Summary
Liver tumors account for approximately 2% of all pediatric malignancies. Children with advanced stages of hepatoblastoma (HB) are cured only 50–70% of the time while children with advanced hepatocellular carcinoma (HCC) have a <20% 5-year overall survival. This scoping review was performed to highlight the paucity of rigorous, reliable data guiding the management of relapsed pediatric HB or HCC. When these patients are enrolled on prospective trials, the trials are often histology-agnostic, exclude patients less than a year of age, lack a liquid formulary of the drug under study, exclude recipients of a solid organ transplant, and enroll only 1–2 patients limiting the ability to deduce efficacious regimens for current use or future study. We highlight the creation of a global pediatric consortium intended to source retrospective relapse data from over 100 institutions spanning 4 continents. The data collected from this effort will inform future relapse trials.
Keywords: Review, Pediatric, Relapse, Hepatoblastoma, Carcinoma, Registry
Research in context.
Evidence before this study
Relapse disease characteristics and salvage therapies are vastly under-reported and under-studied for pediatric patients with liver tumors due to the rarity of these diseases. While it is estimated that 25% of patients relapse, 97% of published studies report on cohorts of less than 10 patients receiving a particular therapy.
Added value of this study
This scoping review was undertaken to compile all published literature describing agents trialed for relapsed or refractory pediatric HB or HCC. We demonstrate that there are no available studies properly powered or randomized to identify or conclude treatment efficacy.
Implications of all the available evidence
The RELIVE consortium leads an international collaborative effort intended to address these limitations and collect comprehensive data on over 300 patients treated for relapsed/refractory pediatric liver tumors.
Introduction
Liver tumors comprise approximately 1–2% of all pediatric malignancies occurring in children under the age of 18 years.1 Hepatoblastoma (HB) accounts for two-thirds of these tumors. The risk for developing HB is perceived to be multifactorial with low birth weight cited as the most frequently associated cause. Overall incidence has been increasing potentially related to the improved survival of premature infants.1,2 Hepatocellular carcinoma (HCC) is the second most commonly occurring pediatric primary hepatic neoplasm. While greater than 80% of HCC cases in adults arise in the context of cirrhotic liver disease, cirrhosis is uncommon in pediatric HCC (<20%),3 with most pediatric HCC tumors occurring de novo within a structurally and functionally normal liver.
It is estimated that approximately 10–20% of patients diagnosed with HB will relapse. Generally, risk for relapse is related to the extent of disease at diagnosis which likely reflects disease biology.4 The recently concluded Children’s Oncology Group trial COG AHEP0731 (NCT00980460) demonstrated that patients with high-risk disease, denoted by the presence of metastases at diagnosis, relapse approximately 50% of the time.5 A recently concluded trial in Japan (JPLT-2) identified that patients with a poor upfront response to chemotherapy tend to have poor outcomes independent of treatment intensification.6 In a recent Epithelial Liver Tumor Study Group (SIOPEL) clinical trial (SIOPEL4), patients with either PRETEXT IV disease (disease involving all four quadrants of the liver) or metastases, were estimated to progress or relapse nearly 30% of the time, the lowest rate yet reported suggesting the best performing chemotherapy regimen studied to-date.7 Patients with low-risk disease at diagnosis, tend to have lower rates of recurrence in the 10–20% range.4,8,9
The success of salvage therapy depends upon the nature of relapse (site and disease extent), the prior chemotherapeutic agents received, resectability of the recurrence site, end-organ dysfunction from disease or chemotherapy-related toxicities and underlying comorbid illnesses. Currently reported salvage rates are 50% or less for patients with HB, taking into account the factors noted above.4 For reference, nearly 75% of pediatric patients with HCC present with advanced disease, rarely achieve remission, and have a dismal prognosis with a <20% 5-year overall survival. These patients are rarely cured upon disease recurrence.10,11
There is no standard treatment approach for relapsed HB and HCC; there is a paucity of literature guiding the management of pediatric patients with relapsed/refractory HB, and even fewer publications detailing novel or promising agents for relapsed/refractory pediatric HCC. When pediatric patients with relapsed/refractory liver tumors are enrolled on prospective trials, these are often histology-agnostic basket trials which exclude patients less than a year of age, lack a liquid formulary of the drug under study, and are available at limited sites.12,13 In addition, most new drug trials prohibit patients who have previously undergone a solid organ transplant, limiting access to new agents for some pediatric patients with liver tumors who required a liver transplant for local control.
This scoping review was initiated to perform an in-depth analysis of the existing data on systemic agents utilized to treat pediatric patients with relapsed/refractory HB, recognizing that there is virtually no data guiding the treatment of relapsed/refractory pediatric HCC. Anticipating the need for a mechanism to collect more reliable data, the RELIVE consortium was conceived in parallel with this scoping review during the 2019 International Society of Pediatric Oncology Europe (SIOPE/SIOPEL) meeting in Prague, Czech Republic. The RELIVE registry was designed to utilize the international infrastructure created for COG AHEP1531/PHITT, an open international trial anticipated to enroll up to 1200 pediatric patients with newly diagnosed HB or HCC, to create a centralized data repository for the collection of granular data surrounding the natural history, treatments, and outcomes of pediatric patients with relapsed/refractory liver tumors.
Methods
Search strategy and selection criteria
The current understanding of relapsed/refractory HB or HCC is largely based on individual experience and personal communication, published small series, case-reports, or outcomes from single patients enrolled on prospective basket trials for investigational agents. Given these limitations, it is difficult to adequately conclude true drug efficacy and reliable outcomes. A thorough analysis of the existing literature for pediatric patients undergoing treatment for relapsed/refractory HB or HCC was conducted (Table 1, Supplement Table S1, Supplement Figure S1). Data for this review were first identified by performing a citation update for “relapse” and “hepatoblastoma” from two comprehensive articles published by Trobaugh-Lotrario et al. on therapies for relapsed HB. These citations were then cross-referenced with a PubMed database search from 1989 to 2023 with expanded criteria to include “relapse” and “pediatric HCC.” Reports were excluded if chemotherapy details were absent, if no chemotherapy was documented as given, or if disease was resected prior to receipt of relapse therapy. The Children’s Oncology Group bibliography report was then referenced with studies excluded for the reasons noted above, if non-disease applicable, or if chemotherapy was provided in the upfront settling only (Supplement, PRISMA).
