Abstract
Objectives. Despite the recent expansion of direct-to-patient telehealth abortion care in the United States, patient experiences with the service are not well understood.
Methods. We described care experiences of 1600 telehealth abortion patients in 2021 to 2022 and used logistic regression to explore differences by race or ethnicity and between synchronous (phone or video) and asynchronous (secure messaging) telehealth abortion care.
Results. Most patients trusted the provider (98%), felt telehealth was the right decision (96%), felt cared for (92%), and were very satisfied (89%). Patients most commonly cited privacy (76%), timeliness (74%), and staying at home (71%) as benefits. The most commonly reported drawback was initial uncertainty about whether the service was legitimate (38%). Asian patients were less likely to be very satisfied than White patients (79% vs 90%; P = .008). Acceptability was high for both synchronous and asynchronous care.
Conclusions. Telehealth abortion care is highly acceptable, and benefits include privacy and expediency.
Public Health Implications. Telehealth abortion can expand abortion access in an increasingly restricted landscape while maintaining patient-centered care. (Am J Public Health. 2024;114(2):241–250. https://doi.org/10.2105/AJPH.2023.307437)
In the wake of the June 2022 Dobbs v Jackson Supreme Court decision that allowed states to ban abortion, telehealth medication abortion has played a vital role in abortion provision and access in the United States. Telehealth can help mitigate surges in demand for abortion care in states where it remains legal. 1 , 2 For patients in states with abortion bans, telehealth services can also increase abortion access through methods like mail forwarding and mailing medications to a postal address or post office box in neighboring states over the border, minimizing the amount of travel required.
Medication abortion has emerged as the leading abortion method both within 3 and outside of 4 the health care system in the United States in recent years. Concurrently, there has been a rise in medication abortion provided via telehealth, facilitated by regulatory changes that allowed abortion medications to be mailed beginning in the COVID-19 pandemic. 5 Before the pandemic, telehealth abortion models were primarily “site-to-site,” requiring patients to travel to abortion clinics, where they received ultrasonography and other in-person tests and then remotely consulted with a clinician who was at another location. 6 , 7
Direct-to-patient telehealth abortion care first became widely available in the United States in 2020 and has been found to be safe and effective. 8 – 10 Since then, virtual clinics—online-only abortion providers—began providing this model of telehealth abortion care in states where it is legally permitted. 11 ‒ 13 Patients are screened for eligibility remotely by a clinician, receiving an ultrasound only if desired or medically indicated, and subsequently receive medications from a mail-order pharmacy. 14 In all medication abortion care models, patients typically take the medications, pass the pregnancy, and complete follow-up at home. 15 Patient‒provider communication is either entirely over secure text messaging (asynchronous care) or with a videoconference or phone call (synchronous care). 16
As of November 2023, telehealth for abortion was legally permitted in 24 states and Washington, DC (Figure A, available as a supplement to the online version of this article at https://ajph.org). 17 Between April 2022 and June 2023, the number of abortions provided by virtual clinics nearly doubled, accounting for almost 1 in 10 US abortions by June 2023. 2
Despite the critical role that telehealth plays in maintaining access to abortion across an increasingly restricted landscape, the acceptability of direct-to-patient telehealth for abortion in the United States is not well understood. Evidence from the TelAbortion study has demonstrated US patients’ positive experiences with synchronous telehealth abortion care within a clinical study. 9 , 18 – 20 No studies have examined differences in patient experiences between synchronous and asynchronous care. Telehealth medication abortion care models are less medicalized compared with in-clinic care, and differences in experiences by patient sociodemographic characteristics have not been documented. As ongoing legal cases threaten to curtail access to telehealth abortion, it is critical to understand how patients experience these models of care. Therefore, we aimed to explore the real-world acceptability of novel direct-to-patient abortion services provided by US virtual clinics and to examine differences in abortion care experiences between synchronous and asynchronous models and patient sociodemographic characteristics.
METHODS
We used data from the California Home Abortion by Telehealth (CHAT) Study, which evaluates the safety, effectiveness, and acceptability of telehealth abortion care provided by 3 United States‒based virtual clinics. The CHAT Study began in California and increased in scope as virtual clinics expanded to provide care in 20 states and Washington, DC. The study collected electronic clinical data from all abortions provided by the participating clinics for a defined period between April 2021 and January 2022. During clinic intake, patients consented to share anonymized data with our research team. Patients approved for care between June 2021 and January 2022 were also invited to participate in a series of 3 surveys: 1 at abortion intake, another in the week after intake, and a final survey 4 weeks after intake. The baseline survey assessed patient sociodemographic characteristics and initial reasons for choosing telehealth. The first follow-up survey assessed medication administration and additional medical care received. The final survey assessed additional medical care received and experiences with the telehealth model including open-ended and closed-ended questions. Surveys were administered until all 3 surveys were completed by approximately 400 participants from each clinic. Participants received $50 as remuneration after the completion of all 3 surveys.
