Video
Video describing the case, procedure, and outcomes.
Small intestinal strictures that are distal to the duodenum, particularly the jejunum, are challenging to manage. Uncovered self-expandable metal stents have been used in the past, but covered stents could not be used because of their large size, rigidity, and inability to pass through the endoscope channel.1,2 Biodegradable stents were also used, but migration and mucosal hyperplasia were reported.3 A double-balloon enteroscopy was used for strictures in the past, but it is unable to place stents.4 Unfortunately, the double-balloon enteroscopy technique is only suitable for strictures less than 3 cm and is often not feasible because of adhesions.5,6 We describe the case of a jejunal stricture caused by a primitive neuroectodermal tumor (PNET) that was managed palliatively by placing 3 esophageal stents in the proximal jejunum using a pediatric colonoscope (Video 1, available online at www.videogie.org).
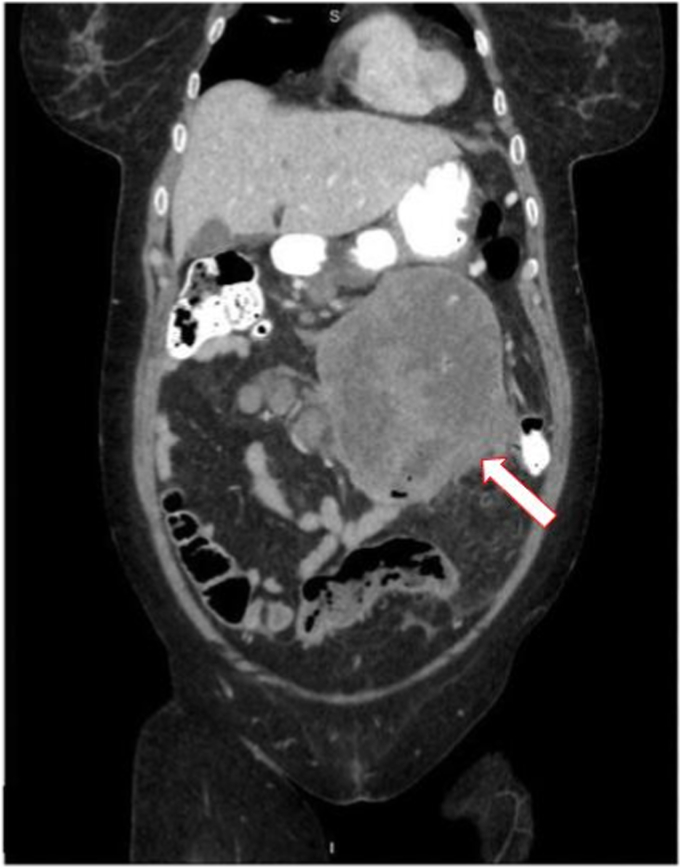
A 56-year-old woman with hypertension, obstructive lung disease, and a prior ischemic stroke presented to the hospital for 4 days of postprandial emesis, abdominal distention, epigastric pain, and constipation. She previously underwent appendectomy and hysterectomy, and she had no prior endoscopic studies. A CT scan was performed, demonstrating a large mid-abdominal mass, mural thickening of the distal duodenum, and partial occlusion of the small bowel with regional lymphadenopathy (Fig. 1). An EGD was performed and showed severe stenosis with biopsy specimens taken, which demonstrated histology consistent with PNET. The patient provided informed consent to this publication.
Figure 1.
Coronal CT image of a large abdominal mass involving loops of bowel and jejunum. The arrow points to the mass.
