Abstract
Optimum serotonin level in the serotonergic synapses of the central nervous system (CNS) is related to mood, behavior, and sleep. Serotonin syndrome (SS) is a rare yet very dangerous adverse effect resulting from increased serotonin in CNS. The diagnosis of SS is based on the presence of clinical symptoms, which can include agitation, confusion, rapid heart rate, high blood pressure, dilated pupils, muscle rigidity, tremors, sweating, and diarrhea. SS is invariably caused by inadvertent use of serotonergic medicines. There is an ever-growing list of medicines that are associated with the risk of SS. Some of the common classes of drugs that can contribute to the development of SS include selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, tricyclic antidepressants, stimulants (e.g., amphetamines and cocaine), lithium, opioids, drugs used for recreational purposes like ecstasy Methylenedioxymethamphetamine (MDMA), and some herbal supplements (e.g., St. John’s Wort). SS can occur when these medications are taken alone or in combination, especially when a new medication is added, or the dose of an existing medication is changed. The management of SS typically involves discontinuing the use of the substance that caused the excess serotonin levels and providing supportive care, such as intravenous fluids and electrolytes. In severe cases, benzodiazepines may be used to control agitation and muscle rigidity, while serotonin antagonists, such as cyproheptadine, may be used to reduce serotonin levels. The literature review points to a general unawareness among physicians about the condition or drugs associated with it. Consequently, this potentially fatal condition is overlooked. There is a need for regular information updates and reminders to all those who prescribe medications to the patients.
Keywords: Selective serotonin reuptake inhibitors, serotonin, serotonin syndrome
Introduction
Serotonin syndrome (SS) is a potentially life-threatening condition caused by an excess of serotonin, a neurotransmitter in the central nervous system (CNS). It is usually associated with starting or dose adjustments of serotonin receptor reuptake inhibitors (SSRIs) and other serotonergic drugs, especially when serotonergic drugs are inadvertently used in combination. The literature indicates a dearth of knowledge about this syndrome, its presentation, its management, and its prevention. This review will help to increase the awareness of healthcare professionals of this syndrome that is on the rise as a result of the increasing use of serotonergic substances that include medications, food supplements as well as recreational drugs.
Methodology
The objective of this review of the available literature on SS is to increase awareness of this often-neglected side effect of serotonergic medicines. A literature search was made in PubMed for literature published from 2003 to 2023 (20 years) using the keywords “serotonin,” “serotonin syndrome,” and “serotonergic medicines.” In addition, we used specific keywords and MeSH terms to discover case reports and studies reported from the region (Middle East and EMRO region). We reviewed the literature about risk factors and particularly drug–drug interactions leading to serotonin surge. Finally, we consulted various reference books to review the essentials of diagnosis and best evidence for available treatment options.
Results of Literature Search
Serotonin (5HT), an important neurotransmitter, is derived from tryptophan and its metabolism is mainly by monoamine oxidase (MAO) to 5-hydroxyindolacetic acid. It is mainly produced in the neurons of CNS, enterochromaffin cells of the gastrointestinal tract (GIT), and platelet granules.[1] In the CNS, it is associated with control of mood, behavior, and sleep, while in the GIT, it has a secretomotor role along with other control mechanisms. It has been associated with many other functions including (but not limited to) bone health, coagulation of blood, platelet aggregation, and vascular resistance.[2]
Serotonin action is mediated through seven types of receptors (5-HT1-5-HT7) that are distributed throughout the body. “Serotonergic” is a term that describes anything that has serotonin-like actions, and it operates through the serotonin receptors to Affect a variety of body functions.[3]
Serotonergic neurons originate in the brain stem from dorsal and median raphe nuclei. They then pass through the medulla to the spinal cord. In addition, they are projected to the cerebellum, limbic system, striatum, and cortex. Although these serotonin-dependent neurons number <1% of total brain neurons, their anatomical distribution to the key components of the CNS enables them to influence a wide variety of body functions. These functions include but are not limited to sleep, appetite, and mood. This set of functions is the reason for the link of decreased serotonin with many psychological conditions including insomnia and depression, and the converse, of an increased serotonergic activity that may lead to anorexia and weight loss.[4] Most of the serotonin is removed from the synaptic clefts by “reuptake” after performing its function. Reuptake is then followed by recycling. Different factors related to synthesis, reuptake, recycling, and release might lead to low levels of serotonin in the CNS, which is linked to depression and other mood disorders. The same steps are pivotal in the mechanism of action of different medications used to restore serotonin levels to improve these conditions.
