Abstract
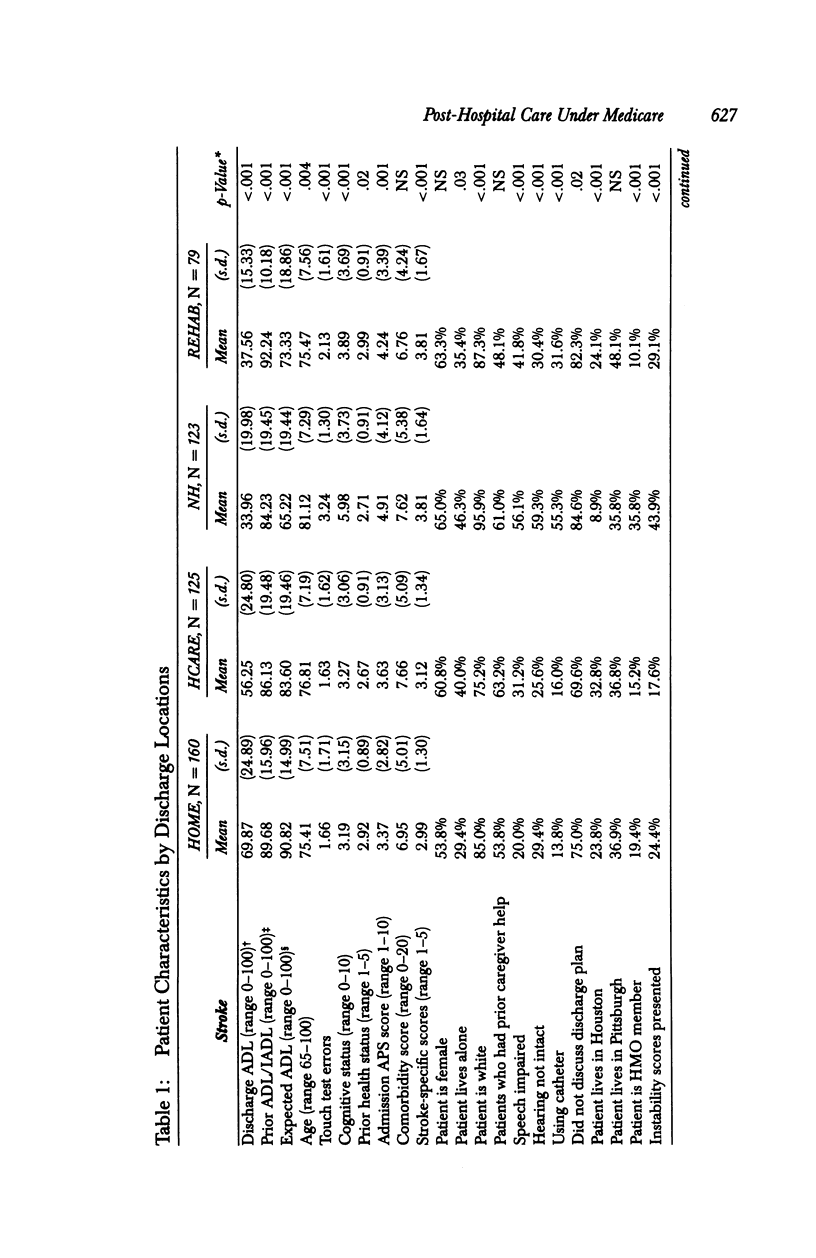
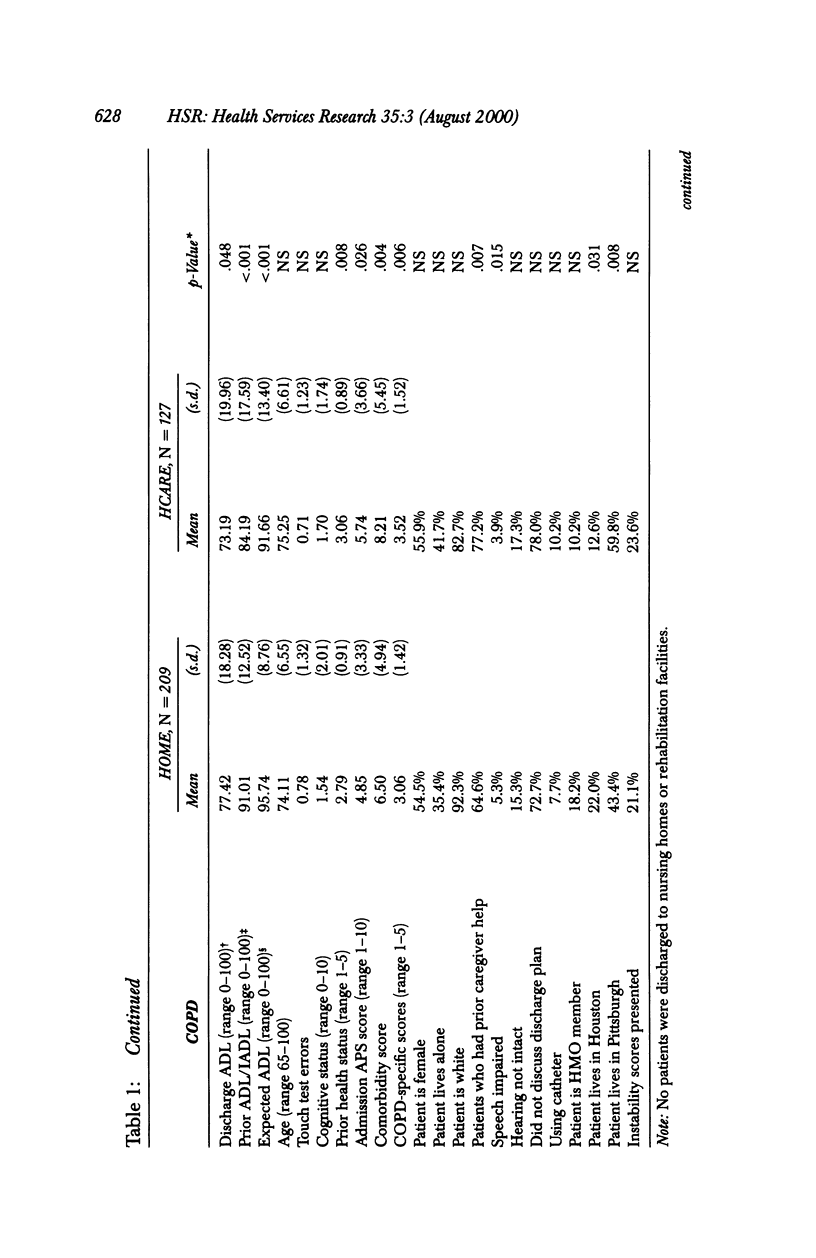
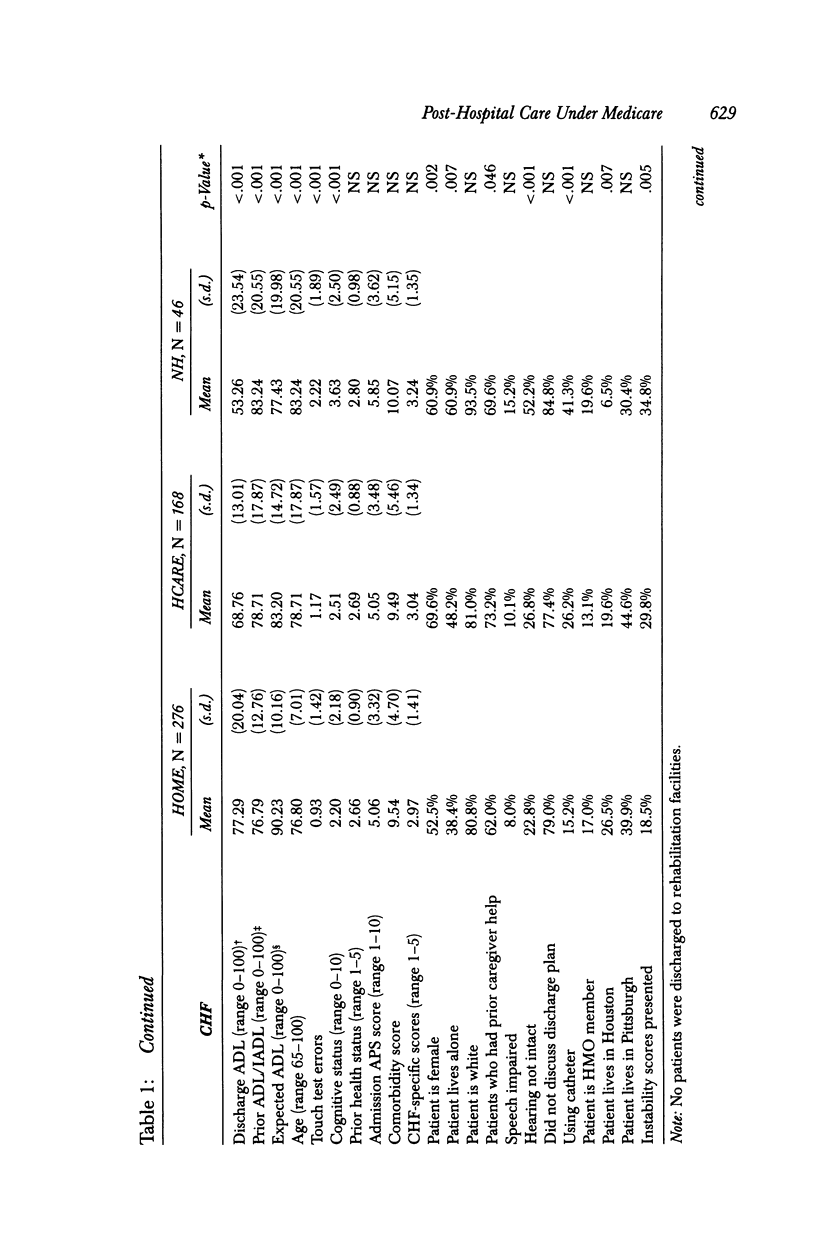
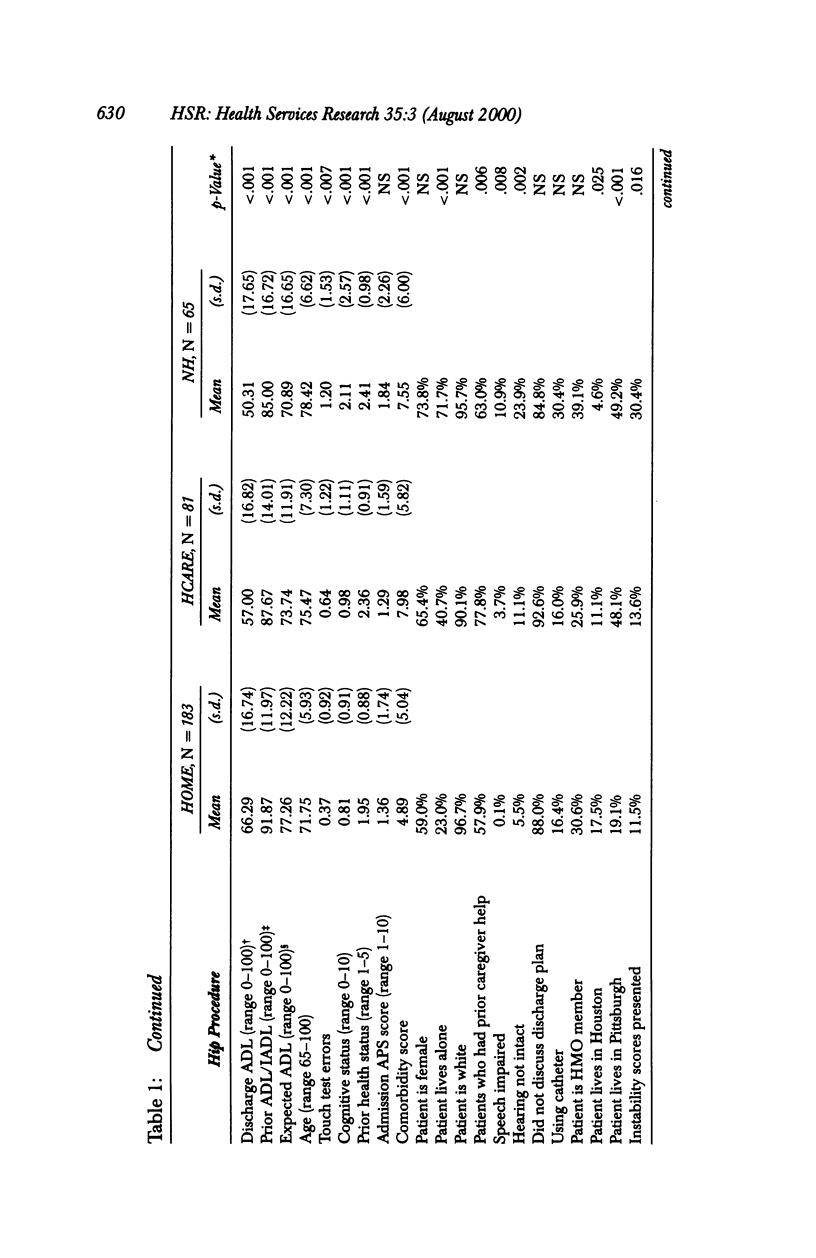
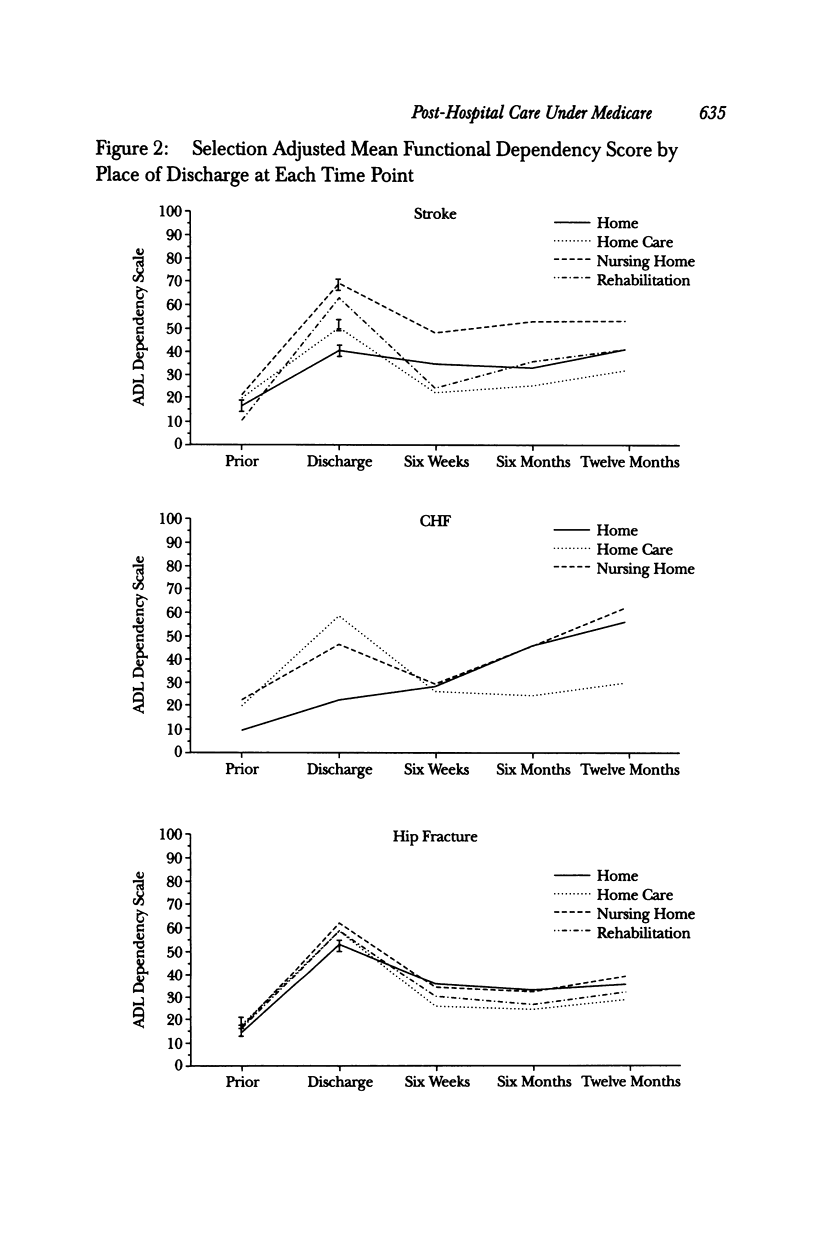
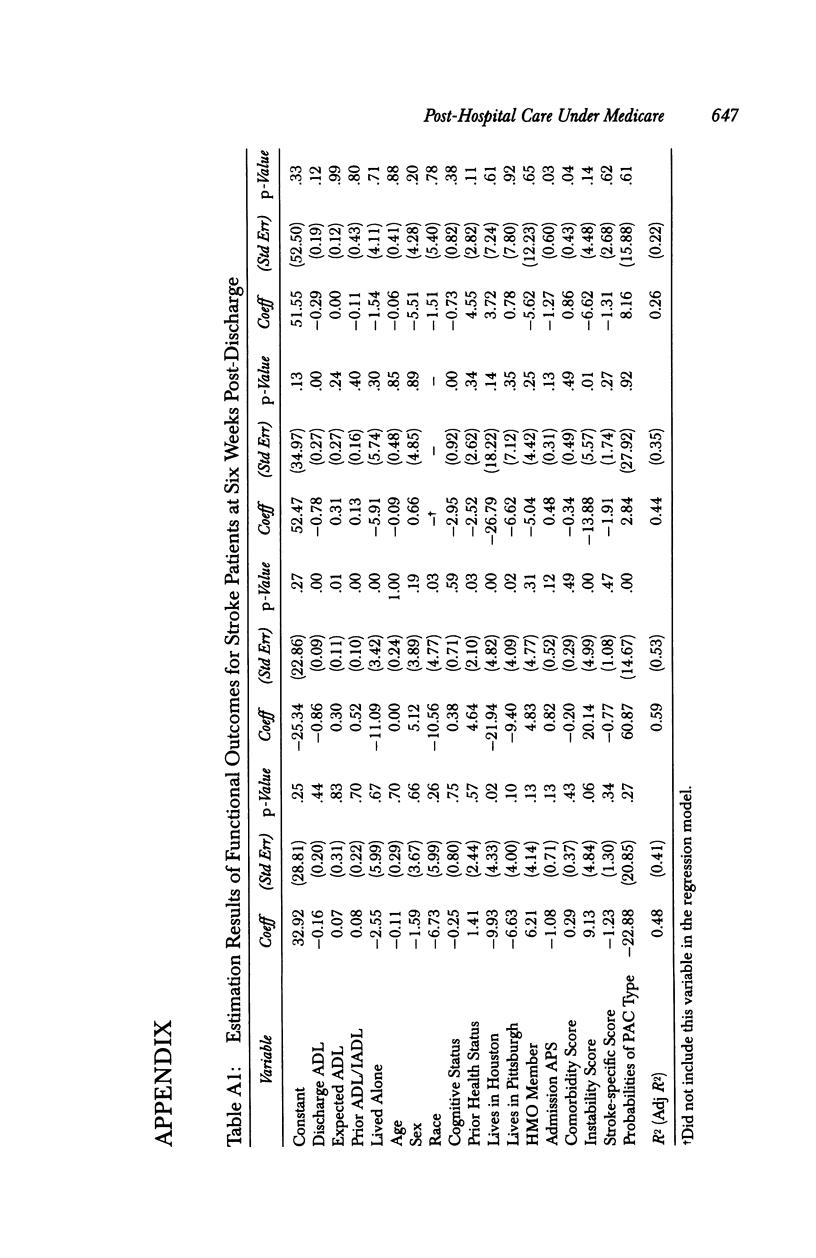
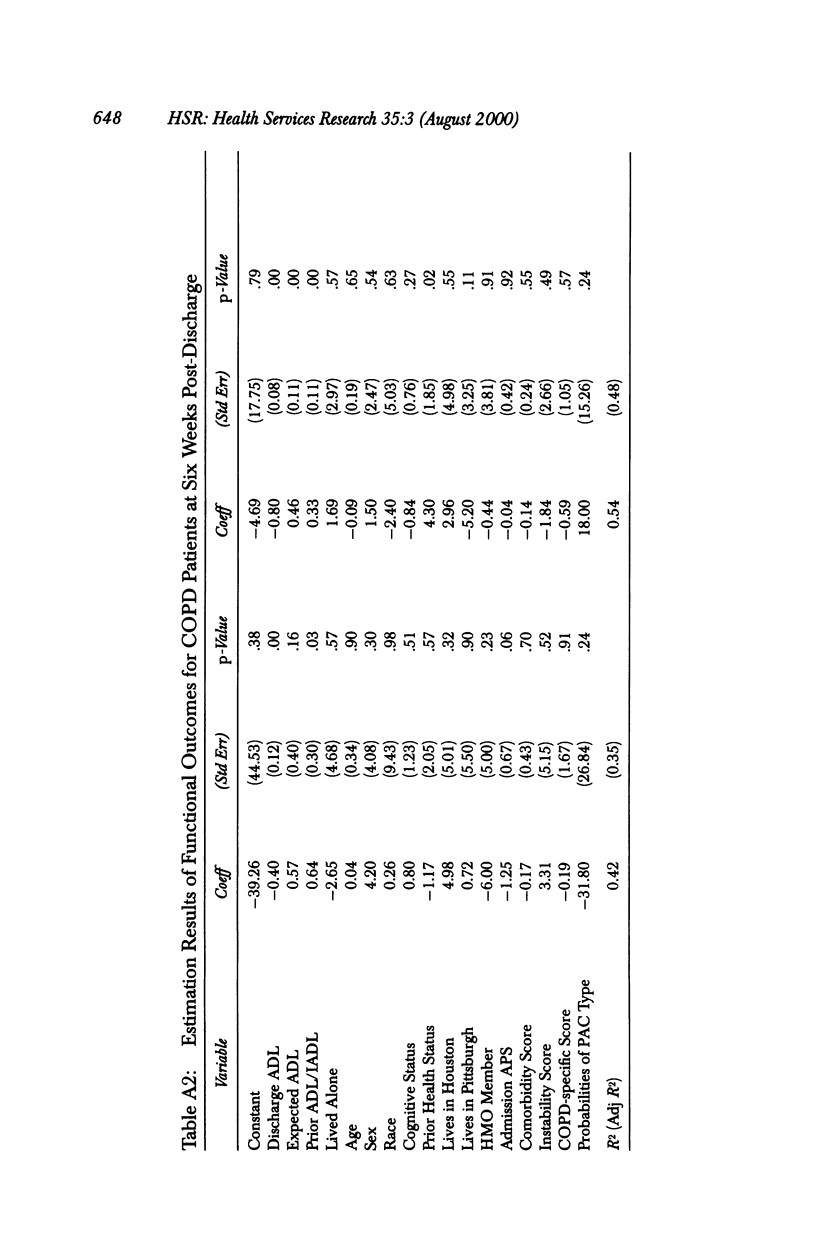
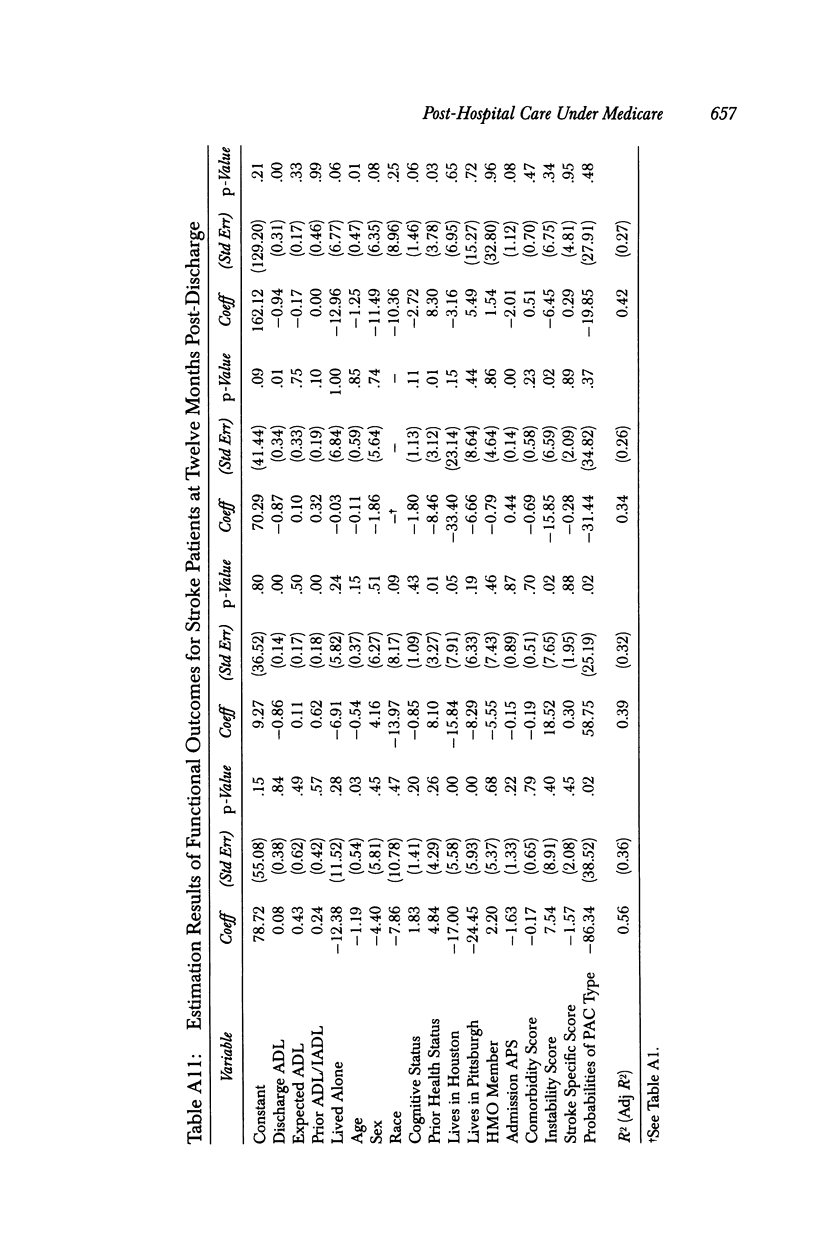
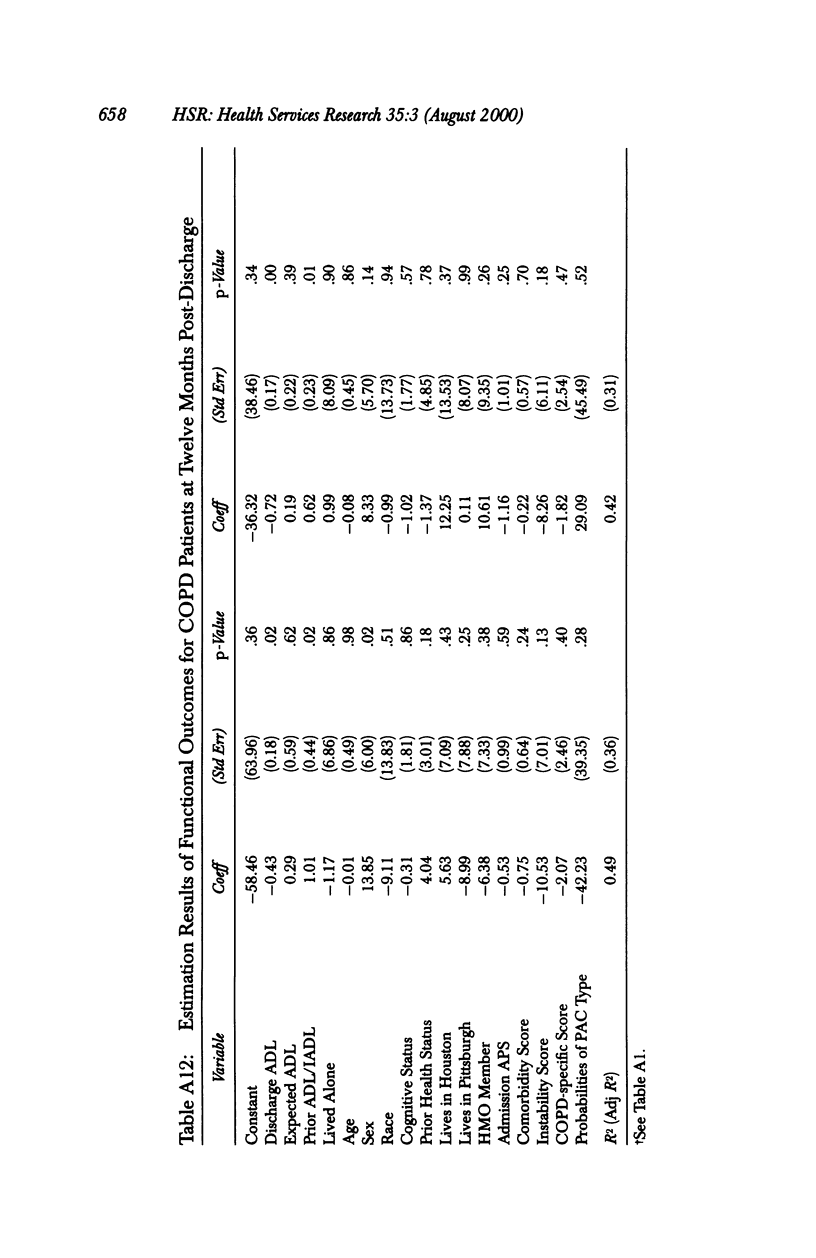
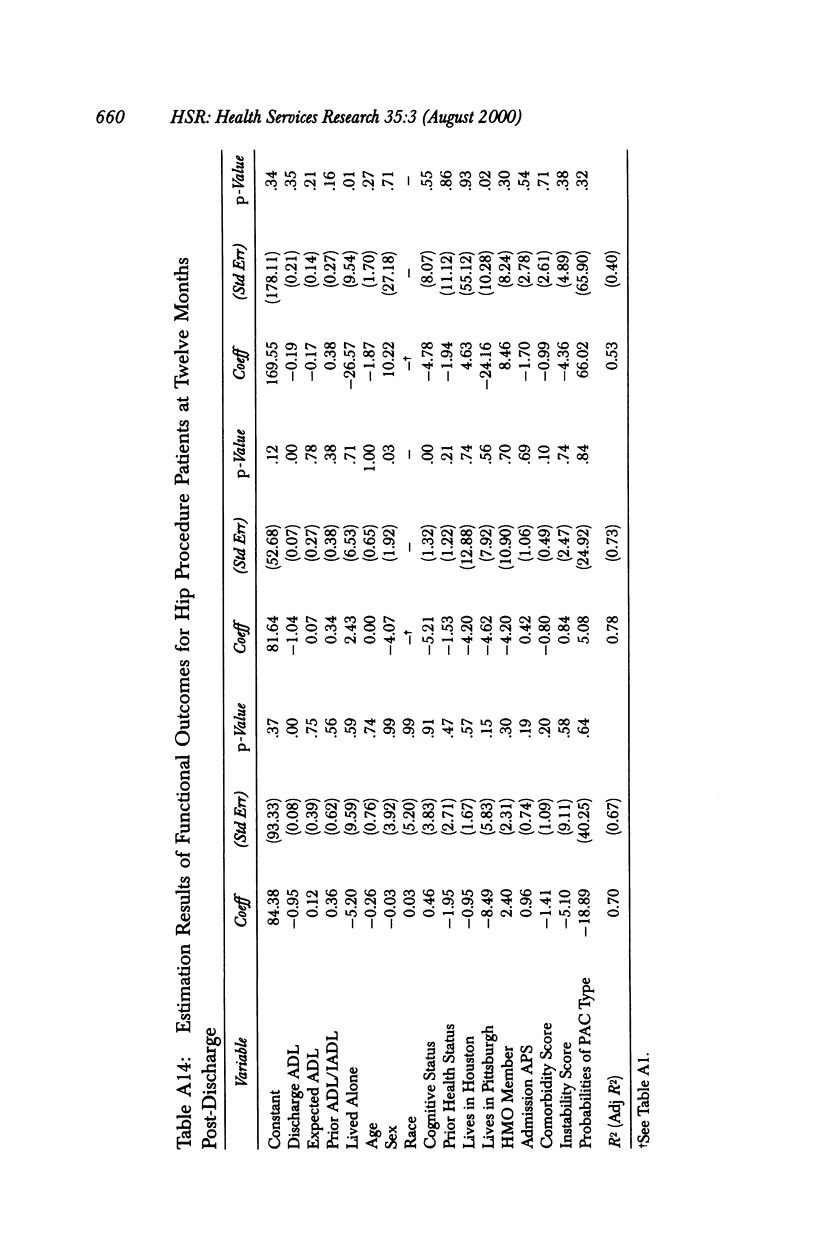
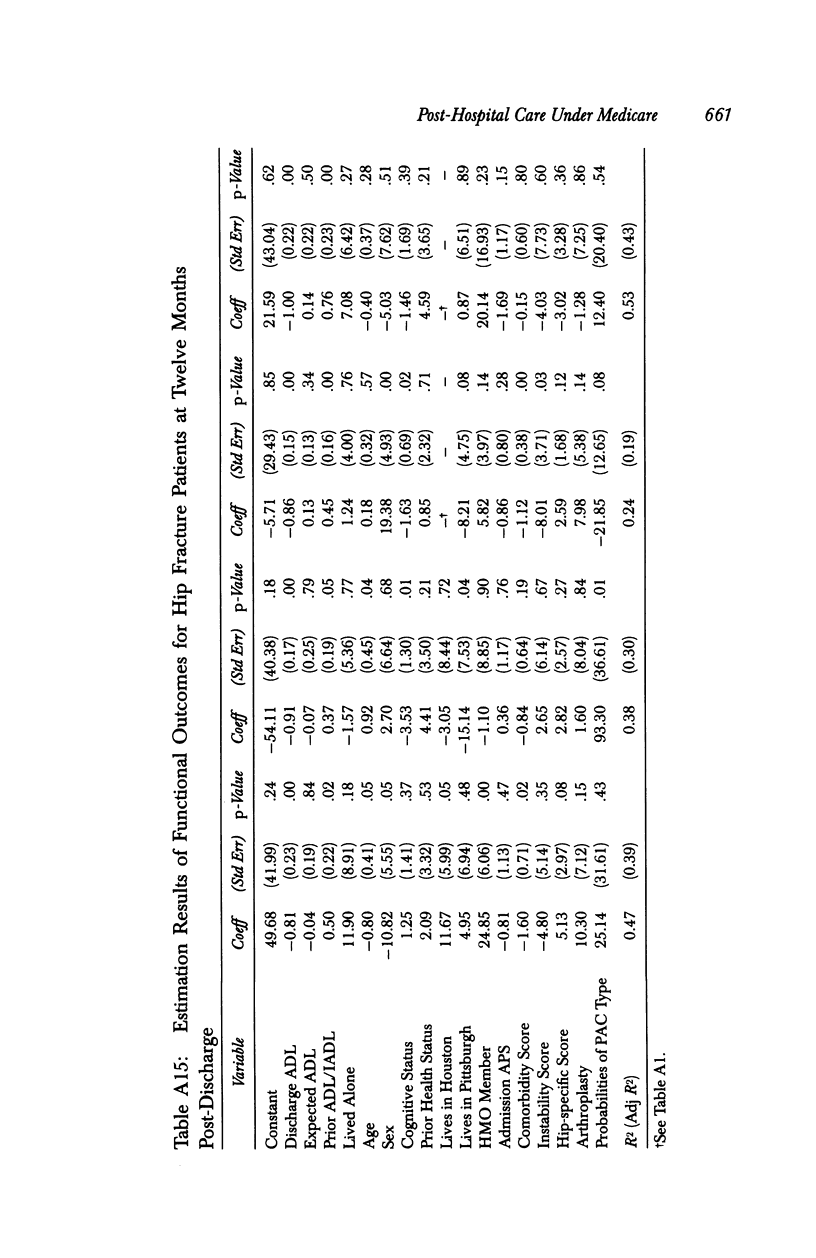
OBJECTIVE: To estimate the differences in functional outcomes attributable to discharge to one of four different venues for post-hospital care for each of five different types of illness associated with post-hospital care: stroke, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), hip procedures, and hip fracture, and to estimate the costs and benefits associated with discharge to the type of care that was estimated to produce the greatest improvement. STUDY SETTING/DATA SOURCES: Consecutive