One clinic used synchronous communication with a phone or video call to screen patients for eligibility. The other 2 screened patients through asynchronous communication, which involved an online consultation form and subsequent communication via secure written messages. One of the clinics that screened patients through asynchronous communication by default also offered the option to request a synchronous intake appointment. Abortion costs from the 3 virtual clinics ranged from $199 to $239. During the study period, virtual clinics did not accept health insurance; however, each clinic offered financial assistance for the cost of the abortion via abortion funds.
Measures
We used several indicators of patient acceptability as the main outcome measures (Table A, available as a supplement to the online version of this article at https://ajph.org). We examined participants’ reasons for choosing telehealth reported in the baseline survey; participants could select all reasons that applied. The remaining outcome measures were asked in the 4-week follow-up survey. We assessed overall satisfaction, with Likert scale response options categorized into “very satisfied” versus other responses. We assessed whether participants could trust the virtual clinic with their care, whether they felt cared for throughout the abortion process, and whether telehealth was the right decision for them using individual dichotomous items (“yes” vs “no” or “don’t know”). Open-ended questions modeled the closed-ended items, assessing reasons for choosing telehealth, benefits of telehealth abortion, why they did or did not feel cared for, and how they felt like they could or could not trust the virtual clinic.
The baseline survey asked participants to identify the benefits and drawbacks of the telehealth abortion model in 2 select-all-that-apply items, with the option to write in other responses. Other responses were coded into closed-ended responses, the most common of which are represented in the results.
Our primary key predictor was whether patient acceptability outcomes differed between those who received synchronous and asynchronous abortion care. Our secondary key predictor was the participant’s race or ethnicity. Covariates included categorized measures of participant age at abortion intake, pregnancy duration on the day of abortion intake, education level, and health insurance coverage. We included binary measures reflecting experiences of food insecurity in the past month, previous medication abortion, whether the participant was born outside of the United States, and whether their zip code corresponded to an urban, or a suburban or rural area.
Statistical Analysis
We reported sample characteristics using descriptive statistics and used the χ2 and Fisher exact test to examine differences between the groups that received synchronous and asynchronous care. We used multivariable logistic regression to examine associations between participant and abortion model characteristics, and each patient acceptability indicator. Patient age (< 25 years; 25–29 years; 30–34 years; ≥ 35 years), pregnancy duration (< 35 days; 35–49 days; ≥ 50 days), and race or ethnicity categories (White; Black; Hispanic or Latinx; Asian, Native Hawaiian, or Pacific Islander; American Indian or Alaska Native, Middle Eastern or North African, or multiracial) were collapsed in the regression analyses to facilitate model convergence. We used predictive margins to calculate adjusted rates of each patient acceptability indicator.
Open-Text Responses
To illustrate meaning and provide context for the quantitative results, we purposively selected from the open-ended survey responses. L. R. K. and U. D. U. identified candidate quotes that corresponded to each patient acceptability indicator, among which L. R. K. selected final quotes for inclusion.
RESULTS
Originally, 1632 participants enrolled in the longitudinal surveys (32% of invited patients). Among those, we excluded 32 participants who took neither mifepristone nor misoprostol, resulting in an initial sample of 1600 survey participants in 20 states and Washington, DC. Ultimately, 1312 (82%) completed the 4-week follow-up survey.
We described sample characteristics in Table 1. At abortion intake, mean participant age was 29 years and mean pregnancy duration was 40 days (< 7 weeks). Across the sample, 53% identified as White; 14% as multiple races or ethnicities; 13% as Hispanic or Latinx; 9% as Black; 6% as Asian, Native Hawaiian, or Pacific Islander; 1% as American Indian, Native American, or Alaska Native; and 1% as Middle Eastern or North African. Nearly half (42%) had completed college or more education, and 21% experienced running out of food in the past month. Most (89%) participants were born in the United States and resided in urban areas (91%). More than half (56%) resided in the US West, 20% in the Northeast, and smaller proportions in the Midwest (12%) and South (12%). One third (29%) had a previous medication abortion and 59% had private health insurance. One third (31%) had a video or phone call during abortion intake (synchronous care). At the clinic that provided asynchronous care but offered the option to request synchronous care, 1% received synchronous care.
