Abstract
Background
Data on national trends in mortality due to infective endocarditis (IE) in the United States are limited.
Methods and Results
Utilizing the multiple causes of death data from the Centers for Disease Control and Prevention's Wide‐Ranging Online Data for Epidemiologic Research database from 1999 to 2020, IE and substance use were identified using the International Classification of Diseases, Tenth Revision, Clinical Modification codes. Between 1999 and 2020, the IE‐related age‐adjusted mortality rates declined. IE‐related crude mortality accelerated significantly in the age groups 25–34 years (average annual percentage change, 5.4 [95% CI, 3.1–7.7]; P<0.001) and 35–44 years (average annual percentage change, 2.3 [95% CI, 1.3–3.3]; P<0.001), but remained stagnant in those aged 45–54 years (average annual percentage change, 0.5 [95% CI, −1.9 to 3]; P=0.684), and showed a significant decline in those aged ≥55 years. A concomitant substance use disorder as multiple causes of death in those with IE increased drastically in the 25–44 years age group (P<0.001). The states of Kentucky, Tennessee, and West Virginia showed an acceleration in age‐adjusted mortality rates in contrast to other states, where there was predominantly a decline or static trend for IE.
Conclusions
Age‐adjusted mortality rates due to IE in the overall population have declined. The marked acceleration in mortality in the 25‐ to 44‐year age group is a cause for alarm. Regional differences with acceleration in IE mortality rates were noted in Kentucky, Tennessee, and West Virginia. We speculate that this acceleration was likely due mainly to the opioid crisis that has engulfed several states and involved principally younger adults.
Keywords: age‐adjusted mortality, infective endocarditis, mortality, opioid epidemic, trends, United States
Subject Categories: Epidemiology, Cardiovascular Disease
Nonstandard Abbreviations and Acronyms
- AAMR
age‐adjusted mortality rates
- AAPC
average annual percentage changes
- CDC WONDER
Centers for Disease Control and Prevention Wide‐Ranging Online Data for Epidemiologic Research
- IDU
injection drug use
- IDU‐IE
injection drug use–related infective endocarditis
- IE
infective endocarditis
- MCOD
multiple causes of death
- UCOD
underlying cause of death
Clinical Perspective.
What Is New?
In this national cross‐sectional study, despite an overall declining trend in infective endocarditis–related mortality, an acceleration in deaths was noted among younger adults aged 25 years to 44 years.
A notable increase in the prevalence of substance use disorder in those with infective endocarditis as the underlying cause of death was observed in the younger age groups.
State‐level trends revealed that Kentucky, Tennessee, and West Virginia had a drastic increase in infective endocarditis–related mortality.
What Are the Clinical Implications?
The acceleration in infective endocarditis deaths noted among adults aged 25 years to 44 years is a cause for concern.
Further studies are needed to identify the reasons for increased mortality in the younger age groups and in the above states.
It remains to be seen whether harm reduction programs addressing injection drug use will impact the epidemiology of infective endocarditis.
Infective endocarditis (IE) is associated with significant morbidity and mortality. Despite an increase in IE‐related hospitalizations in the United States over recent years, a declining trend in in‐hospital mortality has been reported. 1 Similar trends were observed globally, except that the age‐standardized death rate has been stable. 2 Although these prior studies attempted to examine the contemporary IE trends among the US adults, they reported either in‐hospital outcomes only 1 , 3 or were restricted to a geographic area. 4 , 5 , 6 The United States is currently in the midst of the worst opioid crisis, with at least 1 in 10 Americans using illicit drugs. 7 IE remains one of the most dreaded complications of injection drug use (IDU). 8 The traditional epidemiology of IE in the United States has transformed with the ongoing opioid epidemic, wherein increased prevalence of IDU, especially among younger, otherwise healthy adults, has made them the most vulnerable population. 9 , 10 , 11 , 12 Furthermore, data on the impact of the opioid epidemic on IE‐related mortality at the national level is limited. In this context, we examined the US national trends in mortality related to IE and evaluated age‐, sex‐, race‐, and geography‐related mortality differences among individual states in the United States using death certificate data and the association with substance use disorder, considering the emergence of the opioid epidemic.
METHODS
Study data can be requested at the Centers for Disease Control and Prevention Wide‐Ranging Online Data for Epidemiologic Research (CDC WONDER) website at https://wonder.cdc.gov/mcd‐icd10.html.
