Abstract
Background
Life's Essential 8 (LE8) is a new metric to define cardiovascular health. We aimed to describe LE8 among Hispanics/Latinos and its association with incident hypertension.
Methods and Results
The HCHS/SOL (Hispanic Community Health Study/Study of Latinos) is a study of Hispanic/Latino adults aged 18 to 74 years from 4 US communities. At visit 1 (2008–2011), information on behavioral and clinical factors (diet, smoking status, physical activity, sleep duration, body mass index, blood pressure, cholesterol, fasting glucose, and medication use) were measured and used to estimate an LE8 score (range, 0–100) for 14 772 participants. Hypertension was defined as systolic blood pressure ≥130 mm Hg or diastolic blood pressure ≥80 mm Hg, or self‐reported use of antihypertensive medications. Among the 5667 participants free from hypertension at visit 1, we used Poisson regression models to determine the multivariable adjusted association between LE8 and incident hypertension in 2014 to 2017. All analyses accounted for the complex survey design of the study. Mean population age was 41 years, and 21.6% (SE, 0.7) had high cardiovascular health (LE8 ≥80). Mean LE8 score (68.2; SE, 0.3) varied by Hispanic/Latino background (P<0.05), ranging from 72.6 (SE, 0.3) among Mexican Americans to 62.2 (SE, 0.4) among Puerto Ricans. Each 10‐unit decrement in LE8 score was associated with a 22% increased risk of hypertension over ≈6 years (incident density ratio, 1.22 [95% CI, 1.16–1.29]).
Conclusions
Only 1 in 5 Hispanic/Latino adults had high cardiovascular health, and LE8 varied substantially across Hispanic/Latino background groups. Improvements in other components of cardiovascular health may result in a lower risk of developing hypertension.
Keywords: cardiovascular health, Hispanic/Latino health, hypertension, Life's Essential 8
Subject Categories: Hypertension, Race and Ethnicity, Risk Factors, Epidemiology, Cardiovascular Disease
Nonstandard Abbreviations and Acronyms
- HCHS/SOL
Hispanic Community Health Study/Study of Latinos
- LE8
Life's Essential 8
- LS7
Life's Simple 7
- NHANES
National Health and Nutrition Examination Survey
Clinical Perspective.
What Is New?
Defined using the updated American Heart Association's Life's Essential 8 metric, only 1 in 5 US Hispanic/Latino adults has high cardiovascular health, with differences across US Hispanic/Latino background groups.
Among US Hispanic/Latino adults, lower Life's Essential 8 score is associated with an increased risk of developing hypertension over 6 years.
What Are the Clinical Implications
Improvements in cardiovascular health among US Hispanic/Latino adults are warranted; differences in individual Life's Essential 8 health metrics by Hispanic/Latino origin should be considered in public health initiatives and clinical decision making.
Improvements in other components of cardiovascular health may result in lower risk of developing hypertension.
In 2022, the American Heart Association developed a framework called Life's Essential 8 (LE8) to describe cardiovascular health. 1 An update of Life's Simple 7 (LS7), 1 LE8 summarizes behavioral and clinical health factors, including diet, physical activity, nicotine exposure, body mass index (BMI), blood glucose, blood lipids, blood pressure, and, more recently, sleep health, which contribute to cardiovascular health. 1 Optimal levels of these 8 factors have an inverse and graded association with incident cardiovascular disease (CVD). 1 In fact, recent findings from the National Health and Nutrition Examination Survey (NHANES), 2 corroborated by a study in a Finnish sample of men, 3 showed that LE8 was strongly and inversely associated with an increased risk for all‐cause and CVD‐specific death.
Despite this strong association, ideal cardiovascular health is uncommon. Only 20% of the US population is considered to have high cardiovascular health, 1 and LE8 scores differ according to race and ethnicity. 4 For example, among Hispanic adults of Mexican American background sampled in NHANES, LE8 scores were lower (less favorable) compared with non‐Hispanic White adults. 4 LE8 has yet to be described among US Hispanic/Latino adults of diverse backgrounds. However, findings from the HCHS/SOL (Hispanic Community Health Study/Study of Latinos) showed that <1% of US Hispanic/Latino adults met ideal criteria for all LS7 metrics and that cardiovascular health profiles differed by Hispanic/Latino background group. 5 For example, the prevalence and incidence of hypertension differ substantially by Hispanic/Latino background group. 6 , 7
As the leading contributor to CVD, elevated blood pressure, or hypertension, is an important risk factor. 8 Though blood pressure is an LE8 metric, 1 other LE8 components are also considered risk factors for elevated blood pressure. 9 , 10 Among African American participants of the Jackson Heart Study, compared with meeting 1 or 0 LS7 metrics, meeting 6, 5, 4, 3, or 2 LS7 metrics was associated with a 90%, 74%, 70%, 43%, and 21% reduction, respectively, in incident hypertension over 8 years. 11 To date, the association between LE8 and incident hypertension has yet to be described, especially among diverse US Hispanic/Latino adults. Therefore, the objectives of this study were 2‐fold. Our first goal was to describe, for the first time, cardiovascular health defined by LE8, overall and according to Hispanic/Latino background group. Our second goal was to determine the association between LE8 with incident hypertension across 6 years, and whether this association differed by Hispanic/Latino background group. To do so, we leveraged longitudinal data from the HCHS/SOL study.
Methods
The data, analytic methods, and study materials can be been made available to other researchers who apply to the HCHS/SOL Publications Committee for purposes of reproducing the results or replicating the procedure.
Study Population
The HCHS/SOL is a population‐based study of diverse Hispanic/Latino adults aged 18 to 74 years from 4 US communities (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA). 12 , 13 A 2‐stage area probability sample of households was selected; stratification and oversampling at each stage were used to obtain a diverse sample representative of the 4 target communities. 13 Participants were initially examined at visit 1 in 2008 to 2011 and reexamined 6 years later at visit 2 in 2014 to 2017. At both visits, participants completed standardized medical examinations and questionnaires and underwent blood and laboratory measurements. Each local site's institutional review board approved the study protocol, and all participants provided informed consent.
