Abstract
Internal migrants with chronic diseases (IMCDs) are a specific subgroup of the internal migrants, but few studies have focused on health service utilization among this group. Social integration is an essential element in the maintenance of health and well-being in migrants. However, the measurement of social integration remains inconsistent. This study aimed to measure social integration more comprehensively and evaluate the association between social integration and National Basic Public Health Services (NBPHS) utilization among IMCDs in China, thereby providing theoretical support for health promotion among IMCDs. The data of this study were obtained from the China Migrants Dynamic Survey (CMDS) in 2017. A total of 9272 internal migrants who self-reported hypertension and/or type 2 diabetes were included in the analysis. Four factors were extracted through exploratory factor analysis to measure the social integration of IMCDs: psychological identity, community involvement, social security, and sociocultural adaptation. The results show the IMCDs underutilized NBPHS, with 26.80 % stating that they have not used any of the services in the NBPHS. We confirmed the positive association between social integration and NBPHS use among IMCDs. The social integration of IMCDs in developed regions was relatively worse than in developing regions, further exacerbating the underutilization of NBPHS in developed regions. Therefore, targeted government measures and supportive policies are necessary, especially in developed regions, to encourage IMCDs to participate in social organizations and community activities and stimulate their active participation in the NBPHS.
Keywords: Social integration, Internal migrants with chronic diseases, National basic public health service, Structural equation modelling
1. Introduction
Internal migrants are the individuals who migrate between different regions of a country. Over the past few decades, as China's economic development and urbanization have accelerated, the number of internal migrants has exploded. According to Report on China's Migrant Population Development of 2017, an estimated 245 million internal migrants, originally from less developed regions in the central and western parts of the country, who have migrated to the developed coastal regions, such as Beijing, Shanghai, Jiangsu for better job opportunities and income [1]. Like international migrants, internal migrants experience similar acculturation since China has significant disparities in culture, economic, and social environment across regions [2]. The existing literature has often underscored the “healthy migrant” effect and the “salmon bias”, i.e., healthier individuals are more likely to migrate [[3], [4], [5]]. However, the number of elderly internal migrants has increased nearly 1.6 times from 5.03 million in 2000 to 13.04 million in 2015 [6]. More than 30 % of internal migrants suffer from chronic diseases such as hypertension and diabetes, and are often exposed to high health risks. In this study, we adopted the definition of internal migrants with chronic diseases (IMCDs) in the 2017 China Migrants Dynamic Survey (CMDS), in which IMCDs were the individuals who did not have “Hukou” (permanent registered resident card) and who had lived in their place of residence for more than one month and self-reported having hypertension and/or diabetes. Due to long-standing household registration (“Hukou”) policy, with its dual governance system between rural and urban areas, IMCDs face many obstacles in health services utilization in particular [1].
In 2009, the Chinese government implemented the National Basic Public Health Services (NBPHS), a free service provided by primary healthcare institutions to all urban and rural residents, including IMCDs [7]. Currently, NBPHS consist mostly of 14 service components, such as health record establishment, health education, chronic diseases management and immunization for children [8]. Chronic disease management is an important component of the NBPHS, providing long-term, ongoing health management services to patients with hypertension and type 2 diabetes, including the establishment of health records, follow-ups, health education, and regular medical checkups, which help achieve early detection of chronic diseases, improve patients' unhealthy lifestyles, and track the development of the patient's condition [8,9]. Numerous studies have indicated that community-based standardized chronic disease management can significantly improve the health status of patients with chronic diseases and reduce the chances of complications and premature death [9,10].
The government has successively introduced supportive measures to strengthen the equalization of NBPHS. Additionally, the Report of the 20th Communist Party of China National Congress made strong statements for expediting the equalization of NBPHS and implementing the Healthy China 2030 [11,12]. Promoting the utilization of NBPHS is the basis and prerequisite for achieving the equalization of NBPHS [13]. However, the problem of underutilization of NBPHS by the internal migrants, especially IMCDs, remains prominent [14]. One study noted that only 33.9 % of internal migrants had received chronic disease education [15]. Another study found that less than 50 % of elderly internal migrants have established health records in their inflow communities [16]. Unfortunately, evidence regarding using NBPHS among IMCDs is generally unavailable. Several factors are associated with the underutilization of NBPHS by internal migrants. Existing research indicates that internal migrants who are female, more educated, married, and have longer stays in the destination city are more likely to utilize public health services [17,18]. Additionally, previous studies explored regional disparity in the inadequate use of NBPHS by migrants [19,20]. However, few studies have examined in detail the influence of social integration on the utilization of public health services among IMCDs.
Social integration theory was initially proposed to explain and understand the behavior, adaptation, and cultural integration of international immigrants, although most applications were in Western society [21]. Social integration is an essential element in the maintenance of health and well-being in migrants [22,23]. Previous studies have found that active social integration protects against communicable and non-communicable diseases [24]. Specifically, a Greece study demonstrated that low social integration contributes to poor self-reported health among immigrants [25]. Another study showed that social integration is positively associated with physical and mental health among African-American women [26]. Currently, there is no unified definition of social integration, but there is no doubt that it is a multidimensional variable with various proxies across different disciplines. Consequently, measures of social integration are usually based on self-developed or cited maturation scales that summarize an individual's social role or social network score [27]. In this study, we used the social integration theoretical framework of the 2017 CMDS, which measured the social integration of IMCDs with 16 question.
