Abstract
The prevalence of nonalcoholic fatty liver disease (NAFLD) in the United States is 38%, having increased by 50% within the past 3 decades. The estimated NAFLD prevalence among people with type 2 diabetes is 55–70%. The presence of type 2 diabetes is associated with a higher likelihood of progression of NAFLD to fibrosis development, liver transplant, and death. Cardiovascular disease is the main cause of mortality among people with NAFLD, and the risk of death is significantly higher in people with both NAFLD and type 2 diabetes. NAFLD carries high patient and economic burdens but low awareness among both the general public and health care providers. This article reviews the epidemiology of NAFLD and discusses the need for appropriate risk stratification, referral for specialty care, management of cardiometabolic risk factors, and treatment of the disease. The authors present a call to action to raise awareness of NAFLD and address its increasing burden in a systematic and efficient manner.
Nonalcoholic fatty liver disease (NAFLD) was first recognized in the 1980s, when its natural history was not entirely clear but its histological features were similar to alcoholic fatty liver disease. The main differentiating characteristics were the lack of excessive alcohol consumption and its close association with metabolic comorbidities, including type 2 diabetes, high cholesterol, hypertension, and obesity (1). In the past 4 decades, an enormous amount of research has been undertaken, providing a better understanding of this important form of chronic liver disease.
However, before continuing our discussion, it is important to acknowledge that a new name for NAFLD has been proposed. The proposed new term is “metabolic dysfunction–associated steatotic liver disease” (MASLD), which would fall under the broader category of steatotic liver disease. The name change was recommended as a way to increase awareness of the disease by decreasing perceived stigma associated with the terms “nonalcoholic” and “fatty liver.” Additionally, the “nonalcoholic” component of NAFLD was considered inappropriate when this terminology was used to describe the disease if it occurs in children or in individuals from countries or cultures in which alcohol consumption is prohibited. Given how recently the change to MASLD was proposed, additional research may be needed to determine whether MASLD is simply NAFLD by a different name or whether it is indicative of a different form of the disease. For now, the American Diabetes Association (ADA) has not adopted MASLD. Therefore, for the purpose of this article, we continue to use the term “nonalcoholic fatty liver disease” (2–4).
Our current understanding is that NAFLD is not only a complex liver disease but also part of a multisystemic disease associated with metabolic abnormalities (5–7). In this context, type 2 diabetes has a reciprocal relationship with NAFLD through which the prevalence of NAFLD is higher among people with type 2 diabetes and the incidence of type 2 diabetes is higher in people with NAFLD. In fact, the incidence of NAFLD among individuals with type 2 diabetes is estimated to be 65 cases per 1,000 person-years compared with 44 cases per 1,000 person-years among those without diabetes (8). Furthermore, the incidence of NAFLD is three times higher in people with overweight or obesity compared with those of normal weight (5,7,9–12).
Cardiovascular disease (CVD) is the leading cause of death in both people with NAFLD and those with type 2 diabetes. In people with NAFLD, extrahepatic malignancies and liver-related complications are the other top causes of death (1,5,11,13,14).
Given its close association, NAFLD has been considered the hepatic manifestation of metabolic syndrome, although hepatic steatosis in NAFLD seems to arise more from the liver’s lipid toxicity, which results from the presence of insulin resistance and/or type 2 diabetes (1,5,6). It has also been shown that the increasing components of metabolic abnormalities can promote more rapid progression of liver disease, leading to a higher risk of mortality (15). Nevertheless, the presence of NAFLD has been shown to be an independent risk factor for increased mortality (16).
Although visceral obesity is its most important risk factor, NAFLD can be present among individuals of normal weight (sometimes referred to as “lean NAFLD”) (17). Nevertheless, individuals with lean NAFLD still have underlying metabolic abnormalities such as higher rates of insulin resistance and/or type 2 diabetes (17). In fact, a large number of these individuals who are considered lean based on their BMI still have an abnormal waist circumference, suggesting visceral obesity. In this context, visceral adiposity can lead to hepatic steatosis and may be a driver of adverse outcomes in these individuals (17).
NAFLD can lead to cirrhosis, hepatocellular carcinoma (HCC), liver transplantation, and death. From the spectrum of NAFLD, patients with nonalcoholic steatohepatitis (NASH; also known as metabolic dysfunction–associated steatohepatitis) are predisposed to progressive liver disease. In this context, ∼20% of people with NASH may progress to end-stage liver disease. The presence of hepatic fibrosis, especially in the setting of type 2 diabetes, can be an important predictor of adverse outcomes. In fact, the presence of stage 2 fibrosis is a predictor of mortality (i.e., high-risk NAFLD) (13,18–24). It is important to recognize that NAFLD can progress directly to HCC without first transitioning into cirrhosis. However, the rate of HCC is significantly higher among people with cirrhosis than those without cirrhosis. Therefore, screening for NAFLD-related HCC is reserved only for people with cirrhosis (25–27).
In the past decade, NAFLD and NASH have been recognized as the leading indications for liver transplant in the United States. In fact, NASH is the top indication for women, individuals >55 years of age, and those with diabetes (28–30). Nevertheless, individuals with NAFLD/NASH have added challenges both pre- and post-transplantation given their high rate of comorbidities (e.g., obesity, diabetes, and hypertension), which not only extends their waitlist time, but also increases waitlist mortality (31). In addition, people with NASH are at higher risk for developing post-transplant diabetes, chronic kidney disease, myocardial infarction, and recurrence of NAFLD. Therefore, an extensive work-up that includes cardiology, bariatric surgery, nephrology, and nutrition consultations is needed, and strict follow-up post-transplant, with an emphasis on diet and exercise, is required, with close monitoring for post-transplant immunosuppression (31).
The following sections will present information on the burden, natural history, and outcomes of NAFLD.
Global Epidemiology
The latest estimates suggest that the period prevalence of NAFLD (2009–2019) among adults was between 23 and 32% (32,33). The wide variation of prevalence rates is the result of different measures being used to estimate prevalence. The lower rate of 23% comes from the Global Burden of Disease 2019 report, which was inclusive of 204 countries around the world (32). The higher prevalence rate is from the most recent meta-analysis (33). In fact, the prevalence of NAFLD from studies published between 2016 and 2019 was 38%, representing an increase of >50% within the past 3 decades (33). The global prevalence of NASH, which is the more progressive form of NAFLD, is between 5 and 7%, but among people with type 2 diabetes, the estimated prevalence is more than seven times higher, at 37%, and the estimated prevalence of advanced fibrosis is 17% (33,34). Additionally, the overall pooled global incidence of NAFLD for the 1994–2014 period was reported to be 48.89 per 1,000 patient-years; however, for only the 2010–2014 survey period, the pooled incidence rate was 59.11 per 1,000 patient-years (95% CI 39.64–87.26 per 1,000 patient-years), an increase of 58% from the earliest time period of 1994–2006 (33).
