Abstract
Purpose of Review
This review summarizes the current knowledge regarding osteoporosis and fracture among older US Asian adults.
Recent Findings
Asian adults have lower (areal) bone density than non-Hispanic White adults and thus are more likely to be diagnosed and treated for osteoporosis, despite their lower risk of hip fracture. The latter may relate to favorable characteristics in hip geometry, volumetric bone density, and bone microarchitecture; lower risk of falls; and other clinical factors. The fracture risk calculator FRAX accounts for the lower risk of hip fracture among US Asian adults. However, data on major osteoporotic fracture risk remain limited. Fracture rates also vary by Asian subgroup, which may have implications for fracture risk assessment. Furthermore, among women receiving bisphosphonate drugs, Asian race is a risk factor for atypical femur fracture, an uncommon complication associated with treatment duration. Recent clinical trial efficacy data pertaining to lower bisphosphonate doses and longer dosing intervals may be relevant for Asian adults.
Summary
More research is needed to inform osteoporosis care of US Asian adults, including risk-benefit considerations and the optimal duration of bisphosphonate treatment. Greater evidence-based guidance for primary fracture prevention among US Asian adults will ensure health equity in the prevention of osteoporotic fractures.
Keywords: Asian race, ethnicity, osteoporosis, fracture, risk assessment, health equity
INTRODUCTION
The past fifty years have been marked by tremendous increase in the racial and ethnic diversity of the US population, with the Asian population now the fastest growing race group since the turn of the century [1, 2]. Following the repeal of the Chinese Exclusion Act in 1943, the 1965 Immigration Act, major wars in East and Southeast Asia, changing international relations, labor migration, and economic opportunities led to an early growing Asian population in the US [3] that has now nearly doubled from 2000 to 2020 [2]. In 2021, one-fifth of all US immigrants were from India (6.0%), China (5.3%), the Philippines (4.4%), Vietnam (3.0%), and Korea (2.2%) [4, 5]. Currently, 6.0% of the US population is of Asian race [6]. Chinese, Asian Indian, and Filipino ethnicities are the three largest subgroups and together with Vietnamese, Korean, and Japanese ethnicities account for 85% of the US Asian population [1, 7]. Native Hawaiian and Pacific Islander (PI) groups comprise an additional 0.3–0.5% of the overall US population [7].
In another demographic shift, one in five US residents will be over age 65 years by 2030 [8], with even greater ethnic diversity. In California, where nearly one third of all US Asians reside [1, 9], Asian/PI adults represent 16.9% of the state’s older population [10]. Osteoporosis is a serious public health issue for older adults and the burden of osteoporosis among Asian adults will increase substantially as the population ages. Yet the relative dearth of data pertaining to the epidemiology of osteoporosis and fracture among Asian ethnic groups presents unique healthcare challenges for this diverse population [11, 12]. The US Census has tracked Chinese, Japanese, Filipino, Korean, Asian Indian, and Vietnamese ethnicities since 1980 and earlier [13], but for the vast majority of epidemiologic studies focused on osteoporosis and fracture outcomes, this heterogeneous population has been grouped more broadly as “Asian”.
A challenge in clinical management is that Asian adults tend to have lower bone mineral density (BMD) than non-Hispanic White (NHW) adults, due in part to measurement of areal BMD by dual energy x-ray absorptiometry (DXA), which is influenced by bone size [14]. As such, Asian women are over-represented among post-menopausal women receiving osteoporosis therapy for primary fracture prevention [15, 16]. Yet hip fracture rates among US Asian adults are much lower than among NHW adults [17–21]. Bone structural properties and other factors that may explain these observed differences are briefly summarized in the current report and have been extensively reviewed elsewhere [22–24]. Another concern is the more recent recognition that Asian race is a risk factor for atypical femur fracture (AFF) among women who received bisphosphonate therapy [15, 25–28]. This uncommon treatment complication, first reported in the US [29–31] and Singapore [32, 33], is an additional consideration when determining the optimal length of bisphosphonate therapy for Asian women. In this review, we discuss the skeletal health of older US Asian adults, Asian subgroups, and clinical management considerations in primary care and suggest future research to guide evidence-based practice for this understudied population.
BONE STRUCTURE AND STRENGTH
Bone Mineral Density
A major determinant of bone strength is BMD which is typically measured by DXA, reflecting areal BMD (g/cm2) [34]. But in persons with small bone size, this two-dimensional measurement may underestimate true volumetric BMD, a three-dimensional property that can be assessed by quantitative computerized tomography (QCT) [14]. In the Osteoporotic Fractures in Men (MrOS) study, femoral neck areal BMD was lower in Asian compared to White men but femoral neck QCT data showed higher trabecular volumetric BMD and thicker cortices [35]. An estimate of volumetric BMD (bone mineral apparent density, BMAD) has also been calculated from DXA measurement of vertebral size and mineral content. The Study of Women’s Health Across the Nation (SWAN) found that areal BMD was lower in Japanese and Chinese women than in White women, but BMAD was higher in Asian women [36]. Others have also observed that calculation of BMAD reduces or eliminates BMD differences among Asian subgroups and White adults [37].
Few studies have compared (areal) BMD among other US Asian subgroups. Table 1 summarizes population studies that report areal BMD data for US Asian ethnic subgroups. In an early study of 449 South Asian women and 2245 age-matched Chinese women, age-specific femoral neck BMD was slightly lower for Chinese compared to South Asian women age 50–69 years [38]. In a more recent report, mean femoral neck BMD among 11,147 Filipina, 10,648 Chinese, and 2,519 Japanese women generally differed by ≤3%, but were collectively lower than NHW counterparts – at least 6–8% lower among older women [39]. While adjustment for stature (which was 6–8 cm lower among Asian women) reduced the Asian-NHW BMD differences by 30–40%, persisting BMD differences observed among older women suggested a potential age cohort effect [39].
Table 1.
Population studies examining bone mineral density (BMD) or fracture incidence among adult and older US Asian ethnic subgroups
| Author (Year) | Cohort Setting & Years of Study | Sex and Age | Racial and Ethnic Subgroups (N) | Outcome: BMD or Fracture |
Primary findings pertaining to the US Asian subgroups studied |
|---|---|---|---|---|---|
| Lauderdale, DS, et al. (1997) Reference [17] |
US Medicare 1992–1993 |
women men ≥65 y |
Chinese (24,366) Japanese (28,762) Korean (5470) |
hip fracture | Age-adjusted incidence of hip fracture was generally lower for Chinese, Japanese, and Korean vs White adults, with incidence lowest for Chinese adults. |
| Ross PD, et al. (1991) Reference [99] |
Oahu, Hawaii
1979–1981 Okinawa, Japan 1984–1985 Rochester, MN 1978–1982 |
women men 50–84 y |
Japanese (Hawaii) Japanese (Okinawa) Caucasian (Hawaii) Caucasian (Rochester, MN) |
hip fracture | Hip fracture incidence did not differ between Japanese adults in Hawaii vs Japanese adults in Okinawa Japan but were about half the hip fracture incidence of Caucasian adults in Hawaii and Rochester, MN. |
| Kin K, et al. (1993) Reference [137] |
San Diego county,
CA 1991–1992 |
women 18–89 y |
US-born Japanese (151) Japan-born immigrant (137) |
femoral neck BMD lumbar spine BMD |
US-born Japanese women had higher BMD and higher percentage of body fat than immigrant Japanese women |
| Marquez, MA, et al. (2001) Reference [37] |
Rochester, MN 1997 (Asian) 1989–1992 (White) |
women men ≥20 y |
Vietnamese (172) Cambodian (171) Laotian (53) White (684) |
femoral neck BMD lumbar spine BMD |
BMD was lower in Southeast Asian vs White adults. Some differences were reduced or eliminated when bone mineral apparent density (BMAD) was calculated, depending on sex and age/menopause status. |
| Morton DJ, et al. (2003) Reference [157] |
San Diego county,
CA 1992–1997 1995–1998 |
women 50–69 y |
Filipina (285) Hispanic (164) Caucasian (354) Northern European |
femoral neck BMD total hip BMD lumbar spine BMD |
Adjusting for body size and lifestyle factors minimized BMD differences between Filipina, Hispanic, and Caucasian women. |
| Walker MD, et al. (2006) Reference [48] |
New York City 2002–2004 |
women 20–90 y |
Chinese (359) | femoral neck BMD total hip BMD lumbar spine BMD |
US Chinese referent BMD values (for T-score calculation) are lower than Caucasian referent BMD values and would result in half reclassified from osteoporosis to osteopenia. |
| Melamed A, et al. (2010) Reference [47] |
MASALA study; San Francisco Bay Area,
CA 2006–2007 |
women men 45–79 y |
South Asian Indian (150) | total hip BMD lumbar spine BMD |
13–40% of South Asian adults were reclassified to normal BMD with a North or South Indian-based referent population instead of the NHW referent population |
| Finkelstein JS, et al. (2002) Reference [36] |
Study of Women’s Health Across the
Nation (SWAN) 1996–1997 |
women 42–52 y |
Chinese (232–235) Japanese (257) African American (591–608) Caucasian (1051–1076) |
femoral neck BMD lumbar spine BMD |
BMD was highest in African American followed by Caucasian women and lowest in Chinese and Japanese women. Adjusting for body weight and covariates resulted in similar BMD for Chinese, Japanese, and Caucasian women. |
| Finkelstein JS, et al. (2008) Reference [91] |
Study of Women’s Health Across the
Nation (SWAN) 1996–2002 (includes follow-up) |
women 42–52 y (baseline) |
Chinese (221) Japanese (243) African American (494) Caucasian (944) |
total hip BMD lumbar spine BMD |
Japanese and Chinese women had greater spine BMD loss than Caucasian women; African American women had the least. Ethnic variations in bone loss were mainly attributed to body weight differences and were no longer evident after restricting analyses to women weighing 50–78 kg. |
| Shieh A, et al. (2022) Reference [105] |
Study of Women’s Health Across the
Nation (SWAN) 1996–2016 (includes follow-up) |
women 42–52 y (baseline) |
Chinese (147) Japanese (178) Black (443) Hispanic (105) White (681) |
clinical fracture | Fracture risk for Black (HR 0.55 [CI 0.46–0.75]) and Japanese (HR 0.47 [CI 0.27–0.84]) women was lower than White women (reference), but non-significant for Chinese (HR 0.73 [CI 0.41–1.31]) and Hispanic women (0.50 [CI 0.22–1.14]). |
| Khandelwal S, et al. (2012) Reference [38] |
Kaiser Permanente Northern
California 1997–2010 (includes follow-up) |
women 50–85 y (baseline) |
Chinese (2,245) South Asian (449) NHW (4,490) |
femoral neck BMD wrist fracture humerus fracture (proximal, shaft) hip fracture |
BMD-osteoporosis prevalence tended to be higher for Chinese vs. South Asian women, both higher than NHW women. Wrist fracture incidence was similar for South Asian vs NHW women, both higher than Chinese women. |
| Lo JC, et al. (2016) Reference [49] |
Kaiser Permanente Northern
California 1997–2003 |
women 50–79 y |
Chinese (4,039) NHW (20,195) |
femoral neck BMD total hip BMD lumbar spine BMD FRAX score |
A US Chinese T-score reduced osteoporosis prevalence by about half for US Chinese women. For those age <65y reclassified to femoral neck osteopenia, most had FRAX hip fracture risk <3%. |
| Lo JC, et al. (2020) Reference [39] |
Kaiser Permanente Northern
California 1998–2017 |
women 50–79 y |
Chinese (10,648) Filipina (11,147) Japanese (2,519) NHW (115,318) |
femoral neck BMD | Mean femoral neck BMD differed by ≤3% for older Chinese, Filipino, and Japanese women but was 6–8% lower than NHW women. Asian-White differences were partly attenuated with height adjustment but remained greater for older women. |
| Lo JC, et al. (2023) Reference [20] |
Kaiser Permanente Northern
California 2000–2021 (includes follow-up) |
women men ≥50 y |
Chinese (91,556) Filipino (106,643) South Asian (24,359) Japanese (19,782) Other/unspecified Asian/PI (161,347) NHW (1,473,885) |
hip fracture | Hip fracture incidence rate ratios for US Asian/PI adults in aggregate vs NHW were 0.45 (women) and 0.34 (men) but varied among the four major Asian subgroups: ranging 0.45–0.64 for women (lower for Filipina, higher for Japanese and South Asian vs Chinese) and 0.32–0.55 for men (lower for Filipino, Japanese, Chinese vs South Asian) |
| Lo JC, et al. (2023) Reference [104] |
Kaiser Permanente Northern
California 2000–2021 (includes follow-up) |
women men ≥50 y |
Chinese (91,556) Filipino (106,643) South Asian (24,359) Japanese (19,782) Other/unspecified Asian/PI (161,347) NHW (1,473,885) |
wrist fracture humerus fracture (proximal) |
Humerus fracture incidence was lower for Filipino, higher for Japanese adults, and even higher for South Asian men vs. Chinese adults. Wrist fracture incidence was lower for Filipino and higher for South Asian adults and Japanese women vs. Chinese adults. Wrist fracture incidence for South Asian men approached that of NHW men. |
y = year; BMD = bone mineral density; NHW = non-Hispanic White; PI = Pacific Islander; HR = hazard ratio; CI = confidence interval;
MASALA = Metabolic Syndrome and Atherosclerosis in South Asians Living in Americas (recruited from San Francisco Bay Area, CA)
This Table focuses on studies of central areal BMD (dual energy x-ray absorptiometry) and fracture incidence among US Asian ethnic subgroups.