The serotonin syndrome
SS usually presents as a potentially life-threatening combination of changed mental status along with autonomic hyperactivity, hemodynamic manifestations, and neuromuscular problems. This presentation results from initiation, dosage change, or the use of combinations of serotonergic substances, possibly pharmaceutical agents, herbs, recreational drugs, or even food supplements. There is evidence that the frequency of SS is on a rise after the multifold increase in the use of drugs that interfere with production, reuptake, or metabolism of serotonin. Likewise, the evidence indicates that there is not much awareness of SS by physicians.[5]
Pathophysiology
SS is the result of an increased concentration of serotonin in the synaptic clefts owing to a variety of drugs. The major cause of the symptoms and signs is increased and sustained stimulation of 5-HT1A receptors in the medulla and central gray nuclei. There is a significant role of 5HT2A receptors as well. Very little data are available in most countries about the exact frequency of SS, its determinants, and its presentation. However, the available data from advanced healthcare systems indicate an increased frequency of SS after the introduction of new serotonergic drugs the world over. Most reported cases are the result of polypharmacy, but cases have been reported with monotherapy as well, especially by overdosing. The combined use of some serotonergic drugs that form the backbone of treatment of neurological or psychological problems is, therefore, the major risk factor for SS.[6]
A number of drugs can cause SS [Table 1], and this number is growing as more cases are reported. Many of these drugs are not even marketed as serotonergic agents [like some of the medicines shown in Table 2], although they have potent serotonergic activity when used in combination. These include but are not limited to over-the-counter flu medicine dextromethorphan, opiate analgesic tramadol, antiemetic ondansetron, and even antimicrobials like linezolid [Table 2].[6,7,8,9] The drugs that have been linked directly with SS include MAO inhibitors (MAOIs), serotonin–norepinephrine reuptake inhibitors (SNRIs), SSRIs, and tricyclic antidepressants (TCAs). In addition, a variety of other drugs such as antipsychotics, anticonvulsants, antiparkinsonian agents, antimigraine agents, triptans, some analgesics, buspirone, dextromethorphan, some antibiotics (like linezolid), some herbal products (e.g., St. John’s Wort), and drugs of abuse (e.g., cocaine and ecstasy) are also associated with SS.[6] Cases are most frequent when two or more antidepressant drugs from different pharmacologic classes are taken together. There have been occasions when patients presenting with SS have died as a result of medicines given to control symptoms of SS.[10]
Table 1.
Serotonergic drugs classified by mechanism of enhancing serotonin in synapses
| Pharmacological action leading to increased serotonin level | Examples of drugs/drug groups |
|---|---|
| Increase in production of serotonin | Cocaine, L-tryptophan, phentermine |
| Increased release from presynaptic terminals | Tramadol, meperidine, oxycodone, phentermine, MDMA, mirtazapine, dextromethorphan, L-DOPA |
| Inhibition of serotonin reuptake | SSRIs, TCAs, SNRIs, opiates, cocaine, MDMA, dextromethorphan, chlorpheniramine, phentermine, bupropion, trazodone, nefazodone, ondansetron, granisetron, St. John’s Wort |
| Decrease/inhibit serotonin degradation | MAO inhibitors, triptans, buspirone, St. John’s Wort |
| Inhibition of microsomal oxidases (cytochrome-P450) | Fluconazole, citalopram, methadone, oxycodone, venlafaxine, ciprofloxacin, ritonavir, fluoxetine, sertraline, dextromethorphan, phentermine, tramadol, risperidone |
| Serotonin receptor activation | Lithium, buspirone, mirtazapine, trazodone, triptans, dihydroergotamine, fentanyl, meperidine, metoclopramide, LSD |
The data for this table were acquired from different resources including, but not limited to, Buckley et al. and Volpi-Abadie et al. SSRIs=Selective serotonin reuptake inhibitors, TCAs=Tricyclic antidepressants, SNRI=Serotonin–norepinephrine reuptake inhibitors, MAO=Monoamine oxidase, MDMA=Methylenedioxymethamphetamine, LSD=Lysergic acid diethylamide
Table 2.
