Abstract
This study compares pain interventions received by nursing home residents with and without dementia. Secondary data analyses of cross-sectional data from 50,673 nursing home residents in New York State were collected by the Minimum Data Set 3.0. Frequency distributions and bivariate analyses with χ2 tests were used to organize and summarize the data. Logistic regression analyses were performed to quantify the relationship between dementia and pain interventions. Our results show that residents with dementia had significantly fewer pain assessments and less reported pain presence than their counterparts. After adjusting for covariates, the results indicate that residents with dementia were significantly less likely to receive pro re nata and nonmedication pain intervention. However, there were no significant differences in scheduled pain medication between the 2 groups. To address the gap, we need more research to design a pain assessment tool that can differentiate severity of pain so that appropriate interventions can be applied.
Keywords: dementia, pain assessment, pain intervention, nursing home, Minimum Data Set 3.0
Introduction
Depending on the study designs, it is estimated that between 41.5% and 80% of nursing home residents have dementia. 1 -4 Individuals with dementia have trouble communicating meaningfully because of memory loss and difficulties in thinking and problem-solving. This declined cognition greatly reduces their self-care ability (activities of daily living [ADL]) including daily routines (eg, grooming, dressing) and their ability to express their care needs. In addition to loss of functional independence, residents with dementia also experience the higher burden of disease.
Nursing home residents frequently have chronic conditions and cognitive impairments, and the prevalence of pain is high (45%-80%) among older adults with or without dementia. 5,6 The burdens of disease among nursing home residents include depression, arthritis, hypertension, a composite of vascular diseases, gastroesophageal reflux disease, congestive heart failure, dementia, and anemia. 7 More specifically, health problems among residents with advanced dementia include skin problems (95%), nutrition/dehydration (85%), psychiatric/behavioral problems (85%), gastrointestinal problems (81%), and infections (80%). 8 Sixty-three percent of residents with advanced dementia recognized pain and 95% of those received medication. 8,9 As diseases progress, Lyketos and associates found that 80% of residents with dementia experience neuropsychiatric symptoms 10 such as physical aggression, agitation, disruptive vocalizations, anxiety, and depression. Residents with dementia having a pain experience with neuropsychiatric symptoms may also engage in challenging behaviors such as psychosis, apathy, or hyperactivities. 9 In order to manage challenging symptoms and behaviors, pharmacological intervention may be required, for example, antipsychotics for agitation or psychosis, β-adrenergic blockers for aggression, and cholinesterase inhibitors for behavioral symptoms. 10
Depending on study design, the prevalence of pain has been estimated to vary from 29% to 83% among residents in long-term care facilities. 11 -14 This pain prevalence is higher than that of older adults living in the community (20%-50%). 12 A previous study indicated that more than 40% of nursing home residents endure persistent pain. Of these, as many as 6.4% were untreated and 32% undertreated. 15 If pain is not properly addressed, there are negative consequences such as depression, insomnia, anxiety, loss of appetite, change in activity, and a lower quality of life. 16
Pain assessment in people with dementia is challenging. Pain is a subjective experience and pain tolerance varies by person. Three methods used to evaluate levels of pain are self-reported, observational, and/or proxy; each has its own challenges. 5 For example, self-reported pain is often problematic for people with dementia as it relates to the level of cognitive impairment. 17 As dementia and other coexisting conditions progress, the individual’s ability to report pain and articulate sites of pain may become more difficult. 5 Consequently, their pain is often undertreated or inadequately treated. 11,18 -20 Other studies examined different aspects of pain and medication management–related issues. For example, Nakanishi and her colleagues reported that residents with dementia in nursing homes were less likely to receive pain management in the last month of life. 21 Neumann and associates examined trends in the administration of “as-needed” medication to inpatients in psychiatric facilities 22 and found residents were more likely to receive pro re nata (PRN, or as needed) medication if they were younger and the afternoon and night shifts changed. Stokes and associates examined factors influencing the use of PRN medication in nursing homes 23 and found higher PRN medication use among residents with lower care needs, recent hospitalizations, and more frequent doses of regularly scheduled medications. In addition, Weiner and Hanlon identified pain management strategies for nursing home residents, in general, 11 which provided a comprehensive review underlying causes of pain, pain management strategies related to levels of pain, and adverse effects of analgesics. These studies contribute to a better understanding of pain medication with the purpose of maximizing therapeutic effect and mitigating pain. To our knowledge, pain interventions among residents with dementia in nursing homes have not been fully studied. Our study aimed to compare pain interventions (scheduled pain medication, PRN pain medication, and nonmedication intervention for pain) between nursing home residents with and without dementia in New York State.