Table 1.
Literature documenting response, by drug, for patients with relapsed or refractory HB or HCC.
| Treatment | Number of patients | Reported response | Reference | Quality rating |
|---|---|---|---|---|
| Reponses | ||||
| Doxorubicin-containing | RECIST or Descriptive response | |||
| Doxorubicin (often administered with cisplatin) | 36 HB | 13 PR | Malogolowkin, 200814 | 3 |
| Irinotecan-containing | ||||
| Irinotecan | 1 HB | 1 Prolonged SD in HB; 1 decreased AFP in HB, 1 in HCC | Blaney, 200115 | 2 |
| Irinotecan | 3 HB | 3 decreased AFP; 1 of the 3 with decreased tumor size | Katzenstein, 200216 | 4 |
| Irinotecan | 1 HB | Normalization of AFP | Palmer, 200317 | 5 |
| Irinotecan | 5 HB | 1 SD | Vassal, 200318 | 2 |
| Irinotecan | 1 HB | 1 Decreased AFP, decreased tumor size | Ijichi, 200619 | 5 |
| Irinotecan | 8 HB, 3 HCC | 1 CR (HB) | Bomgaars, 200720 | 2 |
| VCR/irinotecan/tem | 4 HB, 1 HCC | 3 SD (HB); 2 PD (1 HB, 1 HCC) | McKnall-Knapp, 201021 | 2 |
| Irinotecan | 1 HB | 1 CR | Qayed, 201022 | 4 |
| VCR/irinotecan | 1 HB | 1 PR | Qayed, 201022 | 4 |
| VCR/irinotecan/tem | 3 HB | 1 SD then PD | Wagner, 201023 | 2 |
| Irinotecan | 23 HB | 6 PR; 11 SD; 6 PD | Zsiros, 201224 | 2 |
| Temsirolimus, irinotecan/tem | 2 HB | 1 “objective response” | Bagatell, 201425 | 2 |
| VCR/irinotecan | 7 HB | 4 PR; 2 SD; 1 PD | Zhang, 201526 | 2 |
| VCR/irinotecan | 1 HB | 1 PR | Powers, 201927 | 5 |
| Irinotecan/sorafenib | 4 HB, 2 HCC | 1 PR and 3 with PD (HB); 1 PR and 1 SD (HCC); all with previous receipt of irinotecan | Keino, 202028 | 2 |
| Platinum/etoposide-containing | ||||
| Carbo/etop | 1 HB | Decreased size of primary; pulm clearance | Lockwood, 199329 | 5 |
| Ifos/cisplatin/etop | 1 HB | 1 CR | Van Hoff, 199530 | 2 |
| Carbo/etop | 12 HB | 1 CR; 5 PR; 1 SD; 5 PD | Fuchs, 199931 | 2 |
| Ifos/carbo/etop | 1 HB | Decreased AFP | Katzenstein, 200216 | 4 |
| Ifos/carbo/etop | 1 HB | 1 NR | Matsunaga, 200332 | 4 |
| CTX/etop/cisplatin/doxo | 1 HB | 1 NR | Matsunaga, 200332 | 4 |
| Melphalan/etop/carbo | 2 HB | 2 NR | Matsunaga, 200332 | 4 |
| Carbo/doxo/etop | 1 HB | 1 NR | Matsunaga, 200332 | 4 |
| Ifos/carbo/etop | 2 HB | 1 SD; 1 PD | Loss, 200433 | 2 |
| Ifos/carbo/etop | 1 HB | Transient decrease in AFP | Qayed, 201022 | 4 |
| Carbo/ifos/doxo/etop | 1 HB | 1 NR | Miyamura, 201134 | 5 |
| Ifos/carbo/etop | 1 HB | 1 CR | Natarajan, 202035 | 5 |
| Ifos/carbo/etop | 1 HB | Not well documented; DOD | Hou, 202136 | 4 |
| VCR/carbo/5FU (1 with carbo/etop, 2 with ifos/carbo/etop, 1 with VCR/CTX/5FU) | 4 HB | Not well documented; ultimately NED | Hou, 202136 | 4 |
| Targeted therapy | ||||
| GPC-3 vaccine | 7 HB (2 with image evaluable disease) | Not well documented; 2 NE | Tsuchiya, 201737 | 2 |
| Other | ||||
| Thiotepa/melphalan (with autologous stem cell rescue) | 4 | 3 CR, 1 PR | Hara, 199838 | 4 |
Quality rating key: 1) Properly powered and conducted randomized clinical trial or scoping review with meta-analysis; 2) Well-designed controlled trial without randomization or prospective comparative cohort trial; 3) Case-control studies or retrospective cohort study; 4) Case series with or without intervention or cross-sectional study; 5) Opinion of respected authorities or case reports.
AFP, alpha-fetoprotein; ANED, alive no evidence of disease; CR, complete response; DOD, died of disease; HB, hepatoblastoma; NE, non-evaluable; NED, no evidence of disease; NR, no response; PD, progressive disease; PR, partial response; RT, radiation therapy; SD, stable disease; Ifos, ifosfamide; carbo, carboplatin; etop, etoposide; VCR, vincristine; tem, temozolomide; 5FU, 5-fluorouracil; CTX, cyclophosphamide; doxo, doxorubicin.
Role of funding source
The RELIVE endeavor, i.e., the retrospective global registry formed to source relapse data, is funded by CANSEARCH and Cancer Research Switzerland. The Funders did not have any role in study design, data collection, data analyses, interpretation or writing of this report.