NAFLD is also more prevalent in males than females, but NASH seems to be more prevalent in postmenopausal females (35). Although NAFLD has been considered a disease of older adults, given the epidemics of obesity and type 2 diabetes among youth, the prevalence of NAFLD in children and young adults (ages 6–29 years) has been reported to range from 10 to 20%, representing an increase of ∼40% since the early 2000s. Here, too, NAFLD seems to be more prevalent among males and is driven primarily by obesity and hypertension (36).
Natural History
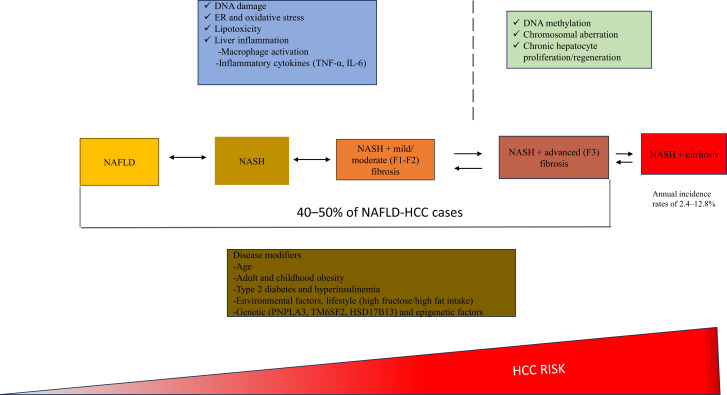
NAFLD is a complex liver disease that can progress and regress, hindering a full appreciation of its natural history (10). Nonetheless, Figure 1 presents the natural history of NAFLD, including the impact of metabolic comorbidities. Other factors can also influence the development and progression of NAFLD, including a number of genes (e.g., PNPLA, TMSF2, MBOAT7, GCKR, and HSD17B13) as well as environmental factors (e.g., lack of access to affordable nutrient-dense foods and/or safe areas to perform physical activity and areas high in air pollution), gut dysbiosis, and race/ethnicity (5–7,10).
Figure 1.
Natural history of NAFLD. F1, portal fibrosis without septa; F2, portal fibrosis with few septa; F3, numerous septa without cirrhosis; IL-6, interleukin-6; TNF-α, tumor necrosis factor-α. Reprinted with permission from Pais R, Maurel T. Natural history of NAFLD. J Clin Med 2021;10:1161.
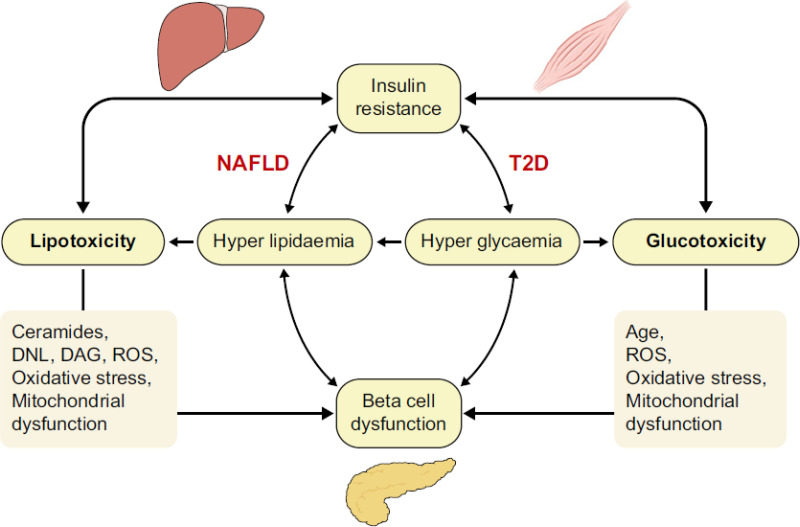
In most cases, NAFLD develops when there are alterations in glucose and lipid metabolism, as well as in the presence of insulin resistance (IR)—hence its close association with type 2 diabetes. Specifically, individuals with NAFLD and type 2 diabetes are insulin resistant at the level of the muscle, liver, and adipose tissue. These states contribute to ectopic fat accumulation, worsening of IR, lipotoxicity, impaired β-cell function, and excess free fatty acids (FFAs). The excess FFAs cause inflammation, mitochondrial dysfunction, increased oxidative stress, and uncoupled oxidative phosphorylation, which then activates a fibrogenic response in hepatic cells that can promote disease progression to NASH and cirrhosis. Chronic hyperglycemia (glucotoxicity), if present, can also add to hepatocyte dysfunction and death. Because lipotoxicity and glucotoxicity are generally both present, the combination leads to further IR and impaired insulin secretion in type 2 diabetes (Figure 2) (37,38).
Figure 2.
Relationship between lipotoxicity and glucotoxicity in the development of NAFLD. DAG, diacylglycerol; DNL, de novo lipogenesis; ROS, reactive oxygen species; T2D, type 2 diabetes. Reprinted with permission from Gastaldelli A, Cusi K. From NASH to diabetes and from diabetes to NASH: mechanisms and treatment options. JHEP Rep 2019;1:312–328.
IR and type 2 diabetes have also been shown to be associated with accelerated disease progression (38,39). In fact, a recent U.S. natural history study involving >5,000 community members with NAFLD (median follow-up of 6.4 years [range 1–23 years]) found that the presence of type 2 diabetes increased the risk of progression to cirrhosis by three times (hazard ratio 3.0, P = 0.003) (40). This study also indicated that people with NAFLD spent roughly 15 years in an NAFLD state in which 14% died of another cause and 3% progressed to cirrhosis, at which point another 8% died within the next 2 years. Individuals who entered the study with a Fibrosis-4 (FIB-4) score >1.3 at the time of diagnosis were at the highest risk of disease progression. The investigators concluded that, among adults with compensated NASH cirrhosis, the risk of progression to decompensation or death was 10% per year, and, among adults who incurred a decompensation event, the risk of progression to liver death was 32% per year. In this context, the overall probability of death was 22%, of which 26% was from cancer, 20% was from CVD, and 6% was liver-related. This risk of death was higher than the expected rate of death for a similar-aged cohort (40).
Although rates varied, these results were similar to other recently published natural history studies in which CVD and cancer were the leading causes of death (41–46). Studies have suggested that the most likely underlying mechanisms through which NAFLD increases the risk of CVD and its complications are exacerbation of hepatic and systemic IR, promotion of atherogenic dyslipidemia, induction of hypertension, and triggering of proatherogenic, procoagulant, and proinflammatory mediators (45,46).
Given the proinflammatory state associated with NAFLD, individuals with NAFLD had a higher mortality rate during the coronavirus disease 2019 (COVID-19) pandemic compared with those without NAFLD. In a single-center study of almost 5,000 inpatients with COVID-19, those with NAFLD were sicker on admission (i.e., with hypoxemia and febrile), requiring more hospital resources. Researchers determined that the independent predictors of mortality included being at high risk for fibrosis, having multiple comorbidities, being older, and having morbid obesity (47). Interestingly, in a gene-based study, people with leukemia, NAFLD, type 2 diabetes, psoriasis, or pulmonary arterial hypertension were at higher risk for adverse outcomes of COVID-19 (48).
