Abstract
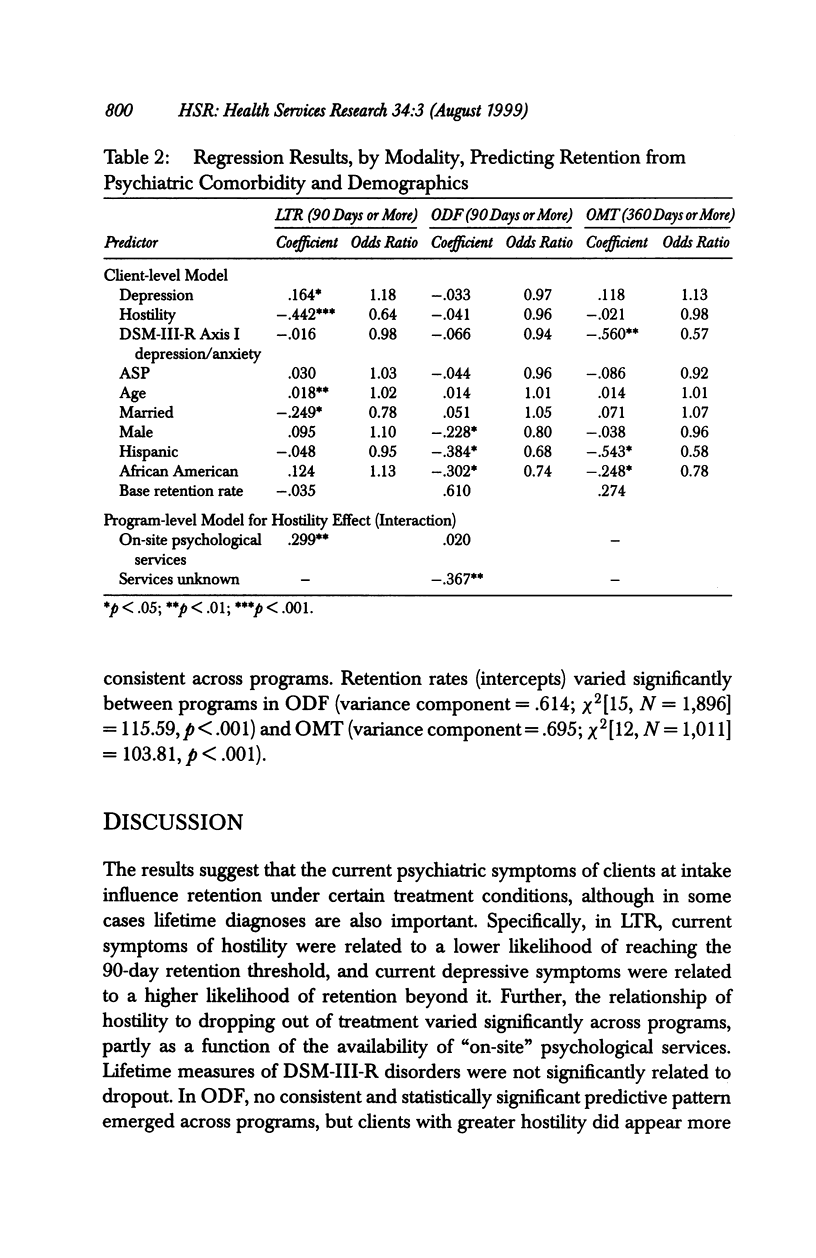
OBJECTIVE: To examine lifetime and current psychiatric comorbidity measures as predictors of drug abuse treatment retention, and to test the generalizability of results across treatment agencies in diverse settings and with varying practices. DATA SOURCES/STUDY SETTING: The national Drug Abuse Treatment Outcome Studies (DATOS), a longitudinal study of clients from 96 treatment agencies in 11 U.S. cities. STUDY DESIGN: The design is naturalistic and uses longitudinal analysis of treatment retention in long-term residential, outpatient drug-free, and outpatient methadone treatment modalities; client background (including psychiatric comorbidity) and program service provision are predictors. Clinical thresholds for adequate treatment retention were 90 days for long-term residential and outpatient drug-free, and 360 days for outpatient methadone. Psychiatric indicators included lifetime DSM-III-R diagnoses of depression/anxiety and antisocial personality, and dimensional measures of current symptoms for depression and hostility. DATA COLLECTION/EXTRACTION METHODS: Data include structured interviews with clients, a survey of treatment program administrators, and program discharge records. PRINCIPAL FINDINGS: Dimensional measures of current psychiatric symptoms emerged as better predictors than lifetime DSM-III-R diagnoses. In addition, the predictive association of hostility with retention varied significantly across treatment agencies, both in the long-term residential and outpatient drug-free modalities. Other notable findings were that on-site mental health services in long-term residential programs were associated with better retention for clients with symptoms of hostility. CONCLUSIONS: Assessment issues and stability of results across programs are important considerations for treatment research and practice.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agosti V., Nunes E., Stewart J. W., Quitkin F. M. Patient factors related to early attrition from an outpatient cocaine research clinic: a preliminary report. Int J Addict. 1991 Mar;26(3):327–334. doi: 10.3109/10826089109058888. [DOI] [PubMed] [Google Scholar]
- Alterman A. I., Rutherford M. J., Cacciola J. S., McKay J. R., Woody G. E. Response to methadone maintenance and counseling in antisocial patients with and without major depression. J Nerv Ment Dis. 1996 Nov;184(11):695–702. doi: 10.1097/00005053-199611000-00007. [DOI] [PubMed] [Google Scholar]
- Condelli W. S., De Leon G. Fixed and dynamic predictors of client retention in therapeutic communities. J Subst Abuse Treat. 1993 Jan-Feb;10(1):11–16. doi: 10.1016/0740-5472(93)90093-h. [DOI] [PubMed] [Google Scholar]
- Condelli W. S. Domains of variables for understanding and improving retention in therapeutic communities. Int J Addict. 1994 Apr;29(5):593–607. doi: 10.3109/10826089409047402. [DOI] [PubMed] [Google Scholar]
- D'Aunno T., Vaughn T. E. Variations in methadone treatment practices. Results from a national study. JAMA. 1992 Jan 8;267(2):253–258. [PubMed] [Google Scholar]
- De Leon G. Psychopathology and substance abuse: what is being learned from research in therapeutic communities. J Psychoactive Drugs. 1989 Apr-Jun;21(2):177–188. doi: 10.1080/02791072.1989.10472158. [DOI] [PubMed] [Google Scholar]