Results
Relapsed HB
What is known about relapsed HB can be derived from recently conducted consortia trials either in the US, Europe, and Japan. Of the 542 patients with hepatoblastoma enrolled on SIOPEL trials 1, 2 and 3, 59 (11%) patients relapsed; this does not include the number of patients who never achieved an initial remission (i.e., those who progressed on therapy prior to achieving remission). Of the 59 who relapsed after remission, 52% achieved a second remission but the 3-year event free and overall survival (EFS and OS) were only 34% and 43%, respectively.4 Factors associated with improved outcomes in relapsed patients included lower PRETEXT stage, high AFP at relapse, and attempts at delivery of systemic therapy.4
Data from the recently concluded COG AHEP0731 trial demonstrates that of the 226 patients enrolled on strata 2, 3 and 4, 47 (21%) patients relapsed or had refractory disease.5,8,9 Among these, 25 (53%) died of disease, the majority of whom (96%) had intermediate or high-risk disease at diagnosis.5,9 These results highlight the relevance of disease stage, possibly as a reflection of disease biology, and resectability for disease recurrence. Relapse can occur for patients with initial low-stage disease but these events are rare and salvage is high.8 When patients recur, they tend to do so at the primary tumor site (i.e., in the liver), in the lung (either at the site of prior nodules or at new parenchymal sites), in both the liver and lung, and in rare circumstances in brain, lymph nodes or bone.39 Almost all patients relapse within 2 years of diagnosis facilitating relatively rapid data maturity.
The key requisites for cure following disease recurrence are systemic control of disease and complete resection of liver and metastatic sites, as surgery is the cornerstone of treatment. There are rare exceptions to the need for systemic therapy following relapse as evidenced by case reports or anecdotal experience demonstrating long-term salvage of solitary lung relapses addressed successfully with pulmonary metastatectomy sparing the use of adjuvant chemotherapy.40 The majority of patients, however, require chemotherapy delivered before and after repeat attempts at surgical disease control.
The traditional backbone of chemotherapy for HB used in the upfront setting consists of cisplatin monotherapy or a cisplatin-containing regimen (i.e., cisplatin/5-fluorouracil/vincristine/doxorubicin or cisplatin/carboplatin/doxorubicin).7, 8, 9,41,42 For patients who relapse without having previously been treated with doxorubicin or carboplatin, success has been demonstrated with use of these agents as part of relapse therapy.4,14,31,33 Re-introduction of cisplatin, depending on cumulative dose previously received, upfront response, and end-organ function has also contributed to improved outcomes and is the topic of study in a recently initiated trial (NCT05756660). Apart from cisplatin, carboplatin and doxorubicin, irinotecan and etoposide19,22,27,28,31, 32, 33,43 have been the most rigorously studied agents for relapsed HB if not used in the upfront setting (Table 1). The largest study enrolling 23 patients treated with irinotecan demonstrated 6 partial responses and 11 patients with stable disease.24 Even so, overall success rates with use of these agents alone, or in combination with other chemotherapeutics, are still less than 50%.44
Additional studies, with a robust number of enrollees, have investigated high-dose cyclophosphamide (n = 17), oxaliplatin (n = 10) and cixutumumab (anti-IGFR antibody, n = 10), all with disappointing results.45, 46, 47 There are partial responses peppered amongst other studies enrolling smaller numbers of patients, for example: aurora kinase inhibition (n = 2), pazopanib (n = 2), or alisertib (n = 1), but it is difficult to derive conclusions from these small numbers.13,20,25,48,49 A long list of alternative agents have proven disappointing in small patient cohorts (Table 1, Supplement Table S1).12,13 High-dose chemotherapy and stem cell rescue has been attempted but with considerable variation in the use of conditioning regimens and with highly variable results making clinical efficacy of this therapy unproven.12,16,50, 51, 52, 53 Targeting glypican-3 peaked interest in a pilot vaccine study and is the focus of current ongoing trials.37
For circumstances in which local control cannot be achieved with conventional surgery or when systemic therapies are ineffective at controlling disease, small series have been published detailing the use of external beam radiotherapy and interventional approaches to local control (chemoembolization, radioembolization, and microwave or radiofrequency ablation).12,54, 55, 56, 57, 58 The benefit of rescue liver transplantation, in the context of an incomplete upfront resection or a liver recurrence continues to evolve as early data, published by Otte et al., suggests inferior outcomes but more recent data reflects outcomes similar to those reported when transplant is pursued as an upfront local control measure.59,60
Relapsed HCC
Relapsed/refractory HCC carries a uniformly poor prognosis in comparison to relapsed HB. Until PHITT, there were no preceding consortia trials with a dedicated therapeutic arm designed to prospectively enroll pediatric patients with HCC. In keeping, there are no dedicated trials reporting on efficacious therapies for pediatric HCC relapse. PHITT is anticipated to explore the efficacy of chemotherapy in the upfront disease setting and proposes a mechanism for the collection of HCC tumor samples for genomic profiling. Much of therapy for relapsed pediatric HCC currently relies upon data sourced from the treatment of adults with HCC despite the fact that pediatric HCC is perceived to be a unique entity from the standpoint of pathophysiology and by cursory genomic analyses.61
Genomics of relapse
As genomic profiling becomes mainstream, identification of genomic predictors of poor prognosis have recurrently surfaced. NFE2L2 mutations have been associated with an increased risk of metastasis and vascular invasion.62 TERT promotor mutations have been consistently linked to hepatocellular neoplasm not otherwise specified (HCN NOS), a term used to describe cases of mixed or hybrid HB and HCC histology, and pediatric HCC cases.62,63 Methylation assays have also recently identified patients with higher risk disease and worse outcomes.63 Unfortunately, none of these genomic abnormalities are actionable. Alterations in the CTNNB1 gene are observed in nearly all HB tumors and are believed to occur in up to 2/3rds of patients with pediatric HCC.62,63 A clinical trial recently opened through COG studying tegavivint, a small molecule inhibitor which binds to transducin beta-like protein 1 (TBL1) and disrupts the binding of beta-catenin to TBL1, may demonstrate promise in relapsed or refractory primary liver tumors (NCT04851119). There is likewise increasing interest in the study of immunotherapies for this patient population: checkpoint inhibition (NCT04134559), antibody or chimeric T-cells to target GPC3 (NCT04928677, NCT02932956), or engineered T-cells targeting HLA:A2 bound AFP peptide and GPC3 as a co-stimulatory domain (NCT04634357) are currently under study. In short, there is a critically unmet need to more adequately source data regarding promising therapies and to identify novel agents worthy of prospective study.