Data Source
The CDC WONDER multiple causes of death (MCOD) data set was used to analyze deaths occurring within the United States with IE listed as the underlying cause of death (UCOD). The MCOD data set contains mortality and population counts for all US. counties. The death certificate data are reported by 57 vital statistics jurisdictions (the states, District of Columbia, New York City, and 5 territories) in the United States through the Vital Statistics Cooperative. The MCOD data are compiled by the National Center for Health Statistics at the CDC. The UCOD, MCOD, and demographic descriptors are indicated on the death certificates. Each death certificate contains a single UCOD, up to 20 additional multiple (or contributing) causes, and demographic data. The deaths need not have been in the hospital and could have occurred outside of the hospital as well. The CDC WONDER database has been utilized to study trends of mortality in various disease states. 13 , 14 Informed consent was not applicable as the data are deidentified and public. This study was exempt from local institutional review board approval because the CDC WONDER database includes only deidentified publicly available data.
Study Design, Setting, and Participants
This study uses a cross‐sectional study design examining the deaths of all individuals with a diagnosis of IE who were 15 years and older during 1999 to 2020. IE was identified as the UCOD using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10CM) I33.0, I33.9, I38, and B37.6 (Table S1). Substance use was defined as any mention of the following ICD‐10 codes in the MCOD section: T40.0–T40.4, T40.6, F11, F13–F16, F19, X42, and B17.1 (intravenous drug abuse, psychoactive substance abuse, or acute hepatitis C). 15
Study Variables
Outcome Variables
Our study investigated the following end points: (1) trends in overall IE‐related age‐adjusted mortality rates (AAMR) and corresponding standard errors; (2) trends in IE‐related AAMR stratified by sex, race, and urbanicity in the United States; (3) trends in IE‐related crude mortality in different age groups; (4) state‐level trends in AAMR (based on average annual percentage change), where IE was listed as the UCOD; (5) IE mortality (IE as the UCOD); and (6) IE and substance use disorder (listed as comorbidities) in different age groups.
Other Variables Included in the Analyses
Sex was included as a dichotomous variable. Participants' race was reported as American Indian or Alaska Native, Asian or Pacific Islander, Black or African American, and White. Individuals who identified as American Indian, Alaskan Native, Asian, or Pacific Islander were merged into a group referred to as others, due to the limited number of cases occurring in each individual racial group. Metropolitan areas are reported as large central and large fringe metro (population >1 million persons), medium metro (population between 250 000 to <1 million persons), small metro (population <250 000 persons), micropolitan (urban cluster with a population between 10 000 and <50 000 persons) and noncore (not meeting any of the above definitions) according to the 2013 National Center for Health Statistics Urban–Rural Classification Scheme for Counties. 16 Metropolitan areas were grouped as large metro (large central metro, large fringe metro), small metro (medium metro, small metro), and nonmetro areas (micropolitan and noncore). The location of death was also determined from the death certificates as medical facilities, home, hospice, and nursing home/long‐term care facility.
Statistical Analysis
AAMRs, SEs, and 95% CI were calculated by standardizing IE‐related deaths to the corresponding year 2000 US population, as described by the National Center for Health Statistics. 17 , 18 The Joinpoint regression program (version 5.0.2; National Cancer Institute) was used to describe trends in AAMR of IE‐related mortality. 19 Temporal trends in AAMR were determined by fitting log‐linear regression models. We applied Joinpoint segmented regression to identify inflection points in the temporal trends of AAMR for IE from 1999 to 2020 based on published methodological guidelines. 20 Data points with <20 mortality events were flagged unreliable and treated as missing data. For data containing 22 to 26 time points, the guidelines recommend that the analysis identify a maximum of 4 joinpoints across the study period. In the current investigation, 22 years were included; therefore, the Joinpoint regression statistical software was set to determine a maximum of 4 joinpoints where significant temporal variation existed in the trend. Best‐fit models with 1 joinpoint were suggested by the software. The grid search method (2, 2, 0), permutation test, and parametric method were used to estimate annual percent change (APC) and 95% CIs. The average annual percent change (AAPC) over 22 years was then calculated using a weighted average of the slope coefficients of the underlying joinpoint regression line with weights equal to the length of each segment divided by 22. AAPC was considered increasing or decreasing if the slope describing the change in age‐adjusted mortality was significantly different from 0 using 2‐tailed t test with P values <0.05 considered statistically significant. National, state, and age group–specific crude mortality rates were performed in different age groups (15–24 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years, 65–74 years, 75–84 years, and ≥85 years). Analyses were further stratified by race, sex, and urbanicity, where appropriate. Age period cohort analysis was also performed to distinguish between birth cohort and period effect. A secondary analysis was performed using IE as a contributing cause of death.
Temporal trends in AAMR were also determined in the 50 states in the United States and the District of Columbia. Comparison of mortality in IE as the UCOD and IE with substance use disorders as comorbidities during 3 arbitrary time periods, 1999–2006, 2007–2013, and 2013–2020, are described for the 25‐ to 64‐year age groups.
RESULTS
General Population
The IE‐related AAMR in the United States was 26.19 (95% CI, 25.5–26.88) per million persons in 1999 and 22.41 (95% CI, 21.88–22.95) per million persons in 2020. There was a significant decline in the IE‐related AAMR with an average annual percent change of −0.8 (95% CI, −1.2 to 0.4; P<0.001). The trend line is shown in Figure 1A.