Studies examining US Asian adults as an aggregate group are described in a recent comprehensive review by Noel, et. al. [11] and not included in this table.
The Study of Women’s Health Across the Nation (SWAN) examined BMD and fracture in midlife Chinese (recruited in Oakland, CA) and Japanese (recruited in Los Angeles, CA) women. https://www.swanstudy.org/publications/
Areal BMD has been used to define osteoporosis, but because BMD differs depending on the densitometer manufacturer, it is reported in relative terms as a T-score, representing standard deviations from peak bone mass [40]. In 1994, an expert committee sponsored by the World Health Organization recommended that osteoporosis be defined as a BMD T-score ≤ −2.5, osteopenia between −1.0 and −2.5, and normal ≥ −1.0 [41]. These definitions relied on reference populations of White women. When men were studied, new reference data allowed T-scores by sex, and additional race and ethnicity data added early sets of sex-specific ethnic T-scores, depending on the densitometer [42]. Once the uniform NHW femoral neck BMD reference from National Health and Nutrition Examination Survey (NHANES) III was used for all densitometers [43, 44], the NHW T-score was reported for Asian adults. NHANES III (1988–1994) studied NHW, Black, and Mexican men and women but not Asian adults [45, 46].
Using relative values for areal BMD (T-scores according to the distribution within a population), individuals with the same areal BMD but different ethnicity could have different ethnic T-scores that impact BMD classification. For example, a study of 150 South Asian women in California found that 13% were reclassified from low to normal BMD using a North India BMD reference (total hip), whereas 40% were reclassified using a South India BMD reference (lumbar spine) [47]. In 2006, Walker et al. published a Chinese American referent BMD database derived from 359 healthy Chinese American women aged 20–90 years in New York City [48]. Using this reference, the prevalence of T-score ≤ −2.5 in Chinese women fell from 43% to 21% based on the lowest of femoral neck, total hip, and lumbar spine T-scores [48]. This same Chinese BMD reference applied to Chinese women in northern California [49] showed similarly large shifts in T-score classification (Figure 1). Although Chinese women in New York may differ from those in California, the question remains how to best risk stratify Asian adults with BMD measured by DXA.
Figure 1.
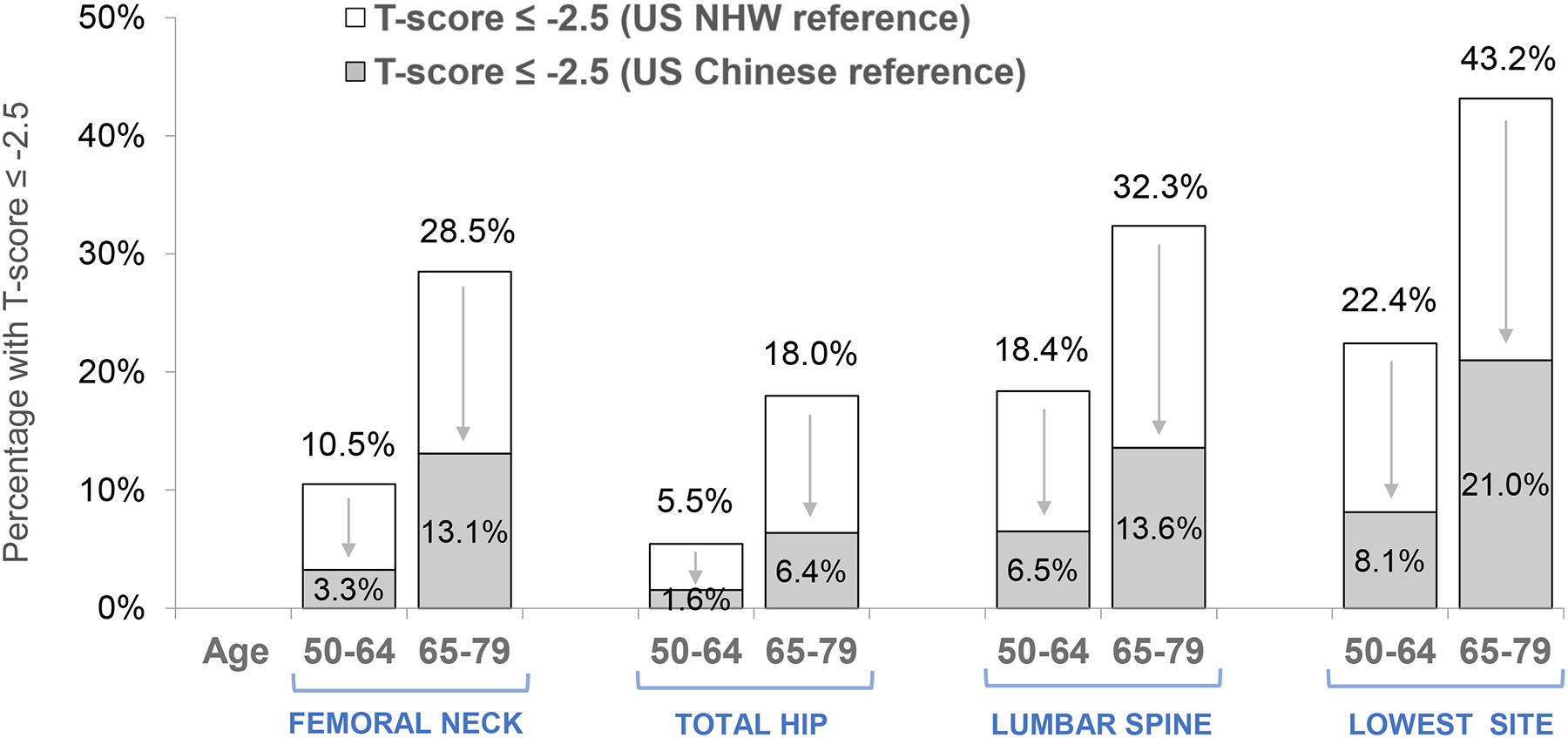
Change in the percentage of Chinese women with T-score ≤−2.5 when bone mineral density T-score is calculated using US Chinese reference data compared to US Non-Hispanic White (NHW) reference data.
A much lower percentage of Chinese women are classified with bone mineral density (BMD) T-score ≤ −2.5 when a US Chinese BMD reference [48] is used for T-score calculation compared to the NHW BMD reference [43,48,49].
Figure redrawn from reference 49 (Lo JC, et al. Applying ethnic-specific bone mineral density T-scores to Chinese women in the USA. Osteoporos Int. 2016; 27:3477–3484) with permission.
Since 2002–2006 for women [42, 50] and 2013 for men [51], the International Society for Clinical Densitometry has recommended using the NHW female reference to calculate BMD T-scores for adults of all races and ethnicities [52]. Although local recommendations may vary with regard to sex- or race-specific T-scores [52, 53], the general consensus was to use an absolute definition for osteoporosis: areal BMD T-score relative to the peak bone mass of NHW women in the NHANES III, thereby providing a standard referent [54]. At the femoral neck, this osteoporosis threshold is an areal BMD of 0.577 g/cm2 (Hologic densitometer; cross-calibration equations convert to other manufacturer densitometers) [43, 54]. The absolute value was defined in NHW women but is independent of age, sex, and ethnicity. However, this is an areal BMD and size differences must be considered. Even with volumetric bone density, BMD assignment does not fully convey the risk of fracture or whether any treatment will reduce the risk of fracture.
For NHW women, large population studies were conducted to enable estimation of fracture risk from areal BMD and other risk factors. The NIH-funded Study of Osteoporosis Fractures (SOF) enrolled nearly 10,000 women (99.7% White) in 1986–1988 [55] . Black women were excluded because of their low incidence of hip fractures; Asian and Hispanic women were not mentioned. The only “ethnic origin” information was Northern or Southern European ancestry [55]. Since then, more studies have included US Asian adults (as an aggregate group), but disparities remain in the amount of data examining the relationship of BMD and other risk factors to fracture. A major gap in the field is the lack of data pertaining to US Asian subgroups. The National Osteoporosis Risk Assessment (NORA) study characterized low peripheral BMD (heel, forearm, finger), risk factors, and fracture incidence in postmenopausal women, but only 1% of subjects were of Asian race [56]. The mean T-score for Asian women was lower compared to White women in each age decade, whereas their relative risk for fracture at one year was 0.32, adjusting for BMD, weight, and other covariates [57]. Within each racial and ethnic group in the NORA study, the associations of peripheral BMD (T-score) and fracture were similar [57].
