Abstract
Background:
The relationship between remaining anterior knee laxity and poorer clinical outcomes after anterior cruciate ligament reconstruction (ACLR) may be underrated, and the criteria for failure of revision ACLR have not been defined.
Purpose/Hypothesis:
To evaluate a possible association between remaining knee laxity and functional scores in patients after revision ACLR. We hypothesized that a postoperative side-to-side-difference (SSD) in knee laxity of ≥6 mm will be an objective parameter for failure.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A total of 200 patients (77 women and 123 men; mean age, 30.8 ± 11 years; range, 18-61 years) who underwent revision ACLR between 2016 and 2019 were evaluated; The mean follow-up period was 30.2 ± 9 months (range, 24-67 months). Patients were divided into 3 groups according to postoperative SSD (<3 mm, 3-5 mm, or ≥6 mm). Preoperative and postoperative outcome measures (Lachman, pivot shift, visual analog scale [VAS] for pain, Tegner, Lysholm, International Knee Documentation Committee, and Knee injury and Osteoarthritis Outcome Score) were compared between the groups.
Results:
Of the 200 patients, 74% (n = 148) had a postoperative SSD of <3 mm at the latest follow-up, 19.5% (n = 39) had a postoperative SSD of 3 to 5 mm, and 6.5% (n = 13) had a postoperative SSD of ≥6 mm. Patients in all groups saw significant pre- to postoperative reductions in positive Lachman and pivot-shift tests as well as significant improvements in VAS pain, Lysholm, and Tegner scores (P < .001 for all). All postoperative functional scores of the patients with SSDs of <3 mm and 3-5 mm were significantly increased compared with those of patients with an SSD of ≥6 mm (P≤ .01 for all).
Conclusion:
In patients following revision ACLR, anterior and rotational knee laxity were successfully reduced while increasing postoperative functional outcomes. A remaining postoperative SSD of ≥6 mm was associated with inferior patient outcomes compared with an SSD <6 mm. An SSD of ≥6 mm represents an objective parameter in the definition of failure of revision ACLR.
Keywords: revision ACL reconstruction, failure criteria ACL surgery, inferior patients’ outcome correlates with laxity, side-to-side- difference knee
The aim of anterior cruciate ligament reconstruction (ACLR) is to reduce elevated anterior and rotational knee laxity while increasing clinical outcome measures.10,32,33 Low rates of recurrent knee laxity and a significant increase in functional scores with good or excellent outcomes have been reported in 75% to 90% of patients after ACLR.19,28 However, the reduced anterior knee laxity after ACLR is not necessarily associated with subjective symptoms or improved functional outcome as has been reported in the current literature.7,20,23,32 A remaining increased Lachman grade or an elevated side-to-side difference (SSD) in anterior knee laxity therefore do not seem to be associated with inferior clinical outcome measures.
A limitation in studies of primary ACLR is the relatively small number of patients with poor postoperative outcomes and remaining anterior knee laxity.29,30,32 Very low rates (2.5%) of patients with persisting SSD of >4 mm have been reported after primary ACLR. 32 The analysis of functional outcomes in such a small number of patients may be error prone in a study population of primary ACLR patients. Therefore, the relationship between a remaining anterior knee laxity and poorer clinical outcome measures after primary ACLR may be underrated.
The outcome of revision ACLR is known to be inferior compared with primary ACLR with an increased number of a remaining anterior knee laxity.1,2,4,11,12 Knee laxity may be associated with functional scores in a patient population of revision ACLR. Although the number of clinical studies of primary and revision ACLR is rising, the criteria for failure of revision ACLR have not been uniformly defined in the current literature.11,36 Further, there is need for objective outcome parameters in the therapy for ligamentous instability. 9
The purpose of this study was to evaluate the clinical outcomes of patients after revision ACLR to demonstrate a possible association between remaining knee laxity and functional scores. The hypothesis was that a postoperative SSD of ≥6 mm will be associated with poorer clinical outcomes and represent an objective parameter for failure of revision ACLR.
Methods
Study Population
In this retrospective single-center study, patients were included if they had undergone revision ACLR between 2016 and 2019 and had provided written informed consent for participation in the study. Exclusion criteria were an additional lesion of the posterior cruciate ligament, infection of the knee, or signs of generalized hypermobility based on a Beighton score of ≥5 of 9. 31 Of 234 initial patients, 6 patients were excluded because of additional posterior cruciate ligament lesion, 3 patients because of generalized hypermobility, and 25 patients from loss to follow-up, leaving 200 patients with a minimum follow-up of 24 months who were included in this retrospective study. The study protocol was approved by the local ethics committee.