Research gaps exist in the relationship between social integration and the inadequate use of NBPHS among IMCDs. One study explored how improving the social integration of elderly migrants might help enhance the equalization of NBPHS [16]. Another study showed that social integration was associated with a higher likelihood of utilizing health records and health education [28]. However, it is uncertain whether this association exists for the IMCDs group, a priority population that is more likely to be exposed to NBPHS. Additionally, some studies have pointed out that the utilization of NBPHS by internal migrants is related to the economic level of their destination city [19,20]. Contrary to previous perceptions, NBPHS utilization among internal migrants was lower in areas with good economic development. Whether there is a positive correlation between social integration and the utilization of NBPHS among IMCDs in different regions remains to be seen, which may indicate a research gap.
Structural equation modelling (SEM) is an appropriate statistical method for multidimensional variables and has been widely used in recent years. Specifically, SEM is a statistical method for analyzing the relationship between variables based on a covariance matrix that merges factor analysis and path analysis methods to simultaneously examine the interaction between multiple variables, including the direct and indirect effects between variables [29,30]. Moreover, SEM compensates for the fact that traditional statistical analysis methods cannot measure multivariate problems directly and accurately. Finally, both errors and individual differences can be considered in the SEM.
Therefore, considering that social integration is a multidimensional variable, exploratory factor analysis was employed to explore the various dimensions of social integration. We also sought to assess the association between social integration and the utilization of NBPHS among IMCDs in China across different regional development levels using SEM.
2. Materials and methods
2.1. Data source
The data for this study were obtained from the 2017 China migrants dynamic survey (CMDS), provided by the Migrant Population Service Center. The CMDS is an annual national sample survey of the internal migrants conducted by the National Health Commission (formerly the National Health and Family Planning Commission) from 2009, covering 31 provinces (autonomous regions and municipalities) and the Xinjiang Production and Construction Corps, with an annual sample size of approximately 200,000 households. The participants of the survey were internal migrants (aged 15 and over) who had migrated from their hometowns to other regions/cities/provinces for at least one month but did not have local household registration (“Hukou”).
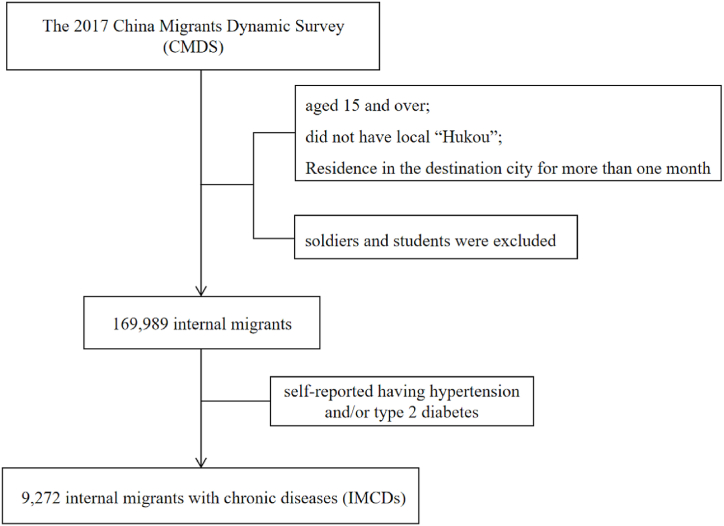
The stratified, multi-stage sampling was adopted based on Probability Proportionate to Size sampling method (PPS). The previous year's annual report data of the full internal migrants were used as the basic sampling frame, all provinces were taken as sub-population, capital cities and individual key cities were taken as mandatory layers, and randomly stratified extraction was carried out in the order of districts, counties, townships and followed by village or neighborhoods. Interviewers received standardized training by local health department staff, and quality control was implemented in data collection. The 2017 CMDS included standardized measurement of social integration and utilization of public health services among IMCDs. To analyze IMCDs' use of health services specifically, only self-reported hypertension and/or type 2 diabetes were retained for this study. Finally, 9272 participants were included in our study, and the flow chart was shown in Fig. 1. Relevant data and details are available at http://www.chinaldrk.org.cn/wjw/#/application/index.
Fig. 1.
Flow chart of participants included in the study.
2.2. Measures
2.2.1. NBPHS utilization
In this study, the IMCDs' utilization of NBPHS was the dependent variable, and we measured it from four aspects: establishment of health records, health education, regular follow-ups, and regular medical checkups. These four aspects are important elements of chronic disease management in the NBPHS. Specifically, IMCDs were asked whether local health records had been established. There are four options available: 1 indicates that it is established, 2 indicates that it is not established but has been heard of, 3 indicates that it is not established and that it has not been heard of, and 4 indicates that it is unclear. We unified recoded 2, 3, and 4 as 0, indicating that the IMCDs did not establish health records in the destination city. IMCDs were asked if they had received any health education about chronic disease control in the local area (1 = yes, 0 = no). The question “In the past year, have you received follow-up/medical checkups services for chronic diseases provided free of charge by your local community health service centre?” with “Yes” and “No” response options were used to measure the utilization of follow-ups and medical checkups (1 = yes, 0 = no).
2.2.2. Social integration
As a multidimensional variable, there is no uniform and accepted system of indicators for quantifying social integration. We used the social integration scale of the 2017 CMDS, which measured the social integration of IMCDs through 16 questions, covering various aspects of social security, cultural adaptation, and participation in community activities. The options for questions 1 to 8 were “completely disagree”, “disagree”, “basically agree”, and “completely agree”, which were assigned scores of 1, 2, 3, and 4, respectively, and questions 4 to 6 were assigned reverse scores; the answers to questions 9 to 13 were “never”, “occasionally”, “sometimes”, and “often”, which were assigned scores of 1, 2, 3, and 4, respectively, and the answers to questions 14 to 16 are “yes” and “no”, which are assigned scores of 1, 0 scores. The questionnaire had a score range of 15–55 points. The higher the total score, the higher the social integration of the respondents, and vice versa.