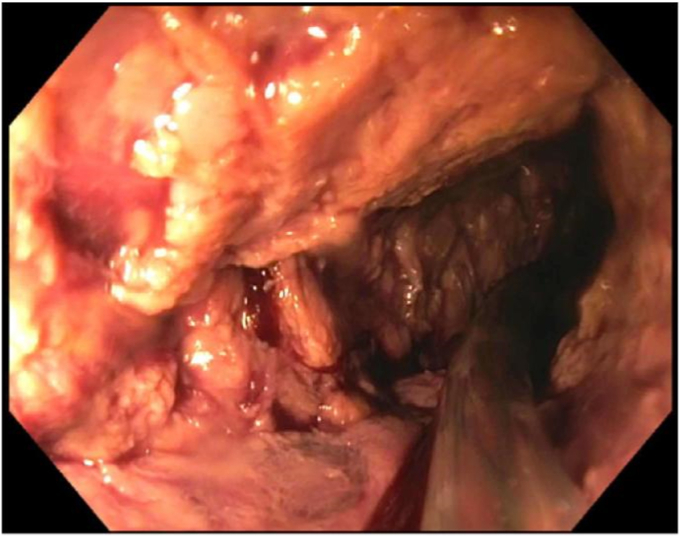
Given the presence of mesenteric adhesion and extensive stenosis, it was decided to treat the stricture endoscopically rather than with surgical intervention. A pediatric colonoscope was advanced to the distal duodenum, where a mass-like area with no normal bowel mucosa was seen (Fig. 2). To prevent blindly advancing the pediatric colonoscope, a long guidewire was inserted fluoroscopically. The guidewire was passed to the distal end of the stricture and a 20-mm stone-extraction balloon introduced contrast to ensure luminal patency (Figs. 3 and 4). The pediatric colonoscope was then advanced through the mass to reach the normal jejunum. Normal saline was flushed through the stent catheter to lubricate the guidewire and reduce its movement with stent deployment.
Figure 2.
Endoscopic view of the mass-like lesion in the distal duodenum with no normal mucosa present.
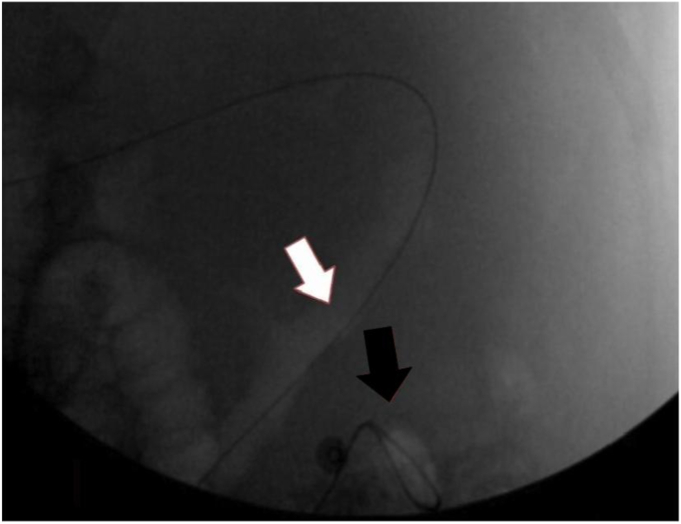
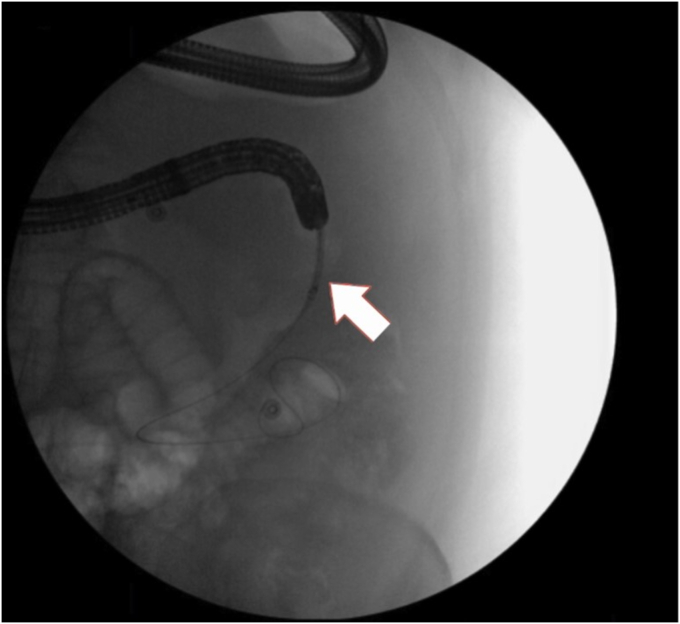
Figure 3.