Discussion
In April 2017 pediatric oncologists from the COG, SIOPEL, and JCCG met in Paris, France for a Childhood Liver Tumors Strategy Group (SIOPEL) conference. A focus of this meeting, and previous annual SIOPEL meetings, was to plan the now open and enrolling PHITT trial. This trial prospectively enrolls patients with HB and HCC across four continents (North America, Europe, East Asia, Australia) and is anticipated to accrue 1200 patients: 1000 patients with HB and 200 patients with pediatric HCC. As of today, more than 900 patients have been recruited in PHITT. The overarching trial goals of PHITT are to reduce therapy for patients with low-risk HB, optimize therapy for patients with intermediate risk HB, and intensify therapy for patients with high-risk HB. Embedded are analyses of comprehensive surgical, pathology, radiology, biology, pharmacology, and toxicity endpoints. Patients with pediatric HCC are enrolled to one of two arms differentiated by upfront resectable versus advanced disease. The overarching goals here are to collect biologic specimens and assess for chemotherapeutic efficacy. The trial is anticipated to contribute meaningfully to our clinical and biological understanding of HB and HCC worldwide but is also anticipated to identify the subset of patients for whom long-term remission is not attained.
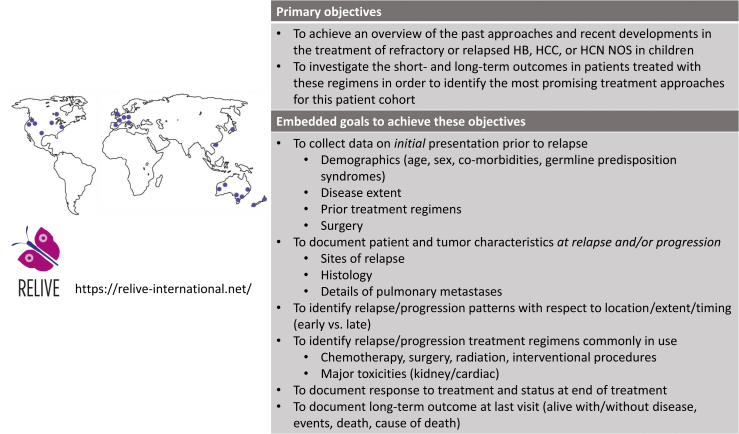
A working group of attendees at the Paris meeting identified a key limitation in our understanding of relapsed pediatric HB and HCC: limited available data describing relapse disease incidence, characteristics, effective therapies, prognostic risk factors, relapse-associated genomic alterations, and ultimately outcomes. Stemming from this discussion came the nomination of key stakeholders—i.e., oncologists, pathologists, and surgeons with expertise in the treatment of pediatric liver tumors—from each of the three consortia. These nominated personnel were then tasked with establishing a network of regional institutions as depicted in Fig. 1 (left).
Fig. 1.
Geographic description of the network of institutions engaged in the RELIVE initiative (left) and primary objectives and goals embedded within the RELIVE registry(right).
A series of conference calls ensued identifying a global interest in launching the first international retrospective registry intended to collect granular data for pediatric patients previously treated for relapsed/refractory HB or HCC. An estimate of the global incidence of relapsed/refractory HB and HCC, utilizing anticipated accruals to the PHITT trial, was first performed to estimate accruals to such a registry and substantiate further work (Table 2).
Table 2.
Anticipated frequency of risk for relapse for patients enrolled on PHITT.
| Strata | Number of patients | Estimated 3-yr EFS | Approximate number of patients predicted to have an EFS event |
|---|---|---|---|
| A–Very low risk HBa | 200 | 85–92.5% | 15–30 |
| B–Low risk HBa | 320 | 87.5% | 40 |
| C–Intermediate risk HBa | 210 | 80% | 42 |
| D–High risk HBa | 210 | 60% | 84 |
| E–Resected HCC | 50 | 82.5% | 8 |
| F–Unresected or metastatic HCC | 150 | 0–20% | 120 |
Risk classification as defined in the PHITT protocol.
Geneva University Hospital (HUG) was identified as the International Sponsor and correspondingly the Geneva PI was nominated as the International Chair. A Steering Committee was assembled to include the International Chair and nominated Chairs for Europe, North America, East Asia, Australia, and New Zealand, as well as the registry statistician. An administrative team was assembled in Geneva to include individuals with expertise in web-based design, ethics board approvals, protocol and consent writing, legal stipulations, electronic database creation, patient and family outreach, as well as informatics.
The Steering Committee met regularly to facilitate protocol design and agree upon study objectives including the goal to source data on upfront therapy and each line of relapse therapy (Fig. 1, right). To address the frequently discordant patterns observed between AFP levels and radiographic imaging64 and to aid with data collection, the following definitions were agreed upon: 1) Complete Remission: normal AFP (for age) and, per institutional read, low/negative suspicion of residual tumor on imaging examinations; 2) Relapse after a prior complete remission: a) progressive rise in AFP (on 3 successive AFP levels), or b) new findings on imaging examinations consistent with disease [either on conventional computed tomography (CT) or magnetic resonance imaging (MRI), or alternatively by metabolic detection on positron emission tomography (PET)]; 3) Progression/refractory disease: a) progressive rise in AFP (in 3 successive AFP levels), or b) unequivocal tumor growth on imaging examinations. Response to systemic therapy prior to local control was defined as one or more of the following: 1) clinical trial defined response (e.g., RECIST), 2) a >1 log fold decline of AFP, 3) any unequivocal decrease in size on imaging, or 4) complete remission (per the definition above).