Patient Outcomes
Patient-related variables before revision ACLR included the Lysholm and Tegner score and physical examination under anesthesia at the time of revision ACLR.27,34 Two years after revision ACLR, the patients were contacted by telephone and invited for an examination in which range of motion, medial and lateral laxity, Lachman test, pivot-shift test, and the SSD in anterior laxity (measured using a Rolimeter (Aircast)) were recorded. 35 According to the 2000 International Knee Documentation Committee (IKDC) knee examination form, 13 participants were divided into 3 groups according to their postoperative SSD: <3 mm, 3-5 mm, or ≥6 mm.
The Lachman test, pivot-shift test, and Rolimeter testing were used to determine the anterior and anterolateral laxity of the knee. The pivot-shift test was graded as 0 (absent), 1 (glide), 2 (clunk), or 3 (gross), and the Lachman test was graded as 0 (absent), 1 (2-5 mm), 2 (6-10 mm), or 3 (>10 mm). 17 At the time of follow-up, the following scores were recorded: Lysholm, Tegner, subjective IKDC, and Knee injury and Osteoarthritis Outcome Score (KOOS; subscores Pain, Symptoms, Activities of Daily Living, function in Sport and Recreation [Sport/Rec], and Quality of Life [QoL]).8,22 Pain was quantified using a visual analog scale (VAS). 24
Surgical Technique for Revision ACLR
A single-stage procedure was performed in the case of a small previous bone tunnel (size <12 mm) and the ability to place a new tunnel without overlapping the previous tunnel; 91 patients had a single-stage revision ACLR. In 109 patients, a 2-stage revision procedure was performed, either because of the enlarged diameter of one of the bone tunnels or the previous bone tunnel position. Two-stage revisions were performed with soft tissue, partially layered quadriceps, or hamstring grafts. Bone tunnel filling was performed using cancellous allograft (DIZG). ACLR was carried out ≥4 months after bone tunnel grafting and assessment of the bony incorporation by computed tomography.
All revision ACLR procedures were performed with autografts during single-bundle ACLR using bone–patellar tendon–bone (BPTB), hamstring, or quadriceps grafts. If hamstring or BPTB grafts had already been harvested from the ipsilateral side, the grafts were taken from the contralateral side or the quadriceps tendon from the ipsilateral side; there was no previous quadriceps removal in any of the patients. The choice of graft was left up to the patient.
The ACLR was performed arthroscopically with drilling of the femoral tunnel via the anteromedial portal. Before the femoral and tibial bone tunnels were created, fluoroscopy was used to check the position of the guide wires. Tibial fixation was achieved with a combination of a bioabsorbable interference screw (GENESYS; Conmed) and extracortical suture fixation (No. 2 Fiberwire; Arthrex) via a button (Suture Washer; Smith & Nephew). For the femoral fixation, an adjustable button was used (TightRope RT; Arthrex).
The aim was to preserve the meniscus whenever possible. Peripheral meniscal lesions that could be repaired were sutured. Posterior horn lesions were treated with all-inside sutures, ramp lesions with direct sutures through a posteromedial portal, and lesions of the pars intermedia with outside-in sutures. When meniscal tears were not suitable for repair, partial meniscectomy was carried out. Cartilaginous lesions were treated nonoperatively.
When preoperative high-grade knee laxity occurred, patients received an additional lateral extra-articular tenodesis (LET). An approximately 7-cm long and 5 to 7 mm−wide strip of the iliotibial band starting from the Gerdy tubercle was fixed femorally. 3 The LET was placed superficially to the lateral collateral ligament. The harvesting defect in the iliotibial tract was closed using a braided absorbable suture (No. 2 Vicryl; Ethicon) sutures. When medial knee instability grade 2 or 3 was diagnosed preoperatively, 15 additional medial collateral ligament (MCL) reconstruction with an autologous graft was performed. MCL reconstruction was performed according to the descriptions of Preiss et al. 25 A gracilis tendon or peroneal tendon split graft of ≥15-cm length was placed in doubled fashion in a femoral tunnel positioned at the intersection of an imaginary extension of the posterior edge of the tibia with the Blumensaat line, creating 2 free branches. The ventral branch was placed in the center of the tibial superficial MCL (sMCL) insertion 3 to 5 mm above the pes anserinus; the posterior branch was placed in the tibial insertion of the posterior oblique ligament just above and medial to the semimembranosus insertion. Both branches were passed below the fascia. Medial knee instability was assessed clinically according to Hughston et al 15 (grade 1, 0-5 mm; grade 2, 6-10 mm; grade 3, >10 mm).