Figure 1. Trend of age‐adjusted mortality rates related to infective endocarditis in the United States (A) and stratified by sex (B), race (C), and urbanicity (D) in the United States from 1999 to 2020.
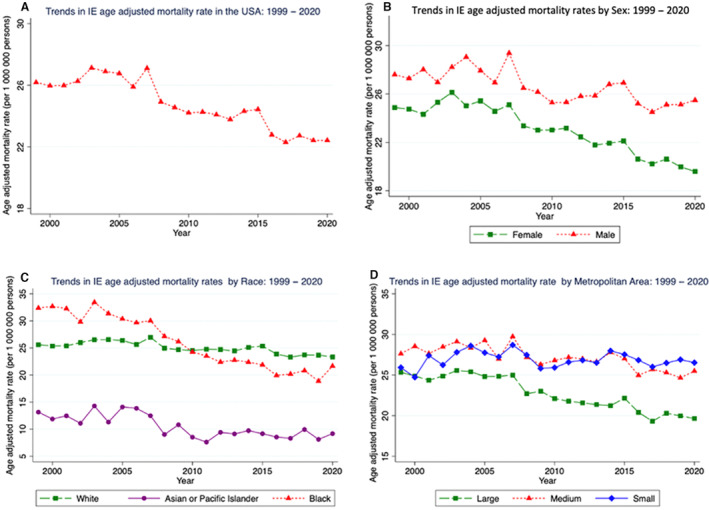
IE indicates infective endocarditis.
The Joinpoint analysis identified 2 time periods (1999–2004, 2004–2020). A nonsignificant increase in the AAMR was noted from 1999 to 2004 with an AAPC of 0.6 (95% CI, −1.0 to 2.3), followed by a significant drop through 2020 with an AAPC of −1.2 (95% CI, −1.5 to −0.9) (Figure S1). The Table shows the demographic characteristics of the study cohort. Of the overall IE deaths, 84 had any mention of immunodeficiency, 10 803 had diabetes, and 9911 had chronic kidney disease, mentioned as MCOD (ICD codes for comorbidities are provided in Table S1).
Table .
Characteristics of Persons Who Died With Infective Endocarditis Listed as the Underlying Cause of Death From 1999 to 2020 in the United States
| Variable | Category | Proportion (%) N=141 516 |
|---|---|---|
| Age groups | 15–40 y | 4.2 |
| 40–65 y | 20.4 | |
| ≥65 y | 75.4 | |
| Sex | Female | 55.1 |
| Male | 44.9 | |
| Place of death | Inpatient | 52.9 |
| Home | 19.0 | |
| Nursing home or long‐term care | 14.5 | |
| Others | 13.6 | |
| Race | White | 87.2 |
| Black | 10.6 | |
| Asian | 1.6 | |
| American Indian or Alaska native | 0.6 | |
| Hispanic origin | Hispanic | 5.0 |
| Non‐Hispanic | 94.8 | |
| Not stated | 0.2 | |
| Metro residence | Large | 47.4 |
| Medium | 33.8 | |
| Small | 18.8 |
Age period cohort analysis revealed that relative risk across birth cohorts was lowest for those born around the year 1960 and has since been on the rise for birth cohorts following the year 1960, with a relative risk of ≈2.3 in the most recent 1990 cohort (Figure S2).
Age
Between 1999 and 2020, IE‐related mortality increased significantly in age groups 25 to 34 years (AAPC 5.4 [95% CI, 3.1–7.7]; P<0.001) and 35 to 44 years (AAPC 2.3 [95% CI, 1.3– 3.3]; P<0.001). IE mortality remained stagnant in those aged 45 to 54 years (0.5 [95% CI, −1.9 to 3]; P=0.684) and showed a significant decline in those aged 55 years and older (−0.4 [95% CI, −0.7 to −0.2]; P=0.003) (Figure 2, Table S2).
Figure 2. Trends in crude mortality by age group from 1999 to 2020.
