Abstract
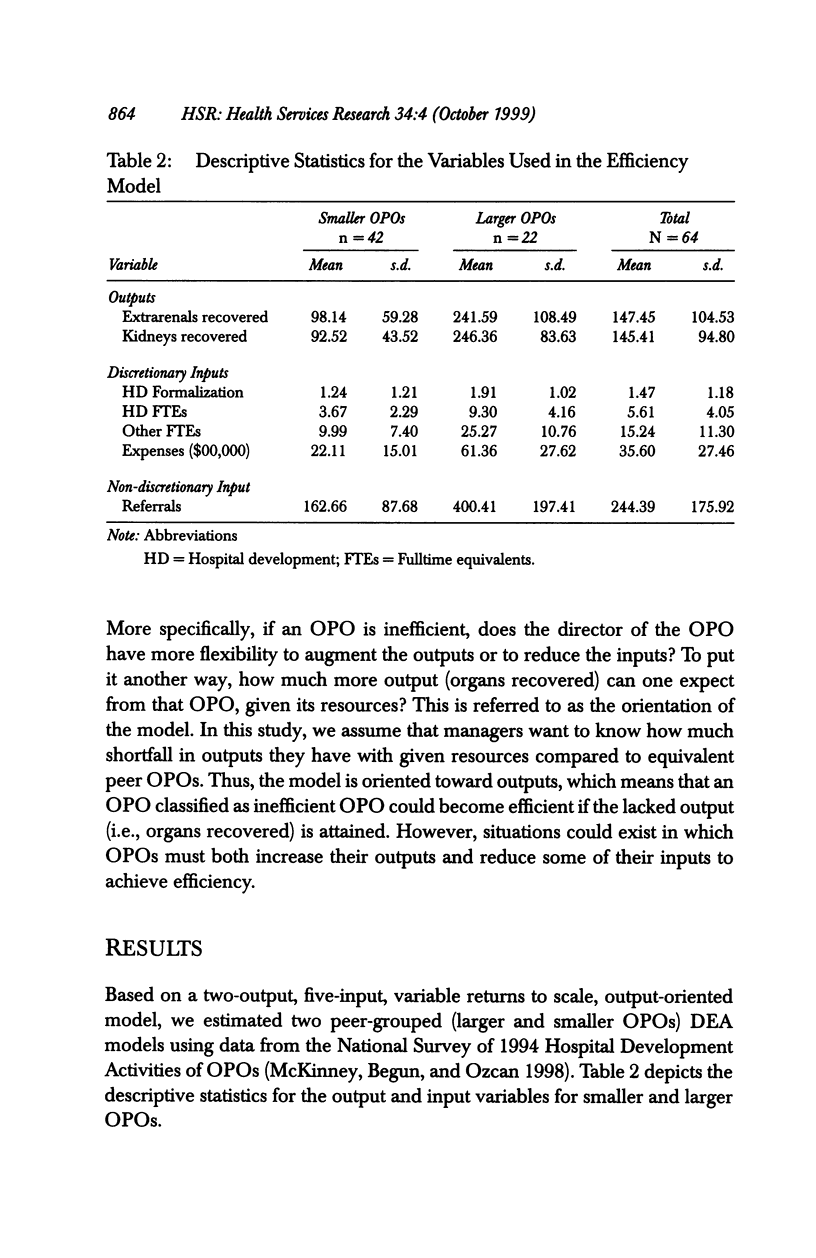
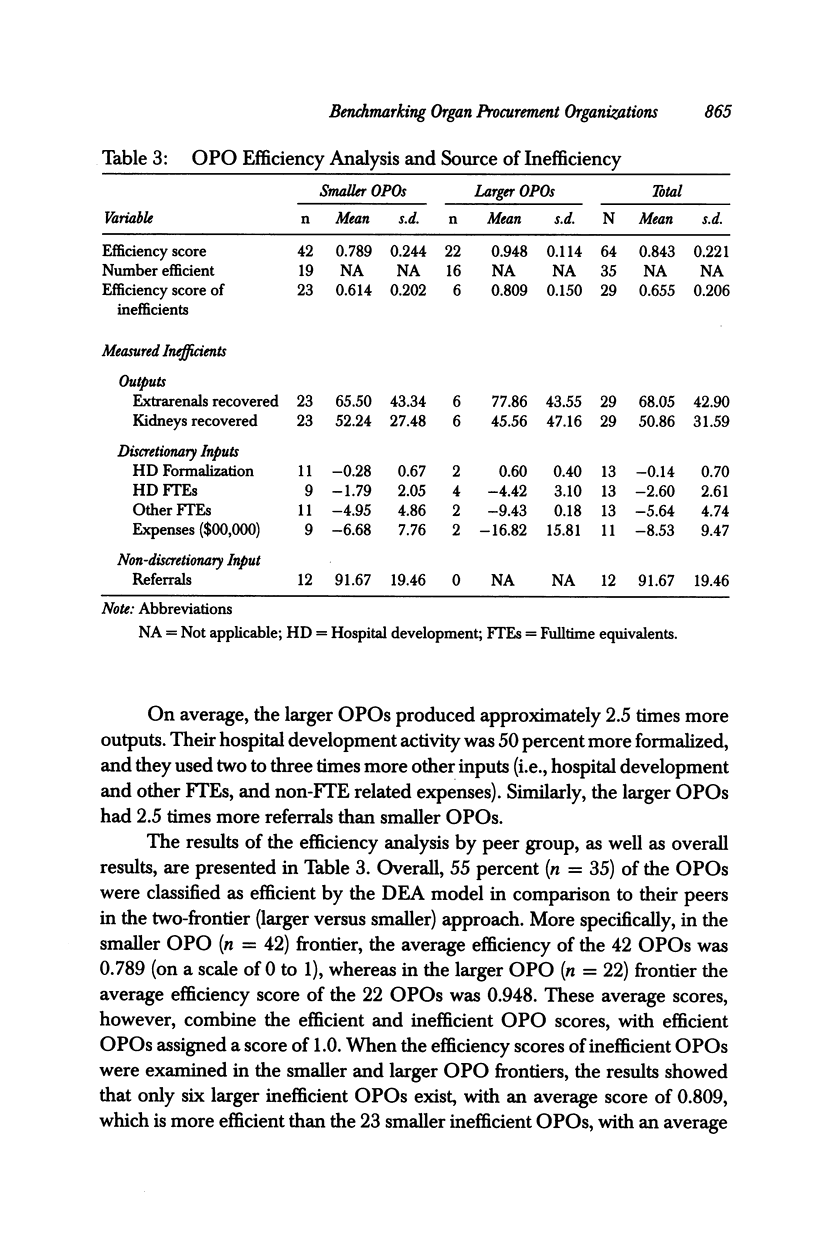
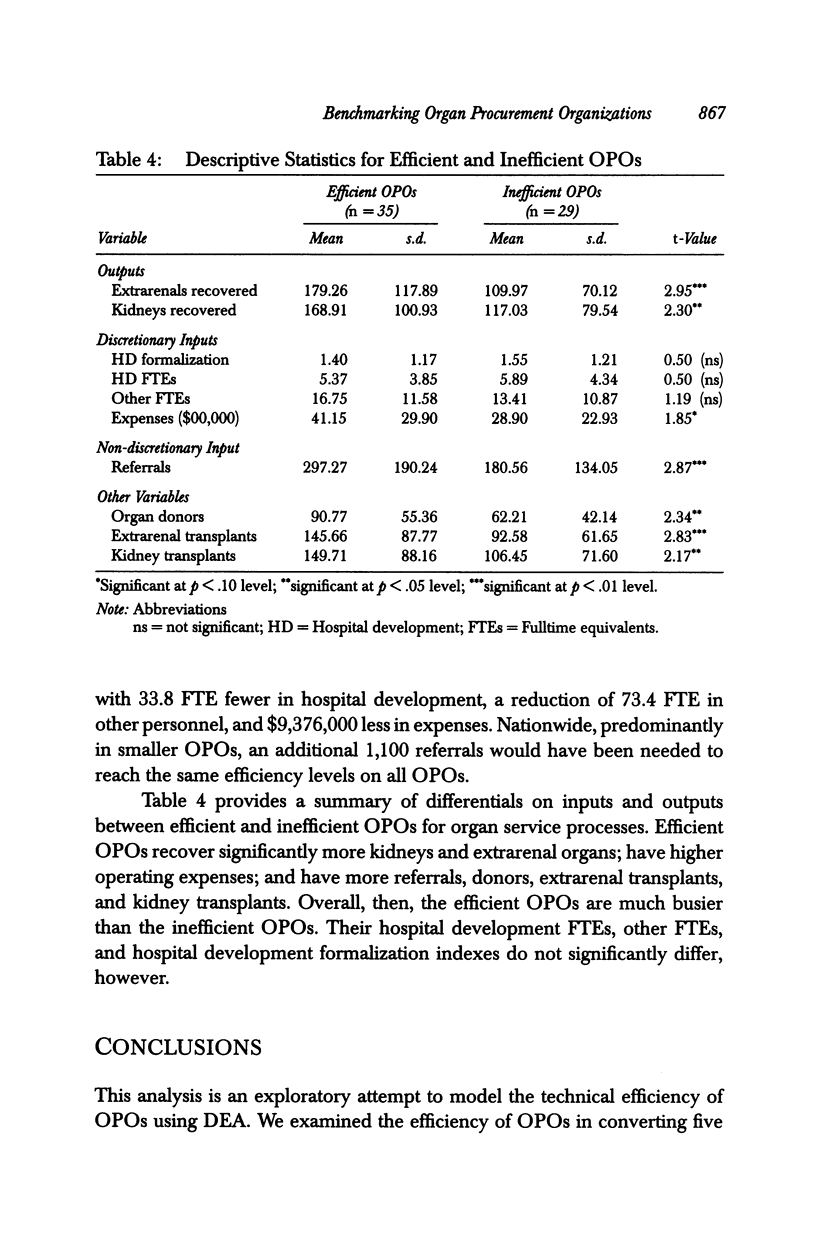
OBJECTIVE: An exploratory examination of the technical efficiency of organ procurement organizations (OPOs) relative to optimal patterns of production in the population of OPOs in the United States. DATA SOURCES: A composite data set with the OPO as the unit of analysis, constructed from a 1995 national survey of OPOs (n = 64), plus secondary data from the Association of Organ Procurement Organizations and the United Network for Organ Sharing. STUDY DESIGN: The study uses data envelopment analysis (DEA) to evaluate the technical efficiency of all OPOs. PRINCIPAL FINDINGS: Overall, six of the 22 larger OPOs (27 percent) are classified as inefficient, while 23 of the 42 smaller OPOs (55 percent) are classified as inefficient. Efficient OPOs recover significantly more kidneys and extrarenal organs; have higher operating expenses; and have more referrals, donors, extrarenal transplants, and kidney transplants. The quantities of hospital development personnel and other personnel, and formalization of hospital development activities in both small and large OPOs, do not significantly differ. CONCLUSIONS: Indications that larger OPOs are able to operate more efficiently relative to their peers suggest that smaller OPOs are more likely to benefit from technical assistance. More detailed information on the activities of OPO staff would help pinpoint activities that can increase OPO efficiency and referrals, and potentially improve outcomes for large numbers of patients awaiting transplants.