Measurement of LE8 Cardiovascular Health Metrics
At visit 1, information on cardiovascular health metrics (diet, physical activity, nicotine exposure, sleep health, body mass index, blood lipids, blood glucose, and blood pressure) was collected and described as follows. Diet intake was assessed with two 24‐hour dietary recalls, and diet quality was measured through the Alternative Healthy Eating Index–2010. 14 Physical activity was assessed through the modified Global Physical Activity Questionnaire. 15 , 16 Participants self‐reported separately the number of days and minutes of moderate or higher‐intensity physical activity per week, and this information was used to calculate an average of moderate/vigorous minutes per week. Nicotine exposure was self‐reported and based on current smoking status (never, current, or former smoker), time since quitting among former smokers, and self‐report of sharing a household with a current smoker. Assessment of nicotine exposure was limited to cigarette smoking, as more detailed data on the use of other combustible tobacco products (eg, cigars or little cigarettes) were not available. Sleep health was calculated from self‐reported time going to bed and time waking up per weekend and weekday night. A weighted‐average sleep duration during an entire week was used to reflect both weekday and weekend sleep duration. BMI in kg/m2 was derived from measured weight and height wearing light clothing. 12 Blood lipids were obtained after a minimum 8‐hour fast and assessed through laboratory measurement of plasma total and high‐density lipoprotein cholesterol (in mg/dL). We scored blood lipids from non–high‐density lipoprotein cholesterol (in mg/dL), calculated as the difference between total and high‐density lipoprotein cholesterol. 17 Blood glucose was obtained after a minimum 8‐hour fast and assessed through laboratory measurement of fasting blood glucose (in mg/dL) or through glycosylated hemoglobin (%). 18 Following a 5‐minute rest period, blood pressure was measured on the right arm using a cuff that was sized to the upper right arm circumference. 19 Using an OMRON HEM‐907 XL (Omron Healthcare, Inc., Lake Forest, IL) 6 automated sphygmomanometer, a trained technician took 3 blood pressure measurements spaced 1 minute apart from seated participants. The average of the 3 measurements was used. At visit 1, use of hypoglycemic agents, lipid‐lowering medication, and antihypertensive medication was documented through scanned medications and used for the calculation of LE8.
Measurement of LE8 and Cardiovascular Health
Using methodology described in detail by Lloyd‐Jones et al, 1 we defined each cardiovascular health metric on a scale of 0 to 100. LE8 score was subsequently calculated as the average of all 8 scaled cardiovascular health metrics. Based on LE8 score, cardiovascular health was defined as low (LE8 score <50), moderate (LE8 score 50 to <80), or high (LE8 score ≥80). In a sensitivity analysis, we calculated LE8 as the average of all available cardiovascular health metrics among individuals with at least 6 available cardiovascular health metrics. Finally, given our interest in incident hypertension as an outcome, we created a secondary LE8 metric, which we refer to as LE7 going forward. LE7 was calculated as the mean of all LE8 cardiovascular health metrics except for blood pressure. Based on this LE7 score, we also calculated cardiovascular health categories using the thresholds defined above.
Hypertension
During both visits, participants were asked to self‐report all current medications, including medications for blood pressure, which were recorded by study staff. Hypertension was defined according to the American College of Cardiology/American Heart Association as systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥80 mm Hg, or self‐reported use of antihypertensive medication. 20
Other Variables
Participants self‐reported their age (in years), sex, education level (less than a high school education or at least a high school education), household income (<$30 000, at least $30 000, or not reported), health insurance status (yes or no), marital status (married/living with partner or single/separated/divorced/widowed), nativity/years in the 50 US states/District of Columbia (born in 50 US states/District of Columbia, born outside 50 US states/District of Columbia with ≥10 years or with <10 years residence), Hispanic/Latino background (Central American, Cuban, Dominican, Mexican, Puerto Rican, South American, more than one, or other), alcohol behavior (current use or former/never alcohol use), and depression symptoms (assessed through the Center for Epidemiologic Studies Depression Scale–10). 21 Participant field center and follow‐up time (years) between visit 1 and visit 2 were also recorded.
Analytic Sample
Of 16 415 HCHS/SOL participants, we restricted our main analytical sample to people with full information required for the calculation of LE8 at visit 1 (n=14 772) and, in a sensitivity analysis, participants with at least 6 of 8 LE8 cardiovascular health metrics (n=16 245). For our second aim, to assess the relationship between LE8 and incident hypertension, from 10 615 individuals with complete LE8 information who also participated in visit 2, we excluded 4856 people with hypertension at visit 1 and 92 people with missing data on hypertension, resulting in an analytic sample size of n=5667 for aim 2. Characteristics of participants with and without hypertension at visit 1, who participated in visit 2 are shown in Table S1.
Statistical Analysis
We described demographic and socioeconomic characteristics of the full sample and among participants without baseline hypertension. Next, we estimated mean LE8 score overall and according to Hispanic/Latino background by demographic characteristics (age, sex, education, income, and nativity/years in the US 50 states/District of Columbia). Then, we described the distribution of cardiovascular health overall and by Hispanic/Latino background. To compare our results to nationally reported estimates, 4 we age‐standardized LE8 scores to reflect the age distribution of the US population. 22 We also estimated the mean score for each LE8 cardiovascular health metric overall and by age, sex, Hispanic/Latino background, education, income, and nativity/years in the mainland United States. In a sensitivity analysis to assess any potential impact of missing data, we also estimated mean LE8 score overall and by Hispanic/Latino background group among individuals with at least 6 of 8 LE8 CV health metrics.
For our second aim, among participants without hypertension at visit 1, we estimated the cumulative incidence of hypertension according to categories of cardiovascular health. Next, we used multivariable adjusted Poisson regression models to determine (1) the association between 10‐unit decrements in LE8 score with incident hypertension and (2) the association between cardiovascular health with incident hypertension. We repeated this analysis using our LE7 variable (excluding blood pressure from the cardiovascular health calculation). We also used Poisson models to estimate the associations between 20‐unit decrements in each LE8 cardiovascular health metric with incident hypertension. All models were adjusted for age, sex, Hispanic/Latino background, income, education, nativity/years in the US 50 states/District of Columbia, health insurance, marital status, and study site. For all Poisson models, years of follow‐up between visits 1 and 2 was used as an offset. Finally, we tested whether Hispanic/Latino background modifies (1) the association of LE8 score with incident hypertension or (2) the association between each individual LE8 cardiovascular health metric with incident hypertension. Significance was determined using α=0.05 or 0.10 for interactions. Analyses were conducted in SUDAAN version 11.0.1 (Research Triangle Institute, Research Triangle Park, NC) to account for the complex survey design and the sampling weights.
Results
Mean age in the population was 41.2 (SE, 0.3) years, with 52.6% (SE, 0.6) women and was composed of Hispanic/Latino adults of 7.5% (SE, 0.6) Central American, 20.6% (SE, 1.7) Cuban, 9.5% (SE, 0.7) Dominican, 38.1% (SE, 1.7) Mexican, 15.2% (SE, 0.8) Puerto Rican, and 4.9% (SE, 0.3) South American background (Table 1). Overall, 32.2% (SE, 0.8) had less than a high school education, 61.1% (SE, 1.0) had an annual household income <$30 000, 22.3% (SE 0.8) were born in the US 50 states/District of Columbia, 50.3% (SE, 1.0) had health insurance, and 49.6% (SE, 0.8) were married or living with a partner. Those without baseline hypertension tended to be younger, were more likely to be women, were less likely to be of Cuban background and more likely to be of Mexican background, were more likely to live in San Diego, and had lived in the US 50 states/District of Columbia for a longer period of time (Table S1).
