Abstract
There is strong preference among people with disabling conditions to receive care at home rather than in an institutional setting. Differences in state policies may make this more feasible in some states than others. Yet no study to date has examined trends in the long-term care workforce across states. Using state-level data on direct care workers from the period 2009–20, we examine trends in the sizes of the nursing home and home care workforces. We show that since 2009 most states have increased the size of their home care workforces and decreased the size of their nursing home workforces, but there is substantial variation across states in the magnitude of these changes. In addition, the gap between leading and lagging states in home care workforce size has grown over time. This suggests that more targeted efforts may be needed to ensure that people with disabling conditions can have their needs met in their desired setting across the nation.
As the US population ages, the demand for long-term care will increase, placing pressure on the direct care workforce to meet that demand. Most people prefer to receive care at home rather than in an institutional setting,1,2 and the trend has been away from institutional care toward home and community-based services for several decades.3 There is evidence that if current demographic and policy trends persist, projected growth in the demand for home health and personal care aides will require nearly 1.2 million additional jobs by 2030.4 This growing demand suggests a need to understand whether the direct care workforce is keeping up with consumers’ needs and preferences across the US.
Differences in policy support for home and community-based services could create disparities across states in the types of settings where people can receive services. State Medicaid programs, for instance, could influence patterns of long-term care use and the settings in which such care is provided. Medicaid accounted for more than 40 percent of the $366 billion spent on long-term care in 2016 in the US.5 The Centers for Medicare and Medicaid Services has spent the past several decades trying to “rebalance” long-term care from facilities to the community when the setting is appropriate, partly to accommodate individual preferences but also to facilitate opportunities for people with care needs to remain in the community when appropriate, in compliance with the Americans with Disabilities Act and the Olmstead decision.2 However, some states have been more successful at rebalancing their long-term services and supports than others. Although all Medicaid programs must continue to offer institutional care, states have tremendous flexibility in the extent to which they provide optional home and community-based services. This includes eligibility criteria as well as what home and community-based services benefit packages cover.6
In addition, some states have been working more than others to expand the direct care workforce by providing wage and benefit enhancements and career ladder initiatives such as training, mentoring, and credentialing. For example, in states such as Washington and Oregon, in which in-home individual providers paid by Medicaid are represented by the Service Employees International Union in collective bargaining, unions helped raise wages for home care workers in Medicaid and other state programs. States in which home care workers do not have union bargaining rights have been less successful at improving these careers and growing their home care workforces.
There are several ways to capture state-level changes in the provision of home and community-based services. For example, one could track spending, the number of services provided, or the quality of care.We focused on workforce size, as it directly captures the number of caregivers actively engaged in care in different settings. Specifically, we examined the number of direct care workers in each state. These are the key providers of daily support to people with functional limitations.7 They include personal care aides and home health aides, who are employed in home and community-based settings, as well as nursing assistants, who are typically employed in institutional settings. Overall, the direct care worker occupation has seen enormous growth in recent years, from 3 million workers in 2009 to 4.6 million workers in 2019,8 and long-term care direct care workers make up about one-fifth of the entire US total health care workforce.9 However, this growth has not been uniform across settings. Since 2009 there has been a shift in the ratio of direct care workers employed in institutional versus home settings. Nationally, the home care workforce has had a more than twofold increase since 2009, whereas the number of nursing assistants in nursing homes has decreased slightly.8
Although there is evidence that the home care workforce has been increasing at a faster rate than the nursing home workforce at the national level,8 no study to date has examined shifts in the long-term services and supports workforce at the state level. Variation in state policies and support for home and community-based services could suggest that some states may be moving forward in service provision while others lag. Using state-level data on direct care workers between 2009 and 2020, we examined trends in the nursing home and home care workforces. Specifically, we examined the extent to which there is variation in these workforces across states; whether growth in the home care workforce is substituting for declines in the nursing home workforce; and whether states have begun to converge, over time, in the size of their home care workforces.
Study Data And Methods
We used data for 2009–20 from the Occupational Employment and Wage Statistics program,10 a Bureau of Labor Statistics program that produces annual estimates of employment and wages for almost 800 occupations. After exploring a variety of data sets that could be used to examine the direct care workforce, we decided that the Occupational Employment and Wage Statistics program data were best for our analyses because they are the only data source that allows us to disaggregate home health aides and personal care aides from nursing aides, provides information on trends going back to 2009, and includes state-level variation. To adjust for state-level differences in long-term care needs, we calculated the ratio of the size of the state-level workforce and the number of people with disabilities, using data from the American Community Survey, an ongoing survey conducted by the Census Bureau.
We defined the home care workforce as the combined employment counts for two occupation codes: personal care aides (SOC 39–9021) and home health aides (SOC 31–1011). Personal care aides assist older adults or people of all ages who have disabilities with activities of daily living at the person’s home or community-based residential setting (for example, a retirement community or assisted living facility). Duties may include light housekeeping (for example, making beds, doing laundry, and washing dishes) and preparing meals, as well as personal care (for example, bathing, dressing, and grooming). Home health aides, in contrast, provide routine individualized health care (for example, changing bandages, dressing wounds, and applying topical medications) and personal care.