Statistical Analysis
Statistical analysis was performed using SPSS for Statistics (Version 29; IBM). For continuous variables the mean ± SD was used. The mean differences among the 3 SSD groups (<3, 3-5, ≥6 mm) were compared with the Kruskal-Wallis test, with the Dunn test for comparison of ≥2 groups and for nonnormally distributed parameters due to nonnormal distribution of the values. Categorical parameters were compared using the chi-square test. In case of small subgroups (n < 5), the Fisher exact text was used for categorical parameters. A P value of <.05 was considered significant.
In addition, we performed multiple linear regression analysis to identify predictors for reduced postoperative IKDC score after revision ACLR, including SSD of 3 to 5 mm, SSD ≥6 mm, body mass index (BMI), and medial meniscal lesions. Medial meniscal lesion and obesity were chosen as independent variables in the multiple linear regression analysis, as they are proven in the literature to be related to a worse functional outcome. 4
Results
Baseline patient characteristics are displayed in Table 1. The 200 patients comprised 77 women and 123 men with a mean age of 30.8 ± 11 years (range, 18-61 years) and a mean follow-up of 30.2 ± 9 months (range 24-67 months). Of these patients, 74% (n = 148) had a postoperative SSD of <3 mm at the latest follow-up, 19.5% (n = 39) had a postoperative SSD of 3 to 5 mm, and 6.5% (n = 13) had a postoperative SSD of ≥6 mm. The patients with an SSD of ≥6 mm had a significantly higher incidence of BMI >30 kg/m2 compared with the groups with SSD of <6 mm (46% vs 31% [SSD, 3-5 mm] and 12% [SSD, <3 mm]; P < .001). In addition, the BPTB graft was used more often in the group with SSD ≥6 mm versus the groups with SSD of <6 mm (62% vs 46% [SSD, 3-5 mm] and 33% [SSD, <3 mm]; P = .043), whereas the quadriceps tendon graft was used more often in the group with SSD <3 mm versus the groups with SSD of ≥3 mm (43% vs 33% [SSD, 3-5 mm] and 15% [SSD, ≥6 mm]; P = .043).
Table 1.
Baseline Patient Characteristics a
| Characteristic | Total (N = 200) | SSD <3 mm (n = 148) | SSD 3-5 mm (n = 39) | SSD ≥6 mm (n = 13) | P |
|---|---|---|---|---|---|
| Male sex | 123 (62) | 92 (62) | 25 (64) | 6 (46) | .493 |
| Age, y | 30.8 ± 11 (18-61) | 30.8 ± 11 (18-58) | 30.2 ± 11 (18-61) | 33.8 ± 12 (18-52) | .598 |
| Right knee affected | 120 (60) | 89 (60) | 22 (56) | 9 (69) | .715 |
| BMI >30 kg/m2 | 36 (18) | 18 (12) | 12 (31) | 6 (46) | <.001 |
| Two-stage revision ACLR | 109 (55) | 82 (55) | 22 (56) | 5 (39) | ns |
| Choice of revision ACLR graft | .043 | ||||
| Bone–patellar tendon–bone | 75 (38) | 49 (33) | 18 (46) | 8 (62) | |
| Hamstring tendon | 46 (23) | 35 (24) | 8 (21) | 3 (23) | |
| Quadriceps tendon | 79 (40) | 64 (43) | 13 (33) | 2 (15) | |
| Posterior tibial slope, deg | 9.5 ± 1.9 (5-16) | 9.5 ± 1.9 (6-16) | 9.4 ± 1.6 (5-13) | 10 ± 2.8 (6-16) | .935 |
| Lateral extra-articular tenodesis | 119 (60) | 89 (60) | 25 (64) | 5 (39) | .252 |
| Additional medial reconstruction | 16 (8) | 15 (10) | 0 | 1 (8) | .08 |
Data are reported as mean ± SD (range) or n (%). Boldface P values indicate statistically significant difference among the SSD groups (P < .05; Kruskal-Wallis test). ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; ns, not significant; SSD, side-to-side-difference.
The meniscal status at the time of revision ACLR is displayed in Table 2. There was a significant difference between the SSD ≥6 mm group and <6 mm groups in preoperative medial meniscal lesions (100% [SSD, ≥6 mm] vs 44% [SSD, 3-5 mm] and 56% [SSD, <3 mm]; P = .002) and lateral meniscal lesions (46% [SSD, ≥6mm] vs 33% [SSD, 3-5 mm] and 36% [SSD, <3 mm]; P = .012).
Table 2.