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chilingerian J. A., Sherman H. D. Managing physician efficiency and effectiveness in providing hospital services. Health Serv Manage Res. 1990 Mar;3(1):3–15. doi: 10.1177/095148489000300101. [DOI] [PubMed] [Google Scholar]
- DeJong W., Drachman J., Gortmaker S. L. Options for increasing organ donation: the potential role of financial incentives, standardized hospital procedures, and public education to promote family discussion. Milbank Q. 1995;73(3):463–479. [PubMed] [Google Scholar]
- Denny D. W. The non-physician coordinator's contribution to the development of an organ procurement program. Transplant Proc. 1985 Dec;17(6 Suppl 4):83–87. [PubMed] [Google Scholar]
- Dunn S. M., McBride V. T. Collaboration, consultation, and care: developing an effective donor program. Crit Care Nurs Clin North Am. 1994 Sep;6(3):599–605. [PubMed] [Google Scholar]
- Evans R. W., Orians C. E., Ascher N. L. The potential supply of organ donors. An assessment of the efficacy of organ procurement efforts in the United States. JAMA. 1992 Jan 8;267(2):239–246. [PubMed] [Google Scholar]
- Hauptman P. J., O'Connor K. J. Procurement and allocation of solid organs for transplantation. N Engl J Med. 1997 Feb 6;336(6):422–431. doi: 10.1056/NEJM199702063360607. [DOI] [PubMed] [Google Scholar]