We defined the nursing home workforce as nursing assistants (SOC 31–1014) and orderlies (SOC 31–1015)—groups that are combined in the data. They feed, bathe, dress, and move patients and transfer or transport patients or residents. Workforce counts were standardized by computing the number of workers per 1,000 people with disabilities.
A small number of estimates were missing for certain years in the Occupational Employment and Wage Statistics program files. We filled in missing data through a simple linear interpolation, using the Stata command -ipolate-. This takes a simple linear trend between nonmissing values for the state in the years before and after the missing value. If the missing value is at the beginning or end of the time series, the value is extrapolated from the linear trend from the other nonmissing values. In total, missing values ranged from 0.2 percent to 3.9 percent.
Within each state, we used data from the American Community Survey to obtain estimates for the annual population with disabilities as a weighted count of people with two categories of disabilities that should be correlated with the need for care: reports of self-care disability and independent living disability. This combination of information on state workforce and disability counts allowed us to calculate a standardized rate of workforce size per 1,000 people with disabilities at the state level.
STATISTICAL ANALYSES
We began our analyses by using maps to explore statewide variation in the home care and nursing home workforces. To do this, we used mapping software (ArcMap 1 .7, ESRI, 2018) to plot state-by-state changes (estimated as 2020 value minus 2009 value) and color-coded states to show increase or decrease in temporal changes during the study period. Next, we explored whether the home care workforce substitutes for the nursing home workforce—that is, whether we see one-to-one replacement of the home care workforce by members of the nursing home workforce. We did this by examining scatterplots with changes in home care workforce size per 1,000 people with disabilities on the x axis and changes in nursing home workforce size per 1,000 people with disabilities on the y axis; this allowed us to examine the relationship between these variables. We also ran linear regression models and t-tests to estimate whether the slope was statistically significant and different from zero.
Finally, we examined the extent to which changes in home care workforce trends converged or diverged across states over time by plotting time trends of home care workforce size per 1,000 people with disabilities for each quartile of their respective baseline distribution and conducting a pairwise t-test for quartiles 1, 2, and 3 versus quartile 4 to identify statistically significant differences in slope.
SENSITIVITY ANALYSES
In 2017 the Occupational Employment and Wage Statistics program changed its industry classification from North American Industry Classification System 2012 to North American Industry Classification System 2017 to be more inclusive of different types of businesses providing services to older adults. This resulted in the inclusion of more business establishments with our occupations of interest in the study starting in 2017—a change that is particularly pronounced in certain states. To determine whether state trends were sensitive to classification changes, we visually inspected trends in home care and nursing home workforce sizes between 2009 and 2020 for each state (online appendix exhibit S-1).11 Two states, California and Washington, had a large jump in their home care workforce size in 2017, suggesting that they may be sensitive to the new coding. We therefore excluded these states from the main analyses. Our final analytic sample included forty-eight states and Washington, D.C. (forty-nine total “state” data points).
LIMITATIONS
Although the Occupational Employment and Wage Statistics program data are the most appropriate for our analyses, there are several inherent limitations. As mentioned above, the classification of some businesses changed in 2017, making it difficult to compare data over these two periods across all states. Because we were interested in long-term trends to the present time, we combined data from pre-2017 and post-2017. For the most part, we did not see large changes in states across the two periods, suggesting that the combined data were not particularly sensitive to the changes in North American Industry Classification System classification. However, as stated above, two states that showed large changes in workforce size in 2017 were dropped from these analyses because we could not assess whether the changes were real or due to a shift in classification.
We tried to get as close as possible to occupational groupings that capture the home care and nursing home workforces; accordingly, we used occupational titles for these groupings. However, for some occupations we could not be certain of the industries in which they worked. For instance, “nursing assistants” and “orderlies,” whom we include in the nursing home workforce, could be employed across a range of settings. Most of the settings outside of nursing homes are hospitals, which we would not expect to show a declining workforce. If anything, we would expect even stronger findings if we could remove nursing assistants and orderlies working outside nursing home settings. Orderlies also do not provide basic care but are included in these analyses by necessity, given the organization of the Occupational Employment and Wage Statistics program data (they cannot be disaggregated). Finally, the Occupational Employment and Wage Statistics program surveys a panel of business establishments every six months, taking three years to collect the full sample of 1.1 million establishments. This may make it less sensitive to year-over-year comparisons.
Study Results
CHANGES IN WORKFORCE PATTERNS
We began by examining state-level variation in changes in the home care and nursing home workforce sizes during the period 2009–20 (exhibits 1 and 2). Both workforces are computed per 1,000 people with disabilities. The color scheme indicates increase, decrease, or no real change; light to dark shading within each color grouping indicates the extent of the change.