Meniscal Status at Revision ACLR a
| Lesion | Total (N = 200) | SSD <3 mm (n = 148) | SSD 3-5 mm (n = 39) | SSD ≥6 mm (n = 13) | P |
|---|---|---|---|---|---|
| Medial meniscal lesion | 113 (57) | 83 (56) | 17 (44) | 13 (100) | .002 |
| Repair | 75 (38) | 60 (41) | 11 (28) | 4 (31) | <.001 b |
| Partial resection | 35 (18) | 23 (16) | 5 (13) | 7 (54) | |
| Total resection | 3 (2) | 0 (0) | 1 (3) | 2 (15) | |
| Lateral meniscal lesion | 72 (36) | 53 (36) | 13 (33) | 6 (46) | .012 |
| Repair | 57 (29) | 45 (30) | 9 (23) | 3 (23) | .191 b |
| Partial resection | 15 (8) | 8 (5) | 4 (10) | 3 (23) | |
| Total resection | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Data are reported as n (%). Boldface P values indicate statistically significant difference among the SSD groups (P < .05; Kruskal-Wallis test). SSD side-to-side-difference.
Comparison of repair, partial resection, and total resection between the SSD groups.
The pre- and postoperative ligamentous laxity is displayed in Table 3. The percentage of positive Lachman tests was significantly reduced postoperatively compared with the preoperative examination (from 100% [N = 200] to 21% [n = 41]; P < .001), and the percentage of positive pivot-shift tests was also significantly reduced from pre- to postoperatively (from 97% [n = 193] to 16% [n = 31]; P < .001). In the preoperative assessment, the distribution of positive Lachman and pivot-shift tests was not significantly different between the 3 SSD groups. Postoperatively, however, Lachman grade 3 occurred significantly more often in the patients with SSD of ≥6 mm (69%) compared with an absent positive Lachman test in the patients with SSD <3 mm (92%; P < .001). Also, positive postoperative pivot-shift grading was seen significantly more often in the group with SSD of ≥6 mm compared with the patients with SSD <6 mm (92% vs 36% [SSD, 3-5 mm] and 3.4% [SSD, <3 mm]; P < .001) at the latest follow-up (Table 3).
Table 3.
Pre- and Postoperative Ligamentous Laxity a
| Test | Total (N = 200) | SSD <3 mm (n = 148) | SSD 3-5 mm (n = 39) | SSD ≥6 mm (n = 13) | P |
|---|---|---|---|---|---|
| Preoperative Lachman test | .158 | ||||
| Absent | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Grade 1 (2-5 mm) | 33 (17) | 28 (19) | 3 (8) | 2 (15) | |
| Grade 2 (6-10 mm) | 133 (67) | 99 (67) | 27 (69) | 7 (54) | |
| Grade 3 (>10 mm) | 34 (17) | 21 (14) | 9 (23) | 4 (31) | |
| Postoperative Lachman test | <.001 | ||||
| Absent | 159 (80) | 136 (92) | 0 (0) | 0 (0) | |
| Grade 1 (2-5 mm) | 28 (14) | 12 (8) | 22 (56) | 1 (8) | |
| Grade 2 (6-10 mm) | 13 (7) | 0 (0) | 17 (44) | 3 (23) | |
| Grade 3 (>10 mm) | 0 (0) | 0 (0) | 0 (0) | 9 (69) | |
| Preoperative pivot-shift test | .671 | ||||
| Absent | 7 (4) | 7 (5) | 0 (0) | 0 (0) | |
| Grade 1 (glide) | 46 (23) | 37 (25) | 6 (15) | 3 (23) | |
| Grade 2 (clunk) | 80 (40) | 57 (39) | 18 (46) | 5 (39) | |
| Grade 3 (gross) | 67 (34) | 47 (32) | 15 (39) | 5 (39) | |
| Postoperative pivot-shift test | <.001 | ||||
| Absent | 169 (85) | 143 (97) | 25 (64) | 1 (8) | |
| Grade 1 (glide) | 17 (9) | 4 (3) | 9 (23) | 4 (31) | |
| Grade 2 (clunk) | 13 (7) | 1 (0.7) | 5 (13) | 7 (54) | |
| Grade 3 (gross) | 1 (0.5) | 0 (0) | 0 (0) | 1 (8) |
Data are reported as n (%). Boldface P values indicate statistically significant difference among the SSD groups (P < .05; Kruskal-Wallis test). SSD side-to-side-difference.
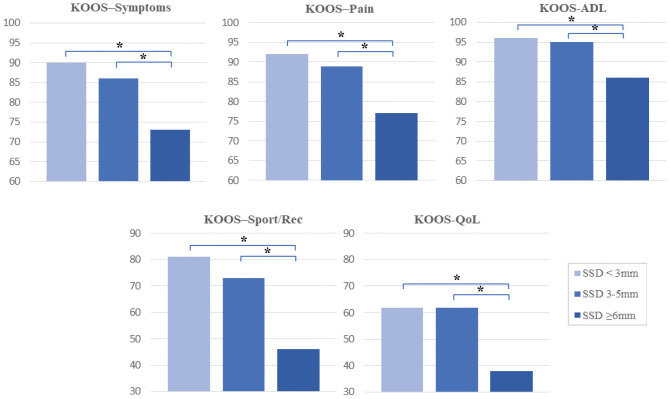
Postoperative functional scores are shown in Table 4. The VAS, Lysholm, and Tegner scores significantly improved from pre- to postoperatively for all groups (P < .001) and the patients showed good to excellent postoperative functional scores, with the exception of the KOOS Sport/Rec and KOOS QoL. All postoperative outcome measures were significantly different among the SSD groups, with scores in the SSD <6 mm groups significantly increased compared with the SSD ≥6 mm group (P≤ .01 for all) (Figure 1).