Table 1.
Characteristics of the Population With Complete Information on LE8, HCHS/SOL, 2008 to 2011
| All visit 1 participants unweighted (N=14 772) | Visit 1 participants without hypertension who participated in visit 2 unweighted (N=5667) | |
|---|---|---|
| Characteristic | % (95% CI) | % (95% CI) |
| Age group, y | ||
| 18–39 | 47.5 (45.9–49.2) | 63.5 (61.5–65.4) |
| 40–64 | 43.8 (42.5–45.2) | 34.2 (32.3–36.1) |
| 65–74 | 8.6 (7.9–9.4) | 2.3 (1.8–3.0) |
| Female | 52.6 (51.5–53.8) | 54.6 (52.6–56.6) |
| Hispanic/Latino background | ||
| Central American | 7.5 (6.5–8.7) | 7.7 (6.4–9.4) |
| Cuban | 20.6 (17.4–24.2) | 15.7 (13.0–18.8) |
| Dominican | 9.5 (8.2–10.9) | 8.6 (7.2–10.3) |
| Mexican | 38.1 (34.8–41.5) | 44.8 (41.3–48.5) |
| Puerto Rican | 15.2 (13.7–16.8) | 13.0 (11.3–14.8) |
| South American | 4.9 (4.3–5.5) | 5.3 (4.3–6.4) |
| Mixed/other | 4.3 (3.7–4.9) | 4.9 (4.0–6.0) |
| <High school education | 32.2 (30.7–33.7) | 29.0 (27.1–31.0) |
| Annual income <$30 000 | 61.1 (59.2–63.0) | 59.9 (57.7–62.2) |
| Nativity/years in the mainland United States | ||
| <10 y in US 50 states/District of Columbia | 28.2 (26.3–30.2) | 31.0 (28.5–33.5) |
| ≥10 y in US 50 states/District of Columbia | 49.5 (47.9–51.1) | 41.9 (39.9–44.0) |
| Born in US 50 states/District of Columbia | 22.3 (20.7–23.9) | 27.1 (25.1–29.3) |
| Study site | ||
| Bronx, New York | 27.3 (24.5–30.2) | 26.2 (23.2–29.5) |
| Chicago, Illinois | 16.2 (14.2–18.3) | 18.4 (16.0–21.0) |
| Miami, Florida | 30.1 (25.9–34.5) | 25.5 (21.6–29.7) |
| San Diego, California | 26.5 (23.2–30.2) | 30.0 (26.2–34.0) |
HCHS/SOL indicates Hispanic Community Health Study/Study of Latinos; and LE8, Life's Essential 8.
Overall, mean LE8 score was 68.2 (95% CI, 67.6–68.7), with differences according to Hispanic/Latino background (Figure 1). Compared with Mexican background (mean, 72.6 [95% CI, 72.1–73.2]), LE8 score was significantly lower (less favorable) in all other Hispanic/Latino background groups: mean score of 62.2 (95% CI, 61.4–63.0) among Puerto Ricans; 62.3 (95% CI, 61.3–63.2) among Cubans; 69.3 (95% CI, 68.5–70.1) among Central Americans, 70.2 (95% CI, 69.2–71.2) among Dominicans; and 70.2 (95% CI, 68.9–71.5) among South Americans. LE8 score also differed by important demographic, socioeconomic, and geographic characteristics. For example, LE8 score was higher (more favorable) among Hispanics/Latinos who were younger, with higher educational attainment, and who were foreign‐born with fewer years in the US 50 states/District of Columbia. LE8 score was higher in San Diego (72.2 [95% CI, 71.5–72.9]) and Chicago (71.5 [95% CI, 70.7–72.2]) compared with the Bronx (67.0 [95% CI, 66.3–67.6]) or Miami (63.9 [95% CI, [63.2–64.7]). These trends were largely consistent across Hispanic/Latino background groups. The proportion of US Hispanic/Latino adults with high cardiovascular health was 21.6% (95% CI, 20.3%–22.9%) and also differed by Hispanic/Latino background with the highest prevalence among Mexican (30.8% [95% CI, 28.8%–32.9%]) compared with all other Hispanic/Latino backgrounds (P<0.05; Figure 2). LE8 scores and trends across Hispanic/Latino background were similar when age standardized to the US age distribution (Table S2) or when including participants with an average of ≥6 LE8 cardiovascular components (Table S3).
Figure 1. Mean Life's Essential 8 score across US Hispanic/Latino Backgrounds, HCHS/SOL, 2008 to 2011.
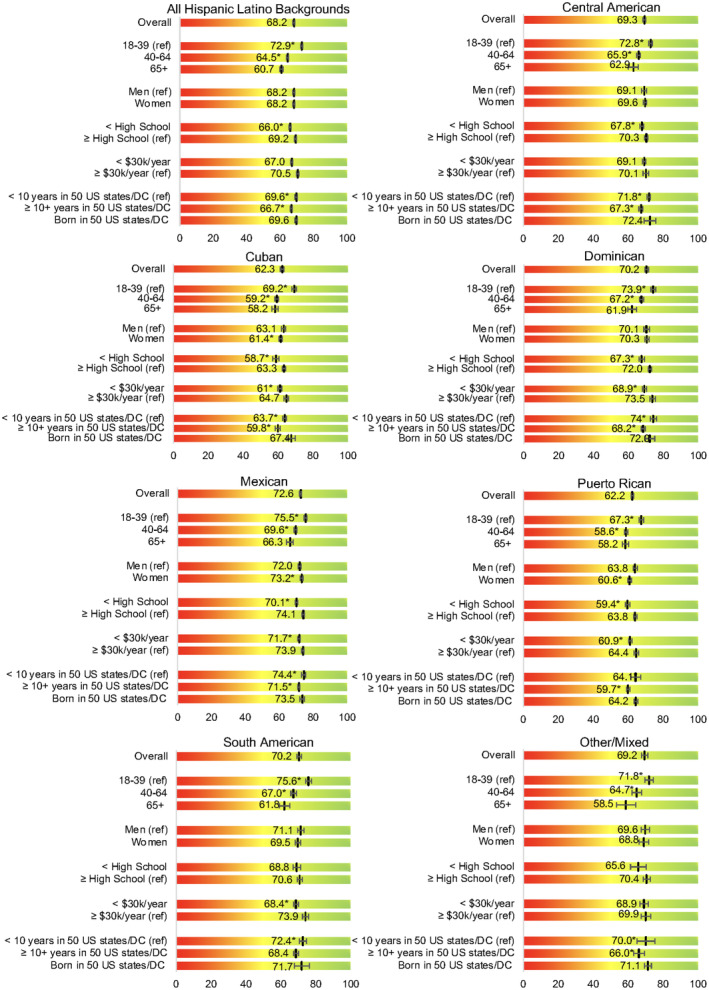
DC indicates District of Columbia; and HCHS/SOL, Hispanic Community Health Study/Study of Latinos. * indicates estimate differs from the given reference category (P<0.05).
Figure 2. Distribution of cardiovascular health measured by Life's Essential 8 among US Hispanics/Latinos, HCHS/SOL, 2008 to 2011.
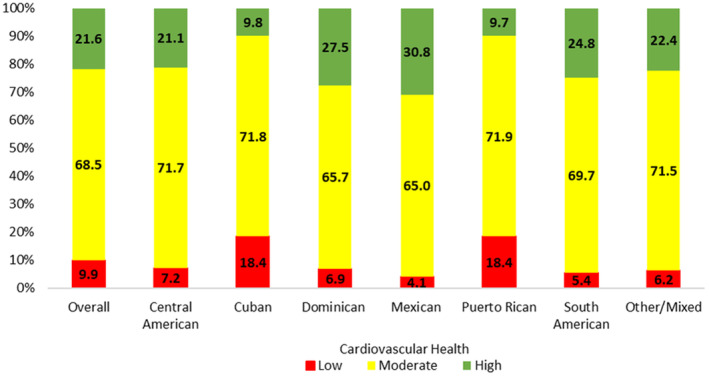
HCHS/SOL indicates Hispanic Community Health Study/Study of Latinos
Mean score for each LE8 cardiovascular health metric overall and by demographic characteristics is shown in Figure 3. Overall, mean scores were lowest for diet (40.4 [95% CI, 39.0–41.8]) and highest for sleep health (84.6 [95% CI, 84.0–85.3]). Younger Hispanics/Latino adults had significantly higher scores for physical activity, BMI, blood glucose, blood lipids, and blood pressure but lower scores for diet and nicotine exposure. Compared with men, women had less favorable scores for diet, physical activity, and BMI and more favorable scores for nicotine exposure, blood lipids, and blood pressure. There were also significant differences in LE8 cardiovascular health metrics by Hispanic/Latino background group, with most favorable scores among Mexican background for diet (59.1 [95% CI, 57.6–60.6]), sleep health (mean, 86.7 [95% CI, 85.7–87.7]), and blood pressure (80.0 [95% CI, 78.8–81.1]); among Dominicans for nicotine exposure (mean, 83.3 [95% CI, 80.7–85.8]) and blood lipids (mean, 67.6 [95% CI, 65.2–70.1]), among Central Americans for physical activity (mean, 78.9 [95% CI, 76.7–81.1]); and among South Americans for BMI (mean, 64.2 [95% CI, 61.5–67.0) and blood glucose (mean, 84.4 [95% CI, 82.2–86.5]). Individual LE8 cardiovascular health metrics also differed by socioeconomic and geographic characteristics (Table S4), with more favorable scores associated with greater educational attainment, higher income, and shorter duration of US residence among immigrants and among participants recruited in San Diego. When standardized by study site (Table S5), Mexican American participants had significantly higher LE8 scores compared with participants of Cuban or Puerto Rican background. Study‐site standardized LE8 component scores were most favorable among participants of Mexican background for physical activity, sleep health, and blood pressure; among Dominicans for diet and nicotine exposure; among South Americans for BMI and blood glucose; and among other/mixed for blood lipids.
Figure 3. Life's Essential 8 cardiovascular health metrics among US Hispanics/Latinos, HCHS/SOL, 2008 to 2011.
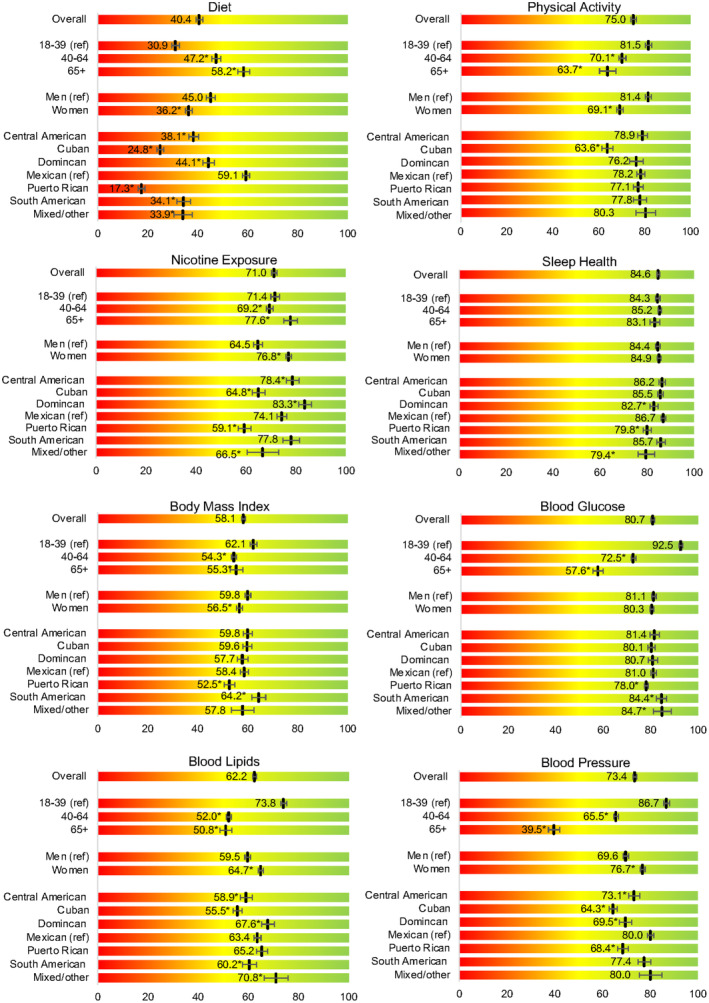
HCHS/SOL indicates Hispanic Community Health Study/Study of Latinos. * indicates estimate differs from the given reference category (P<0.05).
Among individuals without hypertension at visit 1, the age‐standardized cumulative incidence of hypertension was significantly greater among Hispanic/Latino adults with low cardiovascular health (34.0% [95% CI, 25.8%–43.4%]) and moderate cardiovascular health (22.7% [95% CI, 20.9%–24.6%) compared with those with high cardiovascular health (14.2% [95% CI, 12.1%–16.6%]; not shown). In multivariable adjusted models, each 10‐unit decrement in LE8 score was associated with a 22% increased risk of hypertension (incidence density ratio, 1.22 [95% CI, 1.16–1.29]; Table 2). Results were attenuated but still significant in our sensitivity analysis assessing the association between LE7 score with incident hypertension (Table S6). Overall, each 20‐unit decrement (worse) in individual LE8 cardiovascular health metrics was associated with greater risk of hypertension by 4% for nicotine exposure (incidence density ratio, 1.04 [95% CI, 1.00–1.08]), 17% for BMI (incidence density ratio, 1.18 [95% CI, 1.13–1.23]), and 13% for blood glucose (incidence density ratio, 1.13 [95% CI, 1.08–1.18]). The interaction term between Hispanic/Latino background and LE8 score was not significant but was significant for the LE8 BMI metric.
Table 2.
Associations Between LE8 Score and LE8 Cardiovascular Health Metrics With Incident Hypertension Overall and by Hispanic/Latino Background, HCHS/SOL 2008 to 2017
| Overall | Central American (n=1585) | Cuban (n=2168) | Dominican (n=1280) | Mexican (n=5958) | Puerto Rican (n=2346) | South American (n=966) | Mixed/other (N=469) | Interaction term P value | |
|---|---|---|---|---|---|---|---|---|---|
| Exposure | IDR (95% CI) | IDR (95% CI) | IDR (95% CI) | IDR (95% CI) | IDR (95% CI) | IDR (95% CI) | IDR (95% CI) | IDR (95% CI) | |
| LE8 (decrement of 10) | 1.22* (1.16–1.29) | 1.50* (1.32–1.71) | 1.15* (1.04–1.27) | 1.23 (0.96–1.56) | 1.21* (1.11–1.32) | 1.27* (1.10–1.45) | 1.11 (0.91–1.34) | 1.19 (0.83–1.69) | 0.20 |
| Cardiovascular health | |||||||||
| Low vs high | 2.13* (1.61–2.81) | 2.82* (1.25–6.35) | 1.95* (1.03–3.69) | 0.67 (0.12–3.62) | 1.97* (1.15–3.37) | 2.32* (1.22–4.38) | 3.07* (1.23–7.62) | 0.74 (0.06–9.64) | 0.20 |
| Moderate vs high | 1.50* (1.23–1.81) | 1.51 (0.76–2.98) | 1.61 (0.93–2.80) | 1.29 (0.72–2.31) | 1.45* (1.13–1.84) | 1.17 (0.61–2.24) | 1.30 (0.76–2.21) | 4.71* (1.42–15.55) | |
| LE8 cardiovascular health metric (decrement of 20) | |||||||||
| Diet | 1.02 (0.96–1.08) | 0.93 (0.79–1.10) | 1.01 (0.89–1.15) | 1.00 (0.78–1.30) | 1.03 (0.95–1.13) | 1.03 (0.87–1.21) | 1.00 (0.85–1.16) | 1.37* (1.01–1.87) | 0.23 |
| Physical activity | 0.98 (0.95–1.01) | 1.04 (0.96–1.13) | 0.96 (0.90–1.02) | 0.99 (0.89–1.11) | 0.99 (0.94–1.04) | 1.00 (0.93–1.07) | 0.93 (0.82–1.07) | 0.91 (0.69–1.21) | 0.72 |
| Nicotine | 1.04* (1.00–1.08) | 1.13* (1.02–1.26) | 1.04 (0.98–1.10) | 0.88 (0.74–1.05) | 1.02 (0.96–1.09) | 1.06 (0.98–1.15) | 1.02 (0.88–1.18) | 1.01 (0.86–1.18) | 0.37 |
| Sleep health | 1.04 (0.98–1.09) | 0.98 (0.79–1.22) | 1.08 (0.97–120) | 0.86 (0.69–1.07) | 1.03 (0.93–1.14) | 1.10* (1.01–1.21) | 0.95 (0.82–1.11) | 0.96 (0.69–1.34) | 0.60 |
| Body mass index | 1.17* (1.13–1.23) | 1.35* (1.20–1.51) | 1.11* (1.01–1.22) | 1.36* (1.19–1.55) | 1.16* (1.08–1.24) | 1.12* (1.02–1.23) | 1.18 (0.99–1.41) | 1.05 (0.89–1.25) | 0.08 |
| Blood lipids | 1.06* (1.02–1.11) | 1.08 (0.93–1.25) | 1.05 (0.96–1.15) | 1.01 (0.90–1.14) | 1.06 (0.98–1.15) | 1.10 (0.98–1.22) | 1.00 (0.85–1.18) | 1.27 (0.97–1.68) | 0.82 |
| Blood glucose | 1.13* (1.08–1.18) | 1.21* (1.09–1.35) | 1.09 (1.00–1.20) | 1.23 (0.98–1.55) | 1.11* (1.04–1.19) | 1.10 (0.98–1.23) | 1.19 (0.95–1.49) | 1.27 (0.83–1.96) | 0.67 |
Models are adjusted for age, sex, Hispanic/Latino background (except in stratified models), income, education, nativity, health insurance, marital status, and field center. The interaction term of Hispanic/Latino background group and each LE8 cardiovascular health metric is significant (P<0.1) for body mass index only. Cardiovascular health was defined as low (LE8 score <50%), moderate (LE8 score 50% to <80%), or high (LE8 score ≥80%). HCHS/SOL indicates Hispanic Community Health Study/Study of Latinos; IDR, incidence density ratio; and LE8, Life's Essential 8.
Indicates estimates are significant (P<0.05).
Discussion
In a large cohort of diverse US Hispanic/Latino adults, only 1 in 5 adults had high cardiovascular health. Described for the first time using the American Heart Association's recently updated LE8, the prevalence of high cardiovascular health varied, with people of Mexican background having more favorable cardiovascular health compared with all other Hispanic/Latino background groups. We also found a strong association between a less favorable LE8 score with incidence of hypertension over 6 years. This finding was unchanged when excluding blood pressure from the calculation of LE8. Our results demonstrate a need for improvement in population‐level cardiovascular health among US Hispanics/Latinos and emphasize the importance of cardiovascular health for the prevention of hypertension.
Among US Hispanics/Latinos, LE8 ranged from 62.2 among Puerto Ricans to 72.6 among those of Mexican background. While these findings are largely consistent with a prior study showing heterogeneity in cardiovascular health across Hispanic/Latino subgroups study (defined using LS7), 5 in the current study, Mexican background had the highest prevalence of high cardiovascular health. The higher LE8 score among those of Mexican background can be explained by relatively favorable scores for all LE8 cardiovascular health metrics, especially diet. 23 Mexican diet score (59.1) was at least 15 higher than any other Hispanic/Latino background group. Other LE8 cardiovascular metrics with substantial variation across Hispanic/Latino background group included nicotine exposure, blood lipids, physical activity, and blood pressure. Notably, as the key addition to LS7, sleep health, an important cardiovascular health risk factor, 1 , 24 , 25 , 26 did not vary considerably by Hispanic/Latino background, except for a lower score among Puerto Ricans. Taken together, these findings offer insights that can inform potential interventions strategies to reduce CVD disparities among US Hispanic/Latino adults. For example, targeting sleep health or nicotine exposure among Puerto Ricans 27 or diet among Cubans 5 , 23 may be particularly beneficial for these groups.
Consistent with results from the nationally representative NHANES study, 22 we found that higher SES (greater educational attainment and income) was associated with more favorable LE8 scores. However, results from NHANES also showed a significantly lower (less favorable) LE8 score among Mexican Americans (62.8) 22 compared with our results among HCHS/SOL participants of Mexican background (71.4), even when age‐standardized to the US age distribution. Among other Hispanic/Latinos, not of Mexican background, our results were similar to what was reported nationally from NHANES. 22 We posit that the discrepant findings, particularly among Hispanic/Latinos of Mexican background may be due to key differences in the populations sampled. First, we note that the HCHS/SOL sample is an urban population and not representative of all Hispanics/Latinos in the United States. Next, the share of the US Hispanic/Latino population that is foreign‐born, including Mexican‐born, 28 has decreased in recent decades from 40% in 2000 to 33% in 2019. 29 On the other hand, the HCHS/SOL sample is roughly 80% US territory– or foreign‐born and of disproportionately lower socioeconomic status than US Hispanics/Latinos as a whole.
The healthy immigrant effect 30 posits that immigrants have better health than comparable natives when they first arrive in the host country, but as time spent in the new country increases, immigrant health worsens and converges to that of natives and sometimes worsens further. 31 , 32 In our study, LE8 score was least favorable among Puerto Ricans, a group with the smallest proportion born outside of the US 50 states/District of Columbia (50%). 33 Further, among US territory‐ and foreign‐born HCHS/SOL participants, scores for LE8 and individual LE8 cardiovascular health metrics were consistently lower (worse) with more time lived in the United States. However, it is important to acknowledge that the acculturative process is multi‐dimensional, complex, and not necessarily linear. 34 , 35 Health benefits of acculturation and second‐generation status have also been reported among Hispanic/Latino communities in the United States. In our study, Hispanic/Latino people who were born in the 50 US states/District of Columbia tended to have similar LE8 scores compared with those who had recently migrated to the 50 US states/District of Columbia. This is attributed to the different patterns across different LE8 cardiovascular health metrics. For example, as shown in Table S2 and consistent with a large body of literature, 23 , 36 Hispanics/Latinos born in the 50 US states/District of Columbia had the least favorable diet score. Yet this same group also had the most favorable scores for physical activity, nicotine exposure, and clinical LE8 cardiovascular health metrics (eg, blood pressure, glucose, lipids). These findings may reflect improvement in certain behaviors (self‐reported physical activity) 37 or better access and uptake of medical care 38 , 39 with increasing acculturation or second‐generation status.
Importantly, though blood pressure is an LE8 cardiovascular health metric, other LE8 cardiovascular health metrics such as diet 9 and physical activity 10 are also risk factors for hypertension. Studies that have included non‐Hispanic/Latino Black or White adults have shown strong graded associations with less favorable LS7 scores and incident hypertension. 11 , 40 We extend these findings to Hispanics/Latinos and, to our knowledge, report for the first time that less favorable LE8 score is associated with incident hypertension. In fact, low compared with high cardiovascular health was associated with a more than doubling of hypertension risk, even when blood pressure was not factored into the cardiovascular health score, emphasizing the importance of a healthy lifestyle for the prevention of hypertension, the leading cause of CVD. 8 , 41 Within this context, it is not surprising that among diverse US Hispanics/Latinos, the lowest rates of incident hypertension have been reported among Mexican Americans, 7 the group with the most favorable cardiovascular health profile. Our findings also highlight that even moderate improvements to cardiovascular health are associated with lower rates of hypertension. Such improvements could be achieved through larger changes to few LE8 cardiovascular health metrics or smaller changes to multiple LE8 cardiovascular health metrics. For example, decrements of 10 points to LE8 or 20 points to nicotine exposure, BMI, blood lipids, and blood glucose score were all associated with hypertension.
This work is not without limitations. All behavioral LE8 cardiovascular health metrics were defined on the basis of self‐reported information. However, measures used in HCHS/SOL are directly comparable to other large surveys, including the NHANES study. Further, it is unlikely that any measurement error associated with self‐reported measures are more likely in certain Hispanic/Latino background groups. Differences in subject cognition, memory status, and cooperation levels may have further affected recall, but given that 90% of the population is aged <65 years, it is unlikely that these contributions are substantial. Further, our definition of nicotine exposure was limited to information on secondhand smoke exposure and cigarette smoking. Therefore, nicotine exposure may be underestimated in this sample, as it fails to account for exposure to other combustible tobacco products such as cigars or little cigarettes previously reported in this sample. 27 However, we emphasize that measurement of LE8 cardiovascular health metrics, including nicotine exposure, within the HCHS/SOL sample is comparable to other large population‐based surveys such as NHANES. Another limitation is that HCHS/SOL sample does not include other US racial and ethnic groups for comparison. However, by age‐standardizing our LE8 estimates, we were able to contrast our results with nationally reported data. Another important consideration is the impact of geography or place with respect to health risk factors. Countless studies have shown that the neighborhood physical and social environment can influence health‐related behaviors, including but not limited to sleep, 42 physical activity, 43 and overall cardiovascular health. 44 , 45 In the current study, across all Hispanic/Latino background groups, mean LE8 scores were consistently more favorable in San Diego or Chicago compared with Miami or the Bronx (as shown in Table S3). While Mexican Americans had the most favorable cardiovascular health scores, Mexican Americans in the HCHS/SOL were also overwhelmingly sampled from San Diego, California. To address this issue, we standardized all LE8 estimates to geographic site and found similar yet attenuated findings (as shown in Table S5). However, we acknowledge as a limitation that we could not fully disentangle Hispanic/Latino background from study site, as we were relatively limited in site‐specific sample size for some Hispanic/Latino groups. We also acknowledge a substantial loss to follow‐up in the 6 years between study visits. Though we could not overcome this limitation, HCHS/SOL survey weights were calculated to account for participant nonresponse at visit 2. Finally, though we used standardized approaches to measure blood pressure, 6 , 19 diagnosis of hypertension requires an elevated blood pressure measurement on 2 separate occasions. 46 Despite these limitations, this study has numerous strengths. First, the HCHS/SOL sample is large and diverse, with over 16 000 participants at baseline. It also includes clinically ascertained measures in addition to validated questionnaires for the assessment of LE8 score. Finally, this research makes an important contribution to the literature by providing a first description of cardiovascular health among diverse US Hispanic/Latino adults using the updated American Heart Association's LE8 metric.
Maintaining high cardiovascular health is critical for the prevention of CVD. Among diverse US Hispanic/Latino persons, only 1 in 5 adults had high cardiovascular health, with differences by Hispanic/Latino background group. Though Hispanic/Latino cardiovascular health was favorable compared with the US population as a whole, improvements to cardiovascular health among Hispanics/Latinos are warranted, especially as the US Hispanic/Latino population continues to grow at a fast rate. Our findings further demonstrate that cardiovascular health is associated with hypertension and suggest that even moderate improvements to cardiovascular health may prevent hypertension, a leading risk factor for CVD.
Sources of Funding
The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute to the University of North Carolina (N01‐HC65233), University of Miami (N01‐HC65234), Albert Einstein College of Medicine (N01‐HC65235), Northwestern University (N01‐HC65236), and San Diego State University (N01‐HC65237).
Disclosures
Dr Elfassy is supported by the National Institute on Minority Health and Health Disparities (K01MD014158); Dr Bello is supported by NIH/National Heart, Lung, and Blood Institute (K23‐HL136853), (R01‐HL153382), and NIH/National Institute on Aging (R01‐AG074355). The remaining authors have no disclosures to report.
Supporting information
Tables S1–S6
This manuscript was sent to Tiffany M. Powell‐Wiley, MD MPH, Associate Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.031337
For Sources of Funding and Disclosures, see page 11.
References
- 1. Lloyd‐Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, Grandner MA, Lavretsky H, Perak AM, Sharma G, et al. Life's Essential 8: updating and enhancing the American Heart Association's construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yi J, Wang L, Guo X, Ren X. Association of Life's Essential 8 with all‐cause and cardiovascular mortality among US adults: a prospective cohort study from the NHANES 2005‐2014. Nutr Metab Cardiovasc Dis. 2023;33:1134–1143. doi: 10.1016/j.numecd.2023.01.021 [DOI] [PubMed] [Google Scholar]
- 3. Isiozor NM, Kunutsor SK, Voutilainen A, Laukkanen JA. Life's Essential 8 and the risk of cardiovascular disease death and all‐cause mortality in Finnish men. Eur J Prev Cardiol. 2023;30:658–667. doi: 10.1093/eurjpc/zwad040 [DOI] [PubMed] [Google Scholar]
- 4. Lloyd‐Jones DM, Ning H, Labarthe D, Brewer L, Sharma G, Rosamond W, Foraker RE, Black T, Grandner MA, Allen NB, et al. Status of cardiovascular health in US adults and children using the American Heart Association's new "Life's Essential 8" metrics: prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013–2018. Circulation. 2022;146:822–835. [DOI] [PubMed] [Google Scholar]
- 5. González HM, Tarraf W, Rodríguez CJ, Gallo LC, Sacco RL, Talavera GA, Heiss G, Kizer JR, Hernandez R, Davis S, et al. Cardiovascular health among diverse Hispanics/Latinos: Hispanic Community Health Study/Study of Latinos (HCHS/SOL) results. Am Heart J. 2016;176:134–144. doi: 10.1016/j.ahj.2016.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sorlie PD, Allison MA, Avilés‐Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, Lavange LM, Raij L, Schneiderman N, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27:793–800. doi: 10.1093/ajh/hpu003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Elfassy T, Hazzouri AZA, Cai J, Baldoni PL, Llabre MM, Rundek T, Raij L, Lash JP, Talavera GA, Wassertheil‐Smoller S, et al. Incidence of hypertension among US Hispanics/Latinos: the Hispanic Community Health Study/Study of Latinos, 2008 to 2017. J Am Heart Assoc. 2020;9:e015031. doi: 10.1161/JAHA.119.015031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75:285–292. doi: 10.1161/HYPERTENSIONAHA.119.14240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Appel L, Brands BW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension. A scientific statement from the American Heart Association. Hypertension. 2006;47:296–308. doi: 10.1161/01.HYP.0000202568.01167.B6 [DOI] [PubMed] [Google Scholar]
- 10. Hegde SM, Solomon SD. Influence of physical activity on hypertension and cardiac structure and function. Curr Hypertens Rep. 2015;17:77. doi: 10.1007/s11906-015-0588-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Booth JN III, Abdalla M, Tanner RM, Diaz KM, Bromfield SG, Tajeu GS, Correa A, Sims M, Ogedegbe G, Bress AP, et al. Cardiovascular health and incident hypertension in blacks: JHS (the Jackson Heart Study). Hypertension. 2017;70:285–292. doi: 10.1161/HYPERTENSIONAHA.117.09278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sorlie PD, Avilés‐Santa LM, Wassertheil‐Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lavange LM, Kalsbeek WD, Sorlie PD, Avilés‐Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–1018. doi: 10.3945/jn.111.157222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hoos T, Espinoza N, Marshall S, Arredondo EM. Validity of the Global Physical Activity Questionnaire (GPAQ) in adult Latinas. J Phys Act Health. 2012;9:698–705. doi: 10.1123/jpah.9.5.698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6:790–804. doi: 10.1123/jpah.6.6.790 [DOI] [PubMed] [Google Scholar]
- 17. Rodriguez CJ, Daviglus ML, Swett K, González HM, Gallo LC, Wassertheil‐Smoller S, Giachello AL, Teng Y, Schneiderman N, Talavera GA, et al. Dyslipidemia patterns among Hispanics/Latinos of diverse background in the United States. Am J Med. 2014;127:1186–1194.e1181. doi: 10.1016/j.amjmed.2014.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schneiderman N, Llabre M, Cowie CC, Barnhart J, Carnethon M, Gallo LC, Giachello AL, Heiss G, Kaplan RC, LaVange LM, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014;37:2233–2239. doi: 10.2337/dc13-2939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. HCHS/SOL . Manual 2: Field center procedures. Published 2011. Updated 1/18/2011. Accessed 04/25/2023. https://sites.cscc.unc.edu/hchs/system/files/protocols‐manuals/UNLICOMMManual02FieldCenterProceduresv2301182011.pdf
- 20. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e484–e594. doi: 10.1161/CIR.0000000000000596 [DOI] [PubMed] [Google Scholar]