The accrual goal was set at 200 patients with relapsed/refractory HB and 100 patients with relapsed/refractory HCC or HCN NOS65 with the plan to acquire data in a rolling fashion, every 2 years, to retain a retrospective approach to data acquisition over the 8 years the registry is projected to remain open. Clinical research forms (CRFs) were designed and a REDCap database and Microsoft OneDrive was built to allow international data collection as well as upload of anonymized pathology, surgery, genomic and radiology reports. The study was launched 9 months after the project’s inception (Timeline, Supplement Figure S1, Supplement Table S2) and a consent form was drafted in 6 languages (French, English, Italian, German Dutch, and Spanish) for use at sites unable to obtain a waiver of consent. At the time of this manuscript’s submission, data for more than 200 patients has been collected. It is anticipated that data analysis will be largely descriptive in nature; however it is possible that findings of statistical significance will be detected.
The Steering Committee continues to meet quarterly to assure site activations run smoothly, to track data collection, and to coordinate updates at annual consortium meetings. PHITT is anticipated to accrue until December 2023; accordingly the goal is to align data accrual by the RELIVE consortium effort with writing efforts for the AHEP1531/PHITT successor trial which is intended to include a prospective, therapeutic relapse arm. It is our expectation that data analyzed from the RELIVE consortium will identify therapies of most promise to consider for prospective study.
The RELIVE consortium has successfully united over 80 investigators committed to the care of pediatric patients with liver tumors and invested in sourcing data regarding best available therapies for the rare subset of patients with relapsed or refractory disease.
To support this initiative, the RELIVE consortium sponsor has designed an accessible, educational website (https://relive-international.net/) housing information regarding the consortium’s infrastructure and mission, secured access to the REDCap database for participating institutes, a quarterly newsletter, and a patient and family forum uniting advocacy groups across the world.
Outstanding questions
The pediatric oncology community is well-versed in challenges germane to the study of rare disease. AHEP1531/PHITT was the latest in a series of steps to solidify an international infrastructure for the study of exceptionally rare liver tumors across continents. The RELIVE initiative capitalizes on PHITT’s existing infrastructure and collaborative network to proactively address challenges faced in data collection and understand the relapse landscape. Once data is collected, the appropriate application of this data to inform future relapse treatment algorithms and the optimal approach to the prospective study of relapse in a successor international trial will require additional thought and planning. Until then, the approach taken to establish the RELIVE consortium can serve as a valuable paradigm for the study of rare disease affecting both adult and pediatric patients.
Contributors
Allison F. O'Neill MD: literature search, figures, study design, data collection, data analysis, data interpretation, writing.
Angela Trobaugh-Lotrario MD: literature search, figures, study design, data collection, data analysis, data interpretation, writing.
James I. Geller MD: study design, data interpretation, writing.
Eiso Hiyama MD, PhD: study design, data interpretation, writing.
Kenichiro Watanabe MD: study design, data interpretation, writing.
Isabelle Aerts MD: study design, data interpretation, writing.
Brice Fresneau MD: study design, data interpretation, writing.
Fabienne Toutain MD: study design.
Michael J Sullivan MD: study design, data interpretation, writing.
Howard M. Katzenstein MD: study design, data interpretation, writing.
Bruce Morland MD: study design, data interpretation, writing.
Sophie Branchereau MD: study design, data interpretation, writing.
József Zsiros, MD PhD: study design, data interpretation, writing.
Rudolf Maibach PhD: study design, data analysis, data interpretation, writing.
Marc Ansari MD: figures, study design, data collection, data analysis, data interpretation, writing.
Declaration of interests
Howard Katzenstein is employed by Merck, Rayway NJ but has no conflicts with this manuscript. Marc Ansari’s institute receives financial support from CANSEARCH and Jazz Pharmaceuticals, but this does not constitute a personal conflict. All other authors report no conflicts of interest.
Acknowledgements
On behalf of the RELIVE consortium (RELIVE site PIs): Reto Baertschiger, Benedicte Brichard, Alan KS Chiang, Hetal Dholaria, Hanna Garnier, Anthony PY Liu, Kathelijne Kraal, Arun Rangaswami, Irene Schmid, and Barbara Wildhaber. Special acknowledgement to Aurore Britan for her coordination of the database and consortium infrastructure.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2024.102446.
Appendix A. Supplementary data
References
- 1.Howlander N.A., Noone A.M., Krapcho M., et al., editors. SEER cancer statistics review, 1975-2009. National Cancer Institute; 2009. [Google Scholar]
