Abstract
Introduction
The goal of this review is to highlight the significance of dental health during pregnancy, carefully investigate how it affects the health of both the mother and the fetus, and provide practical prevention strategies and therapeutic choices. The main goal is to increase awareness of potential dental problems during pregnancy, understand their effects on the expectant mothers and the fetus's health, and outline practical prevention and management techniques.
Data sources
Conduct a rapid literature search using databases focusing on papers published in English within the last ten years, such as PubMed, Google Scholar, and other relevant platforms from 1st September to 1st October 2023. Use appropriate keywords and search terms related to dental problems, pregnancy, dental care in Bangladesh, and related topics. Include articles published in peer-reviewed journals, books, reports, and official documents.
Study selection
Studies selected on common pregnancy-related dental issues include gingivitis, periodontitis, tooth erosion, xerostomia, tooth decay, and pregnancy tumours. The prevention measures are conditions include regular dental check-ups, maintaining good oral hygiene, and professional cleanings. Treatment options range from scaling and root surface instrumentation to dental restorations and surgical removal, if necessary.
Conclusion
The different dental problems that may develop during pregnancy along with their possible effects on oral health and general wellbeing. Underscores the importance of prioritizing dental care during pregnancy to ensure the well-being of both the mother and the developing baby.
Clinical significance
Dental issues that arise during pregnancy affect both the mother and the fetus, and if left untreated, can result in pain, swelling, and even tooth loss. Recent studies suggest a connection between periodontal disease and unfavourable pregnancy outcomes, emphasizing the importance of precise dental care throughout pregnancy. To minimize hazards and advance general well-being, it is essential to give oral health priority throughout pregnancy. For effective management, routine exams, preventative measures, and oral hygiene practices are crucial. Dental professionals are crucial in helping expecting mothers maintain their best oral health for the sake of both the mother and the unborn child.
Keywords: Pregnancy-related oral problems, Oral hygiene, Oral care in pregnancy, dental management during pregnancy
1. Introduction
Females progress through several stages of development before reaching adulthood. Hormone level fluctuation is primarily responsible for ageing and various physiological changes in the female reproductive system [1]. Pregnancy is a life experience that causes the woman to undergo physiological and psychological changes [2]. While the primary attention throughout pregnancy is on the fetus's well-being, it is critical not to disregard the potential impact of pregnancy on maternal dental health [3]. Pregnancy-related dental conditions can occur as a result of hormonal changes, altered immunological responses, and changes in oral hygiene and food habits [4] (see Table 1, Fig. 1, Fig. 2).
Table: 1.
Outcomes, prevention, and treatments for the common oral problems during pregnancy.
| Pregnancy-related oral diseases | Outcomes | Prevention and Treatment |
|---|---|---|
| Gingivitis [9] | Gingival inflammation, and bleeding on probing/brushing. |
|
| ||
| ||
| ||
| ||
| Periodontitis | Teeth can be lost, and the gums can become infected. And has also been associated with poor pregnancy outcomes, including preterm birth and low birth weight [10] |
|
| ||
| ||
| ||
| Tooth erosion | Sensitivity of the teeth [12] |
|
| ||
| ||
| Xerostomia | Dryness of mouth |
|
| ||
| ||
| ||
| Tooth decay | Food accumulation in the cavity cause pain. |
|
| ||
| ||
| Pregnancy tumor(18), (19) [3], | Another name is pyogenic granuloma or Pregnancy epulis. Hyperplastic lesion or overgrowth on gingiva. |
|
| ||
| ||
| ||
|
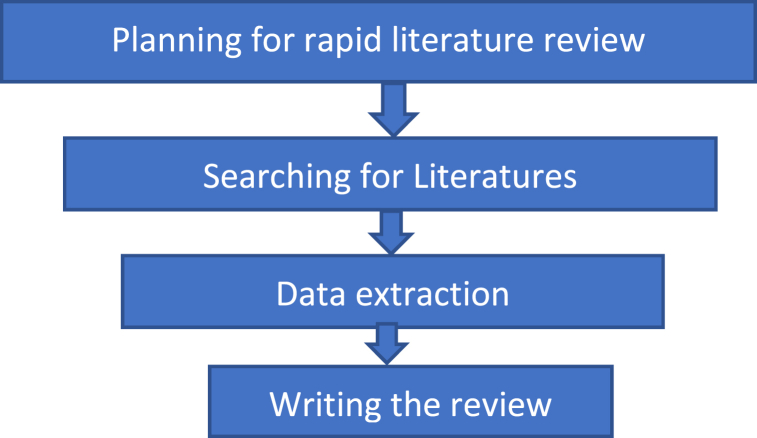
Fig. 1.
