Abstract
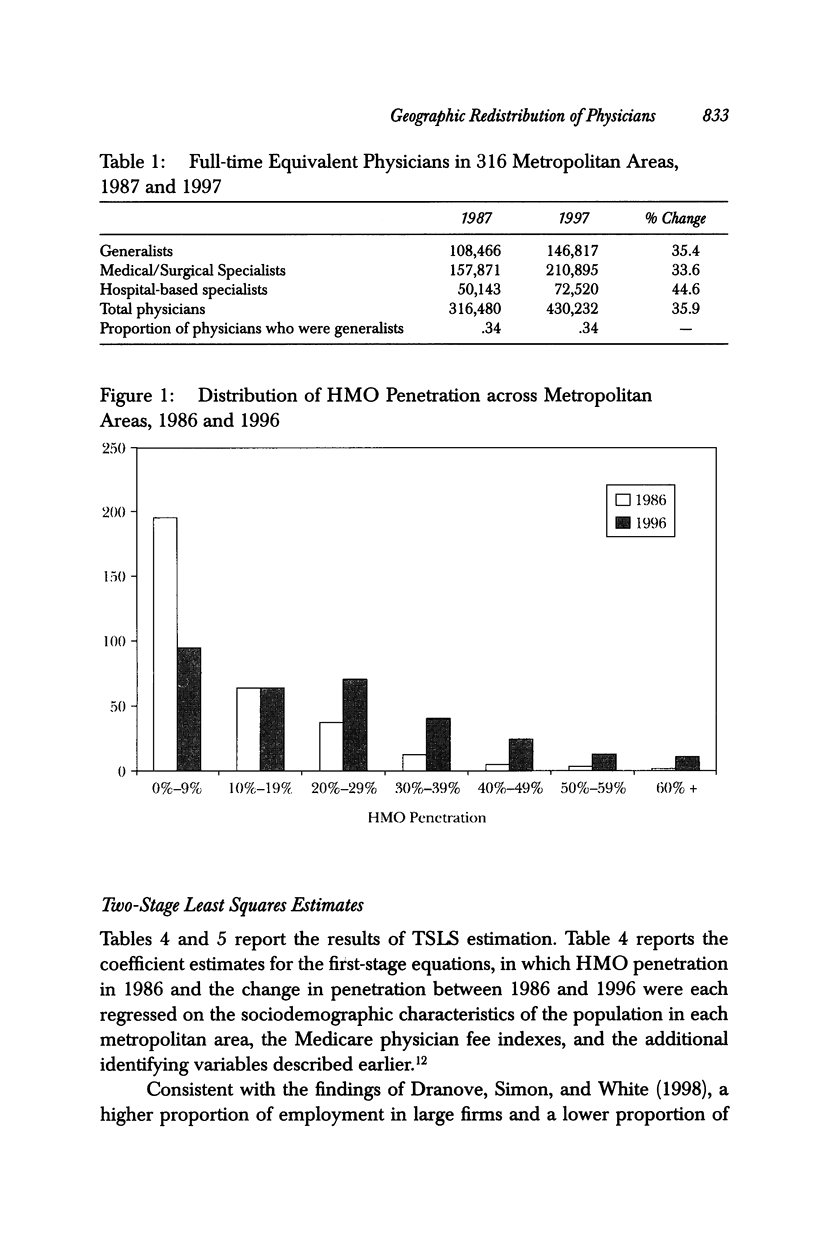
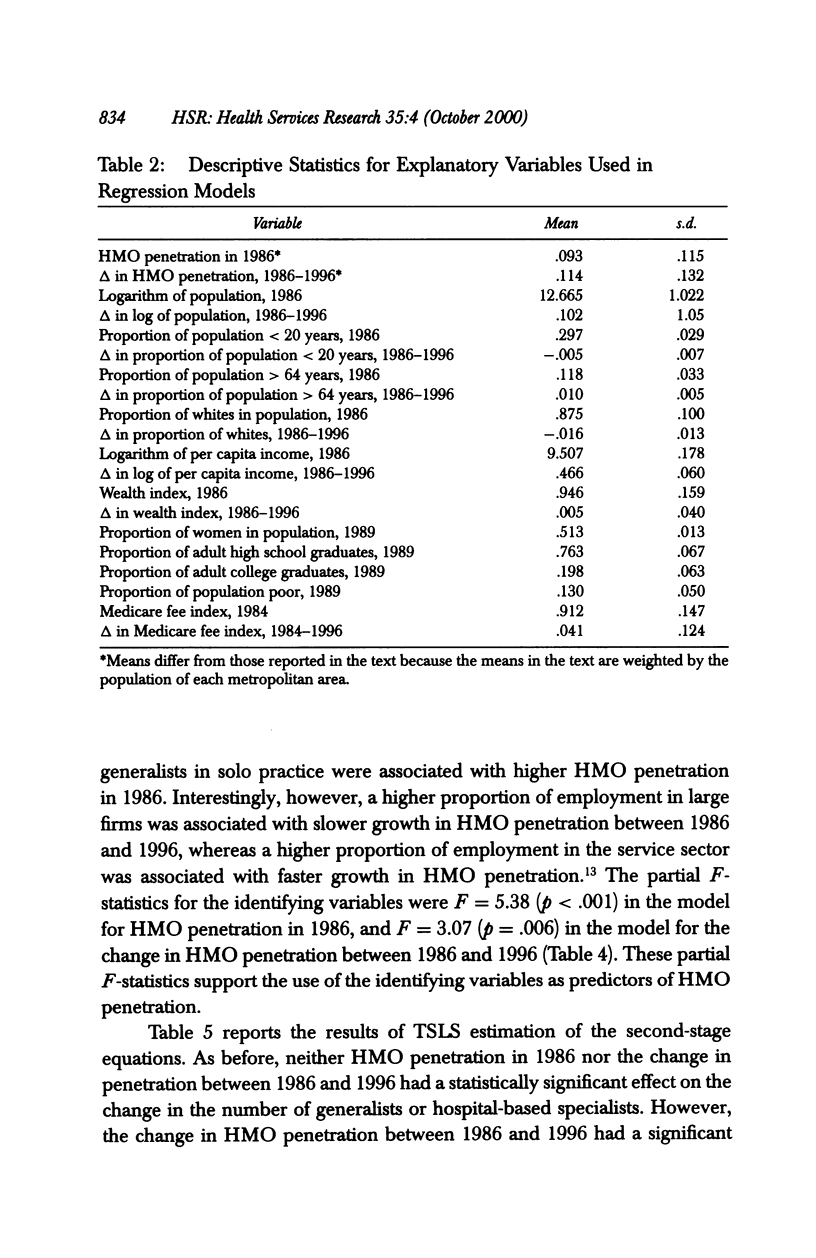
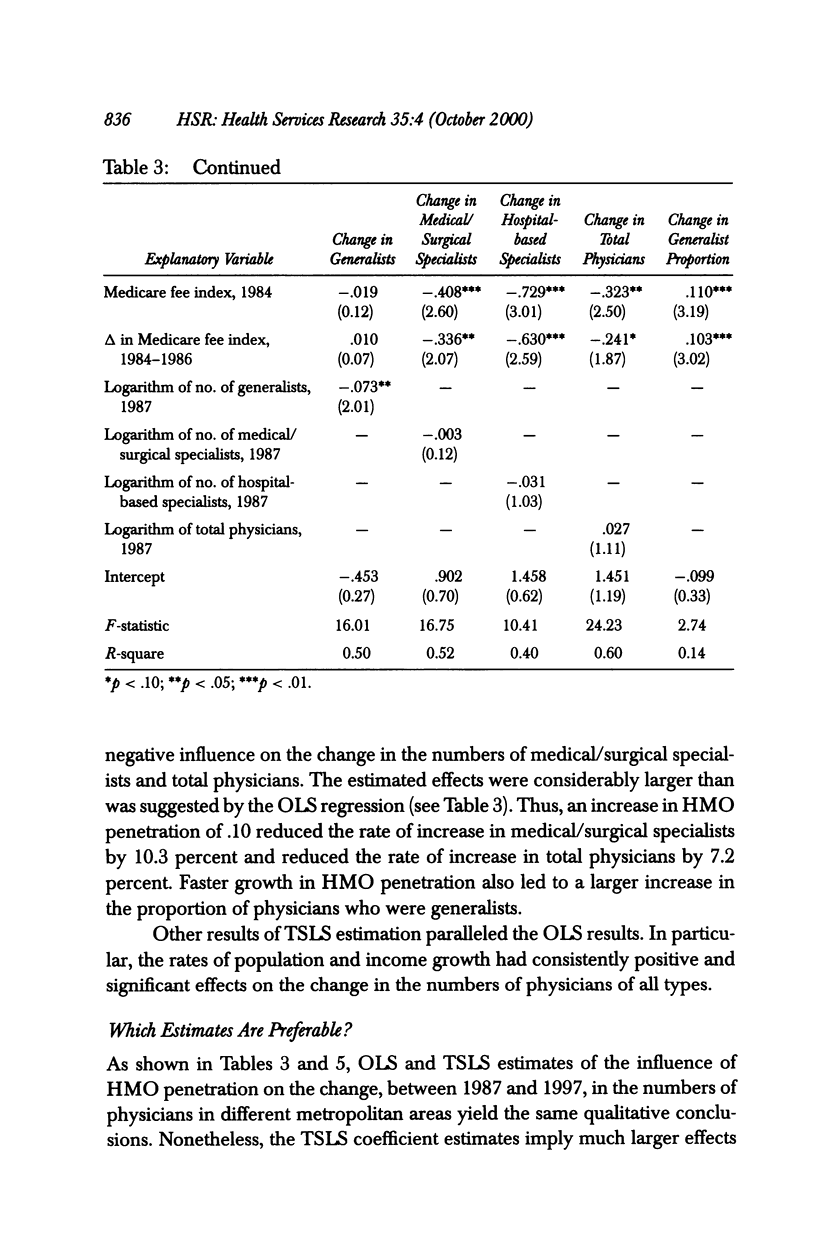
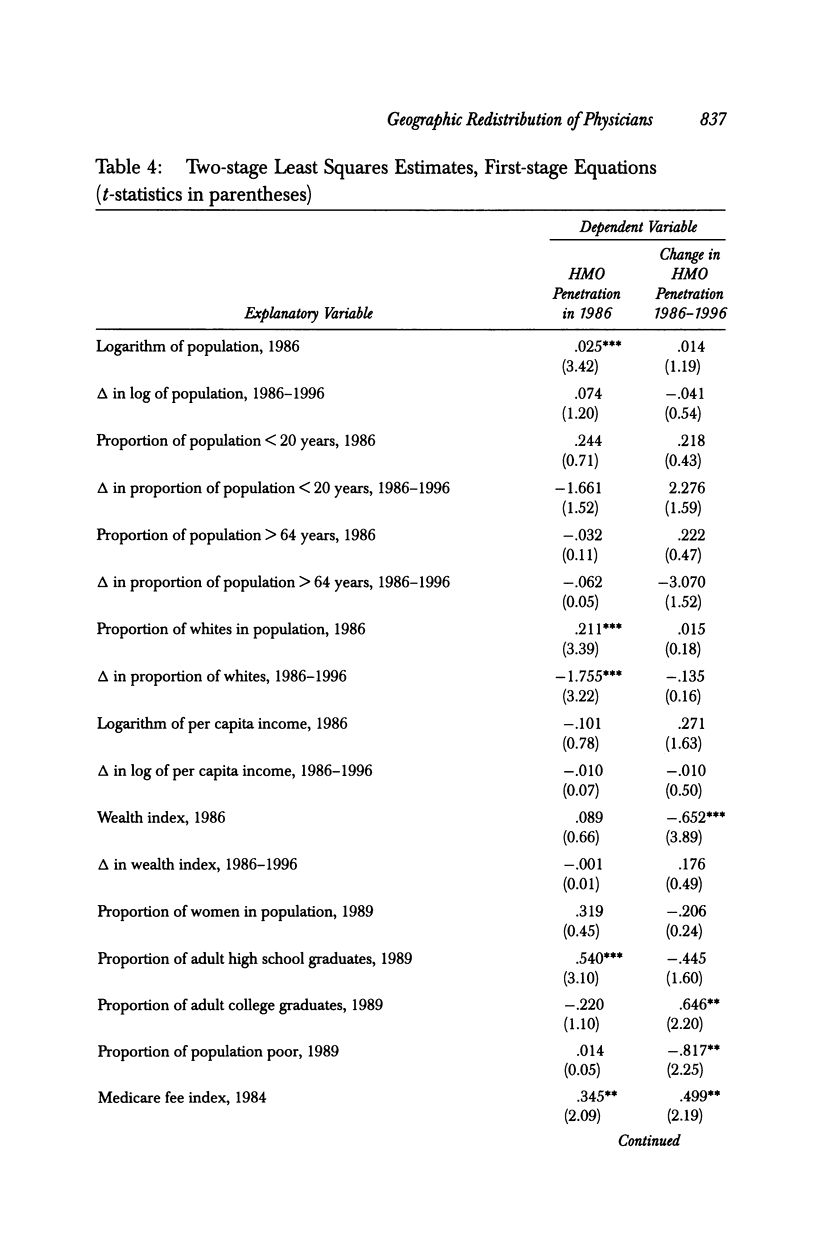
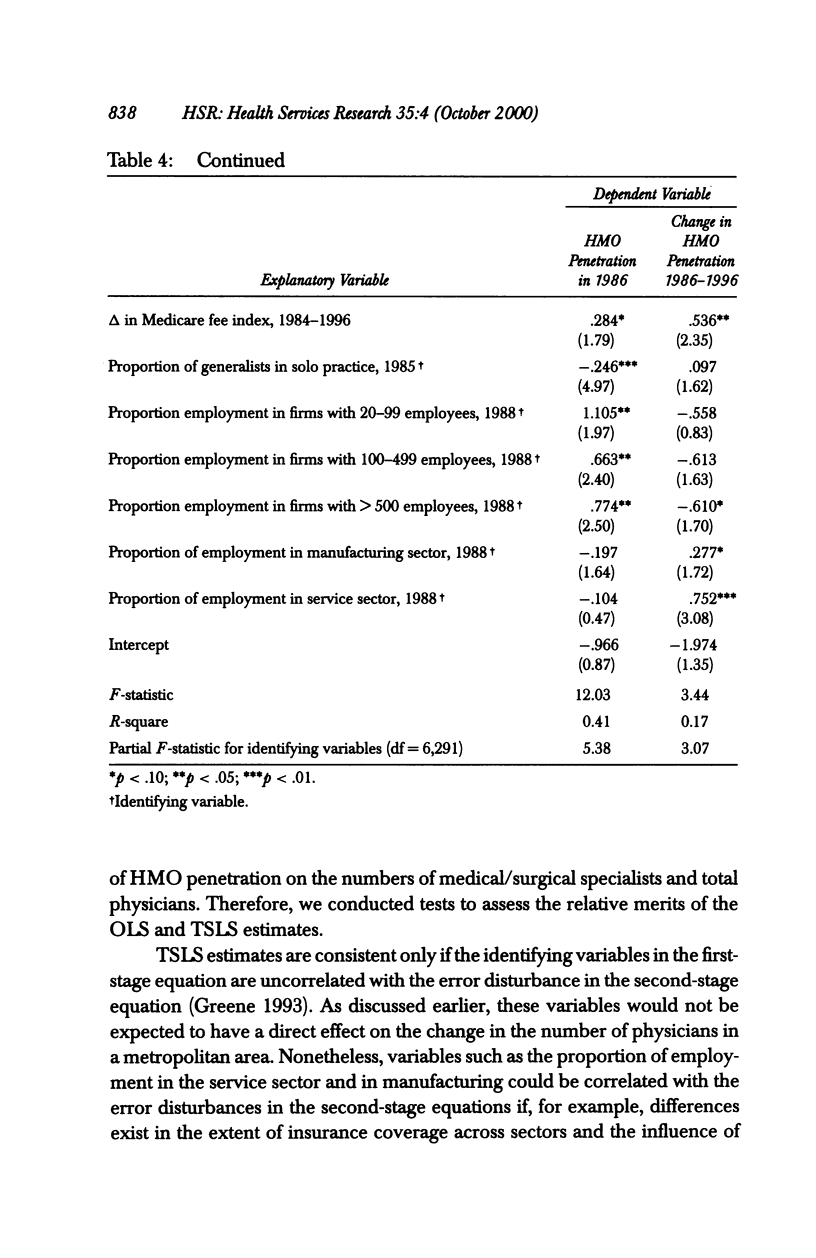
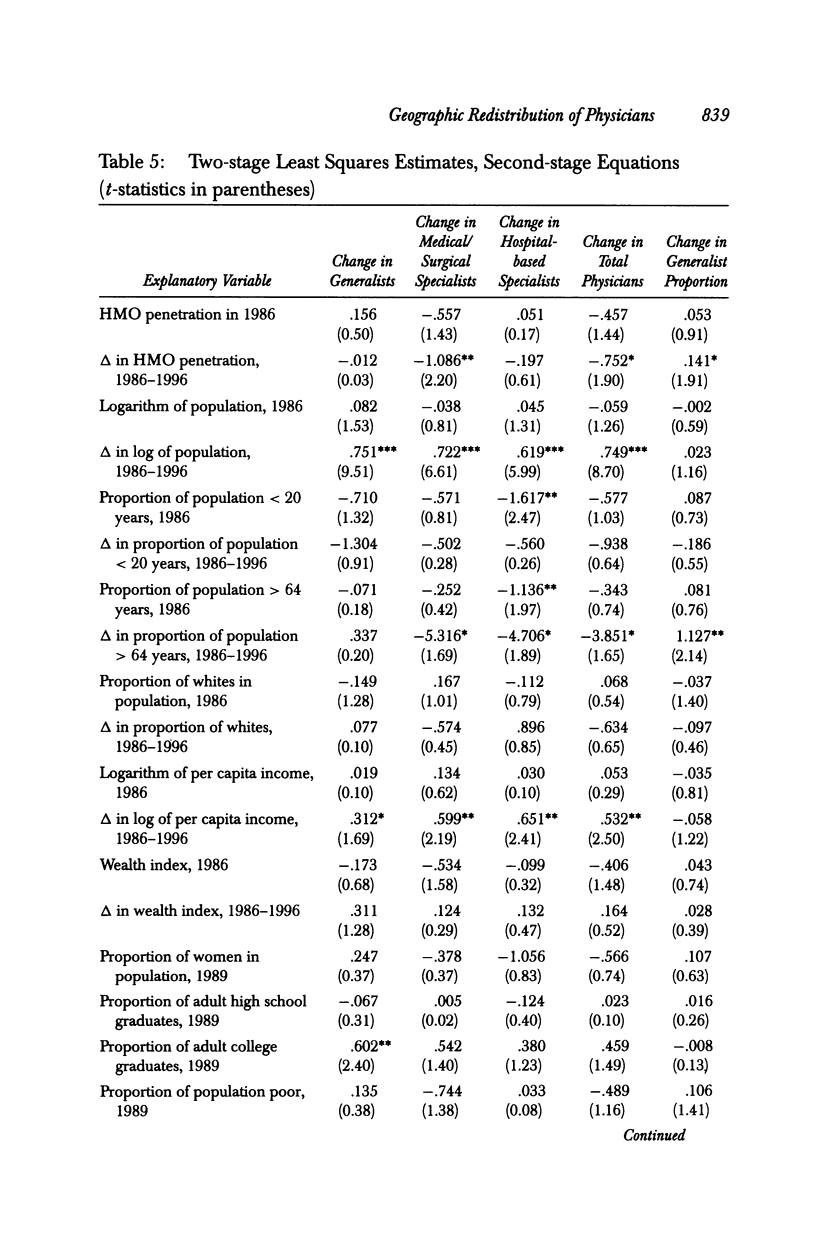
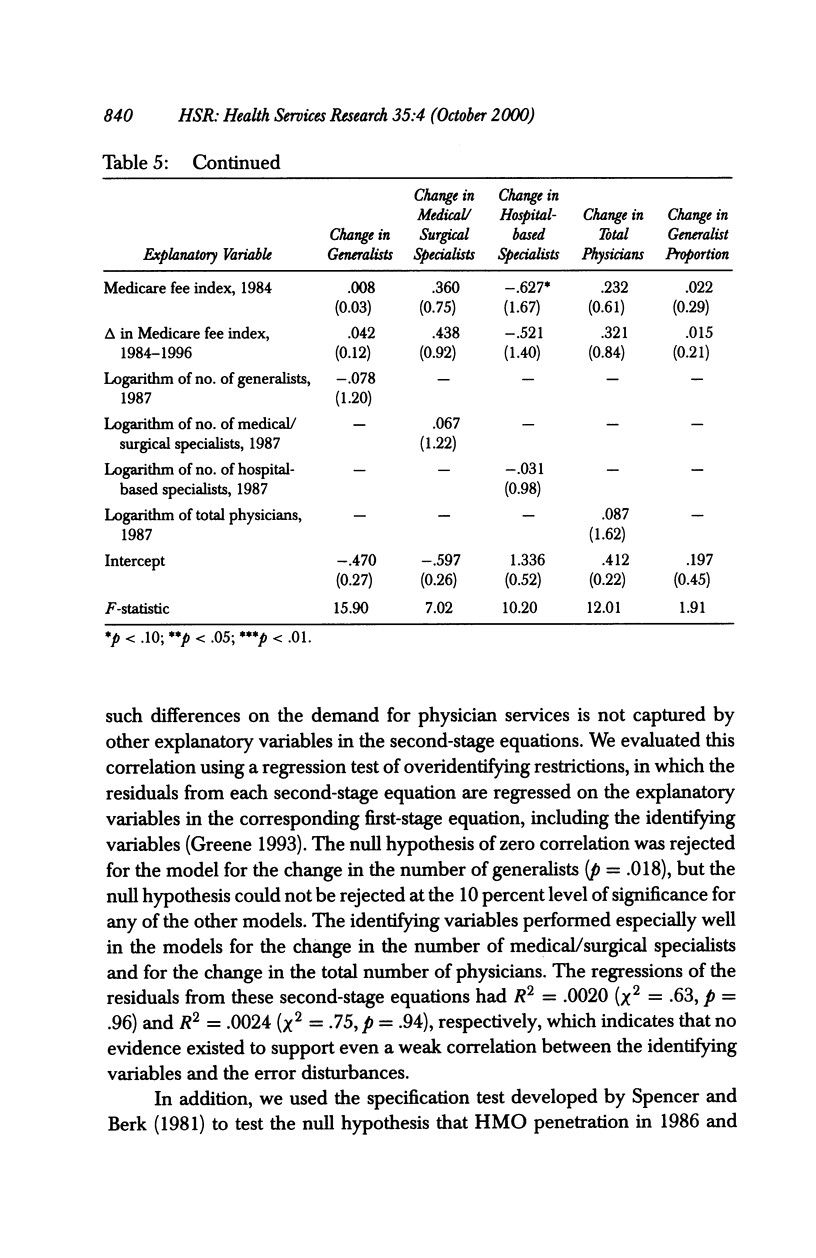
OBJECTIVE: To assess the impact of the growth in HMO penetration in different metropolitan areas on the change in the number of generalists, specialists, and total physicians, and on the change in the proportion of physicians who are generalists. DATA SOURCES/STUDY SETTING: The American Medical Association Physician Masterfile, to obtain the number of patient care generalists and specialists in 1987 and in 1997 who were practicing in each of 316 metropolitan areas in the