Finally, given the association of sarcopenia with type 2 diabetes and obesity, the role of sarcopenia in people with NAFLD is now being explored (49–52). Although sarcopenia, defined as the loss of muscle mass and strength generally associated with the elderly, is highly prevalent in people with end-stage liver disease, the prevalence of noncirrhotic sarcopenia is high among those with NAFLD. The exact pathophysiological mechanisms explaining sarcopenia’s impact on NAFLD outcomes is unclear; however, the common features of both sarcopenia and NAFLD (i.e., IR, low vitamin D levels, inflammatory myokines, and physical inactivity) lead to increased proteolysis, myosteatosis, increased oxidative stress, and decreased uptake of glucose in the muscle, in turn leading to poorer outcomes (49–52). In fact, the presence of sarcopenia in people with NAFLD is linked with an almost twofold higher risk for all-cause mortality, a threefold higher risk for cardiac-related mortality, a twofold higher risk for cancer-related mortality, and an 11% higher risk for significant hepatic fibrosis. Indeed, the interaction of NAFLD and sarcopenia accounted for 55% of significant hepatic fibrosis cases (52). In this context, assessment for sarcopenia and NAFLD in people with type 2 diabetes is important for its prognostic and therapeutic implications.
Patient-Reported Outcomes, Economic Burden, and Awareness
In addition to adverse clinical outcomes, NAFLD and NASH are also associated with impairment of patient-reported outcomes (PROs) such as health-related quality of life and work productivity, which can further worsen with progression to advanced liver disease (53–56). In addition, people with NAFLD report high levels of fatigue and have higher rates of anxiety and depression compared with the general population (56,57). These factors most likely help to explain patient reports of low physical activity, lower physical functioning scores, and decreased work productivity (57,58).
Numerous economic studies from around the world have found that there is a tremendous economic burden associated with NAFLD and NASH, especially when advanced liver disease is present (12,59–64). Additionally, the presence of type 2 diabetes, CVD, and renal impairment can increase costs substantially (12,61). Furthermore, costs increase with advanced liver disease and the requirement for liver transplantation, contributing to approximate overall lifetime costs of NASH in the United States of $223 billion in 2017 (60). These costs were most likely underestimated given that they are not inclusive of lost worker productivity, an important direct cost of NAFLD. Another study suggested that NAFLD among people with type 2 diabetes in the United States can lead to a $55.8 billion 20-year cost, 65,000 liver transplants, 1.37 million cardiovascular-related deaths, and 812,000 liver-related deaths (12).
Despite the clinical, PRO, and economic burdens of NALFD, awareness of the disease remains low, not only among the general public, but also among health care providers (65,66). Addressing this gap in awareness is especially important for those involved in the care of people with type 2 diabetes who see a large number of patients at risk for progressive NAFLD.
Reasons for the low awareness of NAFLD may include a lack of appreciation of the NAFLD disease burden, as well as a perception that there is no NASH-specific treatment available. Although there are no approved pharmacological therapies for NASH with fibrosis, there are a number of interventions that can be implemented to either prevent the development of NAFLD or treat NAFLD and stop its progression to more advanced stages. These include lifestyle modification and highly effective treatments approved for the treatment of type 2 diabetes and obesity, the two most important drivers of the NAFLD-related disease burden (67).
Diagnosis and Risk Stratification of High-Risk NAFLD
Although lifestyle modification can be recommended to all people with NAFLD, specific treatment and clinical management should be recommended to those considered to have high-risk NAFLD (stage F2 or higher) (41,67).
Historically, liver biopsy was used to determine the stage of fibrosis. Given the shortcoming of liver biopsy, the use of noninvasive tests has become increasingly popular (68). The use of noninvasive tests is especially important in primary care and endocrinology practices where a large number of patients at risk for progressive NAFLD (those with type 2 diabetes or other components of metabolic syndrome) are treated. In this context, the presence of fibrosis can be determined with the use of simple serum markers such as the FIB-4 score, which can be followed by the Enhanced Liver Fibrosis assessment or vibration-controlled transient elastography to assess liver stiffness. These tests have been used to develop practical algorithms that can be implemented easily in the clinic to determine whether patients require referral to a specialist (gastroenterology or hepatology) or whether they can be managed in the primary care setting. A full discussion of these algorithms and tests is beyond the scope of this article. However, the American Association of Clinical Endocrinology and the ADA, as well as others, have developed appropriate guidelines to help clinicians in these settings (69–71).
Treatment
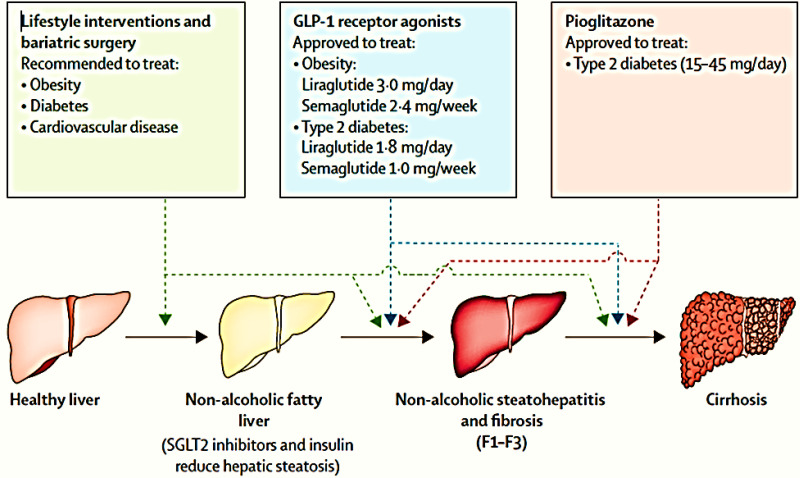
Treatment of NAFLD is summarized in Figure 3. The primary treatment goal should be to prevent the development of NAFLD by maintaining a healthy weight through the use of diet (the most commonly recognized eating pattern is one that is based on the components of the Mediterranean diet) and physical activity performed at a moderate effort for at least 150 minutes/week (67). These efforts can lower the risk of IR, type 2 diabetes, and other metabolic comorbidities (72). However, there are barriers to meeting these goals, including limited access to healthy, culturally appropriate food and a lack of safe spaces in which to perform physical activity (73–75). Therefore, efforts must continue to encourage policymakers to design and reconfigure neighborhoods and public spaces to meet these needs.
Figure 3.
Treatment of NAFLD. F1, portal fibrosis without septa; F3, numerous septa without cirrhosis. Reprinted with permission from ref. 1.
