Abstract
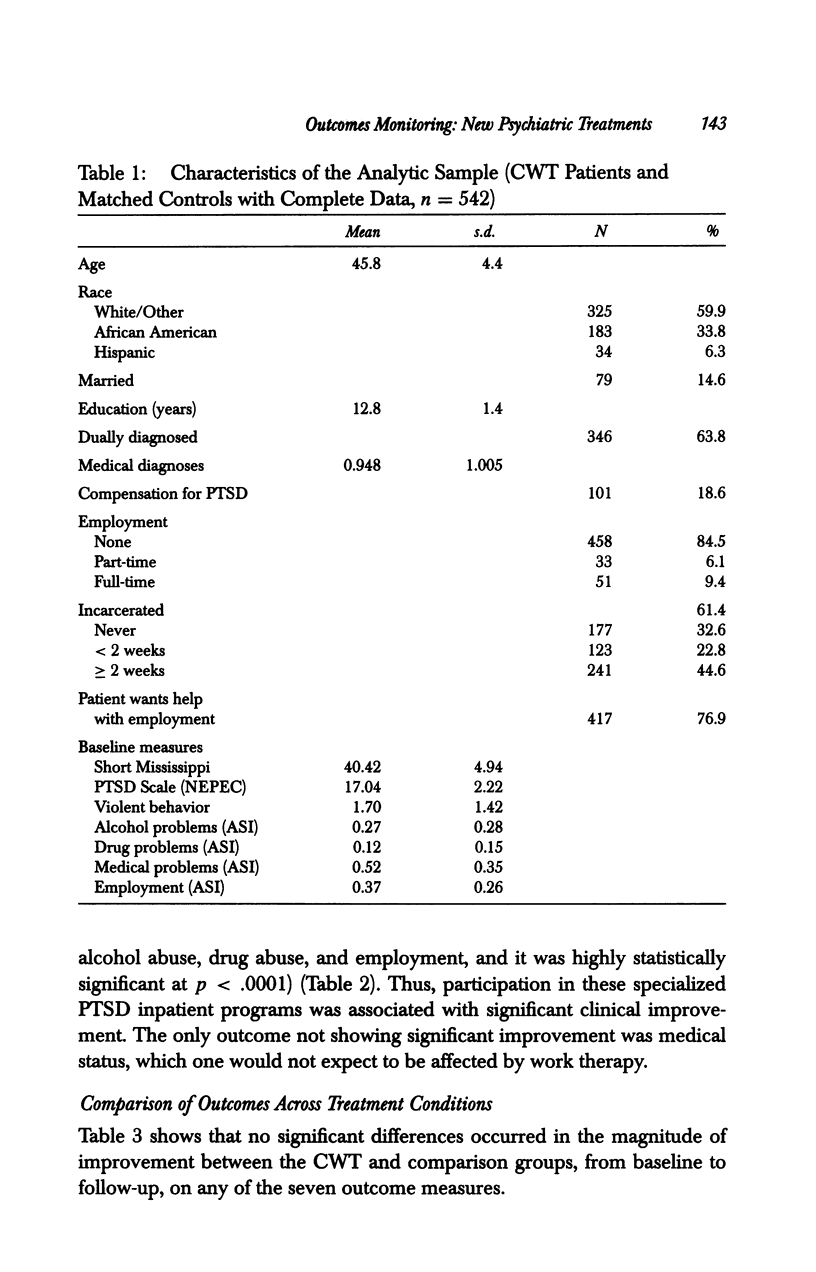
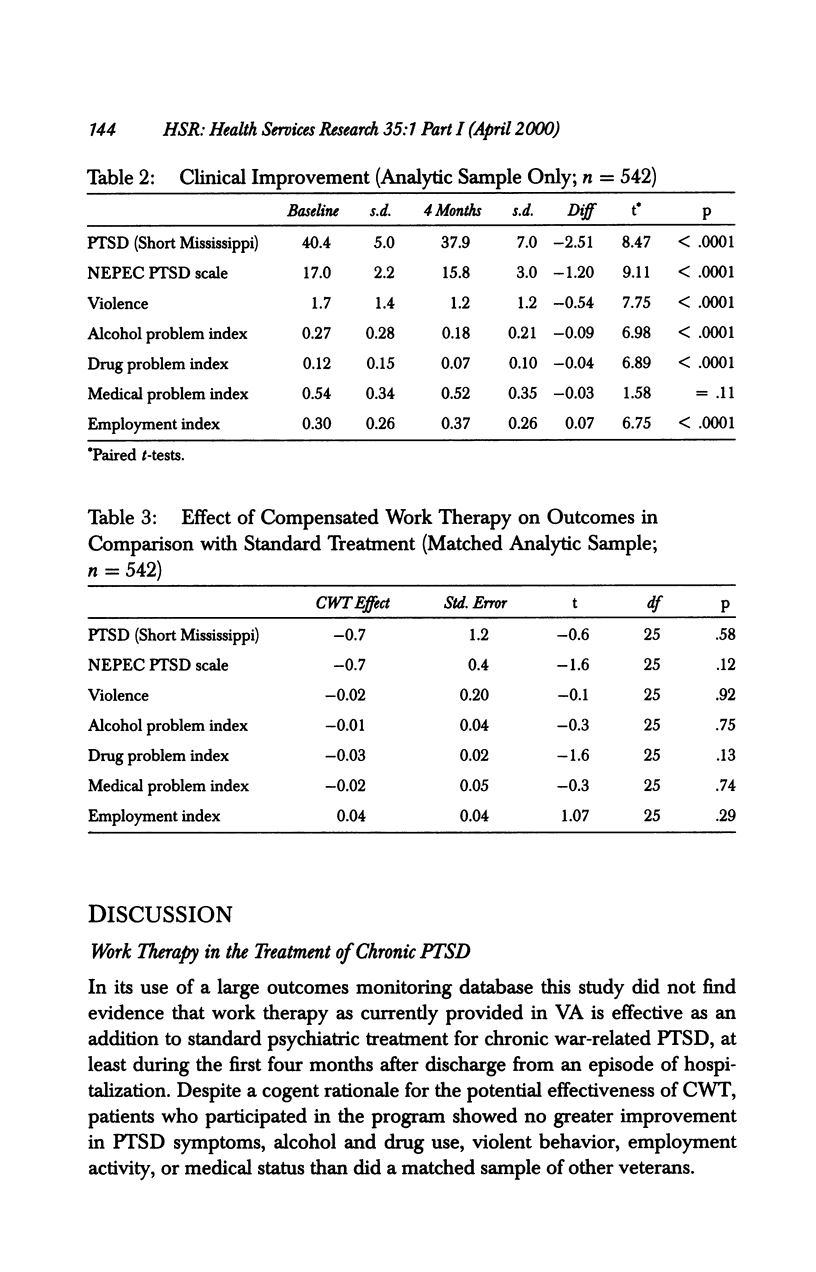
OBJECTIVE: To evaluate the effectiveness of a work therapy intervention, the Department of Veterans Affairs (VA) Compensated Work Therapy program (CWT), in the treatment of patients suffering from chronic war-related post-traumatic stress disorder (PTSD); and to demonstrate methods for using outcomes monitoring data to screen previously untested treatments. DATA SOURCES/STUDY SETTING: Baseline and four-month follow-up questionnaires administered to 3,076 veterans treated in 52 specialized VA inpatient programs for treatment of PTSD at facilities that also had CWT programs. Altogether 78 (2.5 percent) of these patients participated in CWT during the four months after discharge. STUDY DESIGN: The study used a pre-post nonequivalent control group design. DATA COLLECTION/EXTRACTION METHODS: Questionnaires documented PTSD symptoms, violent behavior, alcohol and drug use, employment status, and medical status at the time of program entry and four months after discharge from the hospital to the community. Administrative databases were used to identify participants in the CWT program. Propensity scores were used to match CWT participants and other patients, and hierarchical linear modeling was used to evaluate differences in outcomes between treatment groups on seven outcomes. PRINCIPAL FINDINGS: The propensity scaling method created groups that were not significantly different on any measure. No greater improvement was observed among CWT participants than among other patients on any of seven outcome measures. CONCLUSIONS: Substantively this study suggests that work therapy, as currently practiced in VA, is not an effective