Methods
Study Design
This was a cross-sectional study. Inclusion criteria for the study population mandated that the sample include older adults (aged 65 years) who received care from a nursing home in New York State and had an annual assessment in 2012. The study was approved by the internal review board of the University at Albany.
Data Source
The Minimum Data Set 3.0 (MDS3.0) from 2012 contains assessment forms for each patient residing in a Medicare- and Medicaid-certified nursing home in New York State. For residents with more than one annual assessment, we retained the latest record for the analysis. The data set was provided by the NYS Department of Health; unique resident identifiers were removed before being given to the researchers.
Study Variables
The MDS3.0 included information on age (in years), gender, ADL, comorbidities, pain assessment, and pain interventions. All ADL functional disability measures in MDS3.0 are performance based on a scale from 0 (independent) to 4 (total dependence). For purposes of this study, if a resident’s ADL item was recorded as “activity did not occur during entire 7 days,” that ADL was considered missing. The overall ADL disability was a summary variable including bathing, toileting, dressing, transferring, eating, and personal hygiene. The presence of comorbidities was a dichotomous variable (yes vs no). Dementia status was coded as yes versus no, based on a diagnosis of Alzheimer disease or dementia other than Alzheimer disease. Pain presence (yes vs no) was derived from 3 questionnaires: “Should a pain assessment interview be conducted?” If the answer was yes, we moved to the next question: “Have you had pain (or hurting) at any time in the last 5 days?” If the answer was yes, it means that the residence reported pain presence (yes) versus else (no). The outcome variable under study was pain interventions. Pain intervention options were (1) scheduled pain medication, (2) PRN pain medication, and (3) nonmedication intervention for pain. Nonmedication interventions for pain include heat, therapy, massage, stretching, and muscle release techniques used for muscle spasm or myofascial pain, walkers, or raised chairs used for lower extremity arthritis and carpometacarpal braces used for painful hand osteoarthritis. 9 Although some residents received more than 2 pain intervention options, we focused on each option and coded yes versus no.
Data Analysis
Frequency distributions and bivariate analyses with χ 2 tests were used to organize and summarize the data. Logistic regressions were performed to compare the pain interventions received by nursing home residents with and without dementia while adjusting for age, gender, overall ADL disability, and comorbidity. Analyses were conducted using Statistical Analysis Software, version 9.3 (SAS Institute, Inc, Cary, North Carolina). The significance level was set at α = .05 (2-tailed).
Results
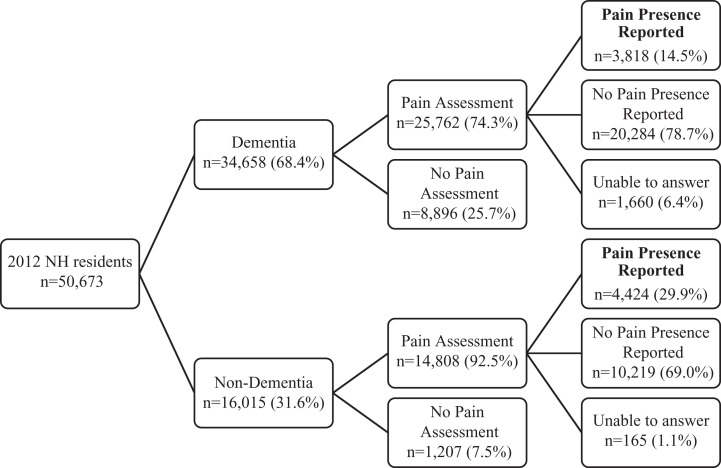
As Figure 1 shows, of the 50,673 nursing home residents in New York State, 34 658 (68.4%) had dementia in 2012. Residents with dementia had significantly fewer pain assessments than those without dementia (74.3% vs 92.5%; P < .0001). Likewise, residents with dementia had significantly less pain presence than their counterparts (14.5% vs 29.9%; P < .0001).
Figure 1.
Flowcharts of pain assessment and pain presence between residents with and without dementia (2012).