Diet
Management of NAFLD requires recognition of both modifiable factors (i.e., diet, exercise, and metabolic risk factors) and nonmodifiable factors (i.e., genetics, age, ethnicity, and sex) associated with progressive liver disease. The majority of people with NAFLD report having an unhealthy eating pattern and a lack of physical activity (76). Therefore, the first step in management of people with NAFLD is to address the modifiable risk factors with the goal of achieving a 5–10% weight loss (or 3–5% for those without overweight or obesity), which can reduce steatosis at the lower percentage of weight loss and reverse fibrosis at the higher percentage (77).
The eating pattern most commonly recognized as providing weight loss and delaying the need for antidiabetic medications is the green-Mediterranean diet, which is a lower-carbohydrate version of the Mediterranean diet that includes plenty of vegetables, poultry, and fish rather than lamb and beef, 28 g/day of walnuts, and other phenol-rich foods such as green tea and Mankai (although availability of this green aquatic plant varies by country) (78,79). For some people, benefits can be realized from other diets (e.g., low-calorie ketogenic, high-protein, anti-inflammatory, and/or whole-grain diets), as long as the principles of healthy eating are followed (79–82). Avoidance of advanced glycation end products, which are generated from high-fat and high-sugar foods, high heat–processed food and beverages, and processed and well-done red meat, is also encouraged (80–82). The consumption of three or more cups of coffee is also recommended because of its antifibrotic and antioxidant properties in the liver, while avoiding sugar-sweetened beverages, fructose-laden products, and ultra-processed foods (e.g., foods that contain hydrolyzed proteins, fructose, high-fructose corn syrup, hydrogenated oil, and cosmetic additives such as flavorings, coloring agents, and emulsifiers) (83–86).
Physical Activity
It is known that physical activity improves both hepatic and peripheral insulin sensitivity and, through associated weight loss, decreases the proinflammatory and oxidative stress markers associated with NASH while improving liver enzymes and decreasing intrahepatic lipids and potentially improving the gut microbiome (87,88). However, the majority of people with NAFLD are sedentary, and those with both NAFLD and type 2 diabetes are the most sedentary and least physically active (76). As a result, individuals with NAFLD and IR or type 2 diabetes who maintain even a short-term reduction in physical activity as assessed by step count have demonstrated deleterious effects on insulin sensitivity and hepatic steatosis (89).
Thus, engagement in physical activity is imperative for people with NAFLD and type 2 diabetes. As previously mentioned, the current goal is to engage in moderate physical activity for at least 150 minutes/week (67,90). Moderate physical activity is defined as any activity during which a person finds it somewhat difficult to carry on a conversation, and vigorous activity is any activity during which a person finds it challenging to carry on conversation (91,92). Another way to help people understand what moderate activity is involves giving a few examples, such as brisk walking, water aerobics, riding a bike on level ground or with few hills, playing doubles tennis, or pushing a lawn mower (93). The addition of resistance training has also been shown to promote a better environment for liver and cardiac health while also addressing the presence of sarcopenia (94).
Therefore, among this population, incorporating physical activity is imperative. However, people may face many barriers to incorporating exercise into their daily routine, including deconditioning resulting from sedentary behavior and the presence of more advanced liver disease or CVD. For this reason, physical activity programs should be individualized and overseen by a professional and should include an accountability component and obtainable goals to help ensure success (95,96). Although Web-based programs are showing promise, especially for people who do not have access to a workout facility, there is no large-study current research on the outcomes of these programs for people with NAFLD and type 2 diabetes, so, at this time, these Web-based programs cannot be recommended for this population (97,98).
Bariatric Surgery
The use of bariatric surgery has also been shown to be beneficial for those who fail to lose weight or maintain a weight loss through lifestyle interventions (99–102). In general, the use of bariatric surgery to lose weight has been found not only to translate into the reversal of hepatic steatosis, NASH, and fibrosis, but also to result in improved management or resolution of type 2 diabetes, dyslipidemia, and hypertension, along with reductions in cardiovascular morbidity or mortality (99–102).
Bariatric surgery procedures fall into two categories: purely restrictive (e.g., laparoscopic adjustable gastric banding and vertical sleeve gastrectomy) or a combination of restrictive and malabsorptive (Roux-en-Y gastric bypass). However, to date, there are no guidelines for the use of bariatric surgery in the treatment of people with NAFLD or those with NAFLD and type 2 diabetes.
This lack of guidelines is most likely due to the inconsistency of results reported from cross-sectional or retrospective studies, despite the positive outcomes noted (99–102). As a result, a new clinical trial (ClinicalTrials.gov identifier NCT04366999) was registered in April 2020 and is now underway to investigate the effect of bariatric surgery on NAFLD remission in people with obesity (102). The trial will include ∼150 people with obesity who will undergo one of the following surgical procedures: sleeve gastrectomy, Roux-en-Y gastric bypass, or one anastomosis gastric bypass. Prospective follow-up will occur at 3 months, 6 months, 1 year, and 2 years after surgery. At the end of the trial, a more definite approach to bariatric surgery in the treatment paradigm for people with NAFLD may be forthcoming (103).
Pharmaceutical Treatment
Management of the metabolic comorbidities associated with NAFLD is also of great importance. Such intervention could potentially help by reversing NAFLD and lowering the risk for cardiovascular-related mortality (104–107). Therefore, identifying, evaluating, and treating diabetes, hypertension, coronary artery disease, and high cholesterol are all essential in the care of people with NAFLD. In this context, the use of statins is considered safe for all patients with NAFLD except for those with decompensated cirrhosis (104–107).
More specifically, several medications used for the treatment of diabetes have shown promise in managing liver disease, including the thiazolidinedione pioglitazone, glucagon-like peptide 1 (GLP-1) receptor agonists, and sodium–glucose cotransporter 2 (SGLT2) inhibitors (108–112). GLP-1 receptor agonists are promising in that, in addition to improving glycemia, they also promote weight loss, improve upregulations of fatty acid metabolism and insulin signaling pathways, improve hepatic steatosis and histological components of NASH if present, and provide good cardiovascular protection; however, long-term studies are still needed. Although SGLT2 inhibitors are also promising for improving hepatic steatosis, liver enzyme levels, BMI, and inflammatory markers, additional studies are needed to assess their safety and side effects (e.g., hypoglycemia, ketoacidosis, and urinary tract and genital infections) (108–111). Pioglitazone has shown promise for yielding histological improvement in people with NAFLD/NASH and type 2 diabetes; however, its use requires familiarity with potential side effects (112). Additionally, there are ongoing clinical trials for medications that can either resolve NASH without furthering fibrosis, reduce fibrosis without worsening NASH, or both (113–115). At this time, none of these agents have been approved, although several are being considered for approval. In this context, the initial surrogate end points must be confirmed with long-term outcomes data (116).