EXHIBIT 1: Geographic variation in home care workforce changes per 1,000 people with disabilities, 2009–20.
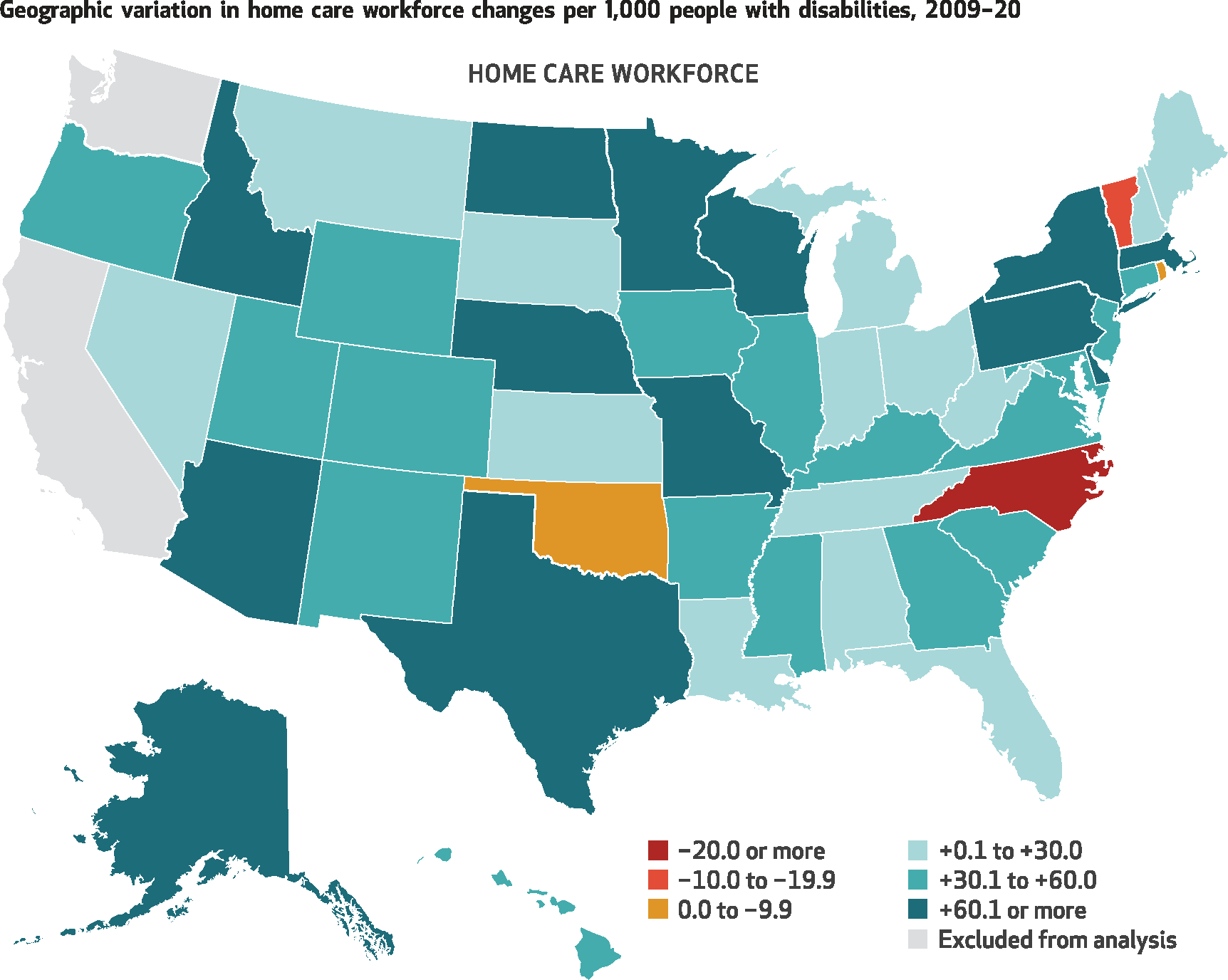
SOURCES Occupational Employment and Wage Statistics program and American Community Survey, 2009–20. NOTE The omission of California and Washington is explained in the text.
EXHIBIT 2: Geographic variation in nursing home workforce changes per 1,000 people with disabilities, 2009–20.