Table 1 presents the sociodemographic and selected health conditions of the study population. Of the 8,242 residents, the mean age was 83.2 years; 24.5% were male and 78.1% were white. The average overall ADL disability was 2.3 and a higher score indicates a higher level of disability. Regarding health characteristics, 46.3% had dementia, 79.3% hypertension, 57.2% depression, and 39.4% arthritis. The percentage of residents receiving scheduled pain medication was 71.3%, PRN pain medication 53.1%, and nonmedication intervention for pain 20.1%. In comparison to residents without dementia, residents with dementia were significantly older (85.0 vs 81.7; P < .0001), had a lower proportion of men (22.7% vs 26.0%; P < .0004), and had higher overall ADL disability (2.4 vs 2.2; P < .0001). Regarding health conditions, residents with dementia had lower prevalence of arthritis (41.0% vs 38.2%), cancer (5.1% vs 6.5%), depression (61.5% vs 53.5%), heart failure (24.4% vs 28.1%), and psychotic disorder (9.4% vs 3.7%). For pain intervention, dementia residents had a lower proportion of PRN pain medication (21.5% vs 31.6%; P < .0001) and of nonmedication intervention for pain (8.4% vs 11.7%; P < .0001). There is a total of 6.6% of residents who reported pain but didn’t receive any pain intervention; of these, a higher proportion of dementia residents received no intervention compared to residents without dementia, respectively (3.7% vs 2.9%; P < .0001).
Table 1.
Characteristics of NYS Nursing Home Residents Who Received Pain Assessment and Reported Pain Presence in the Dementia and No-Dementia Groups.
| Characteristics | Totala (N = 8242) | Dementiaa (n = 3818) | No Dementiaa (n = 4424) | P Value | |||
|---|---|---|---|---|---|---|---|
| # | % | # | % | # | % | ||
| Age, mean (SD) | 83.2 | 8.9 | 85.0 | 8.0 | 81.7 | 9.4 | <.0001 |
| Male | 2017 | 24.5 | 866 | 22.7 | 1151 | 26.0 | .0004 |
| White | 6435 | 78.1 | 2891 | 75.7 | 3544 | 80.1 | <.0001 |
| Overall ADL, mean (SD) | 2.3 | 1.0 | 2.4 | 0.9 | 2.2 | 1.0 | <.0001 |
| Health characteristics | |||||||
| Anemia | 2819 | 34.2 | 1299 | 34.0 | 1520 | 34.4 | .75 |
| Arthritis | 3250 | 39.4 | 1567 | 41.0 | 1689 | 38.2 | .008 |
| Cancer | 484 | 5.9 | 196 | 5.1 | 288 | 6.5 | .009 |
| Depression | 4715 | 57.2 | 2349 | 61.5 | 2366 | 53.5 | <.0001 |
| Heart failure | 2177 | 26.4 | 932 | 24.4 | 1245 | 28.1 | .0001 |
| Hypertension | 6537 | 79.3 | 3050 | 79.9 | 3487 | 78.8 | .23 |
| Gastroesophageal | 2923 | 35.5 | 1316 | 34.5 | 1607 | 36.3 | .08 |
| Stroke | 1402 | 17.0 | 649 | 17.0 | 753 | 17.0 | .98 |
| Psychotic disorder | 523 | 6.4 | 360 | 9.4 | 163 | 3.7 | <.0001 |
| Pain intervention | |||||||
| Scheduled pain medication | 5878 | 71.3 | 2713 | 71.1 | 3165 | 71.5 | .63 |
| PRN pain medication | 4378 | 53.1 | 1773 | 46.4 | 2605 | 58.9 | <.0001 |
| Nonmedication intervention for pain | 1657 | 20.1 | 689 | 18.1 | 968 | 21.9 | <.0001 |
| No intervention | 549 | 6.7 | 305 | 8.0 | 244 | 5.5 | <.0001 |
Abbreviations: ADL, activities of daily living; PRN, pro re nata; SD, standard deviation.
aComponents may not sum to totals because of rounding.
The results of multivariate logistic regression analysis in Table 2 indicate dementia residents had significantly lower odds of receiving PRN pain medication (odds ratio [OR] = 0.67, 95% confidence interval [CI] = 0.61-0.73) and nonmedication intervention for pain (OR = 0.77, 95% CI = 0.69-0.87). That being the case, there were no significant differences in scheduled pain medication between the 2 groups.