Combination of drugs known to cause excessive serotonin
| Drug group/drug | SSRIs | SNRIs | MAOIs | TCAs | Opiates | Triptans | Combinations with excessive evidence |
|---|---|---|---|---|---|---|---|
| SSRIs | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Most SSRIs with L-tryptophan Fluoxetine with carbamazepine, fentanyl, phentermine |
| SNRIs | ✓ | ✓ | ✓ | ✓ | ✓ | Venlafaxine alone or in combination with amitriptyline, calcineurin inhibitors, fluoxetine, lithium, meperidine, methadone, mirtazapine, quetiapine, sertraline, tramadol, tranylcypromine, trazodone | |
| MAOI | ✓ | ✓ | ✓ | ✓ | ✓ | - | Phenelzine with meperidine Tranylcypromine with imipramine Methylene blue with paroxetine, clomipramine |
| TCAs | ✓ | ✓ | ✓ | - | - | - | - |
| Opiates | ✓ | ✓ | ✓ | - | - | ✓ | Tramadol alone or with mirtazapine, olanzapine |
| Dextromethorphan | ✓ | - | - | - | - | - | Amitriptyline Chlorpheniramine Risperidone |
| Buspirone | ✓ | - | - | - | - | - | - |
| Mirtazapine | ✓ | - | - | - | - | - | - |
| Linezolid | ✓ | - | - | - | - | Tapentadol | |
| Olanzapine | - | - | - | - | - | Lithium Citalopram |
|
| Trazodone | - | - | - | - | - | Amitriptyline Lithium |
|
| Risperidone | - | - | - | - | - | Dextromethorphan Fluoxetine Paroxetine |
|
| Ciprofloxacin | - | - | - | - | - | Venlafaxine, methadone | |
| Fluconazole | - | - | - | - | - | Citalopram |
Tick mark means that the group on left side in combination with group/drug on column title may cause Serotonin Syndrome. SSRIs=Selective serotonin reuptake inhibitors, SNRIs=Serotonin–norepinephrine reuptake inhibitors, MAOI=Monoamine oxidase inhibitors, TCAs=Tricyclic antidepressants
Mechanisms include increased serotonin production (L-tryptophan), decreased reuptake (e.g., SSRIs, chlorpheniramine, cyclobenzaprine, and dextromethorphan), decreased metabolism (e.g., isocarboxazid, linezolid, methylene blue, phenelzine, selegiline, and tranylcypromine), enhanced release (e.g., dextromethorphan, meperidine, mirtazapine, methadone, methylenedioxymethamphetamine also known as MDMA, or ecstasy), and stimulation of serotonergic receptors (e.g., buspirone, dihydroergotamine, and lithium).[6,7,8,9] Different drugs act at the different steps of synaptic transmission; however, the ultimate effect is to increase the level of serotonin. TCAs inhibit the reuptake of serotonin in synaptic cleft, MAOIs prevent the metabolism of serotonin in nerve terminals, while cocaine inhibits the reuptake of serotonin in the synaptic cleft. In addition, the serotonergic drugs are metabolized by the cytochrome P450 family of enzymes. If the activity of cytochrome P450 enzymes is compromised, the metabolism of some serotonergic drugs may be reduced leading to increased chances of SS.[11] These mechanisms and associated drugs are summarized in Table 1.
Patients who are prescribed larger doses of the serotoninergic drugs are especially at risk, and SS generally appears within a day of exposure to the causative factor. Differentiating SS from other syndromes with similar presentation is quite difficult. As reflected in Figure 1, some neurological manifestations of diseases such as neuroleptic malignant syndrome, malignant hyperthermia, anticholinergic toxicity, and CNS effects of some infectious diseases, such as meningitis and encephalitis, very closely match SS.[12]
Figure 1.
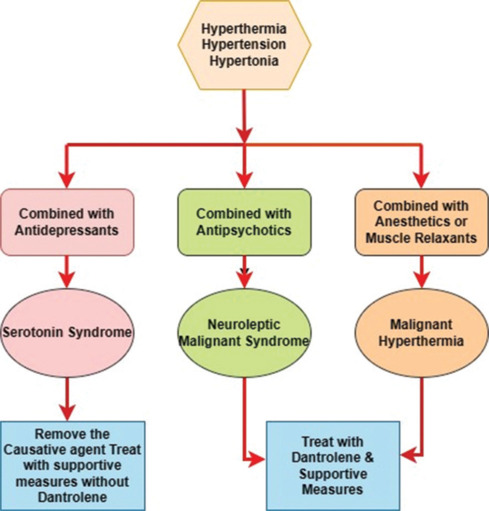
Conditions mimicking serotonin syndrome
Special link of serotonin receptor reuptake inhibitors with serotonin syndrome
SSRIs act by inhibiting the reuptake of serotonin back into the presynaptic neurons, making more serotonin available for sustained neuronal activity. This helps in better impulse transmission in the neurons with subnormal serotonin. This has a miraculous effect if these neurons are related to the control of mood, behavior, or sleep. SSRIs are preferred as they are “selective” for serotonin only and are generally well tolerated with relatively fewer side effects. The most severe complication is SS that is rare but potentially fatal if not diagnosed promptly and managed.
SSRIs act by increasing serotonin levels in the brain. They are considered the best-known treatment of depression. In addition, they have proved their worth in the management of other psychological diseases including, but not limited to, anxiety, panic disorder, posttraumatic stress disorder, phobias, and even eating disorders like bulimia.[13] This has led to a trend of prescribing them as the first-choice medicine for psychiatric disorders.