The diagram of Methodology for a rapid review article.
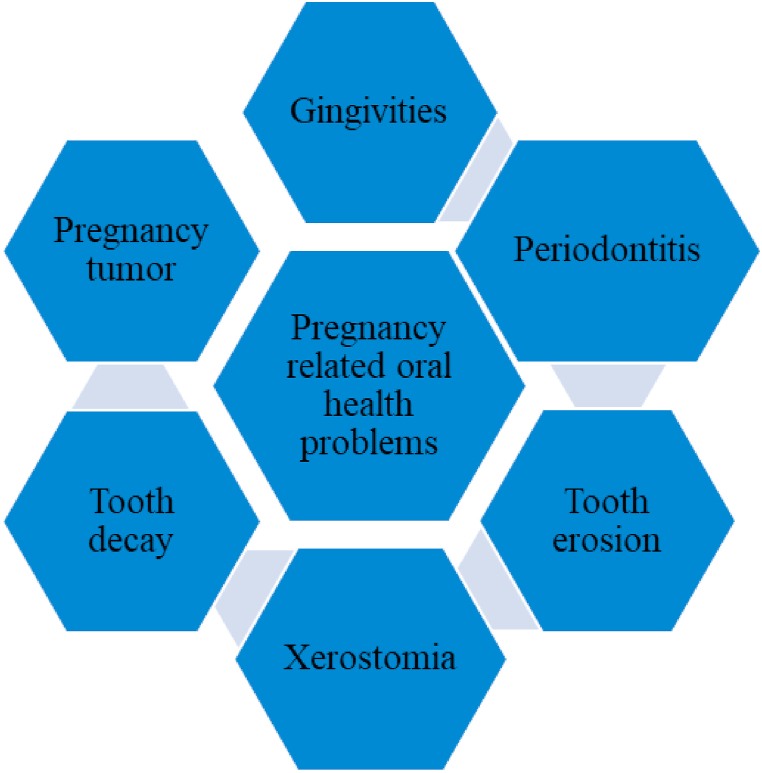
Fig. 2.
Pregnancy-related common oral diseases are.
The link between oral health and general well-being is widely documented, with new research showing the interaction between pregnancy and oral health outcomes [3]. Poor dental health during pregnancy has been linked to negative pregnancy outcomes such as premature birth, low birth weight, and hypertension [3,5]. As a result, it is critical to recognize the unique dental concerns that may arise during pregnancy and to apply effective prevention and management techniques to promote optimal oral health for both the mother and the developing infant [3].
The purpose of this review is to provide an in-depth overview of pregnancy-related dental difficulties, with an emphasis on common issues such as gingivitis, pregnant tumours, tooth erosion, tooth decay, periodontal disease, and xerostomia because they have serious consequences on both the mother's and the fetus's health (Fig. 2). This article wants to increase awareness of the issue, highlight its significance, and offer helpful insights for better healthcare at this crucial time. Each condition's hazards and recommended management techniques are mentioned.
2. Methodology
This review article aims to offer a complete overview of dental disorders associated with pregnancy. This rapid review approach included completing a thorough literature search (Fig. 1) using electronic databases such as PubMed, and Google Scholar from 1st September to 1st October 2023.
The following keywords were used in the search: “pregnancy,” “dental problems,” “oral health,” “gingivitis,” “pregnancy tumours,” “tooth erosion,” “tooth decay,” “periodontal disease,” and “xerostomia.” To ensure validity and relevance, the search was limited to papers published in English within the last ten years.
3. Pregnancy-related common oral diseases are-
Maintaining good dental health throughout pregnancy is vital for both the mother's and the developing baby's overall health. Pregnancy may increase women's susceptibility to periodontal (gum) disease and cavities [6]. Because poor oral health during pregnancy can contribute to poor health outcomes for the mother and baby, dental health may be considered an important element of prenatal care [7,8].