TABLE 1—
Characteristics of the Sample: United States, 2021‒2022
| Characteristic | Overall (n = 1600), No. (%) | Synchronous (n = 503), No. (%) | Asynchronous (n = 1097), No. (%) | P |
| Patient age at abortion intake, y | .07 | |||
| 16–17 | 8 (< 1) | 0 (0) | 8 (1) | |
| 18–19 | 67 (4) | 14 (3) | 53 (5) | |
| 20–24 | 381 (24) | 111 (22) | 270 (25) | |
| 25–29 | 418 (26) | 138 (27) | 280 (26) | |
| 30–34 | 405 (25) | 140 (28) | 265 (24) | |
| ≥ 35 | 321 (20) | 100 (20) | 221 (20) | |
| Pregnancy duration at abortion intake, d | < .001 | |||
| < 35 | 448 (28) | 161 (32) | 287 (26) | |
| 35–49 | 885 (55) | 294 (58) | 591 (54) | |
| 50–62 | 229 (14) | 46 (9) | 183 (17) | |
| ≥ 63 | 38 (2) | 2 (< 1) | 36 (3) | |
| Race or ethnicity | < .001 | |||
| Non-Hispanic White | 841 (53) | 285 (57) | 556 (51) | |
| Non-Hispanic Black or African American | 148 (9) | 68 (14) | 80 (7) | |
| Hispanic or Latinx | 203 (13) | 46 (9) | 157 (14) | |
| American Indian, Alaska Native, Middle Eastern, North African, or multiracial | 237 (15) | 60 (12) | 177 (16) | |
| Asian, Native Hawaiian, or Pacific Islander | 105 (7) | 19 (4) | 86 (8) | |
| Unknown | 66 (4) | 25 (5) | 41 (4) | |
| Food did not last, last month | < .001 | |||
| No | 1207 (75) | 393 (78) | 814 (74) | |
| Yes | 340 (21) | 82 (16) | 258 (24) | |
| Unknown | 53 (3) | 28 (6) | 25 (2) | |
| Previous medication abortion | .61 | |||
| No | 1136 (71) | 349 (69) | 787 (72) | |
| Yes | 457 (29) | 152 (30) | 305 (28) | |
| Unknown | 7 (< 1) | 2 (< 1) | 5 (< 1) | |
| US region | < .001 | |||
| West | 896 (56) | 177 (35) | 719 (66) | |
| Northeast | 313 (20) | 99 (20) | 214 (20) | |
| South | 195 (12) | 181 (36) | 14 (1) | |
| Midwest | 196 (12) | 46 (9) | 150 (14) | |
| Highest level of education achieved | < .001 | |||
| High school or less | 274 (17) | 62 (12) | 212 (19) | |
| Some college or technical school | 659 (41) | 200 (40) | 459 (42) | |
| Completed 4-y degree or more | 667 (42) | 241 (48) | 426 (39) | |
| Health insurance coverage | .019 | |||
| Private insurance | 941 (59) | 315 (63) | 626 (57) | |
| No insurance | 317 (20) | 83 (17) | 234 (21) | |
| Medicaid | 293 (18) | 96 (19) | 197 (18) | |
| Unknown | 49 (3) | 9 (2) | 40 (4) | |
| Nativity | < .001 | |||
| Born in the United States | 1430 (89) | 435 (86) | 995 (91) | |
| Born outside the United States | 138 (9) | 44 (9) | 94 (9) | |
| Unknown | 32 (2) | 24 (5) | 8 (1) | |
| Residence | .59 | |||
| Suburban or rural | 146 (9) | 43 (9) | 103 (9) | |
| Urban | 1454 (91) | 460 (91) | 994 (91) | |
| Completion of 4-wk follow-up survey | < .001 | |||
| Did not complete survey | 288 (18) | 27 (5) | 261 (24) | |
| Completed survey | 1312 (82) | 476 (95) | 836 (76) |
Note. The sample size was 1600.
Motivations for and Benefits of Telehealth
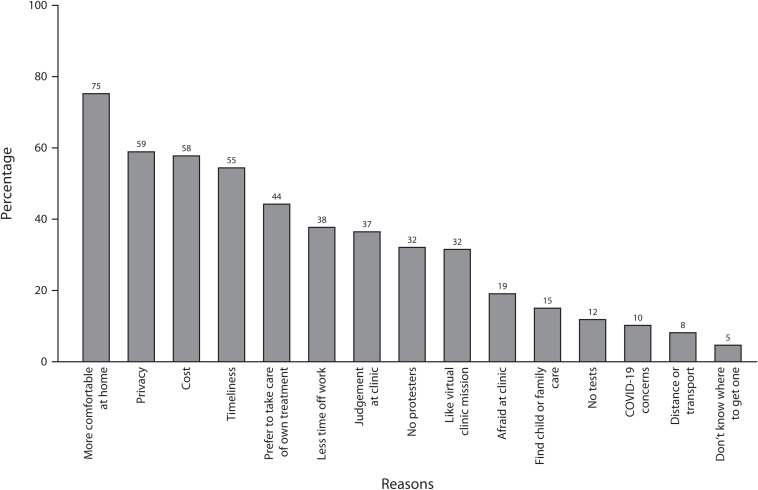
We examined participants’ reasons for choosing telehealth at baseline (Figure 1). The most common reasons for choosing telehealth were feeling more comfortable at home (75%) and privacy (59%). Participants explained the importance of these features in open-ended responses:
FIGURE 1—
Reasons for Choosing Telehealth: United States, 2021‒2022
Note. The sample size was 1600.