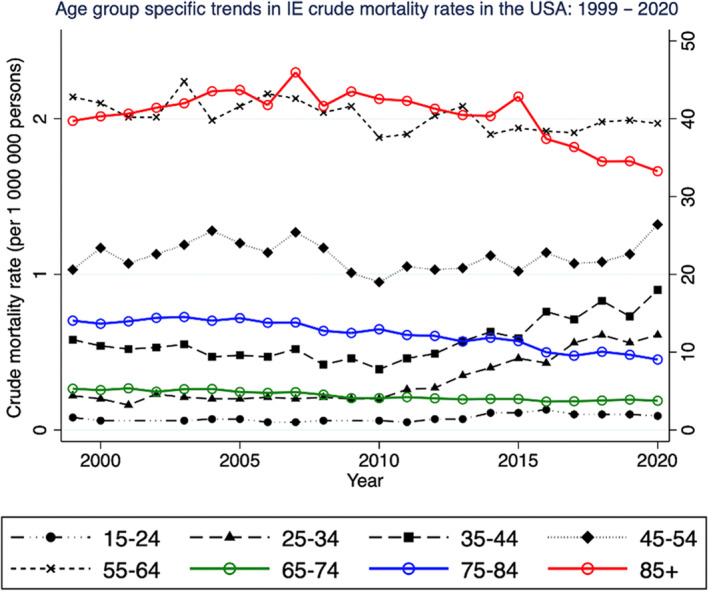
The y axis for all trend lines in color with hollow circle markers (age groups 65–74, 75–84, and 85+ years) is on the right. For all other age groups, use the y axis on the left. IE indicates infective endocarditis.
Sex
The IE‐related AAMR in females decreased from 24.87 (95% CI, 24.01–25.74) per million in 1999 to 19.59 (95% CI, 18.92–20.26) per million in 2020, with an AAPC of −1.0 (95% CI, −1.4 to −0.7; P<0.001). There was a significant decline in the IE‐related AAMR in men from 27.61 (95% CI, 26.47–28.75) per million in 1999 to 25.49 (95% CI, 24.62–26.35) per million in 2020, with an AAPC of −0.6 (95% CI, −0.8 to −0.3; P<0.001). The trend line is shown in Figure 1B.
Race
There was a decline in IE‐related AAMR among all races. The IE‐related AAMR for Black individuals declined from 32.38 (95% CI, 29.87–34.9) per 1 million in 1999 to 21.65 (95% CI, 20.07–23.25) per 1 million in 2020, with an AAPC of −2.1 (95% CI, −3.2 to 1.0; P<0.001). There was a statistically significant decline in IE‐related mortality among White individuals with an AAPC of −0.5 (95% CI, −0.7 to −0.3; P<0.001) as well as Asian and Pacific Islander individuals with an AAPC −1.3 (95% CI, −1.7 to −0.9; P<0.001). IE‐related AAMR in Asian and Pacific Islander individuals dropped from 13.15 (95% CI, 9.9–17.11) per 1 million in 1999 to 9.18 (95% CI, 7.72–10.65) per 1 million in 2020 with a P<0.001. The trend line is shown in Figure 1C. Analysis based on Hispanic origin showed a decline in both Hispanic and non‐Hispanic groups. IE‐related AAMR in Hispanic individuals declined from 17.7 (95% CI, 14.7–19.7) per 1 million in 1999 to 11.5 (95% CI, 10.3–12.7) per 1 million in 2020, with an AAPC of –1.3 (95% CI, −1.9 to −0.5; P<0.05). IE‐related AAMR in non‐Hispanic individuals declined from 26.5 (95% CI, 25.8–27.2) per 1 million in 1999 to 23.7 (95% CI, 23.1–24.3) per 1 million in 2020, with an AAPC of −0.6 (95% CI, −1 to −0.1; P<0.05) (Figure S3).
Urbanicity
There was a significant decline in IE‐related deaths in large metros, with an AAPC −1.4% (95% CI, −1.6 to −1.1; P<0.001) and medium metros with an AAPC of −0.6% (95% CI, −3.1 to −1.3; P<0.001), while there was no significant change in small metros with an AAPC of 0% (95% CI, −0.3 to 0.2; P=0.862). The trend line is shown in Figure 1D.
State‐Level Trends
Between 1999 and 2020, some states showed no significant change in IE‐related AAMR, while other states witnessed either a statistically significant decrease or an increase. States such as Kentucky (AAPC, 1.2 [95% CI, 0.7–1.7]; P<0.001), Tennessee (AAPC, 0.8 [95% CI, 0.2–1.4]; P=0.010), and West Virginia (AAPC, 2 [95% CI, 0.7–3.2]; P=0.003) noted a significant increase in IE‐related mortality during the study period. Figure 3 shows the AAPC in IE‐related AAMR by the state. Table S3 shows the AAPC in IE‐related AAMR for each of the 50 states and District of Columbia for the study period.
Figure 3. State‐level trends in age‐adjusted mortality rates (based on average annual percentage change) with IE listed as the underlying cause of death between 1999 and 2020.
