Abstract
Purpose
Every year around 70,000 people in Germany suffer from an abdominal incisional hernia that requires surgical treatment. Five years after reconstruction about 25% reoccur. Incisional hernias are usually closed with mesh using various reconstruction techniques, summarized here as standard reconstruction (SR). To improve hernia repair, we established a concept for biomechanically calculated reconstructions (BCR). In the BCR, two formulas enable customized patient care through standardized biomechanical measures. This study aims to compare the clinical outcomes of SR and BCR of incisional hernias after 1 year of follow-up based on the Herniamed registry.
Methods
SR includes open retromuscular mesh augmented incisional hernia repair according to clinical guidelines. BCR determines the required strength (Critical Resistance to Impacts related to Pressure = CRIP) preoperatively depending on the hernia size. It supports the surgeon in reliably determining the Gained Resistance, based on the mesh-defect-area-ratio, further mesh and suture factors, and the tissue stability. To compare SR and BCR repair outcomes in incisional hernias at 1 year, propensity score matching was performed on 15 variables. Included were 301 patients with BCR surgery and 23,220 with standard repair.
Results
BCR surgeries show a significant reduction in recurrences (1.7% vs. 5.2%, p = 0.0041), pain requiring treatment (4.1% vs. 12.0%, p = 0.001), and pain at rest (6.9% vs. 12.7%, p = 0.033) when comparing matched pairs. Complication rates, complication-related reoperations, and stress-related pain showed no systematic difference.
Conclusion
Biomechanically calculated repairs improve patient care. BCR shows a significant reduction in recurrence rates, pain at rest, and pain requiring treatment at 1-year follow-up compared to SR.
Keywords: Incisional hernia, Biomechanically calculated incisional hernia repair, Abdominal wall reconstruction, Propensity score matching for incisional hernia repair, STRONGHOLD, Herniamed
Introduction
Incisional ventral hernias occur frequently after abdominal surgeries. They can also occur in physically active people or after pregnancy. Hernia patients can experience pain and loss of their physical strength. This leads to unemployment, social withdrawal, depression, and great medical needs [3, 4]. In the US, more than $7 billion US is spent each year on incisional hernia repair, sick leave, and early retirement [5]. In Germany, the cost amount is at least € 1.8 billion. In the United States, more than 100,000 patients require hernia surgery each year [5]. However, the recurrence rate after surgery remains high [6]. The care and clinical practice of hernia surgery varies widely with different techniques and guidelines [7, 8]. A tailored approach to hernia surgery is recommended by hernia societies [7]. However, even when tailored by experts, individualized repair often fails [9].
In 2013, repetitive pressure impacts were recognized as a destructive force leading to incisional hernia formation [10, 11]. The durability of reconstructions can be determined by subjecting reconstructed tissues to cyclic pressure impacts on a test bench. Each material used, e.g., mesh and fixation, can be assigned a specific holding force [1, 12]. It has been found that considering the mesh–defect area ratio (MDAR) allows for a more reliable reconstruction than considering the mesh overlap alone [13, 14]. This provides the basis for the development of a biomechanically driven repair concept, the Gained/Critical Resistance to Impacts related to Pressure (GRIP/CRIP) concept. It includes two mathematical formulas to allow for individual hernia reconstruction. The CRIP formula determines the required durability of a reconstruction based on the defect size and tissue characteristics. The formula results in a numerical value that must be reached by an individual reconstruction to be durable. Larger hernias, extensible tissue, and repeated repairs require a stronger reconstruction, i.e., higher CRIP values. The GRIP formula advises the surgeon whether the selected reconstruction will achieve a sufficient stability for the individual patient. It allows the surgeon to fill in the selected reconstruction technique and materials and assigns them numerical factors. Then, the algorithm determines whether the stability achieved by the repair (GRIP) reaches the necessary stability (CRIP). Once the GRIP exceeded the CRIP value, the tested reconstructions withstood hundreds of impulse loads [1]. The GRIP/CRIP concept satisfies the need for personalized hernia repair. It enables biomechanically calculated repair (BCR) by determining the minimum force required for abdominal wall repair (CRIP) in each patient and assists the surgeon in achieving reliable and durable abdominal wall reconstruction (GRIP) [1]. Tissue distension of each patient’s abdominal wall was determined by clinical assessment of stability. Unstable abdominal walls were analyzed with CT scans at rest and during a Valsalva maneuver, allowing for individualization of complex hernia repair with excellent results at 1 year (Kallinowski, 2021a #77).
The STRONGHOLD registry was established as a subgroup of the Herniamed registry to evaluate the outcome of biomechanically calculated reconstruction (BCR) of the abdominal wall. STRONGHOLD consists of nine German hospitals where hernia care is performed according to the GRIP/CRIP concept [15]. This manuscript represents the first clinical application of the GRIP/CRIP concept by a larger group of surgeons.
After 1 year of follow-up, we compared the outcome of the BCR outcome with standard repair (SR) within the Herniamed registry. The comparison included intraoperative, postoperative, and overall complications, complication-related reoperations, and pain and recurrence rates at 1 year. We used propensity score matching. This statistical method forms control groups for a sample from a larger heterogeneous control population. It allows control subjects with similar characteristics to the study population to be found for comparison on an outcome variable.
Methods
Herniamed and STRONGHOLD
Herniamed is a German internet-based registry for inpatient and outpatient hernia surgery. It aims to monitor and evaluate important outcome data and improve the quality of patient care for all types of hernia surgeries. All interested hospitals and surgeons can easily enter data on all their hernia surgeries according to a scientifically validated standard procedure with the patient’s consent [16]. STRONGHOLD follows the same principles as a subset of Herniamed. It collects additional data for the biomechanically calculated reconstruction.