Fluoroscopic image of the guidewire passing through the stricture. The white arrow indicates the beginning of the stricture. The black arrow shows the guidewire passing through the stricture.
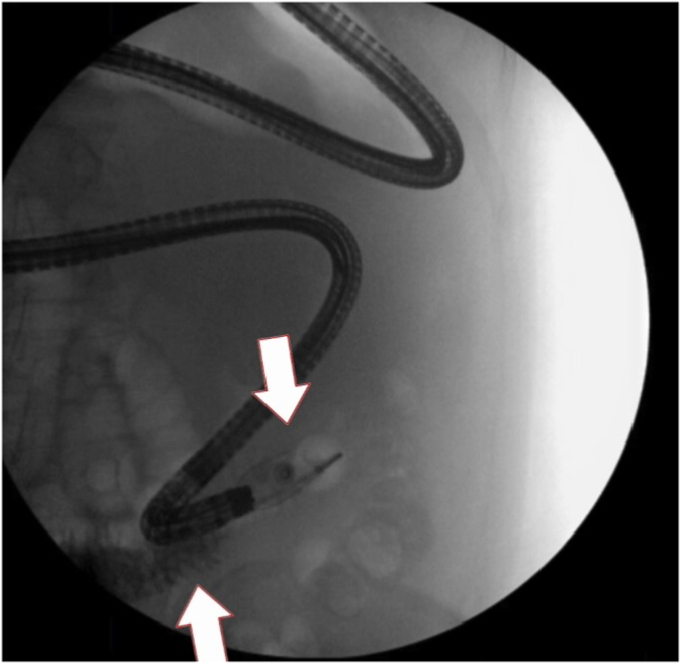
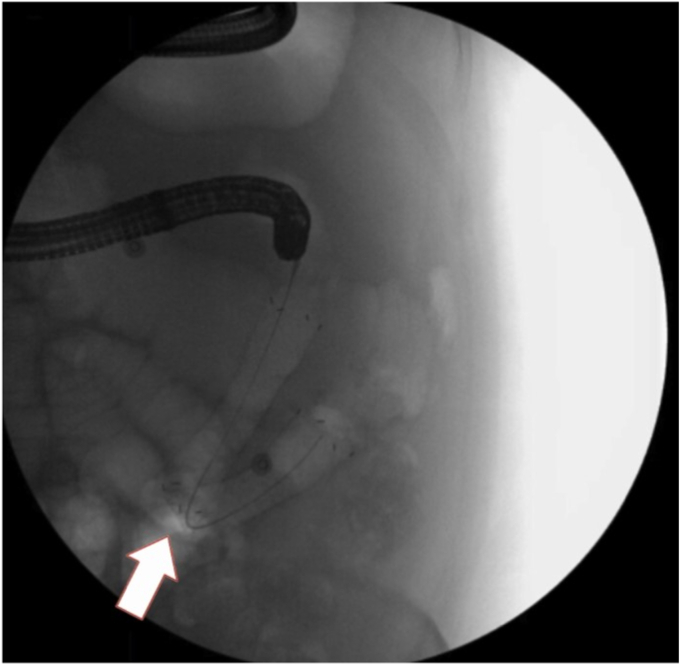
Figure 4.
Fluoroscopic image of contrast being delivered by a 20-mm stone-extraction balloon showing luminal patency. The top arrow indicates the tip of the balloon where contrast was introduced into the lumen. The bottom arrow indicates contrast past the area of stricture.
A fully covered 20- × 120-mm esophageal stent was advanced to the distal normal jejunum and was deployed under fluoroscopic guidance (Fig. 5). The stent maintained the U-shaped angle of the small bowel given its flexibility (Fig. 6). Since we were unable to bridge the whole stricture, a partially covered 18- × 97-mm esophageal stent was deployed into the proximal end of the previously placed stent to telescope it. This still did not reach the distal duodenum, so a fully covered 20- × 60-mm esophageal stent was placed, which bridged the whole stricture (Figure 7, Figure 8, Figure 9). A fully covered stent was used to prevent leaks given the malignant-appearing tissue.
Figure 5.
Fluoroscopic image of the first esophageal stent being advanced. The arrow points to the stent.
Figure 6.