Table 2.
Multivariate Logistic Regression Results on Pain Intervention in the Dementia and No-Dementia Groups.a
| Outcome | ORb | 95% CI | P Value |
|---|---|---|---|
| Scheduled pain medication | 0.91 | 0.82-1.01 | .07 |
| PRN pain medication | 0.67 | 0.61-0.73 | <.0001 |
| Nonmedication intervention for pain | 0.77 | 0.69-0.87 | <.0001 |
Abbreviations: CI, confidence interval; OR, odds ratio; PRN, pro re nata.
aN = 8,242.
bOdd ratios were adjusted by age, gender, white, arthritis, cancer, depression, heart failure, and psychotic disorder.
Discussion
For pain intervention, our study indicates no significant difference in the administration of scheduled pain medication between residents with or without dementia. This finding is consistent with previous studies. 11,24 However, the pain intervention related to PRN pain medication and nonmedication intervention for pain shows discrepancies. Our study result indicates residents with dementia are less likely to receive PRN pain medication, and this result is consistent with previous studies. 24 For nonmedication intervention for pain, our results indicate residents with dementia are less likely to receive this intervention option compared to their counterpart (18% vs 22%). One study indicated that approximately one-third of the residents had moderate to severe pain regardless of regularly scheduled pain medication. 25 There is a possibility that residents with dementia may experience pain but are unable to articulate it at the time and, thus, get overlooked. For residents with dementia who cannot effectively verbalize their pain using self-report questionnaires, alternative pain assessment modalities should be considered (eg, observational methods, the pain thermometer, the pain map). 5,11 For example, one observational method is the Pain Assessment in Advance Dementia scale. This is an option that assesses 5 pain behaviors: breathing not including vocalization, vocalization, console ability, facial expression, and body posturing. The scale is completed by an independent rater and collected while the person with dementia is receiving nursing care. 5 Another example is the Pain Assessment Check List for Seniors with Limited Ability to Communicate (PACSLAC) scale. 26 This scale is a checklist that is used to assess pain in nursing home residents who have dementia and are unable to communicate verbally. The PACSLAC includes 4 subscales: facial expressions, activity/body movement, social/personality mood, and other. A higher score (indicated by the number of check marks in each subscale) suggests an increase in pain. This is a starting point that indicates that further pain assessment is required. These assessment tools can measure the extent of pain, and the results may be useful for prescribing appropriate pain interventions to alleviate pain, leading to a better quality of life. With an appropriate assessment, there is a possibility that nonmedication intervention for pain such as heat, therapy, massage, hydrotherapy, and so on, can alleviate pain, avoid polypharmacy and adverse drug reactions, and should be considered as an alternative when instituting pain management strategies.
In addition, it was found that a systematic approach to pain management significantly reduced agitation in residents of nursing homes with moderate to severe dementia. 27 Appropriate and effective pain management could reduce the number of unnecessary prescriptions for psychotropic medication to control agitation resulting from untreated pain. To improve quality of life of residents with dementia who seem to have pain, it is of paramount importance to recognize and detect pain before pain treatments can be initiated. In relation to undertreated and untreated pain, it is clear that a comprehensive assessment program is needed that can take into account of disease burden, functional disabilities, and neuropsychiatric and behavior disorders. Also, more focus should be on how pain management could use specific and tailored approaches adjusted to individual needs at appropriate times. It is recommended that health-care providers and caregivers receive proper education and training in the assessment of pain and administration of appropriate treatment modalities. 14,23,28 Therefore, it is important to solicit the assistance of knowledgeable hands-on caregivers to identify typical pain behaviors for residents with dementia using appropriate pain assessment tools so that pain interventions can be administered.