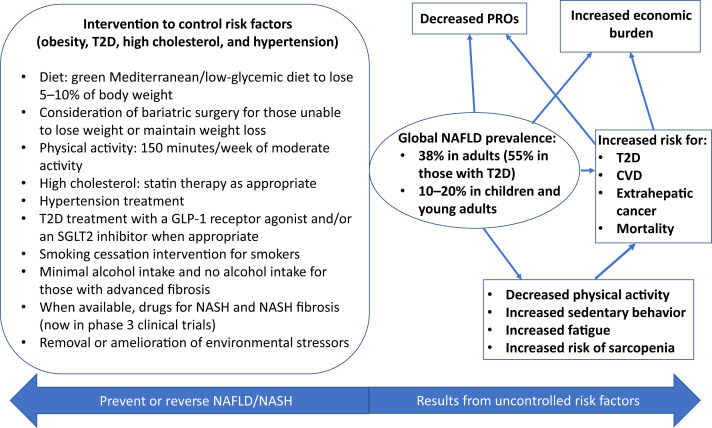
Nonetheless, interventions are currently available to help prevent or reverse NAFLD, and all stakeholders will need to work together to meet the growing burden of this disease, as summarized in Figure 4.
Figure 4.
Scope of NAFLD. T2D, type 2 diabetes.
Conclusion
NAFLD is a complex, multisystem disease that is increasing dramatically around the world in parallel with increases in the rates of type 2 diabetes and obesity. Today, more than one-third of adults and up to one-fifth of children have NAFLD. Some of these individuals have developed advanced liver disease and HCC.
Based on the sheer number of people with NAFLD, this type of liver disease is rapidly becoming the most common cause of liver mortality and is considered an indication for liver transplantation and a cause of HCC. Given its tremendous clinical, PRO, and economic burdens, NAFLD requires early recognition and aggressive intervention involving a multidisciplinary health care team to facilitate weight loss, increased physical activity, and management of cardiometabolic comorbidities. In the near future, NASH-specific drugs currently under study may also play an important role in the management of patients with NAFLD. Moving forward, multidisciplinary teams of health care professionals must work together to identify, assess, and treat people with high-risk NAFLD, while also working with community leaders and national and international policymakers to advocate for the provision of known treatments and the development of more interventions to reverse the current trends.
Article Information
Duality of Interest
Z.M.Y. has received research funds or served as a consultant to Abbvie, BMS, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, Novo Nordisk, Siemens, Terns, and Viking. No other potential conflicts of interest relevant to this article were reported.
Author Contributions
Both authors contributed equally to the study design, literature review, writing, and critical revision of the article. Z.M.Y. is the guarantor of this work and, as such, had full access to all the data included in the review and takes responsibility for the integrity and accuracy of the content.
References
- 1. Stefan N, Cusi K. A global view of the interplay between non-alcoholic fatty liver disease and diabetes. Lancet Diabetes Endocrinol 2022;10:284–296 [DOI] [PubMed] [Google Scholar]
- 2. Rinella ME, Lazarus JV, Ratziu V, et al.; NAFLD Nomenclature Consensus Group . A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol 2023;79:1542–1556 [DOI] [PubMed] [Google Scholar]
- 3. Rinella ME, Lazarus JV, Ratziu V, et al.; NAFLD Nomenclature Consensus Group . A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology 2023;78:1966–1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rinella ME, Lazarus JV, Ratziu V, et al.; NAFLD Nomenclature Consensus Group . A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Ann Hepatol 2024;29:101133. [DOI] [PubMed] [Google Scholar]
- 5. Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut 2017;66:1138–1153 [DOI] [PubMed] [Google Scholar]
- 6. Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol 2013;10:330–344 [DOI] [PubMed] [Google Scholar]
- 7. Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol 2015;62(Suppl.):S47–S64 [DOI] [PubMed] [Google Scholar]
- 8. Younossi ZM, Gramlich T, Matteoni CA, Boparai N, McCullough AJ. Nonalcoholic fatty liver disease in patients with type 2 diabetes. Clin Gastroenterol Hepatol 2004;2:262–265 [DOI] [PubMed] [Google Scholar]
- 9. Björkström K, Stål P, Hultcrantz R, Hagström H. Histologic scores for fat and fibrosis associate with development of type 2 diabetes in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2017;15:1461–1468 [DOI] [PubMed] [Google Scholar]
- 10. Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med 2011;43:617–649 [DOI] [PubMed] [Google Scholar]
- 11. Park SK, Seo MH, Shin HC, Ryoo JH. Clinical availability of nonalcoholic fatty liver disease as an early predictor of type 2 diabetes mellitus in Korean men: 5-year prospective cohort study. Hepatology 2013;57:1378–1383 [DOI] [PubMed] [Google Scholar]
- 12. Younossi ZM, Tampi RP, Racila A, et al. Economic and clinical burden of nonalcoholic steatohepatitis in patients with type 2 diabetes in the U.S. Diabetes Care 2020;43:283–289 [DOI] [PubMed] [Google Scholar]
- 13. Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015;149:389–97.e10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Haflidadottir S, Jonasson JG, Norland H, et al. Long-term follow-up and liver-related death rate in patients with non-alcoholic and alcoholic related fatty liver disease. BMC Gastroenterol 2014;14:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Golabi P, Otgonsuren M, de Avila L, Sayiner M, Rafiq N, Younossi ZM. Components of metabolic syndrome increase the risk of mortality in nonalcoholic fatty liver disease (NAFLD). Medicine (Baltimore) 2018;97:e0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. de Avila L, Henry L, Paik JM, Ijaz N, Weinstein AA, Younossi ZM. Nonalcoholic fatty liver disease is independently associated with higher all-cause and cause-specific mortality. Clin Gastroenterol Hepatol 2023;21:2588–2596.e3 [DOI] [PubMed] [Google Scholar]
- 17. Golabi P, Paik JM, Arshad T, Younossi Y, Mishra A, Younossi ZM. Mortality of NAFLD according to the body composition and presence of metabolic abnormalities. Hepatol Commun 2020;4:1136–1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Taylor RS, Taylor RJ, Bayliss S, et al. Association between fibrosis stage and outcomes of patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Gastroenterology 2020;158:1611–1625.e12 [DOI] [PubMed] [Google Scholar]
- 19. Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology 2018;155:443–457.e17 [DOI] [PubMed] [Google Scholar]
- 20. Hagström H, Nasr P, Ekstedt M, et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol 2017;67:1265–1273 [DOI] [PubMed] [Google Scholar]
- 21. Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology 2017;65:1557–1565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Canbay A, Kachru N, Haas JS, Sowa JP, Meise D, Ozbay AB. Patterns and predictors of mortality and disease progression among patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther 2020;52:1185–1194 [DOI] [PubMed] [Google Scholar]
- 23. Younossi ZM, Stepanova M, Rafiq N, et al. Nonalcoholic steatofibrosis independently predicts mortality in nonalcoholic fatty liver disease. Hepatol Commun 2017;1:421–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ekstedt M, Hagström H, Nasr P, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 2015;61:1547–1554 [DOI] [PubMed] [Google Scholar]