Standard repair
Standard repair includes open retromuscular mesh placement performed, which is without consideration of the BCR concept. SR monitors 30 patient- and hernia-related factors, such as risk factors, previous surgeries, and hernia size. The general recommendations (e.g., from the European Hernia Society [7]) for hernia repair are well known and largely reflected in the surgical expertise available in certified hernia centers.
Biomechanically calculated repair (BCR) in theory and practice
The aim of the BCR is to balance the forces acting on the abdominal wall and the retaining forces of the reconstructed tissue. The abdominal cavity is supported by several layers of connective and muscular tissue. The abdominal wall must be able to withstand the weight of the internal organs and additional physiological loads. The total intra-abdominal pressure can be understood as a hydraulic system influenced by gravity, compression, and shear deformation [17]. Coughing, jumping, or weight lifting increases the intra-abdominal pressure [18, 19]. The abdominal wall needs to be sufficiently stable to withstand these forces. During the initial period after a repair, a reconstruction adapts to the mechanical influences with an elastic–plastic deformation. This process determines the long-term durability of the reconstruction. Repeated microplastic deformations can add up to a large plastic deformation. Recurrence begins with each microplastic deformation but only becomes apparent over time [20–22]. In contrast, an elastic deformation pattern allows healing [23].
All surgeons contributing to Herniamed are interested, well-educated surgeons. Compared to surgeons contributing only to Herniamed, BCR surgeons document seven additional items to the thirty factors considered by the SR: the MDAR, the shape of the mesh, the minimal overlap, the kind of fixation elements, the amount of fixation elements, the suture closure of the defect, and the peritoneal closure. At Heidelberg University Hospital, an assessment of tissue elasticity is added as a sixth factor (as explained below). An algorithm calculates CRIP and GRIP values for all hernia repairs from the STRONGHOLD data, as explained below.
The calculations leading to the BCR are based on more than 240 preclinical studies performed on porcine and bovine tissues. The concept was developed in more than 2000 experiments over a period of 10 years. For this purpose, bovine and porcine tissues were systematically reconstructed with different meshes and sutures using different techniques [1, 24]. Afterwards, the reconstructed tissues were then tested on a test bench, which loaded the tissues with 425 repetitive pressure impacts of approximately 210 mmHg [25]. From these preclinical results, factors were calculated to estimate the durability of each reconstruction. The results were then gradually incorporated into clinical practice.
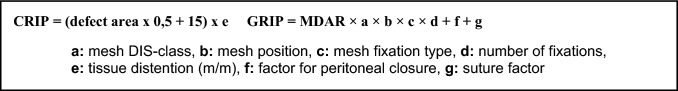
The BCR formula is based on the ratio of the defect size to the size of the implanted mesh (MDAR) [13]. The MDAR formula has been extended to include several biomechanical factors, which influence the durability of an abdominal wall repair. This extension represents the GRIP/CRIP concept. The Critical Resistance to Impacts related to Pressure (CRIP) provides a factor for the strength required to achieve a durable repair. It is a function of hernia size and patient tissue characteristics (e). The acronym GRIP describes the gained resistance of the repair to pressure effects. The GRIP formula includes several biomechanical factors that influence the durability of a customized mesh repair [1, 2]. It is based on the MDAR and considers the hernia area, various mesh (a–d), and suture factors (f, g). The separate factors are broken down in Fig. 1 and Table 1 and explained below.
Fig. 1.
CRIP formula for calculating the necessary stability. GRIP formula with factors for calculating the achieved stability [1, 2]. MDAR = mesh–defect area ratio. The letters indicate the coefficient for the material and/or technique used
Table 1.
Overview of the GRIP factors in detail with their numerical value known to date
| Factor | Meaning | Number value | ||
|---|---|---|---|---|
| MDAR | Mesh-area ÷ defect area | Varying | ||
| a | Mesh DIS-class | A: DynaMesh®, Progrip® | 1 | |
| B: | Ultrapro® Advance | 0.5 | ||
| Optilene® | 0.4 | |||
| C: | Ultrapro® | 0.25 | ||
| Adhesix® | 0.1 | |||
| b | Mesh position | Sublay | 1 | |
| Onlay | 0.5 | |||
| IPUM/Underlay | 0.9 | |||
| c | Mesh fixation typed | Sutures, Protack®, Securestrap® | 0.5 per fixation | |
| Absorbatack®, Glubran® | 0.33 per fixation | |||
| Fibrin glue | 0.15 per fixation | |||
| d | Number of mesh fixations | n | ||
| e | Tissue distention (m/m) | 1 – ∞ | ||
| f | Peritoneal closure | 4 | ||
| g | Suture factor | 0.5 per suture for correct horizontal + 0.5 for correct vertical placement = 1 per precise suture | ||
Preoperatively, the surgeon calculates the CRIP according to the patient’s individual defect size and tissue quality. The area of the hernia orifice is assessed clinically or measured on a CT scan.
After assessing the CRIP, the surgeon selects an appropriate customized reconstruction based on the GRIP formula. The calculations are performed by an algorithm based on the data provided by the surgeon in the STRONGHOLD registry. For better understanding, the algorithm is explained here.
First, the mesh area is divided by the defect area, giving the MDAR. The mesh reconstruction is then determined using four parameters (a–d). Factor a describes the adhesiveness of a particular mesh type to the tissue, which was assessed by evaluating the mesh displacement during repetitive loading. Different meshes have different adhesion properties to the surrounding tissue. This is defined by the DIS-class (a). Highly gripping meshes are classified as DIS-class A meshes, and less gripping meshes are classified as DIS-class B or C [25]. For factor b, three mesh positions in the porcine abdominal wall were investigated for the highest reconstruction stability. Sublay mesh placement provides a higher stability than onlay or underlay placement (Table 1) [10, 26]. Factors c and d were obtained by evaluating various mesh fixation techniques and devices. Different types of mesh fixation provide different ranges of stability, adding 0.15–0.5 to the GRIP with each fixation point (d). Factor e was only analyzed in detail in Heidelberg using a CT scan. The other Stronghold clinics do not perform imaging in every suspected patient.
