Introduction
Workplace injuries are a serious issue for the health and social care industry, with the sector accounting for 20 % of all serious claims reported. The aim of this systematic review was to determine whether patient handling training interventions that included instruction on patient transfer techniques are effective in preventing musculoskeletal injuries in healthcare workers. Methods: Electronic databases MEDLINE (Ovid), EMBASE (Ovid), CINAHL (EBSCO) and Health and Safety Science Abstracts (ProQuest) were searched for controlled trials from January 1996–August 2022. Risk of bias was evaluated using the PEDro scale and overall certainty of evidence assessed using the Grading of Recommendations, Assessment, Development and Evaluation for each meta-analysis. Results: A total of nine studies (3903 participants) were included. There is moderate certainty evidence that could not conclude whether patient handling training affects the 12-month incidence of lower back pain (OR = 0.83, 95 % CI [0.59, 1.16]). There is low certainty evidence that patient handing training does not prevent lower back pain in health professionals without pre-existing pain (MD = −0.06, 95 % CI [-0.63, 0.52]) but may reduce lower back pain in those with pre-existing pain (MD = −2.92, 95 % CI [-5.44, −0.41]). The results also suggest that there may be a positive effect of training incorporating risk assessment on musculoskeletal injury rates; however the evidence is of very low certainty. There is low certainty evidence from a single study that training may have a short-term effect on sickness absences.) Conclusions: There is a lack of evidence to support patient handling training when delivered to all healthcare staff. Training in its current form may be an ineffective strategy for reducing musculoskeletal injuries and pain. High quality disinvestment studies or trials incorporating risk assessment strategies are warranted. Practical Applications: This review suggests health service managers question the effectiveness of current patient handling training practices and consider evaluating current practices before allocating resources to meet employee risk reduction obligations.
Keywords: Occupational injuries, Low back pain, Nurses, Health personnel, Safety, Hospitals, Manual handling
Highlights
-
•
Patient handling training likely does not prevent lower back pain in health professionals without pre-existing pain.
-
•
Patient handling training may reduce lower back pain in those with pre-existing pain.
-
•
Evaluation of current patient handling training practices is recommended prior to allocation of health service resources.
1. Introduction
Workplace injuries are a serious issue for the health and social care industry. The sector accounts for 20 % of all serious claims resulting in a total absence from work for one working week or more in Australia; this equates to 26,239 claims annually [1]. In 2021, the USA recorded 6.1 non-fatal work-related injuries for every 100 full-time hospital employees and 7.3 for nursing and residential aged care workers, with 2.3 and 4.0 of these resulting in days away from work respectively [2]. Musculoskeletal injuries make up approximately 68 % of those serious claims and health professionals, specifically those working in hospitals and residential aged care, are most at risk [3]. Over a third of injuries resulting in days away from work are associated with patient interactions [4] and can occur during the bending, twisting, lifting or generating of excessive physical effort that is associated with moving or transferring patients [5].
Patient handling describes the movement of patients with or without the use of equipment. Following the introduction of key manual handling legislation in the UK in 1992 [6], patient handling programs have been put in place to mitigate the risks faced by health professionals. The ‘no-lift’ movement was pioneered by the UK Royal College of Nursing [7] and controversial manual lifts such as the orthodox lift and shoulder lift have since ceased to be recommended in practice [8]. The replacement of manual lifts with the provision of lifting equipment, mechanised patient beds and training in the use of equipment has reduced injuries [[8], [9], [10], [11], [12]] but overall injury rates remain high.
Patient handling training interventions are one strategy by which organisations aim to build upon the beneficial impact of patient handling equipment to minimise the ongoing risk to their staff. Training can include education in self-protective behaviours, use of lifting equipment and modification strategies for high-risk tasks [13]. Conventional patient handling training is delivered on employment commencement, then annually, and includes a combination of face-to-face and online learning [14,15]. Although robust economic data are not readily available in this field, costs associated with staff training have been estimated from approximately $3217 USD [16] to $9500 USD [17] per hospital ward and are therefore substantial when incurred year on year across a health service. Previous reviews have suggested that there is either no evidence [[18], [19], [20]] or conflicting evidence [13,21,22] for the effectiveness of training interventions at reducing work-related musculoskeletal injuries when delivered as a single intervention or when associated with co-interventions.
Previous reviews have not focused on controlled trials investigating patient handling training, inclusive of instruction on patient transfer techniques, with or without the assistance of equipment as a way of reducing risk, across the health, aged and disability sectors. While one recent review concluded that there was a lack of research investigating the relationship between the effect of staff training on incidence of work-related injuries in the health setting [23], another recent review of 6 studies (including 2 randomised controlled trials) found training in the use of equipment was effective in reducing workplace injuries in the health setting, whereas a review of 12 studies (4 randomised controlled trials) found education and training comprising various interventions was not effective [12]. There are also several earlier reviews that were not able to conclude that patient handling training was able to effectively reduce workplace musculoskeletal injuries. These included an early review of interventions to reduce musculoskeletal injuries that found training of patient handling techniques to have no effect on injuries. However, 33 of the 63 included studies were published prior to 1996 during a time when it was common to teach now-banned manual patient lifts [24]. Richardson, McNoe [22] reviewed controlled trials and trials using a pre-post design to investigate a variety of interventions to reduce musculoskeletal injuries and pain in nurses. Of the 20 included studies, three studies reported on patient handling training. One study received a strong quality rating and found no effect of training on pain, while two studies received a moderate rating and found training to reduce injuries. The authors concluded that training may be beneficial but high-quality further research is needed. Clemes, Haslam [13] investigated patient handling training across a number of industrial sectors. Of the 53 included studies, 15 reported on patient handling training in the healthcare sector and a high proportion of those studies were of low quality. The authors concluded there is very little evidence of the effectiveness of training. It is unclear whether the patient handling training interventions investigated in previous reviews taught patient handling techniques beyond standard operating procedures of equipment use. It is important to conduct a review of training inclusive of and beyond safe use of patient handling equipment as this type of instruction may have the potential to improve outcomes beyond those seen initially following the introduction of patient handling equipment. Given the low quality of evidence previously reviewed, our review will focus on controlled studies.