I felt more comfortable and less anxious about the whole process from being able to be home. I really appreciate having the opportunity to be in the comfort of my own home for the abortion and with my spouse for the entire duration and not in a cold room with strangers to have an uncomfortable procedure. –Age 26 years, Georgia, synchronous care
More than half (58%) identified lower costs relative to in-clinic care as a reason for using telehealth, a theme that participants expanded on in open-ended responses:
I couldn’t afford a surgical or medical abortion from the clinic. [Telehealth care] is half the price of abortions where I live. –Age 21 years, Oregon, synchronous care
More than half (55%) of respondents endorsed a desire to have the abortion as soon as possible, and many cited long waiting times at abortion clinics as a reason for choosing telehealth in open-ended fields:
The biggest thing was time. [Clinics were] booked out for weeks, and I didn’t want to wait weeks. –Age 32 years, Oregon, synchronous care
Meanwhile, 44% were motivated to use telehealth because it allowed them to take care of their own treatment. One participant explained,
I appreciate this experience of having the autonomy to be able to manage my own care with adequate support from a nurse practitioner. –Age 32 years, Illinois, asynchronous care
Similarly, another participant wrote,
I felt more safe or secure, more empowered doing it my own way. –Age 26 years, California, asynchronous care
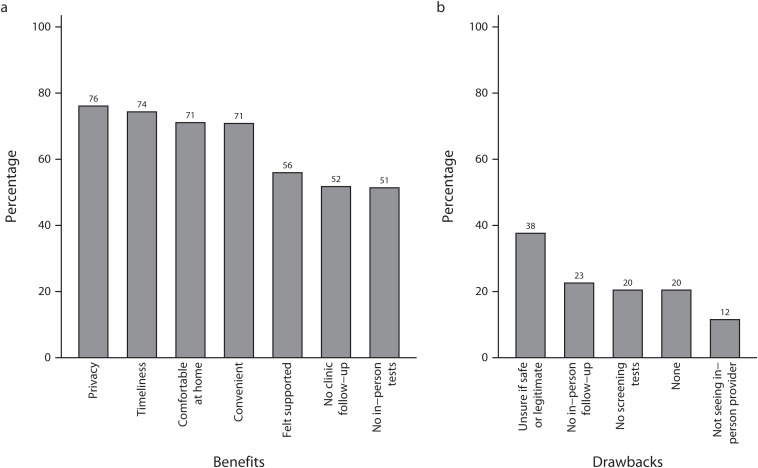
At the 4-week follow-up survey, the most common benefits of telehealth that participants cited were privacy (76%), expediency (74%), being more comfortable at home (71%), and convenience (71%; Figure 2). Overall, 56% of participants endorsed feeling supported as a benefit, and half cited not needing to go to the clinic for in-person screening tests (51%) or for follow-up (52%). One participant described their preference to have their abortion without ultrasound:
FIGURE 2—
Telehealth Abortion (a) Benefits and (b) Drawbacks: United States, 2021‒2022
Note. The sample size was 1312.
At a stressful time, I don’t want to be subjected to a vaginal ultrasound and blood work. If I know when I got pregnant, I don’t need an ultrasound. –Age 36 years, Illinois, asynchronous care
Drawbacks of Telehealth
When asked about the drawbacks of telehealth, the most common response was uncertainty about whether the service was safe or legitimate (38%). Some participants described deciding to place their trust in the virtual clinic as a leap of faith:
Not having any other option made me trust the service. There were times I doubted it could possibly be this easy or straightforward without there being some horrible catch. –Age 36 years, New Jersey, synchronous care
Overall, 20% reported no drawbacks. About one fifth cited not having screening (20%) and follow-up (23%) tests as drawbacks of their telehealth abortion experience. One participant stated,
I would have liked confirmation that it was complete via ultrasound. –Age 29 years, New York, asynchronous care
A smaller proportion (12%) listed not seeing a provider in person as a drawback of the telehealth model. In the open-ended responses, some participants also described being unable to reach the virtual clinic at times:
I took my pills on the weekend, so I had nobody to contact, which was unfortunate because I really wasn’t sure if the severity of what I was experiencing was normal. –Age 24 years, California, asynchronous care
Overall Rates of Acceptability Indicators
We next examined the adjusted proportion of participants who reported each of the 4 patient acceptability indicators of interest: trust, right decision, cared for, and satisfied (Table 2). Overall, 98% trusted the virtual clinic, 96% felt telehealth was the right decision, 92% felt cared for, and 90% of participants were very satisfied with the telehealth model of care. Full regression output is presented in Table B (available as a supplement to the online version of this article at https://ajph.org).