If there is clinical suspicion of a highly distensible abdominal wall (> 20% or > 15 mm ventral shift), we recommend additional imaging to further clarify the instability [15, 27]. A preoperative CT scan of the patient’s abdomen a rest and during Valsalva maneuver can enhance the tailored approach. It provides crucial information about the behavior of the hernia orifice under stress and can identify unstable zones in the abdominal wall, that require additional reinforcement to ensure a stable, biomechanically calculated repair [15, 27]. The patients’ tissue extensibility in % (multiplication factor “e”) represents potential instability. It is determined by dividing the hernia diameter measured on the CT scan during the Valsalva maneuver by the hernia diameter at rest. The scan must be analyzed at least 12 times with three individual assessments to reduce inter- and intraindividual variation to less than 5%. Half of our patients show tissue distensions of more than 20% during a Valsalva maneuver, as it is performed in Heidelberg [27]. In this case, it is advisable to increase the CRIP value by a factor (e) of 1.2. Elastic tissue requires a stronger reconstruction [15, 26].
Factor f was added, since the closure of the peritoneum adds stability by providing an additional layer of support and a larger mesh-tissue interface [12]. Suturing the defect (factor g) adds strength to the reconstruction depending on its precision. Precisely placed sutures in the horizontal and vertical planes can increase the GRIP by a factor of 1 per stitch [24]. Standardized suturing may be included in BCR but is currently not part of the Stronghold registry. Stronghold surgeons are closely following the guidelines, using a running small-stitch-small-bite suture aiming for a suture-to-wound-length-ratio greater than 4:1.
Surgeons performing BCR-based hernia reconstruction were trained in a seminar that included personal coaching and a ten-page introduction to the topic and a four-page application guide. Additional coaching via telephone or Zoom was available to facilitate the use of BCR. All surgeons are free in their choice of technique. It is not required to store all kinds of materials mentioned above. The concept allows every surgeon to choose a combination that suits them, their hospital and the patient. None of the cases included in this study was bridging documented as the chosen closure technique.
Clinical evaluation: propensity score matching
We conducted a matched-pair analysis to compare the outcome of incisional hernia surgery considering BCR with SR surgery based on prospectively collected data of the Herniamed database. Included were fully documented elective incisional hernia surgeries by open—sublay or component separation using approved meshes with valid GRIP and valid MDAR. The surgeries had to be performed before 01/01/2021 including 1-year follow-up in patients with valid minimum age of 16 years.
After confirmation of the inclusion criteria and univariable explorative statistics of the patient population, a 1:1 pairwise matching was performed.
Thirteen matching variables were defined to form the propensity scores: BMI (kg/m2), age (years), mesh size/defect size ratio, ASA-Score (I/II/III–IV), EHS-Classification (medial/lateral/combined), defect size (W1 < 4 cm/W2 > = 4 – 10 cm/W3 > 10 cm), preoperative pain (yes/no/unknown), and presence of risk factors (without immunosuppression) (yes/no), as well as gender (m/f), recurrence (yes/no), surgical procedure (open-sublay/component separation), immunosuppression (yes/no), and fixation (yes/no). The last five variables are fixed matching variables, which means that no deviation between matched patients is allowed in each case.
Risk factors are present when at least one of the following factors is applicable: COPD, diabetes, aortic aneurysm, cortisone, smoking, coagulopathy, antiplatelet drugs during the last 7 days, and coumarin derivatives.
The robust greedy algorithm (with a caliper of 0.2 standard deviations) was used to assign the elements from the BCR population to appropriate cases of the SR population.
After matching, the balance of the matched samples was assessed using standardized differences. A good balance with respect to the included variables is ensured with a standardized difference of less than 10% (< 0.1). The results are illustrated in Tables 4 and 5. The examined outcome parameters were: intraoperative, postoperative, and general complications, consecutive reoperations, as well as pain at rest and at movement, pain requiring treatment, and recurrences after 1-year follow-up.
Table 4.
Standardized differences of the stable matching parameters before and after matching
| BCR | ||||||
|---|---|---|---|---|---|---|
| Yes | No | Standardized differences | ||||
| n | % | n | % | Matched sample | Original sample | |
| Open—sublay* | 196 | 67.4 | 196 | 67.4 | 0.000 | 0.752 |
| Component separation* | 95 | 32.6 | 95 | 32.6 | 0.000 | 0.752 |
| Male* | 160 | 55.0 | 160 | 55.0 | 0.000 | 0.065 |
| ASA score I | 19 | 6.5 | 15 | 5.2 | 0.059 | 0.092 |
| ASA score II | 153 | 52.6 | 167 | 57.4 | 0.097 | 0.113 |
| ASA score III–IV | 119 | 40.9 | 109 | 37.5 | 0.070 | 0.166 |
| Medial | 262 | 90.0 | 261 | 89.7 | 0.011 | 0.126 |
| Lateral | 76 | 26.1 | 74 | 25.4 | 0.016 | 0.173 |
| Combined | 47 | 16.2 | 44 | 15.1 | 0.028 | 0.347 |
| Defect size W1 (< 4 cm) | 62 | 21.3 | 68 | 23.4 | 0.050 | 0.081 |
| Defect size W2 (> = 4–10 cm) | 134 | 46.0 | 123 | 42.3 | 0.076 | 0.190 |
| Defect size W3 (> = 10 cm) | 95 | 32.6 | 100 | 34.4 | 0.036 | 0.286 |
| Fixation* | 249 | 85.6 | 249 | 85.6 | 0.000 | 0.157 |
| Preoperative pain | 191 | 65.6 | 183 | 62.9 | 0.057 | 0.167 |
| Unknown preoperative pain | 28 | 9.6 | 32 | 11.0 | 0.045 | 0.043 |
| No preoperative pain | 72 | 24.7 | 76 | 26.1 | 0.032 | 0.206 |
| Recurrent operation* | 59 | 20.3 | 59 | 20.3 | 0.000 | 0.057 |
Table 5.