The aim of the current study was to systematically review the literature for controlled trials to determine whether patient handling training interventions, that included instruction on patient transfer techniques inclusive of and beyond correct manual handling equipment use are effective at preventing musculoskeletal injuries in healthcare workers.
2. Methods
This review was reported as per the PRISMA guidelines [25] and was registered prospectively in the PROSPERO database (CRD42021275281).
2.1. Search strategy
The electronic databases MEDLINE (Ovid), EMBASE (Ovid), CINAHL (EBSCO) and Health and Safety Science Abstracts (ProQuest) were searched from January 1996–August 2022. The 1996 date restriction was selected due to the UK Royal College of Nursing [7] Code of Practice for Patient Handling being published at this time. The publication influenced global changes in clinical practice away from controversial manual patient lifts [8]. Only including studies published after this time ensures the examination of contemporary clinical practices.
The database search strategy had four components: healthcare professional or worker; injury or pain; patient manual handling or moving and lifting; and controlled trial. For each concept, key words and MeSH terms and synonyms were combined with the OR operator. The results of each concept were then combined with the AND operator. Database searching was supplemented by searching reference lists of included studies and forward citation tracking of included studies on Google Scholar. An example of the search strategy can be viewed in Appendix 1.
Database searches were downloaded to Endnote with duplicates removed and then managed in Covidence. Two reviewers independently screened titles and abstracts for inclusion. Full text of remaining articles not excluded based on title and abstract were obtained and two reviewers independently screened these for inclusion. Agreement between reviewers was assessed using Cohen's kappa [26] where greater than 0.80 is considered almost perfect agreement, 0.61–0.80 substantial agreement, 0.41–0.60 moderate agreement, 0.21–0.40 fair agreement and 0.00–0.20 slight agreement. Disagreements were resolved through discussion and reaching of consensus; where consensus could not be met, a third reviewer was consulted.
2.2. Eligibility criteria
Included studies were limited to controlled trials as this study design is associated with higher quality studies with a reduced risk of bias. Studies were eligible if: the study population consisted of health professionals working in hospital and aged care facilities, home care, community or disability support settings; participants received patient handling training that included patient handling techniques - interventions that taught correct equipment use could be included provided they also taught patient moving and handling techniques; and outcomes reported work-related musculoskeletal injuries (Table 1). There were no language restrictions.
Table 1.
Inclusion/exclusion criteria.
| Inclusion | exclusion | |
|---|---|---|
| Population | Health professionals in hospital and aged care facility, home care, community, disability support settings | Other settings, non-health professionals not part of the care team such as orderlies, administration workers. |
| Intervention | Face-to-face, training of patient handling techniques/skills. Interventions that taught correct equipment use could be included provided they also taught patient moving and handling techniques. Interventions could be a single training intervention or multimodal | Online only, training on use of equipment only, training of now-banned patient lifts |
| Comparison | No training or usual care. Usual care may include online workplace induction, equipment use or back care education. | |
| Outcomes | Studies reporting on work-related musculoskeletal injuries which may include number of injuries, worker compensation claims or individual pain levels or the prevalence of pain. | Studies that do not include the primary outcome and only include psychological, emotional or mental injuries. |
| Study type | Controlled trials, including randomised controlled trials (RCT), cluster randomised controlled trials, non-randomised controlled trial. | Uncontrolled trials, including pre-post studies. |
| Date limit | 1996–Aug 2022 | Pre-1996 |
2.3. Quality assessment
To evaluate the quality of the included papers, the PEDro scale was used [27]. PEDro is an 11-item scale scored from 0 to 10 for internal validity items. Rasch analysis has confirmed that PEDro measures a single concept and can be scaled [28]. Scores of 0–3 are considered ‘poor’, 4–5 ‘fair’, 6–8 ‘good’, and 9–10 ‘excellent’ [29]. Two reviewers independently assessed the included studies. Disagreements were managed as described earlier.
2.4. Data extraction
Data extracted from the full text included details of study characteristics, participant characteristics, intervention and control group characteristics as per the Template for Intervention Description and Replication (TIDieR) checklist [30], and outcomes. A second reviewer checked the extracted data. Disagreements were resolved through discussion and reaching of a consensus; where consensus could not be met, a third reviewer was consulted.
2.5. Analysis
Meta-analysis was performed on clinically homogeneous randomised controlled trials with comparable outcome measures [31] using REVman software [32]. Consistent with recommendations, non-randomised studies of interventions were not included in meta-analyses [33]. For continuous data (pain intensity), post-intervention means and standard deviations were extracted from data tables and analysed using the inverse variance method and random effects model with estimate of effect expressed as mean difference. For dichotomous data (prevalence of pain), the number of participants experiencing pain was recorded and analysed using the Mantel-Haenszel method and random effects model to estimate odds ratios.
The certainty of evidence for each meta-analysis was determined with the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach [34] and were applied by one researcher and checked by a second. Evidence was downgraded from high to moderate to low and to very low quality in the following circumstances: If the PEDro score for at least 50 % of the included studies was less than 6 indicating a risk of bias; if there were greater than low levels of statistical heterogeneity between the trials (I2 ≥ 25 %) [35] indicating inconsistency; or if confidence intervals were large such that the possible effect could range from a large effect to no effect indicating imprecision. Single, controlled trials were considered both inconsistent and imprecise and were therefore determined to provide low certainty evidence. This could be further downgraded to very low certainty evidence if there was also high risk of bias [36].
To evaluate the effect of co-interventions (e.g. psychological intervention, exercise intervention) and the use of equipment when added to patient handling training, we completed a descriptive synthesis. Study results, whether favouring or inconclusive regarding patient handling training, were tabulated against the presence of co-interventions and use of equipment and any patterns described.