We performed an exploratory factor analysis (EFA) on the 16 questions in the social integration part to reduce dimensionality and summarize the main indicators of social integration. The Kaiser-Meyer-skin index (KMO), a measure of sampling adequacy, was 0.802, which was greater than 0.5, and the approximate χ2 in Bartlett's spherical test was 27878.513, with P < 0.001, indicating that the data were suitable for EFA. Principal component analysis (PCA) was used to extract shared factors, and based on eigenvalues >1, a scree plot and the interpretability of the derived factors were used to determine the final number of factors to be extracted in our EFA. The Kaiser standardized orthogonal rotation was also performed, which converged after five iterations, the rotated factor matrix was examined, and items with factor loadings level >0.4 were identified as contributing to a factor and retained. Finally, the extracted factors were named according to the items' content, and each factor’ weights were calculated based on the explanatory rate of variance after rotation of each factor.
2.2.3. Regional development disparity
The development level of the destination city is a widely discussed factor affecting the utilization of health services among internal migrants. Nevertheless, most existing studies have only used GDP. We adopted criteria for regional disparity classification different from those of previous studies. The human development index (HDI) was introduced to scientifically measure regional development differences, which is a composite index measured by calculating the normalized geometric mean of the indicator levels for three important dimensions: life expectancy at birth, years of education for adults aged 25 years and older, and GDP per capita [31]. We used data from the China HDI in the 2017 Human Development Report published by the United Nations Development Program. The data and details are available at https://hdr.undp.org/data-center. The HDI scores range from 0 to 1, with higher scores indicating higher levels of regional development. We defined the 10 provinces (Beijing, Shanghai, Tianjin, Liaoning, Guangdong, Jilin, Zhejiang, Jiangsu, Neimenggu, and Shandong) with the HDI ≥0.75 as developed regions, while the remaining 21 provinces were classified as developing regions (1 = “developed regions”, 0 = “developing regions”).
2.2.4. Control variables
Standardized questionnaires in the 2017 CMDS obtained information on sociodemographic and migration characteristics, including sex, age, education, Hukou, employment status, place of origin, chronic conditions, migrating reason, length of residence, and migration range. Among these variables, gender was categorized into male and female. Age was divided into five groups: 1) under 35, 2) 35 to 44, 3) 45 to 54, 4) 55 to 64, and 5) 65 and older. The Hukou had two alternatives: urban and rural. Educational status was classified into four levels: 1) elementary school and below, 2) middle school, 3) high school, and 4) university and above. Personal employment status was grouped as employed or unemployed. The migration range was divided into two groups: interprovincial and intraprovincial. Additionally, years of living locally were considered as a continuous variable to capture migration characteristics.
2.3. Data analysis
The mean ± standard deviation (mean ± SD) of continuous variables and frequencies of categorical variables were used to represent the distribution characteristics of variables related to individuals, migration, and the utilization of the NBPHS. Exploratory factor analysis (EFA) was performed to explore social integration factors and confirmatory factor analysis (CFA) allowed further determination of the suitability of EFA. IBM SPSS Statistics for Windows, version 20.0, was used for the descriptive statistical analysis and EFA. Structural equation modelling (SEM) was employed to test further the correlation and degree of correlation between social integration, regional development disparity, and the utilization of NBPHS items among IMCDs in China. SEM uses the bootstrap maximum likelihood estimation. The goodness-of-fit index (GFI), normal fit index (NFI), comparative fit index (CFI), incremental fit index (IFI) of 0.90 or above, parsimonious baseline fit index (PNFI) of 0.50 or above, and root mean square error of approximation (RMSEA) < 0.08 were used to assess the degree of model fit [32]. IBM SPSS AMOS 24.0 was used to establish the SEM. All statistical tests were two-sided, and a P value of less than 0.05 was considered statistically significant.
3. Results
3.1. The distribution characteristics of IMCDs
Table 1 shows the distribution of demographic and migration characteristics among the 9272 IMCDs. The average age of the respondents was 51.15 years (SD = 11.84), and more than half were male (59.12 %). The main education level was junior school or lower (76.62 %). Moreover, one-third of the respondents were unemployed, and 72.81 % were rural Hukou. Regarding the characteristics of migration, 47.69 % were interprovincial migrants, and 66.53 % of IMCDs were from rural area. Median of migrating time was 3.83 years, Interquartile range (IQR) was 1.24–6.75 years, and migrants with shorter than 3 years of residences accounted for more than half of the population. 37.04 % of the respondents lived in ten developed regions. The main reason of migration were working or engaging in trade and family reasons (76.56 %).
Table 1.