In the USA, the SSRIs approved by the Food and Drug Administration (FDA) are citalopram, escitalopram, fluoxetine, paroxetine, and sertraline. Sertraline (Zoloft) is the most commonly prescribed medication for psychiatry patients in the USA. It is also the 14th in the list of all prescription medicines in the USA. Likewise, most of the approved SSRIs are in the top 25 prescribed psychiatric drugs.[14] An interesting study carried out in Pakistan to determine “Which antidepressant would psychiatrists from a developing country choose for themselves in a depressive illness?” reported that fluoxetine was the first choice of the interviewed psychiatrists if they ever needed it, followed by escitalopram and then TCAs. The major reason for the choice of SSRIs was the experience of their efficacy and safety.[15] Unfortunately, commercial interests in countries with little or no drug control have led to unchecked prescribing by healthcare professionals who are either unaware of the side effects or are unqualified to prescribe.
Selective SSRIs are being increasingly prescribed to children and adolescents all over the world.[16] SSRIs are generally the first-line medication for depression in children and adolescents because of the less chance of side effects and the convenience of once-a-day dose. Some regulators in various countries have identified the minimum age below which SSRI cannot be given (like 7 years by the FDA) or medicines that can or cannot be prescribed to the pediatric age group. Fluoxetine is most extensively studied and recommended for use in the pediatric age group, but sertraline, escitalopram, citalopram, fluvoxamine, and paroxetine are also recommended.[17] Therefore, both drug and patient factors such as age and body mass index of the patient may contribute to adverse effects, especially in the pediatric age group. This increases the vulnerability of countries with poor regulation of healthcare systems to preventable conditions like SS. A significant study based on an analysis of 2400 outpatient department prescriptions in a tertiary care hospital of a developing country identified SS as a significant potential drug–drug interaction, although the authors did not include any of the SSRIs or SNRIs in the top 30 prescribed medicines.[18]
Presentation and diagnosis of serotonin syndrome
SS is very much underdiagnosed mainly because it is not caused by only one type or even class of drugs, and the overlap of its symptoms with many neurological and general conditions [Figure 1] and the range of its symptoms make diagnosis difficult, especially in the absence of proper history of medication or substance use.[19]
Sometimes, the symptoms of SS typically begin within a few hours of the start of a new medicine, addition of a medicine, or alteration in the dosage. A significant proportion (67%) of cases report mild-to-moderate symptoms within 6 h of the start of medication, an alteration in the dosage, or an overdose. Likewise, most (75%) report to a healthcare facility within 24 h of the triggering event.[20,21,22] Rapidly increasing temperature and rigidity of muscles are of course a real emergency in these patients as multiorgan failure can occur within very short time.[22]
The most important in the diagnosis is the history of drugs being used, or recently started, or recent dose adjustment. In order to decrease morbidity and mortality, it is important to suspect SS if a patient using a serotonergic agent presents with any new symptom or deterioration of previously reported symptoms.[23] There is evidence of SS developing many weeks the after date of discontinuation of some long-acting serotonergic medicines such as fluoxetine, isocarboxazid, and phenelzine. Therefore, asking for the history of previous medicine use should extend to a few months.
The diagnosis of SS is totally based on careful history-taking and clinical examination. The laboratory tests are done to exclude other similar conditions. In the past, the popular sets of criteria based on clinical assessment and judgment were “Sternbach’s criteria”[24] and “Radomski’s criteria.”[25] However, those that are now extensively used are called Hunter Serotonin Toxicity Criteria [Figure 2] and have been reported to have around 84% sensitivity and 97% specificity.[22]
Figure 2.
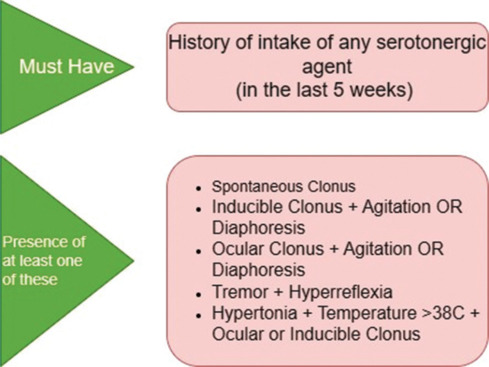
Hunter’s criteria for diagnosis of serotonin syndrome
Hunter’s Serotonin Toxicity Criteria SS uses the “triad” of clinical features:
Cognitive OR changes in the mental status: For example, nervousness (agitation), delirium, hallucinations, confusion, hyperactivity, hypomania, and hypervigilance
Neuromuscular abnormalities: Most common among them is clonus that may be inducible or spontaneous, ocular clonus, exaggerated reflexes (hyperreflexia), hypertonia, muscle spasms, rigidity, tremors, shivering, restlessness, and rhabdomyolysis
Symptoms of autonomic hyperactivity: For example, fever, diaphoresis, diarrhea, flushing, increased or decreased blood pressure, increased bowel sounds, mydriasis, tachypnea, and tachycardia.
