell LC, et al. : Are the acute effects of THC different in aging adults? Brain Sci 2021; 11:590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trivedi RB, Post EP, Sun H, et al. : Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health 2015; 105:2564–2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Finnegan A, Randles R: Prevalence of common mental health disorders in military veterans: using primary healthcare data. BMJ Mil Health 2022:e002045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Betancourt JA, Granados PS, Pacheco GJ, et al. : Exploring health outcomes for US veterans compared to non-veterans from 2003 to 2019. Healthcare (Basel) 2021; 9:604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turna J, MacKillop J: Cannabis use among military veterans: a great deal to gain or lose? Clin Psychol Rev 2021; 84:101958. [DOI] [PubMed] [Google Scholar]
- 39.Livne O, Mannes ZL, McDowell YE, et al. : Mental and physical health conditions among US veterans with cannabis use and cannabis use disorders. Curr Addict Rep 2023; 10:441–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mannes ZL, Malte CA, Olfson M, et al. : Increasing risk of cannabis use disorder among US veterans with chronic pain: 2005–2019. Pain 2023; 164:2093–2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hasin DS, Wall MM, Choi CJ, et al. : State cannabis legalization and cannabis use disorder in the US Veterans Health Administration, 2005 to 2019. JAMA Psychiatry 2023; 80:380–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cerda M, Mauro C, Hamilton A, et al. : Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry 2020; 77:165–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hasin DS, Shmulewitz D, Sarvet AL: Time trends in US cannabis use and cannabis use disorders overall and by sociodemographic subgroups: a narrative review and new findings. Am J Drug Alcohol Abuse 2019; 45:623–643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Compton WM, Grant BF, Colliver JD, et al. : Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA 2004; 291:2114–2121 [DOI] [PubMed] [Google Scholar]
- 45.Gorfinkel LR, Stohl M, Hasin D: Association of depression with past-month cannabis use among US adults aged 20 to 59 years, 2005 to 2016. JAMA Netw Open 2020; 3:e2013802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Halladay J, Woock R, Xu A, et al. : Professor Hippo-on-Campus: developing and evaluating an educational intervention to build mental health literacy among university faculty and staff. J Am Coll Health 2022:1–12 [DOI] [PubMed] [Google Scholar]
- 47.Pacek LR, Weinberger AH, Zhu J, et al. : Rapid increase in the prevalence of cannabis use among people with depression in the United States, 2005–17: the role of differentially changing risk perceptions. Addiction 2020; 115:935–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Livne O, Shmulewitz D, Sarvet AL, et al. : Association of cannabis use-related predictor variables and self-reported psychotic disorders: US adults, 2001–2002 and 2012–2013. Am J Psychiatry 2022; 179:36–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Salas-Wright CP, Vaughn MG, Cummings-Vaughn LA, et al. : Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002–2014. Drug Alcohol Depend 2017; 171:97–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Han BH, Palamar JJ: Trends in cannabis use among older adults in the United States, 2015–2018. JAMA Intern Med 2020; 180:609–611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cypel Y, Schnurr PP, Schneiderman AI, et al. : The mental health of Vietnam theater veterans: the lasting effects of the war: 2016–2017 Vietnam Era Health Retrospective Observational Study. J Trauma Stress 2022; 35:605–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bonn-Miller MO, Vujanovic AA, Drescher KD: Cannabis use among military veterans after residential treatment for posttraumatic stress disorder. Psychol Addict Behav 2011; 25:485–491 [DOI] [PubMed] [Google Scholar]
- 53.Fink DS, Stohl M, Mannes ZL, et al. : Comparing mental and physical health of US veterans by VA healthcare use: implications for generalizability of research in the VA electronic health records. BMC Health Serv Res 2022; 22:1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pacek LR, Mauro PM, Martins SS: Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend 2015; 149:232–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Steigerwald S, Wong PO, Khorasani A, et al. : The form and content of cannabis products in the United States. J Gen Intern Med 2018; 33: 1426–1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