Matched-pair results: proportion of pairs with complication/pain in both paired patients (concordant cases) and of those pairs with complication/pain in only one of the paired patients (disadvantageous cases), n = 291 matched pairs
| Concordant cases [%] | Disadvantageous cases [%] | OR for matched samples | |||||
|---|---|---|---|---|---|---|---|
| BCR [yes] | BCR [no] | p-Value | OR | Lower limit | Upper limit | ||
| Intraoperative complications | 0.00 | 3.09 | 1.03 | 0.146 | 3.000 | 0.749 | 17.228 |
| General complications | 0.69 | 4.81 | 3.78 | 0.690 | 1.273 | 0.537 | 3.098 |
| Postoperative complications | 0.69 | 5.84 | 8.59 | 0.280 | 0.680 | 0.345 | 1.310 |
| Complication-related reoperations | 0.00 | 2.06 | 4.47 | 0.167 | 0.462 | 0.144 | 1.302 |
| Recurrence on 1-year follow-up | 0.00 | 1.72 | 5.15 | 0.041 | 0.333 | 0.095 | 0.965 |
| Pain on exertion on 1-year follow-up | 3.78 | 14.09 | 19.24 | 0.155 | 0.732 | 0.477 | 1.115 |
| Pain at rest on 1-year follow-up | 1.37 | 6.87 | 12.71 | 0.033 | 0.541 | 0.297 | 0.956 |
| Pain requiring treatment on 1-year follow-up | 0.34 | 4.12 | 12.03 | 0.001 | 0.343 | 0.162 | 0.676 |
The exact McNemar test was performed for testing for a systematic deviation between the comparison groups (BCR vs. SR) with respect to an outcome parameter. An odds ratio adjusted for matched samples (95% confidence interval) was additionally provided. All analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA) and are deliberately considered at the full 5% significance level, i.e., no adjustment for multiple testing is applied and any p value ≤ 0.05 corresponds to a significant result.
Results
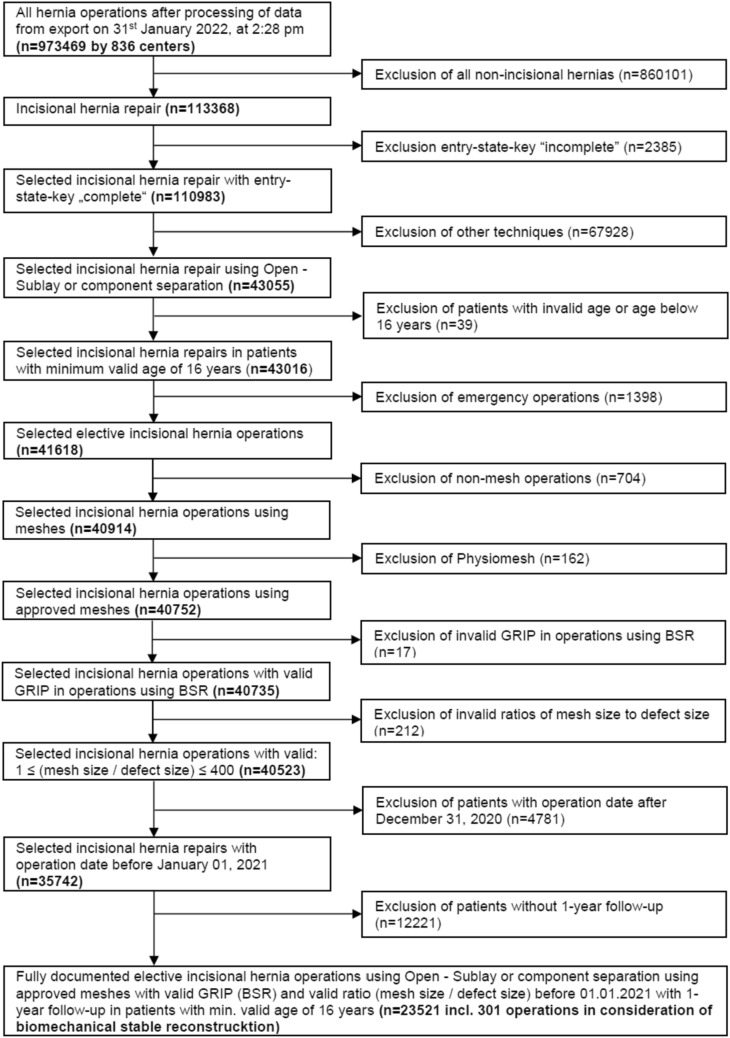
The patients were selected as shown in Fig. 2. After patient selection, 301 patients were found that had undergone BCR hernia surgery and 23,220 patients that had a standard repair as shown in Table 2.
Fig. 2.
Flowchart of patient inclusion for analysis
Table 2.
Distribution of frequency of operations with and without BCR consideration
| BCR | N | % |
|---|---|---|
| Yes | 301 | 1.28 |
| No | 23,220 | 98.72 |
| Total | 23,521 | 100.00 |
The 301 patients underwent BCR hernia surgery in one of the nine hospitals that participate in the STRONGHOLD study. The distribution of BCR surgeries among the STRONGHOLD clinics is shown in Table 3.
Table 3.