Fluoroscopic image of the U-shaped bend in the first esophageal stent placement. The arrow indicates the bend in the stent.
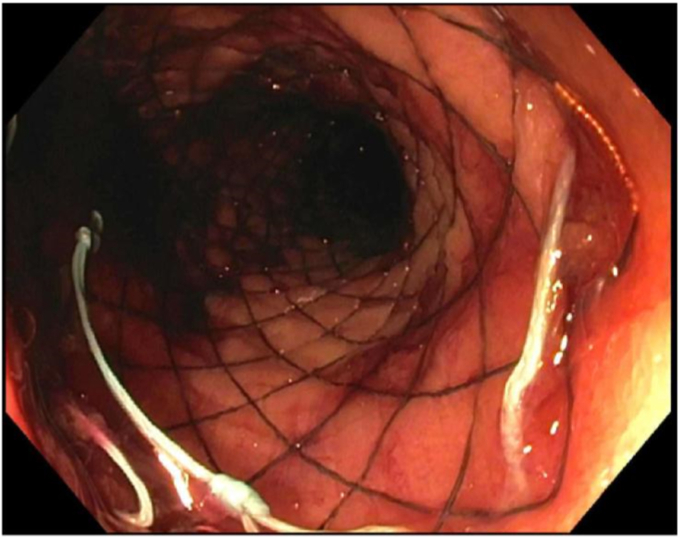
Figure 7.
Endoscopic view of the third esophageal stent after placement.
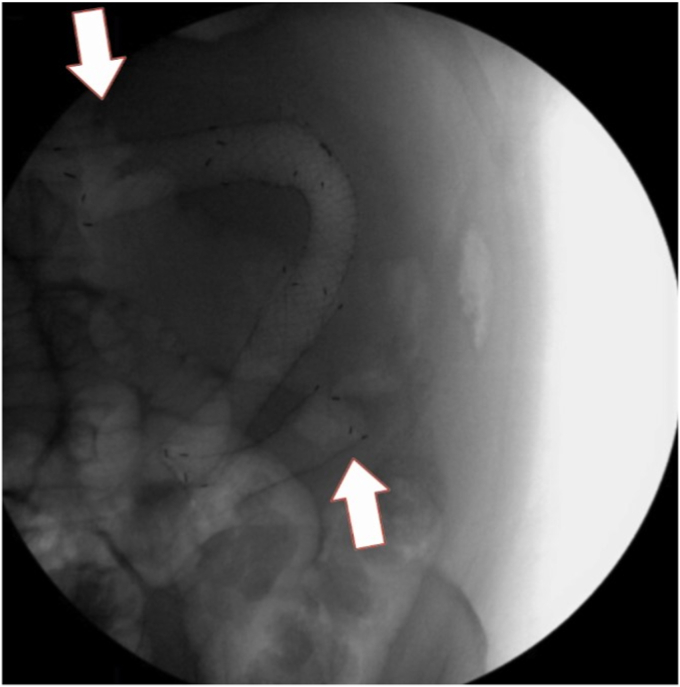
Figure 8.
Fluoroscopic images of all 3 esophageal stents bridging the entire stricture. The top arrow indicates the beginning of the first esophageal stent. The bottom arrow indicates the end of the third esophageal stent.