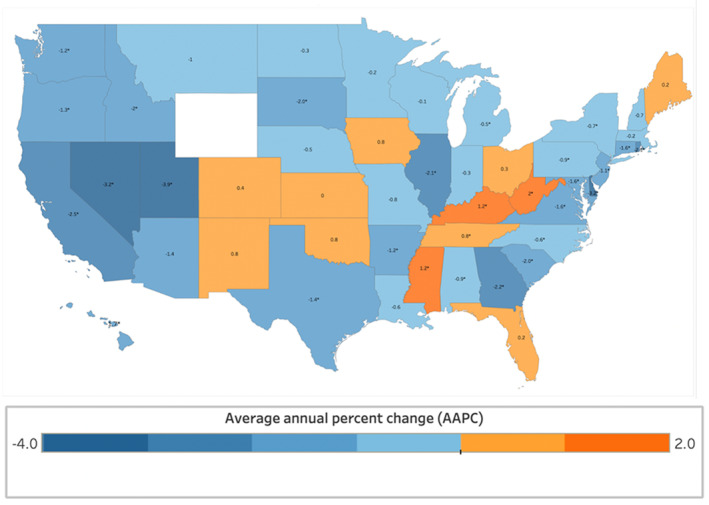
IE indicates infective endocarditis.
The results of secondary analysis using IE as a contributing cause of death are also reported. Overall, the trends in the overall IE and in the subgroups showed largely similar trends to the above analysis (Figures S4 and S5).
IE and Substance Use Disorder
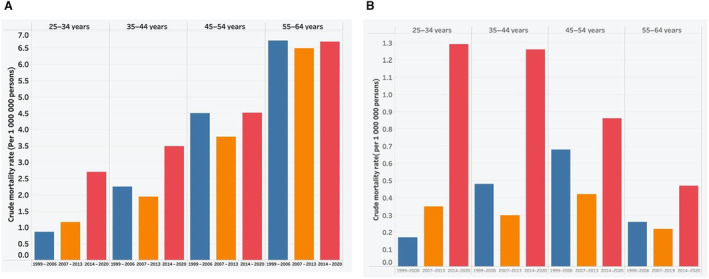
There was a rise in deaths where IE and substance use disorder were listed as comorbidities in those 25 to 34 years of age (0.17/1 million between 1999 and 2006 to 1.29/1 million between 2014 and 2020; P<0.001) and those 35 to 44 years of age (0.48/1 million between 1999 and 2006 to 1.26/1 million between 2014 and 2020; P<0.001) (Figure 4B). Crude mortality due to IE as the UCOD in similar age groups and for the same time periods is shown in Figure 4A. A state‐level analysis with IE and substance use as comorbidities showed Kentucky, Tennessee, and West Virginia to have the highest AAMR (Figure S6).
Figure 4. Comparison of crude mortality rates in different age groups related to infective endocarditis as the underlying cause of death (A) and infective endocarditis and underlying substance use disorders (listed as the underlying cause of death and comorbidities, respectively) (B).
DISCUSSION
Our analysis of the CDC WONDER database to examine IE‐related mortality revealed several notable findings. First, the overall IE‐related mortality declined between 1999 and 2020. However, an acceleration in mortality was noted in the 25–34 and 35–44 year age groups. Second, there was heterogeneity in state‐level trends, with some US states showing an acceleration in IE‐related AAMR contrary to the overall declining trend. Third, IE and substance use disorder were contributing factors to the observed IE‐related mortality trends in the United States among the younger age groups and the states of Kentucky, Tennessee, and West Virginia.
The trends in mortality related to IE have not been studied at a national level. Numerous factors impacted the epidemiology of IE in recent years. First, there has been an increase in the incidence of IE‐related hospitalizations in the United States. A prior study reported a 50% increase in IE hospitalizations in the United States between 2003 and 2016. 1 A few studies have assessed mortality due to IE in hospitalized patients and demonstrated a decline in adjusted mortality over the years. 6 Data from the National Inpatient Sample, for example, showed a 50% decline in mortality between 2003 and 2016. 1 , 21 However, large‐scale studies on mortality due to IE in the community are not available, and a few factors need to be taken into account. First, prior studies reporting a decline in in‐hospital mortality lacked data related to deaths occurring outside of the hospital. 1 , 6 , 21 A study from Finland showed that 9% of IE‐related deaths occur at home. 22 Second, in studies evaluating microbial trends, Staphylococcus aureus has emerged as the predominant microbe and is generally associated with poorer outcomes. 6 Third, the opioid epidemic has transformed the epidemiology of IE. Our study period included 2 waves of the opioid epidemic in 2010 and 2013, as reported by the CDC. 23 In particular, the bulk of right‐sided IE cases among persons who inject drugs is due to S. aureus, as is the majority of left‐sided IE. Moreover, suboptimal use of addiction management in patients with IDU‐related IE has resulted in increased rates of IE relapse and reinfection among younger adults, both of which are related to increased morbidity and mortality. Our study provides the latest data on mortality trends in IE at a national level amidst the backdrop of the above‐mentioned factors. The declining trend in IE mortality in our investigation is likely due to multiple factors. A multidisciplinary approach, advancements in microbiology, antimicrobial therapies, and surgical management (with early surgery associated with reduced mortality) could have contributed to the overall decline in mortality.