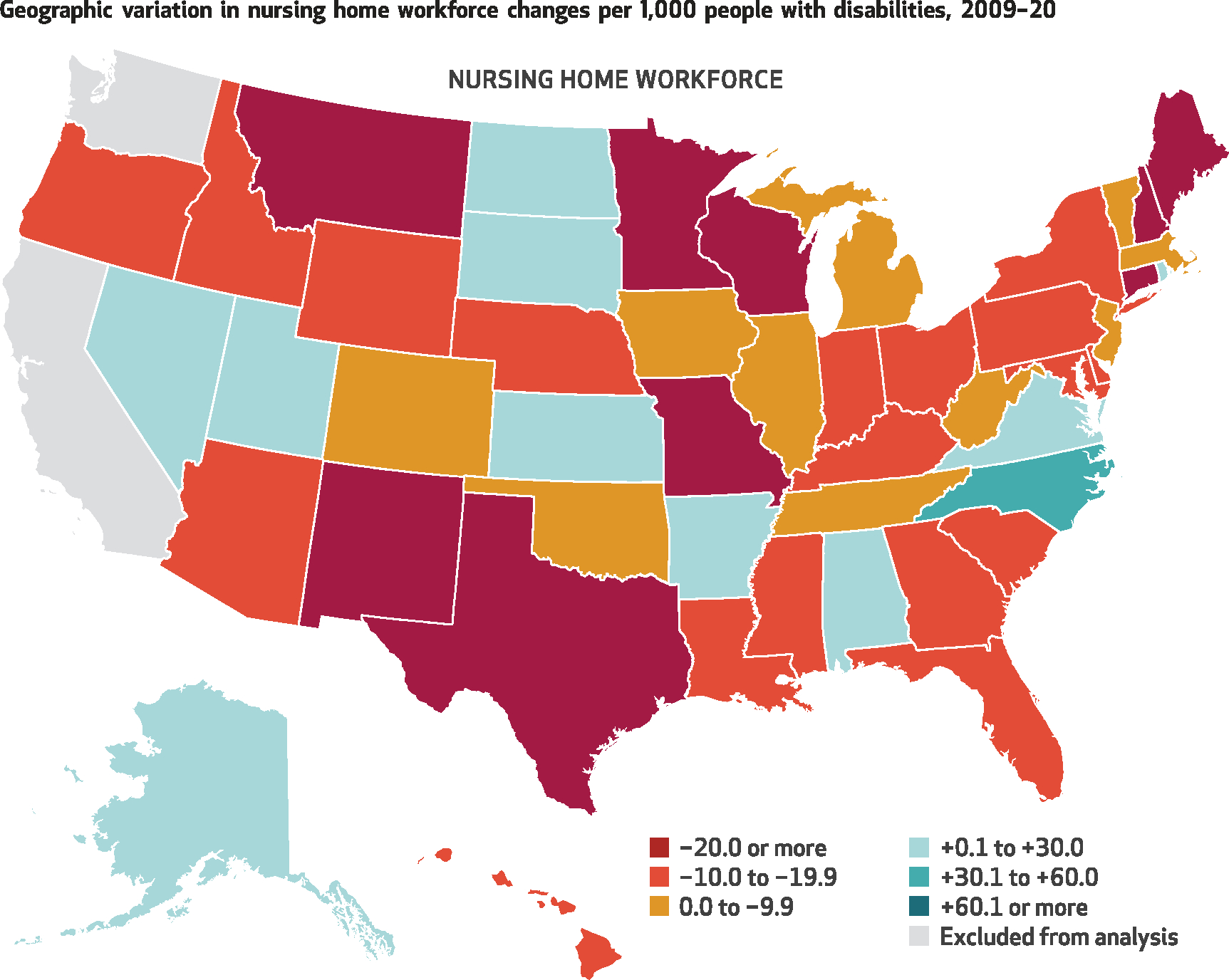
SOURCES Occupational Employment and Wage Statistics program and American Community Survey, 2009–20. NOTE The omission of California and Washington is explained in the text.
There are two points worth noting. First, most states saw an increase in the size of their home care workforce (with only three states experiencing a decline). During the same period, most states experienced a decrease in their nursing home workforce size (with only ten states experiencing an increase). Second, although there are no regional differences that stand out, there is considerable variation in the magnitude of change across states.
WORKFORCE SUBSTITUTION
To explore whether states reduced the size of their nursing home workforces when the home care workforce size increased, we examined the magnitude and direction of the association between change in home care workforce size and change in nursing home workforce size from 2009 to 2020. Exhibit 3 shows a statistically significant (slope = −0.09; p = 0.026) inverse relationship between change in home care workforce size (x axis) and change in nursing home workforce size (y axis). The negative direction suggests substitution: As the home care workforce size increased, the size of the nursing home workforce declined.
EXHIBIT 3: Relationship between change in the number of home care workers and change in the number of nursing home workers per 1,000 people with disabilities in US states from 2009 to 2020.