United States. Additional data for each metropolitan area were obtained from a variety of sources, and included HMO penetration in 1986 and 1996. STUDY DESIGN: We estimated multivariate regression models in which the change in the number of physicians between 1987 and 1997 was a function of HMO penetration in 1986, the change in HMO penetration between 1986 and 1996, population characteristics and physician fees in 1986, and the change in population characteristics and fees between 1986 and 1996. Each model was estimated using ordinary least squares (OLS) and two-stage least squares (TSLS). PRINCIPAL FINDINGS: HMO penetration did not affect the number of generalist physicians or hospital-based specialists, but faster HMO growth led to smaller increases in the numbers of medical/surgical specialists and total physicians. Faster HMO growth also led to larger increases in the proportion of physicians who were generalists. Our best estimate is that an increase in HMO penetration of .10 between 1986 and 1996 reduced the rate of increase in medical/surgical specialists by 10.3 percent and reduced the rate of increase in total physicians by 7.2 percent. CONCLUSIONS: The findings of this study support the notion that HMOs reduce the demand for physician services, particularly for specialists' services. The findings also imply that, during the past decade, there has been a redistribution of physicians-especially medical/surgical specialists-from metropolitan areas with high HMO penetration to low-penetration areas.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker L. C. The effect of HMOs on fee-for-service health care expenditures: evidence from Medicare. J Health Econ. 1997 Aug;16(4):453–481. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- Dranove D., Simon C. J., White W. D. Determinants of managed care penetration. J Health Econ. 1998 Dec;17(6):729–745. doi: 10.1016/s0167-6296(97)00045-3. [DOI] [PubMed] [Google Scholar]
- Escarce J. J., Polsky D., Wozniak G. D., Pauly M. V., Kletke P. R. Health maintenance organization penetration and the practice location choices of new physicians: a study of large metropolitan areas in the United States. Med Care. 1998 Nov;36(11):1555–1566. doi: 10.1097/00005650-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Gold M. R., Hurley R., Lake