The prevalence of dementia and pain both increase with advancing age. The prevalence of nursing home residents with dementia in New York State (68.4%) is comparable to previous studies. 11,13,29 Our study results show those who received pain assessment and reported pain is about 20%, which is lower than previous studies (29%-83%). 11 -14 It is noted that no-dementia residents are more likely to receive pain assessment (92.5% vs 74.3%) and twice as likely to report having pain compared to dementia residents (29.9% vs 14.8%). This difference may be due to their difficulty expressing pain through verbal communication. 30 In terms of social demographics, residents with dementia who receive pain assessment and had pain are significantly older (85 vs 81.7) and being women (77.3% vs 74%) than residents without dementia; this result is comparable to previous studies. 13,31
Study Limitations
There are limitations to consider in our study. We could not analyze the situation of the residents unable to indicate their pain. In future research, we need to focus on the residents with severe dementia. MDS3.0 did not assess the reasons why the residents had pain and what kinds of pain medication or nonmedication intervention for pain they received for their pain. Given the nature of secondary data analysis, we were not able to address this question in our study. Future studies related to pain management among nursing home residents with dementia should focus on clinical (eg, arthritis) and nonclinical factors (eg, prescription adherence) associated with PRN pain medication and nonmedication interventions for pain.
Conclusion
Our study results indicate that no significant difference exists in the administration of scheduled pain medication between residents with or without dementia; however, residents with dementia are less likely to receive PRN pain medication and nonmedication intervention for pain. There is a possibility that residents with dementia may experience pain but are unable to articulate it at the time and, thus, get overlooked. To address the gap, more research is needed to design a pain assessment tool that can be sensitive to differentiating severity of pain; thus, appropriate interventions can be applied.
Footnotes
Author's Note: Taeko Nakashima is now affiliated with Department of Social Healthcare and Business Management, Nihon Fukushi University, Aichi, Japan.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Taeko Nakashima  https://orcid.org/0000-0003-4048-2780
https://orcid.org/0000-0003-4048-2780
References
- 1. Helvik AS, Engedal K, Benth JŠ, Selbæk G. Prevalence and severity of dementia in nursing home residents. Dement Geriatr Cogn Disord. 2015;40(3-4):166–177. [DOI] [PubMed] [Google Scholar]
- 2. Helvik AS, Høgseth LD, Bergh S, Šaltytė-Benth J, Kirkevold Ø, Selbæk G. A 36-month follow-up of decline in activities of daily living in individuals receiving domiciliary care. BMC Geriatr. 2015;15:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int Psychogeriatr. 2010;22(7):1025–1039. [DOI] [PubMed] [Google Scholar]
- 4. Kowalska J, Rymaszewska J, Szczepańska-Gieracha J. Occurrence of cognitive impairment and depressive symptoms among the elderly in a nursing home facility. Adv Clin Exp Med. 2013;22(1):111–117. [PubMed] [Google Scholar]
- 5. Ngu SSC, Tan MP, Subramanian P, et al. Pain assessment using self-reported, nurse-reported, and observational pain assessment tools among older individuals with cognitive impairment. Pain Manag Nurs. 2015;16(4):595–601. [DOI] [PubMed] [Google Scholar]
- 6. Ferrell BA. Pain evaluation and management in the nursing home. Ann Intern Med. 1995;123(9):681–687. [DOI] [PubMed] [Google Scholar]
- 7. Moore KL, Boscardin WJ, Steinman MA, Schwartz JB. Patterns of chronic co-morbid medical conditions in older residents of U.S. nursing homes: differences between the sexes and across the agespan. J Nutr Health Aging. 2014;18(4):429–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Black BS, Finucane T, Baker A, et al. Health problems and correlates of pain in nursing home residents with advanced dementia. Alzheimer Dis Assoc Disord. 2006;20(4):283–290. [DOI] [PubMed] [Google Scholar]
- 9. Walid MS, Zaytseva N. Pain in nursing home residents and correlation with neuropsychiatric disorders. Pain Physician. 2009;12(5):877–880. [PubMed] [Google Scholar]
- 10. Lyketos C, Lopez O, Jones B, Fitzpatrick A, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment. JAMA. 2002;288(12):1475–1483. [DOI] [PubMed] [Google Scholar]