TABLE 2—
Associations Between Patient and Abortion Characteristic and Acceptability Indicators: United States, 2021‒2022
| Very Satisfied, PPR (95% CI) | Right Decision, PPR (95% CI) | Trust Provider, PPR (95% CI) | Cared for, PPR (95% CI) | |
| Overall | 89.7 (88.0, 91.4) | 95.6 (94.4, 96.7) | 98.0 (97.1, 98.8) | 91.9 (90.4, 93.4) |
| Model of care | ||||
| Synchronous (n = 476; Ref) | 90.4 (87.7, 93.2) | 97.1 (95.6, 98.6) | 97.3 (95.8, 98.8) | 88.5 (85.5, 91.4) |
| Asynchronous (n = 836) | 88.7 (86.5, 90.9) | 94.7 (93.1, 96.2) | 98.3 (97.5, 99.2) | 93.4 (91.7, 95.1)** |
| Race or ethnicity | ||||
| Non-Hispanic White (n = 689; Ref) | 89.5 (87.2, 91.8) | 95.4 (93.7, 97.0) | 97.9 (96.7, 99.1) | 92.7 (90.7, 94.6) |
| Non-Hispanic Black or African American (n = 121) | 91.4 (86.3, 96.5) | 95.1 (91.3, 99.0) | 97.9 (95.4, 100.0) | 88.6 (83.0, 94.3) |
| Hispanic or Latinx a (n = 166) | 90.7 (86.1, 95.2) | 97.3 (94.9, 99.7) | 98.8 (97.5, 100.0) | 95.1 (91.5, 98.7) |
| American Indian, Alaska Native, Middle Eastern, North African, or multiracial (n = 194) | 91.1 (87.2, 95.0) | 97.1 (94.8, 99.4) | 96.8 (94.3, 99.3) | 89.6 (85.4, 93.9) |
| Asian, Native Hawaiian, or Pacific Islander a (n = 87) | 78.5 (69.0, 87.9)** | 91.5 (85.4, 97.7) | 98.8 (97.5, 100.0) | 87.7 (79.9, 95.6) |
Note. CI = confidence interval; PPR = predicted prevalence rate. The sample size was n = 1312. Estimates are PPRs that draw from marginal estimates of multivariable logistic regression models. P values compare each category to the reference group in the multivariable logistic regression models. Multivariable models are adjusted for synchronous versus asynchronous care, patient age at abortion intake, pregnancy duration at abortion intake, food insecurity in the past month, race or ethnicity, previous medication abortion, education level, health insurance coverage, US nativity, and urban residence.
Variable for race or ethnicity combined Hispanic or Latinx with Asian, Native Hawaiian, or Pacific Islander for the “trust provider” model.
*P < .05; **P < .01; ***P < .001.
Differences in Patient Acceptability by Participant Characteristics
Finally, we assessed differences in adjusted prevalence rates of each patient acceptability indicator by participant characteristics (Table 2). Asian, Native Hawaiian, and Pacific Islander participants were less likely than White participants to be very satisfied (79% vs 90%; P = .008). Similar proportions of patients who received synchronous and asynchronous care were very satisfied, felt telehealth was the right decision, and felt cared for by the telehealth provider. However, participants who had asynchronous care were slightly more likely to feel cared for (93% vs 89%; P = .004).