3. Results
3.1. Study selection
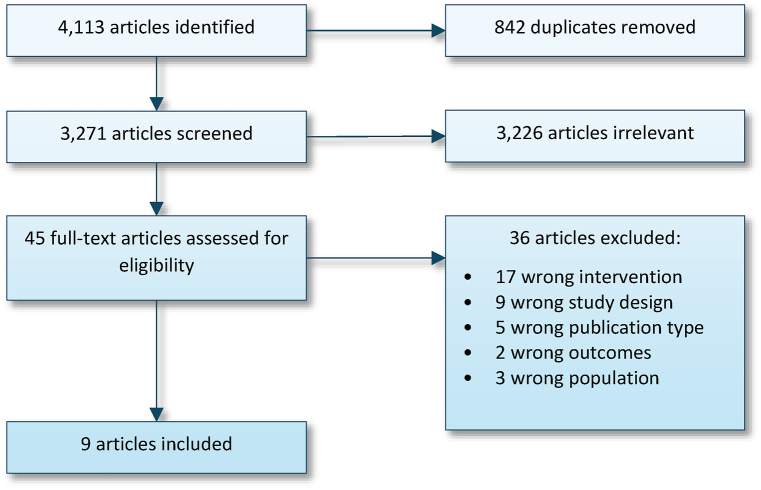
A total of 4113 articles were identified by the database searches (Fig. 1); 842 duplicates were removed and the remaining 3271 were screened by title and abstract. Of these, 3226 were removed and the remaining 45 full-text studies were screened for eligibility. There was moderate agreement between the reviewers during the title and abstract screening (κ = 0. 49, 95 % CI 0.38 to 0.60) and during full-text screening (κ = 0. 43, 95 % CI 0.15 to 0.70). The most common reason for exclusion of full-text articles was ‘wrong intervention’ (n = 17). A number of studies with large sample sizes [9,37,38] were excluded as the methods did not indicate that patient handling techniques were taught beyond basic techniques of moving a patient with equipment. Searching the reference lists and forward citation tracking of the included studies did not result in the inclusion of any additional studies.
Fig. 1.
PRISMA flowchart.
3.2. Risk of bias assessment
Of the nine studies, the majority (n = 5) scored less than 6 out of 10, indicating methodological limitations (Table 2). The most common methodological limitations were related to blinding. No studies blinded participants or the trainers and only the four higher-quality studies reported blinding of the assessors [[39], [40], [41], [42]]. Six studies reported random allocation to groups and only one study [42] reported concealed allocation. Less than half of the studies (n = 4) achieved key outcome measures for more than 85 % of their participants.
Table 2.
Study characteristics.
| Author | Participants | Intervention | Control | Design | Setting | Outcomes | Results | Quality Rating | ||||
| Number | Age, M (SD) | M/F (%F) | Number | Age, M (SD) | M/F (%F) | /10 | ||||||
| Hartvigsen 2005 | 316 nurses & nursing assistants | 171 | 44.6 (7.17a) | 100 | 145 | 44.4 (7.2a) | 100 | Pre-post with nonrandomized control | Home care | No. days with LBP past 12 months; No. episodes of LBP past 12 months | No sig. differences at 24 months | 3 |
| Svensson 2009 | 688 Nursing assistant students | 389 | 32 (10) | 100 | 279 | 33 (11) | 100 | Cluster randomised prospective study | Higher education | Sickness absence (days) during the last 14 months; No. participants experienced LBP last 12 months | Sig. higher sickness absence in control group at 14 months; No sig. difference in LBP | 6 |
| Svensson 2011 | 306 Nursing assistant students | 177 | 35 (12) | 90 | 129 | 35 (11) | 84 | Cluster randomised prospective study | Higher education | No. participants experienced continuous LBP for >3 months; Sickness absence (days) in last 12 months | No sig. differences at 36 months | 6 |
| Black 2011 | 766 Direct care workers | 151a | 40.89 (10.2)b | 94b | 165b | 39.1 (10.7)b | 94 %b | Retrospective pre- post, with nonrandomized control | Hospital and residential aged care | Injury rate: No. injuries per 100 FTE hours | Sig. decrease in injury rates in intervention group | 5 |
| Lim 2011 | 1480 Direct care workers | 782 | 41.2 (10.1) | 93 | 689 | 39.3 (10.2) | 91 | quasi-experimental with non-randomised control | Hospital and residential aged care | No. repeated injuries | Sig. fewer repeated injuries in small and medium hospitals, no difference in large hospitals | 5 |
| Jaromi 2018 | 137 nurses with LBP | 67 | 41.73 (3.54) | 93 | 70 | 41.4 (3.7) | 94 | RCT | Hospital | LBP intensity (VAS) previous 1 week | Sig. reduction in VAS at conclusion of 12-week program | 4 |
| Jensen 2006 | 142 nurses, nursing assistants and home care workers | 65 | 44.6 (9.8) | 100 | 77 | 44 (8.5) | 100 | RCT | Home care, disability and residential aged care | LBP intensity (VAS) last 3 and 12 months | No sig. differences at 24 months | 5 |
| Shojaei 2017 | 125 nursing assistants with LBP | 63 | <30 = 14 30-45 = 36, >45 = 13 |
17.5 | 62 | <30 = 15 30-45 = 40, >45 = 7 |
24.2 | RCT | Hospital | LBP intensity (VAS), period undefined | Sig. reduction in VAS at 6 months | 6 |
| Warming 2008 | 181 nurses | 105 | 33.65 (8.4)c | 92c | 76 | 35.7 (10.9) | 90 | Cluster randomised prospective study | Hospital | No. participants experienced LBP last 3 and 12 months; Average pain intensity (VAS) last 3 and 12 months; No. participants who have taken sick leave due to LBP last 3 and 12 months; LBP Disability score (Nordic Questionnaire) 12 months | No sig. differences | 6 |
Abbreviations: No. – number, LBP – lower back pain, sig. – significant(ly), FTE – full-time equivalent, VAS – visual analogue scale, RCT – randomised controlled trial.
Range converted to SD as per method describes by Hozo, Djulbegovic [43].
post cohort data only.
pooled for both intervention arms.
3.3. Study designs
Three of the studies were individually randomised [[42], [44], [45]] and three were cluster randomised [[39], [40], [41]]. Two were pre-post studies with non-randomised controls [46,47] and one study was quasi-experimental with a non-randomised control [48].