The distribution Characteristics of IMCDs (n = 9272).
| Variables | % or Mean (SD) | Variables | % or Mean (SD) |
|---|---|---|---|
| Gender | Place of origin | ||
| Male | 59.12 | Urban | 33.46 |
| Female | 40.88 | Rural | 66.54 |
| Age(years) | 51.15(11.84) | Migrating reason | |
| <35 | 7.48 | Working or engaging in trade | 41.62 |
| 35–44 | 20.66 | Family reasons | 34.94 |
| 45–54 | 37.68 | Marriage | 11.43 |
| 55–64 | 19.89 | Visit relatives | 8.52 |
| 65+ | 14.29 | Other reason | 3.49 |
| Education | Migrate range | ||
| Illiterate or primary school | 36.70 | Interprovincial | 47.69 |
| Junior school | 39.92 | Intraprovincial | 52.31 |
| High school | 16.16 | Development of destination city | |
| University and above | 7.22 | Developed regions | 37.04 |
| Hukou | Developing regions | 62.96 | |
| Urban | 27.19 | Chronic conditions | |
| Rural | 72.81 | Hypertension only | 77.46 |
| Employment Status | Type 2 diabetes only | 12.45 | |
| Employed | 64.10 | Both of the above | 10.09 |
| Unemployed | 35.90 | Years of residence | 4.76 (2.11) |
3.2. The utilization of NBPHS among IMCDs
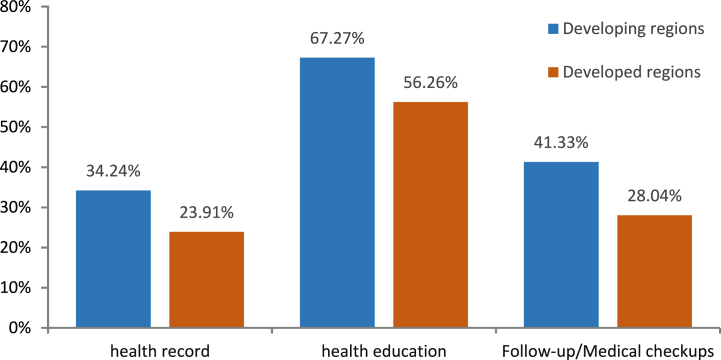
Of the 9272 IMCDs, 5859 (63.19 %) had received health education, only 30.41 % had established a local health record, and 36.41 % received follow-up/medical checkups services. A total of 26.80 % of participants reported that they had not received any of these health services. The average number of health services received by IMCDs was 1.57 (SD = 1.434). Fig. 2 depicts the utilization of NBPHS at the regional level of development. According to the chi-square test, the utilization rates of these services in developing regions were higher than those in developed regions (P < 0.001).
Fig. 2.
The utilization of NBPHS by regional level of development(%).
According to the effect of control variables on NBPHS use among IMCDs in Supplementary Table 1, IMCDs who were female, older, more educated, urban Hukou, migrate within the province, and migrate to developing regions were more likely to utilize health NBPHS, whether it is for health records, health education, or follow-ups/medical checkups. Further, IMCDs with established health records were more likely to use health education and follow-ups/medical checkups.
3.3. Social integration
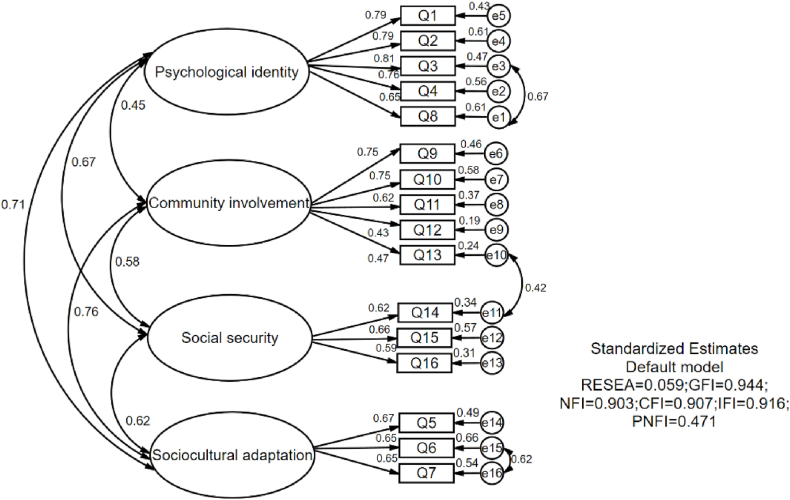
In the exploratory factor analysis, four factors with eigenvalues >1 and loading level >0.4 were extracted for the social integration of IMCDs. As illustrated in Table 2, Factor 1 included items 1, 2, 3, 4, and 8 due to the higher loadings on these items, and was named psychological identity based on the item content. Factor 2 consisted of five items, items 9, 10, 11, 12, and 13, named community involvement. Factor 3 and Factor 4 each included three items, with Factor 3 loading higher on items 14, 15, and 16, and Factor 4 loading higher on items 5, 6, and 7. Factor 3 and Factor 4 were named social security and sociocultural adaptation, respectively. The post-rotation variance contribution ratio for the four factors was 50.40 %. We constructed CFA measurement models for further validation. As shown in Fig. 3, the final models were calibrated to have acceptable goodness-of-fit indices (RMSEA = 0.059, GFI = 0.944, NFI = 0.903, CFI = 0.907, IFI = 0.917 and PNFI = 0.471).
Table 2.
Factor Loadings for four social integration factors derived from exploratory Factor Analysis.