Table 4.
Comparison of Postoperative Functional Outcome Scores Between SSD Groups a
| Outcome Measure | Total (N = 200) | SSD <3 mm (n = 148) | SSD 3-5 mm (n = 39) | SSD ≥6 mm (n = 13) | P |
|---|---|---|---|---|---|
| VAS pain | |||||
| Preoperative | 4.1 ± 2.5 (0-10) | 4 ± 2.5 (0-10) | 4.4 ± 2.5 (0-10) | 5 ± 2.4 (2-9) | .35 |
| Postoperative | 1.3 ± 1.7 (0-9) | 1.1 ± 1.7 (0-9) | 1.2 ± 1.4 (0-5) | 3 ± 2.1 (0-6) | .001 |
| IKDC postoperative | 80.9 ± 15 (13.8-100) | 83.2 ± 13.8 (13.8-100) | 79.6 ± 12 (58.6-98) | 59.1 ± 11.2 (32-75.9) | <.001 |
| Tegner activity level | |||||
| Preoperative | 3 ± 1.4 (0-6) | 3 ± 1.5 (0-6) | 3 ± 1.5 (1-5) | 2.6 ± 1.3 (0-5) | .714 |
| Postoperative | 5.9 ± 1.6 (1-9) | 6.1 ± 1.5 (1-9) | 5.8 ± 1.7 (3-9) | 4.4 ± 1.1 (3-6) | <.001 |
| Lysholm | |||||
| Preoperative | 50.6 ± 22 (0-100) | 51.5 ± 22.5 (0-100) | 49.2 ± 21.2 (5-100) | 45.2 ± 23.6 (3-78) | .604 |
| Postoperative | 84.5 ± 15.3 (6-100) | 86.4 ± 15 (6-100) | 84.1 ± 12.5 (55-100) | 65 ± 13.7 (41-92) | <.001 |
| KOOS, postoperative | |||||
| Symptoms | 88.1 ± 14.3 (25-100) | 90.1 ± 13.6 (25-100) | 85.7 ± 14 (61-100) | 72.6 ± 13 (54-89.3) | <.001 |
| Pain | 90 ± 12 (36.11-100) | 91.5 ± 11.5 (36.1-100) | 88.8 ± 9.2 (58-100) | 77.2 ± 14.7 (39-94.4) | <.001 |
| ADL | 94.8 ± 8.2 (59-100) | 95.6 ± 7.8 (59-100) | 94.5 ± 7 (71-100) | 85.7 ± 10.8 (60-100) | <.001 |
| Sport/Rec | 77.5 ± 21 (10-100) | 81.3 ± 18.9 (20-100) | 72.9 ± 20.3 (30-100) | 45.8 ± 22 (5-85) | <.001 |
| QoL | 60 ± 20.4 (12.5-93.75) | 61.6 ± 19.2 (12.5-93.75) | 62.3 ± 21.7 (25-93.75) | 38 ± 19.1 (6-68.75) | .01 |
Data are reported as mean ± SD (range). Boldface P values indicate statistically significant difference among the SSD groups (P < .05; Kruskal-Wallis test). ADL, Activities of Daily Living; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; QoL, Quality of Life; Sport/Rec, Sport and Recreation; SSD, side-to-side difference; VAS, visual analog scale.
Figure 1.
Comparison of KOOS scores among the SSD groups. *Statistically significant difference between groups (P < .05). ADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; QoL, Quality of Life; Sport/Rec, Sport and Recreation.
The results of the linear regression analysis for predictors of inferior outcome of the postoperative IKDC score are displayed in Table 5. Postoperative SSD of ≥6 mm (odds ratio, −22.6 [95% CI, −30.4 to −14.7]; P < .001) was determined to be an independent risk factor associated with a reduced postoperative IKDC score after revision ACLR. BMI of ≥30 kg/m2 was also found to be an independent risk factor for reduced postoperative IKDC score (odds ratio, −5.1 [95% CI, (−10.1 to −0.02]; P = .049).
Table 5.