3.4. Participants
The nine studies included 3903 individual participants. The mean age of participants ranged from 33 to 44 years old and the majority were from the nursing discipline, including nurses, nursing assistants and nursing students (Table 2). Black, Metcalfe [46] and Lim, Black [48] expanded their cohort to all healthcare workers providing direct patient care while Jaromi, Kukla [44] and Shojaei, Tavafian [42] restricted their participants to nurses with a history of lower back pain. Reflective of the typical nursing workforce, the vast majority of participants were female (range 84 %–100 %). Shojaei, Tavafian [42], a study conducted in Iran, was an exception with females accounting for approximately 21 % of participants.
3.5. Interventions
The nine papers reported on seven different interventions. As per the inclusion criteria, all interventions included patient transfer technique training; however, there was variability in the interventions. Only Jensen, Gonge [45] and one of the intervention arms in Warming, Wiese [41] contained patient handling training as a single intervention. The interventions in each of the other studies were multi-modal, whereby patient transfer training was delivered with one or two co-intervention conditions including psychological interventions [39,40,42,47] and physical exercise training [[39], [40], [41],44]. Seven of the nine included studies reported the incorporation of patient handling equipment into training. Four studies incorporated low-tech aids such as slide sheets [[39], [40], [41],47] and three incorporated the use of high-tech equipment such as lifting machines in addition to low tech aids [45,46,48]. For the final two studies, the use of equipment in training was not reported [42,44]. Only the Transfer, Lifting and Repositioning (TLR) program reported on by Black, Metcalfe [46] and Lim, Black [48] included patient handling risk assessment in the content of the training. In the TLR program the risk assessment was taught in the form of patient handling algorithms. Training interventions across the included studies varied considerably in dose and duration from as little as two stand-alone 4-h sessions to weekly 1-h sessions over two years (Table 3).
Table 3.
Intervention description.
| Author | Name | Rationale | Materials | Procedures | Who provided | How | Where | When and how much | Tailoring | Modifications | Fidelity- planned | Fidelity - delivered |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hartvigsen, Lauritzen [47] | Intervention group | Bobath principle: reduce load on the body by maximising patient participation, reducing friction and maintaining natural body positions | Low-tech equipment | Practical training on lifting techniques and body mechanics according to the Bobath principle. | Train the trainer model. Nurse or nurse aid instructor trained by a physiotherapist skilled in body mechanics and lifting techniques | Face- to-face, group | NR | 1 × 1hr per week session for 2 yrs +4 × 2hr psychology sessions |
Encouraged to provide feedback on transfers during sessions. | NR | NR | NR |
| Svensson, Stroyer [39] | LBP Prevention program | Improve fitness to cope with sudden spinal loading, improve transfer techniques to reduce spinal loading, improve psychological coping strategies to LBP | Low-tech equipment | Physical training: unexpected trunk loading and balance. Patient transfers: theoretical education and practical exercises. Stress management: theoretical exercises and group discussions to increase coping capacity |
School teaching teams | Face- to-face, group | NR | Physical training (48 × 1 hr). Patient transfer technique education (20 h) and Stress management (22 h). | NR | NR | All students in intervention group | NR |
| Svensson, Marott [40] | LBP Prevention program | Improve fitness to cope with sudden spinal loading, improve transfer techniques to reduce spinal loading, improve psychological coping strategies to LBP | Low-tech equipment | Physical training: unexpected trunk loading and balance. Patient transfers: theoretical education and practical exercises. Stress management: theoretical exercises and group discussions to increase coping capacity |
School teaching teams | Face- to-face, group | NR | Physical training (48 × 1 hr). Patient transfer technique education (20 h) and Stress management (22 h). | NR | NR | All participants in intervention group | NR |
| Black, Metcalfe [46] | Transfer, Lifting and Repositioning (TLR) Program | To prevent patient handling-related musculoskeletal injuries | A course booklet and training materials, low- and high-tech equipment | Education on anatomy, injuries, body mechanics, personal health, lifting and patient handling procedures, standardized patient handling needs assessment, and patient handling algorithms. Practical patient handling skill component | NR | Face- to-face, group | NR | Initial 1 × 8hr session + on-ward coaching + 1 h/year follow-up | NR | NR | Mandatory for all direct care working | NR |
| Lim, Black [48] | Transfer, Lifting and Repositioning (TLR) Program | To prevent patient handling-related musculoskeletal injuries | A course booklet and training materials. low- and high-tech equipment | Education on anatomy, injuries, body mechanics, personal health, lifting and patient handling procedures, standardized patient handling needs assessment, and patient handling algorithms. Practical patient handling skill component | NR | Face- to-face, group | NR | Initial 1 × 8hr session + on-ward coaching + 1 h/year follow-up | NR | NR | Mandatory for all direct care working | NR |
| Jaromi, Kukla [44] | Spine care for nurses | Increase knowledge of spinal biomechanics and patient handling techniques and strengthen muscles in order to avert microtrauma | Written materials detailing exercise program and patient handling skills, equipment use not reported | Theoretical sessions to educate on the spinal anatomy, biomechanics, injury prevention and lifting techniques. Practical sessions to practise spinal strengthening exercises and patient transfers according to the Dotte and Bobath methods | NR | Face- to-face, group | NR | 2 × 60min sessions per week for 12 weeks | NR | NR | All participants in intervention group | NR |
| Jensen, Gonge [45] | Transfer Technique Intervention | Education based on Stockholm training concept to reduce biomechanical load on the back, minimise asymmetric posture and avoid sudden loads | Low- and high-tech equipment | Practical classroom education with 30 transfer situations taught, followed by implementation period of on-site training | Classroom sessions: project supervisors trained in Stockholm training concept. On-site group participants with additional 30hrs training | Face-to-face, group | On-site training in usual work setting | 2 × 4hrs classroom education, 2–6 months of on-site training | On-site training adapted to individual work situations | NR | All staff | NR |
| Shojaei, Tavafian [42] | Educational Program | Education based on social cognitive theory increase likelihood of healthy behaviours of safe patient handling | Equipment use not reported | Education on self-efficacy, self-regulation, highlighting outcome expectation and emotional coping related to safe postures while moving patients. Education methods included, skills training, negotiation, role-playing, goal setting and self-assessment. | Health education specialist | Face- to-face, group | NR | 4 × 2hr sessions | Individualised goal setting and addressing of barriers to safe handling | NR | All participants | NR |
| Warming, Wiese [41] | Transfer Training | Train the trainer model used to adapt knowledge from an expert to their local setting. Transfer techniques taught based on gravity, friction and lever arm principles | Low-tech equipment | Trainers trained colleagues on the ward. No further information about specific activities | Nurses with 4 days of training | Face-to-face | Hospital | Trainer available on ward for 2 × 6week blocks to train staff. No indication of dose per participant | Training individualised to wards and on the job situations | NR | All ward nurses | No. who complete training reported |
| Transfer Training + Physical Training | As per TT with addition of physical training to increase physical capacity | Low-tech equipment, gym equipment and heart rate monitor watch | As per Transfer Training with addition of circuit training for aerobic fitness of 5 × 6mins, Strength of 4 × 5mins, 5min cool-down | NR | face- to-face, group | Hospital | Physical training: 2 × 1 h/week for 8 weeks | Programs individualised to work at 70–90 % of VO2 max | NR | All participants in the TT + PT group | No. who complete part of intervention reported (Physical Training reported, not Transfer Training) |
Abbreviations: NR – not reported, LBP – lower back pain, VO2 max – maximum volume of oxygen consumption.