In the open-ended responses, we found that some participants stated clear preferences for synchronous care, while others clearly preferred asynchronous care. One participant explained their preference for asynchronous care because it facilitated anonymity:
Everything was very professional and never pressed for any information. There was no pressure to do an appointment showing who I was. Privacy was well respected, and the ball was in my court to decide how much care I wish to receive (ex. seeing the doctor or nurse). –Age 29 years, California, asynchronous care
However, some participants who received asynchronous care described how asynchronous communication could feel impersonal. One participant wrote,
Since I talked to a nurse through chat, it didn’t feel personable, and I wasn’t sure if I was getting an automated message or if I was chatting with an actual person. –Age 27 years, California, asynchronous care
Another participant described how their synchronous care facilitated trust in the virtual clinic, despite initial reluctance about a video call:
It was the video call! It proved it was a real service and that it was their focus at [the virtual clinic]. As much as I didn’t want to do a video call, it helped solidify the legitimacy of the service. –Age 41 years, California, asynchronous care
One participant explained how being offered options for both synchronous and asynchronous services was important to their care:
I knew it was legitimate because they were considering all the right things: the 24/7 hotline, video calls if we want but also that they aren’t necessary. You can make it into the right abortion care for you. I personally didn’t make any calls or message much, but I trust the service because I know I can get whatever help I need. –Age 23 years, Washington, asynchronous care
Another participant stated,
They gave me a number to call if I needed, texted multiple times, and always said to text (which I love because I hate talking on the phone), or to call if I needed anything or had questions. –Age 43 years, California, asynchronous care
DISCUSSION
In this study, we found high acceptability of telehealth for abortion, whether it involved synchronous or asynchronous services. Nearly all participants were very satisfied with telehealth abortion. Telehealth abortion care is a new service and, thus, it was previously unknown whether this less medicalized model that eliminates in-person patient‒provider interaction would negatively impact patient acceptability. Of course, telehealth abortion care is not for everyone, including individuals who are seeking abortion care later in pregnancy, those who prefer procedural abortions, and those who prefer to have screening and follow-up tests as a part of their medication abortion care. Thus, while access to in-person abortion care remains critical, this study indicates that telehealth is an important addition to the abortion landscape and offers substantial benefits over in-person care for some patients.
The most common reason for choosing telehealth was that patients felt more comfortable at home. Most patients also reported choosing telehealth for greater privacy, lower cost, expediency, and more agency in managing their abortion care. Thus, telehealth abortion appears to help mitigate some barriers patients face in accessing care from an abortion clinic. Beyond its role in increasing access to abortion care and addressing the surges abortion facilities face as patients travel in wake of Dobbs, telehealth can promote patient-centered care for some people seeking an abortion. 18 , 21
We found few differences in acceptability between synchronous or asynchronous telehealth abortion care: patients were equally likely to be highly satisfied, trust the virtual clinic, and feel telehealth was the right decision. These findings suggest that both synchronous and asynchronous models are highly acceptable to patients. We found slightly higher rates of feeling cared for among participants who received asynchronous services. When patients from one clinic were offered asynchronous telehealth abortion services by default with an additional option for synchronous communication, almost no patients opted for synchronous care. While our results were largely similar for the 2 models, there may be different benefits and drawbacks of synchronous and asynchronous care with implications for providers and administrators. Services without real-time communication are presumed to feel less personable, but messaging can facilitate more frequent and responsive communication, which may contribute to patients feeling cared for. In addition, asynchronous models can require less time to provide, making them more cost-effective. 22 , 23 Our results demonstrate that asynchronous services can be provided while maintaining high levels of patient acceptability.
Nearly 40% of the sample was initially uncertain whether the virtual clinic services were safe or legitimate. At the time of the study, telehealth abortion services and virtual clinics were newly available within the formal US health care system. We expect that skepticism about legitimacy will decrease over time as public awareness about the safety and effectiveness of telehealth abortion increases. While these data draw from a time when interest in telehealth was very high because of the COVID-19 pandemic, use of telehealth abortion has continued to expand as barriers to access abortion care mount. 2
We found few differences in acceptability of telehealth abortion care by race or ethnicity in this sample, apart from finding lower rates of satisfaction among Asian versus White participants. Asian Americans are underrepresented among abortion patients, which could contribute to stigma and help to explain these findings. 24 Research has found lower levels of broader telehealth adoption among Asian individuals despite high levels of digital connectedness, which may be explained by discrimination in medical settings. 25
Limitations
This analysis has several limitations. First, all participants self-selected into telehealth care. Participants in our study were disproportionately older, White, and more financially secure than the national population of abortion patients, 24 although our sample may be more representative of the 24 states where telehealth abortion is legal. In addition, virtual clinic abortion services were available only in English and required a credit or debit card. These factors may limit the generalizability of our findings, leading us to find higher acceptability than we would have seen if patients had been more representative of the general abortion patient population. While our follow-up rate was high compared with other medication abortion studies, 18% of the sample was lost to follow-up, which may have introduced selection bias. This could have overestimated patient acceptability if those less satisfied dropped out of the study at higher rates or underestimated acceptability if participants for whom privacy was very important were more likely to be lost to follow-up. Finally, our study had limited variation in synchronous and asynchronous care among the 3 included clinics and an insufficient number of clusters to calculate clustered standard errors within each virtual clinic. Therefore, our study may have overestimated differences in acceptability of care if the observed differences between synchronous and asynchronous are truly attributable to differences in acceptability across the virtual clinics. However, each virtual clinic had multiple clinicians, bolstering the validity of the differences we detected.