- Huang Y. G., McLaughlin C. P. Relative efficiency in rural primary health care: an application of data envelopment analysis. Health Serv Res. 1989 Jun;24(2):143–158. [PMC free article] [PubMed] [Google Scholar]
- McKinney M. M., Begun J. W., Ozcan Y. A. Hospital development and the performance of organ procurement organizations. J Transpl Coord. 1998 Jun;8(2):74–80. doi: 10.7182/prtr.1.8.2.b62721h727814443. [DOI] [PubMed] [Google Scholar]
- Nunamaker T. R. Measuring routine nursing service efficiency: a comparison of cost per patient day and data envelopment analysis models. Health Serv Res. 1983 Summer;18(2 Pt 1):183–208. [PMC free article] [PubMed] [Google Scholar]
- Ozcan Y. A., Cotter J. J. An assessment of efficiency of area agencies on aging in Virginia through data envelopment analysis. Gerontologist. 1994 Jun;34(3):363–370. doi: 10.1093/geront/34.3.363. [DOI] [PubMed] [Google Scholar]
- Ozcan Y. A., Luke R. D. A national study of the efficiency of hospitals in urban markets. Health Serv Res. 1993 Feb;27(6):719–739. [PMC free article] [PubMed] [Google Scholar]
- Ozcan Y. A., Luke R. D., Haksever C. Ownership and organizational performance. A comparison of technical efficiency across hospital types. Med Care. 1992 Sep;30(9):781–794. [PubMed] [Google Scholar]
- Ozcan Y. A. Physician benchmarking: measuring variation in practice behavior in treatment of otitis media. Health Care Manag Sci. 1998 Sep;1(1):5–17. doi: 10.1023/a:1019026114859. [DOI] [PubMed] [Google Scholar]
- Sexton T. R., Leiken A. M., Nolan A. H., Liss S., Hogan A., Silkman R. H. Evaluating managerial efficiency of Veterans Administration medical centers using Data Envelopment Analysis. Med Care. 1989 Dec;27(12):1175–1188. doi: 10.1097/00005650-198912000-00009. [DOI] [PubMed] [Google Scholar]
- Sherman H. D. Hospital efficiency measurement and evaluation. Empirical test of a new technique. Med Care. 1984 Oct;22(10):922–938. doi: 10.1097/00005650-198410000-00005. [DOI] [PubMed] [Google Scholar]
- Siminoff L. A., Arnold R. M., Caplan A. L. Health care professional attitudes toward donation: effect on practice and procurement. J Trauma. 1995 Sep;39(3):553–559. doi: 10.1097/00005373-199509000-00025. [DOI] [PubMed] [Google Scholar]
- Siminoff L. A., Arnold R. M., Caplan A. L., Virnig B. A., Seltzer D. L. Public policy governing organ and tissue procurement in the United States. Results from the National Organ and Tissue Procurement Study. Ann Intern Med. 1995 Jul 1;123(1):10–17. doi: 10.7326/0003-4819-123-1-199507010-00037. [DOI] [PubMed] [Google Scholar]
- Skelley L. Using CQI to improve quality in the organ procurement organization. Continuous quality improvement. Nephrol News Issues. 1991 Sep;5(9):31-2, 34-5. [PubMed] [Google Scholar]
- Smith-Brew S., Yanai L. The organ donation process through a review of the literature. Part I. Accid Emerg Nurs. 1996 Jan;4(1):5–11. doi: 10.1016/s0965-2302(96)90029-6. [DOI] [PubMed] [Google Scholar]
- Tyler L. H., Ozcan Y. A., Wogen S. E. Mental health case management and technical efficiency. J Med Syst. 1995 Oct;19(5):413–423. doi: 10.1007/BF02260831. [DOI] [PubMed] [Google Scholar]