- 2.Hubbard A.K., Spector L.G., Fortuna G., Marcotte E.L., Poynter J.N. Trends in international incidence of pediatric cancers in children under 5 years of age: 1988-2012. JNCI Cancer Spectr. 2019;3 doi: 10.1093/jncics/pkz007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khanna R., Verma S.K. Pediatric hepatocellular carcinoma. World J Gastroenterol. 2018;24:3980–3999. doi: 10.3748/wjg.v24.i35.3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Semeraro M., Branchereau S., Maibach R., et al. Relapses in hepatoblastoma patients: clinical characteristics and outcome--experience of the International Childhood Liver Tumour Strategy Group (SIOPEL) Eur J Cancer. 2013;49:915–922. doi: 10.1016/j.ejca.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Katzenstein H.M., Furman W.L., Malogolowkin M.H., et al. Upfront window vincristine/irinotecan treatment of high-risk hepatoblastoma: a report from the Children’s Oncology Group AHEP0731 study committee. Cancer. 2017;123:2360–2367. doi: 10.1002/cncr.30591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hiyama E., Hishiki T., Watanabe K., et al. Outcome and late complications of hepatoblastomas treated using the Japanese Study Group for pediatric liver tumor 2 protocol. J Clin Oncol. 2020;38:2488–2498. doi: 10.1200/JCO.19.01067. [DOI] [PubMed] [Google Scholar]
- 7.Zsiros J., Brugieres L., Brock P., et al. Dose-dense cisplatin-based chemotherapy and surgery for children with high-risk hepatoblastoma (SIOPEL-4): a prospective, single-arm, feasibility study. Lancet Oncol. 2013;14:834–842. doi: 10.1016/S1470-2045(13)70272-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katzenstein H.M., Langham M.R., Malogolowkin M.H., et al. Minimal adjuvant chemotherapy for children with hepatoblastoma resected at diagnosis (AHEP0731): a Children’s Oncology Group, multicentre, phase 3 trial. Lancet Oncol. 2019;20:719–727. doi: 10.1016/S1470-2045(18)30895-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katzenstein H.M., Malogolowkin M.H., Krailo M.D., et al. Doxorubicin in combination with cisplatin, 5-flourouracil, and vincristine is feasible and effective in unresectable hepatoblastoma: a Children’s Oncology Group study. Cancer. 2021;128(5):1057–1065. doi: 10.1002/cncr.34014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Czauderna P., Mackinlay G., Perilongo G., et al. Hepatocellular carcinoma in children: results of the first prospective study of the International Society of Pediatric Oncology group. J Clin Oncol. 2002;20:2798–2804. doi: 10.1200/JCO.2002.06.102. [DOI] [PubMed] [Google Scholar]
- 11.Katzenstein H.M., Krailo M.D., Malogolowkin M.H., et al. Hepatocellular carcinoma in children and adolescents: results from the Pediatric Oncology Group and the Children’s Cancer Group intergroup study. J Clin Oncol. 2002;20:2789–2797. doi: 10.1200/JCO.2002.06.155. [DOI] [PubMed] [Google Scholar]
- 12.Trobaugh-Lotrario A.D., Feusner J.H. Relapsed hepatoblastoma. Pediatr Blood Cancer. 2012;59:813–817. doi: 10.1002/pbc.24218. [DOI] [PubMed] [Google Scholar]
- 13.Trobaugh-Lotrario A.D., Meyers R.L., Feusner J.H. Outcomes of patients with relapsed hepatoblastoma enrolled on Children's Oncology Group (COG) phase I and II studies. J Pediatr Hematol Oncol. 2016;38:187–190. doi: 10.1097/MPH.0000000000000474. [DOI] [PubMed] [Google Scholar]
- 14.Malogolowkin M.H., Katzenstein H.M., Krailo M., et al. Redefining the role of doxorubicin for the treatment of children with hepatoblastoma. J Clin Oncol. 2008;26:2379–2383. doi: 10.1200/JCO.2006.09.7204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blaney S., Berg S.L., Pratt C., et al. A phase I study of irinotecan in pediatric patients: a pediatric oncology group study. Clin Cancer Res. 2001;7:32–37. [PubMed] [Google Scholar]
- 16.Katzenstein H.M., Rigsby C., Shaw P.H., et al. Novel therapeutic approaches in the treatment of children with hepatoblastoma. J Pediatr Hematol Oncol. 2002;24:751–755. doi: 10.1097/00043426-200212000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Palmer R.D., Williams D.M. Dramatic response of multiply relapsed hepatoblastoma to irinotecan (CPT-11) Med Pediatr Oncol. 2003;41:78–80. doi: 10.1002/mpo.10300. [DOI] [PubMed] [Google Scholar]
- 18.Vassal G., Doz F., Frappaz D., et al. A phase I study of irinotecan as a 3-week schedule in children with refractory or recurrent solid tumors. J Clin Oncol. 2003;21:3844–3852. doi: 10.1200/JCO.2003.08.175. [DOI] [PubMed] [Google Scholar]
- 19.Ijichi O., Ishikawa S., Shinkoda Y., et al. Response of heavily treated and relapsed hepatoblastoma in the transplanted liver to single-agent therapy with irinotecan. Pediatr Transplant. 2006;10:635–638. doi: 10.1111/j.1399-3046.2006.00517.x. [DOI] [PubMed] [Google Scholar]
- 20.Bomgaars L.R., Bernstein M., Krailo M., et al. Phase II trial of irinotecan in children with refractory solid tumors: a Children’s Oncology Group Study. J Clin Oncol. 2007;25:4622–4627. doi: 10.1200/JCO.2007.11.6103. [DOI] [PubMed] [Google Scholar]
- 21.McNall-Knapp R.Y., Williams C.N., Reeves E.N., Heideman R.L., Meyer W.H. Extended phase I evaluation of vincristine, irinotecan, temozolomide, and antibiotic in children with refractory solid tumors. Pediatr Blood Cancer. 2010;54:909–915. doi: 10.1002/pbc.22460. [DOI] [PubMed] [Google Scholar]
- 22.Qayed M., Powell C., Morgan E.R., Haugen M., Katzenstein H.M. Irinotecan as maintenance therapy in high-risk hepatoblastoma. Pediatr Blood Cancer. 2010;54:761–763. doi: 10.1002/pbc.22408. [DOI] [PubMed] [Google Scholar]
- 23.Wagner L.M., Perentesis J.P., Reid J.M., et al. Phase I trial of two schedules of vincristine, oral irinotecan, and temozolomide (VOIT) for children with relapsed or refractory solid tumors: a Children’s Oncology Group phase I consortium study. Pediatr Blood Cancer. 2010;54:538–545. doi: 10.1002/pbc.22407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zsiros J., Brugieres L., Brock P., et al. Efficacy of irinotecan single drug treatment in children with refractory or recurrent hepatoblastoma--a phase II trial of the childhood liver tumour strategy group (SIOPEL) Eur J Cancer. 2012;48:3456–3464. doi: 10.1016/j.ejca.2012.06.023. [DOI] [PubMed] [Google Scholar]