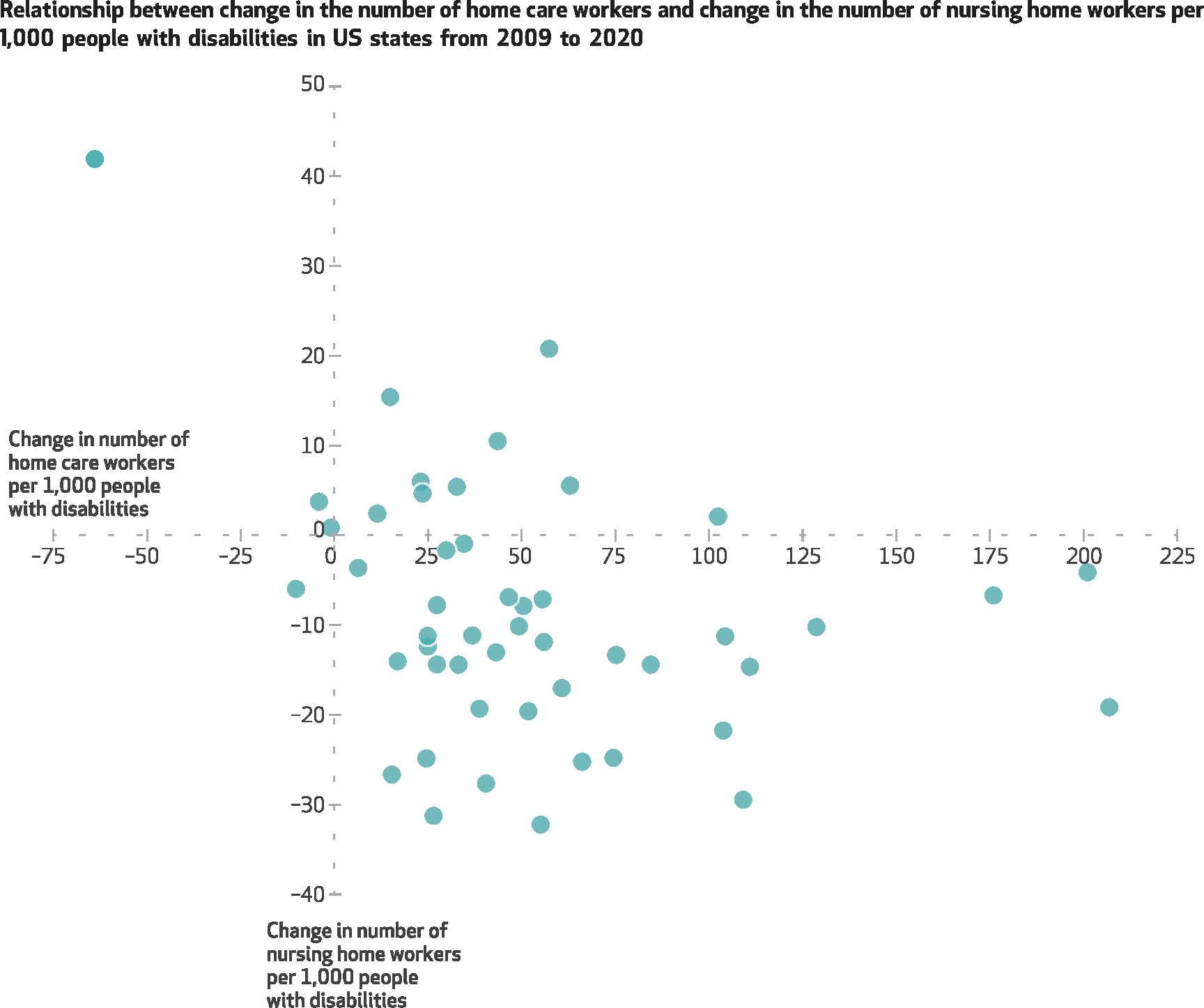
SOURCES Occupational Employment and Wage Statistics program and American Community Survey, 2009–20. NOTES Each dot represents one of forty-nine states (including Washington, D.C.). California and Washington were omitted, as described in the text. The association between change in home care workforce size and change in nursing home workforce size is statistically significant (slope = −0.09; p = 0.026).
CHANGES IN WORKFORCE SIZES OVER TIME
Finally, although we observed considerable state variation in the size of the direct care workforce, a key interest was whether states are converging or diverging over time. Our final analysis incorporated a time element to assess whether states became more similar over time in workforce size. Exhibit 4 groups US states by their 2009 quartiles of home care workforce size (quartile 1 is the lowest, quartile 4 the highest) and plots trends in the home care workforce size for these groups through 2020. During this period, the size of the home care workforce increased overall and for each of the four quartiles. From 2009 to 2020 the overall home care workforce size increased from 100.7 per 1,000 people with disabilities to 160.8 per 1,000. The size of the total home care workforce increased from 1,456,900 to 2,556,060 workers. We also see a divergence, or widening, across the smallest and largest quartiles. Quartile 1 shows an increase, but at a significantly slower pace than quartile 4, and the difference in slopes for these two groups was statically significant (p < 0.001).
EXHIBIT 4: Trends in mean number of home care workers per 1,000 people with disabilities, by quartile of baseline (2009) distribution of workers per 1,000 people with disabilities, 2009–20.