- De Leon G., Skodol A., Rosenthal M. S. Phoenix House. Changes in psychopathological signs of resident drug addicts. Arch Gen Psychiatry. 1973 Jan;28(1):131–135. doi: 10.1001/archpsyc.1973.01750310103017. [DOI] [PubMed] [Google Scholar]
- Derogatis L. R., Lipman R. S., Covi L. SCL-90: an outpatient psychiatric rating scale--preliminary report. Psychopharmacol Bull. 1973 Jan;9(1):13–28. [PubMed] [Google Scholar]
- Fisch A., Patch V. D., Greenfield A., Raynes A. E., McKenna G., Levine M. Depression and self-concept as variables in the differential response to methadone maintenance combined with therapy. Proc Natl Conf Methadone Treat. 1973;1:440–446. [PubMed] [Google Scholar]
- Friedman A. S., Glickman N. W. Effects of psychiatric symptomatology on treatment outcome for adolescent male drug abusers. J Nerv Ment Dis. 1987 Jul;175(7):425–430. doi: 10.1097/00005053-198707000-00006. [DOI] [PubMed] [Google Scholar]
- Joe G. W., Brown B. S., Simpson D. Psychological problems and client engagement in methadone treatment. J Nerv Ment Dis. 1995 Nov;183(11):704–710. doi: 10.1097/00005053-199511000-00006. [DOI] [PubMed] [Google Scholar]
- Leshner A. I. Drug abuse and addiction treatment research. The next generation. Arch Gen Psychiatry. 1997 Aug;54(8):691–694. doi: 10.1001/archpsyc.1997.01830200015002. [DOI] [PubMed] [Google Scholar]
- McLellan A. T., Luborsky L., O'Brien C. P., Barr H. L., Evans F. Alcohol and drug abuse treatment in three different populations: is there improvement and is it predictable? Am J Drug Alcohol Abuse. 1986;12(1-2):101–120. doi: 10.3109/00952998609083746. [DOI] [PubMed] [Google Scholar]
- Ravndal E., Vaglum P. Psychopathology and substance abuse as predictors of program completion in a therapeutic community for drug abusers: a prospective study. Acta Psychiatr Scand. 1991 Mar;83(3):217–222. doi: 10.1111/j.1600-0447.1991.tb05528.x. [DOI] [PubMed] [Google Scholar]
- Robins L. N., Helzer J. E., Croughan J., Ratcliff K. S. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981 Apr;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Sheehan M. F. Dual diagnosis. Psychiatr Q. 1993 Summer;64(2):107–134. doi: 10.1007/BF01065865. [DOI] [PubMed] [Google Scholar]
- Shwartz M., Mulvey K. P., Woods D., Brannigan P., Plough A. Length of stay as an outcome in an era of managed care. An empirical study. J Subst Abuse Treat. 1997 Jan-Feb;14(1):11–18. doi: 10.1016/s0740-5472(96)00095-5. [DOI] [PubMed] [Google Scholar]
- Simpson D. D., Joe G. W., Rowan-Szal G. A. Drug abuse treatment retention and process effects on follow-up outcomes. Drug Alcohol Depend. 1997 Sep 25;47(3):227–235. doi: 10.1016/s0376-8716(97)00099-9. [DOI] [PubMed] [Google Scholar]
- Simpson D. D., Joe G. W., Rowan-Szal G. A., Greener J. M. Drug abuse treatment process components that improve retention. J Subst Abuse Treat. 1997 Nov-Dec;14(6):565–572. doi: 10.1016/s0740-5472(97)00181-5. [DOI] [PubMed] [Google Scholar]
- Simpson D. D. Treatment for drug abuse. Follow-up outcomes and length of time spent. Arch Gen Psychiatry. 1981 Aug;38(8):875–880. doi: 10.1001/archpsyc.1981.01780330033003. [DOI] [PubMed] [Google Scholar]
- Spitzer R. L., Endicott J., Robins E. Clinical criteria for psychiatric diagnosis and DSM-III. Am J Psychiatry. 1975 Nov;132(11):1187–1192. doi: 10.1176/ajp.132.11.1187. [DOI] [PubMed] [Google Scholar]
- Steer R. A. Psychosocial correlates of retention in methadone maintenance. Int J Addict. 1980 Oct;15(7):1003–1009. doi: 10.3109/10826088009040074. [DOI] [PubMed] [Google Scholar]