Agitation is one of the most common and major symptoms of SS. It is accompanied by some neurological signs such as tremor, hypertonia, hyperreflexia, and clonus that need careful observation and neurological examination. Many physicians fail to note these essentials of neurological examination as they do not suspect the condition.[26] The most severe cases get fits, coagulopathies, rhabdomyolysis, and renal or multiorgan failure.[27]
SS can pose a special diagnostic challenge in the pediatric population because of a variety of presentations. A recent study reviewed all the literature on SSRI-related SS (n = 18 case reports) in children aged 4–18 years. The most frequent symptoms were again agitation, confusion, hyperreflexia, rigidity, tachycardia, hypertension, and tremor. In the 18 cases reviewed, SS developed after the first dose in 7 cases, the result of an overdose in 5 and in 6 instances in which SSRI was given in combination with some other serotonergic agent. This study recognized high starting doses and polypharmacy as the potential risk factors in the pediatric age group.[16]
Likewise, the diagnosis is often challenging in patients with severe neurological or psychological conditions as well as noncooperative patients or those in nursing homes. Unfortunately, all these classes of patients are at risk of polypharmacy and SS. Another class that is often overlooked is fitness freaks who use dietary supplements, try to lose weight with medicines, and have associated psychological issues for which they use prescription medicines. The mix of serotonergic medicines with serotonergic dietary supplements in otherwise fit persons puts them in a high-risk category.
SS has a presentation similar to neuroleptic malignant syndrome, but causative medicines are different. SS results from the use of serotonergic drugs, but the dopamine antagonists are the usual cause of neuroleptic malignant syndrome. In addition, the onset of SS syndrome is within 24 h of medication intake while neuroleptic malignant syndrome has a much slower onset that may extend up to 2 weeks of the start or modification of therapy [Figure 1].[28]
Management of serotonin syndrome
The mechanism of improvement of SS is clearly linked to the restoration of normal levels of serotonin achievable by the discontinuation of the offending agent in mild cases. Careful management ensures good prognosis in most cases of severe SS as long as rhabdomyolysis or organ failure has not set in. When the offending substance(s) are stopped and the patient is given supportive care, mild-to-moderate cases usually resolve on their own within 24–72 h. Improvement in severe instances might take longer. Choosing a medication that does not worsen the condition is really difficult. Supportive care, drug withdrawal, and the use of some drugs, like 5 mg of diazepam intravenously to control hypertonicity and neuronal overexcitation, may be adequate for minor symptoms. Patients with severe symptoms may require sedation and induction of paralysis along with intubation. Antipyretic therapy is typically not advised because in SS, fever is brought on by increased muscle activity and not as a result of a resetting of temperature set point in the hypothalamus. Intravenous (IV) administration of chlorpromazine is also recommended in severe SS.[29,30,31] Serotonin antagonist drugs such as cyproheptadine and chlorpromazine might be useful. Cyproheptadine that is a specific 5-HT 2A receptor antagonist in an oral dose of 4 mg is considered an antidote for the effects of raised serotonin in SS.[32,33]
After making the diagnosis and removal of the causative agent, supportive treatment only is enough for most of the cases and complete resolution of symptoms occurs within 24 h. However, most patients need monitoring in intensive care during this initial recovery period. They might need oxygen, IV fluids, continuous monitoring of QTc and QRS duration in electrocardiogram, and airway support. In SS with hyperthermia (>40°C), active external cooling is most beneficial as the fever originates from increased muscle activity and antipyretics are of no benefit. Instead, paralytic medicines might help in reducing the fever by decreasing muscular activity. Benzodiazepines are useful for many of the neurological and neuromuscular symptoms of SS including agitation. Dexmedetomidine may also be useful for both hemodynamic instability and agitation. Antihypertensive medicines such as clevidipine and esmolol can be used to manage high blood pressure. There is also evidence of the use of cyproheptadine, a serotonin antagonist, and mirtazapine, a 5-HT3 and 5-HT2 antagonist in SS. However, some medicines must be avoided. These include chlorpromazine, propranolol, bromocriptine, olanzapine, and dantrolene.[5] There is evidence that improper selection of therapy sometimes leads to even more increase in serotonin level in patients presenting with SS.
Awareness about serotonin syndrome and prevention
Ignorance of physicians about SS, limited knowledge of combination of drugs that may lead to SS, and the lack of care in starting or altering the dosage of serotonergic drugs are the main causes of this purely iatrogenic syndrome. Since this syndrome was first identified in the 1960s, there has been no improvement on knowledge. Most cases never get reported, though occasionally one or two cases are made public. “A case that shook medicine” was the moniker given to one such incident that occurred in October 1984. An 18-year-old college student Libby Zion was brought to a hospital in New York with agitation, fever, confusion, and jerky body movements. She was receiving phenelzine treatment for depression. She was given meperidine to calm her and stop her muscular hyperactivity. Later, as her nervousness increased, she was administered a haloperidol injection. Her temperature shot up to 107°F. All the attempts to reduce hyperthermia failed, and she died of cardiac arrest.[9] This case stands out as an example of ignorance of SS and its management even in the most advanced healthcare systems.