Bone Microarchitecture
In addition to bone mass, bone microarchitecture plays an important role in bone strength [58]. Bone microarchitecture assessed by high-resolution peripheral QCT (HR-pQCT) of the distal radius and tibia demonstrates higher (volumetric) trabecular and cortical bone density and thickness in premenopausal Chinese American women compared to White women, despite smaller bone area [59], as well as better trabecular microstructure [60]. In postmenopausal women, higher cortical bone density and thickness and lower trabecular number but higher trabecular thickness have been observed in Chinese compared to White women, with similar estimates of whole bone stiffness [61]. Recent interest has focused on trabecular bone score (TBS), an index derived from lumbar spine DXA images [62] that correlates with bone microarchitectural properties at the spine and hip [63]. Leslie, et al. [64] examined data from 29,407 women in Manitoba, Canada and found that lumbar spine TBS predicted major osteoporotic fracture in women with diabetes and captured diabetes-associated fracture risk more optimally than BMD (BMD tends to be higher in patients with diabetes). Whether these same relationships exist for Asian adults, a demographic group with prevalent diabetes and lower body weight [65], has not been examined. Racial and ethnic differences in TBS have been reported [66–68], and more studies examining TBS in racial and ethnic minority populations have been advocated [69].
Hip Geometry
Faulkner and colleagues [70] were the first to report that longer hip axis length predicts increased hip fracture risk among postmenopausal White women. Cummings, et al. [71] further observed that US Asian women (89% were Japanese-American) had shorter hip axis length independent of height differences, which could be a potential explanation for their lower risk of hip fracture. Other subsequent studies have also identified shorter hip (or femoral neck) axis length in Asian compared to White adults, as summarized in prior reviews [22, 72]. In the SWAN study, differences in hip structure analysis measures and higher composite strength indices which may confer lower hip fracture risk were observed in midlife Chinese and Japanese women when compared to White women [73–75].
Mineral Metabolism
Important racial and ethnic differences are seen in vitamin D metabolism [76], along with variations in sun exposure and supplement use [77, 78]. In the Multi-Ethnic Study of Atherosclerosis (MESA), community-dwelling Chinese adults had 25OH-vitamin D levels that were lower than NHW adults, similar to Hispanic adults, and higher than Black adults [76]. Increased prevalence of vitamin D deficiency has been reported in some but not all US Asian subgroups compared to NHW adults [79–82], although Filipino adults are less likely than East Asian adults to have low 25OH-vitamin D levels [77, 81]. As a group, Asian adults with vitamin D deficiency are less likely than NHW adults to achieve successful repletion after initial pharmacologic therapy [83]. Serum vitamin D levels also depend on binding protein levels, which are diverse. Despite widespread interest in vitamin D, there is insufficient data about the optimal vitamin D level for adults of Asian race. Asian subjects (1.5%) were under-represented in the recent large Vitamin D and Omega-3 Trial (VITAL) of vitamin D [84]. Few studies have examined cultural variation in diet and relation to fracture risk among the Asian diasporas. Traditional diets in many Asian countries are low in calcium [85], but calcium intake among Asian Americans may be higher, with variation by subgroup and generational status [86].
Bone Remodeling
Multiple studies from China, Japan, and Singapore confirm a positive relationship between bone turnover markers and risk of fracture [87–89]. In the SWAN study, increases in the bone resorption marker urinary crosslinked N-telopeptide of type I collagen (NTX) across the menopause transition were greatest for Japanese followed by Chinese women compared to White women, but ethnic differences were attenuated after adjusting for BMI and other covariates [90]. These findings extend earlier observations that ethnic variation in perimenopausal bone loss appear to be largely attributable to differences in body weight [90, 91]. The SWAN study also found that pre- and early perimenopausal levels of serum osteocalcin, a bone formation marker, were lower in Chinese and Japanese women compared to White women [92, 93]. Serum sclerostin, a protein that inhibits osteoblast differentiation and bone formation, has been associated with hip fracture risk in White women [94], but levels do not appear to differ between White and Chinese women and are not associated with volumetric BMD or microarchitecture [95]. To our knowledge, no studies in the US have examined bone biopsies in a population of Asian adults to directly measure their bone turnover rates.
FRACTURE EPIDEMIOLOGY
Hip Fracture
Epidemiologic research over four decades consistently demonstrate much lower hip fracture incidence among US Asian compared to NHW adults [17–21, 96–99]. These reports are summarized in a recent comprehensive review by Noel and colleagues [11]. However, the Asian population has been largely studied in aggregate [11], with or without inclusion of Native Hawaiian/PI adults, comprising ≤7% of the Asian/PI population [7]. Overall, among older US Asian adults, hip fracture rates have generally ranged about 35–65% lower than in NHW adults, varying by sex, ethnicity, and era.
Few studies have compared hip fracture incidence among US Asian subgroups. Table 1 summarizes the existing US studies that have reported on fracture outcomes among one or more Asian subgroups. In an early study of East Asian adults using 1992 US Medicare data, sex-specific hip fracture incidence was higher for Japanese and Korean adults compared to Chinese adults, with all three groups generally lower than White adults [17]. The standardized fracture ratios relative to White women/men were 0.30/0.42 for Chinese, 0.73/0.58 for Japanese, and 0.53/0.91 for Korean adults, respectively [17]. In a more contemporary population of northern California adults aged ≥50 years in an integrated healthcare system, age-adjusted hip fracture incidence ratios for Asian/PI compared to NHW adults were 0.45 for women and 0.34 for men, with heterogeneity by Asian subgroup [20]. Compared to Chinese women, hip fracture incidence was lower for Filipina and higher for Japanese and South Asian women, and compared to Chinese men, fracture incidence was similar for Filipino and Japanese but higher for South Asian men [20]. The corresponding hip fracture incidence rate ratios compared to NHW women/men were: 0.45/0.35 for Chinese, 0.64/0.39 for Japanese, 0.37/0.32 for Filipino, and 0.56/0.55 for South Asian adults among the four major Asian subgroups examined [20].
Several factors may explain the lower risk of hip fracture in Asian populations, including differences in hip geometry and other bone structure or strength indices that confer additional skeletal advantages (as previously discussed). Lower stature and weight may result in less impact during ground level falls, reducing the likelihood of fracture [61]. Other health or lifestyle factors such as balance, physical mobility, nutrition, diet, smoking, alcohol intake, and clinical factors [53] that differ by race and ethnicity may also contribute, despite the lower weight and lower BMI typically observed in Asian adults [39, 65, 100, 101]. The risk of falls also differs by race and ethnicity; several studies report that US Asian women are one-third less likely to have ≥1 or ≥2 falls within the past year compared to NHW women [102, 103], although subgroup differences have not been studied. Anthropometric differences include higher BMI among Filipino adults and recent trends in younger populations also suggest that BMI is higher among Japanese and South Asian adults compared to Chinese, Vietnamese, and other Southeast Asian adults [65, 100, 101].
Other Major Osteoporotic Fracture
Fewer studies have examined humerus and wrist fractures in US Asian populations, and findings for Asian subgroups remain sparse (Table 1). In a study using 2000–2005 Medicare claims data, the fracture incidence ratio comparing Asian to White adults was 0.63 for distal radius or ulna fracture and 0.52 for humerus fracture, adjusting for age, sex, and other factors [19]. Differences between Asian men and women were not characterized, but in the same population, the fracture incidence ratio for hip fracture was 0.61 [19]. Among older South Asian women and age-matched Chinese and NHW women in an integrated Northern California healthcare system, Khandelwal et al. observed that South Asian women had a higher incidence and relative rate of wrist fracture compared to Chinese women, with rates approaching that of NHW women [38]. In a much larger and more contemporary population of Asian adults age ≥50 years from the same Northern California healthcare system (Table 1), Lo and colleagues observed that wrist fracture rates were lower for Filipino compared to Chinese adults, but higher for Japanese women and South Asian adults, with South Asian men not significantly different from NHW men [104]. The age-adjusted wrist fracture incidence rate ratios compared to NHW women/men were: 0.62/0.68 for Chinese, 0.82/0.75 for Japanese, 0.27/0.42 for Filipino, and 0.76/0.90 for South Asian adults, respectively [104]. In this same study, proximal humerus fracture rates also varied but were lower than NHW adults, except for South Asian men where differences did not reach statistical significance; the incidence rate ratios compared to NHW women/men were: 0.40/0.35 for Chinese, 0.56/0.50 for Japanese, 0.30/0.25 for Filipino, and 0.41/0.79 for South Asian adults [104]. These results highlight differences in upper extremity fracture incidence by Asian ethnicity, lower for Filipino and higher for selected Japanese and South Asian subsets, depending on the skeletal site and sex [104]. In addition, findings from the SWAN study suggest that ethnic patterns in fracture risk further differ for the outcome of any clinical fracture [105].
Studies from countries in Asia suggest that vertebral fracture prevalence and incidence are high in older Asian adults, but methodologic approaches vary, including methods for morphometric ascertainment [106–108]. To our knowledge, there are no data comparing vertebral fracture incidence and risk among US Asian subgroups, and the vertebral fracture incidence ratios comparing US Asian and Asian subgroups to NHW adults remain somewhat uncertain.
Atypical Femur Fracture
Atypical femur fractures (AFF) are an uncommon complication of potent antiresorptive therapy, first reported with bisphosphonate drugs [29–33, 109]. Prolonged suppression of bone turnover coupled with impaired micro-crack repair in areas of higher mechanical stress are hypothesized to predispose susceptible patients to AFF [30, 110, 111]. The risk of AFF is evident after three years of bisphosphonate treatment [112], increases substantially with treatment duration [27, 111, 113], and varies by race and ethnicity. Notably, 5- to 6-fold greater risk is observed in US Asian women [15, 26, 27]. Two independent California populations of primarily women who received bisphosphonate therapy (13–17% Asian) demonstrate an age-adjusted incidence of AFF ranging from 2–3 per 100,000 person-years for <2 years treatment to 112–113 per 100,000 person-years for ≥8 years [111, 113]. Among women with any bisphosphonate use, Black et al. reported 9-fold and 43-fold higher risk of AFF after 3–5 years and ≥8 years of treatment, respectively, compared to ≤3 months [27]. The risk of AFF appears to decline rapidly following bisphosphonate cessation [27, 114]. Atypical femur fracture can occur with denosumab, but the additional risk associated with Asian race has not been well characterized.
The mechanisms underlying the increased risk of AFF in Asian women with bisphosphonate exposure have not been clearly elucidated. Although BMD may be associated with AFF location in the diaphyseal femur [115], the risk of AFF appears to be independent of hip BMD [26, 27]. One hypothesis is that differences in femur geometry and greater femur bowing in Asian populations result in biomechanical forces that predispose to peak tensile stress and formation of (atypical) stress fractures [15, 26, 115–120]. This could explain the frequent symmetric bilaterality of AFF findings (incomplete AFF or stress reaction in the contralateral femur in a patient with complete AFF). A recent Australian study examined women with typical femur fracture and those with AFF and found that Asian ethnicity remained a strong independent predictor of AFF after accounting for differences in femur geometry [121]. However, AFF risk has not been examined in prospective cohorts with respect to measures of femur geometry [120], bone turnover [122], and genetic factors [123].