4. Discussion
Pregnancy brings about numerous changes in a woman's body, including hormonal shifts that can affect oral health. Pregnancy-related dental issues can have serious consequences for both the mother and the developing baby's overall health [3]. Several common oral problems that can occur during pregnancy have been emphasized in this article, including gingivitis, periodontitis, tooth erosion, xerostomia, tooth decay, and pregnant tumours [11]. Understanding the results, prevention, and treatment options for these diseases is critical to promoting good oral health during pregnancy.
Gingivitis, characterized by gum inflammation and bleeding, is a common disease during pregnancy. Regular dental check-ups, good oral hygiene, and expert cleanings can all assist in preventing and controlling gingivitis [12]. To control plaque and prevent gingival inflammation, it is critical to emphasize the importance of frequent brushing, flossing, and interdental cleaning.
Untreated periodontitis can result in tooth loss and gum infections [13]. It has also been linked to negative pregnancy outcomes like preterm birth and low birth weight. Gingivitis can be prevented from progressing to periodontitis if diagnosed and treated early [14]. Scaling and root surface instrumentation can be performed safely during the second trimester, and root canal procedures can be explored if necessary.
The illness hyperemesis gravidarum (severe morning sickness), which can induce tooth sensitivity, is frequently linked to problems like tooth erosion. After vomiting, pregnant women should rinse their mouths with water and wait at least an hour before brushing their teeth. Pregnancy-safe dental restorations can be done to fix any erosion-related tooth damage.
A dry mouth, also known as xerostomia [10], can make feel like an oasis in the middle of a desert. But has some solutions, like practicing proper dental hygiene, drinking lots of water to stay hydrated, and abstaining from caffeine, tobacco, and alcohol. Additionally, eating sugar-free gum or alternatives for saliva can be protected from xerostomia [15].
Pregnancy can sometimes bring the appearance of pregnancy tumours [12]. These hyperplastic growths, also known as pyogenic granulomas or pregnancy epulis, can be a cause of untreated periodontitis and bad oral conditions.
To prevent oral problems, Smoking, and tobacco use should be avoided to reduce the risk of pregnancy tumours. By removing plaque and tartar, routine professional cleanings aid in preventing and managing these growths. Managing your hormone levels under your doctor's supervision can also lessen your risk of developing pregnancy oral diseases. Dentists skilled in treating oral disorders during pregnancy may undertake surgical removal, as necessary. If pregnant women observe any unusual gum growths, should speak with a dentist or healthcare practitioner. Socioeconomic and cultural factors also affect pregnancy-related dental problems, and more research is needed to understand and fill the gap of dental problems during pregnancy.
5. Conclusion
The study emphasizes the different dental issues that may arise during pregnancy and their potential consequences on oral health as well as overall health. It highlights how crucial it is to give dental care priority throughout pregnancy to protect both the mother's overall health and the unborn child's development. A potential link between periodontal disease and unfavourable pregnancy outcomes is also shown by the study, highlighting the importance of receiving accurate dental treatment throughout pregnancy. The study suggests prioritizing dental health during pregnancy, including routine exams, preventive measures, and good oral hygiene practices, to reduce risks and increase overall well-being. It also acknowledges the critical role played by dental practitioners in helping expecting moms maintain excellent oral health for the benefit of both the mother and the unborn child.
6. Recommendation
Some suggestions based on the review's findings on pregnancy-related dental issues are listed below:
-
1.
Encourage to do oral health assessments in prenatal care.
-
2.
Guide to maintain good oral hygiene during pregnancy.
-
3.
If necessary both healthcare providers and expectant mothers should be instructed on how to maintain oral health.
-
4.
Community initiatives should be taken to improve pregnant women's dental health.
CRediT authorship contribution statement
Nabhira Aftabi Binte Islam: Writing – review & editing, Writing – original draft, Visualization, Validation, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Atiqul Haque: Supervision.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:Not applicable. Its a review article. So no financial support is required. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Nabhira Aftabi Binte Islam, Email: nabhira22@bsmmu.edu.bd.