| Items | Factor1 | Factor2 | Factor3 | Factor4 |
|---|---|---|---|---|
| Q1: Love the city/place where I live now | 0.797a | −0.005 | 0.029 | 0.047 |
| Q2: Follow the changes in the city/place where I live now | 0.793a | 0.027 | 0.063 | 0.010 |
| Q3: Love to integrate with the locals and be one of them | 0.835a | 0.013 | 0.040 | 0.076 |
| Q4: Think the locals are willing to accept me as one of them | 0.776a | 0.007 | 0.048 | 0.148 |
| Q5: Feel like I'm already a native | 0.208 | 0.000 | 0.011 | 0.700a |
| Q6: Feel the locals look down on internal migrants | −0.006 | 0.016 | 0.090 | 0.661a |
| Q7: It's more important to follow the customs of my hometown | 0.154 | 0.010 | 0.022 | 0.737a |
| Q8: Hygiene habits are quite different from local residents | 0.655a | 0.016 | 0.033 | 0.174 |
| Q9: Give advice to the unit/community/village | 0.032 | 0.741a | 0.108 | 0.018 |
| Q10: Policy recommendations to local government | 0.026 | 0.762a | −0.017 | −0.024 |
| Q11: Participate in discussions on social events online | −0.064 | 0.592a | −0.016 | −0.005 |
| Q12: Participate in donations, volunteer activities, etc. | 0.115 | 0.594a | 0.404 | 0.021 |
| Q13: Participate in party/group organization activities or meetings | 0.045 | 0.588a | 0.394 | 0.091 |
| Q14: Participate the activities organized by the trade union | 0.012 | 0.207 | 0.602a | −0.006 |
| Q15: Have the local social health insurance | 0.046 | −0.073 | 0.692a | 0.020 |
| Q16: A social security card locally | 0.031 | −0.056 | 0.635a | 0.075 |
The factor loadings of the constituent items of Factor1, Factor2, Factor3 and Factor4.
Fig. 3.
Measurement model for four factors of the social integration among IMCDs by CFA.
Table 3 presented the scores of social integration among IMCDs by regional level of development. The respondents' mean total score was 30.71 (SD = 4.11) out of 55, with a higher mean score in developing regions than in developed regions (35.89 vs. 26.78). In the aspect of psychological identity, IMCDs in developing regions scored higher than those in developed regions, indicating that IMCDs have a stronger sense of belonging in developing regions. IMCDs, whether in developed or developing regions, were hardly involved in any community organizations and activities (both averages are below 10 out of a possible 20 points). IMCDs in developing regions scored higher in the sociocultural adaptation dimension than those in developed regions, indicating that IMCDs in developing regions are more likely to adapt to local culture and customs. We found no statistical difference in the average score of social security between IMCDs in developed and developing regions.
Table 3.
The scores of social integration factors by regional level of development (mean ± SD).
| Factors | Developing regions | Developed regions | P value |
|---|---|---|---|
| Psychological identity | 18.11 ± 2.76 | 15.63 ± 3.04 | 0.014 |
| Community involvement | 8.05 ± 4.19 | 5.17 ± 2.83 | 0.001 |
| Social security | 1.58 ± 0.62 | 1.53 ± 0.97 | 0.155 |
| Sociocultural adaptation | 9.17 ± 2.29 | 5.49 ± 3.62 | 0.001 |
| Overall | 35.89 ± 5.73 | 26.78 ± 4.88 | 0.001 |
3.4. Relationship between social integration and NBPHS utilization
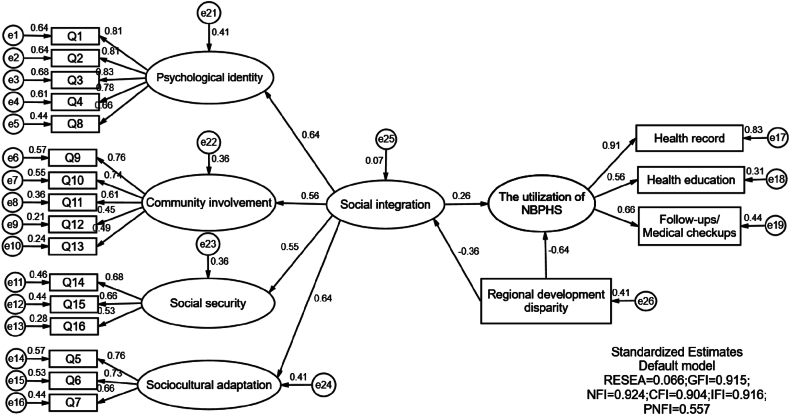
The SEM plot with standardized estimates indicated significant relationship between social integration and NBPHS utilization among IMCDs in China (Fig. 4). We corrected the initial model by increasing the residual correlations and modification indices, and the goodness-of-fit indices of the final model indicated an acceptable fit (RMSEA = 0.066, GFI = 0.915, NFI = 0.924, CFI = 0.904, IFI = 0.916, and PNFI = 0.557). As shown in Table 4, all paths are reported to be significant. The final model demonstrated that the utilization of NBPHS among IMCDs was directly associated with two variables: negative with regional development disparity (standardized regression coefficient = −0.643) and positive with social integration (standardized regression coefficient = 0.262). We also found that regional development disparity influenced the social integration of IMCDs (standardized regression coefficient = −0.364).
Fig. 4.
Final path diagram of the structural equation modelling; n = 9272. Ellipses represent unobserved latent constructs, rectangles represent observed variables, and single-headed arrows indicate the influence of one variable on another. Circles shown as e1-30 represent error terms. The number by the arrow represents the estimate of standardized regression coefficients.
Table 4.
Parameter Estimates from the SEM of social integration, regional development disparity, and the utilization of NBPHS among IMCDs.
| Components | Non-Standardized Coefficients |
Standardized Coefficients |
S.E.a | C.R.b | P value |
|---|---|---|---|---|---|
| Social integration→the utilization of NBPHS | 0.165 | 0.269 | 0.005 | 0.616 | 0.001 |
| Regional development disparity→the utilization of NBPHS | −0.533 | −0.678 | 0.024 | 0.877 | 0.001 |
| Regional development disparity→Social integration | −0.307 | −0.364 | 0.016 | 0.725 | 0.006 |
Standard error.
Composite reliability.