Equipment category descriptions: 1. Use of equipment not reported 2. Use of low-tech aids such as slide sheets and slings 3. Use of high-tech equipment such as hoists and lifting machines.
The details of each intervention were not well described (Table 3). Intervention rationale, content, modifications and fidelity/attendance were the areas most lacking. In particular, training procedures and the dose of ‘coaching on the ward’ were unclear in Black, Metcalfe [46], Lim, Black [48], Jensen, Gonge [45] and Warming, Wiese [41]. Control conditions were very poorly described (Supplementary Table 1).
3.6. Outcomes
The summary of findings and certainty of evidence from meta-analyses can be viewed in Table 4.
Table 4.
Summary of findings and certainty of evidence.
| No. of Studies |
Quality Assessment |
Outcome |
No. of Participants |
Effect (95 %CI) |
Certainty (GRADE) |
|||
|---|---|---|---|---|---|---|---|---|
| Risk of Bias | Inconsistency | Imprecision | Training | No Training | ||||
| Effect of training on 12-month LBP incidence | ||||||||
| 2 | Not serious | Not serious | Serious | Nordic Questionnaire | 432 | 317 | OR = 0.83 (0.59,1.16) | Moderate |
| Effect of training on LBP intensity – Pre-existing LBP | ||||||||
| 2 | Serious | Serious | Not Serious | VAS | 130 | 132 | MD = −2.92 (−5.44 -0.41) | Low |
| Effect of training on LBP intensity – No pre-existing LBP | ||||||||
| 2 | Serious | Not Serious | Serious | VAS | 113 | 112 | MD = −0.06 (−0.63, 0.52) | Low |
Abbreviations: GRADE – Grading of Recommendations, Assessment, Development and Evaluations, LBP – lower back pain, VAS – visual analogue scale, MD – mean difference (units out of 10), OR – odds ratio.
3.6.1. Lower back pain
Lower back pain was the most common variable measured with seven of the studies reporting measures related to this outcome. There was variability in the measures used to assess lower back pain, including differences in follow-up periods. Three studies [39,41,47] measured the incidence of lower back pain in the last 12-month period using the Nordic Questionnaire, while one study [40] defined incidence of lower back pain as continuous pain for a period of greater than 3 months. Three studies [41,44,45] measured the intensity of lower back pain using the Visual Analogue Scale (VAS). Follow-up periods for average VAS scores varied from 1 week [44] to 3 and 12 months [41,45].
Meta-analysis of two studies [39,41] with 749 participants provided moderate certainty evidence (Table 4) that could not conclude whether patient handling training affects the 12-month incidence of lower back pain (Fig. 2). Two studies not included in the metanalysis provided low [40] and very low [47] certainty evidence to support the inconclusive findings of the meta-analysis.
Fig. 2.
No effect of intervention on incidence of lower back pain over 12 months.
Metanalysis of two studies with 262 participants targeting health professionals with pre-existing lower back pain [42,44] provided low certainty evidence that training reduces lower back pain intensity in people with pre-existing lower back pain (Fig. 3). In the studies reporting on general populations, 65 % [41] and 76 % [45] of participants did not report a history of lower back pain. Metanalysis of these two studies with 225 participants targeting general healthcare staff populations [41,45] provided low certainty evidence that could not conclude whether training affects pain intensity in people without pre-existing lower back pain (Fig. 4).
Fig. 3.
Change in lower back pain VAS in nurses with pre-existing lower back pain.
Fig. 4.
No change in lower back pain VAS in nurses without pre-existing lower back pain.
3.6.2. Musculoskeletal injuries
Two papers reporting on the one training program measured musculoskeletal injuries by investigating injury claim data [46,48]. These single papers each provided very low certainty evidence that patient handling training incorporating risk assessment reduced overall injury rates (number of injuries per 100 full-time-equivalent hours) in a general population of direct care workers [46] and reduced the number of repeated musculoskeletal injuries in workers with a history of previous injury [48].
3.6.3. Sickness absences
Svensson, Stroyer [39] monitored sickness absences taken for any reason by nursing students during their 14-month course and placements. This study provided low certainty evidence that training significantly reduced absences in the intervention group. Positive effects were not maintained at 3 years [40]. Warming et al. (2008) monitored sick leave due to lower back pain over a 3-month period and reported no significant differences in either of the intervention groups [41].
3.6.4. Co-interventions and use of equipment
The presence of co-interventions and the category of equipment use did not appear to be associated with the outcome of the training intervention (Table 5). Of the four studies that included a physical exercise intervention, two reported positive outcomes [39,44] and two reported no effect [40,41]. Of the four studies that included a psychological intervention, two reported positive outcomes [39,42] and two reported no effect [40,47]. Of the four studies that reported the use of low-tech equipment, one reported positive outcomes [39] and three reported no effect [40,41,47]. Of the three studies that reported the use of low- and high-tech equipment, two reported positive outcomes [46,48] and one reported no effect [45].