Atiqul Haque, Email: atiqulm25@bsmmu.edu.bd, atiqulm26@bsmmu.edu.bd.
References
- 1.Yenen Z., Ataçağ T. Oral care in pregnancy. J. Turk. Ger. Gynecol. Assoc. 2019 Dec;20(4):264–268. doi: 10.4274/jtgga.galenos.2018.2018.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bjelica A., Cetkovic N., Trninic-Pjevic A., Mladenovic-Segedi L. The phenomenon of pregnancy - a psychological view. Ginekol. Pol. 2018;89(2):102–106. doi: 10.5603/GP.a2018.0017. [DOI] [PubMed] [Google Scholar]
- 3.Hemalatha V.T., Manigandan T., Sarumathi T., Aarthi Nisha V., Amudhan A. Dental considerations in pregnancy-a critical review on the oral care. J. Clin. Diagn. Res. JCDR. 2013 May;7(5):948–953. doi: 10.7860/JCDR/2013/5405.2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sajjan P., Pattanshetti J.I., Padmini C., Nagathan V.M., Sajjanar M., Siddiqui T. Oral health related awareness and practices among pregnant women in bagalkot district, Karnataka, India. J Int Oral Health JIOH. 2015 Feb;7(2):1–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Jahan S.S., Hoque Apu E., Sultana Z.Z., Islam M.I., Siddika N. Oral healthcare during pregnancy: its importance and challenges in lower-middle-income countries (LMICs) Int. J. Environ. Res. Publ. Health. 2022 Aug 27;19(17) doi: 10.3390/ijerph191710681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.AlSharief M., Alabdurubalnabi E. Periodontal pathogens and adverse pregnancy outcomes: a narrative review. Life. 2023 Jul;13(7):1559. doi: 10.3390/life13071559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al Agili D.E., Khalaf Z.I. The role of oral and prenatal healthcare providers in the promotion of oral health for pregnant women. BMC Pregnancy Childbirth. 2023 May 3;23(1):313. doi: 10.1186/s12884-023-05654-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naseem M., Khurshid Z., Khan H.A., Niazi F., Zohaib S., Zafar M.S. Oral health challenges in pregnant women: recommendations for dental care professionals. Saudi J Dent Res. 2016 Jul;7(2):138–146. [Google Scholar]
- 9.Knowledge of Oral Health during Pregnancy and Associated Factors Among Pregnant Mothers Attending Antenatal Care at South Omo Zone Public Hospitals. Southern Ethiopia; 2021. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0273795 PLOS ONE [Internet]. [cited 2023 Oct 4]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fakheran O., Keyvanara M., Saied-Moallemi Z., Khademi A. The impact of pregnancy on women's oral health-related quality of life: a qualitative investigation. BMC Oral Health. 2020 Oct 27;20(1):294. doi: 10.1186/s12903-020-01290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han Y.W. Oral health and adverse pregnancy outcomes – what's next? J. Dent. Res. 2011 Mar;90(3):289–293. doi: 10.1177/0022034510381905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agrawal A.A. Gingival enlargements: differential diagnosis and review of literature. World J Clin Cases WJCC. 2015 Sep 16;3(9):779–788. doi: 10.12998/wjcc.v3.i9.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar P., Magon N. Hormones in pregnancy. Niger Med J J Niger Med Assoc. 2012;53(4):179–183. doi: 10.4103/0300-1652.107549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corbella S., Taschieri S., Del Fabbro M., Francetti L., Weinstein R., Ferrazzi E. Adverse pregnancy outcomes and periodontitis: a systematic review and meta-analysis exploring potential association. Quintessence Int Berl Ger. 1985;47(3):193–204. doi: 10.3290/j.qi.a34980. 2016 Mar. [DOI] [PubMed] [Google Scholar]
- 15.Dodds M.W.J., Haddou M.B., Day J.E.L. The effect of gum chewing on xerostomia and salivary flow rate in elderly and medically compromised subjects: a systematic review and meta-analysis. BMC Oral Health. 2023 Jun 20;23:406. doi: 10.1186/s12903-023-03084-x. [DOI] [PMC free article] [PubMed] [Google Scholar]