patients with any of the target diagnoses were enrolled from 52 hospitals in three cities. Data sources included interviews with patients or their proxies, medical record reviews, and the Medicare Automated Data Retrieval System. ANALYSIS: A two-stage regression model looked first at the factors associated with discharge to each type of post-hospital care and then at the outcomes associated with each location. An instrumental variables technique was used to adjust for selection bias. A predictive model was created for each patient to estimate how that person would have fared had she or he been discharged to each type of care. The optimal discharge location was determined as that which produced the greatest improvement in function after adjusting for patients' baseline characteristics. The costs of discharge to the optimal type of care was based on the differences in mean costs for each location. DATA COLLECTION/EXTRACTION METHODS: Data were collected from patients or their proxies at discharge from hospital and at three post-discharge follow-up times: six weeks, six months, and one year. In addition, the medical records for each participant were abstracted by trained abstractors, using a modification of the Medisgroups method, and Medicare data were summarized for the years before and after the hospitalization. PRINCIPAL FINDINGS: In general, patients discharged to nursing homes fared worst and those sent home with home health care or to rehabilitation did best. Because the cost of rehabilitation is high, greater use of home care could result in improved outcomes at modest or no additional cost. CONCLUSIONS: Better decisions about where to discharge patients could improve the course of many patients. It is possible to save money by making wiser discharge planning decisions. Nursing homes are generally associated with poorer outcomes and higher costs than the other post-hospital care modalities.