- 25.Bagatell R., Norris R., Ingle A.M., et al. Phase 1 trial of temsirolimus in combination with irinotecan and temozolomide in children, adolescents and young adults with relapsed or refractory solid tumors: a Children’s Oncology Group Study. Pediatr Blood Cancer. 2014;61:833–839. doi: 10.1002/pbc.24874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Y.T., Feng L.H., Zhong X.D., Wang L.Z., Chang J. Vincristine and irinotecan in children with relapsed hepatoblastoma: a single-institution experience. Pediatr Hematol Oncol. 2015;32:18–25. doi: 10.3109/08880018.2014.909913. [DOI] [PubMed] [Google Scholar]
- 27.Powers J.M., Pacheco M.M., Wickiser J.E. Addition of vincristine and irinotecan to standard therapy in a patient with refractory high-risk hepatoblastoma achieving long-term relapse-free survival. J Pediatr Hematol Oncol. 2019;41:e171–e173. doi: 10.1097/MPH.0000000000001171. [DOI] [PubMed] [Google Scholar]
- 28.Keino D., Yokosuka T., Hirose A., et al. Pilot study of the combination of sorafenib and fractionated irinotecan in pediatric relapse/refractory hepatic cancer (FINEX pilot study) Pediatr Blood Cancer. 2020;67 doi: 10.1002/pbc.28655. [DOI] [PubMed] [Google Scholar]
- 29.Lockwood L., Heney D., Giles G.R., Lewis I.J., Bailey C.C. Cisplatin-resistant metastatic hepatoblastoma: complete response to carboplatin, etoposide, and liver transplantation. Med Pediatr Oncol. 1993;21:517–520. doi: 10.1002/mpo.2950210711. [DOI] [PubMed] [Google Scholar]
- 30.van Hoff J., Grier H.E., Douglass E.C., Green D.M. Etoposide, ifosfamide, and cisplatin therapy for refractory childhood solid tumors. Response and toxicity. Cancer. 1995;75:2966–2970. doi: 10.1002/1097-0142(19950615)75:12<2966::aid-cncr2820751226>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 31.Fuchs J., Bode U., von Schweinitz D., et al. Analysis of treatment efficiency of carboplatin and etoposide in combination with radical surgery in advanced and recurrent childhood hepatoblastoma: a report of the German Cooperative Pediatric Liver Tumor Study HB 89 and HB 94. Klin Padiatr. 1999;211:305–309. doi: 10.1055/s-2008-1043805. [DOI] [PubMed] [Google Scholar]
- 32.Matsunaga T., Sasaki F., Ohira M., et al. Analysis of treatment outcome for children with recurrent or metastatic hepatoblastoma. Pediatr Surg Int. 2003;19:142–146. doi: 10.1007/s00383-002-0906-0. [DOI] [PubMed] [Google Scholar]
- 33.Loss J.F., Santos P.P., Leone L.D., Brunetto A.L. Outcome of pediatric recurrent and refractory malignant solid tumors following ifosfamide/carboplatin/etoposide (ICE): a phase II study in a pediatric oncology centre in Brazil. Pediatr Blood Cancer. 2004;42:139–144. doi: 10.1002/pbc.10375. [DOI] [PubMed] [Google Scholar]
- 34.Miyamura T., Yoshida R., Yagi T., et al. Successful treatment of unresectable advanced hepatoblastoma: living liver transplantation after surgical removal of lung metastasis. Pediatr Transplant. 2011;15:E87–E91. doi: 10.1111/j.1399-3046.2009.01262.x. [DOI] [PubMed] [Google Scholar]
- 35.Natarajan E., Auerbach C., Cheron R., Pashankar F. Sustained remission after maintenance irinotecan in patient with multiply relapsed hepatoblastoma. J Pediatr Hematol Oncol. 2020;42:e659–e661. doi: 10.1097/MPH.0000000000001544. [DOI] [PubMed] [Google Scholar]
- 36.Hou J.Y., Yeh T.C., Huang T.H., Sheu J.C., Liu H.C. A retrospective study of clinical features and outcome in patients with refractory or recurrent hepatoblastoma: a single institution experience. Pediatr Neonatol. 2021;62:400–405. doi: 10.1016/j.pedneo.2021.03.018. [DOI] [PubMed] [Google Scholar]
- 37.Tsuchiya N., Hosono A., Yoshikawa T., et al. Phase I study of glypican-3-derived peptide vaccine therapy for patients with refractory pediatric solid tumors. OncoImmunology. 2017;7 doi: 10.1080/2162402X.2017.1377872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hara J., Osugi Y., Ohta H., et al. Double-conditioning regimens consisting of thiotepa, melphalan and busulfan with stem cell rescue for the treatment of pediatric solid tumors. Bone Marrow Transplant. 1998;22:7–12. doi: 10.1038/sj.bmt.1701283. [DOI] [PubMed] [Google Scholar]
- 39.Rai P., Feusner J.H. Cerebral metastasis of hepatoblastoma: a review. J Pediatr Hematol Oncol. 2016;38:279–282. doi: 10.1097/MPH.0000000000000554. [DOI] [PubMed] [Google Scholar]
- 40.Shi Y., Geller J.I., Ma I.T., et al. Relapsed hepatoblastoma confined to the lung is effectively treated with pulmonary metastasectomy. J Pediatr Surg. 2016;51:525–529. doi: 10.1016/j.jpedsurg.2015.10.053. [DOI] [PubMed] [Google Scholar]
- 41.Perilongo G., Maibach R., Shafford E., et al. Cisplatin versus cisplatin plus doxorubicin for standard-risk hepatoblastoma. N Engl J Med. 2009;361:1662–1670. doi: 10.1056/NEJMoa0810613. [DOI] [PubMed] [Google Scholar]
- 42.Zsiros J., Maibach R., Shafford E., et al. Successful treatment of childhood high-risk hepatoblastoma with dose-intensive multiagent chemotherapy and surgery: final results of the SIOPEL-3HR study. J Clin Oncol. 2010;28:2584–2590. doi: 10.1200/JCO.2009.22.4857. [DOI] [PubMed] [Google Scholar]
- 43.Fuchs J., Rydzynski J., Von Schweinitz D., et al. Pretreatment prognostic factors and treatment results in children with hepatoblastoma: a report from the German Cooperative Pediatric Liver Tumor Study HB 94. Cancer. 2002;95:172–182. doi: 10.1002/cncr.10632. [DOI] [PubMed] [Google Scholar]
- 44.Zsiros J., Brugières L. In: Pediatric liver tumors. Zimmerman A., et al., editors. Springer-Verlag Berlin Heidelberg; 2011. [Google Scholar]