- 25. Kanwal F, Kramer JR, Mapakshi S, et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology 2018;155:1828–1837.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stine JG, Wentworth BJ, Zimmet A, et al. Systematic review with meta-analysis: risk of hepatocellular carcinoma in non-alcoholic steatohepatitis without cirrhosis compared to other liver diseases. Aliment Pharmacol Ther 2018;48:696–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tan DJH, Ng CH, Lin SY, et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. Lancet Oncol 2022;23:521–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Younossi ZM, Harring M, Younossi Y, Ong JP, Alqahtani SA, Stepanova M. The impact of NASH to liver transplantations with hepatocellular carcinoma in the United States. Clin Gastroenterol Hepatol 2022;20:2915–2917.e1 [DOI] [PubMed] [Google Scholar]
- 29. Noureddin M, Vipani A, Bresee C, et al. NASH leading cause of liver transplant in women: updated analysis of indications for liver transplant and ethnic and gender variances. Am J Gastroenterol 2018;113:1649–1659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hoehn RS, Singhal A, Wima K, et al. Effect of pretransplant diabetes on short-term outcomes after liver transplantation: a national cohort study. Liver Int 2015;35:1902–1909 [DOI] [PubMed] [Google Scholar]
- 31. Steggerda JA, Mahendraraj K, Todo T, Noureddin M. Clinical considerations in the management of non-alcoholic steatohepatitis cirrhosis pre- and post-transplant: a multi-system challenge. World J Gastroenterol 2020;26:4018–4035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Paik JM, Henry L, Younossi Y, Ong J, Alqahtani S, Younossi ZM. The burden of nonalcoholic fatty liver disease (NAFLD) is rapidly growing in every region of the world from 1990 to 2019. Hepatol Commun 2023;7:e0251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology 2023;77:1335–1347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Younossi ZM, Golabi P, de Avila L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol 2019;71:793–801 [DOI] [PubMed] [Google Scholar]
- 35. Ballestri S, Nascimbeni F, Baldelli E, Marrazzo A, Romagnoli D, Lonardo A. NAFLD as a sexual dimorphic disease: role of gender and reproductive status in the development and progression of nonalcoholic fatty liver disease and inherent cardiovascular risk. Adv Ther 2017;34:1291–1326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Arshad T, Paik JM, Biswas R, Alqahtani SA, Henry L, Younossi ZM. Nonalcoholic fatty liver disease prevalence trends among adolescents and young adults in the United States, 2007–2016. Hepatol Commun 2021;5:1676–1688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol 2014;2:901–910 [DOI] [PubMed] [Google Scholar]
- 38. Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients 2013;5:1544–1560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hu M, Phan F, Bourron O, Ferré P, Foufelle F. Steatosis and NASH in type 2 diabetes. Biochimie 2017;143:37–41 [DOI] [PubMed] [Google Scholar]
- 40. Allen AM, Therneau TM, Ahmed OT, et al. Clinical course of non-alcoholic fatty liver disease and the implications for clinical trial design. J Hepatol 2022;77:1237–1245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Loomba R, Wong R, Fraysse J, et al. Nonalcoholic fatty liver disease progression rates to cirrhosis and progression of cirrhosis to decompensation and mortality: a real world analysis of Medicare data. Aliment Pharmacol Ther 2020;51:1149–1159 [DOI] [PubMed] [Google Scholar]
- 42. Sanyal AJ, Van Natta ML, Clark J, et al.; NASH Clinical Research Network (CRN) . Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N Engl J Med 2021;385:1559–1569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nyberg LM, Cheetham TC, Patton HM, et al. The natural history of NAFLD, a community-based study at a large health care delivery system in the United States. Hepatol Commun 2020;5:83–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sanyal AJ, Harrison SA, Ratziu V, et al. The natural history of advanced fibrosis due to nonalcoholic steatohepatitis: data from the simtuzumab trials. Hepatology 2019;70:1913–1927 [DOI] [PubMed] [Google Scholar]
- 45. Targher G, Corey KE, Byrne CD. NAFLD, and cardiovascular and cardiac diseases: factors influencing risk, prediction and treatment. Diabetes Metab 2021;47:101215. [DOI] [PubMed] [Google Scholar]
- 46. Byrne CD, Targher G. Non-alcoholic fatty liver disease-related risk of cardiovascular disease and other cardiac complications. Diabetes Obes Metab 2022;24(Suppl. 2):28–43 [DOI] [PubMed] [Google Scholar]
- 47. Younossi ZM, Stepanova M, Lam B, et al. Independent predictors of mortality among patients with NAFLD hospitalized with COVID-19 infection. Hepatol Commun 2022;6:3062–3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Singh MK, Mobeen A, Chandra A, Joshi S, Ramachandran S. A meta-analysis of comorbidities in COVID-19: which diseases increase the susceptibility of SARS-CoV-2 infection? Comput Biol Med 2021;130:104219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lee YH, Jung KS, Kim SU, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: nationwide surveys (KNHANES 2008-2011). J Hepatol 2015;63:486–493 [DOI] [PubMed] [Google Scholar]
- 50. Li AA, Kim D, Ahmed A. Association of sarcopenia and NAFLD: an overview. Clin Liver Dis (Hoboken) 2020;16:73–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Golabi P, Gerber L, Paik JM, Deshpande R, de Avila L, Younossi ZM. Contribution of sarcopenia and physical inactivity to mortality in people with non-alcoholic fatty liver disease. JHEP Rep 2020;2:100171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Harring M, Golabi P, Paik JM, et al. Sarcopenia among patients with nonalcoholic fatty liver disease (NAFLD) is associated with advanced fibrosis. Clin Gastroenterol Hepatol 2023;21:2876–2888.e5 [DOI] [PubMed] [Google Scholar]
- 53. Younossi Z, Aggarwal P, Shrestha I, et al. The burden of non-alcoholic steatohepatitis: a systematic review of health-related quality of life and patient-reported outcomes. JHEP Rep 2022;4:100525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Younossi ZM, Stepanova M, Anstee QM, et al. Reduced patient-reported outcome scores associate with level of fibrosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol 2019;17:2552–2560.e10 [DOI] [PubMed] [Google Scholar]
- 55. Younossi ZM, Yilmaz Y, Yu ML, et al.; Global NASH Council . Clinical and patient-reported outcomes from patients with nonalcoholic fatty liver disease across the world: data from the Global Nonalcoholic Steatohepatitis (NASH)/Non-Alcoholic Fatty Liver Disease (NAFLD) Registry. Clin Gastroenterol Hepatol 2022;20:2296–2306.e6 [DOI] [PubMed] [Google Scholar]
- 56. Younossi ZM, Wong VW, Anstee QM, et al. Fatigue and pruritus in patients with advanced fibrosis due to nonalcoholic steatohepatitis: the impact on patient-reported outcomes. Hepatol Commun 2020;4:1637–1650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Weinstein AA, Kallman Price J, Stepanova M, et al. Depression in patients with nonalcoholic fatty liver disease and chronic viral hepatitis B and C. Psychosomatics 2011;52:127–132 [DOI] [PubMed] [Google Scholar]
- 58. Weinstein AA, De Avila L, Kannan S, et al. Interrelationship between physical activity and depression in nonalcoholic fatty liver disease. World J Hepatol 2022;14:612–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology 2016;64:1577–1586 [DOI] [PubMed] [Google Scholar]
- 60. Younossi ZM, Tampi R, Priyadarshini M, Nader F, Younossi IM, Racila A. Burden of illness and economic model for patients with nonalcoholic steatohepatitis in the United States. Hepatology 2019;69:564–572 [DOI] [PubMed] [Google Scholar]
- 61. Noureddin M, Jones C, Alkhouri N, Gomez EV, Dieterich DT; NASHNET . Screening for nonalcoholic fatty liver disease in persons with type 2 diabetes in the United States is cost-effective: a comprehensive cost-utility analysis. Gastroenterology 2020;159:1985–1987.e4 [DOI] [PubMed] [Google Scholar]
- 62. Sayiner M, Arshad T, Golabi P, Paik J, Farhat F, Younossi ZM. Extrahepatic manifestations and healthcare expenditures of non-alcoholic fatty liver disease in the Medicare population. Hepatol Int 2020;14:556–566 [DOI] [PubMed] [Google Scholar]
- 63. Nguyen AL, Park H, Nguyen P, Sheen E, Kim YA, Nguyen MH. Rising inpatient encounters and economic burden for patients with nonalcoholic fatty liver disease in the USA. Dig Dis Sci 2019;64:698–707 [DOI] [PubMed] [Google Scholar]
- 64. Younossi ZM, Paik JM, Henry L, et al. The growing economic and clinical burden of nonalcoholic steatohepatitis (NASH) in the United States. J Clin Exp Hepatol 2023;13:454–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Alqahtani SA, Paik JM, Biswas R, Arshad T, Henry L, Younossi ZM. Poor awareness of liver disease among adults with NAFLD in the United States. Hepatol Commun 2021;5:1833–1847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Younossi ZM, Ong JP, Takahashi H, et al.; Global Nonalcoholic Steatohepatitis Council . A global survey of physicians knowledge about nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2022;20:e1456–e1468 [DOI] [PubMed] [Google Scholar]
- 67. Younossi ZM, Zelber-Sagi S, Henry L, Gerber LH. Lifestyle interventions in nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol 2023;20:708–722 [DOI] [PubMed] [Google Scholar]
- 68. Anstee QM, Castera L, Loomba R. Impact of non-invasive biomarkers on hepatology practice: past, present and future. J Hepatol 2022; 76:1362–1378 [DOI] [PubMed] [Google Scholar]
- 69. Kanwal F, Shubrook JH, Adams LA, et al. Clinical care pathway for the risk stratification and management of patients with nonalcoholic fatty liver disease. Gastroenterology 2021;161:1657–1669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Cusi K, Isaacs S, Barb D, et al. American Association of Clinical Endocrinology clinical practice guideline for the diagnosis and management of nonalcoholic fatty liver disease in primary care and endocrinology clinical settings: co-sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract 2022;28:528–562 [DOI] [PubMed] [Google Scholar]
- 71. Srivastava A, Gailer R, Tanwar S, et al. Prospective evaluation of a primary care referral pathway for patients with non-alcoholic fatty liver disease. J Hepatol 2019;71:371–378 [DOI] [PubMed] [Google Scholar]
- 72. Quattrocchi E, Goldberg T, Marzella N. Management of type 2 diabetes: consensus of diabetes organizations. Drugs Context 2020;9:212607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Giammarino AM, Qiu H, Bulsara K, et al. Community socioeconomic deprivation predicts nonalcoholic steatohepatitis. Hepatol Commun 2022;6:550–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Hu MD, Lawrence KG, Bodkin MR, Kwok RK, Engel LS, Sandler DP. Neighborhood deprivation, obesity, and diabetes in residents of the US Gulf Coast. Am J Epidemiol 2021;190:295–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Tatulashvili S, Fagherazzi G, Dow C, Cohen R, Fosse S, Bihan H. Socioeconomic inequalities and type 2 diabetes complications: a systematic review. Diabetes Metab 2020;46:89–99 [DOI] [PubMed] [Google Scholar]
- 76. Gerber L, Otgonsuren M, Mishra A, et al. Non-alcoholic fatty liver disease (NAFLD) is associated with low level of physical activity: a population-based study. Aliment Pharmacol Ther 2012;36:772–781 [DOI] [PubMed] [Google Scholar]
- 77. Koutoukidis DA, Koshiaris C, Henry JA, et al. The effect of the magnitude of weight loss on non-alcoholic fatty liver disease: a systematic review and meta-analysis. Metabolism 2021;115:154455. [DOI] [PubMed] [Google Scholar]
- 78. Yaskolka Meir A, Rinott E, Tsaban G, et al. Effect of green-Mediterranean diet on intrahepatic fat: the DIRECT PLUS randomised controlled trial. Gut 2021;70:2085–2095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Zelber-Sagi S, Grinshpan LS, Ivancovsky-Wajcman D, Goldenshluger A, Gepner Y. One size does not fit all: practical, personal tailoring of the diet to NAFLD patients. Liver Int 2022;42:1731–1750 [DOI] [PubMed] [Google Scholar]
- 80. Kosmalski M, Frankowski R, Ziółkowska S, Różycka-Kosmalska M, Pietras T. What’s new in the treatment of non-alcoholic fatty liver disease (NAFLD). J Clin Med 2023;12:1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. BDA: The Association of U.K. Dieticians . Practice-based evidence in nutrition (PEN). Available from https://www.bda.uk.com/practice-and-education/practice-based-evidence-in-nutrition-pen.html. Accessed 23 October 2023
- 82. Ivancovsky-Wajcman D, Zelber-Sagi S, Fliss Isakov N, et al. Serum soluble receptor for AGE (sRAGE) levels are associated with unhealthy lifestyle and nonalcoholic fatty liver disease. Clin Transl Gastroenterol 2019;10:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Chen YP, Lu FB, Hu YB, Xu LM, Zheng MH, Hu ED. A systematic review and a dose-response meta-analysis of coffee dose and nonalcoholic fatty liver disease. Clin Nutr 2019;38:2552–2557 [DOI] [PubMed] [Google Scholar]
- 84. Salomone F, Ivancovsky-Wajcman D, Fliss-Isakov N, et al. Higher phenolic acid intake independently associates with lower prevalence of insulin resistance and non-alcoholic fatty liver disease. JHEP Rep 2020;2:100069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Zhang S, Gu Y, Bian S, et al. Soft drink consumption and risk of nonalcoholic fatty liver disease: results from the Tianjin Chronic Low-Grade Systemic Inflammation and Health (TCLSIH) cohort study. Am J Clin Nutr 2021;113:1265–1274 [DOI] [PubMed] [Google Scholar]
- 86. Schwarz J-M, Noworolski SM, Erkin-Cakmak A, et al. Effects of dietary fructose restriction on liver fat, de novo lipogenesis, and insulin kinetics in children with obesity. Gastroenterology 2017;153:743–752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Hashida R, Kawaguchi T, Bekki M, et al. Aerobic vs. resistance exercise in non-alcoholic fatty liver disease: a systematic review. J Hepatol 2017;66:142–152 [DOI] [PubMed] [Google Scholar]
- 88. Alkhouri N, Poordad F, Lawitz E. Management of nonalcoholic fatty liver disease: lessons learned from type 2 diabetes. Hepatol Commun 2018;2:778–785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Bowden Davies KA, Pickles S, Sprung VS, et al. Reduced physical activity in young and older adults: metabolic and musculoskeletal implications. Ther Adv Endocrinol Metab 2019;10:2042018819888824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Younossi ZM, Paik JM, Golabi P, Younossi Y, Henry L, Nader F. The impact of fatigue on mortality of patients with non-alcoholic fatty liver disease: data from National Health and Nutrition Examination Survey 2005–2010 and 2017–2018. Liver Int 2022;42:2646–2661 [DOI] [PubMed] [Google Scholar]
- 91. Reed JL, Pipe AL. The talk test: a useful tool for prescribing and monitoring exercise intensity. Curr Opin Cardiol 2014;29:475–480 [DOI] [PubMed] [Google Scholar]
- 92. Creemers N, Foster C, Porcari JP, Cress ML, De Koning JJ. The physiological mechanism behind the talk test. Kinesiology 2017;49:3–8 [Google Scholar]
- 93. Centers for Disease Control and Prevention . How much physical activity do adults need? Available from https://www.cdc.gov/physicalactivity/basics/adults/index.htm. Accessed 23 October 2023
- 94. Hallsworth K, Adams LA. Lifestyle modification in NAFLD/NASH: facts and figures. JHEP Rep 2019;1:468–479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Nguyen VH, Yeo YH, Zou B, et al. Discrepancies between actual weight, weight perception and weight loss intention amongst persons with NAFLD. J Intern Med 2021;289:840–850 [DOI] [PubMed] [Google Scholar]
- 96. Keating SE, Adams LA. Exercise in NAFLD: just do it. J Hepatol 2016;65:671–673 [DOI] [PubMed] [Google Scholar]
- 97. Pfirrmann D, Huber Y, Schattenberg JM, Simon P. Web-based exercise as an effective complementary treatment for patients with nonalcoholic fatty liver disease: intervention study. J Med Internet Res 2019;21:e11250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Motz V, Faust A, Dahmus J, Stern B, Soriano C, Stine JG. Utilization of a directly supervised telehealth-based exercise training program in patients with nonalcoholic steatohepatitis: feasibility study. JMIR Form Res 2021;5:e30239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Aminian A, Al-Kurd A, Wilson R, et al. Association of bariatric surgery with major adverse liver and cardiovascular outcomes in patients with biopsy-proven nonalcoholic steatohepatitis. JAMA 2021;326:2031–2042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology 2015;149:379–388; quiz e15–e16 [DOI] [PubMed] [Google Scholar]
- 101. Chauhan M, Singh K, Thuluvath PJ. Bariatric surgery in NAFLD. Dig Dis Sci 2022;67:408–422 [DOI] [PubMed] [Google Scholar]
- 102. Wei L, Li M, Zeng N, et al. Bariatric surgery for non-alcoholic fatty liver disease in individuals with obesity (Base-NAFLD): protocol of a prospective multicenter observational follow-up study. BMC Surg 2021;21:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. ClinicalTrials.gov . Bariatric surgery effect nonalcoholic fatty liver disease. Available from https://classic.clinicaltrials.gov/ct2/show/NCT04366999. Accessed 18 August 2023
- 104. Neuschwander-Tetri BA. Therapeutic landscape for NAFLD in 2020. Gastroenterology 2020;158:1984–1998.e3 [DOI] [PubMed] [Google Scholar]
- 105. Ciardullo S, Perseghin G. Statin use is associated with lower prevalence of advanced liver fibrosis in patients with type 2 diabetes. Metabolism 2021;121:154752. [DOI] [PubMed] [Google Scholar]
- 106. Doumas M, Imprialos K, Dimakopoulou A, Stavropoulos K, Binas A, Athyros VG. The role of statins in the management of nonalcoholic fatty liver disease. Curr Pharm Des 2018;24:4587–4592 [DOI] [PubMed] [Google Scholar]
- 107. Rong L, Zou J, Ran W, et al. Advancements in the treatment of non-alcoholic fatty liver disease (NAFLD). Front Endocrinol (Lausanne) 2023;13:1087260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Cuthbertson DJ, Irwin A, Gardner CJ, et al. Improved glycaemia correlates with liver fat reduction in obese, type 2 diabetes, patients given glucagon-like peptide-1 (GLP-1) receptor agonists. PLoS One 2012;7:e50117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Dhir G, Cusi K. Glucagon like peptide-1 receptor agonists for the management of obesity and non-alcoholic fatty liver disease: a novel therapeutic option. J Investig Med 2018;66:7–10 [DOI] [PubMed] [Google Scholar]
- 110. Gupta NA, Mells J, Dunham RM, et al. Glucagon-like peptide-1 receptor is present on human hepatocytes and has a direct role in decreasing hepatic steatosis in vitro by modulating elements of the insulin signaling pathway. Hepatology 2010;51:1584–1592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Armstrong MJ, Gaunt P, Aithal GP, et al.; LEAN trial team . Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet 2016;387:679–690 [DOI] [PubMed] [Google Scholar]
- 112. Della Pepa G, Russo M, Vitale M, et al. Pioglitazone even at low dosage improves NAFLD in type 2 diabetes: clinical and pathophysiological insights from a subgroup of the TOSCA.IT randomised trial. Diabetes Res Clin Pract 2021;178:108984. [DOI] [PubMed] [Google Scholar]
- 113. Loomba R, Noureddin M, Kowdley KV, et al.; for the ATLAS Investigators . Combination therapies including cilofexor and firsocostat for bridging fibrosis and cirrhosis attributable to NASH. Hepatology 2021;73:625–643 [DOI] [PubMed] [Google Scholar]
- 114. Albhaisi SAM, Sanyal AJ. New drugs for NASH. Liver Int 2021; 41(Suppl. 1):112–118 [DOI] [PubMed] [Google Scholar]
- 115. Cardoso AC, de Figueiredo-Mendes C, Villela-Nogueira CA, Sanyal AJ. New drugs for non-alcoholic steatohepatitis. Liver Int 2020;40(Suppl. 1):96–101 [DOI] [PubMed] [Google Scholar]
- 116. Rinella ME, Tacke F, Sanyal AJ; Participants of the AASLD/EASL Workshop . Report on the AASLD/EASL joint workshop on clinical trial endpoints in NAFLD. Hepatology 2019;70:1424–1436 [DOI] [PubMed] [Google Scholar]