Results of Linear Regression Model for Inferior Postoperative IKDC Score a
| Characteristic | Odds Ratio (95% CI) | P |
|---|---|---|
| SSD 3-5 mm | −2.7 (−7.6 to 2.1) | .267 |
| SSD ≥6 mm | −22.6 (−30.4 to −14.7) | <.001 |
| BMI ≥30 kg/m2 | −5.1 (−10.1 to −0.02) | .049 |
| Preoperative medial meniscal lesion | −0.57 (−4.4 to 3.3) | .771 |
Reference value for each characteristic = 1.0. Boldface P values indicate statistical significance (P < .05). BMI, body mass index; SSD, side-to-side difference.
Discussion
The most important finding of this study was that anterior and rotational knee laxity can be successfully reduced while increasing postoperative functional outcome in patients following revision ACLR. A remaining postoperative SSD of ≥6 mm was associated with inferior patient outcomes compared with an SSD of <6 mm.
The relationship between persistent anterior knee laxity after ACLR and clinical outcome measures seems to be unclear in the current literature. In their recent multicenter study, Magnussen et al 23 showed that anterior knee laxity does not affect patient-reported outcome 2 years after primary ACLR, whereas a study by Lindanger et al 21 in 2021 demonstrated that a slightly loose graft of 3 to 5 mm at 6-month follow-up increased the risk of later revision surgery and led to a reduced Lysholm score at a long-term follow-up of 25 years. Redler et al 26 demonstrated a significant improvement on SSD on the KT-1000 arthrometer at the latest follow-up of patients with revision ACLR versus preoperative examination while increasing subjective IKDC, Tegner, and Lysholm score. In the present study, we could point out that the anterior and rotational knee laxity was significantly reduced while increasing the objective and subjective outcome measures. Beyond that, a remaining SSD of ≥6 mm was associated with inferior functional scores.
Some authors claim that the pivot-shift examination might be a better measure than instrumented knee laxity as far as patients’ functional outcome and overall satisfaction is concerned.18,32 Jonsson et al 18 reported that radiographic signs of osteoarthritis did not correlate with anterior knee stability at a follow-up of 5 to 9 years, whereas patients with a positive pivot-shift test 2 years after surgery showed increased signs of osteoarthritis at the latest follow-up and inferior subjective outcome measures at a 2-year follow-up. Streich et al 32 found a significant relationship between the pivot shift and clinical outcome measures in their study cohort of 40 patients. Thus, patients demonstrating a negative pivot shift had significantly better results in the subjective IKDC and Lysholm score than patients with rotational instability postoperatively. No relationship was found between the anteroposterior tibial translation measured by the KT-1000 arthrometer and functional clinical scores. In line with the aforementioned studies, this present study showed that reducing the rate of a positive pivot-shift test significantly increased the functional scores postoperatively. It can be stated that rotational instabilities correlate with poorer patient outcomes and worse overall satisfaction.5,7,16,18
Nevertheless, the studies by Jonsson et al 18 (N = 63 patients) and Streich et al 32 (N = 40 patients) had a small overall patient population. Also, the study by Streich et al only included a low number of patients with remaining anterior knee laxity (6 patients with SSD of 3-5 mm, none >5 mm) in the KT-1000 arthrometer. The relationship between the postoperative knee laxity and inferior functional scores might be underrated in these 2 studies. This present study demonstrates that a remaining knee laxity with SSD of ≥6 mm was associated with inferior postoperative subjective outcome measures in an adequate study population of 200 patients. Patients with a postoperative SSD of ≥6 mm had significantly reduced VAS, Lysholm, Tegner, KOOS, and IKDC scores in comparison with patients with an SSD of <6 mm.
Additionally, previous authors claimed that a remaining positive Lachman test or an elevated SSD seemed to be associated with inferior clinical outcome measures. Sernert et al 29 found that the worst residual functional impairment in ACLR, as measured with the Lysholm score and single-leg hop test, was found in the group with increased knee laxity of SSD ≥6 mm. Hrubesch et al 14 showed that the SSDs using the KT-1000 arthrometer revealed good correlation with the IKDC score.
These studies confirm the hypothesis of the present study that a remaining knee laxity correlates with inferior postoperative subjective outcome. Although in this study there was a significant increase of patients with obesity or a medial meniscal lesion in the group with SSD of ≥6 mm, the linear regression analysis proved that the SSD of ≥6 mm was an independent risk factor associated with a reduced postoperative IKDC in patients following revision ACLR. Thus, patients with a postoperative SSD of ≥6 mm had a significantly elevated risk of a reduced IKDC. This study is the first to show that the SSD of ≥6 mm represents an objective parameter in the definition of failure of revision ACLR.