The finding of increased mortality in the 25–44 year age group is a cause for concern. These younger age groups are less likely to have significant comorbidities and hospitalizations to be at risk for hospital‐acquired bacteremia and IE and lower risk of mortality. Nonetheless, this uptrend parallels the increase in IE incidence in younger age groups that have been reported. 1 , 15 Our study shows that the IE episodes leading to mortality are likely due to IE in those with substance use disorder. The study by Kadri et al also reported an uptrend in injection drug use–related infective endocarditis (IDU‐IE) in the United States. 10 In addition, the median age reported was 38 years in the IDU‐IE compared with 70 years in the nondrug use IE, supporting the findings of our study. Furthermore, a recent investigation reported a 3‐fold increase in IE deaths among persons who inject drugs as compared with a 1.5‐fold increase noted among the general population. 15 The increase in mortality in these age groups can be due to delay in seeking care leading to clinical presentation with complications of IE and/or multiorgan involvement. Social determinants are likely to play a major role; low socioeconomic status, poor social support, and lack of insurance can be reasons for avoidance or delay in seeking care. In addition, mental health illness, including drug use and patient‐directed discharge leading to incomplete therapy, are prevalent in the younger population. Finally, recidivism is also a problem in persons who inject drugs, leading to multiple IE episodes and prosthesis‐related IE. 24 , 25
A few states demonstrated a significant acceleration in IE‐related AAMR compared with other states that have either shown a static trend or a decrease. The states of Kentucky, Ohio, Tennessee, and West Virginia have been the epicenter of the opioid crisis. Social determinants such as low wages, unemployment, and high poverty rates have been reported as factors for the high burden of opioid use in these states. These states also were victims of rampant overprescribing of prescription opioid drugs. This led to an increase in the availability of prescription drugs on street markets as well as an increase in the number of individuals using prescription opioids for nonmedical use. 26 , 27 IDU is a risk factor for IE, accounting for at least 10% of IE‐related admissions (IDU‐IE). 28 Kadri et al reported an increase in IDU‐IE in the entire United States, with the highest increase noted in the Midwest. 10 The regional variations in the incidence of IDU‐IE in the prior study were reported for 4 geographic regions in the United States. In contrast, our study assessed state‐level mortality trends and adds to the current literature on IE geographic trends. The uptrend in mortality could be attributed to the epidemic of IDU‐IE in these states. 5 , 11 , 29 , 30 Indeed, a study from North Carolina reported a >10‐fold increase in the frequency of IDU‐IE hospitalizations and surgically treated IE from 2007 to 2017. 9 Similarly, single‐institution data from the state of West Virginia showed a dramatic increase in the number of surgeries performed in patients with IE with IDU. 30 In an attempt to combat the IDU epidemic, some states have started harm‐reduction program initiatives. 31 A study from Spain reported low rates of IDU‐related IE and hypothesized the low incidence to be consequent to the establishment of a harm‐reduction program. 32
Our study has several strengths. Novel findings in our study include state‐level and age‐related differences in trends of IE‐related mortality, which are valuable insights for policymakers. The opioid crisis has not only resulted in deaths from overdose but also those related to IE. Our findings are a call for action on continued aggressive efforts to address the opioid crisis with a regional focus. Attention to social determinants of health at an individual level and access to mental rehabilitation services are key in addressing the younger demographic affected by IE and substance use disorders.
Limitations
Our study could not adjust mortality for confounders because the data set only includes information noted on death certificates. Also, due to the aggregate nature of the database, a cause–effect relationship between the uptrend in IE mortality in the younger demographic and substance use disorders cannot be assumed. Death certificate data may be inaccurate with the use of ICD‐10 CM coding, including errors in diagnosis, adjudication of cause of death, and data entry. Lack of clinical data, microbiological data, nature of valvular involvement (native versus prosthetic), single/multi‐valve, antimicrobial, and surgical data are also inherent limitations of the data set. The role of other risk factors associated with IE, such as congenital heart disease, dialysis, indwelling venous catheters, and implantable cardiac devices, could not be assessed. Another major limitation of the study is that the mortality reported in the IE and substance use disorders group may not be primarily due to IE, and death could have been from other causes, such as drug overdose. However, analysis of IE and drug overdose deaths yielded significantly lower numbers and hence was less likely to have influenced our analysis.
CONCLUSIONS
We demonstrated a declining trend in the AAMR due to IE, albeit with an acceleration in mortality in the 25‐to‐44‐year age group, which is a cause for alarm. Geographic differences existed, wherein acceleration in mortality rates was noted in the states of Kentucky, Tennessee, and West Virginia. Furthermore, this acceleration could be ascribed to the substance use disorders that have engulfed some of these states and the above age group. The impact of multipronged harm‐reduction programs on IE‐related mortality trends in the most productive age groups and in certain states remains to be seen.
Sources of Funding
None.
Disclosures
Dr Badhwar serves as a nonremunerative consultant to Abbott. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S3
Figures S1–S6
This manuscript was sent to Sakima A. Smith, MD, MPH, Associate Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.031589
For Sources of Funding and Disclosures, see page 8.
References
- 1. Alkhouli M, Alqahtani F, Alhajji M, Berzingi CO, Sohail MR. Clinical and economic burden of hospitalizations for infective endocarditis in the United States. Mayo Clin Proc. 2020;95:858–866. doi: 10.1016/j.mayocp.2019.08.023 [DOI] [PubMed] [Google Scholar]
- 2. Chen H, Zhan Y, Zhang K, Gao Y, Chen L, Zhan J, Chen Z, Zeng Z. The global, regional, and national burden and trends of infective endocarditis from 1990 to 2019: results from the Global Burden of Disease Study 2019. Front Med (Lausanne). 2022;9:774224. doi: 10.3389/fmed.2022.774224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morita Y, Haruna T, Haruna Y, Nakane E, Yamaji Y, Hayashi H, Hanyu M, Inoko M. Thirty‐day readmission after infective endocarditis: analysis from a nationwide readmission database. J Am Heart Assoc. 2019;8:e011598. doi: 10.1161/JAHA.118.011598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Meisner JA, Anesi J, Chen X, Grande D. Changes in infective endocarditis admissions in Pennsylvania during the opioid epidemic. Clin Infect Dis. 2020;71:1664–1670. doi: 10.1093/cid/ciz1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fleischauer AT, Ruhl L, Rhea S, Barnes E. Hospitalizations for endocarditis and associated health care costs among persons with diagnosed drug dependence–North Carolina, 2010‐2015. MMWR Morb Mortal Wkly Rep. 2017;66:569–573. doi: 10.15585/mmwr.mm6622a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Toyoda N, Chikwe J, Itagaki S, Gelijns AC, Adams DH, Egorova NN. Trends in infective endocarditis in California and New York State, 1998‐2013. JAMA. 2017;317:1652–1660. doi: 10.1001/jama.2017.4287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jamil M, Sultan I, Gleason TG, Navid F, Fallert MA, Suffoletto MS, Kilic A. Infective endocarditis: trends, surgical outcomes, and controversies. J Thorac Dis. 2019;11:4875–4885. doi: 10.21037/jtd.2019.10.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baddour LM, Weimer MB, Wurcel AG, McElhinney DB, Marks LR, Fanucchi LC, Esquer Garrigos Z, Pettersson GB, DeSimone DC. Management of infective endocarditis in people who inject drugs: a scientific statement from the American heart association. Circulation. 2022;146:e187–e201. doi: 10.1161/CIR.0000000000001090 [DOI] [PubMed] [Google Scholar]
- 9. Schranz AJ, Fleischauer A, Chu VH, Wu LT, Rosen DL. Trends in drug use‐associated infective endocarditis and heart valve surgery, 2007 to 2017: a study of statewide discharge data. Ann Intern Med. 2019;170:31–40. doi: 10.7326/M18-2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kadri AN, Wilner B, Hernandez AV, Nakhoul G, Chahine J, Griffin B, Pettersson G, Grimm R, Navia J, Gordon S, et al. Geographic trends, patient characteristics, and outcomes of infective endocarditis associated with drug abuse in the United States from 2002 to 2016. J Am Heart Assoc. 2019;8:e012969. doi: 10.1161/JAHA.119.012969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bhandari R, Alexander T, Annie FH, Kaleem U, Irfan A, Balla S, Wiener RC, Cook C, Nanjundappa A, Bates M, et al. Steep rise in drug use‐associated infective endocarditis in West Virginia: characteristics and healthcare utilization. PLoS One. 2022;17:e0271510. doi: 10.1371/journal.pone.0271510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wurcel AG, Anderson JE, Chui KK, Skinner S, Knox TA, Snydman DR, Stopka TJ. Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis. 2016;3:ofw157. doi: 10.1093/ofid/ofw157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nazir S, Ariss RW, Minhas AMK, Issa R, Michos ED, Birnbaum Y, Moukarbel GV, Ramanathan PK, Jneid H. Demographic and regional trends of mortality in patients with aortic dissection in the United States, 1999 to 2019. J Am Heart Assoc. 2022;11:e024533. doi: 10.1161/JAHA.121.024533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khan SU, Kalra A, Kapadia SR, Khan MU, Zia Khan M, Khan MS, Mamas MA, Warraich HJ, Nasir K, Michos ED, et al. Demographic, regional, and state‐level trends of mortality in patients with aortic stenosis in United States, 2008 to 2018. J Am Heart Assoc. 2020;9:e017433. doi: 10.1161/JAHA.120.017433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Njoroge LW, Al‐Kindi SG, Koromia GA, ElAmm CA, Oliveira GH. Changes in the association of rising infective endocarditis with mortality in people who inject drugs. JAMA Cardiol. 2018;3:779–780. doi: 10.1001/jamacardio.2018.1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. NCHS Rural Classification Scheme for Counties. Statistics National Center for Health Statistics . Centers for Disease Control and Prevention. Accessed April 29, 2022. https://www.cdc.gov/nchs/data_access/urban_rural.htm#update