4. Discussion
Similar to international migrants, IMCDs experience a process of social integration due to the differences in cultural, economic and social environments across regions in China [2]. Numerous studies have focused on the general nature of health migrants and access to public health services in China. Less attention has been paid to the health service use among IMCDs who need long-term chronic disease management services [19,20]. This study provide the initial evidence to understand how the complicated migration and social integration process may be associated with NBPHS use among IMCDs.
This study advanced the measurement of social integration with more dimensions through EFA and CFA. In the psychological identity, IMCDs who like the destination city and are concerned about its development have a stronger psychological sense of belonging and are subjectively willing to integrate into the new environment, more active steps, therefore, can be taken to boost their self-identity as local residents. IMCDs were still socially isolated and rarely involved in any community organizations and activities, which could further hurt their physical or mental health [33]. Regarding social security, IMCDs with local health insurance are better informed about local health policies and health resources, increasing the likelihood of equal access to health services. Sociocultural adaptation is closely related to establishing local social networks by IMCDs [34]. Social networks are established based on people's needs for social relations and belonging, which are the most important embodiments of the social integration of IMCDs [35].
We found that IMCDs had lower utilization of NBPHS, aligning with previous findings for healthy immigrants. Specifically, less than 70 % of IMCDs received health education, which is lower than the health education coverage rate of more than 95 % proposed during the 13th Five-year Plan for managing health and family planning services for internal migrants [36]. The utilization of health records and follow-up/medical checkups among IMCDs was less than 40 %, whereas 80 % of residents had access to these services. Notably, health records play an important role in improving patient-physician communication and facilitating continuity of health management [37,38]. We found that IMCDs with established health records were more likely to undergo follow-ups and medical checkups. Therefore, it is necessary to conduct large-scale screenings for chronic diseases in the community and establish health records for IMCDs.
The final model demonstrated the positive association between social integration and NBPHS use among IMCDs. Considerable previous research has found that social integration can affect the behavior of internal migrants [24,25]. A previous study revealed that social integration helps internal migrants build social networks in the destination city and increases their access to informal sources of social support [25]. Those with higher social integration were more likely to use the NBPHS. From the perspective of health resource acquisition, social integration can help IMCDs access health policy and health resource information, thereby increasing their likelihood of utilizing the NBPHS. In the current study, we found that social integration directly and positively influenced the utilization of NBPHS. As an important national policy for preventing and controlling chronic diseases, the NBPHS, including health records and follow-ups, is generally associated with good health outcomes. This study found that IMCDs in developing regions have high levels of social integration. In contrast, IMCDs in developed areas face more obstacles in the process of social integration. This may be attributed to the fact that institutional exclusion in developed regions may weaken the identification and belonging of IMCDs to their destination, which may further reduce their enthusiasm for integration into society, resulting in an enhanced likelihood of the underutilization of NBPHS [39,40]. Accordingly, the government should develop targeted interventions to overcome the social integration barriers for IMCDs caused by the institutional causes, such as improving the social welfare of disadvantaged IMCDs and developing appropriate support policies to stimulate their participation in NBPHS.
This study focused on the social integration of IMCDs and contributes to the enhancement of research on different subgroups within the immigrant population. The measurement of social integration in this study were more comprehensive and specific than previous studies. Moreover, we confirmed the positive association between social integration and NBPHS use among IMCDs. The following limitation was acknowledged to avoid over-interpretation of our results. First, the chronic condition information of the IMCDs collected was self-reported, and recall bias may have induced under-reported information on health status and health utilization. Further detailed information will be obtained in future studies. Second, our study used a cross-sectional design, and the causal relationship between social integration and the utilization of NBPHS could not be determined. Therefore, we propose more research, such as a cohort study, to understand the causation and direction of social integration and NBPHS use, e.g. What are the long-term health effects of health service utilization on IMCDs.
5. Conclusions
In summary, this study provided a more in-depth examination of social integration and NBPHS use among IMCD in China. We measured social integration of IMCDs with four dimensions through EFA and CFA. Among all these social integration factors, community involvement was the weakest, both IMCDs in developed and developing regions. We confirmed the positive association between social integration and NBPHS use among IMCDs which contributed the existing literature in the field. The institutional causes, such as relatively high household registration threshold in developed regions, is a major barrier to promoting the social integration of IMCDs. Therefore, the government should develop targeted interventions to overcome the barriers to the social integration of IMCDs, especially in developed regions, and develop appropriate support policies to encourage the participation of IMCDs in social organizations and community activities to stimulate the participation in the NBPHS. Due to the significant number of IMCDs in China, all these interventions could significantly improve the well-being of this group.
Funding
This work was supported by the Key Projects of the National Social Science Foundation of China [grant number 22AZD082], and the Key Project of Philosophy and Social Science Research in Colleges and Universities in Jiangsu Province [grant number 2022SJZD141].
Data availability statement
The datasets employed in our study were provided by the Migrant Population Service Center, National Health Commission P.R. China and we have signed a legally binding agreement with the institution that we would not share any original data to any third parties. However, interested researchers can apply for access to the data at http://www.chinaldrk.org.cn/wjw/#/application/index and e-mail: ldrkzxsj@163.com.
CRediT authorship contribution statement
Leixia Wang: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Jianqian Chao: Writing – review & editing, Supervision, Project administration, Funding acquisition, Data curation, Conceptualization. Yanqian Wu: Software, Methodology, Investigation, Data curation. Na Zhang: Validation, Resources, Methodology, Data curation. Min Bao: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This analysis used data or information from the CMDS. The authors thank all the staff and participants of this study for their important contributions.Acknowledgments.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e25797.