T., Ensor T., Berenson R. A national survey of the arrangements managed-care plans make with physicians. N Engl J Med. 1995 Dec 21;333(25):1678–1683. doi: 10.1056/NEJM199512213332505. [DOI] [PubMed] [Google Scholar]
- Goldberg L. G., Greenberg W. The determinants of HMO enrollment and growth. Health Serv Res. 1981 Winter;16(4):421–438. [PMC free article] [PubMed] [Google Scholar]
- Hadley J., Mitchell J. M. Effects of HMO market penetration on physicians' work effort and satisfaction. Health Aff (Millwood) 1997 Nov-Dec;16(6):99–111. doi: 10.1377/hlthaff.16.6.99. [DOI] [PubMed] [Google Scholar]
- Miller R. H., Luft H. S. Managed care plan performance since 1980. A literature analysis. JAMA. 1994 May 18;271(19):1512–1519. [PubMed] [Google Scholar]
- Porell F. W., Wallack S. S. Medicare risk contracting: determinants of market entry. Health Care Financ Rev. 1990 Winter;12(2):75–85. [PMC free article] [PubMed] [Google Scholar]
- Remler D. K., Donelan K., Blendon R. J., Lundberg G. D., Leape L. L., Calkins D. R., Binns K., Newhouse J. P. What do managed care plans do to affect care? Results from a survey of physicians. Inquiry. 1997 Fall;34(3):196–204. [PubMed] [Google Scholar]
- Shea J. A., Kletke P. R., Wozniak G. D., Polsky D., Escarce J. J. Self-reported physician specialties and the primary care content of medical practice: a study of the AMA physician masterfile. American Medical Association. Med Care. 1999 Apr;37(4):333–338. doi: 10.1097/00005650-199904000-00003. [DOI] [PubMed] [Google Scholar]
- Simon C. J., Dranove D., White W. D. The effect of managed care on the incomes of primary care and specialty physicians. Health Serv Res. 1998 Aug;33(3 Pt 1):549–569. [PMC free article] [PubMed] [Google Scholar]
- Weiner J. P. Forecasting the effects of health reform on US physician workforce requirement. Evidence from HMO staffing patterns. JAMA. 1994 Jul 20;272(3):222–230. [PubMed] [Google Scholar]
- Welch W. P. HMO enrollment: a study of market forces and regulations. J Health Polit Policy Law. 1984 Winter;8(4):743–758. doi: 10.1215/03616878-8-4-743. [DOI] [PubMed] [Google Scholar]
- Wholey D., Feldman R., Christianson J. B. The effect of market structure on HMO premiums. J Health Econ. 1995 May;14(1):81–105. doi: 10.1016/0167-6296(94)00039-7. [DOI] [PubMed] [Google Scholar]