Barber-Westin and Noyes 6 described criteria for revision ACLR failure in the early 1990s. Grafts were classified as partially functional when the KT-2000 arthrometer indicated an increase of 3 to 5.5 mm, the Lachman test was only slightly positive with a hard stop, and the pivot shift was tested negative. Grafts were designated as nonfunctional when ≥6 mm of increased anteroposterior displacement was detected on the KT-2000 or the pivot-shift test was positive. In line with Barber-Westin and Noyes, 6 we postulate that anterior knee instability of ≥6 mm is associated with revision ACLR failure. Further, this study pointed out that an SSD of ≥6 mm correlated with inferior patient outcomes.
In the present study, obesity (BMI, ≥30 kg/m2) was associated with a reduced postoperative IKDC and obese patients showed significant more often a postoperative SSD of ≥6 mm. A previous study also indicated a relationship between increased BMI and a reduced outcome after ACLR. 4 According to the results presented here, obesity is associated with inferior patient outcomes after revision ACLR.
There are some limitations in this study, as important data such as the preoperative SSD in the Rolimeter testing could not be collected due to the retrospective study design. Further, there were small subgroups of only 13 patients in the group of SSD ≥6 mm or 39 patients in the group of SSD 3 to 5 mm. The follow-up period of 24 months was also limited and postoperative long-term complications such as osteoarthritis or subsequent procedures could not be observed.
Conclusion
Anterior and rotational knee laxity can be successfully reduced in patients after revision ACLR while increasing postoperative functional outcome. A remaining postoperative SSD of ≥6 mm was associated with inferior patient outcomes in terms of lower functional scores compared with an SSD of <6 mm. An SSD of ≥6 mm represents an objective parameter in the definition of failure of revision ACLR.
Footnotes
Final revision submitted July 14, 2023; accepted July 21, 2023.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Ethik-Kommission der Aerztekammer Hamburg (reference No. PV5590).
References
- 1. Akoto R, Alm L, Drenck TC, et al. Slope-correction osteotomy with lateral extra-articular tenodesis and revision anterior cruciate ligament reconstruction is highly effective in treating high-grade anterior knee laxity. Am J Sports Med. 2020;48(14):3478-3485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alm L, Drenck TC, Frings J, et al. Lower failure rates and improved patient outcome due to reconstruction of the MCL and revision ACL reconstruction in chronic medial knee instability. Orthop J Sports Med. 2021;9(3):2325967121989312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alm L, Drenck TC, Frosch KH, Akoto R. Lateral extra-articular tenodesis in patients with revision anterior cruciate ligament (ACL) reconstruction and high-grade anterior knee instability. Knee. 2020;27(5):1451-1457. [DOI] [PubMed] [Google Scholar]
- 4. Alm L, Krause M, Frosch KH, Akoto R. Preoperative medial knee instability is an underestimated risk factor for failure of revision ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2458-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ayeni OR, Chahal M, Tran MN, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):767-777. [DOI] [PubMed] [Google Scholar]
- 6. Barber-Westin SD, Noyes FR. The effect of rehabilitation and return to activity on anterior-posterior knee displacements after anterior cruciate ligament reconstruction. Am J Sports Med. 1993;21(2):264-270. [DOI] [PubMed] [Google Scholar]
- 7. Bhardwaj A, Solanki NS, Jain H, et al. Comparison of outcome after ACL reconstruction in terms of subjective assessment of symptoms and function and clinical assessment of ligament stability. J Clin Orthop Trauma. 2018;9(2):172-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Collins NJ, Prinsen CAC, Christensen R, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317-1329. [DOI] [PubMed] [Google Scholar]
- 9. Davies GJ, McCarty E, Provencher M, Manske RC. ACL return to sport guidelines and criteria. Curr Rev Musculoskelet Med. 2017;10(3):307-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Diermeier T, Rothrauff BB, Engebretsen L, Bartels EM, Terwee CB, Roos EM. Treatment after anterior cruciate ligament injury: Panther Symposium ACL Treatment Consensus Group. Orthop J Sports Med. 2020;8(6):2325967120931097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Eggeling L, Drenck TC, Frings J, et al. Additional lateral extra-articular tenodesis in revision ACL reconstruction does not influence the outcome of patients with low-grade anterior knee laxity. Arch Orthop Trauma Surg. 2022;142(2):291-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Erickson BJ, Cvetanovich GL, Frank RM, Riff AJ, Bach BR., Jr. Revision ACL reconstruction: a critical analysis review. JBJS Rev. 2017;5(6):e1. [DOI] [PubMed] [Google Scholar]