In a survey carried out in the general practitioners (GPs) in the late 1990s, about 85% of the responding physicians were not aware of the SS as a disease entity.[34] Another study carried out 40 years later in 2020 to assess the knowledge, attitude, and practice about SS in 150 neurophysicians found that only 31% of responders could correctly identify the criteria for SS. Just 17% were aware about clonus being one of the most important diagnostic criteria. The state of knowledge about drugs linked to SS or drugs used in the management of SS was much the same.[19] The study pointed out that even neurophysicians lacked awareness of the seven main clinical features of the “Hunter’s criteria,” namely agitation, tremor, fever, diaphoresis, clonus (spontaneous, induced, or ocular), hyperreflexia, and hypertonia or rigidity.[19]
A study that assessed the knowledge and awareness of common psychiatric disorders and medications used by GPs in Karachi, Pakistan, found that most GPs lacked knowledge of recognized diagnostic categories for most mental disorders. In addition, their choice of drugs for mental disorders was not based on recommended standard practice. Only 35.1% of them were familiar with the proper use and side effects of SSRIs while 75.3% of them were well aware about benzodiazepines. This was reflected by the frequency of prescribing benzodiazepines as well.[35]
The clinician must have clear knowledge of the early symptoms of SS, e.g., cognitive changes in patients on serotonergic drugs. They must keep in mind that complaints of agitation and restlessness in a patient may be iatrogenic and not part of the illness for which a patient is receiving treatment.[36] Physicians do not generally consider the possibility of SS with serotonergic drugs. There have been reports of cases where patients who were already using dextromethorphan and tramadol for cough and body pains were given medicines like ondansetron unmindful that all three have serotonergic effects.[37] Likewise, physicians should know that presentation of SS often mimics the actual condition for which the treatment was started.[38,39]
Clonus is one of the most important clinical signs of SS; however, most physicians do not even consider clonus while examining a patient presenting with psychological or neurological symptoms.[19,39] There is a need to apprise physicians of all Hunter’s criteria and most importantly the diagnostic value of clonus.
The signs and symptoms of SS are associated with increased serotonin levels, and therefore, they become milder or disappear as soon as the serotonin levels become normal. Some psychiatric disorders are associated with a reduction in serotonin levels. Many physicians, including neurologists and psychiatrists, want to increase serotonin level by using one or more of the drugs. These drugs have to be used for a long time. Very often, they miss their follow-up appointments. Serotonin level in patients on these medicines increases above the normal level leading to SS. Likewise, in countries without a proper healthcare structure, patients go to different doctors for the treatment of their depression without informing the physician of the previous drug history; sometimes, the doctors do not ask for the drug history and prescribe other antidepressant groups, thus increasing serotonin level.
Conclusion
SS is a highly underdiagnosed condition. It is mainly due to the injudicious use of antidepressants in treating the common disease, depression. All doctors should be aware of the signs and symptoms of SS in order to diagnose and treat this preventable and treatable condition promptly without harming the patients. There are definite gaps in knowledge, attitude, and practice about SS, so these deficiencies must be rectified.
In addition, as there is not much awareness, there are no proper records of the frequency of SS in most countries. Knowledge and practice of healthcare professionals are deficient in all domains of SS. Studies to identify deficiencies in physicians’ knowledge, attitudes, and practices about SS are very necessary.
The following recommendations are made to avoid disasters resulting from the lack of awareness of SS.