In Asian women receiving bisphosphonate therapy, the risk benefit considerations currently favor inclusion of drug holidays to limit the duration uninterrupted therapy beyond five years. After three years of treatment for Asian women, Black et al. estimated that 91 hip fractures and 330 clinical fractures would be prevented compared to 8 AFF events, whereas this difference narrowed to 360 hip fractures and 831 clinical fractures prevented compared to 236 AFF events after ten years of treatment [27]. These projections optimistically assumed that the benefit of bisphosphonate therapy beyond five years is the same as during the first three years, and that the fracture reduction in Asian women is the same as in NHW women [124]. However, the efficacy of neither short nor long-term bisphosphonate therapy has been examined in US Asian women, a population with lower hip fracture risk than NHW women and one scarcely represented in the major US osteoporosis clinical trials [125–128].
FRACTURE RISK ASSESSMENT
Although BMD-based treatment recommendations (T-score ≤ −2.5, NHW reference) do not account for racial and ethnic differences in fracture risk, the fracture risk assessment tool FRAX (https://frax.shef.ac.uk/FRAX/) currently considers the lower population fracture risk in Asian adults by including a calibration factor [129] for the US Asian FRAX (0.50 for women, 0.64 for men). These estimates are based on epidemiologic studies demonstrating lower hip fracture incidence among US Asian compared to White adults [17, 96, 97], thereby reducing potential over-estimation of fracture risk which is relevant for populations with lower BMD and lower fracture incidence. The Canadian FRAX does not account for Asian race and can overestimate their fracture risk [130]. While ongoing refinement of FRAX is expected [131, 132], including new risk factors and efforts to examine FRAX and the efficacy of intervention [133], studies examining how fracture risk prediction can be optimized for US Asian subgroups and accounting for factors such as length of residence in the US are likely to be relevant [134, 135]. Data also suggest there are first immigrant and generational effects on skeletal health [135–137]. Prevalent comorbidities should also be studied; for instance, diabetes has been identified as a rheumatoid arthritis risk equivalent in FRAX based on studies conducted in primarily White populations [138, 139]. On a much larger scale, an updated version of FRAX is planned, that will be informed by pooling multiple large and diverse prospective cohorts with baseline risk factor assessment and fracture outcomes, where ethnicity-specific differences will also be examined [140].
In the meantime, clinicians should be aware that fracture risk may differ amongst Asian ethnicities due to unmeasured risk factors and this should be considered when interpreting FRAX scores calculated under the umbrella of “US Asian”. While data informing major osteoporotic fracture risk for US Asian subgroups remain sparse, some evidence points to greater differences among Asian subgroups at other skeletal sites beyond hip fracture, including differences among East Asian adults [104]. South Asian adults, especially men, may have upper extremity fracture incidence rates closer to the NHW population [38, 104] and some propose that the US Caucasian FRAX is more appropriate for assessing major osteoporotic fracture risk in South Asian men [141]. As we strive for greater health equity in research and clinical practice, the question remains how the known heterogeneity among US Asians can be addressed through FRAX and similar fracture risk calculators, in order to unmask meaningful differences in clinical outcomes.
For first generation adult immigrants, the native country FRAX calculator has been considered [142, 143], but this has not been studied for Asian adults in the US and may yield conflicting guidance for Chinese immigrants from highly industrialized regions in Asia (Taiwan, Hong Kong, and Singapore); their country-region FRAX scores for hip fracture risk are much higher than the US Asian, China, and US Caucasian FRAX scores for the same clinical profile [134, 145] and country-specific intervention thresholds may differ [144]. As the US Asian population ages, there may be further bone health differences among US native-born, foreign-born acculturated, and foreign-born adult immigrant populations that warrant consideration, including the role of biology and social, behavioral, and cultural factors [146–148].
TREATMENT CONSIDERATIONS
What Does Guideline Concordant Care Look Like for the Asian Woman?
Currently, guideline [53] concordant care in the US results in the treatment of Asian women aged 65–70 years with areal BMD T-score ≤ −2.5 and no prior fracture or other risk factors. The vast majority of these women have discordant BMD- and FRAX-based treatment indication that is generally not seen for NHW female counterparts (Table 2). Key questions are whether FRAX, which is clinically used for BMD T-score between −1.0 and −2.5 [53], can help risk stratify postmenopausal Asian women under age 70 years with no risk factors except T-score ≤ −2.5, and whether alternative T-score thresholds might address the lower areal BMD in Asian women with short stature. These questions target the concern of potential overtreatment of Asian women who are otherwise at lower fracture risk except for their BMD categorization [12].
Table 2.
Large discordance in osteoporosis treatment indication is evident for US Asian women aged 65–70 years old with femoral neck T-score ≤ −2.5 and no other clinical risk factors compared to non-Hispanic White women with the same clinical profile
| 10-year risk of hip fracture estimated by FRAX* for women with femoral neck BMD T-score ≤ −2.5 and no clinical risk factors | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 120 pounds, 62 inches | Non-Hispanic White Women (US Caucasian FRAX) | US Asian Women (US Asian FRAX) | ||||||||||
| Age (years) | T −2.5 | T −2.6 | T −2.7 | T −2.8 | T −2.9 | T −3.0 | T −2.5 | T −2.6 | T −2.7 | T −2.8 | T −2.9 | T −3.0 |
| 65 | 2.7 | 3.1 | 3.4 | 3.8 | 4.2 | 4.7 | 1.5 | 1.7 | 1.9 | 2.1 | 2.4 | 2.6 |
| 66 | 2.9 | 3.2 | 3.6 | 4.0 | 4.4 | 4.9 | 1.6 | 1.8 | 2.0 | 2.2 | 2.5 | 2.8 |
| 67 | 3.1 | 3.4 | 3.8 | 4.2 | 4.7 | 5.2 | 1.7 | 1.9 | 2.1 | 2.4 | 2.6 | 2.9 |
| 68 | 3.3 | 3.6 | 4.0 | 4.5 | 4.9 | 5.5 | 1.9 | 2.1 | 2.3 | 2.5 | 2.8 | 3.1 |
| 69 | 3.5 | 3.9 | 4.3 | 4.7 | 5.2 | 5.8 | 2.0 | 2.2 | 2.4 | 2.7 | 3.0 | 3.3 |
| 70 | 3.7 | 4.1 | 4.5 | 5.0 | 5.5 | 6.1 | 2.1 | 2.3 | 2.6 | 2.8 | 3.1 | 3.5 |
| 71 | 4.0 | 4.4 | 4.8 | 5.3 | 5.8 | 6.4 | 2.3 | 2.5 | 2.8 | 3.0 | 3.3 | 3.7 |
| 72 | 4.2 | 4.7 | 5.1 | 5.6 | 6.2 | 6.8 | 2.4 | 2.7 | 2.9 | 3.2 | 3.6 | 3.9 |
| 73 | 4.5 | 5.0 | 5.5 | 6.0 | 6.6 | 7.2 | 2.6 | 2.9 | 3.2 | 3.5 | 3.8 | 4.2 |
| 74 | 4.8 | 5.3 | 5.8 | 6.3 | 6.9 | 7.6 | 2.8 | 3.1 | 3.4 | 3.7 | 4.1 | 4.5 |
| 75 | 5.2 | 5.6 | 6.2 | 6.7 | 7.3 | 8.0 | 3.0 | 3.3 | 3.6 | 4.0 | 4.3 | 4.7 |
Shaded areas indicate when the Bone Health and Osteoporosis Foundation (BHOF) treatment threshold of ≥3% for FRAX-calculated 10-year risk of hip fracture is reached or exceeded, evident for most non-Hispanic White women aged >65 years with BMD T-score ≤ −2.5 (non-Hispanic White reference) and with no other clinical risk factors (body mass index 21.9 kg/m2).
The FRAX scores for 10-year risk of hip fracture are calculated using the FRAX Tool: https://frax.shef.ac.uk/FRAX/ (web version 4.3)
Bisphosphonate Dosing and Drug Holidays
When bisphosphonates were first approved for osteoporosis, guidelines recommended treatment at an areal BMD T-score ≤ −2.0 or when the T-score was ≤ −1.5 with risk factors which could include body weight <127 pounds [149]; in an early era, low body weight was also an osteoporosis screening indication [43]. This may have resulted in disproportionate unnecessary treatment of postmenopausal Asian women undergoing BMD testing. As BMD testing now targets all women aged 65–75 years [150], more evidence-based guidance is needed for primary fracture prevention among Asian women.
The majority of postmenopausal women receiving osteoporosis therapy are treated with bisphosphonate drugs. In NHW women, there is strong clinical trial efficacy data for the first three years. However, over time, prolonged inhibition of bone remodeling may compromise bone micromechanical properties [151, 152] and over-suppression of bone turnover may predispose to AFF. An important area lacking evidence is the bone turnover rate in Asian women and the degree to which bisphosphonate treatment suppresses their bone formation. While drug holidays are now considered after five years of treatment [153], future trials should examine whether earlier drug holidays (e.g., temporary cessation after three years therapy) might result in similar efficacy while limiting the initial length of uninterrupted treatment. Lower dosing regimens have been proposed, based on early comparability of standard and lower oral bisphosphonate dose for fracture prevention [152]. In Japan, the approved alendronate dose for osteoporosis is lower at 5 mg/day [154]. Randomized clinical trial data demonstrate that 5 mg of zoledronate given at wider 18-month intervals over six years reduces the risk of both nonvertebral and vertebral fractures in women with osteopenia [155]. Furthermore, a single dose of 5 mg zoledronate resulted in an increase in spine and hip BMD that persisted for five years and then returned to baseline after nine years [156]. Zoledronate doses as low as 1 mg at baseline result in higher BMD compared to placebo four years later [156]. These findings support efforts to limit the bisphosphonate dose and dosing frequency, which may be especially relevant for Asian women with smaller body size. Finally, studies examining baseline bone turnover and fracture efficacy of osteoporosis drugs in Asian adults may inform individualized treatment considerations.
CONCLUSION
Despite substantial advances in our understanding of bone fragility and fracture risk, there are serious knowledge gaps concerning skeletal health in US Asian adults. More research is needed to inform fracture prevention care of this diverse and heterogeneous population that generally has lower areal BMD, yet lower risk of hip fracture, and important differences by ethnicity, sex, and fracture site. The most critical knowledge gaps concern primary fracture prevention, risk benefit treatment considerations, and counseling of fracture risk, where data pertaining to the association of areal BMD, clinical risk factors, and fracture outcome are lacking for the Asian population and especially for Asian ethnic subgroups. Future studies should target high risk fracture sites, refinement of fracture risk assessment tools, safety and efficacy of osteoporosis medications, evidence-based guidance regarding treatment, and approaches to optimizing the benefit to risk ratio of pharmacologic therapy in this population.