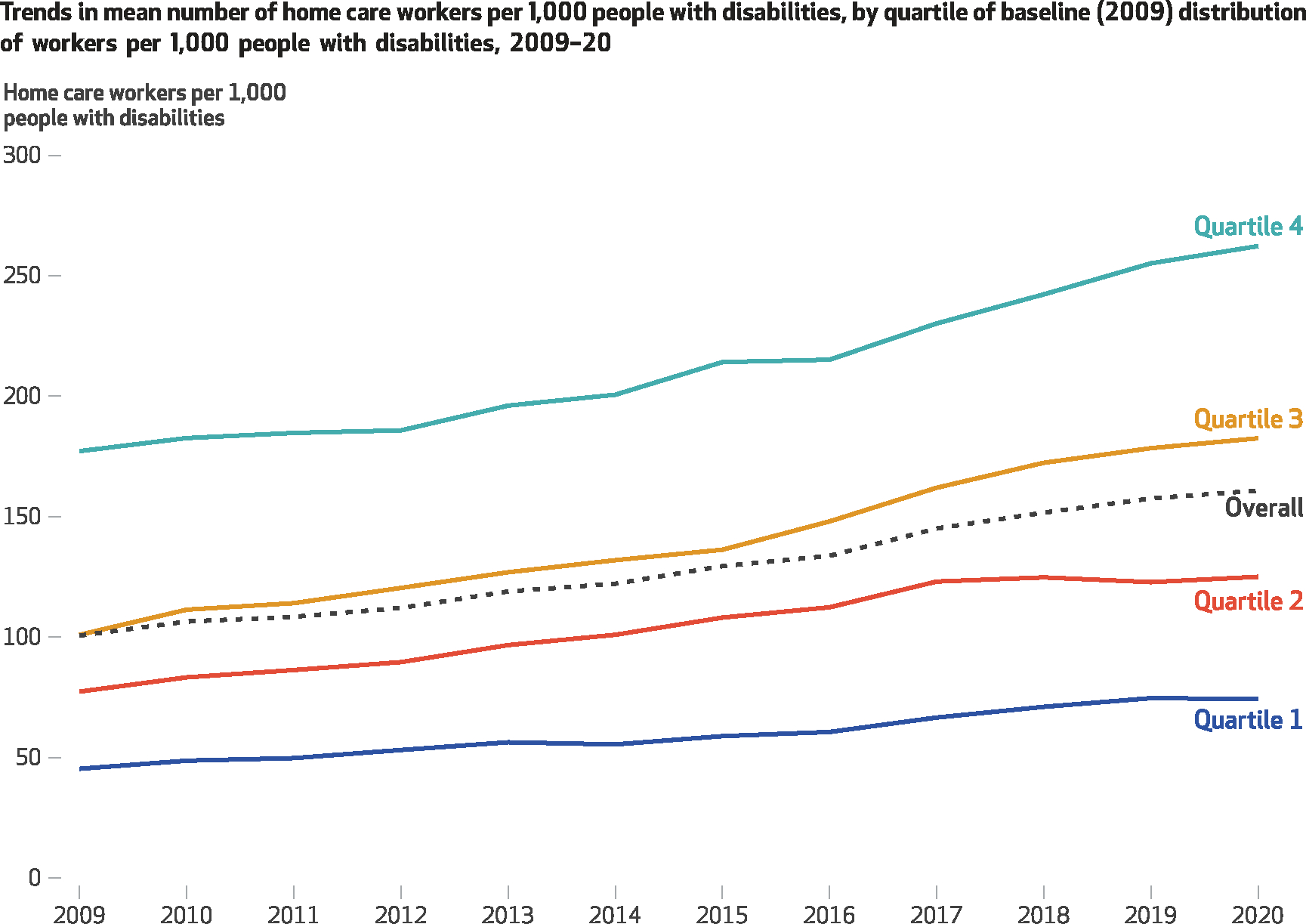
SOURCES Occupational Employment and Wage Statistics program and American Community Survey, 2009–20. NOTES Quartiles 1 and 2 were significantly different from quartile 4, with a bigger positive slope (increase) for quartile 4 (t statistic = 5.25 [p < 0.001] for quartile 1–quartile 4; t statistic = 3.20 [p < 0.001] for quartile 2–quartile 4). The difference between quartiles 3 and 4 was not statistically significant. Change in overall home care workforce size was also statistically significant (slope = 5.74; p < 0.001).
Appendix exhibit S-2 presents a similar figure with nursing home workforce size quartiles.11 The rate of change for the nursing home workforce quartiles was much smaller than that of the home care workforce.
SENSITIVITY ANALYSES
Because of changes in workforce classifications in the data in 2017, we dropped California and Washington from the analyses. In a sensitivity analysis depicted in appendix exhibit S-3,11 we examined trends between 2009 and 2016 with all states included in the analysis. Although the levels changed, the trends were consistent with those for analyses through 2020 without those two states.