intervention, at least in the short term, for chronic, war-related PTSD. Methodologically it illustrates the use of outcomes monitoring data to screen previously untested treatments and the use of propensity scoring and hierarchical linear modeling to adjust for selection biases in observational studies.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blumenthal D. Part 1: Quality of care--what is it? N Engl J Med. 1996 Sep 19;335(12):891–894. doi: 10.1056/NEJM199609193351213. [DOI] [PubMed] [Google Scholar]
- Clardy J. A., Booth B. M., Smith L. G., Nordquist C. R., Smith G. R. Implementing a statewide outcomes management system for consumers of public mental health services. Psychiatr Serv. 1998 Feb;49(2):191–195. doi: 10.1176/ps.49.2.191. [DOI] [PubMed] [Google Scholar]
- Davidson J. R. Biological therapies for posttraumatic stress disorder: an overview. J Clin Psychiatry. 1997;58 (Suppl 9):29–32. [PubMed] [Google Scholar]
- Drake C., Fisher L. Prognostic models and the propensity score. Int J Epidemiol. 1995 Feb;24(1):183–187. doi: 10.1093/ije/24.1.183. [DOI] [PubMed] [Google Scholar]
- Ellwood P. M. Shattuck lecture--outcomes management. A technology of patient experience. N Engl J Med. 1988 Jun 9;318(23):1549–1556. doi: 10.1056/NEJM198806093182327. [DOI] [PubMed] [Google Scholar]
- Fontana A., Rosenheck R. Effects of compensation-seeking on treatment outcomes among veterans with posttraumatic stress disorder. J Nerv Ment Dis. 1998 Apr;186(4):223–230. doi: 10.1097/00005053-199804000-00004. [DOI] [PubMed] [Google Scholar]
- Johnson D. R., Lubin H., James M., Hale K. Single session effects of treatment components within a specialized inpatient posttraumatic stress disorder program. J Trauma Stress. 1997 Jul;10(3):377–390. doi: 10.1023/a:1024833119339. [DOI] [PubMed] [Google Scholar]