Frequency distribution of hernias operated with consideration of BCR within the centers participating in the STRONGHOLD study
| Stronghold-clinic | Procedures | |
|---|---|---|
| n | % | |
| 1 | 75 | 24.9 |
| 2 | 44 | 14.6 |
| 3 | 40 | 13.3 |
| 4 | 36 | 12.0 |
| 5 | 34 | 11.3 |
| 6 | 34 | 11.3 |
| 7 | 21 | 7.0 |
| 8 | 15 | 5.0 |
| 9 | 2 | 0.7 |
To investigate whether systematic differences in outcomes between surgeries with and without consideration of biomechanically calculated reconstruction can be found, matched pairs of patients with and without BCR were formed. Propensity score matching resulted in 291 matched pairs. Accordingly, 96.7% of BCR hernia surgeries could be matched to a similar SR case.
Standardized differences of less than 0.1 are found for all variables in the matched samples. Thus, the matched samples are relatively balanced and can be used for analyses without further adjustment for covariables.
An overview over the patient characteristics with standardized differences before and after matching is provided in Table 4.
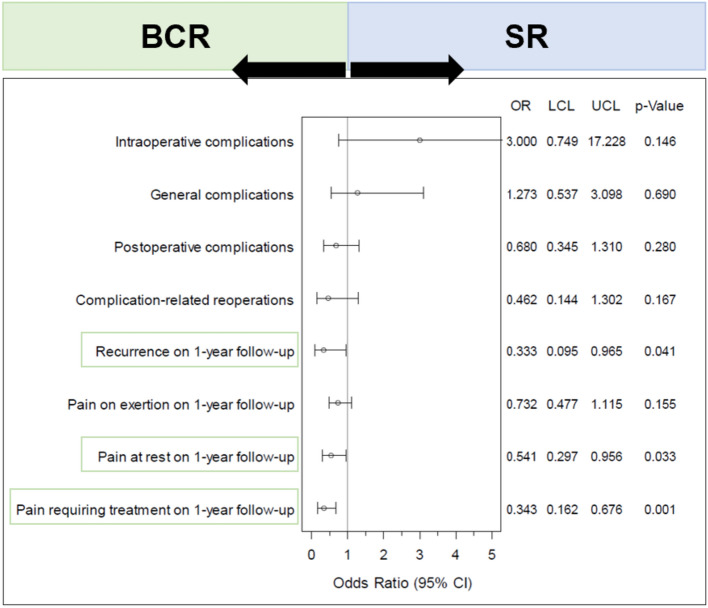
BCR show a significantly lower rate of recurrences, pain at rest, and pain requiring treatment at 1-year follow-up (Table 4; Fig. 3). Recurrence rates show a significant difference in favor of BCR surgeries (1.7% vs. 5.2%; p = 0.041, with no additional concordant cases; Table 5). This means that there are 1.7% matched pairs in which there is a recurrence after BCR surgery but no recurrence for the matched SR surgery. This contrasts with 5.2% recurrences without BCR consideration that do not appear with the matched BCR hernia. Thus, this is a systematic deviation in favor of BCR treatment. For pain at rest (6.9% vs. 12.7%; p = 0.033, with 1.37% concordant cases) and pain requiring treatment (4.1% vs. 12.0%; p = 0.001, with 0.34% concordant cases), there is a significant deviation in favor of the BCR. For all other outcome measures, no systematic deviation between the comparison groups could be shown (Fig. 3).
Fig. 3.
Forest plot—adjusted odds ratios (incl. confidence interval) for all outcome parameters when comparing: surgeries standard repair (SR) and considering biomechanically calculated repair (BCR) form the Herniamed registry
The forest plot in Fig. 3 illustrates the adjusted odds ratios for all outcome measures. The left side covers the surgeries with BCR and the right side covers the surgeries with SR. All outcome measures crossing the vertical line with their confidence interval indicate no conclusive effect for BCR or SR. If the confidence interval is entirely below 1, this indicates a significant disadvantage for operations without BSR consideration; if the interval is entirely above 1, this illustrates the disadvantage of considering BSR. The green boxes indicate significant differences.
Discussion
Today, a wide range of reconstruction techniques for abdominal wall defects is available [28]. This facilitates a tailored approach but makes hernia care inconsistent with high recurrence rates [6]. Experienced surgeons tend to have better outcomes [9]. New combinations of reconstruction techniques are constantly being developed and promise further technical advances [6–8]. Repair based on biomechanical calculations is a new approach [12].
Large national registries such as Herniamed are essential to monitor and improve hernia care consistently. The Scandinavian countries have successfully demonstrated the use of national registries [29, 30]. The collection of large data sets on hernia surgery has shown that not one surgical approach is appropriate for every hernia repair [16]. While registries are useful for real-life data, they lack the consistency of randomized clinical trials. It should be noted that many questions about BCR cannot be fully answered at this time and will require future investigation.
The treatment of a hernia requires an individualized approach that is precisely tailored to the patient [16, 31]. For a reliable treatment, not only the size of the hernia, but also a potential unstable, debris-like zone around the hernia orifice must be taken into account. Anchoring a stabilizing mesh in an unstable area of the abdominal wall is likely to fail. Furthermore, the tissue extensibility and the level of stress are relevant. These factors can be assessed with a preoperative CT scan at rest and during the Valsalva maneuver (CTAV) [15]. CTAV provides additional information. First, it identifies unstable areas of the abdominal wall, that require additional support and are not suitable for mesh fixation. Second, it allows for an estimation of the individual patient’s tissue distension [15, 27]. This is important for a successful reconstruction as highly distensible tissue leads to a greater increase in the size of the hernia under stress and provides less stability to the abdomen [15]. A CT-Scan is particularly advisable mainly in complex cases, when there is a loss of domain or if a great tissue extensibility is suspected. It provides greater insight into the abdominal wall and contributes to improved outcomes. However, regardless of the CT scan, the BCR offers an improvement in outcome after 1 year of follow-up.