Discussion
We examined how the direct care workforce has changed over time and assessed whether states that had lagged in the provision of home and community-based services (measured as being in the lowest quartile of their home care workforce size) have begun to catch up or whether leading states continue to move forward in their service provision. We showed that between 2009 and 2020 most states increased their home care workforce size, but there was substantial state variation in whether and how much the home care workforce grew. In addition, we found that states that increased their home care workforces also decreased their nursing home workforces, although substitution was not one-to-one. The home care workforce has been increasing at a substantially faster rate than nursing home workforce has been declining. Between 2009 and 2020 there was an increase of about sixty home care workers per 1,000 people with disabilities and a decrease of about ten nursing home workers per 1,000 people with disabilities. This pattern was observed for thirty-six of the forty-nine states examined (including Washington, D.C.). Although the reasons for these divergent trends are beyond the scope of this study, future work could explore why the home care workforce has been growing while the nursing home workforce is declining. Our key question is whether there has been a convergence in states over time: Are lagging states on a trajectory to catch up? Our findings suggest that this has not been the case. We see a clear divergence over time across the smallest and largest quartiles of home care workforce size.
Of the forty-nine states (including Washington, D.C.) included in this analysis, those showing the most growth in home care workforce size since 2009 were New York, Massachusetts, and Washington, D.C., with increases of 207, 201, and 175 home care workers per 1,000 people with disabilities between 2009 and 2020, respectively. Four states (North Carolina, Oklahoma, Rhode Island, and Vermont) showed a decrease in their home care workforces during this period.
There are many ways for states to organize, finance, and deliver long-term care across settings that could explain some of the differences we saw across states. One factor that could explain differences among states is higher wages for home care workers in some states than in others, including pass-through wage requirements, which require agencies to pass increased reimbursement directly to workers.12 There are also eight states in which individual providers paid by Medicaid are represented by the Service Employees International Union in collective bargaining, which means that there is a higher, union-negotiated hourly rate in those states. In some states there are career ladders for direct care jobs with additional pay if aides take advanced training. Aides may also receive additional compensation for mentoring new aides. Nonetheless, wages for home care workers, even in these better-paying states, still might not be that competitive compared with those for other jobs available to low-skill workers.13
Some states also have more stringent requirements for training and certification that could keep people out of the home care workforce. At the same time, increased entry-level training and career advancement opportunities are associated with job satisfaction and retention for direct care workers;14 these opportunities could vary by region or state. In addition, differences in workforce size could be influenced by state differences in wage and work hour protections for home care workers15 and differences in work hours and overtime pay resulting from differences in Medicaid policy.16 States also differ in their percentages of foreign-born residents, who constitute just under one-third of the home care workforce nationally.8 In contrast, the nursing home workforce includes a substantial but smaller share of immigrants.8
Data limitations may be partly responsible for some of the differences we saw. North Carolina and Rhode Island, for instance, might show a reduction in home care workers because many direct care workers providing home care services must be certified as nursing assistants in those states. This could suggest that some home care workers may be mistakenly classified as nursing home workers in these states. However, it is unlikely that certified nursing assistants would be guiding the trend in both states because in 2018 only 5.5 percent of nursing assistants worked in the home health care industry, according to the Occupational Employment and Wage Statistics program occupation profile data.
The extent to which the long-term care workforce supply will meet demand is an important issue. The trends we examined here reflect workforce trends since 2009. Attitudes among baby boomers (for example, preferences for aging in place) suggest that even greater demand for home and community-based services might be forthcoming as this cohort ages.1 The development and sustainment of an adequate workforce is one of several necessary improvements to the nation’s long-term services and supports system.17 The COVID-19 pandemic may further exacerbate the supply and demand imbalance if consumers’ preferences for aging in place have shifted as a result of the high rates of mortality associated with institutional settings such as nursing homes during the pandemic.
We show that size of the home care workforce varies by state and that states are becoming more unequal in their home care workforce sizes over time. Future research is needed to explore policy levers that may alter home and community-based services workforce supply, such as Medicaid “rebalancing” programs, programs that increase the availability of assisted living facilities, Medicaid and related policies that affect the number of nursing facility beds, and programs that support higher wages for home care and personal care aides relative to nursing home aides.
Conclusion
Although the home care workforce has grown since 2009, there continue to be vast disparities across states in workforce size even after the number of people with disabilities is accounted for. The widening inequality across states in their home care workforce sizes between 2009 and 2020 suggests a need to understand the drivers of these disparities and to formulate policies that can ensure that older adults and people with disabling conditions will have their needs met in their desired setting.
Supplementary Material
Acknowledgments
This work was supported by the National Institutes of Health under Grant No. R01MD010360 (principal investigator: Regina Shih). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Esther M. Friedman, Institute for Social Research, University of Michigan, in Ann Arbor, Michigan..
Madhumita Ghosh-Dastidar, ESS, RAND Corporation..
Teague Ruder, Research Programming Group, RAND Corporation..