Table 5.
Co-interventions and use of equipment for positive and non-significant studies of patient manual handling.
| Patient handling training | Risk assessment included | Psychological intervention | Exercise intervention | Use of low-tech equipment | Use of high-tech equipment | Equipment use not reported | ||
|---|---|---|---|---|---|---|---|---|
| Reported positive results | ||||||||
| Jaromi et al. (2018) | Reduction in LBP (VAS) | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✓ |
| Shojaei et al. (2017) | Reduction in LBP (VAS) | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | ✓ |
| Svensson et al. (2009) | Reduction in sickness absences | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✗ |
| Black et al. (2011) | Reduction in rate of injury | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ |
| Lim et al. (2011) | Reduction in repeat injuries | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ |
| Reported non-significant results | ||||||||
| Jensen et al. (2006) | No effect on LBP (VAS) | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ |
| Svensson et al. (2011) | No effect on sickness absences | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✗ |
| Hartvigsen et al. (2005) | No effect on LBP (incidence) | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | ✗ |
| Warming et al. (2008) | No effect on LBP (VAS or incidence or sickness absences | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ |
| ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ||
4. Discussion
This review suggests that when patient handling training is applied to whole populations of health professionals, inclusive of and beyond correct manual handling equipment use, it does not reduce musculoskeletal injuries or pain. The results of this study provide low to moderate quality evidence that patient handing training likely does not prevent lower back pain in health professionals without pre-existing pain but may reduce lower back pain in those with pre-existing pain. The results also suggest that there may be a positive effect of training incorporating risk assessment on musculoskeletal injury rates; however, the evidence is of very low certainty. There is low certainty evidence from a single study that training may have a short-term effect on sickness absences. These results are consistent with a number of previous reviews that have suggested that there is little evidence to demonstrate the effectiveness of patient handling training [8,13,[20], [21], [22]].
One possible implication of these findings is that the content of the training that is currently being implemented is ineffective. It has been suggested that training interventions that include patient handling risk assessment may be effective at preventing injuries [8,24,[49], [50], [51]]. Risk assessment training aims to provide a framework by which clinicians use clinical reasoning to assess patient handling scenarios and decide how to proceed based on unique clinical information. This allows for an individualised approach to patient handling that empowers clinicians to deal with the complex and changing situations that they encounter during their workdays. In Australia, 92 % of hospitals and residential aged care services delivering conventional patient handling training identified that risk assessment was missing in part of in whole from their training programs [14]. Risk assessment training has been demonstrated to positively change clinical behaviour during the patient handling interactions [52], while there is very little evidence that conventional patient handling training programs result in behaviour change [20]. Only two reports, each with a high risk of bias, reported on a single trial where the patient handling program included risk assessment [46,48]. While providing very low certainly evidence, these studies had positive results. Higher quality research of programs containing risk assessment are required to further investigate the question of what constitutes effective training content.
In light of the mounting evidence, the possibility that patient handling training in its current form is ineffective at preventing injury and should not continue may be considered by the staff assisting patient movement, and their managers. Given the high cost of implementing large-scale mandatory patient handling training programs, the health industry may consider disinvesting in these programs in their current form. One concern for managers at health networks might be that they feel obliged to continue current training because of legislative requirements. In the Australian context, local legislation states that workplaces provide “… training or supervision to employees … to enable those persons to perform their work in a way that is safe and without risks to health” (Occupational Health and Safe Act 2004 (Vic) div 2(21)). The results from this review suggests that employers may not be meeting these prescribed duty of care requirements with current training strategies. Disinvestment studies, such as those currently being completed for falls sensor alarms [53], patient falls risk screening tools [54] and weekend allied health therapy [55], have been successful in adding valuable contributions to the literature. Reinvestment in establishing programs that target patient handling training to health professional with a history of pre-existing musculoskeletal injuries or pain [42,44] may be an appropriate starting point for refining the scope of this type of intervention. In addition, investment in interventions with some supporting evidence such as risk assessment training or training in the use of equipment [12] with research designs with a low risk of bias may also be warranted. Common to these suggestions is the idea that training interventions should be rigorously evaluated before resources for scaled up, routine implementation are allocated.
This review is relevant to the health professional workforce as nurses, nursing assistants and students, who are at the highest risk of injury, were the majority of the participants included in the studies. A strength of this systematic review is that it built on previous investigations into injury prevention in the healthcare industry by refining the systematic review question to specifically investigate the effect of interventions involving patient handling training. The review followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [25] and only included controlled trials. Where meta-analysis was able to be performed, applying the GRADE approach helped to determine level of certainty of the evidence.
4.1. Limitations
A limitation of the findings of this systematic review is that some of the included studies were not randomised controlled trials and were therefore not able to be included in meta-analyses. Of the meta-analyses that were performed, each included only two trials, the heterogeneity at times was high and the certainty of evidence did not exceed a rating of moderate. This review found that training interventions were poorly described, particularly the dose of intervention and the adherence to the programs. It is therefore difficult to evaluate whether specific content or modes of implementation may contribute to the effectiveness of training. This review focused on studies of patient handling training, described as the movement of patients with or without the use of equipment. We cannot conclude on the effectiveness of other interventions that have been the focus of other reviews. For example, one review that included a focus of training in the use of equipment concluded this type of training was effective in benefiting healthcare worker health compared to no intervention [12]. Therefore, our findings are limited to interventions that train healthcare staff to assist movement of patients and should not be interpreted to provide guidance on other interventions.
4.2. Conclusion and practical applications
The results of this review provide low to moderate quality evidence that patient handling training likely does not prevent lower back pain in health professionals without pre-existing pain but may reduce lower back pain in those with pre-existing pain. The results also suggest that there may be a positive effect of training incorporating risk assessment on musculoskeletal injury rates however the evidence is of very low certainty. There is low certainty evidence from a single study that training may have a short-term effect on sickness absences. Patient handling training, whether delivered with or without co-interventions such as exercise and the use of equipment, in its current form may be an ineffective strategy for reducing musculoskeletal injuries. Health service managers are encouraged to question the effectiveness of current patient handling training practices and consider rigorously evaluating current practice to better allocate resources to meet their employee risk reduction obligations. High quality disinvestment studies or trials incorporating innovative risk evaluation strategies are recommended as the next step to investigating this area.