Hernia formation occurs early in the postoperative period, as indicated by a fascial dehiscence of more than 12 mm at 1 month after surgery [32]. We do not routinely look for such a significant fascial dehiscence 1 month after surgery [33]. However, complex reconstructions can have recurrence rates as high as 10% after 6 months [34]. After 43 months, 94% of all fascial distances greater than 12 mm had developed a manifest hernia [22].
An effective combination of techniques is required to meet the individual needs of the patient. As explained above, the GRIP/CRIP concept is based on the MDAR [1]. For several years, the ratio of the defect area to the mesh area is seen as crucial for a successful repair [13]. However, the meshes differ in their adhesion to the tissue and therefore require different fixations [26]. Also, the suture closure of the peritoneum and abdominal wall play an important role for the long-term durability of the reconstruction [24]. The GRIP/CRIP concept takes these factors into account to guide the surgeon through the jungle of reconstruction options while ensuring a safe outcome [15].
In many cases, the BCR leads to increased overlap and the selection of stronger material. This makes treatment safer, as this study and many others show [14, 35]. Interested hernia surgeons, including Herniamed participants, know the theory, and yet recurrence rates remain high in clinical reality. The BCR guides surgeons to use appropriate mesh size, safe materials, fixation, and techniques by providing them with a standardized algorithm. This improves hernia care. This propensity score matching is just a first step in demonstrating the major impact of biomechanically calculated reconstructions.
The use of propensity score matching in data analysis has limitations. Herniamed and its sub-registry, Stronghold, collect data in a prospective manner but without strict monitoring of data quality. Changes in patient data over time, such as weight, are not documented. Follow-up procedures rely on the efficiency of clinical practice. Timely and complete data collection was a mandatory for this PSM analysis. Analysis of the Herniamed and Stronghold data will allow us to examine effects that were anticipated and recorded. In the future, the unstable abdominal wall area, the magnitude and the distribution of tissue stretching, and the resulting stress–strain-relationships of a mesh repair may be of interest.
We believe that the BCR approach is particularly advantageous for the repair of large, complex, and recurrent hernias, as hernia size is a significant risk factor [36]. The surgeon was responsible for the selection of patients in our study. In the original sample, 20.6% or 23.9% of small hernias (< 4 cm) underwent SR or BCR, respectively. This could indicate the surgeons' learning curve in acquiring experience with incisional hernia repair using the BCR technique.
The following limitations have not been recognized yet. Significant numerical differences may not necessarily be clinically relevant. As the follow-up period increases, the clinical relevance of the results will become clearer. The frequency of recurrences will also become more apparent [37]. Over 3 years, the BCR has demonstrated superb durability with recurrence rates remaining below 3% [38]. We are close to obtaining the 5-year follow-up data, but we have not matched the propensity score yet. After 5 years, we expect the rate of recurrences to be 5% after BCR and 15% after SR [37].
Conclusion
Biomechanical assessment and CT scans before surgery can improve patient care. Using the GRIP concept, over 99% of patients can be pain-free after 1 year with no recurrence [15, 27]. Surgeries with consideration of BCR had a significant advantage over those without BCR consideration in terms of recurrence, as well as pain at rest and treated pain. No significant difference was found between the comparison groups in terms of rates of complications, reoperations related to complications, or pain experienced during exercise in the follow-up period. Improving patient care can be achieved by taking into account the biomechanical factors at play.
Acknowledgements
The authors would like to thank the entire Stronghold Group (Guido Baschleben, Thorsten Löffler, and Johannes Rinn) for supporting this work and making these valuable insights possible. Special gratitude goes to Ferdinand Köckerling as the managing director of the Herniamed registry. Martin Hukauf and Daniela Adolf by StatConsult GmbH performed the statistical analysis and reported the results of the propensity score matching.
Authors’ contributions
Carolin Lesch wrote the present article. Regine Nessel provided important input for the development and clinical application of the BCR. Daniela Adolf and Martin Hukauf performed the statistical analysis of all data and conducted the propensity score matching. Ferdinand Köckerling manages and administers the Herniamed registry. Friedrich Kallinowski developed the BCR concept as well as the CT with Valsalva for Hernia assessment and guided the creation of this manuscript closely.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors would like to thank for the financial support by the Heidelberger Stiftung Chirurgie (Grants 2016/22, 2017/171, 2018/215, 2019/288, 2020/376, and 2021/444).
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without reservation.
Declarations
Conflict of interest
The other authors declare that there is no conflict of interest.
Ethical approval
The studies for computed tomography at rest and during Valsalva maneuver were reviewed and approved by the Ethics Committee of the Heidelberg University vote S-522/2020. STRONGHOLD as part of the HERNIAMED registry complies with the Declaration of Consent of the HERNIAMED database [39]. The Herniamed Registry has ethical approval (BASEC Nr. 2016-00123, 287/2017BO2/F-2022-111). The patients/participants provided their written informed consent to participate in the respective study in accordance with the national legislation and the institutional requirements. I, Carolin Lesch, hereby confirm that for the manuscript “STRONGHOLD First year results of biomechanically calculated abdominal wall repair: A propensity score matching” the following is fulfilled: (1) This material is the authors' own original work, which has not been previously published elsewhere. (2) The paper is not currently being considered for publication elsewhere. (3) The paper reflects the authors' own research and analysis in a truthful and complete manner. (4) The paper properly credits the meaningful contributions of co-authors and co-researchers. (5) The results are appropriately placed in the context of prior and existing research. (6) All sources used are properly disclosed. Literature references are correctly cited. Literally copying of text was not performed. (7) All authors have been personally and actively involved in substantial work leading to the paper and will take public responsibility for its content.