Public Health Implications
In a post-Roe world, telehealth is taking on a greater role in the US abortion care landscape. Therefore, medication abortion, and telehealth medication abortion specifically, has become a focus of abortion restrictions. The high patient satisfaction with telehealth abortion found in this study combined with documentation of the safety and effectiveness of this service delivery modality 8 , 26 supports its continued availability.
Although this study found very high patient satisfaction with telehealth abortion, it is critical to understand abortion service delivery preferences and lower levels of acceptability among Asian patients. Our data suggest that telehealth is disproportionately accessible to patient populations who face fewer barriers to in-clinic abortion care. Policy and service changes that facilitate patients’ use of Medicaid and insurance to pay for the abortion, offer services in multiple languages, and increase minors’ access to care are critical to ensuring a range of accessible and acceptable telehealth abortion models. 21 Given increasing barriers to abortion across the United States, it is essential to further develop innovative models of care and ensure that all people who need abortion care will have access to a service delivery model that is right for them.
ACKNOWLEDGMENTS
This research was supported by the BaSe Family Fund, the Erik E. and Edith H. Bergstrom Foundation, the Lisa and Douglas Goldman Fund, the Isabel Allende Foundation, Jess Jacobs, the Kahle/Austin Foundation, and Preston-Werner Ventures. L. R. Koenig was funded in part by a training grant from the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award T32MD015070 and the National Institute of Child Health and Human Development under award F31HD111277 for the duration of the study. C. R. Lyles was supported by a University of California San Francisco‒Genentech Mid-Career Development Award.
The authors appreciate contributions to data collection and management and other input on the California Home Abortion by Telehealth Study from Linda Shin, Kelly Song, Andréa Becker, and Lisa Peters. We thank Cindy Adam, Mark Adam, Kate Baron, Stephanie Bussmann, Leah Coplon, Lauren Dubey, Lindsay DuBois, Kiki Freedman, Gaby Izarra, Jamie Phifer, and Aisha Wagner for supporting data acquisition.
Note. The funders had no role in the study design, data collection and analysis, writing of the report, or the decision to submit the article for publication.
CONFLICTS OF INTEREST
C. R. Lyles receives contract funding from AppliedVR, InquisitHealth, and Somnology and was a visiting researcher at Google in 2022‒2023.
HUMAN PARTICIPANT PROTECTION
The study was approved by the University of California, San Francisco’s institutional review board (20-32951).
See also Munson and Hall, p. 152.
REFERENCES
- 1. Aiken AR , Upadhyay UD. The future of medication abortion in a post-Roe world . BMJ. 2022. ; 337 : o1393 . 10.1136/bmj.o1393 [DOI] [PubMed] [Google Scholar]
- 2. #WeCount Report April 2022 to June 2023 Findings . Denver, CO: : Society of Family Planning; ; October, 2023. . 10.46621/218569qkgmbl [DOI] [Google Scholar]
- 3. Jones R , Nash E , Cross L , Philbin J , Kirstein M. Medication abortion now accounts for more than half of all US abortions. New York, NY: : Guttmacher Institute; ; 2022. . [Google Scholar]
- 4. Aiken ARA , Starling JE , van der Wal A , et al. Demand for self-managed medication abortion through an online telemedicine service in the United States . Am J Public Health. 2020. ; 110 ( 1 ): 90 – 97 . 10.2105/AJPH.2019.305369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cavazzoni P. Response letter from FDA CDER to American Association of Pro-Life Obstetricians and Gynecologists and American College of Pediatricians . December 17, 2021. . Available at: https://www.regulations.gov/document/FDA-2019-P-1534-0016 . Accessed February 10, 2023. [Google Scholar]
- 6. Grossman DA , Grindlay K , Buchacker T , Potter JE , Schmertmann CP. Changes in service delivery patterns after introduction of telemedicine provision of medical abortion in Iowa . Am J Public Health. 2013. ; 103 ( 1 ): 73 – 78 . 10.2105/AJPH.2012.301097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Seymour JW , Thompson TA , Milechin D , Wise LA , Rudolph AE. Potential impact of telemedicine for medication abortion policy and programming changes on abortion accessibility in the United States . Am J Public Health. 2022. ; 112 ( 8 ): 1202 – 1211 . 10.2105/AJPH.2022.306876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Upadhyay UD , Koenig LR , Meckstroth KR. Safety and efficacy of telehealth medication abortions in the US during the COVID-19 pandemic . JAMA Netw Open. 2021. ; 4 ( 8 ): e2122320 . 10.1001/jamanetworkopen.2021.22320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Anger HA , Raymond EG , Grant M , et al. Clinical and service delivery implications of omitting ultrasound before medication abortion provided via direct-to-patient telemedicine and mail in the US Contraception. 2021. ; 104 ( 6 ): 659 – 665 . 10.1016/j.contraception.2021.07.108 [DOI] [PubMed] [Google Scholar]