- 11. Weiner DK, Hanlon JT. Pain in nursing home residents: management strategies. Drugs Aging. 2001;18(1):13–29. [DOI] [PubMed] [Google Scholar]
- 12. Apinis C, Tousignant M, Arcand M, Tousignant-Laflamme Y. Can adding a standardized observational tool to interdisciplinary evaluation enhance the detection of pain in older adults with cognitive impairments? Pain Med. 2014;15(1):32–41. [DOI] [PubMed] [Google Scholar]
- 13. Tang MM, Wollsen MG, Aagaard L. Pain monitoring and medication assessment in elderly nursing home residents with dementia. J Res Pharm Pract. 2016;5(2):126–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cordner Z, Blass DM, Rabins PV, Black BS. Quality of life in nursing home residents with advanced dementia. J Am Geriatr Soc. 2010;58(12):2394–2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hunnicutt JN, Ulbricht CM, Tjia J, Lapane KL. Pain and pharmacologic pain management in long-stay nursing home residents. Pain. 2017;158(6):1091–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Russell TL, Madsen RW, Flesner M, Rantz MJ. Pain management in nursing homes. J Gerontol Nurs. 2010;36(12):49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aubin M, Giguère A, Hadjistavropoulos T, et al. The systematic evaluation of instruments designed to assess pain in persons with limited ability to communicate. Pain Res Manag. 2007;12(3):195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Husebo BS, Strand LI, Moe-Nilssen R, BorgeHusebo S, Aarsland D, Ljunggren AE. Who suffers most? Dementia and pain in nursing home patients: a cross-sectional study. J Am Med Dir Assoc. 2008;9(6):427–433. [DOI] [PubMed] [Google Scholar]
- 19. Monacelli F, Vasile Nurse A, Odetti P. Doloplus-2 pain assessment: an effective tool in patients over 85 years with advanced dementia and persistent pain. Clin Ter. 2013;164(1):e23–e25. [DOI] [PubMed] [Google Scholar]
- 20. Rostad HM, Utne I, Grov EK, Småstuen MC, Puts M, Halvorsrud L. The impact of a pain assessment intervention on pain score and analgesic use in older nursing home residents with severe dementia: a cluster randomised controlled trial. Int J Nurs Stud. 2018;84:52–60. [DOI] [PubMed] [Google Scholar]
- 21. Nakanishi M, Nakashima T, Shindo Y, Niimura J, Nishida A. Japanese care location and medical procedures for people with dementia in the last month of life. J Alzheimers Dis. 2016;51(3):747–755. [DOI] [PubMed] [Google Scholar]
- 22. Neumann RD, Faris P, Klassen R. Examining trends in the administration of “as needed” medications to inpatients with behavioral and psychological symptoms of dementia. Am J Alzheimers Dis Other Demen. 2015;30(3):247–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stokes JA, Purdie DM, Roberts MS. Factors influencing PRN medication use in nursing homes. Pharm World Sci. 2004;26(3):148–154. [DOI] [PubMed] [Google Scholar]
- 24. Nygaard HA, Jarland M. Are nursing home patients with dementia diagnosis at increased risk for inadequate pain treatment? Int J Geriatr Psychiatry. 2005;20(8):730–737. [DOI] [PubMed] [Google Scholar]
- 25. van Kooten J, Smalbrugge M, van der Wouden JC, Stek ML, Hertogh CMPM. Prevalence of pain in nursing home residents: the role of dementia stage and dementia subtypes. J Am Med Dir Assoc. 2017;18(6):522–527. [DOI] [PubMed] [Google Scholar]
- 26. Thé KB, Gazoni FM, Cherpak GL, et al. Pain assessment in elderly with dementia: Brazilian validation of the PACSLAC scale. Einstein (Sao Paulo). 2016;14(2):152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Husebo BS, Ballard C, Sandvik R, Nilsen OB, Aarsland D. Efficacy of treating pain to reduce behavioural disturbances in residents of nursing homes with dementia: cluster randomised clinical trial. BMJ. 2011;343:d4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Horner JK, Hanson LC, Wood D, Silver AG, Reynolds KS. Using quality improvement to address pain management practices in nursing homes. J Pain Symptom Manage. 2005;30(3):271–277. [DOI] [PubMed] [Google Scholar]
- 29. Monroe TB, Misra SK, Habermann RC, Dietrich MS, Cowan RL, Simmons SF. Pain reports and pain medication treatment in nursing home residents with and without dementia. Geriatr Gerontol Int. 2014;14(3):541–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Booker S, Haedtke C. Controlling pain and discomfort, part 2: assessment in non-verbal older adults. Nursing. 2016; 46(5):66–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ferrell BA, Ferrell BR, Rivera L. Pain in cognitively impaired nursing home patients. J Pain Symptom Manage. 1995;10(8):591–598. [DOI] [PubMed] [Google Scholar]