Informed consent
Jacob Relle, Philipp Lösel, and Vincent Heuveline developed the evaluation routine and analyzed the CT scans as approved by the Ethics Committee of the Heidelberg University vote S-522/2020. The patients/participants had provided their written informed consent to participate in this study.
Footnotes
Disclaimer: F. Kallinowski received financial and material support by Baxter, Becton Dickinson, Corza Medical, Dahlhausen, Ethicon, FEG, GEM, Medtronic, Olympus, and pfm medical based on a Third-Party-Funding-Agreement with the Heidelberg University and/or with Asklepios proresearch. F. Köckerling received speakers’ honoraria from BD Karlsruhe and Medtronic. Additionally, he is board member of BD Karlsruhe.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kallinowski F, Harder F, Gutjahr D, et al. Assessing the GRIP of ventral hernia repair: how to securely fasten DIS classified meshes. Front Surg. 2018;4:78. doi: 10.3389/fsurg.2017.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kallinowski F, Gutjahr D, Vollmer M, Harder F, Nessel R. Increasing hernia size requires higher GRIP values for a biomechanically stable ventral hernia repair. Ann Med Surg. 2019;42:1–6. doi: 10.1016/j.amsu.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gesellschaft DH. Patienteninformationen zur Hernienchirurgie. 2023; Available from: https://herniengesellschaft.de/informationen/informationen-fuer-patienten/
- 4.van Ramshorst GH, Eker HH, Hop WC, Jeekel J, Lange JF. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg. 2012;204(2):144–150. doi: 10.1016/j.amjsurg.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Shubinets V, Fox JP, Lanni MA, et al (2018) Incisional hernia in the United States: trends in hospital encounters and corresponding healthcare charges. Am Surgeon™. 84(1):118–125. 10.1177/000313481808400132 [PubMed]
- 6.Köckerling F. Recurrent incisional hernia repair—an overview. Front Surg. 2019;6:26. doi: 10.3389/fsurg.2019.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deerenberg EB, Henriksen NA, Antoniou GA, et al. Updated guideline for closure of abdominal wall incisions from the European and American Hernia Societies. Br J Surg. 2022;109(12):1239–1250. doi: 10.1093/bjs/znac302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bittner R, Bain K, Bansal VK, et al. Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—Part A. Surg Endosc. 2019;33(10):3069–3139. doi: 10.1007/s00464-019-06907-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hassan AM, Shah NR, Asaad M, et al. Association between cumulative surgeon experience and long-term outcomes in complex abdominal wall reconstruction. Hernia. 2023;27(3):583–592. doi: 10.1007/s10029-022-02731-6. [DOI] [PubMed] [Google Scholar]
- 10.Kallinowski F, Baumann E, Harder F, et al. Dynamic intermittent strain can rapidly impair ventral hernia repair. J Biomech. 2015;48(15):4026–4036. doi: 10.1016/j.jbiomech.2015.09.045. [DOI] [PubMed] [Google Scholar]
- 11.Karkhaneh Yousefi AA, Pierrat B, Le Ruyet A, Avril S. Patient-specific computational simulations of wound healing following midline laparotomy closure. Biomech Model Mechanobiol. 2023 doi: 10.1007/s10237-023-01708-3. [DOI] [PubMed] [Google Scholar]
- 12.Kallinowski F, Ludwig Y, Löffler T, et al. Biomechanics applied to incisional hernia repair - Considering the critical and the gained resistance towards impacts related to pressure. Clin Biomech (Bristol, Avon) 2021;82:105253. doi: 10.1016/j.clinbiomech.2020.105253. [DOI] [PubMed] [Google Scholar]
- 13.Tulloh B, de Beaux A. Defects and donuts: the importance of the mesh:defect area ratio. Hernia. 2016;20(6):893–895. doi: 10.1007/s10029-016-1524-4. [DOI] [PubMed] [Google Scholar]
- 14.Hauters P, Desmet J, Gherardi D, Dewaele S, Poilvache H, Malvaux P. Assessment of predictive factors for recurrence in laparoscopic ventral hernia repair using a bridging technique. Surg Endosc. 2017;31(9):3656–3663. doi: 10.1007/s00464-016-5401-0. [DOI] [PubMed] [Google Scholar]
- 15.Kallinowski F, Gutjahr D, Harder F, et al. The grip concept of incisional hernia repair-dynamic bench test, CT abdomen with valsalva and 1-year clinical results. Front Surg. 2021;8:602181. doi: 10.3389/fsurg.2021.602181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stechemesser B, Jacob DA, Schug-Paß C, Köckerling F. Herniamed: an Internet-based registry for outcome research in hernia surgery. Hernia. 2012;16(3):269–276. doi: 10.1007/s10029-012-0908-3. [DOI] [PubMed] [Google Scholar]
- 17.De Keulenaer BL, De Waele JJ, Powell B, Malbrain ML. What is normal intra-abdominal pressure and how is it affected by positioning, body mass and positive end-expiratory pressure? Intensive Care Med. 2009;35(6):969–976. doi: 10.1007/s00134-009-1445-0. [DOI] [PubMed] [Google Scholar]