ACKNOWLEDGEMENT:
This publication was supported by a grant from the National Institute on Aging at the National Institutes of Health (AG069992). The opinions expressed in this review do not represent the official viewpoints of the National Institutes of Health, Kaiser Permanente, or the University of Washington.
Footnotes
Conflict of Interest:
Joan Lo reports funding from the National Institute on Aging at the National Institutes of Health. The authors declare no competing interests.
Human and Animal Rights:
All reported data come from human studies performed by the authors that have been previously published and complied with all applicable institutional review board standards and guidelines.
Code Availability:
Not applicable
REFERENCES
Papers of importance, published more recently, are annotated below
• Of importance
• • Of major importance
- 1.Budiman A, Ruiz NG. Key facts about Asian Americans, a diverse and growing population. April 29, 2021. Pew Research Institute, Washington, DC. https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-americans/ (accessed May 25, 2023). [Google Scholar]
- 2.Budiman A, Ruiz NG. Asian Americans are the fastest-growing racial or ethnic group in the U.S. April 9, 2021. Pew Research Institute, Washington, DC. https://www.pewresearch.org/fact-tank/2021/04/09/asian-americans-are-the-fastest-growing-racial-or-ethnic-group-in-the-u-s/ (accessed May 25, 2023). [Google Scholar]
- 3.Carlson AW. One century of foreign immigration to the United States: 1880–1979. Int Migr. 1985;23(3):309–34. 10.1111/j.1468-2435.1985.tb00322.x [DOI] [PubMed] [Google Scholar]
- 4.Zong J, Batalova J. Frequently requested statistics on immigrants and immigration in the United States. Migration Immigration Source. March 8, 2017. Migration Policy Institute, Washington, DC. http://www.migrationpolicy.org/print/15856#.WPJLepqgu5s (accessed May 25, 2023). [Google Scholar]
- 5.Largest U.S. Immigrant Groups over Time, 1960-Present. Migration Policy Institute, Washington, DC. https://www.migrationpolicy.org/programs/data-hub/charts/largest-immigrant-groups-over-time (accessed May 25, 2023). [Google Scholar]
- 6.Asian American and Pacific Islander Heritage Month: May 2022. Press Release Number CB22-FF05: April 18, 2022. United States Census Bureau. https://www.census.gov/newsroom/facts-for-features/2022/asian-american-pacific-islander.html (accessed May 25, 2023). [Google Scholar]
- 7.United States Census Bureau. https://www.census.gov/. Accessed May 25, 2023.
- 8.Vespa J, Medina L, Armstrong DM. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. Current Population Reports. P25–1144. Issued March 2018, revised February 2020. United States Census Bureau. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf (accessed May 25, 2023). [Google Scholar]
- 9.Hoeffel EM, Rastogi S, Kim MO, Shahid H. The Asian Population: 2010. 2010 Census Briefs. Issued March 2012. United States Census Bureau. https://www2.census.gov/library/publications/cen2010/briefs/c2010br-11.pdf (accessed May 25, 2023). [Google Scholar]
- 10.Johnson H, McGhee E, Mejia MC. California’s Population. Fact Sheet January 2023: Public Policy Institute of California. https://www.ppic.org/publication/californias-population/ (accessed May 25, 2023). [Google Scholar]
- 11.••.Noel SE, Santos MP, Wright NC. Racial and Ethnic Disparities in Bone Health and Outcomes in the United States. J Bone Miner Res. 2021;36(10):1881–905. 10.1002/jbmr.4417. [DOI] [PMC free article] [PubMed] [Google Scholar]; This important and comprehensive review paper summarizes racial and ethnic differences in bone density, fracture, and osteoporosis care that can inform efforts to address bone health disparities.
- 12.Lo JC, Ettinger B. How should we counsel Asian Americans about fracture risk? J Am Geriatr Soc. 2020;68(7):1613–6. 10.1111/jgs.16444 [DOI] [PubMed] [Google Scholar]
- 13.What Census Calls Us. Pew Research Institute, Washington, DC. February 6, 2020. https://www.pewsocialtrends.org/interactives/multiracial-timeline/ (accessed May 25, 2023). [Google Scholar]
- 14.Jain RK, Vokes T. Dual-energy X-ray Absorptiometry. J Clin Densitom. 2017;20(3):291–303. 10.1016/j.jocd.2017.06.014 [DOI] [PubMed] [Google Scholar]
- 15.••.Lo JC, Hui RL, Grimsrud CD, Chandra M, Neugebauer RS, Gonzalez JR, et al. The association of race/ethnicity and risk of atypical femur fracture among older women receiving oral bisphosphonate therapy. Bone. 2016;85:142–7. 10.1016/j.bone.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was the first to quantify the increased risk of atypical femur fracture among Asian compared to White women who received bisphosphonate drugs. An association of AFF and Asian race was first reported by references #28 and #113 in 2012.
- 16.Wysowski DK, Greene P. Trends in osteoporosis treatment with oral and intravenous bisphosphonates in the United States, 2002–2012. Bone. 2013;57(2):423–8. 10.1016/j.bone.2013.09.008 [DOI] [PubMed] [Google Scholar]
- 17.Lauderdale DS, Jacobsen SJ, Furner SE, Levy PS, Brody JA, Goldberg J. Hip fracture incidence among elderly Asian-American populations. Am J Epidemiol. 1997;146(6):502–9. 10.1093/oxfordjournals.aje.a009304 [DOI] [PubMed] [Google Scholar]
- 18.Wright NC, Saag KG, Curtis JR, Smith WK, Kilgore ML, Morrisey MA, et al. Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res. 2012;27(11):2325–32. 10.1002/jbmr.1684 [DOI] [PubMed] [Google Scholar]
- 19.Taylor AJ, Gary LC, Arora T, Becker DJ, Curtis JR, Kilgore ML, et al. Clinical and demographic factors associated with fractures among older Americans. Osteoporos Int. 2011;22(4):1263–74. 10.1007/s00198-010-1300-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.•.Lo JC, Chandra M, Lee DR, Darbinian JA, Gordon NP, Zeltser DW, et al. Sex- and ethnic-specific patterns in the incidence of hip fracture among older US Asian and non-Hispanic White adults. J Am Geriatr Soc. 2023. 10.1111/jgs.18242. [DOI] [PMC free article] [PubMed] [Google Scholar]; This contemporary study describes hip fracture incidence among major US Asian subgroups by sex, including Chinese, Filipino, South Asian, and Japanese adults compared to White adults.
- 21.Sullivan KJ, Husak LE, Altebarmakian M, Brox WT. Demographic factors in hip fracture incidence and mortality rates in California, 2000–2011. J Orthop Surg Res. 2016;11(1):4. 10.1186/s13018-015-0332-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cong E, Walker MD. The Chinese skeleton: insights into microstructure that help to explain the epidemiology of fracture. Bone Res. 2014;2:14009. 10.1038/boneres.2014.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zengin A, Prentice A, Ward KA. Ethnic differences in bone health. Front Endocrinol (Lausanne). 2015;6:24. 10.3389/fendo.2015.00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.•.Durdin R, Parsons CM, Dennison E, Harvey NC, Cooper C, Ward K. Ethnic Differences in Bone Microarchitecture. Curr Osteoporos Rep. 2020;18(6):803–10. 10.1007/s11914-020-00642-y. [DOI] [PMC free article] [PubMed] [Google Scholar]; This recent review summarizes ethnic differences in bone microarchitecture, focusing in particular on studies that use peripheral quantitative computed tomography imaging techniques.
- 25.Nguyen HH, Lakhani A, Shore-Lorenti C, Zebaze R, Vincent AJ, Milat F, et al. Asian ethnicity is associated with atypical femur fractures in an Australian population study. Bone. 2020;135:115319. 10.1016/j.bone.2020.115319 [DOI] [PubMed] [Google Scholar]
- 26.Black DM, Condra K, Adams AL, Eastell R. Bisphosphonates and the risk of atypical femur fractures. Bone. 2022;156:116297. 10.1016/j.bone.2021.116297 [DOI] [PubMed] [Google Scholar]
- 27.••.Black DM, Geiger EJ, Eastell R, Vittinghoff E, Li BH, Ryan DS, et al. Atypical Femur Fracture Risk versus Fragility Fracture Prevention with Bisphosphonates. N Engl J Med. 2020;383(8):743–53. 10.1056/NEJMoa1916525. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reports the association of bisphophonate treatment duration and the risk of atypical femur fracture, the increased risk associated with Asian race, and risk reduction after treatment cessation. The authors also provide estimated risk-benefit projections.