- Johnson D. R., Rosenheck R., Fontana A., Lubin H., Charney D., Southwick S. Outcome of intensive inpatient treatment for combat-related posttraumatic stress disorder. Am J Psychiatry. 1996 Jun;153(6):771–777. doi: 10.1176/ajp.153.6.771. [DOI] [PubMed] [Google Scholar]
- Lehman A. F. Vocational rehabilitation in schizophrenia. Schizophr Bull. 1995;21(4):645–656. doi: 10.1093/schbul/21.4.645. [DOI] [PubMed] [Google Scholar]
- McLellan A. T., Luborsky L., Cacciola J., Griffith J., Evans F., Barr H. L., O'Brien C. P. New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Ment Dis. 1985 Jul;173(7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- Mueser K. T., Drake R. E., Bond G. R. Recent advances in psychiatric rehabilitation for patients with severe mental illness. Harv Rev Psychiatry. 1997 Sep-Oct;5(3):123–137. doi: 10.3109/10673229709000298. [DOI] [PubMed] [Google Scholar]
- Rosenheck R., Wilson N. J., Meterko M. Influence of patient and hospital factors on consumer satisfaction with inpatient mental health treatment. Psychiatr Serv. 1997 Dec;48(12):1553–1561. doi: 10.1176/ps.48.12.1553. [DOI] [PubMed] [Google Scholar]
- Rubin D. B. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997 Oct 15;127(8 Pt 2):757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Solomon S. D., Gerrity E. T., Muff A. M. Efficacy of treatments for posttraumatic stress disorder. An empirical review. JAMA. 1992 Aug 5;268(5):633–638. [PubMed] [Google Scholar]
- Steinwachs D. M., Wu A. W., Skinner E. A. How will outcomes management work? Health Aff (Millwood) 1994 Fall;13(4):153–162. doi: 10.1377/hlthaff.13.4.153. [DOI] [PubMed] [Google Scholar]