- 10. Upadhyay UD , Raymond EG , Koenig LR , et al. Outcomes and safety of history-based screening for medication abortion: a retrospective multicenter cohort study . JAMA Intern Med. 2022. ; 182 ( 5 ): 482 – 491 . 10.1001/jamainternmed.2022.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Allsworth JE. Telemedicine, medication abortion, and access after Roe v. Wade. Am J Public Health. 2022. ; 112 ( 8 ): 1086 – 1088 . 10.2105/AJPH.2022.306948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Baker CN. History and politics of medication abortion in the United States and the rise of telemedicine and self-managed abortion . J Health Polit Policy Law. 2023. ; 48 ( 4 ): 485 ‒ 510 . 10.1215/03616878-10449941 [DOI] [PubMed] [Google Scholar]
- 13. Koenig LR , Ko J , Upadhyay UD. Virtual clinic telehealth abortion services in the United States one year after Dobbs: a landscape review [preprint] . Published online July 13, 2023. . 10.2196/preprints.50749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Raymond EG , Grossman D , Mark A , et al. Commentary: no-test medication abortion: a sample protocol for increasing access during a pandemic and beyond . Contraception. 2020. ; 101 ( 6 ): 361 – 366 . 10.1016/j.contraception.2020.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology, Society of Family Planning . Medication abortion up to 70 days of gestation: ACOG Practice Bulletin, Number 225 . Obstet Gynecol. 2020. ; 136 ( 4 ): e31 – e47 . 10.1097/AOG.0000000000004082 [DOI] [PubMed] [Google Scholar]
- 16. Godfrey EM , Thayer EK , Fiastro AE , Aiken ARA , Gomperts R. Family medicine provision of online medication abortion in three US states during COVID-19 . Contraception. 2021. ; 104 ( 1 ): 54 – 60 . 10.1016/j.contraception.2021.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kaiser Family Foundation. The availability and use of medication abortion . September, 2023. . Available at: https://www.kff.org/womens-health-policy/fact-sheet/the-availability-and-use-of-medication-abortion . Accessed December 13, 2023.
- 18. Kerestes C , Delafield R , Elia J , Chong E , Kaneshiro B , Soon R. “It was close enough, but it wasn’t close enough”: a qualitative exploration of the impact of direct-to-patient telemedicine abortion on access to abortion care . Contraception. 2021. ; 104 ( 1 ): 67 – 72 . 10.1016/j.contraception.2021.04.028 [DOI] [PubMed] [Google Scholar]
- 19. Kerestes C , Delafield R , Elia J , Shochet T , Kaneshiro B , Soon R. Person‐centered, high‐quality care from a distance: a qualitative study of patient experiences of TelAbortion, a model for direct‐to‐patient medication abortion by mail in the United States . Perspect Sex Reprod Health. 2022. ; 54 ( 4 ): 177 ‒ 187 . 10.1363/psrh.12210 [DOI] [PubMed] [Google Scholar]
- 20. Chong E , Shochet T , Raymond E , et al. Expansion of a direct-to-patient telemedicine abortion service in the United States and experience during the COVID-19 pandemic . Contraception. 2021. ; 104 ( 1 ): 43 – 48 . 10.1016/j.contraception.2021.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Koenig LR , Becker A , Ko J , Upadhyay UD. The role of telehealth in promoting equitable abortion access in the United States: spatial analysis . JMIR Public Health and Surveillance . 2023. ; 9 : e45671 . 10.2196/45671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fiastro AE , Sanan S , Jacob-Files E , et al. Remote delivery in reproductive health care: operation of direct-to-patient telehealth medication abortion services in diverse settings . Ann Fam Med. 2022. ; 20 ( 4 ): 336 – 342 . 10.1370/afm.2821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stephens J , Greenberg GM. Asynchronous telehealth . Prim Care. 2022. ; 49 ( 4 ): 531 – 541 . 10.1016/j.pop.2022.05.004 [DOI] [PubMed] [Google Scholar]
- 24. Jones RK , Jerman J. Characteristics and circumstances of US women who obtain very early and second-trimester abortions . PLoS One. 2017. ; 12 ( 1 ): e0169969 . 10.1371/journal.pone.0169969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eberly LA , Kallan MJ , Julien HM , et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic . JAMA Netw Open. 2020. ; 3 ( 12 ): e2031640 . 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aiken A , Lohr PA , Lord J , Ghosh N , Starling J. Effectiveness, safety and acceptability of no-test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study . BJOG. 2021. ; 128 ( 9 ): 1464 – 1474 . 10.1111/1471-0528.16668 [DOI] [PMC free article] [PubMed] [Google Scholar]