Abstract
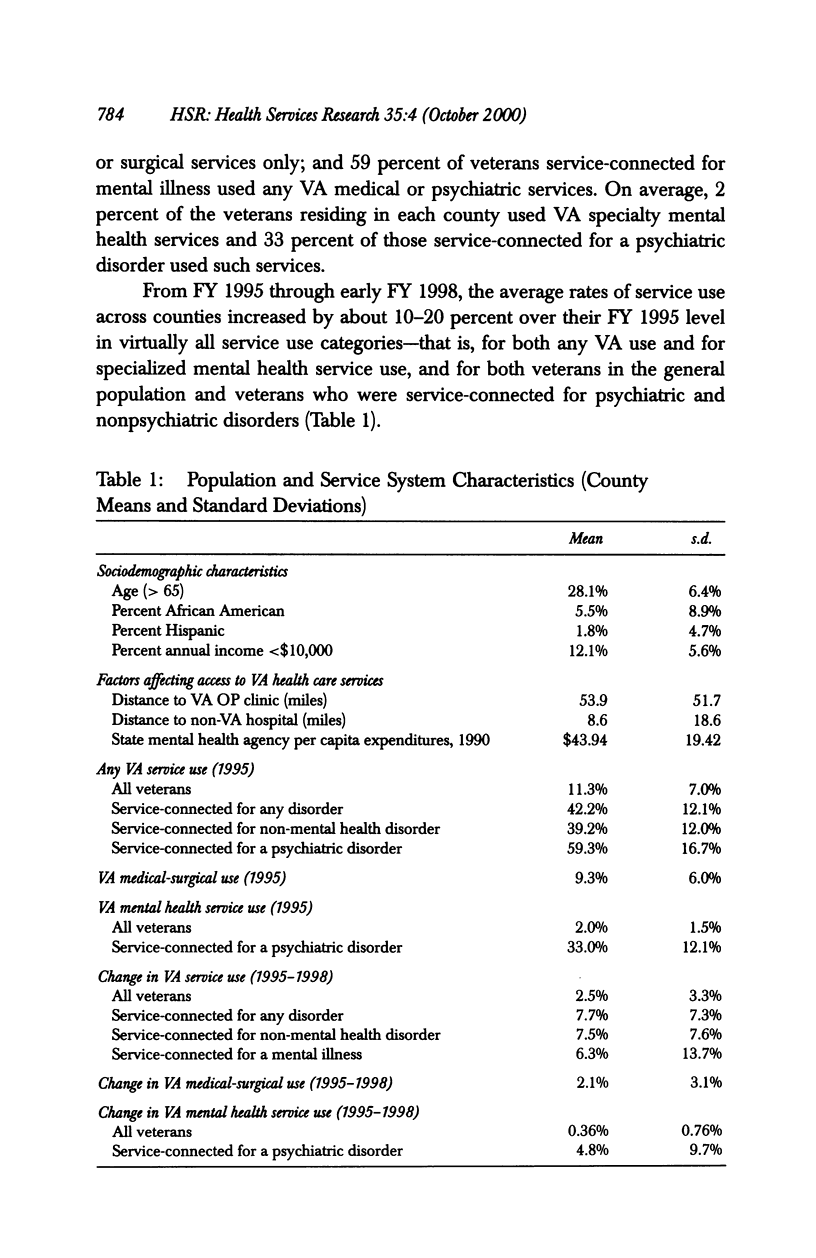
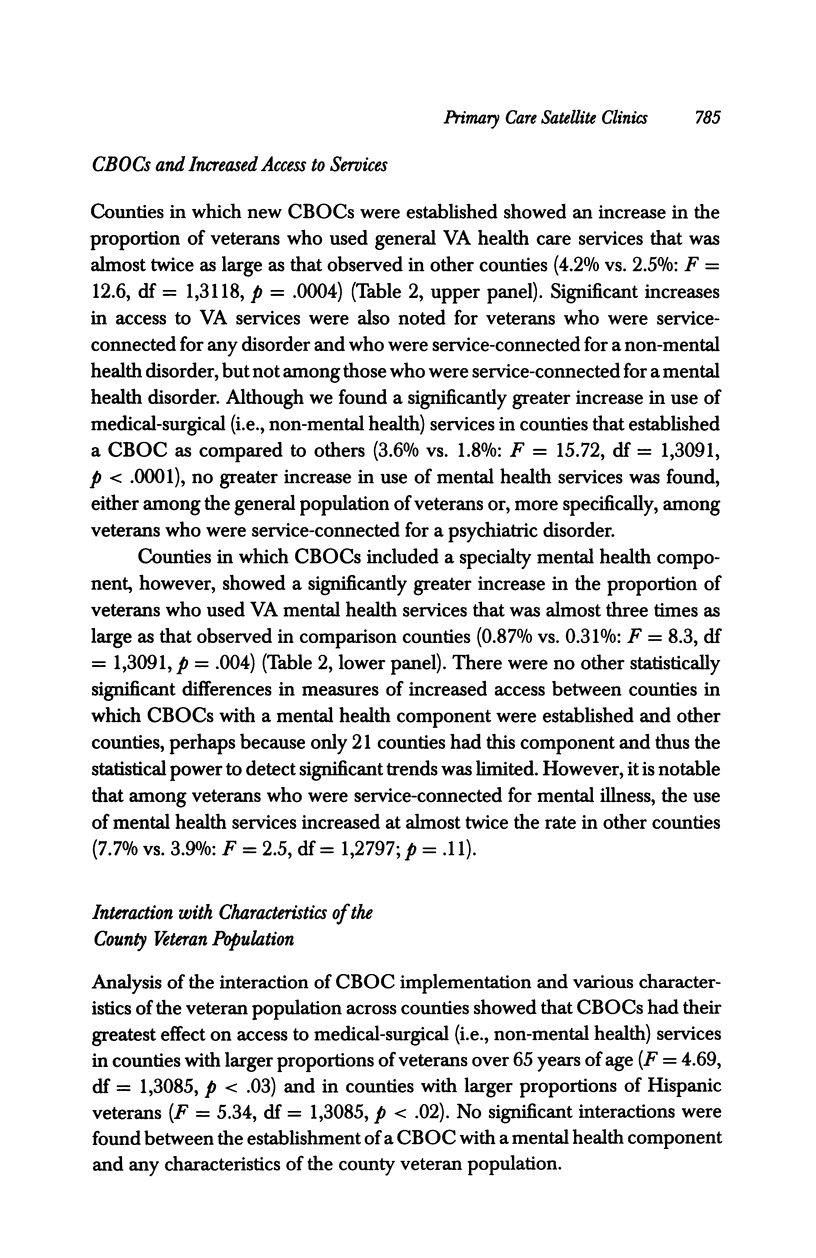
OBJECTIVES: To evaluate the relationship between the implementation of community-based primary care clinics and improved access to general health care and/or mental health care, in both the general population and among people with disabling mental illness. STUDY SETTING: The 69 new community-based primary care clinics in underserved areas, established by the Department of Veterans Affairs (VA) between the last quarter of FY 1995 and the second quarter of FY 1998, including the 21 new clinics with a specialty mental health care component. DATA SOURCES: VA inpatient and outpatient workload files, 1990 U.S. Census data, and VA Compensation and Pension files were used to determine the proportion of all veterans, and the proportion of disabled veterans, living in each U.S. county who used VA general health care services and VA mental health services before and after these clinics began operation. DESIGN: Analysis of covariance was used to compare changes, from late FY 1995 through early FY 1998, in access to VA services in counties in which new primary care clinics were located, in counties in which clinics that included specialized mental health components were located, and for comparison, in other U.S. counties, adjusting for potentially confounding factors. KEY FINDINGS: Counties in which new clinics were located showed a significant increase from the FY 1995-FY 1998 study dates in the proportion of veterans who used general VA health care services. This increase was almost twice as large as that observed in comparison counties (4.2% vs. 2.5%: F = 12.6, df = 1,3118, p = .0004). However, the introduction of these clinics was not associated with a greater use of specialty VA mental health services in the general veteran population, or of either general health care services or mental health services among veterans who received VA compensation for psychiatric disorders. In contrast, in counties with new clinics that included a mental health component the proportion of veterans who used VA mental health services increased to almost three times the proportion in comparison counties (0.87% vs. 0.31%: F = 8.3, df = 1,3091, p = .004). CONCLUSIONS: Community-based primary care clinics can improve access to general health care services, but a specialty mental health care component appears to be needed to improve access to mental health services.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cohen J. J. Transforming the size and composition of the physician work force to meet the demands of health care reform. N Engl J Med. 1993 Dec 9;329(24):1810–1812. doi: 10.1056/NEJM199312093292412. [DOI] [PubMed] [Google Scholar]