Abbreviations
- NBPHS
National basic public health service
- IMCDs
Internal migrants with chronic diseases
- CMDS
China migrants dynamic survey
- HDI
Human development index
- SEM
Structural equation modelling
- EFA
Exploratory factor analysis
- CFA
Confirmatory factor analysis
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Migrant Population Service Center of the National Health Commission . 2017. Report on China's Migrant Population Development 2017; pp. 4–16. [Google Scholar]
- 2.Ma Z. Acculturation strategies, age at migration, and self-rated health: an empirical study on internal migrants in China. Soc. Sci. Res. 2021;93 doi: 10.1016/j.ssresearch.2020.102487. [DOI] [PubMed] [Google Scholar]
- 3.Westphal C. Healthy migrants? Health selection of internal migrants in Germany. Eur. J. Popul. 2016;32(5):703–730. doi: 10.1007/s10680-016-9397-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Newbold K.B. Self-rated health within the Canadian immigrant population: risk and the healthy immigrant effect. Soc. Sci. Med. 2005;60(6):1359–1370. doi: 10.1016/j.socscimed.2004.06.048. [DOI] [PubMed] [Google Scholar]
- 5.Elshahat S., Moffat T., Newbold K.B. Understanding the healthy immigrant effect in the context of mental health challenges: a systematic critical review. J. Immigr. Minority Health. 2022;24(6):1564–1579. doi: 10.1007/s10903-021-01313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeng W., Wang C., Chen H., Tong B., Li D., Zou Z., Liu P., Yao Y., Shang S. Health status and public health education for internal older migrants in China: evidence from a nationally representative survey. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.937361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L., Wang Z., Ma Q., Fang G., Yang J. The development and reform of public health in China from 1949 to 2019. Glob. Health. 2019;15(1):45. doi: 10.1186/s12992-019-0486-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qin J., Zhang Y., Fridman M., Sweeny K., Zhang L., Lin C., Mao L. The role of the Basic Public Health Service program in the control of hypertension in China: results from a cross-sectional health service interview survey. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0217185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yan L., Ji N., Xu J., Liu M., Guan L., Liu K., Jia A., Ding X., Liu D., Li M., Zhao Y., Mi S., Zhao W., Wang Z., Bai Y. Evaluating behavioral risk factor interventions for hypertensive and diabetic patient management in the national basic public health service programs from 2009. China CDC weekly. 2022;4(19):411–416. doi: 10.46234/ccdcw2022.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li X., Krumholz H.M., Yip W., Cheng K.K., De Maeseneer J., Meng Q., Mossialos E., Li C., Lu J., Su M., Zhang Q., Xu D.R., Li L., Normand S.T., Peto R., Li J., Wang Z., Yan H., Gao R., Chunharas S., Gao X., Guerra R., Ji H., Ke Y., Pan Z., Wu X., Xiao S., Xie X. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–1812. doi: 10.1016/S0140-6736(20)30122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Government of the People's Republic of China . 2022. The Report to the 20th National Congress of the Communist Party of China.http://english.www.gov.cn/news/topnews/20220/215/content_WS6357df20c6d0a757729e1bfc.html Retrieved January 10, 2023, from. [Google Scholar]
- 12.Tan X., Zhang Y., Shao H. Healthy China 2030, a breakthrough for improving health. Global health promotion. 2019;26(4):96–99. doi: 10.1177/1757975917743533. [DOI] [PubMed] [Google Scholar]
- 13.Yu C., Lou C., Cheng Y., Cui Y., Lian Q., Wang Z., Gao E., Wang L. Young internal migrants' major health issues and health-seeking barriers in Shanghai, China: a qualitative study. BMC Publ. Health. 2019;19(1):336. doi: 10.1186/s12889-019-6661-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ginsburg C., Bocquier P., Menashe-Oren A., Collinson M.A. Migrant health penalty: evidence of higher mortality risk among internal migrants in sub-Saharan Africa. Glob. Health Action. 2021;14(1) doi: 10.1080/16549716.2021.1930655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo M., Zhu Z., Dong T., Mi H., Wu B. Provincial and age disparity on chronic disease education among migrants in China: the migrants population dynamic monitoring survey. Inquiry: a journal of medical care organization, provision and financing. 2019;56 doi: 10.1177/0046958019895897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jing Z., Wang Y., Ding L., Tang X., Feng Y., Zhou C. Effect of social integration on the establishment of health records among elderly migrants in China: a nationwide cross-sectional study. BMJ Open. 2019;9(12) doi: 10.1136/bmjopen-2019-034255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin Y., Wang T., Zhu T. Do migration characteristics influence the utilization of basic public health services in internal elderly migrants in China? Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.514687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ginsburg C., Collinson M.A., Gómez-Olivé F.X., Gross M., Harawa S., Lurie M.N., Mukondwa K., Pheiffer C.F., Tollman S., Wang R., White M. J, Internal migration and health in South Africa: determinants of healthcare utilisation in a young adult cohort. BMC Publ. Health. 2021;21(1):554. doi: 10.1186/s12889-021-10590-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie Y., Guo Q. The health service use of aged rural-to-urban migrant workers in different types of cities in China. BMC Health Serv. Res. 2021;21(1):606. doi: 10.1186/s12913-021-06638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang Z., Jiang C.H., Hu J. Moderating effects of regional disparities on the relationship between individual determinants and public health service utilization among internal migrants: evidence from the China migrant dynamic survey in 2017. BMC Publ. Health. 2022;22(1):564. doi: 10.1186/s12889-022-12870-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Butler M., Warfa N., Khatib Y., Bhui K. Migration and common mental disorder: an improvement in mental health over time? Int. Rev. Psychiatr. 2015;27(1):51–63. doi: 10.3109/09540261.2014.996858. [DOI] [PubMed] [Google Scholar]