Funding statement
This work was supported by La Trobe University and the Cabrini Foundation via an industry funded PhD scholarship. The funding bodies have no role in the design, analysis or dissemination of the results.
Date availability statement
Upon reasonable request, the template data collection forms, data extracted from included studies and data used for all analyses can be made available.
CRediT authorship contribution statement
Helen L. Kugler: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Nicholas F. Taylor: Writing – review & editing, Visualization, Validation, Supervision, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Natasha K. Brusco: Writing – review & editing, Visualization, Validation, Supervision, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e24937.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Safe Work Australia . 2022. Key Work Health and Safety Statistics; p. 2022. Australia. [Google Scholar]
- 2.U.S Bureau of Labor Statistics . 2022. Injuries, Illnesses, and Fatalities.https://www.bls.gov/iif/nonfatal-injuries-and-illnesses-tables/table-1-injury-and-illness-rates-by-industry-2021-national.htm#soii_n17_as_t1.f.1 25/07/2023]; Available from: [Google Scholar]
- 3.Safe Work Australia . Statistics on workers in Australia; 2018. Number, Frequency Rate and Incidence Rate of Serious Claims by Occupation 2011-12 to 2015-16p.https://www.safeworkaustralia.gov.au/system/files/documents/1805/number-frequency-incidence-serious-claims-by-occupation-2011-12-to-2015-16p.pdf [cited 2021 March 4]; Available from: [Google Scholar]
- 4.Occupational Safety and Health Administration . 2013. Facts about Hospital Worker Safety.https://www.osha.gov/sites/default/files/1.2_Factbook_508.pdf Available from: [Google Scholar]
- 5.Sampath S.L., et al. Reality of safe patient handling policies and programs in hospitals across the United States. International Journal of Safe Patient Handling & Mobility. 2019;9(2):69–76. [Google Scholar]
- 6.Health, Executive Safety. 2016. Manual Handling Operations Regulations 1992 (As Amended)https://www.hse.gov.uk/pubns/books/l23.htm [cited 2021 March 4]; Available from: [Google Scholar]
- 7.Royal College of Nursing . Royal College of Nursing; London: 1996. RCN Code of Practice for Patient Handling. [Google Scholar]
- 8.Hignett S., et al. Evidence-based patient handling: systematic review. Nurs. Stand. 2003;17(33):33–36. doi: 10.7748/ns2003.04.17.33.33.c3383. [DOI] [PubMed] [Google Scholar]
- 9.Engkvist I.L. Evaluation of an intervention comprising a no lifting policy in Australian hospitals. Appl. Ergon. 2006;37(2):141–148. doi: 10.1016/j.apergo.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Koppelaar E., et al. Determinants of implementation of primary preventive interventions on patient handling in healthcare: a systematic review. Occup. Environ. Med. 2009;66(6):353–360. doi: 10.1136/oem.2008.042481. [DOI] [PubMed] [Google Scholar]
- 11.Hegewald J., et al. Do Technical aids for patient handling prevent musculoskeletal complaints in health care Workers?-A systematic review of intervention studies. Int. J. Environ. Res. Publ. Health. 2018;15(3) doi: 10.3390/ijerph15030476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wahlin C., Stigmar K., Nilsing Strid E. A systematic review of work interventions to promote safe patient handling and movement in the healthcare sector. Int. J. Occup. Saf. Ergon. 2022;28(4):2520–2532. doi: 10.1080/10803548.2021.2007660. [DOI] [PubMed] [Google Scholar]
- 13.Clemes S.A., Haslam C.O., Haslam R.A. What constitutes effective manual handling training? A systematic review. Occup. Med. (Lond.) 2010;60(2):101–107. doi: 10.1093/occmed/kqp127. [DOI] [PubMed] [Google Scholar]
- 14.Brusco N., et al. In Australian hospitals and residential aged care facilities, how do we train nursing and direct care staff to assist patients and residents to move? A national survey. Aust. Health Rev. 2023;47(3):331–338. doi: 10.1071/AH22296. [DOI] [PubMed] [Google Scholar]
- 15.McDermott H., et al. Investigation of manual handling training practices in organisations and beliefs regarding effectiveness. Int. J. Ind. Ergon. 2012;42(2):206–211. [Google Scholar]
- 16.Nelson A., et al. Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. Int. J. Nurs. Stud. 2006;43(6):717–733. doi: 10.1016/j.ijnurstu.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Dang T., et al. A return-on-investment model using clinical and economic data related to safe patient handling and mobility programs in the ICU. Int. J. Ind. Ergon. 2022;92 [Google Scholar]
- 18.Caponecchia C., et al. Musculoskeletal disorders in aged care workers: a systematic review of contributing factors and interventions. Int. J. Nurs. Stud. 2020;110 doi: 10.1016/j.ijnurstu.2020.103715. [DOI] [PubMed] [Google Scholar]
- 19.Martimo K.P., et al. Effect of training and lifting equipment for preventing back pain in lifting and handling: systematic review. BMJ. 2008;336(7641):429–431. doi: 10.1136/bmj.39463.418380.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hogan D.A., Greiner B.A., O'Sullivan L. The effect of manual handling training on achieving training transfer, employee's behaviour change and subsequent reduction of work-related musculoskeletal disorders: a systematic review. Ergonomics. 2014;57(1):93–107. doi: 10.1080/00140139.2013.862307. [DOI] [PubMed] [Google Scholar]
- 21.Dawson A.P., et al. Interventions to prevent back pain and back injury in nurses: a systematic review. Occup. Environ. Med. 2007;64(10):642–650. doi: 10.1136/oem.2006.030643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Richardson A., et al. Interventions to prevent and reduce the impact of musculoskeletal injuries among nurses: a systematic review. Int. J. Nurs. Stud. 2018;82:58–67. doi: 10.1016/j.ijnurstu.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Johnson K., et al. Manual patient handling in the healthcare setting: a scoping review. Physiotherapy. 2023;120:60–77. doi: 10.1016/j.physio.2023.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Hignett S. Intervention strategies to reduce musculoskeletal injuries associated with handling patients: a systematic review. Occup. Environ. Med. 2003;60(9) doi: 10.1136/oem.60.9.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Page M.J., et al. Bmj; 2021. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 27.Maher C.G., et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 28.de Morton N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust. J. Physiother. 2009;55(2):129–133. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 29.Cashin A.G., McAuley J.H. Clinimetrics: physiotherapy evidence database (PEDro) scale. J. Physiother. 2020;66(1):59. doi: 10.1016/j.jphys.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Hoffmann T.C., et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ Br. Med. J. (Clin. Res. Ed.) 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 31.Cumpston M., et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019;10 doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The Cochrane Collaboration . The Nordic Cochrane Centre; Copenhagen: 2014. Review Manager (RevMan) [Computer Program] 5.3. [Google Scholar]
- 33.Reeves, B.C., et al. Chapter 24: Including non‐randomized studies on intervention effects. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022) 2022 23/02/2023]; Available from: www.training.cochrane.org/handbook..