- 45.Beaty O., 3rd, Berg S., Blaney S., et al. A phase II trial and pharmacokinetic study of oxaliplatin in children with refractory solid tumors: a Children’s Oncology Group study. Pediatr Blood Cancer. 2010;55:440–445. doi: 10.1002/pbc.22544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weigel B., Malempati S., Reid J.M., et al. Phase 2 trial of cixutumumab in children, adolescents, and young adults with refractory solid tumors: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2014;61:452–456. doi: 10.1002/pbc.24605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cacciavillano W.D., Brugieres L., Childs M., et al. Phase II study of high-dose cyclophosphamide in relapsing and/or resistant hepatoblastoma in children: a study from the SIOPEL group. Eur J Cancer. 2004;40:2274–2279. doi: 10.1016/j.ejca.2004.01.042. [DOI] [PubMed] [Google Scholar]
- 48.Mosse Y.P., Lipsitz E., Fox E., et al. Pediatric phase I trial and pharmacokinetic study of MLN8237, an investigational oral selective small-molecule inhibitor of Aurora kinase A: a Children’s Oncology Group Phase I Consortium study. Clin Cancer Res. 2012;18:6058–6064. doi: 10.1158/1078-0432.CCR-11-3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Glade Bender J.L., Lee A., Reid J.M., et al. Phase I pharmacokinetic and pharmacodynamic study of pazopanib in children with soft tissue sarcoma and other refractory solid tumors: a Children’s Oncology Group phase I consortium report. J Clin Oncol. 2013;31:3034–3043. doi: 10.1200/JCO.2012.47.0914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nishimura S., Sato T., Fujita N., et al. High-dose chemotherapy in children with metastatic hepatoblastoma. Pediatr Int. 2002;44:300–305. doi: 10.1046/j.1442-200x.2002.01549.x. [DOI] [PubMed] [Google Scholar]
- 51.Inaba H., Handgretinger R., Furman W., Hale G., Leung W. Allogeneic graft-versus-hepatoblastoma effect. Pediatr Blood Cancer. 2006;46:501–505. doi: 10.1002/pbc.20404. [DOI] [PubMed] [Google Scholar]
- 52.Niwa A., Umeda K., Awaya T., et al. Successful autologous peripheral blood stem cell transplantation with a double-conditioning regimen for recurrent hepatoblastoma after liver transplantation. Pediatr Transplant. 2009;13:259–262. doi: 10.1111/j.1399-3046.2008.00948.x. [DOI] [PubMed] [Google Scholar]
- 53.Karski E.E., Dvorak C.C., Leung W., et al. Treatment of hepatoblastoma with high-dose chemotherapy and stem cell rescue: the pediatric blood and marrow transplant consortium experience and review of the literature. J Pediatr Hematol Oncol. 2014;36:362–368. doi: 10.1097/MPH.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 54.Habrand J.L., Nehme D., Kalifa C., et al. Is there a place for radiation therapy in the management of hepatoblastomas and hepatocellular carcinomas in children? Int J Radiat Oncol Biol Phys. 1992;23:525–531. doi: 10.1016/0360-3016(92)90007-5. [DOI] [PubMed] [Google Scholar]
- 55.Czauderna P., Zbrzezniak G., Narozanski W., et al. Preliminary experience with arterial chemoembolization for hepatoblastoma and hepatocellular carcinoma in children. Pediatr Blood Cancer. 2006;46:825–828. doi: 10.1002/pbc.20422. [DOI] [PubMed] [Google Scholar]
- 56.Aguado A., Ristagno R., Towbin A.J., et al. Transarterial radioembolization with yttrium-90 of unresectable primary hepatic malignancy in children. Pediatr Blood Cancer. 2019;66 doi: 10.1002/pbc.27510. [DOI] [PubMed] [Google Scholar]
- 57.Cui R., Yu J., Gu Y., et al. Microwave ablation assisted by three-dimensional visualization system as local therapy for relapsed hepatoblastoma: a small pilot study. Abdom Radiol. 2019;44:2909–2915. doi: 10.1007/s00261-019-02011-5. [DOI] [PubMed] [Google Scholar]
- 58.Jiang Y., Zhou S., Shen G., Jiang H., Zhang J. Microwave ablation combined with transcatheter arterial chemoembolization is effective for treating unresectable hepatoblastoma in infants and children. Medicine. 2018;97 doi: 10.1097/MD.0000000000012607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Otte J.B., Pritchard J., Aronson D.C., et al. Liver transplantation for hepatoblastoma: results from the International Society of Pediatric Oncology (SIOP) study SIOPEL-1 and review of the world experience. Pediatr Blood Cancer. 2004;42:74–83. doi: 10.1002/pbc.10376. [DOI] [PubMed] [Google Scholar]
- 60.Triana Junco P., Cano E.M., Dore M., et al. Prognostic factors for liver transplantation in unresectable hepatoblastoma. Eur J Pediatr Surg. 2019;29:28–32. doi: 10.1055/s-0038-1668148. [DOI] [PubMed] [Google Scholar]
- 61.Weeda V.B., Aronson D.C., Verheij J., Lamers W.H. Is hepatocellular carcinoma the same disease in children and adults? Comparison of histology, molecular background, and treatment in pediatric and adult patients. Pediatr Blood Cancer. 2019;66 doi: 10.1002/pbc.27475. [DOI] [PubMed] [Google Scholar]
- 62.Sumazin P., Chen Y., Trevino L.R., et al. Genomic analysis of hepatoblastoma identifies distinct molecular and prognostic subgroups. Hepatology. 2016;65(1):104–121. doi: 10.1002/hep.28888. [DOI] [PubMed] [Google Scholar]
- 63.Nagae G., Yamamoto S., Fujita M., et al. Genetic and epigenetic basis of hepatoblastoma diversity. Nat Commun. 2021;12:5423. doi: 10.1038/s41467-021-25430-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rojas Y., Guillerman R.P., Zhang W., et al. Relapse surveillance in AFP-positive hepatoblastoma: re-evaluating the role of imaging. Pediatr Radiol. 2014;44:1275–1280. doi: 10.1007/s00247-014-3000-6. [DOI] [PubMed] [Google Scholar]
- 65.Lopez-Terrada D., Alaggio R., de Davila M.T., et al. Towards an international pediatric liver tumor consensus classification: proceedings of the Los Angeles COG liver tumors symposium. Mod Pathol. 2014;27:472–491. doi: 10.1038/modpathol.2013.80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.