Records must be kept on the true incidence of SS at the level of practices, hospitals, regions, and countries so that awareness programs for patients and healthcare workers could be planned accordingly
All clinicians, especially GPs and ER (Emergency Room) physicians, must be vigilant to recognize SS in a timely manner. There is a need for specially designed educational workshops and videos to increase the awareness of healthcare professionals about SS
Drug history of previous treatment must be sought by the doctor to avoid prescribing drug combinations with potential to cause adverse drug interactions and complications. This is especially important in healthcare systems where proper records are not kept for each patient or in cases when patients do not always see the same doctor
It is very important to recognize the role of clinical pharmacologists and pharmacists about individual drugs and drug combinations with the tendency to cause SS
There is a need to promote the use of modern pharmacy software that alert physicians about a potential drug–drug interaction
To avoid increased risk of SS, the use of serotonergic drugs in Alzheimer’s disease patients must be done with extreme care since most Alzheimer’s disease drugs increase serotonergic neurotransmission
Every patient on SSRIs and their caretakers must be made aware of the side effects of SSRIs including SS. They must be told to report severe anxiety, agitation, high fever, sweating, confusion, tremors, restlessness, lack of coordination, major changes in blood pressure, and a rapid heart rate, especially after the change in the dosage or the start of any medication for any condition while on SSRIs
It is better to overreport than lose a patient to this preventable and curable condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mitro P, Hijova E, Mudrakova K. Role of the peripheral serotoninergic system in the pathogenesis of vasovagal syncope. Bratisl Lek Listy. 2006;107:248–52. [PubMed] [Google Scholar]
- 2.Berger M, Gray JA, Roth BL. The expanded biology of serotonin. Annu Rev Med. 2009;60:355–66. doi: 10.1146/annurev.med.60.042307.110802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nichols DE, Nichols CD. Serotonin receptors. Chem Rev. 2008;108:1614–41. doi: 10.1021/cr078224o. [DOI] [PubMed] [Google Scholar]
- 4.Wright P, O’Neill MF. Chapter-39 – Psychopharmacology. In: Wright P, Stern J, Phelan M, editors. Core Psychiatry. 3rd. Philadelphia: W. B. Saunders; 2012. pp. 585–615. [Google Scholar]
- 5.Simon LV, Keenaghan M. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Serotonin syndrome. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482377/ [Last updated on 2023 Jul 17] [PubMed] [Google Scholar]
- 6.Brown CH. Drug-induced serotonin syndrome. US Pharm. 2010;12:2010. Available from: https://www.uspharmacist.com/article/drug-induced-serotonin-syndrome. [Last accessed on 2021 Aug 14] [Google Scholar]
- 7.Buckley NA, Dawson AH, Isbister GK. Serotonin syndrome. BMJ. 2014;348:g1626. doi: 10.1136/bmj.g1626. [DOI] [PubMed] [Google Scholar]
- 8.Volpi-Abadie J, Kaye AM, Kaye AD. Serotonin syndrome. Ochsner J. 2013;13:533–40. [PMC free article] [PubMed] [Google Scholar]
- 9.Sun-Edelstein C, Tepper SJ, Shapiro RE. Drug-induced serotonin syndrome: A review. Expert Opin Drug Saf. 2008;7:587–96. doi: 10.1517/14740338.7.5.587. [DOI] [PubMed] [Google Scholar]
- 10.Lerner BH. Case that Shook Medicine. Washington Post; 2006 Available from: https://www.washingtonpost.com/archive/lifestyle/wellness/2006/11/28/a-case-that-shook-medicine-span-classbankheadhow-one-mans-rage-over-his-daughters-death-sped-reform-of-doctor-training-span/3b84b0a6-3066-4c3f-b1b2-a570b8269b9c/ [Last accessed on 2023 Oct 21] [Google Scholar]
- 11.Piatkov I, Mann G, Jones T, McLean M, Gunja N. Serotonin toxicity and cytochrome p450 poor metabolisergenotype patient case. J Investig Genomics. 2017;4:1–5. [Google Scholar]
- 12.Boyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112–20. doi: 10.1056/NEJMra041867. [DOI] [PubMed] [Google Scholar]
- 13.Mayo Clinic Staff . Mayo Clinic, Mayo Foundation for Medical Education and Research; 2019. “Selective Serotonin Reuptake Inhibitors (SSRIs)”. Available from: https://www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825. [Last accessed on 2021 Aug 12] [Google Scholar]
- 14.Grohol JM. Top 25 Psychiatric Medications For; 2018. Available from: https://psychcentral.com/blog/top-25-psychiatric-medications-for-2018#Most-Prescribed-Psychiatric-Drugs-for-2018. [Last accessed on 2023 Oct 21] [Google Scholar]
- 15.Chaudhry IB, Rahman R, Minhas HM, Chaudhry N, Taylor D, Ansari M, et al. Which antidepressant would psychiatrists and nurses from a developing country choose for themselves? Int J Psychiatry Clin Pract. 2011;15:74–8. doi: 10.3109/13651501.2010.530668. [DOI] [PubMed] [Google Scholar]
- 16.Xuev S, Ickowicz A. Serotonin syndrome in children and adolescents exposed to selective serotonin reuptake inhibitors – A review of literature. J Can Acad Child Adolesc Psychiatry. 2021;30:156–64. [PMC free article] [PubMed] [Google Scholar]
- 17.Moreland CS, Bonin L. Patient education: Depression treatment options for children and adolescents (beyond the basics) In: Brent D, editor. UpToDate. Wolters Kluwer; Available from: https://www.uptodate.com/contents/depression-treatment-options-for-children-and-adolescents-beyond-the-basics. [Last accessed on 2023 Dec 27] [Google Scholar]
- 18.Ismail M, Noor S, Harram U, Haq I, Haider I, Khadim F, et al. Potential drug-drug interactions in outpatient department of a tertiary care hospital in Pakistan: A cross-sectional study. BMC Health Serv Res. 2018;18:762. doi: 10.1186/s12913-018-3579-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prakash S, Rathore C, Rana K. Knowledge, attitude, and practice (KAP) study on serotonin syndrome among neuro physicians. Ann Indian Acad Neurol. 2020;23:638–43. doi: 10.4103/aian.AIAN_603_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pedavally S, Fugate JE, Rabinstein AA. Serotonin syndrome in the intensive care unit: Clinical presentations and precipitating medications. Neurocrit Care. 2014;21:108–13. doi: 10.1007/s12028-013-9914-2. [DOI] [PubMed] [Google Scholar]
- 21.Bijl D. The serotonin syndrome. Neth J Med. 2004;62:309–13. [PubMed] [Google Scholar]
- 22.Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The hunter serotonin toxicity criteria: Simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635–42. doi: 10.1093/qjmed/hcg109. [DOI] [PubMed] [Google Scholar]
- 23.Prakash S, Rathore C, Rana K. Serotonin syndrome: A syndrome on syndrome. Ann Indian Acad Neurol. 2021;24:430–2. doi: 10.4103/aian.AIAN_421_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991;148:705–13. doi: 10.1176/ajp.148.6.705. [DOI] [PubMed] [Google Scholar]
- 25.Radomski JW, Dursun SM, Reveley MA, Kutcher SP. An exploratory approach to the serotonin syndrome: An update of clinical phenomenology and revised diagnostic criteria. Med Hypotheses. 2000;55:218–24. doi: 10.1054/mehy.2000.1047. [DOI] [PubMed] [Google Scholar]
- 26.Prakash S, Patel V, Kakked S, Patel I, Yadav R. Mild serotonin syndrome: A report of 12 cases. Ann Indian Acad Neurol. 2015;18:226–30. doi: 10.4103/0972-2327.150612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wyatt JP, Taylor RG, de Wit K, Hotton EJ. 5th. London, England: Oxford University Press; 2020. Oxford Handbook of Emergency Medicine. [Google Scholar]
- 28.Perry PJ, Wilborn CA. Serotonin syndrome versus neuroleptic malignant syndrome: A contrast of causes, diagnoses, and management. Ann Clin Psychiatry. 2012;24:155–62. [PubMed] [Google Scholar]
- 29.Watson WA, Litovitz TL, Rodgers GC, Jr., Klein-Schwartz W, Reid N, Youniss J, et al. 2004 Annual report of the American Association of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med. 2005;23:589–666. doi: 10.1016/j.ajem.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Gillman PK. Triptans, serotonin agonists, and serotonin syndrome (serotonin toxicity): A review. Headache. 2010;50:264–72. doi: 10.1111/j.1526-4610.2009.01575.x. [DOI] [PubMed] [Google Scholar]
- 31.Gillman PK. The serotonin syndrome and its treatment. J Psychopharmacol. 1999;13:100–9. doi: 10.1177/026988119901300111. [DOI] [PubMed] [Google Scholar]
- 32.Lappin RI, Auchincloss EL. Treatment of the serotonin syndrome with cyproheptadine. N Engl J Med. 1994;331:1021–2. doi: 10.1056/NEJM199410133311514. [DOI] [PubMed] [Google Scholar]
- 33.Watson WA. Facts about serotonin syndrome. Pharm Lett Prescr Lett. 2009;25:251002. [Google Scholar]
- 34.Mackay FJ, Dunn NR, Mann RD. Antidepressants and the serotonin syndrome in general practice. Br J Gen Pract. 1999;49:871–4. [PMC free article] [PubMed] [Google Scholar]
- 35.Naqvi HA, Sabzwari S, Hussain S, Islam M, Zaman M. General practitioners’ awareness and management of common psychiatric disorders: A community-based survey from Karachi, Pakistan. East Mediterr Health J. 2012;18:446–53. doi: 10.26719/2012.18.5.446. [DOI] [PubMed] [Google Scholar]
- 36.Bhutto N, Siddiqi MN. Serotonin syndrome. Pak J Neurol Sci (PJNS) 2007;2:99–100. [Google Scholar]
- 37.Paauw DS. Why is Serotonin Syndrome on the Rise? Available from: https://www.medscape.com/viewarticle/941567. [Last accessed on 2023 Aug 31] [Google Scholar]
- 38.Khan SS, Kattan AS. Serotonin Syndrome: Practice Essentials, Problem, Management. Available from: https://emedicine.medscape.com/article/2500075-overview#showall. [Last accessed on 2023 Aug 31] [Google Scholar]
- 39.Prakash S, Rathore C, Rana KK, Dave A, Joshi H, Patel J. Refining the clinical features of serotonin syndrome: A prospective observational study of 45 patients. Ann Indian Acad Neurol. 2019;22:52–60. doi: 10.4103/aian.AIAN_344_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