- 28.Lo JC, Huang SY, Lee GA, Khandelwal S, Provus J, Ettinger B, et al. Clinical correlates of atypical femoral fracture. Bone. 2012;51(1):181–4. 10.1016/j.bone.2012.02.632 [DOI] [PubMed] [Google Scholar]
- 29.Neviaser AS, Lane JM, Lenart BA, Edobor-Osula F, Lorich DG. Low-energy femoral shaft fractures associated with alendronate use. J Orthop Trauma. 2008;22(5):346–50. 10.1097/BOT.0b013e318172841c [DOI] [PubMed] [Google Scholar]
- 30.Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90(3):1294–301. 10.1210/jc.2004-0952 [DOI] [PubMed] [Google Scholar]
- 31.Lenart BA, Lorich DG, Lane JM. Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med. 2008;358(12):1304–6. 10.1056/NEJMc0707493 [DOI] [PubMed] [Google Scholar]
- 32.Goh SK, Yang KY, Koh JS, Wong MK, Chua SY, Chua DT, et al. Subtrochanteric insufficiency fractures in patients on alendronate therapy: a caution. J Bone Joint Surg Br. 2007;89(3):349–53. 10.1302/0301-620X.89B3.18146 [DOI] [PubMed] [Google Scholar]
- 33.Kwek EB, Goh SK, Koh JS, Png MA, Howe TS. An emerging pattern of subtrochanteric stress fractures: a long-term complication of alendronate therapy? Injury. 2008;39(2):224–31. 10.1016/j.injury.2007.08.036 [DOI] [PubMed] [Google Scholar]
- 34.Ammann P, Rizzoli R. Bone strength and its determinants. Osteoporos Int. 2003;14 Suppl 3:S13–8. 10.1007/s00198-002-1345-4 [DOI] [PubMed] [Google Scholar]
- 35.Marshall LM, Zmuda JM, Chan BK, Barrett-Connor E, Cauley JA, Ensrud KE, et al. Race and ethnic variation in proximal femur structure and BMD among older men. J Bone Miner Res. 2008;23(1):121–30. 10.1359/jbmr.070908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Finkelstein JS, Lee ML, Sowers M, Ettinger B, Neer RM, Kelsey JL, et al. Ethnic variation in bone density in premenopausal and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab. 2002;87(7):3057–67. 10.1210/jcem.87.7.8654 [DOI] [PubMed] [Google Scholar]
- 37.Marquez MA, Melton LJ 3rd, Muhs JM, Crowson CS, Tosomeen A, O’Connor MK, et al. Bone density in an immigrant population from Southeast Asia. Osteoporos Int. 2001;12(7):595–604. 10.1007/s001980170083 [DOI] [PubMed] [Google Scholar]
- 38.Khandelwal S, Chandra M, Lo JC. Clinical characteristics, bone mineral density and non-vertebral osteoporotic fracture outcomes among post-menopausal U.S. South Asian women. Bone. 2012;51(6):1025–8. 10.1016/j.bone.2012.08.118 [DOI] [PubMed] [Google Scholar]
- 39.Lo JC, Chandra M, Lee C, Darbinian JA, Ramaswamy M, Ettinger B. Bone mineral density in older U.S. Filipino, Chinese, Japanese, and White women. J Am Geriatr Soc. 2020;68(11):2656–61. 10.1111/jgs.16785 [DOI] [PubMed] [Google Scholar]
- 40.Faulkner KG. The tale of the T-score: review and perspective. Osteoporos Int. 2005;16(4):347–52. 10.1007/s00198-004-1779-y [DOI] [PubMed] [Google Scholar]
- 41.Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9(8):1137–41. 10.1002/jbmr.5650090802 [DOI] [PubMed] [Google Scholar]
- 42.Binkley NC, Schmeer P, Wasnich RD, Lenchik L, International Society for Clinical Densitometry Position Development P, Scientific Advisory C. What are the criteria by which a densitometric diagnosis of osteoporosis can be made in males and non-Caucasians? J Clin Densitom. 2002;5 Suppl:S19–27. 10.1385/jcd:5:3s:s19 [DOI] [PubMed] [Google Scholar]
- 43.Bonnick SL. Bone Densitometry in Clinical Practice. Third ed. New York: Humana Press; 2010. [Google Scholar]
- 44.Chen Z, Maricic M, Lund P, Tesser J, Gluck O. How the new Hologic hip normal reference values affect the densitometric diagnosis of osteoporosis. Osteoporos Int. 1998;8(5):423–7. 10.1007/s001980050086 [DOI] [PubMed] [Google Scholar]
- 45.Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, et al. Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int. 1998;8(5):468–89. 10.1007/s001980050093 [DOI] [PubMed] [Google Scholar]
- 46.Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, et al. Proximal femur bone mineral levels of US adults. Osteoporos Int. 1995;5(5):389–409. 10.1007/BF01622262 [DOI] [PubMed] [Google Scholar]
- 47.Melamed A, Vittinghoff E, Sriram U, Schwartz AV, Kanaya AM. BMD reference standards among South Asians in the United States. J Clin Densitom. 2010;13(4):379–84. 10.1016/j.jocd.2010.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Walker MD, Babbar R, Opotowsky AR, Rohira A, Nabizadeh F, Badia MD, et al. A referent bone mineral density database for Chinese American women. Osteoporos Int. 2006;17(6):878–87. 10.1007/s00198-005-0059-9 [DOI] [PubMed] [Google Scholar]
- 49.Lo JC, Kim S, Chandra M, Ettinger B. Applying ethnic-specific bone mineral density T-scores to Chinese women in the USA. Osteoporos Int. 2016;27(12):3477–84. 10.1007/s00198-016-3673-9 [DOI] [PubMed] [Google Scholar]
- 50.Binkley N, Bilezikian JP, Kendler DL, Leib ES, Lewiecki EM, Petak SM, et al. Official positions of the International Society for Clinical Densitometry and Executive Summary of the 2005 Position Development Conference. J Clin Densitom. 2006;9(1):4–14. 10.1016/j.jocd.2006.05.002 [DOI] [PubMed] [Google Scholar]
- 51.Schousboe JT, Shepherd JA, Bilezikian JP, Baim S. Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitom. 2013;16(4):455–66. 10.1016/j.jocd.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 52.2019 ISCD Official Positions: Adult. International Society for Clinical Densitometry. 2019. https://iscd.org/learn/official-positions/adult-positions/ (accessed May 25, 2023).
- 53.LeBoff MS, Greenspan SL, Insogna KL, Lewiecki EM, Saag KG, Singer AJ, et al. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022;33(10):2049–102. 10.1007/s00198-021-05900-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42(3):467–75. 10.1016/j.bone.2007.11.001 [DOI] [PubMed] [Google Scholar]
- 55.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–73. 10.1056/NEJM199503233321202 [DOI] [PubMed] [Google Scholar]
- 56.Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001;286(22):2815–22. 10.1001/jama.286.22.2815 [DOI] [PubMed] [Google Scholar]
- 57.Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20(2):185–94. 10.1359/JBMR.041007 [DOI] [PubMed] [Google Scholar]
- 58.Felsenberg D, Boonen S. The bone quality framework: determinants of bone strength and their interrelationships, and implications for osteoporosis management. Clin Ther. 2005;27(1):1–11. 10.1016/j.clinthera.2004.12.020 [DOI] [PubMed] [Google Scholar]
- 59.Walker MD, McMahon DJ, Udesky J, Liu G, Bilezikian JP. Application of high-resolution skeletal imaging to measurements of volumetric BMD and skeletal microarchitecture in Chinese-American and white women: explanation of a paradox. J Bone Miner Res. 2009;24(12):1953–9. 10.1359/jbmr.090528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu XS, Walker MD, McMahon DJ, Udesky J, Liu G, Bilezikian JP, et al. Better skeletal microstructure confers greater mechanical advantages in Chinese-American women versus white women. J Bone Miner Res. 2011;26(8):1783–92. 10.1002/jbmr.378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Walker MD, Liu XS, Stein E, Zhou B, Bezati E, McMahon DJ, et al. Differences in bone microarchitecture between postmenopausal Chinese-American and white women. J Bone Miner Res. 2011;26(7):1392–8. 10.1002/jbmr.352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N, et al. Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res. 2014;29(3):518–30. 10.1002/jbmr.2176 [DOI] [PubMed] [Google Scholar]
- 63.Silva BC, Walker MD, Abraham A, Boutroy S, Zhang C, McMahon DJ, et al. Trabecular bone score is associated with volumetric bone density and microarchitecture as assessed by central QCT and HRpQCT in Chinese American and white women. J Clin Densitom. 2013;16(4):554–61. 10.1016/j.jocd.2013.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Leslie WD, Aubry-Rozier B, Lamy O, Hans D, Manitoba Bone Density P. TBS (trabecular bone score) and diabetes-related fracture risk. J Clin Endocrinol Metab. 2013;98(2):602–9. 10.1210/jc.2012-3118 [DOI] [PubMed] [Google Scholar]
- 65.Cheng YJ, Kanaya AM, Araneta MRG, Saydah SH, Kahn HS, Gregg EW, et al. Prevalence of Diabetes by Race and Ethnicity in the United States, 2011–2016. JAMA. 2019;322(24):2389–98. 10.1001/jama.2019.19365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Looker AC, Sarafrazi Isfahani N, Fan B, Shepherd JA. Trabecular bone scores and lumbar spine bone mineral density of US adults: comparison of relationships with demographic and body size variables. Osteoporos Int. 2016;27(8):2467–75. 10.1007/s00198-016-3550-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jain RK, Vokes TJ. African Americans have lower TBS than whites among densitometry patients at a Chicago academic center. Osteoporos Int. 2017;28(3):917–23. 10.1007/s00198-016-3796-z [DOI] [PubMed] [Google Scholar]
- 68.•.Cauley JA, Karlamangla AS, Ruppert K, Lian Y, Huang M, Harlow S, et al. Race/ethnic difference in trabecular bone score in midlife women: The Study of Women’s Health Across the Nation (SWAN). Arch Osteoporos. 2021;16(1):91. 10.1007/s11657-021-00951-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; This report from the Study of Women’s Health Across the Nation found that trabecular bone score was similar in Black and White women after accounting for tissue thickness and covariates, whereas Japanese women had modestly lower trabecular bone score.
- 69.Jain RK, Vokes T. Association of trabecular bone score (TBS) and prior fracture differs among minorities in NHANES 2005–2008. Osteoporos Int. 2018;29(9):2093–9. 10.1007/s00198-018-4584-8 [DOI] [PubMed] [Google Scholar]
- 70.Faulkner KG, Cummings SR, Black D, Palermo L, Gluer CC, Genant HK. Simple measurement of femoral geometry predicts hip fracture: the Study of Osteoporotic Fractures. J Bone Miner Res. 1993;8(10):1211–7. 10.1002/jbmr.5650081008 [DOI] [PubMed] [Google Scholar]
- 71.Cummings SR, Cauley JA, Palermo L, Ross PD, Wasnich RD, Black D, et al. Racial differences in hip axis lengths might explain racial differences in rates of hip fracture. Study of Osteoporotic Fractures Research Group. Osteoporos Int. 1994;4(4):226–9. 10.1007/BF01623243 [DOI] [PubMed] [Google Scholar]
- 72.Brownbill RA, Ilich JZ. Hip geometry and its role in fracture: what do we know so far? Curr Osteoporos Rep. 2003;1(1):25–31. 10.1007/s11914-003-0005-8 [DOI] [PubMed] [Google Scholar]
- 73.Danielson ME, Beck TJ, Lian Y, Karlamangla AS, Greendale GA, Ruppert K, et al. Ethnic variability in bone geometry as assessed by hip structure analysis: findings from the hip strength across the menopausal transition study. J Bone Miner Res. 2013;28(4):771–9. 10.1002/jbmr.1781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ishii S, Cauley JA, Greendale GA, Danielson ME, Safaei Nili N, Karlamangla A. Ethnic differences in composite indices of femoral neck strength. Osteoporos Int. 2012;23(4):1381–90. 10.1007/s00198-011-1723-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nagaraj N, Boudreau RM, Danielson ME, Greendale GA, Karlamangla AS, Beck TJ, et al. Longitudinal changes in hip geometry in relation to the final menstrual period: Study of Women’s Health Across the Nation (SWAN). Bone. 2019;122:237–45. 10.1016/j.bone.2019.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.•.Hsu S, Hoofnagle AN, Gupta DK, Gutierrez OM, Peralta CA, Shea S, et al. Race, ancestry, and vitamin D metabolism: the Multi-Ethnic Study of Atherosclerosis. J Clin Endocrinol Metab. 2020;105(12):e4337–50. 10.1210/clinem/dgaa612. [DOI] [PMC free article] [PubMed] [Google Scholar]; This report from the Multi-Ethnic Study of Atherosclerosis examines racial and ethnic differences in vitamin D metabolism measures, including White, Black, Chinese, and Hispanic adults and relationship with ancestry.