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Coulton C. J., Dunkle R. E., Chow J. C., Haug M., Vielhaber D. P. Dimensions of post-hospital care decision-making: a factor analytic study. Gerontologist. 1988 Apr;28(2):218–223. doi: 10.1093/geront/28.2.218. [DOI] [PubMed] [Google Scholar]
- DesHarnais S., Chesney J., Fleming S. Trends and regional variations in hospital utilization and quality during the first two years of the prospective payment system. Inquiry. 1988 Fall;25(3):374–382. [PubMed] [Google Scholar]
- FINK M., GREEN M., BENDER M. B. The face-hand test as a diagnostic sign of organic mental syndrome. Neurology. 1952 Jan-Feb;2(1):46–58. doi: 10.1212/wnl.2.1-2.46. [DOI] [PubMed] [Google Scholar]
- Finch M., Kane R. L., Philp I. Developing a new metric for ADLs. J Am Geriatr Soc. 1995 Aug;43(8):877–884. doi: 10.1111/j.1532-5415.1995.tb05530.x. [DOI] [PubMed] [Google Scholar]
- Gornick M., Hall M. J. Trends in Medicare use of post-hospital care. Health Care Financ Rev. 1988 Dec;Spec No:27–38. [PMC free article] [PubMed] [Google Scholar]
- Guterman S., Dobson A. Impact of the Medicare prospective payment system for hospitals. Health Care Financ Rev. 1986 Spring;7(3):97–114. [PMC free article] [PubMed] [Google Scholar]
- Iezzoni L. I., Moskowitz M. A. A clinical assessment of MedisGroups. JAMA. 1988 Dec 2;260(21):3159–3163. doi: 10.1001/jama.260.21.3159. [DOI] [PubMed] [Google Scholar]
- Jenkins E. L. Workplace homicide: industries and occupations at high risk. Occup Med. 1996 Apr-Jun;11(2):219–225. [PubMed] [Google Scholar]
- Kahn K. L., Rubenstein L. V., Draper D., Kosecoff J., Rogers W. H., Keeler E. B., Brook R. H. The effects of the DRG-based prospective payment system on quality of care for hospitalized Medicare patients. An introduction to the series. JAMA. 1990 Oct 17;264(15):1953–1955. [PubMed] [Google Scholar]
- Kane R. L., Chen Q., Blewett L. A., Sangl J. Do rehabilitative nursing homes improve the outcomes of care? J Am Geriatr Soc. 1996 May;44(5):545–554. doi: 10.1111/j.1532-5415.1996.tb01440.x. [DOI] [PubMed] [Google Scholar]
- Kane R. L., Finch M., Blewett L., Chen Q., Burns R., Moskowitz M. Use of post-hospital care by Medicare patients. J Am Geriatr Soc. 1996 Mar;44(3):242–250. doi: 10.1111/j.1532-5415.1996.tb00909.x. [DOI] [PubMed] [Google Scholar]
- Knaus W. A., Draper E. A., Wagner D. P., Zimmerman J. E. APACHE II: a severity of disease classification system. Crit Care Med. 1985 Oct;13(10):818–829. [PubMed] [Google Scholar]
- Kosecoff J., Kahn K. L., Rogers W. H., Reinisch E. J., Sherwood M. J., Rubenstein L. V., Draper D., Roth C. P., Chew C., Brook R. H. Prospective payment system and impairment at discharge. The 'quicker-and-sicker' story revisited. JAMA. 1990 Oct 17;264(15):1980–1983. [PubMed] [Google Scholar]
- Kramer A. M., Steiner J. F., Schlenker R. E., Eilertsen T. B., Hrincevich C. A., Tropea D. A., Ahmad L. A., Eckhoff D. G. Outcomes and costs after hip fracture and stroke. A comparison of rehabilitation settings. JAMA. 1997 Feb 5;277(5):396–404. [PubMed] [Google Scholar]
- LaMar W. J., Gerberich S. G., Lohman W. H., Zaidman B. Work-related physical assault. J Occup Environ Med. 1998 Apr;40(4):317–324. doi: 10.1097/00043764-199804000-00005. [DOI] [PubMed] [Google Scholar]
- Lanza M. L., Milner J. The dollar cost of patient assault. Hosp Community Psychiatry. 1989 Dec;40(12):1227–1229. doi: 10.1176/ps.40.12.1227. [DOI] [PubMed] [Google Scholar]
- Leigh J. P., Miller T. R. Ranking occupations based upon the costs of job-related injuries and diseases. J Occup Environ Med. 1997 Dec;39(12):1170–1182. doi: 10.1097/00043764-199712000-00010. [DOI] [PubMed] [Google Scholar]
- Liss G. M., McCaskell L. Injuries due to violence: workers' compensation claims among nurses in Ontario. AAOHN J. 1994 Aug;42(8):384–390. [PubMed] [Google Scholar]
- McClellan M., McNeil B. J., Newhouse J. P. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. 1994 Sep 21;272(11):859–866. [PubMed] [Google Scholar]
- Morrisey M. A., Sloan F. A., Valvona J. Medicare prospective payment and posthospital transfers to subacute care. Med Care. 1988 Jul;26(7):685–698. doi: 10.1097/00005650-198807000-00004. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975 Oct;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Shaughnessy P. W., Kramer A. M. The increased needs of patients in nursing homes and patients receiving home health care. N Engl J Med. 1990 Jan 4;322(1):21–27. doi: 10.1056/NEJM199001043220105. [DOI] [PubMed] [Google Scholar]
- Toscano G. Workplace violence: an analysis of bureau of labor statistics data. Occup Med. 1996 Apr-Jun;11(2):227–235. [PubMed] [Google Scholar]
- Yassi A. Assault and abuse of health care workers in a large teaching hospital. CMAJ. 1994 Nov 1;151(9):1273–1279. [PMC free article] [PubMed] [Google Scholar]