- Druss B. G., Hoff R. A., Rosenheck R. A. Underuse of antidepressants in major depression: prevalence and correlates in a national sample of young adults. J Clin Psychiatry. 2000 Mar;61(3):234–239. [PubMed] [Google Scholar]
- Druss B. G., Rosenheck R. A. Locus of mental health treatment in an integrated service system. Psychiatr Serv. 2000 Jul;51(7):890–892. doi: 10.1176/appi.ps.51.7.890. [DOI] [PubMed] [Google Scholar]
- Goldman L. The value of cardiology. N Engl J Med. 1996 Dec 19;335(25):1918–1919. doi: 10.1056/NEJM199612193352510. [DOI] [PubMed] [Google Scholar]
- Greenfield S., Nelson E. C., Zubkoff M., Manning W., Rogers W., Kravitz R. L., Keller A., Tarlov A. R., Ware J. E., Jr Variations in resource utilization among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992 Mar 25;267(12):1624–1630. [PubMed] [Google Scholar]
- Hough R. L., Landsverk J. A., Karno M., Burnam M. A., Timbers D. M., Escobar J. I., Regier D. A. Utilization of health and mental health services by Los Angeles Mexican Americans and non-Hispanic whites. Arch Gen Psychiatry. 1987 Aug;44(8):702–709. doi: 10.1001/archpsyc.1987.01800200028005. [DOI] [PubMed] [Google Scholar]
- Jollis J. G., DeLong E. R., Peterson E. D., Muhlbaier L. H., Fortin D. F., Califf R. M., Mark D. B. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med. 1996 Dec 19;335(25):1880–1887. doi: 10.1056/NEJM199612193352505. [DOI] [PubMed] [Google Scholar]
- Regier D. A., Narrow W. E., Rae D. S., Manderscheid R. W., Locke B. Z., Goodwin F. K. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993 Feb;50(2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Rosenheck R., Stolar M. Access to public mental health services: determinants of population coverage. Med Care. 1998 Apr;36(4):503–512. doi: 10.1097/00005650-199804000-00006. [DOI] [PubMed] [Google Scholar]
- Schur C. L., Bernstein A. B., Berk M. L. The importance of distinguishing Hispanic subpopulations in the use of medical care. Med Care. 1987 Jul;25(7):627–641. doi: 10.1097/00005650-198707000-00006. [DOI] [PubMed] [Google Scholar]