- 77.Oshiro CE, Hillier TA, Edmonds G, Peterson M, Hill PL, Hampson S. Vitamin D deficiency and insufficiency in Hawaii: Levels and sources of serum vitamin D in older adults. Am J Hum Biol. 2021:e23636. 10.1002/ajhb.23636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gordon NP, Caan BJ, Asgari MM. Variation in vitamin D supplementation among adults in a multi-race/ethnic health plan population, 2008. Nutr J. 2012;11:104. 10.1186/1475-2891-11-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Darling AL. Vitamin D deficiency in western dwelling South Asian populations: an unrecognised epidemic. Proc Nutr Soc. 2020;79(3):259–71. 10.1017/S0029665120000063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Herrick KA, Storandt RJ, Afful J, Pfeiffer CM, Schleicher RL, Gahche JJ, et al. Vitamin D status in the United States, 2011–2014. Am J Clin Nutr. 2019;110(1):150–7. 10.1093/ajcn/nqz037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ho SB, Li CF, Chandra M, Lo JC. Vitamin D status among women of different Asian subgroups initiating osteoporosis therapy J Asian Health. 2023;3(1):February. 10.59448/jah.v3i1.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li CF, Ettinger B, Chandra M, Lo JC. Vitamin D status among older women initiating osteoporosis therapy. J Am Geriatr Soc. 2019;67(10):2207–8. 10.1111/jgs.16133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stratton-Loeffler MJ, Lo JC, Hui RL, Coates A, Minkoff JR, Budayr A. Treatment of vitamin D deficiency within a large integrated health care delivery system. J Manag Care Pharm. 2012;18(7):497–505. 10.18553/jmcp.2012.18.7.497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.LeBoff MS, Chou SH, Ratliff KA, Cook NR, Khurana B, Kim E, et al. Supplemental vitamin D and incident fractures in midlife and older adults. N Engl J Med. 2022;387(4):299–309. 10.1056/NEJMoa2202106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Balk EM, Adam GP, Langberg VN, Earley A, Clark P, Ebeling PR, et al. Global dietary calcium intake among adults: a systematic review. Osteoporos Int. 2017;28(12):3315–24. 10.1007/s00198-017-4230-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.•.Ali SH, Yi SS, Kranick J, Lee M, Thorpe LE, Rummo PE. Disentangling the roles of generational status and acculturation on dietary behaviors in disaggregated Asian American subgroups. Appetite. 2022;171:105903. 10.1016/j.appet.2021.105903. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper examines the association of generational status and acculturation in a surveyed cohort of 3018 Asian American adults and includes findings among disaggregated Asian subgroups
- 87.Dai Z, Wang R, Ang LW, Yuan JM, Koh WP. Bone turnover biomarkers and risk of osteoporotic hip fracture in an Asian population. Bone. 2016;83:171–7. 10.1016/j.bone.2015.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tamaki J, Iki M, Kadowaki E, Sato Y, Chiba Y, Akiba T, et al. Biochemical markers for bone turnover predict risk of vertebral fractures in postmenopausal women over 10 years: the Japanese Population-based Osteoporosis (JPOS) Cohort Study. Osteoporos Int. 2013;24(3):887–97. 10.1007/s00198-012-2106-7 [DOI] [PubMed] [Google Scholar]
- 89.Zhao J, Xia W, Nie M, Zheng X, Wang Q, Wang X, et al. The levels of bone turnover markers in Chinese postmenopausal women: Peking Vertebral Fracture study. Menopause. 2011;18(11):1237–43. 10.1097/gme.0b013e31821d7ff7 [DOI] [PubMed] [Google Scholar]
- 90.Sowers MR, Zheng H, Greendale GA, Neer RM, Cauley JA, Ellis J, et al. Changes in bone resorption across the menopause transition: effects of reproductive hormones, body size, and ethnicity. J Clin Endocrinol Metab. 2013;98(7):2854–63. 10.1210/jc.2012-4113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Finkelstein JS, Brockwell SE, Mehta V, Greendale GA, Sowers MR, Ettinger B, et al. Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J Clin Endocrinol Metab. 2008;93(3):861–8. 10.1210/jc.2007-1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sowers MR, Greendale GA, Bondarenko I, Finkelstein JS, Cauley JA, Neer RM, et al. Endogenous hormones and bone turnover markers in pre- and perimenopausal women: SWAN. Osteoporos Int. 2003;14(3):191–7. 10.1007/s00198-002-1329-4 [DOI] [PubMed] [Google Scholar]
- 93.Finkelstein JS, Sowers M, Greendale GA, Lee ML, Neer RM, Cauley JA, et al. Ethnic variation in bone turnover in pre- and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab. 2002;87(7):3051–6. 10.1210/jcem.87.7.8480 [DOI] [PubMed] [Google Scholar]
- 94.Arasu A, Cawthon PM, Lui LY, Do TP, Arora PS, Cauley JA, et al. Serum sclerostin and risk of hip fracture in older Caucasian women. J Clin Endocrinol Metab. 2012;97(6):2027–32. 10.1210/jc.2011-3419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Costa AG, Walker MD, Zhang CA, Cremers S, Dworakowski E, McMahon DJ, et al. Circulating sclerostin levels and markers of bone turnover in Chinese-American and white women. J Clin Endocrinol Metab. 2013;98(12):4736–43. 10.1210/jc.2013-2106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Silverman SL, Madison RE. Decreased incidence of hip fracture in Hispanics, Asians, and blacks: California Hospital Discharge Data. Am J Public Health. 1988;78(11):1482–3. 10.2105/ajph.78.11.1482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zingmond DS, Melton LJ 3rd, Silverman SL. Increasing hip fracture incidence in California Hispanics, 1983 to 2000. Osteoporos Int. 2004;15(8):603–10. 10.1007/s00198-004-1592-7 [DOI] [PubMed] [Google Scholar]
- 98.Lo JC, Zheng P, Grimsrud CD, Chandra M, Ettinger B, Budayr A, et al. Racial/ethnic differences in hip and diaphyseal femur fractures. Osteoporos Int. 2014;25(9):2313–8. 10.1007/s00198-014-2750-1 [DOI] [PubMed] [Google Scholar]
- 99.Ross PD, Norimatsu H, Davis JW, Yano K, Wasnich RD, Fujiwara S, et al. A comparison of hip fracture incidence among native Japanese, Japanese Americans, and American Caucasians. Am J Epidemiol. 1991;133(8):801–9. 10.1093/oxfordjournals.aje.a115959 [DOI] [PubMed] [Google Scholar]
- 100.Gordon NP, Lin TY, Rau J, Lo JC. Aggregation of Asian-American subgroups masks meaningful differences in health and health risks among Asian ethnicities: an electronic health record based cohort study. BMC Public Health. 2019;19(1):1551. 10.1186/s12889-019-7683-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shah NS, Luncheon C, Kandula NR, Khan SS, Pan L, Gillespie C, et al. Heterogeneity in Obesity Prevalence Among Asian American Adults. Ann Intern Med. 2022;175(11):1493–500. 10.7326/M22-0609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Geng Y, Lo JC, Brickner L, Gordon NP. Racial-Ethnic Differences in Fall Prevalence among Older Women: A Cross-Sectional Survey Study. BMC Geriatr. 2017;17(1):65. 10.1186/s12877-017-0447-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cauley JA, Wu L, Wampler NS, Barnhart JM, Allison M, Chen Z, et al. Clinical risk factors for fractures in multi-ethnic women: the Women’s Health Initiative. J Bone Miner Res. 2007;22(11):1816–26. 10.1359/jbmr.070713 [DOI] [PubMed] [Google Scholar]
- 104.•.Lo JC, Lee DR, Chandra M, Zeltser DW, Chu CE, Gordon NP, et al. Differences in proximal humerus and wrist fracture incidence among US Asian subgroups. J Am Geriatr Soc. 2023. 10.1111/jgs.18408. [DOI] [PMC free article] [PubMed] [Google Scholar]; This contemporary study describes proximal humerus and wrist fracture incidence among major US Asian subgroups by sex, including Chinese, Filipino, South Asian, and Japanese adults compared to White adults.
- 105.Shieh A, Ruppert KM, Greendale GA, Lian Y, Cauley JA, Burnett-Bowie SA, et al. Associations of Age at Menopause With Postmenopausal Bone Mineral Density and Fracture Risk in Women. J Clin Endocrinol Metab. 2022;107(2):e561–e9. 10.1210/clinem/dgab690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28(5):1531–42. 10.1007/s00198-017-3909-3 [DOI] [PubMed] [Google Scholar]
- 107.Xia W, Liu Q, Lv J, Zhang Z, Wu W, Xie Z, et al. Prevalent vertebral fractures among urban-dwelling Chinese postmenopausal women: a population-based, randomized-sampling, cross-sectional study. Arch Osteoporos. 2022;17(1):120. 10.1007/s11657-022-01158-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bow CH, Cheung E, Cheung CL, Xiao SM, Loong C, Soong C, et al. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int. 2012;23(3):879–85. 10.1007/s00198-011-1627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29(1):1–23. 10.1002/jbmr.1998 [DOI] [PubMed] [Google Scholar]
- 110.Ettinger B, Burr DB, Ritchie RO. Proposed pathogenesis for atypical femoral fractures: Lessons from material research. Bone. 2013;55(2):495–500. 10.1016/j.bone.2013.02.004 [DOI] [PubMed] [Google Scholar]
- 111.Lo JC, Grimsrud CD, Ott SM, Chandra M, Hui RL, Ettinger B. Atypical femur fracture incidence in women increases with duration of bisphosphonate exposure. Osteoporos Int. 2019;30(12):2515–20. 10.1007/s00198-019-05112-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lo JC, Neugebauer RS, Ettinger B, Chandra M, Hui RL, Ott SM, et al. Risk of complete atypical femur fracture with oral bisphosphonate exposure beyond three years. BMC Musculoskelet Disord. 2020;21(1):801. 10.1186/s12891-020-03672-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dell RM, Adams AL, Greene DF, Funahashi TT, Silverman SL, Eisemon EO, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res. 2012;27(12):2544–50. 10.1002/jbmr.1719 [DOI] [PubMed] [Google Scholar]
- 114.Schilcher J, Koeppen V, Aspenberg P, Michaelsson K. Risk of atypical femoral fracture during and after bisphosphonate use. Acta Orthop. 2015;86(1):100–7. 10.3109/17453674.2015.1004149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kim JW, Kim JJ, Byun YS, Shon OJ, Oh HK, Park KC, et al. Factors affecting fracture location in atypical femoral fractures: A cross-sectional study with 147 patients. Injury. 2017;48(7):1570–4. 10.1016/j.injury.2017.05.033 [DOI] [PubMed] [Google Scholar]
- 116.Chen LP, Chang TK, Huang TY, Kwok TG, Lu YC. The correlation between lateral bowing angle of the femur and the location of atypical femur fractures. Calcif Tissue Int. 2014;95(3):240–7. 10.1007/s00223-014-9887-y [DOI] [PubMed] [Google Scholar]
- 117.Koh JS, Goh SK, Png MA, Ng AC, Howe TS. Distribution of atypical fractures and cortical stress lesions in the femur: implications on pathophysiology. Singapore Med J. 2011;52(2):77–80. [PubMed] [Google Scholar]
- 118.Ng AC, Png MA, Chua DT, Koh JS, Howe TS. Review: Epidemiology and Pathophysiology of Atypical Femur Fractures. Curr Osteoporos Rep. 2014;12(1):65–73. 10.1007/s11914-014-0198-z [DOI] [PubMed] [Google Scholar]
- 119.Taormina DP, Marcano AI, Karia R, Egol KA, Tejwani NC. Symptomatic atypical femoral fractures are related to underlying hip geometry. Bone. 2014;63:1–6. 10.1016/j.bone.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 120.Haider IT, Schneider PS, Edwards WB. The role of lower-limb geometry in the pathophysiology of atypical femoral fracture. Curr Osteoporos Rep. 2019;17(5):281–90. 10.1007/s11914-019-00525-x [DOI] [PubMed] [Google Scholar]
- 121.•.Dhanekula ND, Crouch G, Byth K, Lau SL, Kim A, Graham E, et al. Asian ethnicity and femoral geometry in atypical femur fractures: Independent or interdependent risk factors? JBMR Plus. 2022;6(4):e10607. 10.1002/jbm4.10607. [DOI] [PMC free article] [PubMed] [Google Scholar]; This Australian study examines femur geometry in women with atypical or typical femur fracture and identifies Asian ethnicity as a strong predictor of atypical femur fracture, independent of hip geometry.