- 21. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES‐D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84. doi: 10.1016/S0749-3797(18)30622-6 [DOI] [PubMed] [Google Scholar]
- 22. Lloyd‐Jones DM, Ning H, Labarthe D, Brewer L, Sharma G, Rosamond W, Foraker RE, Black T, Grandner MA, Allen NB, et al. Status of cardiovascular health in US adults and children using the American Heart Association's new “Life's Essential 8” metrics: prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013 through 2018. Circulation. 2022;146:822–835. doi: 10.1161/CIRCULATIONAHA.122.060911 [DOI] [PubMed] [Google Scholar]
- 23. Siega‐Riz AM, Pace ND, Butera NM, Van Horn L, Daviglus ML, Harnack L, Mossavar‐Rahmani Y, Rock CL, Pereira RI, Sotres‐Alvarez D. How well do U.S. Hispanics adhere to the dietary guidelines for Americans? Results from the Hispanic Community Health Study/Study of Latinos. Health Equity. 2019;3:319–327. doi: 10.1089/heq.2018.0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pienaar PR, Kolbe‐Alexander TL, van Mechelen W, Boot CRL, Roden LC, Lambert EV, Rae DE. Associations between self‐reported sleep duration and mortality in employed individuals: systematic review and meta‐analysis. Am J Health Promot. 2021;35:853–865. doi: 10.1177/0890117121992288 [DOI] [PubMed] [Google Scholar]
- 25. García‐Perdomo HA, Zapata‐Copete J, Rojas‐Cerón CA. Sleep duration and risk of all‐cause mortality: a systematic review and meta‐analysis. Epidemiol Psychiatr Sci. 2019;28:578–588. doi: 10.1017/S2045796018000379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yin J, Jin X, Shan Z, Li S, Huang H, Li P, Peng X, Peng Z, Yu K, Bao W, et al. Relationship of sleep duration with all‐cause mortality and cardiovascular events: a systematic review and dose‐response meta‐analysis of prospective cohort studies. J Am Heart Assoc. 2017;6:e005947. doi: 10.1161/JAHA.117.005947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kaplan RC, Bangdiwala SI, Barnhart JM, Castañeda SF, Gellman MD, Lee DJ, Pérez‐Stable EJ, Talavera GA, Youngblood ME, Giachello AL. Smoking among U.S. Hispanic/Latino adults: the Hispanic Community Health Study/Study of Latinos. Am J Prev Med. 2014;46:496–506. doi: 10.1016/j.amepre.2014.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Noe‐Bustamante L, Flores A, Shah S, Center PR. FACTS ON MEXICAN‐ORIGIN LATINOS IN THE U.S., 2017. Published 2019. Accessed 04/25/2023. https://www.california‐mexicocenter.org/facts‐on‐mexican‐origin‐latinos‐in‐the‐u‐s‐2017/
- 29. Funk C, Lopez MH, Center PR. A brief statistical portrait of U.S. Hispanics. Published 2022. Accessed 04/25/2023. https://www.pewresearch.org/science/2022/06/14/a‐brief‐statistical‐portrait‐of‐u‐s‐hispanics/
- 30. Markides KS, Rote S. The healthy immigrant effect and aging in the United States and other western countries. Gerontologist. 2019;59:205–214. doi: 10.1093/geront/gny136 [DOI] [PubMed] [Google Scholar]
- 31. Ichou M, Wallace M. The healthy immigrant effect: the role of educational selectivity in the good health of migrants. Demogr Res. 2019;40:61–94. doi: 10.4054/DemRes.2019.40.4 [DOI] [Google Scholar]
- 32. Juárez SP, Honkaniemi H, Gustafsson NK, Rostila M, Berg L. Health risk behaviours by immigrants' duration of residence: a systematic review and meta‐analysis. Int J Public Health. 2022;67:1604437. doi: 10.3389/ijph.2022.1604437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Daviglus ML, Talavera GA, Avilés‐Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. doi: 10.1001/jama.2012.14517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schumann M, Bug M, Kajikhina K, Koschollek C, Bartig S, Lampert T, Santos‐Hövener C. The concept of acculturation in epidemiological research among migrant populations: a systematic review. SSM Popul Health. 2020;10:100539. doi: 10.1016/j.ssmph.2020.100539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65:237–251. doi: 10.1037/a0019330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Montez JK, Eschbach K. Country of birth and language are uniquely associated with intakes of fat, fiber, and fruits and vegetables among Mexican‐American women in the United States. J Am Diet Assoc. 2008;108:473–480. doi: 10.1016/j.jada.2007.12.008 [DOI] [PubMed] [Google Scholar]
- 37. Camplain R, Sotres‐Alvarez D, Alvarez C, Wilson R, Perreira KM, Castañeda SF, Merchant G, Gellman MD, Chambers EC, Gallo LC, et al. The association of acculturation with accelerometer‐assessed and self‐reported physical activity and sedentary behavior: the Hispanic Community Health Study/Study of Latinos. Prev Med Rep. 2020;17:101050. doi: 10.1016/j.pmedr.2020.101050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Thamer M, Richard C, Casebeer AW, Ray NF. Health insurance coverage among foreign‐born us residents: the impact of race, ethnicity, and length of residence. Am J Public Health. 1997;87:96–102. doi: 10.2105/AJPH.87.1.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Plante TB, Koh I, Judd SE, Howard G, Howard VJ, Zakai NA, Booth JN, Safford MM, Muntner P, Cushman M. Life's Simple 7 and incident hypertension: the REGARDS study. J Am Heart Assoc. 2020;9:e016482. doi: 10.1161/JAHA.120.016482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/S0140-6736(02)11911-8 [DOI] [PubMed] [Google Scholar]
- 42. Desantis AS, Diez Roux AV, Moore K, Baron KG, Mujahid MS, Nieto FJ. Associations of neighborhood characteristics with sleep timing and quality: the Multi‐Ethnic Study of Atherosclerosis. Sleep. 2013;36:1543–1551. doi: 10.5665/sleep.3054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Samuel LJ, Dennison Himmelfarb CR, Szklo M, Seeman TE, Echeverria SE, Diez Roux AV. Social engagement and chronic disease risk behaviors: the Multi‐Ethnic Study of Atherosclerosis. Prev Med. 2015;71:61–66. doi: 10.1016/j.ypmed.2014.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Unger E, Diez‐Roux AV, Lloyd‐Jones DM, Mujahid MS, Nettleton JA, Bertoni A, Badon SE, Ning H, Allen NB. Association of neighborhood characteristics with cardiovascular health in the Multi‐Ethnic Study of Atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7:524–531. doi: 10.1161/CIRCOUTCOMES.113.000698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. [DOI] [PubMed] [Google Scholar]
- 46. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S6