- 34.Guyatt G.H., et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Higgins J.P., et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gluppe S., Engh M.E., Bo K. What is the evidence for abdominal and pelvic floor muscle training to treat diastasis recti abdominis postpartum? A systematic review with meta-analysis. Braz. J. Phys. Ther. 2021;25(6):664–675. doi: 10.1016/j.bjpt.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sabbath E.L., et al. Paradoxical impact of a patient-handling intervention on injury rate disparity among hospital workers. Am. J. Publ. Health. 2019;109(4):618–625. doi: 10.2105/AJPH.2018.304929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dennerlein J.T., et al. Lifting and exertion injuries decrease after implementation of an integrated hospital-wide safe patient handling and mobilisation programme. Occup. Environ. Med. 2017;74(5):336–343. doi: 10.1136/oemed-2015-103507. [DOI] [PubMed] [Google Scholar]
- 39.Svensson A.L., et al. Multidimensional intervention and sickness absence in assistant nursing students. Occup. Med. (Lond.) 2009;59(8):563–569. doi: 10.1093/occmed/kqp124. [DOI] [PubMed] [Google Scholar]
- 40.Svensson A.L., et al. Sickness absence in student nursing assistants following a preventive intervention programme. Occupational medicine (Oxford, England) 2011;61(1):57–61. doi: 10.1093/occmed/kqq142. [DOI] [PubMed] [Google Scholar]
- 41.Warming S., et al. Little effect of transfer technique instruction and physical fitness training in reducing low back pain among nurses: a cluster randomised intervention study. Ergonomics. 2008;51(10):1530–1548. doi: 10.1080/00140130802238606. [DOI] [PubMed] [Google Scholar]
- 42.Shojaei S., et al. A multidisciplinary workplace intervention for chronic low back pain among nursing assistants in Iran. Asian Spine Journal. 2017;11(3):419–426. doi: 10.4184/asj.2017.11.3.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jaromi M., et al. Back School programme for nurses has reduced low back pain levels: a randomised controlled trial. J. Clin. Nurs. 2018;27(5–6):e895–e902. doi: 10.1111/jocn.13981. [DOI] [PubMed] [Google Scholar]
- 45.Jensen L.D., et al. Prevention of low back pain in female eldercare workers: randomized controlled work site trial. Spine. 2006;31(16):1761–1769. doi: 10.1097/01.brs.0000227326.35149.38. [DOI] [PubMed] [Google Scholar]
- 46.Black T.R., et al. Effect of transfer, lifting, and repositioning (TLR) injury prevention program on musculoskeletal injury among direct care workers. J. Occup. Environ. Hyg. 2011;8(4):226–235. doi: 10.1080/15459624.2011.564110. [DOI] [PubMed] [Google Scholar]
- 47.Hartvigsen J., et al. Intensive education combined with low tech ergonomic intervention does not prevent low back pain in nurses. Occup. Environ. Med. 2005;62(1):13. doi: 10.1136/oem.2003.010843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lim H.J., et al. Evaluating repeated patient handling injuries following the implementation of a multi-factor ergonomic intervention program among health care workers. J. Saf. Res. 2011;42(3):185. doi: 10.1016/j.jsr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 49.Carta A., et al. Training in safer and healthier patient handling techniques. Br. J. Nurs. 2010;19(9):576–582. doi: 10.12968/bjon.2010.19.9.48057. [DOI] [PubMed] [Google Scholar]
- 50.Ore T. Evaluation of safety training for manual handling of people with disabilities in specialised group homes in Australia. Aust. N. Z. J. Publ. Health. 2003;27(1):64–69. doi: 10.1111/j.1467-842x.2003.tb00382.x. [DOI] [PubMed] [Google Scholar]
- 51.Johnsson C., Carlsson R., Lagerstrom M. Evaluation of training in patient handling and moving skills among hospital and home care personnel. Ergonomics. 2002;45(12):850–865. doi: 10.1080/00140130210160920. [DOI] [PubMed] [Google Scholar]
- 52.Kugler H.L., et al. Nurses sustain manual handling risk assessment behaviours six-months after a training program to move patients safely: a pre-post study. Disabil. Rehabil. 2022;45(5):927–935. doi: 10.1080/09638288.2022.2048908. [DOI] [PubMed] [Google Scholar]
- 53.Brusco N.K., et al. Mobilisation alarm triggers, response times and utilisation before and after the introduction of policy for alarm reduction or elimination: a descriptive and comparative analysis. Int. J. Nurs. Stud. 2021;117 doi: 10.1016/j.ijnurstu.2020.103769. [DOI] [PubMed] [Google Scholar]
- 54.Morris M.E., et al. Divesting from a scored hospital fall risk assessment tool (FRAT): a cluster randomized non-Inferiority trial. J. Am. Geriatr. Soc. 2021;69(9):2598–2604. doi: 10.1111/jgs.17125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haines T.P., et al. Impact of disinvestment from weekend allied health services across acute medical and surgical wards: 2 stepped-wedge cluster randomised controlled trials. PLoS Med. 2017;14(10) doi: 10.1371/journal.pmed.1002412. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.