Daniel Siconolfi, Behavioral and Policy Sciences (BPS), RAND Corporation..
Regina A. Shih, BPS, RAND Corporation..
NOTES
- 1.Binette J, Vasold K. 2018 home and community preferences: a national survey of adults ages 18-plus [Internet]. Washington (DC): AARP Research; 2018. Aug [last updated 2019 Jul; cited 2021 Oct 12]. Available from: https://www.aarp.org/research/topics/community/info-2018/2018-home-community-preference.html [Google Scholar]
- 2.Musumeci M, Claypool H. Olmstead’s role in community integration for people with disabilities under Medicaid: 15 years after the Supreme Court’s Olmstead decision [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2014. Jun 18 [cited 2021 Oct 12]. Available from: https://www.kff.org/medicaid/issue-brief/olmsteads-role-in-community-integration-for-people-with-disabilities-under-medicaid-15-years-after-the-supreme-courts-olmstead-decision/ [Google Scholar]
- 3.Eiken S, Sredl K, Gold L, Kasten J, Burwell B, Saucier P. Medicaid expenditures for long-term services and supports in FFY 2012 [Internet]. Baltimore (MD): Centers for Medicare and Medicaid; 2014. Apr 28 [cited 2021 Oct 12]. Available from: http://www.advancingstates.org/sites/nasuad/files/LTSS_Expenditures_2012.pdf [Google Scholar]
- 4.Spetz J, Trupin L, Bates T, Coffman JM. Future demand for long-term care workers will be influenced by demographic and utilization changes. Health Aff (Millwood). 2015;34(6):936–45. [DOI] [PubMed] [Google Scholar]
- 5.Collelo KJ. Who pays for long-term services and supports? [Internet] Washington (DC): Congressional Research Service; 2018. Aug 22 [cited 2021 Oct 12]. Available from: https://sgp.fas.org/crs/misc/IF10343.pdf [Google Scholar]
- 6.Musumeci M, Watts MO, Chidambaram P. Key state policy choices about Medicaid home and community-based services [Internet] San Francisco (CA): Henry J. Kaiser Family Foundation; 2020. Feb 4 [cited 2021 Oct 12]. Available from: https://www.kff.org/medicaid/issue-brief/key-state-policy-choices-about-medicaid-home-and-community-based-services/ [Google Scholar]
- 7.Scales K It’s time to care: a detailed profile of America’s direct care workforce [Internet]. Bronx (NY): PHI; 2020. Jan 21 [cited 2021 Oct 12]. Available for download from: https://phinational.org/resource/its-time-to-care-a-detailed-profile-of-americas-direct-care-workforce/ [Google Scholar]
- 8.PHI. U.S. Direct care workers in the United States: key facts [Internet]. Bronx (NY): PHI; 2020. [cited 2021 Oct 26]. Available for download from: https://phinational.org/resource/direct-care-workers-in-the-united-states-key-facts/ [Google Scholar]
- 9.Government Accountability Office. Long-term care workforce: better information needed on nursing assistants, home health aides, and other direct care workers [Internet] Washington (DC): GAO; 2016. Sep 15 [cited 2021 Oct 12]. (Report No. GAO-16–718). Available from: https://www.gao.gov/products/gao-16-718 [Google Scholar]
- 10.Bureau of Labor Statistics. Occupational Employment and Wage Statistics [Internet] Washington (DC): BLS; [cited 2021 Oct 12]. Available from: https://www.bls.gov/oes/ [Google Scholar]
- 11.To access the appendix, click on the Details tab of the article online.
- 12.Baughman RA, Smith K. The effect of Medicaid wage pass-through programs on the wages of direct care workers. Med Care. 2010;48(5):426–32. [DOI] [PubMed] [Google Scholar]
- 13.Espinoza R Would you stay? Rethinking direct care job quality [Internet]. Bronx (NY): PHI; 2020. [cited 2021 Oct 12]. Available for download from: https://phinational.org/caringforthefuture/wouldyoustay/ [Google Scholar]
- 14.Coogle CL, Parham IA, Jablonski R, Rachel JA. Enhanced care assistant training to address the workforce crisis in home care: changes related to job satisfaction and career commitment. Care Manag J. 2007;8(2):71–81. [DOI] [PubMed] [Google Scholar]
- 15.Government Accountability Office. Fair Labor Standards Act: observations on the effects of the home care rule [Internet]. Washington (DC): GAO; 2020. Oct 19 [cited 2021 Oct 12]. (Report No. GAO-21–72). Available from: https://www.gao.gov/products/gao-21-72 [Google Scholar]
- 16.Iezzoni LI, Gallopyn N, Scales K. Historical mismatch between home-based care policies and laws governing home care workers. Health Aff (Millwood). 2019;38(6):973–80. [DOI] [PubMed] [Google Scholar]
- 17.Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, Johnson KS. Actualizing better health and health care for older adults. Health Aff (Millwood). 2021;40(2):219–25. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