- 17. Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47:1–16, 20. [PubMed] [Google Scholar]
- 18. Centers for Disease Control . Multiple Cause of Death 1999–2020: Age‐Adjusted Rates. Accessed September 11, 2023. https://wonder.cdc.gov/wonder/help/mcd.html#Age‐Adjusted%20Rates
- 19. Division of Cancer Controls & Population Sciences NCI . Methodology National Cancer Institute division of cancer control and population sciences. Joinpoint Regression Program, version 5.0.2. Accessed October 4, 2023. https://surveillance.cancer.gov/joinpoint/download
- 20. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: [DOI] [PubMed] [Google Scholar]
- 21. Khan MZ, Munir MB, Khan MU, Khan SU, Benjamin MM, Balla S. Contemporary trends in native valve infective endocarditis in United States (from the National Inpatient Sample Database). Am J Cardiol. 2020;125:1678–1687. doi: 10.1016/j.amjcard.2020.02.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ahtela E, Oksi J, Sipilä J, Rautava P, Kytö V. Occurrence of fatal infective endocarditis: a population‐based study in Finland. BMC Infect Dis. 2019;19:987. doi: 10.1186/s12879-019-4620-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Disease Control and Prevention . Understanding the Opioid Overdose Epidemic. Accessed June 28, 2023. https://www.cdc.gov/opioids/basics/epidemic.htm
- 24. Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication‐assisted therapies—tackling the opioid‐overdose epidemic. N Engl J Med. 2014;370:2063–2066. doi: 10.1056/NEJMp1402780 [DOI] [PubMed] [Google Scholar]
- 25. Thyagaturu HS, Bolton A, Thangjui S, Kumar A, Shah K, Bondi G, Naik R, Sornprom S, Balla S. Effect of leaving against medical advice on 30‐day infective endocarditis readmissions. Expert Rev Cardiovasc Ther. 2022;20:773–781. doi: 10.1080/14779072.2022.2115358 [DOI] [PubMed] [Google Scholar]
- 26. National Institute on Drug Abuse . Drug Overdose Death Rates. National Institute on Drug Abuse (website). Accessed October 24, 2023. https://nida.nih.gov/research‐topics/trends‐statistics/overdose‐death‐rates [Google Scholar]
- 27. Rhodes MB. The Underlying Determinants and Impacts of the Substance Abuse Crisis in Knox, Whitley, and Laurel Counties. Bachelor Thesis. Eastern Kentucky University; 2019;629:1–34. Accessed June 29, 2023. https://encompass.eku.edu/honors_theses/629 [Google Scholar]
- 28. Deo SV, Raza S, Kalra A, Deo VS, Altarabsheh SE, Zia A, Khan MS, Markowitz AH, Sabik JF III, Park SJ. Admissions for infective endocarditis in intravenous drug users. J Am Coll Cardiol. 2018;71:1596–1597. doi: 10.1016/j.jacc.2018.02.011 [DOI] [PubMed] [Google Scholar]
- 29. Bates MC, Annie F, Jha A, Kerns F. Increasing incidence of IV‐drug use associated endocarditis in southern West Virginia and potential economic impact. Clin Cardiol. 2019;42:432–437. doi: 10.1002/clc.23162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cook CC, Rankin JS, Roberts HG, Ailawadi G, Slaughter M, Wei LM, Badhwar V. The opioid epidemic and intravenous drug‐associated endocarditis: a path forward. J Thorac Cardiovasc Surg. 2020;159:1273–1278. doi: 10.1016/j.jtcvs.2019.08.112 [DOI] [PubMed] [Google Scholar]
- 31. Bixler D, Corby‐Lee G, Proescholdbell S, Ramirez T, Kilkenny ME, LaRocco M, Childs R, Brumage MR, Settle AD, Teshale EH, et al. Access to syringe services programs–Kentucky, North Carolina, and West Virginia, 2013‐2017. MMWR Morb Mortal Wkly Rep. 2018;67:529–532. doi: 10.15585/mmwr.mm6718a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Munoz P, Kestler M, De Alarcon A, Miro JM, Bermejo J, Rodriguez‐Abella H, Farinas MC, Cobo Belaustegui M, Mestres C, Llinares P, et al. Current epidemiology and outcome of infective endocarditis: a multicenter, prospective, cohort study. Medicine (Baltimore). 2015;94:e1816. doi: 10.1097/MD.0000000000001816 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3
Figures S1–S6