- 22.Berkman L.F., Glass T. From social integration to health: durkheim in the new millennium. Soc. Sci. Med. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 23.DiBello J., Murphy L., Palacios I. Social integration and community health participation of elderly men in peri-urban Ecuador. Annals of global health. 2020;86(1):138. doi: 10.5334/aogh.3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin Y., Zhang Q., Chen W., Ling L. The social income inequality, social integration and health status of internal migrants in China. Int. J. Equity Health. 2017;16(1):139. doi: 10.1186/s12939-017-0640-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rapp C., Huijts T., Eikemo T.A., Stathopoulou T. Social integration and self-reported health: differences between immigrants and natives in Greece. Eur. J. Publ. Health. 2018;28:48–53. doi: 10.1093/eurpub/cky206. (suppl_5) [DOI] [PubMed] [Google Scholar]
- 26.Fothergill K.E., Ensminger M.E., Robertson J., Green K.M., Thorpe R.J., Juon Effects of social integration on health: a prospective study of community engagement among African American women. Soc. Sci. Med. 2011;72(2):291–298. doi: 10.1016/j.socscimed.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams B.R., Wang M.Q., Holt C.L., Schulz E., Clark E.M. Social integration and health insurance statusamong African American men and women. J. Women Aging. 2015;27(3):195–215. doi: 10.1080/08952841.2014.933635. [DOI] [PubMed] [Google Scholar]
- 28.Liang J., Shi Y., Osman M., Shrestha B., Wang P. The association between social integration and utilization of essential public health services among internal migrants in China: a multilevel logistic analysis. Int. J. Environ. Res. Publ. Health. 2020;17(18):6524. doi: 10.3390/ijerph17186524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Syafiq Muhammad, Sirojuzilam Badaruddin, Purwoko Agus. Integrated structural equation modeling and causal steps in evaluating the role of the mediating variable. MethodsX. 2022;9 doi: 10.1016/j.mex.2022.101777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abe Y., Matsumoto T., Watanabe H., Gupta D.K., Baba K. Structural equation modelling for factors influencing patients' willingness to replace removable dentures. J. Oral Sci. 2021;63(3):231–235. doi: 10.2334/josnusd.20-0635. [DOI] [PubMed] [Google Scholar]
- 31.Cabasag C.J., Fagan P.J., Ferlay J., Vignat J., Laversanne M., Liu L., van der Aa M.A., Bray F., Soerjomataram I. Ovarian cancer today and tomorrow: a global assessment by world region and Human Development Index using GLOBOCAN 2020. Int. J. Cancer. 2022;151(9):1535–1541. doi: 10.1002/ijc.34002. [DOI] [PubMed] [Google Scholar]
- 32.Shi D., DiStefano C., Maydeu-Olivares A. Evaluating SEM model fit with small degrees of freedom. Multivariate Behav. Res. 2022;57(2–3):179–207. doi: 10.1080/00273171.2020.1868965. [DOI] [PubMed] [Google Scholar]
- 33.Raitakari S., Haahtela R., Juhila K. Tackling community integration in mental health home visit integration in Finland. Health Soc. Care Community. 2016;24(5):e53–e62. doi: 10.1111/hsc.12246. [DOI] [PubMed] [Google Scholar]
- 34.Lai H., Wang D., Ou X. Cross-cultural adaptation of Chinese students in the United States: acculturation strategies, sociocultural, psychological, and academic adaptation. Front. Psychol. 2023;13 doi: 10.3389/fpsyg.2022.924561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perry B.L., Roth A.R., Peng S., Risacher S.L., Saykin A.J., Apostolova L.G. Social networks and cognitive reserve: network structure moderates the association between amygdalar volume and cognitive outcomes, the journals of gerontology. Series B, Psychological sciences and social sciences. 2022;77(8):1490–1500. doi: 10.1093/geronb/gbab192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Health and Family Planning Commission . 2017. Circular of the on Issuing National Health Service Planning for Floating Population during the 13th Five-Year Plan.http://law.pharmnet.com.cn/laws/detail_3950.html Retrieved January 13, 2023, from. [Google Scholar]
- 37.Jetelina K.K., Woodson T.T., Gunn R., Muller B., Clark K.D., DeVoe J.E., Balasubramanian B.A., Cohen D.J. Evaluation of an electronic health record (EHR) tool for integrated behavioral health in primary care. Journal of the American Board of Family Medicine:JABFM. 2018;31(5):712–723. doi: 10.3122/jabfm.2018.05.180041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin S.C., Tunalilar O. Rapid adoption of electronic health record and health information exchange among assisted living communities, 2010-2018. J. Am. Med. Inf. Assoc.: JAMIA. 2022;29(5):953–957. doi: 10.1093/jamia/ocac021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qian Y., Ge D., Zhang L., Sun L., Li J., Zhou C. Does Hukou origin affect establishment of health records in migrant inflow communities? A nation-wide empirical study in China. BMC Health Serv. Res. 2018;18(1):704. doi: 10.1186/s12913-018-3519-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ashida T., Fujiwara T., Kondo K. Childhood socioeconomic status and social integration in later life: results of the Japan Gerontological Evaluation Study. SSM-population health. 2022;18 doi: 10.1016/j.ssmph.2022.101090. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets employed in our study were provided by the Migrant Population Service Center, National Health Commission P.R. China and we have signed a legally binding agreement with the institution that we would not share any original data to any third parties. However, interested researchers can apply for access to the data at http://www.chinaldrk.org.cn/wjw/#/application/index and e-mail: ldrkzxsj@163.com.