- 122.Black DM, Abrahamsen B, Bouxsein ML, Einhorn T, Napoli N. Atypical femur fractures: review of epidemiology, relationship to bisphosphonates, prevention, and clinical management. Endocr Rev. 2019;40(2):333–68. 10.1210/er.2018-00001 [DOI] [PubMed] [Google Scholar]
- 123.Zhou W, van Rooij JGJ, Ebeling PR, Verkerk A, Zillikens MC. The genetics of atypical femur fractures – a systematic review. Curr Osteoporos Rep. 2021;19(2):123–30. 10.1007/s11914-021-00658-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ott SM, Heckbert SR. Atypical femur fracture risk versus fragility fracture prevention with bisphosphonates. N Engl J Med. 2020;383(22):2188–9. 10.1056/NEJMc2029828 [DOI] [PubMed] [Google Scholar]
- 125.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348(9041):1535–41. 10.1016/s0140-6736(96)07088-2 [DOI] [PubMed] [Google Scholar]
- 126.Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA. 1998;280(24):2077–82. 10.1001/jama.280.24.2077 [DOI] [PubMed] [Google Scholar]
- 127.McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, et al. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001;344(5):333–40. 10.1056/NEJM200102013440503 [DOI] [PubMed] [Google Scholar]
- 128.Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357(18):1799–809. 10.1056/NEJMoa074941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dawson-Hughes B, Tosteson AN, Melton LJ 3rd, Baim S, Favus MJ, Khosla S, et al. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int. 2008;19(4):449–58. 10.1007/s00198-008-0559-5 [DOI] [PubMed] [Google Scholar]
- 130.•.Leslie WD, Morin SN, Lix LM, McCloskey EV, Johansson H, Harvey NC, et al. Fracture prediction from FRAX for Canadian ethnic groups: a registry-based cohort study. Osteoporos Int. 2021;32(1):113–22. 10.1007/s00198-020-05594-8. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates the overestimation of fracture risk in Canadian Asian and Black women when the Canadian FRAX calculator is used. Overestimation is reduced with US ethnic FRAX calculators.
- 131.Lewiecki EM, Wright NC, Singer AJ. Racial disparities, FRAX, and the care of patients with osteoporosis. Osteoporos Int. 2020;31(11):2069–71. 10.1007/s00198-020-05655-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kanis JA, Johansson H, Harvey NC, McCloskey EV. A brief history of FRAX. Arch Osteoporos. 2018;13(1):118. 10.1007/s11657-018-0510-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kanis JA, Harvey NC, Johansson H, Oden A, Leslie WD, McCloskey EV. FRAX update. J Clin Densitom. 2017;20(3):360–7. 10.1016/j.jocd.2017.06.022 [DOI] [PubMed] [Google Scholar]
- 134.Wu JY. Considering race and ethnicity in the management of bone health. J Bone Miner Res. 2021;36(10):1879–80. 10.1002/jbmr.4437 [DOI] [PubMed] [Google Scholar]
- 135.Morin SN, Berger C, Papaioannou A, Cheung AM, Rahme E, Leslie WD, et al. Race/ethnic differences in the prevalence of osteoporosis, falls and fractures: a cross-sectional analysis of the Canadian Longitudinal Study on Aging. Osteoporos Int. 2022;33(12):2637–48. 10.1007/s00198-022-06539-z [DOI] [PubMed] [Google Scholar]
- 136.Fujiwara S, Huang C, Ross PD, Yamada M, Kodama K, Davis JW, et al. Differences in health characteristics between native Japanese and Japanese-Americans. J Cross Cult Gerontol. 1999;14(3):273–87. 10.1023/a:1006627908855 [DOI] [PubMed] [Google Scholar]
- 137.Kin K, Lee JH, Kushida K, Sartoris DJ, Ohmura A, Clopton PL, et al. Bone density and body composition on the Pacific Rim: a comparison between Japan-born and U.S.-born Japanese-American women. J Bone Miner Res. 1993;8(7):861–9. 10.1002/jbmr.5650080712 [DOI] [PubMed] [Google Scholar]
- 138.Ferrari SL, Abrahamsen B, Napoli N, Akesson K, Chandran M, Eastell R, et al. Diagnosis and management of bone fragility in diabetes: an emerging challenge. Osteoporos Int. 2018;29(12):2585–96. 10.1007/s00198-018-4650-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Leslie WD, Johansson H, McCloskey EV, Harvey NC, Kanis JA, Hans D. Comparison of methods for improving fracture risk assessment in diabetes: The Manitoba BMD Registry. J Bone Miner Res. 2018;33(11):1923–30. 10.1002/jbmr.3538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.••.Vandenput L, Johansson H, McCloskey EV, Liu E, Akesson KE, Anderson FA, et al. Update of the fracture risk prediction tool FRAX: a systematic review of potential cohorts and analysis plan. Osteoporos Int. 2022;33(10):2103–36. 10.1007/s00198-022-06435-6. [DOI] [PubMed] [Google Scholar]; This important report describes plans to assemble international cohorts with prospective data on incident fracture outcomes and baseline risk factors to inform an updated FRAX tool. Ethnicity-specific risk will also be examined.
- 141.Kuruvilla K, Kenny AM, Raisz LG, Kerstetter JE, Feinn RS, Rajan TV. Importance of bone mineral density measurements in evaluating fragility bone fracture risk in Asian Indian men. Osteoporos Int. 2011;22(1):217–21. 10.1007/s00198-010-1237-y [DOI] [PubMed] [Google Scholar]
- 142.Johansson H, Oden A, Lorentzon M, McCloskey E, Kanis JA, Harvey NC, et al. Is the Swedish FRAX model appropriate for Swedish immigrants? Osteoporos Int. 2015;26(11):2617–22. 10.1007/s00198-015-3180-4 [DOI] [PubMed] [Google Scholar]
- 143.McCloskey EV, Harvey NC, Johansson H, Kanis JA. FRAX updates 2016. Curr Opin Rheumatol. 2016;28(4):433–41. 10.1097/BOR.0000000000000304 [DOI] [PubMed] [Google Scholar]
- 144.Chan DC, McCloskey EV, Chang CB, Lin KP, Lim LC, Tsai KS, et al. Establishing and evaluating FRAX probability thresholds in Taiwan. J Formos Med Assoc. 2017;116(3):161–8. 10.1016/j.jfma.2016.03.006 [DOI] [PubMed] [Google Scholar]
- 145.Lo JC, Nath S, Patel M, Chandra M, Yang B, Weintraub MR, et al. Variation in fracture risk estimation among East Asian women. Am J Manag Care. 2021;27(3):e97–e100. 10.37765/ajmc.2021.88604 [DOI] [PubMed] [Google Scholar]
- 146.Cauley JA, Chalhoub D, Kassem AM, Fuleihan Gel H. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10(6):338–51. 10.1038/nrendo.2014.51 [DOI] [PubMed] [Google Scholar]
- 147.Megyesi MS, Hunt LM, Brody H. A critical review of racial/ethnic variables in osteoporosis and bone density research. Osteoporos Int. 2011;22(6):1669–79. 10.1007/s00198-010-1503-z [DOI] [PubMed] [Google Scholar]
- 148.Leslie WD. Clinical review: Ethnic differences in bone mass--clinical implications. J Clin Endocrinol Metab. 2012;97(12):4329–40. 10.1210/jc.2012-2863 [DOI] [PubMed] [Google Scholar]
- 149.Rose VL. NOF urges bone density tests for certain postmenopausal women and all women over age 65. Am Fam Physician. 1999;59(4):1047, 51. [PubMed] [Google Scholar]
- 150.Osteoporosis Screening in Older Women (OSW). HEDIS Measures and Technical Resources. National Committee for Quality Assurance, 2023. https://www.ncqa.org/hedis/measures/osteoporosis-screening-in-older-women/ (accessed May 25, 2023).
- 151.Bala Y, Depalle B, Farlay D, Douillard T, Meille S, Follet H, et al. Bone micromechanical properties are compromised during long-term alendronate therapy independently of mineralization. J Bone Miner Res. 2012;27(4):825–34. 10.1002/jbmr.1501 [DOI] [PubMed] [Google Scholar]
- 152.Ott SM. Consider the Bisphosphonate Dose. J Bone Miner Res. 2022;37(1):1–2. 10.1002/jbmr.4479 [DOI] [PubMed] [Google Scholar]
- 153.Adler RA, El-Hajj Fuleihan G, Bauer DC, Camacho PM, Clarke BL, Clines GA, et al. Managing osteoporosis in patients on long-term bisphosphonate treatment: Report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016;31(10):1910. 10.1002/jbmr.2918 [DOI] [PubMed] [Google Scholar]
- 154.Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, et al. Japanese 2011 guidelines for prevention and treatment of osteoporosis--executive summary. Arch Osteoporos. 2012;7(1–2):3–20. 10.1007/s11657-012-0109-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.••.Reid IR, Horne AM, Mihov B, Stewart A, Garratt E, Wong S, et al. Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med. 2018;379(25):2407–16. 10.1056/NEJMoa1808082. [DOI] [PubMed] [Google Scholar]; This randomized trial compared four 18-month infusions of zoledronate to placebo among women aged ≥65 years with osteopenia and found that the risk of nonvertebral or vertebral fracture was much lower in the zoledronate group.
- 156.••.Grey A, Bolland MJ, Horne A, Mihov B, Gamble G, Reid IR. Bone mineral density and bone turnover 10 Years after a single 5 mg dose or two 5-yearly lower doses of zoledronate in osteopenic older women: An open-label extension of a randomized controlled trial. J Bone Miner Res. 2022;37(1):3–11. 10.1002/jbmr.4453. [DOI] [PubMed] [Google Scholar]; This open label extension study reported higher bone mineral density and lower bone resorption marker levels at 9–10 years following a single 5 mg dose of zoledronate or two 2.5 mg doses given at 5 year intervals.
- 157.Morton DJ, Barrett-Connor E, Kritz-Silverstein D, Wingard DL, Schneider DL. Bone mineral density in postmenopausal Caucasian, Filipina, and Hispanic women. Int J Epidemiol. 2003;32(1):150–6. 10.1093/ije/dyg024 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable


