ABSTRACT
This study examines how staff pooling can be used to create a higher service level at a predetermined total capacity in the healthcare sector. We develop new empirical knowledge through a systematic empirical study, using a mixed-methods approach, with a preliminary interview study followed by a principal quantitative survey study, with data from a multihospital system. The purpose was to explore practical barriers for a staff pooling strategy in healthcare systems. Three barriers were identified:recruitment difficulties, community view, and specialisation. Significant differences in perceived height among these barriers were found. The results from this study have important managerial implications for healthcare systems when implementing a staff pooling approach. This study contributes to the existing literature since, to the best of our knowledge, no previous research has been done where barriers to staff pools are systematically identified using a holistic approach that includes all healthcare professions in a multihospital system.
KEYWORDS: Capacity planning, healthcare management, staff pooling, barriers, mixed-methods
1. Introduction1
Production and capacity planning is an essential part of healthcare management (Bacelar-Silva et al., 2022; Faeghi et al., 2021; Leeftink et al., 2020). However, due to the constantly increasing scale and scope, local staff shortages as a result of short-term variations in the supply and the demand of healthcare are handled with a mostly reactive logic, which is related to cost issues, inefficient capacity use, and a strained system (Fagefors et al., 2020; Wright & Bretthauer, 2010). Instead, a more resilient model that includes proactive elements is needed (Fagefors et al., 2020; Kuntz et al., 2015; Mahar et al., 2011).
One specific form of proactive planning of healthcare staff is the use of staff pools. A staff pool is a general capacity that can be allocated to parts of the system where the existing workload and demand for capacity is unusually high (Gutjahr & Rauner, 2007; Hopp & Lovejoy, 2013; Kuntz et al., 2015; Vanberkel et al., 2012). Like other OR approaches in healthcare (Brailsford et al., 2021; Corsini et al., 2022; Lamé et al., 2022; Wing & Vanberkel, 2021; Zyl-Cillié et al., 2022), staff pooling is a planning method that can be used to improve utilisation of current resources and for managing bottlenecks in the system (e.g., doctors and specialist nurses). It is a well-established tool in healthcare systems (Cattani & Schmidt, 2005; Dziuba-Ellis, 2006; Fagefors et al., 2020; Kuntz et al., 2015; Mahar et al., 2011; Terwiesch et al., 2011).
However, the use of staff pools may, for several reasons, not be fully applicable in a healthcare system, such as that of Sweden. Even though the theoretical arguments for staff pooling in healthcare are strong, there is also a trade-off in terms of capacity needs for a given service level between smaller pools dedicated to more homogeneous patient groups and larger pools dedicated to a more heterogeneous patient or care mix (Utley & Worthington, 2012). Additionally, practical barriers such as professional specialisation and geographical distance usually limit the number of units that can be organised in the same pool.
The previous literature in the staff pooling area is mainly directed towards the so-called float pools (pools of nurses) and is almost exclusively anecdotal (Bard & Purnomo, 2005; Bates, 2013; Lebanik & Britt, 2015; Linzer et al., 2011; Rowse et al., 2013; Rudy & Sions, 2003). Little is known about how they are organised and structured, in particular in multihospital systems. Thus, there is a lack of systematic research on the support of the implementation of staff pools in healthcare systems (Cattani & Schmidt, 2005; Dziuba-Ellis, 2006; Mahar et al., 2011; Mazurenko et al., 2015; Smith-Daniels et al., 1988). Hence, this study aims to explore the practical barriers for staff pooling in a healthcare system as managers perceive them.
In this paper, we present a systematic empirical study, using a mixed-methods approach, with data from a multihospital system comprising 16 individual hospitals and 202 primary care centres. We confirm previous findings in anecdotal studies and conceptual literature, but also develop new empirical knowledge. We also show the relative importance of the identified barriers, which will have substantial implications for managers when implementing a staff pooling approach. Moreover, the potential barriers are analysed and compared for different manager types (department managers, section managers, and care unit managers) across different organisational levels. To the best of our knowledge, there are no previous studies that have systematically identified and analysed barriers to staff pooling in healthcare systems with this holistic approach.
The remainder of this paper is organised as follows. Section 2 provides a literature review and section 3 contains an introduction to the healthcare system in Sweden. In Sections 4 and 5, the research methodology and empirical findings are presented. The results are then discussed in Section 6. Finally, in Section 7, the conclusions with recommendations for future research are detailed.
2. Literature review
There are three potential ways to pool capacity in a healthcare setting (see, Figure 1): staff pooling, hence allocating staff to where resources are needed (see, e.g., Gutjahr & Rauner, 2007; Hopp & Lovejoy, 2013; Kuntz et al., 2015; Vanberkel et al., 2012); patient pooling, hence allocating patients to where resources are available (see, e.g., Song et al., 2020); and resource pooling, hence organising resources (other than staff), for example, hospital beds, to predetermined units (see, e.g., Bagust et al., 1999; Best et al., 2015; Kadri, 2021; Proudlove & Proudlove NC, 2020). Different types of pools will create different advantages and encounter different types of barriers. For example, song et al. (2020) argue that pooling patients by off-service placement in hospitals is associated with an increased length of stay and hospital readmissions. This might, however, not be an issue in a staff pooling system.
Figure 1.
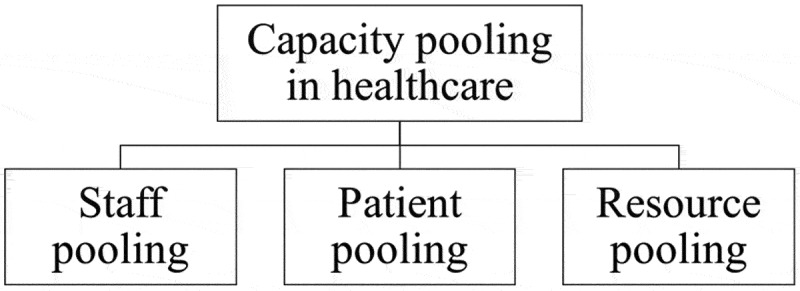
Three types of capacity pools in healthcare services.
Staff pools are a method to achieve the goal of matching current resources effectively with the healthcare demand, yielding shorter waiting times for patients, increased service level, and patient safety (SOU, 2016; Alvekrans et al., 2016; Kc & Terwiesch, 2009; Kuntz et al., 2015; Lupien et al., 2007; Mahar et al., 2011). A recent example where a staff pooling approach was extensively used, although not in a systemised manner, is the allocation of resources during the coronavirus disease (COVID-19) pandemic. In healthcare systems around the world, efforts have been made to identify in-house staff with relevant professional knowledge and reallocate them during a limited period of time to units with COVID-19 patients. For example, in Sweden, Italy and New York, this approach has doubled the capacity of intensive care beds (”Thelocal.com,” 2020; Businessinsider.se, 2020; Zangrillo & Gattinoni, 2020).
In addition, staff pools can be a tool for creating a better working environment, less overtime work and a more attractive workplace (Brandt & Palmgren, 2015; Hultberg, 2007). However, it requires plans to be realised smoothly, even if short-term deviations occur, such as sick leave or unexpectedly high demand. Lu and Lu (2017) argue that staff pools can be used to manage variations in healthcare capacity, thereby reducing excessive use of overtime. Moreover, staff pools are tools that create volume flexibility to manage such deviations, and thus facilitate a better working environment (Hultberg, 2007; Kuntz et al., 2015; Mahar et al., 2011; Noon et al., 2003).
On the other hand, barriers to a staff pooling approach have been reported. For example, professional specialisation in healthcare departments might indicate that it is inappropriate or even impossible to re-allocate staff between units. Furthermore, staff pools can result in a stressful work environment for the employees in the pool, inefficient work due to differing routines and procedures, and possible patient safety issues (Adams et al., 2015; Bates, 2013; Cavouras, 2002; Rudy & Sions, 2003). Rowse et al. (2013) found potential cost savings when organising resources into shared pools through demand simulation, but argued that other ways of working, such as optimising team configurations, could be similarly or even more cost efficient. Moreover, Song et al. (2015) found that the pooling of physicians in an emergency department lead to an increased length of stay, which might have been due to behavioural aspects. According to the authors, the physicians felt a greater responsibility for a smooth patient turnover in a dedicated queueing system compared to a pooled queueing system (ibid.). Observations like these address the importance of taking behavioural considerations into account when designing/implementing staff pooling in healthcare systems (Boudreau et al., 2003; Donohue et al., 2020). Hence, potential barriers to a staff pooling approach must be explored and managed in order to efficiently make use of the potential benefits of a staff pool.
However, from a theoretical perspective, several types of advantages can be achieved through capacity pooling in general, and staff pooling in particular, in healthcare systems (Ata & Van Mieghem, 2009; De Bruin et al., 2007; Cattani & Schmidt, 2005; Hopp & Lovejoy, 2013; Vanberkel et al., 2012). First, the average waiting times can be reduced, sometimes substantially, when a system is characterised by one single queue to all servers rather than individual queues for different servers. Second, when different parts of the system lack different types of essential capacities (e.g., one unit needs more physicians and has a surplus of specialist nurses, while another unit needs more specialist nurses and has a surplus of physicians), a better utilisation can be achieved on an aggregate level through synergy. Third, centralisation of safety capacity can sometimes drastically reduce the need (and therefore the cost) for safety capacity without reducing the service level as some of the variations in actual demand among units will cancel out on an aggregate level.
3. The healthcare system in Sweden
In the Swedish healthcare system, both basic capacity (capacity used to handle expected demand) and safety capacity (capacity used to handle the variations in actual demand) is, to a large extent, planned at the actual unit or department where the short-term need for capacity actually arises (Alvekrans et al., 2016). The advantage of this approach is that the control of capacity is directly linked to the current situation in a unit or department. The significant disadvantage with such an approach is that capacity in different parts of the system is managed independently. Hence, pooling can create the potential for synergy.
One efficient way to handle variations in healthcare capacity is to use temporary agency staff. Hence, it is not surprising to see that the use of temporary agency staff is widespread and increasing. The costs incurred by the Swedish regions for temporary agency staff have increased from SEK 1.9 billion in 2010 to SEK 5.6 billion in 2019.
Since the beginning of 2017, all 21 regions in Sweden operate under an agreement within the Sveriges Kommuner och Regioner (SKR), intending to become independent of costly agency staff in the healthcare sector. SKR is an association for municipalities, county councils, and regions in Sweden. Each region decides, based on its prerequisites, what actions are to be taken to succeed and develop an action plan to achieve the goal. However, a standard measure for all regions is to increase permanent staff by creating more attractive workplaces (SKL, 2017).
According to case studies found in the literature review, a measure to reduce the cost of temporary agency staff is to replace agency staff with a less costly internal staffing agency in order to maintain the flexibility that such staff pools create in staffing planning (Adams et al., 2015; Lebanik & Britt, 2015). The establishment of a region-wide internal staffing agency is also a measure that both Region Västra Götaland and Region Värmland decided to investigate in their action plans to be independent of agency staff. Other Swedish regions are investigating similar arrangements linked to specific parts of their healthcare system, such as primary care and individual hospitals.
4. Materials and methods
4.1. Setting
Region Västra Götaland includes 16 individual hospitals: four university hospitals and twelve rural hospitals. There are also 202 primary health centres and 28 emergency centres in the region. Also, there are four private hospitals with a contractual agreement with the healthcare provider in the region. Furthermore, there are staff pools linked to specific parts of the healthcare system in the region, such as primary care and single hospitals.
The Sahlgrenska University Hospital is a multihospital group in the region and also the biggest in Sweden, with 50 speciality departments. It includes four hospitals and has an internal staffing pool of mainly nurses and assistant nurses. It covers all the specialities in Region Västra Götaland and accounts for approximately 50 % of total healthcare costs in the region. The hospital has approximately 16,500 employees and 2,000 beds and has 50 speciality departments, including cardiology, clinical physiology, children’s medicine, and psychiatry. A designated manager heads each speciality department and has the overall responsibility for the department’s capacity planning. Section managers and care unit managers are responsible for staff scheduling within a speciality department. However, sections managers are responsible for scheduling physicians, while care unit managers are responsible for scheduling nurses and assistant nurses. Hence, capacity planning is decentralised to a specific unit or department within the healthcare organisation.
4.2. Design
A mixed-methods approach was deployed; a qualitative study was first conducted as the complementary method, followed by a quantitative study as the principal method (Morgan, 1998). First, a qualitative design is useful to provide an initial and explorative overview of an area. Therefore, a descriptive study using content analysis (Graneheim & Lundman, 2004) was conducted to provide an overview of the perceived potential barriers of staff pooling in the regional healthcare system. An inductive methodological approach was used, where ten speciality department managers from Sahlgrenska University Hospital and two division managers at Närhälsan, with responsibility for multiple primary care centres, were interviewed regarding their thoughts and experiences of capacity planning in general and staff pooling in particular. Thereafter data from the interviews was analysed using content analysis, which provided knowledge for the deductive methodological approach (Graneheim & Lundman, 2004). Second, a web-based questionnaire was developed and distributed to all departments, units, and section managers in Region Västra Götaland in order to validate the findings in the descriptive study.
4.3. Data collection
In order to ensure representativeness in the descriptive interview study, the speciality departments at Sahlgrenska University hospital were first classified into three different dimensions:
Mainly unplanned or mainly planned activities
Mainly inpatient or mainly outpatient activities
Mainly medical or mainly surgical activities
The respondents were chosen from a total of 50 department managers at the hospital so that all eight possible combinations of dimensions (presented in Figure 2) would be covered during the interviews. For example, the first combination includes mainly medical specialities covering inpatient and unplanned activities.
Figure 2.
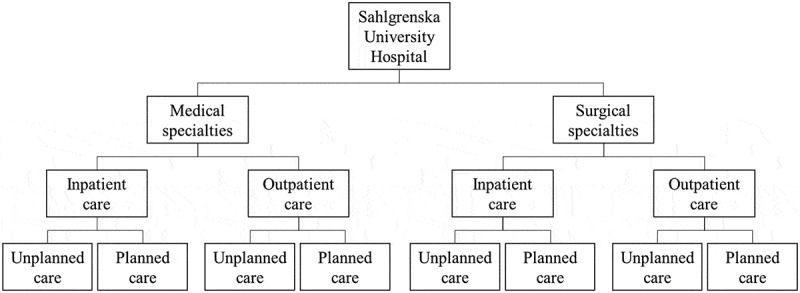
Eight types of departments.
Moreover, department managers at Närhälsan, which consists of 202 primary health centres in the region, were added to cover the local aspect of the healthcare system too. Data were collected during the first half of 2018. Three authors were present at most of the interviews, although a few were conducted by only one or two. All interviews began with a general question on the current situation regarding capacity. During the interviews, the focus was on the perceived need for pooling different categories of staff, if/how pooling is a part of the current capacity management process, and if/how there were plans to develop the pooling perspective within capacity management. All interviews were recorded, transcribed, and used as the basis for the content analysis. The interview study resulted in 22 items grouped in six categories of potential barriers for staff pooling: competence, geography, culture, system, planning, and recruitment.
A web-based questionnaire was thereafter developed in order to validate the findings in the descriptive study. The questionnaire consisted of the 22 items identified in the content analysis. A seven-point Likert scale was used to record answers for each item, where a lower value meant a lower level of agreement with the statement. The questionnaire was tested on the interviewees in the descriptive study before distribution, and after minor adjustments, it was sent to 1,144 managers (at the department, section, and care unit level) in Region Västra Götaland. The questionnaire had a response rate of 41.3 %. The distribution of manager types represented by the participants was in proportion to the distribution of manager types in Region Västra Götaland. There were a few cases of partial nonresponse, but because the typical reason was that the question simply was not relevant to the respondent (as interpreted from the text comments in the questionnaire), this did not cause any particular action. Hence, the study proceeded under the assumption that the data were not characterised by nonresponse bias. Descriptive statistics of the sample are presented in Table 1 below.
Table 1.
Descriptive statistics of the sample.
| Manager type | Number of respondents |
|---|---|
| Care unit managers | 321 |
| Section managers | 46 |
| Department managers | 106 |
4.4. Data analysis
The interview data were analysed using qualitative content analysis (Graneheim & Lundman, 2004) to derive the overall barriers for staff pooling in a healthcare system. The analysis was conducted in four steps (see, Table 2). First, the interview transcriptions were read and re-read in order to generate familiarity with the content. Second, meaning units (usually sentences or paragraphs) corresponding to barriers for staff pooling in a healthcare system were selected using an inductive approach. Third, the meaning units were condensed as descriptions of barriers for staff pooling in a healthcare system and labelled with one of 22 codes. Fourth, six categories of barriers were identified in which the 22 codes were grouped.
Table 2.
Example of analysis of content, with grouping into a category.
| Meaning unit | Condensed content | Coding | Category |
|---|---|---|---|
| We have peaks here at our department in Mölndal, especially now in January, February and March when people slip and break their wrists (informant 1) | Predictable peaks in demand | Seasonality | Planning |
| I have divisions with permanent vacancies and a permanent lack of staff. In such a business, we do not really need a pool, but by more staff (informant 2) | To create a staff pool, excess capacity is needed but is often missing | No excess capacity |
The questionnaire data was initially analysed using a confirmatory factor analysis (CFA) to see if the category structure revealed in the content analysis could be confirmed (Hair et al., 2014). As it could not do so, a more exploratory approach was used instead to analyse these data. A principal component analysis (PCA) was used to determine the underlying factors (ibid.). SPSS version 25.0 with the AMOS plugin was used for all analyses. Finally, a two-way mixed analysis of variance (ANOVA) was conducted to investigate how the different manager types perceived the heights of the barrier types.
5. Results
5.1. Results from the interview study
The results from the content analysis in the descriptive study formed six categories of barriers for staff pooling, consisting of in total 22 items, where the categories of barriers were named after the common denominators of the items within that group:
Competence (5 items)
Geography (3 items)
Culture (5 items)
System (2 items)
Planning (2 items)
Recruitment (5 items)
5.2. Barriers related to competence
Department managers expressed competence category barriers in terms of insufficient competence, the time required to acquire competence, knowledge regarding practical differences between units, and lack of standardisation between units. In order to build efficient pools, the staff involved need to have sufficient competence to be able to work in several different units. A nurse who is a specialist in a particular field may need weeks or even months of training before he or she can work independently in another field, not only because of differences regarding healthcare-related issues but also because the work procedures may differ between units.
5.3. Barriers related to geography
Department managers expressed the geographical category barriers in terms of lack of trust and physical distance. Informants stressed that it may be difficult to have confidence in a staff pool that is supposed to cover a large geographical area and that ad hoc solutions, such as use of overtime and on-call staff, may be preferred instead of relying on the pool. The fact that units far apart in terms of physical distance constitute a pool means that travelling will be necessary, which may be expensive in terms of time as well as money.
5.4. Barriers related to culture
Department managers expressed the cultural category barriers in terms of cultural differences, lack of sense of community, differences in tradition, local IT-solutions incompatible with other IT-systems, and the willingness to be part of a pool. Different cultures among units or hospitals may lead to problems during the pooling process. A sense of community among actors may be a necessary condition in order to make a pooling approach operate smoothly. Ideas resembling a pooling approach have previously been used in some parts of the healthcare system, but self-reliance to solve problems has traditionally been strong. Differences in IT-solutions between units denotes that people may be unwilling to work in other units than their original one in order to avoid practical problems. Moreover, the general willingness among the staff to be part of a pool is unclear.
5.5. Barriers related to the system
Department managers expressed the system-related barriers in terms of unpredictable variation in supply and demand. The local availability of certain categories of staff varies significantly in some specialities, resulting in overstaffing during some periods and understaffing at other times. For example, in some clinics in a healthcare system, there might be a lack of physicians of a certain speciality and an excess of specialist nurses, while in other clinics at the same time there is a lack of nurses within the same speciality but an excess of physicians. This means that the capacity of the entire system can be sufficient, while capacity in separate parts of the system could experience shortage.
5.6. Barriers related to planning
Department managers expressed the barriers related to planning in terms of predictable variation in demand and in the fact that excess capacity is scarce or non-existent. Predictable seasonality in the demand for care is typical in some sectors; for example, orthopaedics departments in Sweden typically have many patients in winter who have slipped and broken their wrists. Since this type of variation is known, it should be part of the capacity planning process. Almost all informants stressed the fact that there is no excess capacity, at least not regarding nurses, and hence that recruitment is necessary.
5.7. Barriers related to recruitment
Department managers expressed the barriers related to recruitment in terms of bad collective agreement, wage competition, working conditions, shortage of nurses, and pay supplements. Some informants thought that differences between hospitals regarding collective agreements created recruitment problems for some. Wage competition from the private sector was also mentioned as a problem when trying to recruit healthcare staff. Other aspects of work, such as training, colleagues, and shift work, can also make recruitment difficult. Some informants opined that the general shortage of nurses in society should be addressed. Pay supplements for staff who accept working in a pool was also suggested as an incentive.
5.8. Results from the questionnaire
The results from the interview study were used to develop 22 questionnaire items that are presented in Table 3. The categories were not mentioned in the questionnaire. Table 4 presents descriptive statistics for the 22 questionnaire items, broken down by manager type. Note that the scales have been reversed for items 2, 3, 4, 5, 6, 9, 10 and 13, so that higher values generally correspond with negative conditions for staff pooling for all items. This is denoted in each case with an added “r” to the item name. Table 4 also presents the results for Brown-Forsythe ANOVA tests for equality of means among manager types within each item. As indicated in Table 4, items Competence1, Competence4r, Geography2 and Recruitment4 are characterised by significant differences in mean values among manager types. Post hoc tests based on Tamhane’s T2 were used in these cases to analyse the differences further. Department managers rated item Competence1 significantly lower than care unit managers did. In addition, department managers rated item Competence4r and Recruitment4 significantly lower than section managers and care unit managers did. Finally, section managers rated item Geography2 significantly lower than care unit managers did.
Table 3.
The 22 items used in the questionnaire.
| Factor | Item | Questionnaire statement |
|---|---|---|
| Competence | Competence1 | A longer training is necessary before new staff can work well on my unit |
| Competence2r | Nurses without specialist training can work well on my unit | |
| Competence3r | Physicians that are not yet specialists can work well on my unit | |
| Competence4r | The practical day-to-day work on my unit reminds to a large extent on the work in other units | |
| Competence5r | The work on my unit is characterised by a high degree of standardisation | |
| Geography | Geography1r | I would have confidence in a regional capacity pool |
| Geography2 | I would have greater confidence in a local than a regional capacity pool | |
| Geography3 | Larger geographical distances would obstruct the possibilities to create capacity pools in my type of unit | |
| Culture | Culture1r | There are no differences in culture between my unit and other similar units that would obstruct capacity pooling |
| Culture2r | There is a community view between my unit and other similar units that would facilitate capacity pooling | |
| Culture3 | Traditionally my unit and other similar units have not been cooperating with capacity | |
| Culture4 | Other similar units have different IT solutions than us | |
| Culture5r | I believe that my staff in general would be positive to be part of a capacity pool | |
| System | System1 | The daily availability of staff is varying to a large extent on my unit |
| System2 | Our patients are often transported to other units when my unit is full | |
| Planning | Planning1 | The variation of healthcare demand over time is to a large extent predictable at my unit |
| Planning2 | In general we do not have a shortage of staff at my unit | |
| Recruitment | Recruitment1 | Poor local agreements mean difficulties when recruiting staff to my unit |
| Recruitment2 | Competition regarding salary at other healthcare providers mean difficulties when recruiting staff to my unit | |
| Recruitment3 | Other factors besides salary are important aspects when recruiting staff to my unit | |
| Recruitment4 | There is a general shortage of nurses, which is a problem when recruiting staff to my unit | |
| Recruitment5r | I believe that there are mainly economic incentives that would be effective to recruit staff to a capacity pool |
Table 4.
Descriptive statistics.
| Item | Manager type | N | Mean | S.D. | 95% C.I. |
Brown-Forsythe |
||
|---|---|---|---|---|---|---|---|---|
| Lower B | Upper B | Statistic | p-value | |||||
| Competence1 | Care unit | 318 | 6.11 | 1.36 | 5.96 | 6.26 | ||
| Section | 39 | 5.51 | 1.59 | 5.00 | 6.03 | |||
| Department | 105 | 5.58 | 1.51 | 5.29 | 5.87 | |||
| Total | 462 | 5.94 | 1.43 | 5.81 | 6.07 | 6.35 | 0.002 | |
| Competence2r | Care unit | 261 | 3.02 | 2.21 | 2.75 | 3.29 | ||
| Section | 29 | 3.48 | 1.62 | 2.87 | 4.10 | |||
| Department | 97 | 3.01 | 2.00 | 2.61 | 3.41 | |||
| Total | 387 | 3.05 | 2.12 | 2.84 | 3.26 | 0.83 | 0.437 | |
| Competence3r | Care unit | 171 | 3.87 | 1.91 | 3.58 | 4.15 | ||
| Section | 43 | 3.93 | 1.72 | 3.40 | 4.46 | |||
| Department | 96 | 3.55 | 1.88 | 3.17 | 3.93 | |||
| Total | 310 | 3.78 | 1.88 | 3.57 | 3.99 | 1.09 | 0.340 | |
| Competence4r | Care unit | 287 | 4.23 | 2.03 | 3.99 | 4.47 | ||
| Section | 37 | 4.41 | 1.76 | 3.82 | 4.99 | |||
| Department | 97 | 3.47 | 2.05 | 3.06 | 3.89 | |||
| Total | 421 | 4.07 | 2.04 | 3.88 | 4.27 | 6.25 | 0.002 | |
| Competence5r | Care unit | 298 | 3.95 | 1.68 | 3.76 | 4.14 | ||
| Section | 41 | 3.98 | 1.37 | 3.54 | 4.41 | |||
| Department | 101 | 3.95 | 1.65 | 3.63 | 4.28 | |||
| Total | 440 | 3.95 | 1.64 | 3.80 | 4.11 | 0.01 | 0.995 | |
| Geography1r | Care unit | 262 | 4.19 | 1.84 | 3.96 | 4.41 | ||
| Section | 34 | 4.29 | 1.61 | 3.73 | 4.85 | |||
| Department | 94 | 4.09 | 1.70 | 3.74 | 4.43 | |||
| Total | 390 | 4.17 | 1.78 | 3.99 | 4.35 | 0.23 | 0.798 | |
| Geography2 | Care unit | 269 | 5.22 | 1.90 | 4.99 | 5.44 | ||
| Section | 33 | 4.33 | 1.74 | 3.71 | 4.95 | |||
| Department | 101 | 4.91 | 1.96 | 4.52 | 5.30 | |||
| Total | 403 | 5.07 | 1.91 | 4.88 | 5.25 | 3.81 | 0.024 | |
| Geography3 | Care unit | 250 | 4.86 | 2.09 | 4.60 | 5.12 | ||
| Section | 29 | 4.76 | 1.73 | 4.10 | 5.41 | |||
| Department | 88 | 5.08 | 1.92 | 4.67 | 5.49 | |||
| Total | 367 | 4.90 | 2.02 | 4.69 | 5.11 | 0.56 | 0.571 | |
| Culture1r | Care unit | 252 | 3.81 | 1.94 | 3.57 | 4.05 | ||
| Section | 35 | 4.23 | 1.57 | 3.69 | 4.77 | |||
| Department | 92 | 3.91 | 1.87 | 3.53 | 4.30 | |||
| Total | 379 | 3.87 | 1.89 | 3.68 | 4.06 | 0.91 | 0.406 | |
| Culture2r | Care unit | 246 | 3.76 | 1.73 | 3.54 | 3.98 | ||
| Section | 34 | 3.94 | 1.25 | 3.50 | 4.38 | |||
| Department | 89 | 3.54 | 1.54 | 3.22 | 3.86 | |||
| Total | 369 | 3.72 | 1.65 | 3.55 | 3.89 | 1.18 | 0.311 | |
| Culture3 | Care unit | 264 | 4.31 | 2.10 | 4.05 | 4.56 | ||
| Section | 36 | 4.39 | 1.98 | 3.72 | 5.06 | |||
| Department | 97 | 4.26 | 1.99 | 3.86 | 4.66 | |||
| Total | 397 | 4.30 | 2.06 | 4.10 | 4.51 | 0.06 | 0.943 | |
| Culture4 | Care unit | 230 | 2.85 | 2.12 | 2.58 | 3.13 | ||
| Section | 36 | 2.92 | 1.84 | 2.29 | 3.54 | |||
| Department | 88 | 2.92 | 2.29 | 2.44 | 3.41 | |||
| Total | 354 | 2.88 | 2.14 | 2.65 | 3.10 | 0.04 | 0.958 | |
| Culture5r | Care unit | 286 | 5.87 | 1.58 | 5.69 | 6.05 | ||
| Section | 37 | 5.84 | 1.39 | 5.38 | 6.30 | |||
| Department | 95 | 5.97 | 1.27 | 5.71 | 6.23 | |||
| Total | 418 | 5.89 | 1.49 | 5.75 | 6.03 | 0.21 | 0.811 | |
| System1 | Care unit | 307 | 3.34 | 1.86 | 3.13 | 3.54 | ||
| Section | 40 | 2.93 | 1.51 | 2.44 | 3.41 | |||
| Department | 105 | 3.35 | 1.75 | 3.01 | 3.69 | |||
| Total | 452 | 3.30 | 1.81 | 3.14 | 3.47 | 1.14 | 0.324 | |
| System2 | Care unit | 221 | 2.43 | 1.96 | 2.17 | 2.69 | ||
| Section | 39 | 2.74 | 2.07 | 2.07 | 3.42 | |||
| Department | 75 | 1.99 | 1.53 | 1.63 | 2.34 | |||
| Total | 335 | 2.37 | 1.90 | 2.16 | 2.57 | 2.49 | 0.087 | |
| Planning1 | Care unit | 288 | 3.94 | 1.97 | 3.71 | 4.17 | ||
| Section | 39 | 3.90 | 1.73 | 3.34 | 4.46 | |||
| Department | 101 | 4.13 | 1.72 | 3.79 | 4.47 | |||
| Total | 428 | 3.98 | 1.89 | 3.80 | 4.16 | 0.48 | 0.617 | |
| Planning2 | Care unit | 316 | 3.66 | 2.14 | 3.43 | 3.90 | ||
| Section | 40 | 3.10 | 1.95 | 2.48 | 3.72 | |||
| Department | 105 | 3.57 | 2.20 | 3.15 | 4.00 | |||
| Total | 461 | 3.59 | 2.14 | 3.40 | 3.79 | 1.32 | 0.27 | |
| Recruitment1 | Care unit | 282 | 3.78 | 2.09 | 3.54 | 4.03 | ||
| Section | 36 | 4.19 | 1.95 | 3.53 | 4.86 | |||
| Department | 94 | 3.43 | 2.02 | 3.01 | 3.84 | |||
| Total | 412 | 3.74 | 2.06 | 3.54 | 3.94 | 2.16 | 0.119 | |
| Recruitment2 | Care unit | 305 | 5.61 | 1.83 | 5.41 | 5.82 | ||
| Section | 40 | 5.58 | 1.62 | 5.06 | 6.09 | |||
| Department | 102 | 5.54 | 1.68 | 5.21 | 5.87 | |||
| Total | 447 | 5.59 | 1.78 | 5.43 | 5.76 | 0.08 | 0.926 | |
| Recruitment3 | Care unit | 315 | 5.57 | 1.47 | 5.41 | 5.73 | ||
| Section | 42 | 5.67 | 1.18 | 5.30 | 6.04 | |||
| Department | 104 | 5.77 | 1.19 | 5.54 | 6.00 | |||
| Total | 461 | 5.62 | 1.39 | 5.50 | 5.75 | 1.06 | 0.348 | |
| Recruitment4 | Care unit | 251 | 5.25 | 2.08 | 4.99 | 5.51 | ||
| Section | 25 | 5.88 | 1.45 | 5.28 | 6.48 | |||
| Department | 95 | 4.63 | 2.15 | 4.19 | 5.07 | |||
| Total | 371 | 5.13 | 2.08 | 4.92 | 5.35 | 6.08 | 0.003 | |
| Recruitment5r | Care unit | 260 | 5.54 | 1.58 | 5.35 | 5.73 | ||
| Section | 33 | 5.52 | 1.68 | 4.92 | 6.11 | |||
| Department | 90 | 5.29 | 1.74 | 4.93 | 5.65 | |||
| Total | 383 | 5.48 | 1.62 | 5.31 | 5.64 | 0.74 | 0.478 | |
Pearson’s correlations between item ratings can be found in Supplementary material Tables 1 and 2. Many pairs of item ratings exhibited substantial correlations, indicating that there might be a smaller number of common underlying factors. Hence, a CFA was performed to confirm the factor structure indicated by the content analysis. Because all respondents in the qualitative study were department managers, only questionnaire responses from department managers were used in the CFA.
The CFA showed that the data fitted the hypothesised factor structure poorly. A closer investigation of the data indicated that the bad reliability of the hypothetical constructs System and Planning, which include only two items each, is the main reason for this result. Hence, these four items were dropped. Instead, an explorative PCA was conducted on the remaining 18 items, again based on department manager responses only, using varimax rotation and Kaiser normalisation, in order to detect the common underlying factors. Bartlett’s test of sphericity was significant (p < 0.001), and the Kaiser-Meyer-Olkin measure of sampling adequacy was 0.589, indicating that the data were (barely) acceptable for a PCA. A solution where six factors had eigenvalues over Kaiser’s criterion of 1 was found, which in combination explained 60.2% of the variance. Table 5 shows the results in terms of factor loadings after rotation.
Table 5.
Factor loadings (PCA with 18 items).
| Item |
Factor |
|||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Competence4r | 0.82 | 0.04 | 0.14 | 0.02 | 0.02 | 0.01 |
| Competence2r | 0.64 | −0.20 | 0.04 | −0.05 | 0.33 | 0.11 |
| Competence3r | 0.64 | −0.07 | 0.01 | −0.19 | 0.05 | 0.11 |
| Competence5r | 0.61 | −0.03 | 0.48 | 0.03 | −0.04 | −0.17 |
| Geography1r | 0.49 | −0.01 | 0.29 | 0.43 | 0.10 | −0.33 |
| Recruitment1 | 0.05 | 0.82 | −0.03 | −0.05 | 0.17 | −0.02 |
| Recruitment2 | −0.03 | 0.81 | −0.14 | 0.10 | 0.06 | 0.09 |
| Recruitment4 | −0.18 | 0.72 | 0.04 | −0.10 | −0.14 | 0.08 |
| Culture1r | 0.04 | 0.00 | 0.84 | −0.04 | 0.00 | −0.04 |
| Culture2r | 0.22 | −0.12 | 0.77 | 0.12 | 0.04 | 0.02 |
| Geography3 | −0.09 | −0.08 | 0.04 | 0.73 | 0.13 | 0.04 |
| Culture5r | 0.14 | 0.16 | −0.05 | 0.70 | −0.04 | 0.03 |
| Geography2 | −0.30 | −0.13 | 0.06 | 0.63 | −0.05 | −0.02 |
| Competence1 | 0.20 | −0.11 | −0.19 | 0.14 | 0.70 | −0.05 |
| Culture4 | 0.17 | 0.13 | 0.21 | −0.14 | 0.67 | 0.18 |
| Recruitment3 | −0.23 | 0.32 | 0.07 | 0.15 | 0.49 | −0.21 |
| Culture3 | 0.15 | −0.05 | 0.15 | 0.01 | 0.12 | 0.79 |
| Recruitment5 | −0.09 | 0.22 | −0.24 | 0.04 | −0.12 | 0.64 |
| Cronbach’s α | 0.67 | 0.68 | 0.61 | 0.39 | 0.23 | 0.20 |
However, because the last three factors did not exhibit acceptable reliability measures, the items in these factors were removed from the dataset and an explorative PCA was conducted on the remaining 10 items, again using varimax rotation and Kaiser normalisation. Bartlett’s test of sphericity was still significant (p < 0.001), and the Kaiser-Meyer-Olkin measure of sampling adequacy increased to 0.691, indicating that the reduced data set was acceptable for a PCA. A solution where three factors had eigenvalues over Kaiser’s criterion of 1 was found, which in combination explained 61.0% of the variance. Table 6 shows the results in terms of factor loadings after rotation.
Table 6.
Factor loadings (PCA with 10 items).
| Item |
Factor |
||
|---|---|---|---|
| Community view | Recruitment difficulties | Specialisation | |
| Culture2r | 0.79 | −0.04 | 0.04 |
| Culture1r | 0.78 | 0.01 | −0.12 |
| Competence5r | 0.63 | 0.04 | 0.43 |
| Geography1r | 0.62 | −0.14 | 0.22 |
| Recruitment2 | −0.06 | 0.83 | −0.02 |
| Recruitment1 | 0.10 | 0.81 | 0.04 |
| Recruitment4 | −0.14 | 0.76 | −0.10 |
| Competence3r | −0.07 | 0.07 | 0.78 |
| Competence4r | 0.42 | 0.10 | 0.70 |
| Competence2r | 0.09 | −0.26 | 0.70 |
| Cronbach’s α | 0.66 | 0.68 | 0.65 |
The items that cluster on the same factor in Tables 5 and 6 indicate that Factor 1 represents community views; Factor 2, recruitment difficulties; and Factor 3, specialisation. Note that these factor names are chosen by the authors, based partly on what the items in each factor signify, and to show divergence from the factors that emerged from the interview study. These three factors exhibit tolerable values of Cronbach’s α indicating acceptable reliability (Hair et al., 2014). In summary, the results from the interview study did not coincide perfectly with the results from the qualitative content analysis, but several major factors, such as conceptual barriers for staff pooling in healthcare systems, were common.
Next, a two-way mixed ANOVA was conducted to investigate how the different manager types, namely 1) care unit managers, 2) section managers, and 3) department managers, perceived the heights of the three barrier types. Note that the barrier type is the within-subject factor (each respondent estimated the height of each barrier type) while the manager type is the between-subject factor (each respondent belongs to one of the three manager types) in this design.
The assumptions of the mixed ANOVA were met – the error variance of the dependent variable was not significantly unequal across groups (Levene’s test, p > 0.05 for all barrier types), and the covariance matrices of the dependent variables were not significantly unequal across groups (Box’s test, p = 0.373).
The descriptive results are displayed in Figure 3. See Supplementary materials Table 3 for details. The mixed ANOVA showed a significant between-subjects effect (F = 4.32, p = 0.014); hence, the different manager types perceived barrier heights in a significantly different way. A post-hoc-analysis conducted with Tukey HSD revealed that department managers perceived barrier heights as lower than the other two manager types did. In addition, there was a significant within-subjects effect (F = 33.89, p < 0.001); thus, the perceived heights of the three barriers were significantly different. A post-hoc-analysis conducted with Bonferroni correction revealed that the barrier type recruitment difficulties was perceived as significantly higher (average height 4.83) than barrier types community view and specialisation (average heights 3.95 and 3.66, respectively). Furthermore, the barrier type community view was perceived as significantly higher than the barrier type specialisation. Finally, there was no significant interaction between barrier type and manager type (F = 1.78, p = 0.170).
Figure 3.
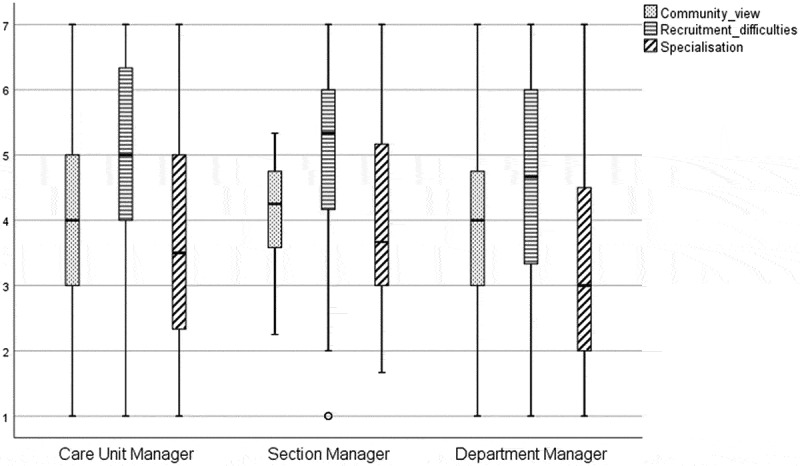
Results from mixed ANOVA.
Finally, the items that did not cluster reliably on common underlying factors and, hence, were excluded from the PCA, may of course still be of some interest in terms of potential barriers for staff pooling. They will be discussed further in the next section.
6. Discussion
The three barriers that could be identified in the PCA are similar but not identical to three of the barriers that were identified in the interview study; “recruitment difficulties” is similar to “recruitment”, “community view” is similar to “culture”, and “specialisation” is similar to “competence”. The factors and items that were excluded after the analysis might still be relevant in different parts of the healthcare system, although correlation with other items could not be proved. The literature that addresses the possibilities and barriers for staff pools in the healthcare system covers the three found barriers but concerns the pool of nurses or float pools solely (e.g., Adams et al., 2015; Cavouras, 2002; Dziuba-Ellis, 2006; Mazurenko et al., 2015).
Interestingly, the confirmation of any difference in priority of perceived barriers between different manager types could not be made, although the department managers were found to perceive the barriers lower compared to other manager types. This indicates that lower-level managers find the practical barriers more prominent than department managers. Since the different manager types are managing various professions at different levels of the organisation, it was expected that the manager types would perceive the presiding barriers of staff pooling differently from one another. Our results might instead indicate that the identified barriers are relevant to all manager types regardless of organisational belonging and profession and that it is of importance for all manager types to address these barriers, and thereby ease the implementation of staff pools.
Of the three barrier types, barriers related to recruitment difficulties were perceived highest, followed by barriers related to community view. This indicates that in order to efficiently implement a staff pooling approach, efforts should be prioritised to form incentives for employees to work in a staff pool (Bates, 2013; Cavouras, 2002; Dziuba-Ellis, 2006; Larson et al., 2012; Lebanik & Britt, 2015). Another solution might be to investigate if pooling could be a speciality in itself, and thereby create career incentives for healthcare employees to be recruited to a staff pool.
6.1. Barriers related to recruitment difficulties
Two items from the interview study were excluded from the barrier related to recruitment after the analysis, namely “Other factors besides salary are important aspects when recruiting staff to my unit” and “I believe that there are mainly economic incentives that would be effective to recruit staff to a staff pool”. These statements are concerned with the importance of economic incentives when recruiting staff to both the own unit and the staff pool. Although these items could not be confirmed in the PCA, they might still be of importance to consider when implementing a staff pool. Nevertheless, barriers related to recruitment difficulties were found to be significantly higher than barriers related to community view and specialisation.
According to department managers, the lack of nurses is one of the main barriers related to recruitment. This shortage is no new phenomenon; in the early 2000s, the use of internal staffing pools was declining in American hospitals due to difficulties in recruiting qualified staff to the pools or due to pool staff leaving for permanent work in clinical units (Cavouras, 2002). The inability to staff the pool leads to inadequate service levels, that is, the inability to fill in gaps in staff schedule due to sick leaves, temporary leaves, and vacancies. Therefore, recruitment and retention of qualified staff are the main challenges for staff pool managers for the pool to be a reliable facility in the healthcare system. Pay supplements, scheduling flexibility, independence, skill development, and networking are widely used incentives for attracting staff to work in staffing pools (Bates, 2013; Cavouras, 2002; Dziuba-Ellis, 2006; Larson et al., 2012; Lebanik & Britt, 2015).
6.2. Barriers related to community view
In the barriers related to culture, the informants claimed that there is a low willingness to be part of a staff pool and that similar units in general do not cooperate with capacity. Moreover, they claimed that different IT solutions are a barrier to using staff pools. However, it could not be confirmed in the factor analysis that this correlates with the other items related to culture, which was unsurprising, and a new barrier was identified as “community view”. Two new items were added to the barrier, namely “I would have confidence in a regional staff pool” and “The work on my unit is characterised by a high degree of standardisation”, which is logical considering that staff pools that are further away in the organisational structure will perceive culture differently, and since standardisation is of importance for the sense of belonging in a community.
The interviewees claimed that there could be a lack of sense of community between the own unit and a staff pool. Several studies indicate a higher job satisfaction and organisational loyalty among permanent nurses compared to temporary agency staff (Mazurenko et al., 2015; Rudy & Sions, 2003). Temporary agency staff typically experience a higher level of frustration, anxiety, occupational stress, and burnout due to inadequate orientation, lack of trust from unit-based staff, and insufficient support from clinical unit management (ibid.). In a clinical unit that uses temporary agency staff to a greater extent, there are also more permanent employees who consider leaving the unit (Bates, 2013; Mazurenko et al., 2015; Rudy & Sions, 2003). According to Diaz et al. (2010), many staffing pool solutions have aggravated staff shortages. Moreover, Song et al. (2015) showed that length of stay increased in an emergency department where physicians were pooled, which might have been because employee behaviour affects performance. According to Bates (2013), one can avoid this by staffing the pool with independent and flexible individuals that enjoy the independence and the variety of challenge and experiences that rotating between multiple clinical units entails. As mentioned above, another important way of making rotations a positive experience is appropriate unit orientation and dedicated pool staff support on the receiving units (Roach et al., 2011; Rudy & Sions, 2003).
6.3. Barriers related to specialisation
A crucial barrier to staff pooling is the category of specialisation in terms of inadequate professional competence and knowledge regarding practical differences between units (i.e., lack of standardised way of working). This barrier was similar to the barrier that was identified as “competence” in the interview study, with the difference that the items “A more extended training is necessary before new staff can work well on my unit” and “The work on my unit is characterised by a high degree of standardisation” were excluded. This similarity could be due to the questionnaire being sent to department managers in both primary care centres and speciality units, whereas the interview study mainly focused on speciality department managers at a university hospital.
The literature in this area is primarily directed towards practical issues. Concerning professional competence, pool staff can either be acting as temporary assistance to unit-based staff or as replacement staff with full patient assessments (Dziuba-Ellis, 2006). In the first case, no specialist competence is required, which facilitates pooling because more clinical units can be considered together. In the second case, specialist competence is required to ensure patient safety and a good working environment, which limits the potential of pooling to pools with cross-trained professionals rotating between different units that require quite similar types of skills (see, e.g., Inman et al., 2005). Song et al. (2020) argue that nursing specialisation seem to have limited effect on length of stay in healthcare pooling systems. For example, recently, efforts were made in order to overcome barriers related to specialisation is the allocation of capacity during the COVID-19 pandemic in Region Västra Götaland. Physicians, nurses, and assistant nurses from multiple specialities received a two day-training programme in order to work at the intensive care units (ICU). These physicians, nurses, and assistant nurses worked in teams to support regular employees at the ICUs during a limited period of time (Sahlgrenskaliv.se, 2020).
Adams et al. (2015) have addressed the problem of temporary agency nurses’ lack of familiarity with organisational policies and procedures. The authors also note that the lack of standardisation of, for example, nursing practice, unit routines, documentation, and patient equipment make it more difficult for pool staff (i.e., nurses) to rotate between different clinical units in a healthcare system. Bates (2013) and Rudy and Sions (2003) describe situations where staff spend much time searching for supplies, asking for codes to locked rooms, and requesting assistance with unit-specific procedures. KC et al. (2020) note that healthcare staff often work under prerequisites with unclear standards, and that employees’ behaviour will contribute to a gap between existing standards and medical outcomes. In order to avoid such barriers, it is vital to train pool staff to work on multiple units in the healthcare system (so-called orientation programmes), and to standardise practice, routines, equipment, among others within the clinical units in the healthcare system (Adams et al., 2015; Roach et al., 2011). According to Agosto et al. (2017), it is crucial to shift from a unit-based to a system-based model of education and practice. In this process, the float pool unit may be an important participant when standardising practice and routines due to their experience from multiple units (Straw, 2018). In addition, developing unit-specific pocket guides or tip sheets and ensuring adequate pool staff support on the receiving unit are useful tools to reduce these practical barriers (Bates, 2013; Roach et al., 2011). However, implementing appropriate orientation programmes and pool staff support may, in many cases, be difficult due to resource shortages (Roach et al., 2011).
6.4. Barriers that could not be confirmed
The items related to the barriers “geography”, “system”, and “planning”, to a large extent, vary depending on the characteristics of the specific unit. Since the questionnaire was sent to managers in both primary care centres and speciality departments, it is not surprising that these factors could not be confirmed in the CFA. However, they could still be relevant for defined parts of the system, for instance, the speciality department managers at larger hospitals.
Although barriers related to geography could not be confirmed, department managers expressed a lack of trust in a staff pool that is supposed to cover a large geographical area. Trust is generally an essential factor when integrating staffing pools in healthcare systems. According to Mazurenko et al. (2015), trust must be built from top to bottom through, for example, effective communication between the staffing pools and the units where the pool staff will be working, and a complete orientation programme to the units on which the pool staff are assigned to work. Staff pools should preferably be organised close to the clinics to reduce time wastage when travelling between facilities. According to Song et al. (2020), digital solutions should be examined as a tool to overcome physical distance in healthcare departments where applicable. For example, Region Västra Götaland recently implemented a psychiatric unit where advanced video and sound technologies are used to create an e-visit resembling a physical meeting (Sahlgrenska Universitetssjukhuset, 2021). Song et al. (2020) further found that, in a patient pooling system, the physical distance contributed to a longer length of stay and higher readmission rate, while mismatch in nursing specialisation did not. Although the results were found in a patient pooling system, it could be argued that the same logic applies in a staff pooling system.
The category barriers related to the system are expressed by department managers in terms of high local variations of the availability of certain categories of staff, resulting in overstaffing during some periods and understaffing at other times. According to Dziuba-Ellis (2006), internal staff pools on an appropriate level in the healthcare system can be a useful approach to balancing understaffed and overstaffed clinical units. Today, a widely used approach to aid understaffed clinical units is to hire costly staff from external staffing pools (Larson et al., 2012).
The barriers related to planning are emphasised by department managers through the fact that excess capacity is more or less non-existent while excess capacity is theoretically required at an aggregate level in order to plan a staff pool. In the literature, on the contrary, internal staffing pools are emphasised as an approach to balance the effect of insufficient staffing levels (i.e., lack of basic capacity) and budget constraints (Dziuba-Ellis, 2006; Linzer et al., 2011; Roach et al., 2011). According to Roach et al. (2011), staffing pools are a short-term measure to ensure adequate staffing in clinical units on an “as-needed basis” to fill gaps in staff schedule due to sick leaves, temporary leaves, and vacancies. Staffing pools can also be a tool for reducing overtime and the cost of external agency staff to maintain minimum nurse-to-patient staffing requirements, to improve work environment, and to create flexibility in staffing planning (Hultberg, 2007; Kuntz et al., 2015; Larson et al., 2012; Lebanik & Britt, 2015; Lu & Lu, 2017; Mahar et al., 2011; Noon et al., 2003).
7. Conclusion and future research
This empirical study, through a mixed-methods approach with data from a multihospital system, identified three different categories of potential barriers for staff pooling in a healthcare system: barriers related to recruitment difficulties, community view, and specialisation. One of the barriers were found to be of greater importance, namely those related to recruitment difficulties, followed by community view. Difference in priority of perceived barrier heights between manager types could not be confirmed, although department managers found barrier heights lower, which indicates an ease in implementation of staff pools. Previous literature has, to a large extent, been anecdotal, directed towards nurses, and focused on single hospital settings and nursing homes. The findings in this study can be used to systematically implement a staff pooling approach on a multihospital system with all types of healthcare professionals and healthcare facilities. A holistic view of resource allocation in healthcare settings has been solicited for many years (Keskinocak & Savva, 2020; Smith-Daniels et al., 1988) and the topic of temporary capacity change has recently in this journal been identified as a direction for future research (Leeftink et al., 2020). To our knowledge, this is the first study that analyses the possibilities for a staff pooling system as a proactive tool to manage variations in a healthcare setting, using a holistic approach with all healthcare professions in a healthcare system.
This study has been limited to barriers in using staff pools consisting of staff in healthcare settings. Hence, there are most likely other potential barriers to be found in other pooling systems, such as patient pooling and resource (other than staff) pooling. Similarly, barriers found in other pooling systems that have been described in previous studies, such as increased length of stay in patient pooling systems, were not expressed by the managers in this study. Moreover, the study has been performed in a Swedish healthcare context. However, the identified barriers to using staff pools have been found and described in international literature and are, therefore, not considered to be specific and limited to a Swedish healthcare context. Finally, one might think that the fact that the respondents in the initial qualitative study were department managers, while the questionnaire was submitted to managers on department, section, and care unit level could indicate some issues with external validity. However, the department managers were asked during the interviews to view our questions from a holistic departmental perspective rather than just from their positions as department managers. In addition, our analyses showed that the different manager types prioritised the different barrier types equally. Therefore, we do not believe that the difference in manager composition between the two studies matters.
There are several managerial implications from this study. Firstly, we could not find differences in priority of barrier types between management types, which helps in the implementation of staff pools. Secondly, to introduce staff pooling successfully in a healthcare system, the identified barriers need to be addressed by both managers of the units that utilise the staff pool as well as managers of that specific pool. For example, standardisation of routines and procedures, proper introduction programmes, and suitable tasks for the staff pool employees can be identified to overcome some of these barriers. Ideally, all identified barriers can be overcome and sufficiently managed when implementing staff pools in healthcare systems. However, if all three barriers cannot be addressed for various reasons, the focus should primarily be upon the two barriers that were found in this study to be significantly higher, namely the barriers related to recruitment difficulties and community view. The barriers related to recruitment difficulties indicate that incentives to work in a staff pool must be identified so that the staff pools can be sufficiently staffed. The barriers related to community view indicate that staff pools should be staffed with flexible individuals that enjoy independence and variety of challenges. Finally, it could be investigated if pooling should be a speciality in itself in order to overcome barriers related to recruitment difficulties.
Furthermore, this study contributes to several implications for future research. Firstly, there is a need for future research to fully understand the identified barriers, and further studies are required to determine the staff pools’ optimal size, the competencies that should be included, where these staff pools should be located in the organisation, and how they should be managed for the most efficient use of resources. Such studies could contribute to what Keskinocak and Savva (2020) identify as an opportunity for future research, namely a holistic approach to an otherwise fragmented system, which can create opportunities for optimised resource allocation. Secondly, previous experience from the COVID-19 pandemic, where staff was reallocated within hospital systems to create an increased number of ICU beds, could be used to better understand the effects of staff pooling. Thirdly, in order to provide more general guidelines on staff pooling, future research should holistically explore how the characteristics of different speciality departments or other organisational units are related to different barriers. A possible way to accomplish this could be to use multiple regression with the perceived weights of the different barriers as dependent variables, and unit characteristics as explanatory variables. In this way, measures of the different barriers’ significance in different system contexts could be obtained. Fourthly, this study considered only staff pools, but a pooling system could consist of multiple types of pools such as staff, patient, and resource. Future research could explore how such a system could be composed to optimise the capacity use in healthcare systems. Finally, KC et al. (2020) specify digitalisation and connected health as an exciting area for future research, and hence, potential benefits with digital solutions in a staff pooling approach should be further researched.
Supplementary Material
Appendix A. Supplementary material
Table A1.
Correlations part 1.
| Competence2r | Competence3r | Competence4r | Competence5r | Geography1r | Geography2 | Geography3 | Culture1r | Culture2r | Culture3 | Culture4 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Competence1 | 0.17 | 0.08 | 0.05 | −0.08 | 0.10 | 0.07 | 0.09 | −0.01 | 0.01 | −0.04 | 0.17 |
| Competence2r | 0.48 | 0.31 | 0.16 | 0.14 | −0.14 | 0.05 | 0.08 | 0.07 | 0.07 | 0.21 | |
| Competence3r | 0.39 | 0.24 | 0.03 | −0.13 | −0.07 | 0.03 | 0.09 | 0.04 | 0.23 | ||
| Competence4r | 0.42 | 0.29 | −0.15 | 0.00 | 0.18 | 0.30 | 0.10 | 0.21 | |||
| Competence5r | 0.26 | −0.13 | −0.05 | 0.20 | 0.32 | −0.02 | 0.12 | ||||
| Geography1r | −0.05 | 0.18 | 0.24 | 0.43 | −0.10 | 0.17 | |||||
| Geography2 | 0.28 | −0.04 | −0.09 | −0.03 | −0.13 | ||||||
| Geography3 | 0.07 | 0.06 | 0.04 | 0.04 | |||||||
| Culture1r | 0.45 | −0.01 | 0.10 | ||||||||
| Culture2r | 0.18 | 0.13 | |||||||||
| Culture3 | 0.11 | ||||||||||
| Culture4 | |||||||||||
| Culture5r | |||||||||||
| System1 | |||||||||||
| System2 | |||||||||||
| Planning1 | |||||||||||
| Planning2 | |||||||||||
| Recruitment1 | |||||||||||
| Recruitment2 | |||||||||||
| Recruitment3 | |||||||||||
| Recruitment4 |
Table A2.
Correlations part 2.
| Culture5r | System1 | System2 | Planning1 | Planning2 | Recruitment1 | Recruitment2 | Recruitment3 | Recruitment4 | Recruitment5r | |
|---|---|---|---|---|---|---|---|---|---|---|
| Competence1 | 0.11 | 0.06 | −0.03 | −0.01 | −0.02 | −0.01 | 0.03 | 0.10 | 0.03 | −0.09 |
| Competence2r | 0.02 | −0.19 | −0.11 | 0.00 | −0.02 | −0.05 | −0.10 | −0.09 | −0.17 | 0.04 |
| Competence3r | −0.04 | −0.11 | −0.08 | −0.03 | 0.01 | −0.01 | −0.01 | −0.04 | −0.03 | 0.06 |
| Competence4r | 0.11 | −0.04 | −0.06 | −0.09 | −0.02 | 0.06 | −0.07 | −0.04 | −0.13 | 0.05 |
| Competence5r | 0.04 | −0.02 | −0.07 | −0.12 | 0.08 | 0.00 | −0.04 | −0.09 | −0.10 | 0.09 |
| Geography1r | 0.28 | −0.09 | 0.02 | −0.09 | 0.08 | −0.05 | −0.13 | −0.01 | −0.19 | 0.18 |
| Geography2 | −0.01 | 0.03 | 0.12 | −0.05 | 0.06 | 0.01 | 0.07 | 0.04 | 0.10 | −0.16 |
| Geography3 | 0.19 | 0.06 | −0.02 | 0.02 | −0.10 | 0.01 | 0.04 | 0.07 | 0.04 | 0.00 |
| Culture1r | −0.01 | −0.01 | −0.04 | −0.06 | 0.00 | −0.01 | −0.08 | 0.03 | −0.08 | 0.08 |
| Culture2r | 0.19 | 0.10 | −0.06 | −0.05 | 0.07 | 0.04 | −0.07 | −0.02 | −0.01 | 0.14 |
| Culture3 | 0.06 | 0.06 | 0.00 | 0.01 | −0.03 | 0.04 | 0.03 | 0.02 | 0.04 | −0.11 |
| Culture4 | 0.05 | 0.07 | 0.08 | −0.09 | −0.03 | 0.04 | 0.03 | 0.04 | 0.06 | −0.06 |
| Culture5r | −0.04 | −0.06 | −0.02 | 0.07 | −0.07 | 0.11 | 0.10 | 0.03 | 0.01 | |
| System1 | 0.15 | −0.05 | −0.19 | 0.17 | 0.06 | 0.05 | 0.22 | −0.08 | ||
| System2 | −0.20 | −0.13 | 0.23 | 0.17 | 0.00 | 0.21 | −0.12 | |||
| Planning1 | 0.01 | −0.04 | 0.01 | −0.03 | 0.01 | 0.02 | ||||
| Planning2 | −0.21 | −0.15 | −0.05 | −0.33 | 0.03 | |||||
| Recruitment1 | 0.47 | 0.10 | 0.40 | −0.19 | ||||||
| Recruitment2 | 0.22 | 0.42 | −0.27 | |||||||
| Recruitment3 | 0.17 | −0.04 | ||||||||
| Recruitment4 | −0.21 |
Table A3.
Descriptive results from mixed ANOVA.
| Barrier type | Manager type | Mean | S.D. | n | 95 % C.I. |
|---|---|---|---|---|---|
| Community view | Care unit managers | 3.94 | 1.32 | 297 | 3.79–4.09 |
| Section managers | 4.14 | 0.79 | 39 | 3.89–4.40 | |
| Department managers | 3.91 | 1.28 | 102 | 3.66–4.16 | |
| Total | 3.95 | 1.27 | 438 | 3.83–4.07 | |
| Recruitment difficulties | Care unit managers | 4.90 | 1.62 | 297 | 4.72–5.09 |
| Section managers | 4.97 | 1.65 | 39 | 4.44–5.50 | |
| Department managers | 4.58 | 1.57 | 102 | 4.27–4.89 | |
| Total | 4.83 | 1.62 | 438 | 4.68–4.99 | |
| Specialisation | Care unit managers | 3.72 | 1.72 | 297 | 3.52–3.91 |
| Section managers | 4.03 | 1.34 | 39 | 3.60–4.47 | |
| Department managers | 3.34 | 1.56 | 102 | 3.03–3.65 | |
| Total | 3.66 | 1.66 | 438 | 3.50–3.81 |
Funding Statement
This work was supported by the Jan Wallanders och Tom Hedelius Stiftelse samt Tore Browaldhs Stiftelse [P2017-0052:1].
Note
This article is an extended and further developed version of a previous conference paper presented by the authors at the NOFOMA 2019 conference in Oslo, Norway
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/20476965.2022.2108729
References
- Adams, J., Kaplow, R., Dominy, J., & Stroud, B. (2015). Beyond a band-aid approach: an internal agency solution to nurse staffing. Nursing Economics, 33(1), 51–58. https://pubmed.ncbi.nlm.nih.gov/26214939/ [PubMed] [Google Scholar]
- Agosto, P., Cieplinski, J. A., Monforto, K., Griffin, M. D., Roberts, K. E., Tracy, E., & Hickerson, K. A. (2017). The central staffing office intensive care nurse residency program: a pilot program. Nursing Economics, 35(3), 147–150. http://www.nursingeconomics.net/necfiles/2017/MJ17/147.pdf [Google Scholar]
- Alvekrans, A. L., Lantz, B., Rosén, P., Siljemyr, L., & Snygg, J. (2016). From knowledge to decision – A case study of sales and operations planning in health care. Production Planning & Control, 27(12), 1019–1026. 10.1080/09537287.2016.1174892 [DOI] [Google Scholar]
- Ata B and Van Mieghem J A. (2009). The Value of Partial Resource Pooling: Should a Service Network Be Integrated or Product-Focused?. Management Science, 55(1), 115–131. 10.1287/mnsc.1080.0918 [DOI] [Google Scholar]
- Bacelar-Silva, G. M., Cox, J. F., III, & Rodrigues, P. P. (2022). Outcomes of managing healthcare services using the Theory of Constraints: A systematic review. Health Systems, 11(1), 1–16. 10.1080/20476965.2020.1813056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagust, A., Place, M., & Posnett, J. W. (1999). Dynamics of bed use in accommodating emergency admissions: Stochastic simulation model. BMJ, 319(7203), 155–158. 10.1136/bmj.319.7203.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bard, J. F., & Purnomo, H. W. (2005). Short-term nurse scheduling in response to daily fluctuations in supply and demand. Health Care Management Science, 8(4), 315–324. 10.1007/s10729-005-4141-9 [DOI] [PubMed] [Google Scholar]
- Bates, K. J. (2013). Floating as a reality: helping nursing staff keep their heads above water. MEDSURG Nursing, 22(3), 197–199. https://pubmed.ncbi.nlm.nih.gov/23865282/ [PubMed] [Google Scholar]
- Best, T. J., Sandıkçı, B., Eisenstein, D. D., & Meltzer, D. O. (2015). Managing hospital inpatient bed capacity through partitioning care into focused wings. Manufacturing & Service Operations Management, 17(2), 157–176. 10.1287/msom.2014.0516 [DOI] [Google Scholar]
- Boudreau, J., Hopp, W., McClain, J. O., & Thomas, L. J. (2003). On the interface between operations and human resources management. Manufacturing & Service Operations Management, 5(3), 179–202. 10.1287/msom.5.3.179.16032 [DOI] [Google Scholar]
- Brailsford, S., Bayer, S., Connell, C., George, A., Klein, J., & Lacey, P. (2021). Embedding OR modelling as decision support in health capacity planning: Insights from an evaluation. Health Systems, 1–14. 10.1080/20476965.2021.1983476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt, J., & Palmgren, M. (2015). Produktionsstyrning i sjukvård. Stockholm:Lyxo. [Google Scholar]
- Businessinsider.se . Converted operating rooms and shuffled patients: How NYC scrambled to turn 1,600 ICU beds into 3,500 to care for the sickest coronavirus patients. Accessed November 18, 2020. https://www.businessinsider.com/coronavirus-nyc-more-than-doubled-its-icu-capacity-in-weeks-2020-4?r=US&IR=T
- Cattani, K., & Schmidt, G. M. (2005). The pooling principle. INFORMS Transactions on Education, 5(2), 17–24. 10.1287/ited.5.2.17 [DOI] [Google Scholar]
- Cavouras, C. A. (2002). Nurse staffing levels in American hospitals: A 2001 report. Journal of Emergency Nursing, 28(1), 40–43. 10.1067/men.2002.121871 [DOI] [PubMed] [Google Scholar]
- Corsini, R. R., Costa, A., Fichera, S., & Pluchino, A. (2022). A configurable computer simulation model for reducing patient waiting time in oncology departments. Health Systems, 1–15. 10.1080/20476965.2022.2030655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin, A. M., van Rossum, A. C., Visser, M. C., & Koole, G. M. (2007). Modeling the emergency cardiac in-patient flow: An application of queueing theory. Health Care Management Science, 10(2), 125–137. 10.1007/s10729-007-9009-8 [DOI] [PubMed] [Google Scholar]
- Diaz, D. M., Erkoc, M., Asfour, S. S., & Baker, E. K. (2010). New ways of thinking about nurse scheduling. Journal of Advances in Management Research, 7(1), 76–93. 10.1108/09727981011042865 [DOI] [Google Scholar]
- Donohue, K., Özer, Ö., & Zheng, Y. (2020). Behavioral operations: past, present, and future. Manufacturing & Service Operations Management, 22(1), 191–202. 10.1287/msom.2019.0828 [DOI] [Google Scholar]
- Dziuba-Ellis, J. (2006). Float pools and resource teams – a review of the literature. Journal of Nurse Care Quality, 21(4), 352–359. 10.1097/00001786-200610000-00013 [DOI] [PubMed] [Google Scholar]
- Faeghi, S., Lennerts, K., & Nickel, S. (2021). Strategic planning of operating room session allocation using stability analysis. Health Systems, 1–14. 10.1080/20476965.2021.1997651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagefors, C., Lantz, B., & Rosén, P. (2020). Creating short-term volume flexibility in healthcare capacity management. Int. J. Environ. Res. Public Health, 17(22), 8514. 10.3390/ijerph17228514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim, U. H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- Gutjahr, W. J., & Rauner, M. S. (2007). An ACO algorithm for a dynamic regional nurse-scheduling problem in Austria. Computers & Operations Research, 34(3), 642–666. 10.1016/j.cor.2005.03.018 [DOI] [Google Scholar]
- Hair, J. F., Black, W. C., Babin, B. J., & Anderson, R. E. (2014). Multivariate data analysis. Pearson Education. [Google Scholar]
- Hopp, W. J., & Lovejoy, W. S. (2013). Hospital operations: principles of high efficiency health care. Pearson Educations Inc. [Google Scholar]
- Hultberg, A. (2007). Ett hälsosammare arbetsliv - Vägledning för goda psykosociala arbetsförhållanden. Socialmedicinsk tidskrift, 84(2), 114–122. https://socialmedicinsktidskrift.se/index.php/smt/article/view/613 [Google Scholar]
- Inman, R. R., Blumenfeld, D. E., & Ko, A. (2005). Cross-Training Hospital Nurses to Reduce Staffing Costs. Health Care Manage. Rev, 30(2), 116–125. 10.1097/00004010-200504000-00006 [DOI] [PubMed] [Google Scholar]
- Kadri, U. (2021). Variation of quantified infection rates of mixed samples to enhance rapid testing during an epidemic. Health Systems, 10(1), 24–30. 10.1080/20476965.2020.1817801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- KC, D. S., Scholtes, S., & Terwiesch, C. (2020). Empirical research in healthcare operations: past research, present understanding, and future opportunities. Manufacturing & Service Operations Management, 22(1), 73–83. 10.1287/msom.2019.0826 [DOI] [Google Scholar]
- Kc, D. S., & Terwiesch, C. (2009). Impact of workload on service time and patient safety: an econometric analysis of hospital operations. Management Science, 55(9), 1486–1498. 10.1287/mnsc.1090.1037 [DOI] [Google Scholar]
- Keskinocak, P., & Savva, N. (2020). A review of the healthcare-management (modeling) literature published in manufacturing & service operations management. Manufacturing & Service Operations Management, 22(1), 59–72. 10.1287/msom.2019.0817 [DOI] [Google Scholar]
- Kuntz, L., Mennicken, R., & Scholtes, S. (2015). Stress on the ward: evidence of safety tipping points in hospital. Management Science, 61(4), 754–771. 10.1287/mnsc.2014.1917 [DOI] [Google Scholar]
- Lamé, G., Crowe, S., & Barclay, M. (2022). “What’s the evidence?” - Towards more empirical evaluations of the impact of OR interventions in healthcare. Health Systems, 11(1), 59–67. 10.1080/20476965.2020.1857663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson, N., Sendelbach, S., Missal, B., Fliss, J., & Gaillard, P. (2012). Staffing patterns of scheduled unit staff nurses vs float pool nurses: a pilot study. MEDSURG Nursing, 21(1), 27–39. https://pubmed.ncbi.nlm.nih.gov/22479872/ [PubMed] [Google Scholar]
- Lebanik, L., & Britt, S. (2015). Float pool nurses come to the rescue. Nursing, 45(3), 50–53. 10.1097/01.NURSE.0000460715.73128.ea [DOI] [PubMed] [Google Scholar]
- Leeftink, A. G., Bikker, A., Vliegen, I. M. H., & Boucherie, R. J. (2020). Multi-disciplinary planning in health care: A review. Health Systems, 9(2), 95–118. 10.1080/20476965.2018.1436909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linzer, P., Tilley, A. M., & Williamson, M. V. (2011). What floats a float nurse´s boat? Creative Nursing, 17(3), 130–138. 10.1891/1078-4535.17.3.130 [DOI] [PubMed] [Google Scholar]
- Lu, S. F., & Lu, L. X. (2017). Do mandatory overtime laws improve quality? staffing decisions and operational flexibility of nursing homes. Management Science, 63(11), 3566–3585. 10.1287/mnsc.2016.2523 [DOI] [Google Scholar]
- Lupien, S. J., Maheu, F., Tu, M., Fiocco, A., & Schramek, T. E. (2007). The effects of stress and stress hormones on human cognition: Implications for the field of brain and cognition. Brain and Cognition, 65(3), 209–237. 10.1016/j.bandc.2007.02.007 [DOI] [PubMed] [Google Scholar]
- Mahar, S., Bretthauer, K. M., & Salzarulo, P. A. (2011). Locating specialized service capacity in a multi-hospital network. European Journal of Operational Research, 212(3), 596–605. 10.1016/j.ejor.2011.03.008 [DOI] [Google Scholar]
- Mazurenko, O., Liu, D., & Perma, C. (2015). Patient care outcomes and temporary nurses. Nursing Management, 46(8), 32–38. 10.1097/01.NUMA.0000469351.33893.61 [DOI] [PubMed] [Google Scholar]
- Morgan, D. L. (1998). Practical strategies for combining qualitative and quantitative methods: applications to health research. Qualitative Health Research, 8(3), 362–376. 10.1177/104973239800800307 [DOI] [PubMed] [Google Scholar]
- Noon, C. E., Hankins, C. T., & Côté, M. J. (2003). Understanding the impact of variation in the delivery of healthcare services. Journal of Healthcare Management, 48(2), 82–98. 10.1097/00115514-200303000-00004 [DOI] [PubMed] [Google Scholar]
- Proudlove, N. C., & Proudlove NC . (2020). The 85% bed occupancy fallacy: The use, misuse and insights of queueing theory. Health Services Management Research, 33(3), 110–121. 10.1177/0951484819870936 [DOI] [PubMed] [Google Scholar]
- Roach, J. A., Tremblay, L. M., & Carter, J. (2011). Hope floats – an orthopaedic tip sheet for float pool nurses. Orthopaedic Nursing, 30(3), 208–212. 10.1097/NOR.0b013e318219aebc [DOI] [PubMed] [Google Scholar]
- Rowse, E. L., Harper, P. R., Williams, J. E., & Smithies, M. (2013). Optimising the use of resources within the district nursing service: A case study. Health Systems, 2(1), 43–52. 10.1057/hs.2012.22 [DOI] [Google Scholar]
- Rudy, S., & Sions, J. (2003). Floating: Managing a Recruitment and Retention Issue. Journal of Nursing Administration, 33(4), 196–198. 10.1097/00005110-200304000-00002 [DOI] [PubMed] [Google Scholar]
- Sahlgrenska Universitetssjukhuset. Nya arbetssätt inom psykiatrin bidrar till mer jämlik vård i regionen. Sahlgrenska Universitetssjukhusets presstjänst. Accessed November 15, 2021. https://www.pressmachine.se/pressrelease/view/nya-arbetssatt-inom-psykiatrin-bidrar-till-mer-jamlik-vard-i-regionen-32063
- Sahlgrenskaliv.se . Uppdrag: Bemanna covid-IVA. Accessed September 28, 2020. https://sahlgrenskaliv.se/sa-bemannades-covid-iva/
- SKL . 2017. Gemensamma tag för att uppnå oberoende av inhyrd personal. Startsida, Accessed October 12, 2020. https://skl.se/arbetsgivarekollektivavtal/personalochkompetensforsorjning/halsoochsjukvard/inhyrdpersonal.11422.html
- Smith-Daniels, V. L., Schweikhart, S. B., & Smith-Daniels, D. E. (1988). Capacity management in health care services: review and future research directions. Decisions Science, 19(4), 889–919. 10.1111/j.1540-5915.1988.tb00310.x [DOI] [Google Scholar]
- Song, H., Tucker, A. L., Graue, R., Moravick, S., & Yang, J. J. (2020). Capacity pooling in hospitals: the hidden consequences of off-service placement. Management Science, 66(9), 3825–3842. 10.1287/mnsc.2019.3395 [DOI] [Google Scholar]
- Song, H., Tucker, A. L., & Murrell, K. L. (2015). The diseconomies of queue pooling: an empirical investigation of emergency department length of stay. Management Science, 61(12), 3032–3053. 10.1287/mnsc.2014.2118 [DOI] [Google Scholar]
- SOU 2016. Effektiv vård. SOU 2016:2. Stockholm:Socialdepartementet. [Google Scholar]
- Straw, C. N. (2018). Engagement and retention in float pools: Keeping the team above water. Nursing Management, 49(10), 30–36. 10.1097/01.NUMA.0000546201.01962.0d [DOI] [PubMed] [Google Scholar]
- Terwiesch, C., Diwa, D., & Kahn, J. M. (2011). Working with capacity limitations: Operations management in critical care. Critical Care, 15, 308. 10.1186/cc10217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thelocal.com ’The biggest challenge of our time’: How Sweden doubled intensive care capacity amid Covid-19 pandemic. Accessed November 18, 2020. https://www.thelocal.com/20200623/how-sweden-doubled-intensive-care-capacity-to-treat-coronavirus-patients
- Utley, M., & Worthington, D. (2012). Capacity Planning. In Hall R. (Ed.), Handbook of healthcare system scheduling (pp. 11–30). Springer. [Google Scholar]
- Vanberkel, P. T., Boucherie, R. J., Hans, E. W., Hurink, J. L., & Litvak, N. (2012). Efficiency evaluation for pooling resources in health care. OR Spectrum, 34(2), 371–390. 10.1007/s00291-010-0228-x [DOI] [Google Scholar]
- Wing, J., & Vanberkel, P. (2021). Simulation optimisation for mixing scheduled and walk-in patients. Health Systems, 1–12. 10.1080/20476965.2021.1943010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, P. D., & Bretthauer, K. M. (2010). Strategies for addressing the nursing shortage: coordinated decision making and workforce flexibility. Decision Sciences, 41(2), 373–401. 10.1111/j.1540-5915.2010.00269.x [DOI] [Google Scholar]
- Zangrillo, A., & Gattinoni, L. (2020). Learning from mistakes during the pandemic: The Lombardy lesson. Intensive Care Med, 46(8), 1622–1623. 10.1007/s00134-020-06137-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zyl-Cillié, M. V., Demirtas, D., & Hans, E. (2022). Wait! What does that mean?: Eliminating ambiguity of delays in healthcare from an OR/MS perspective. Health Systems, 1–19. 10.1080/20476965.2021.2018362 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.