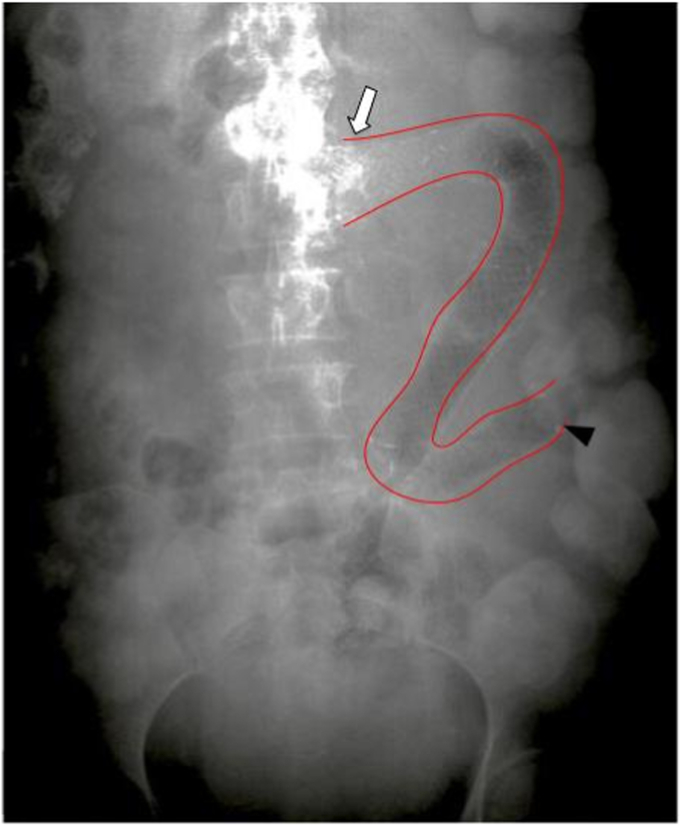
Figure 9.
Abdominal radiograph showing interval placement of stents from the distal duodenum to the proximal jejunum. The entirety of the stenting is outlined by red lines. The white arrow indicates the beginning of the stenting. The black arrowhead indicates the end of the stenting.
There were no immediate adverse events with the procedure. The patient continued to have abdominal discomfort, likely because of the stent expansion. A repeat CT scan showed luminal patency with contrast flowing through the stents (Video 1). The patient tolerated a liquid diet. Long-term follow-up was not possible because our patient died as a result of the extent of her malignancy.
Stent migration is always considered when placing fully covered metal stents. Uncovered stents can be used to prevent migration. However, given the lack of normal mucosa, it was believed that the use of uncovered stents would lead to bleeding and perforation. Furthermore, stent fixation was not used as there was aperistalsis throughout the mass, making stent migration less of a concern.
Distal small-bowel strictures can be difficult to manage. This case demonstrates the feasibility of using multiple covered esophageal stents to help relieve more distal GI obstructions. Covered esophageal stents are useful to keep the natural flow of food and help prevent surgical interventions.
Prior Presentation
The case described in this article was presented in poster form at the American College of Gastroenterology 2022 Annual Meeting in Charlotte, North Carolina, USA.
Disclosure
The authors did not disclose any financial relationships.
Supplementary data
Video describing the case, procedure, and outcomes.
References
- 1.Soetikno R.M., Carr-Locke D.L. Expandable metal stents for gastric-outlet, duodenal, and small-intestinal obstruction. Gastrointest Endosc Clinics North America. 1999;9:447–458. [PubMed] [Google Scholar]
- 2.Yates M.R., 3rd, Morgan D.E., Baron T.H. Palliation of malignant gastric and small intestinal strictures with self-expandable metal stents. Endoscopy. 1998;30:266–272. doi: 10.1055/s-2007-1001253. [DOI] [PubMed] [Google Scholar]
- 3.Rejchrt S., Kopacova M., Brozik J., et al. Biodegradable stents for the treatment of benign stenoses of the small and large intestines. Endoscopy. 2011;43:911–917. doi: 10.1055/s-0030-1256405. [DOI] [PubMed] [Google Scholar]
- 4.Sunada K., Yamamoto H., Kita H., et al. Clinical outcomes of enteroscopy using the double-balloon method for strictures of the small intestine. World J Gastroenterol. 2005;11:1087–1089. doi: 10.3748/wjg.v11.i7.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirai F., Beppu T., Sou S., et al. Endoscopic balloon dilatation using double-balloon endoscopy is a useful and safe treatment for small intestinal strictures in Crohn’s disease. Digestive Endosc. 2010;22:200–204. doi: 10.1111/j.1443-1661.2010.00984.x. [DOI] [PubMed] [Google Scholar]
- 6.Despott E.J., Gupta A., Burling D., et al. Effective dilation of small-bowel strictures by double-balloon enteroscopy in patients with symptomatic Crohn’s disease (with video) Gastrointestinal Endosc. 2009;70:1030–1036. doi: 10.1016/j.gie.2009.05.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video describing the case, procedure, and outcomes.
Video describing the case, procedure, and outcomes.