- 18.Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B. Normal intraabdominal pressure in healthy adults. J Surg Res. 2005;129(2):231–235. doi: 10.1016/j.jss.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 19.Blazek D, Stastny P, Maszczyk A, Krawczyk M, Matykiewicz P, Petr M. Systematic review of intra-abdominal and intrathoracic pressures initiated by the Valsalva manoeuvre during high-intensity resistance exercises. Biol Sport. 2019;36(4):373–386. doi: 10.5114/biolsport.2019.88759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xing L, Culbertson EJ, Wen Y, Franz MG. Early laparotomy wound failure as the mechanism for incisional hernia formation. J Surg Res. 2013;182(1):e35–e42. doi: 10.1016/j.jss.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Israelsson LA, Millbourn D. Closing midline abdominal incisions. Langenbecks Arch Surg. 2012;397(8):1201–1207. doi: 10.1007/s00423-012-1019-4. [DOI] [PubMed] [Google Scholar]
- 22.Pollock AV, Evans M. Early prediction of late incisional hernias. Br J Surg. 1998;76(9):953–954. doi: 10.1002/bjs.1800760926. [DOI] [PubMed] [Google Scholar]
- 23.Carolin L, Yannique L, Fabio K, et al (2023) Cyclic pulse loads pave the road to the GRIP concept in abdominal wall reconstruction. 7:25. 10.20517/2574-1225.2023.31
- 24.Lesch C, Uhr K, Vollmer M, Raschidi R, Nessel R, Kallinowski F. Standardized suturing can prevent slackening or bursting suture lines in midline abdominal incisions and defects. Hernia. 2022 doi: 10.1007/s10029-022-02659-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kallinowski F, Harder F, Silva TG, Mahn A, Vollmer M. Bridging with reduced overlap: fixation and peritoneal grip can prevent slippage of DIS class A meshes. Hernia. 2017;21(3):455–467. doi: 10.1007/s10029-017-1583-1. [DOI] [PubMed] [Google Scholar]
- 26.Kallinowski F, Ludwig Y, Gutjahr D, et al (2021c) Biomechanical influences on mesh-related complications in incisional hernia repair. Front Surg. 10.3389/fsurg.2021.763957 [DOI] [PMC free article] [PubMed]
- 27.Nessel R, Löffler T, Rinn J, et al (2021) Primary and recurrent repair of incisional hernia based on biomechanical considerations to avoid mesh-related complications. Front Surg. 8:764470. 10.3389/fsurg.2021.764470 [DOI] [PMC free article] [PubMed]
- 28.Köckerling F, Hoffmann H, Mayer F, et al. What are the trends in incisional hernia repair? Real-world data over 10 years from the Herniamed registry. Hernia. 2021;25(2):255–265. doi: 10.1007/s10029-020-02319-y. [DOI] [PubMed] [Google Scholar]
- 29.Dahlstrand U, Wollert S, Nordin P, Sandblom G, Gunnarsson U. Emergency femoral hernia repair: a study based on a national register. Ann Surg. 2009;249(4):672–676. doi: 10.1097/SLA.0b013e31819ed943. [DOI] [PubMed] [Google Scholar]
- 30.Helgstrand F, Rosenberg J, Bay-Nielsen M, et al. Establishment and initial experiences from the Danish Ventral Hernia Database. Hernia. 2010;14(2):131–135. doi: 10.1007/s10029-009-0592-0. [DOI] [PubMed] [Google Scholar]
- 31.Köckerling F, Sheen AJ, Berrevoet F, et al. The reality of general surgery training and increased complexity of abdominal wall hernia surgery. Hernia. 2019;23(6):1081–1091. doi: 10.1007/s10029-019-02062-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Playforth MJ, Sauven PD, Evans M, Pollock AV. The prediction of incisional hernias by radio-opaque markers. Ann R Coll Surg Engl. 1986;68(2):82–84. [PMC free article] [PubMed] [Google Scholar]
- 33.Bisgaard T, Kehlet H, Bay-Nielsen MB, et al. Nationwide study of early outcomes after incisional hernia repair. Br J Surg. 2009;96(12):1452–1457. doi: 10.1002/bjs.6728. [DOI] [PubMed] [Google Scholar]
- 34.Pereira-Rodriguez JA, Bravo-Salva A, Montcusí-Ventura B, Hernández-Granados P, Rodrigues-Gonçalves V, López-Cano M. Early outcomes of component separation techniques: an analysis of the Spanish registry of incisional Hernia (EVEREG) Hernia. 2021;25(6):1573–1580. doi: 10.1007/s10029-021-02449-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schumpelick V, Klinge U, Junge K, Stumpf M. Incisional abdominal hernia: the open mesh repair. Langenbecks Arch Surg. 2004;389(1):1–5. doi: 10.1007/s00423-003-0352-z. [DOI] [PubMed] [Google Scholar]
- 36.Köckerling F, Hoffmann H, Adolf D, et al (2021) Potential influencing factors on the outcome in incisional hernia repair: a registry-based multivariable analysis of 22,895 patients. Hernia. 10.1007/s10029-020-02184-9 [DOI] [PMC free article] [PubMed]
- 37.Köckerling F, Koch A, Lorenz R, Schug-Pass C, Stechemesser B, Reinpold W. How long do we need to follow-up our hernia patients to find the real recurrence rate? Front Surg. 2015;2:24. doi: 10.3389/fsurg.2015.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kallinowski F, Löffler T, Rinn J, Nessel R, Görich J, Wielpütz M (2023) BJS-05 DIS CLASS A MESHES PERMIT BIOMECHANICALLY STRONG RECONSTRUCTIONS WHICH ARE DURABLE AFTER A 3 YEAR FOLLOW UP. Br J Surg. 110(Supplement_2):znad080.005. 10.1093/bjs/znad080.005
- 39.Herniamed Qualitätssicherungsstudie. Datenschutzrechtliche Aufklärung und Einwilligung inkl. Information gem. Art.13 DS-GVO und Information über die wesentlichen Inhalte der Vereinbarung über die gemeinsame Verantwortlichkeit nach Art. 26 Abs. 2 S.2 der DS-GVO. 2022; Available from: https://www.herniamed.de/sites/default/files/Einwilligungserklaerung.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without reservation.