- 13. Hefti F, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226-234. [DOI] [PubMed] [Google Scholar]
- 14. Hrubesch R, Rangger C, Reichkendler M, et al. Comparison of score evaluations and instrumented measurement after anterior cruciate ligament reconstruction. Am J Sports Med. 2000;28(6):850-856. [DOI] [PubMed] [Google Scholar]
- 15. Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58(2):159-172. [PubMed] [Google Scholar]
- 16. Hyder N, Bollen SR, Sefton G, Swann AC. Correlation between arthrometric evaluation of knees using KT 1000 and Telos stress radiography and functional outcome following ACL reconstruction. Knee. 1997;4(3):121-124. [Google Scholar]
- 17. Irrgang JJ, Anderson AF. Development and validation of health-related quality of life measures for the knee. Clin Orthop Rel Res. 2002;402:95-109. [DOI] [PubMed] [Google Scholar]
- 18. Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop Scand. 2004;75(5):594-599. [DOI] [PubMed] [Google Scholar]
- 19. Kawashima T, Omi Y, Kuriyama S, Hoshida T, Sugimoto D. Effect of graft rupture prevention training on young athletes after anterior cruciate ligament reconstruction: an 8-year prospective intervention study. Orthop J Sports Med. 2021;9(1):2325967120973593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629-634. [DOI] [PubMed] [Google Scholar]
- 21. Lindanger L, Strand T, Mølster AO, Solheim E, Inderhaug E. Effect of early residual laxity after anterior cruciate ligament reconstruction on long-term laxity, graft failure, return to sports, and subjective outcome at 25 years. Am J Sports Med. 2021;49(5):1227-1235. [DOI] [PubMed] [Google Scholar]
- 22. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150-154. [DOI] [PubMed] [Google Scholar]
- 23. Magnussen R, Reinke EK, Huston LJ, et al. Anterior and rotational knee laxity does not affect patient-reported knee function 2 years after anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(9):2077-2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ohnhaus EE, Adler R. Methodological problems in the measurement of pain: a comparison between the verbal rating scale and the visual analogue scale. Pain. 1975;1(4):379-384. [DOI] [PubMed] [Google Scholar]
- 25. Preiss A, Giannakos A, Frosch KH. [Minimally invasive augmentation of the medial collateral ligament with autologous hamstring tendons in chronic knee instability]. Oper Orthop Traumatol. 2012;24(4-5):335-347. [DOI] [PubMed] [Google Scholar]
- 26. Redler A, Iorio R, Monaco E, et al. Revision anterior cruciate ligament reconstruction with hamstrings and extra-articular tenodesis: a mid- to long-term clinical and radiological study. Arthroscopy. 2018;34(12):3204-3213. [DOI] [PubMed] [Google Scholar]
- 27. Risberg MA, Holm I, Steen H, Beynnon BD. Sensitivity to changes over time for the IKDC form, the Lysholm score, and the Cincinnati knee score: a prospective study of 120 ACL reconstructed patients with a 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):152-159. [DOI] [PubMed] [Google Scholar]
- 28. Samitier G, Marcano AI, Alentorn-Geli E, et al. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg. 2015;3(4):220-240. [PMC free article] [PubMed] [Google Scholar]
- 29. Sernert N, Kartus J, Kohler K, et al. Comparison of functional outcome after anterior cruciate ligament reconstruction resulting in low, normal and increased laxity. Scand J Med Sci Sports. 2002;12(1):47-53. [DOI] [PubMed] [Google Scholar]
- 30. Sernert N, Kartus J, Kohler K, et al. Analysis of subjective, objective and functional examination tests after anterior cruciate ligament reconstruction: a follow-up of 527 patients. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):160-165. [DOI] [PubMed] [Google Scholar]
- 31. Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. J Pediatr. 2011;158(1):119-123, 123 e111-114. [DOI] [PubMed] [Google Scholar]
- 32. Streich NA, Reichenbacher S, Barie A, Buchner M, Schmitt H. Long-term outcome of anterior cruciate ligament reconstruction with an autologous four-strand semitendinosus tendon autograft. Int Orthop. 2013;37(2):279-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Svantesson E, Hamrin Senorski E, Webster KE, et al. Clinical outcomes after anterior cruciate ligament injury: panther symposium ACL injury clinical outcomes consensus group. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2415-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tegner Y, Lysholm J, Odensten M, Gillquist J. Evaluation of cruciate ligament injuries. A review. Acta Orthop Scand. 1988;59(3):336-341. [DOI] [PubMed] [Google Scholar]
- 35. Wiertsema SH, van Hooff HJ, Migchelsen LA, Steultjens MP. Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. Knee. 2008;15(2):107-110. [DOI] [PubMed] [Google Scholar]
- 36. Xu C, Chen J, Cho E, Zhao J. The effect of combined anterolateral and anterior cruciate ligament reconstruction on reducing pivot shift rate and clinical outcomes: a meta-analysis. Arthroscopy. 2021;37(2):694-705. [DOI] [PubMed] [Google Scholar]