Abstract
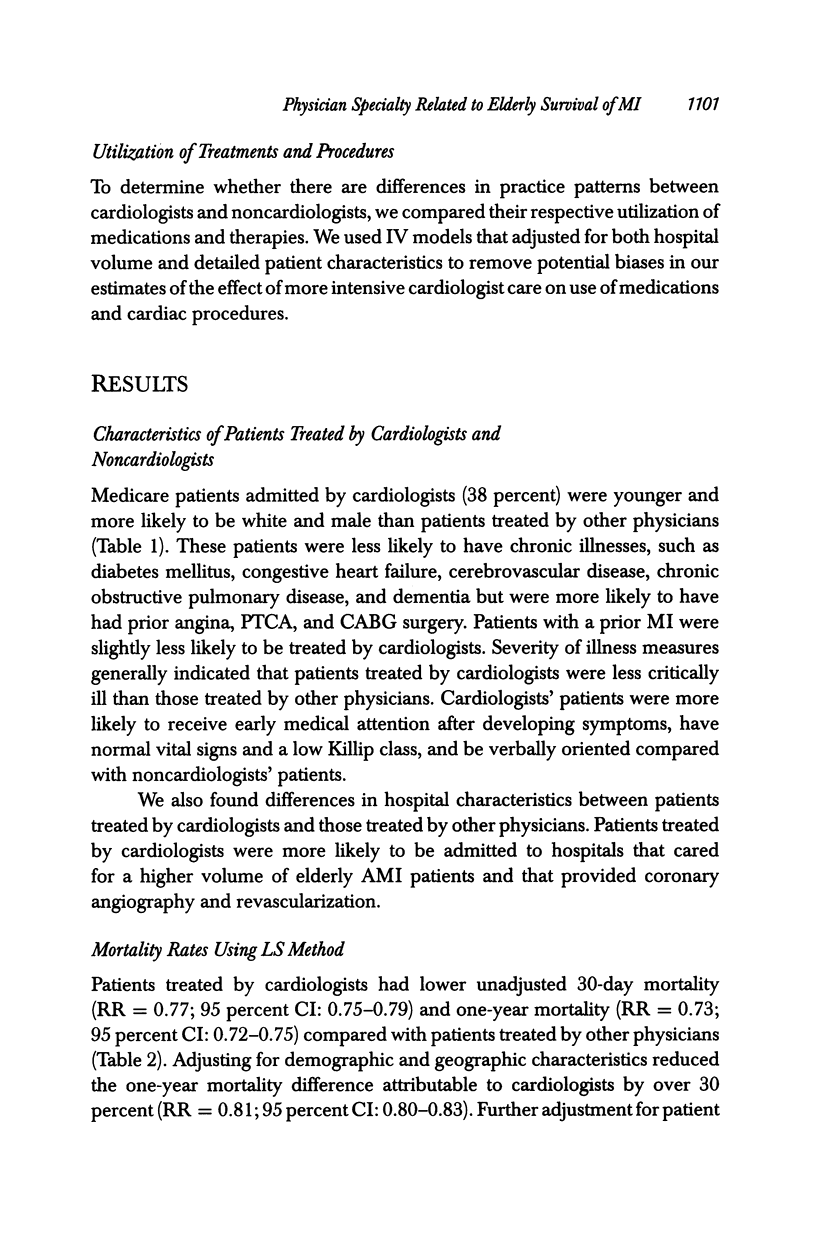
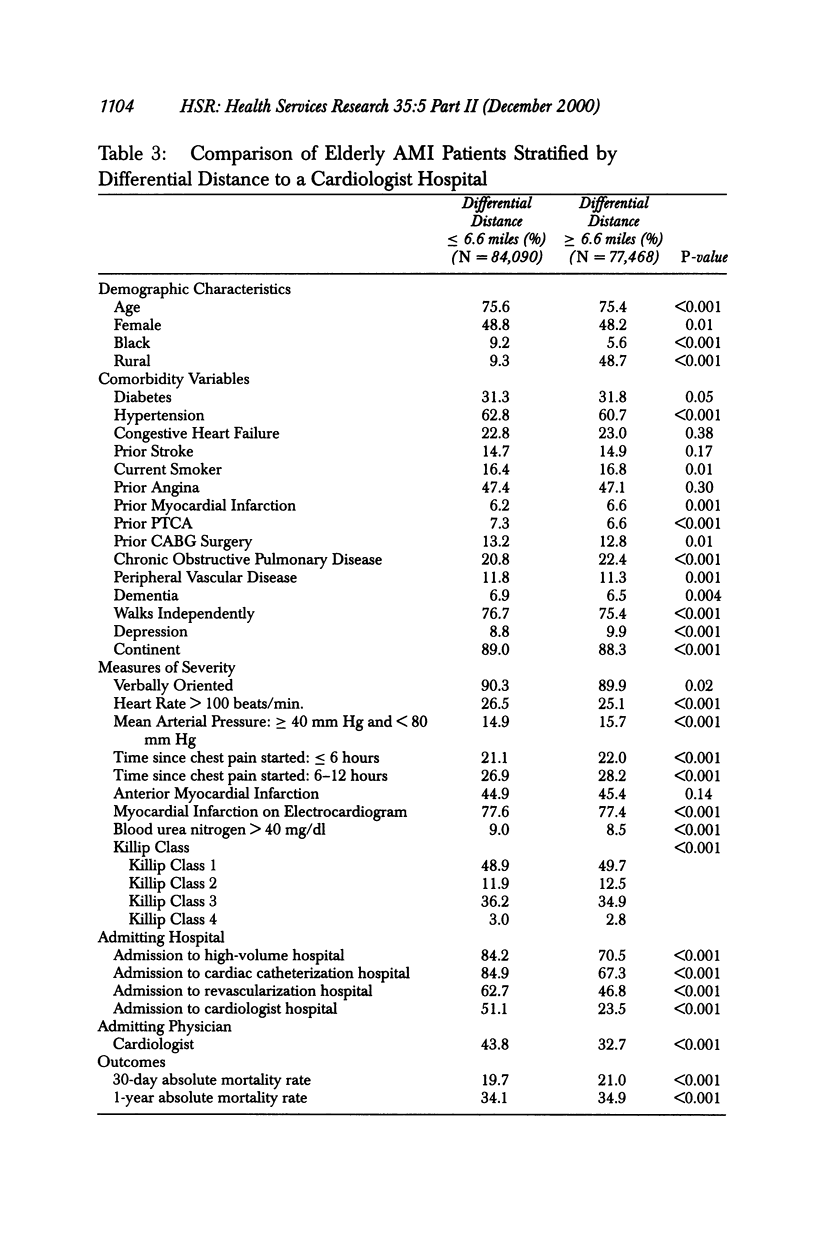
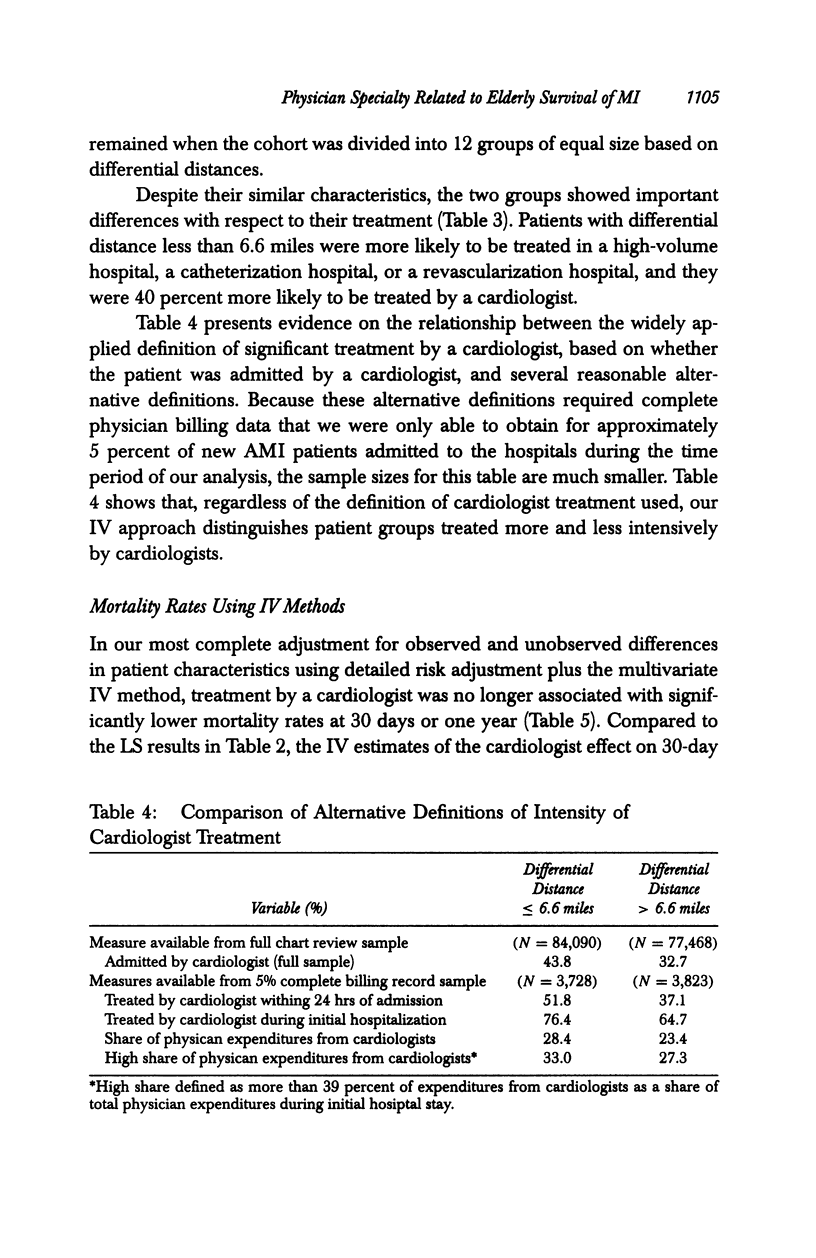
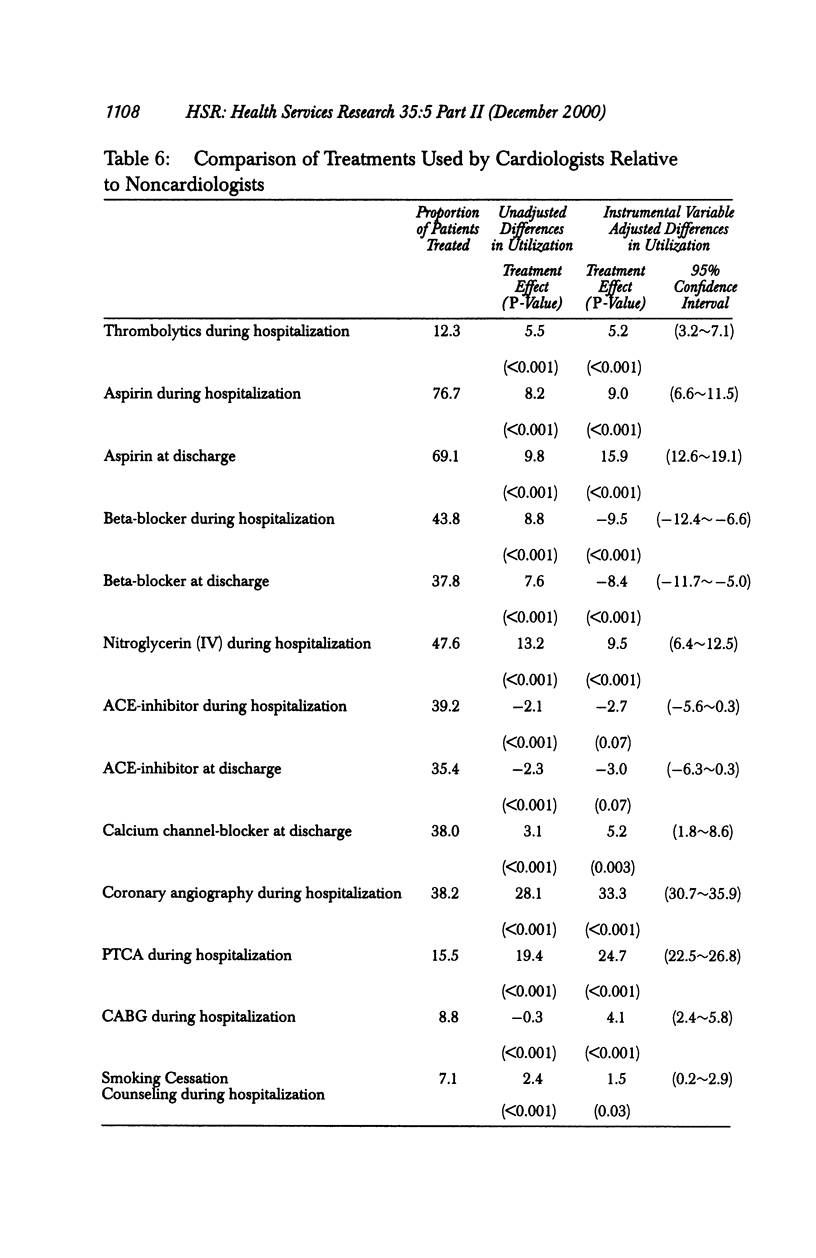
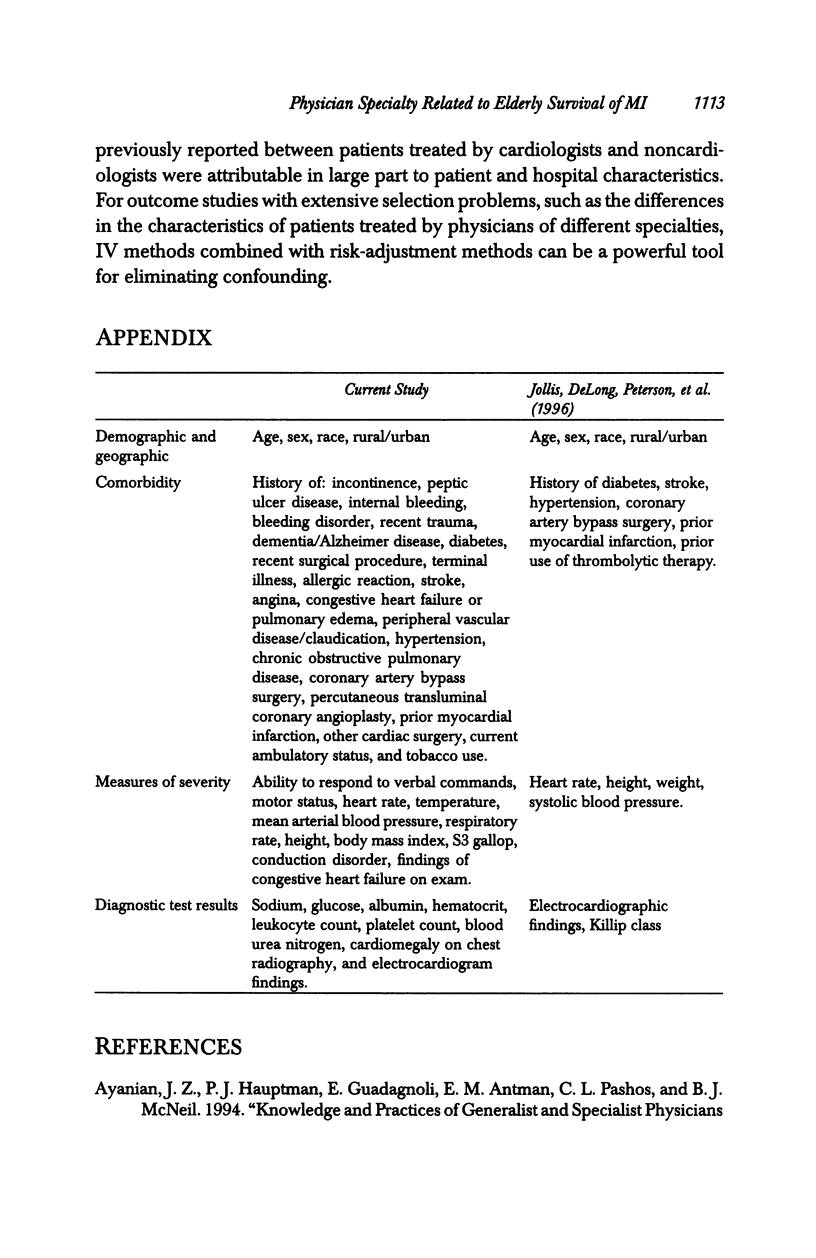
OBJECTIVE: To determine the effect of treatment by a cardiologist on mortality of elderly patients with acute myocardial infarction (AMI, heart attack), accounting for both measured confounding using risk-adjustment techniques and residual unmeasured confounding with instrumental variables (IV) methods. DATA SOURCES/STUDY SETTING: Medical chart data and longitudinal administrative hospital records and death records were obtained for 161,558 patients aged > or =65 admitted to a nonfederal acute care hospital with AMI from April 1994 to July 1995. Our principal measure of significant cardiologist treatment was whether a patient was admitted by a cardiologist. We use supplemental data to explore whether our analysis would differ substantially using alternative definitions of significant cardiologist treatment. STUDY DESIGN: This retrospective cohort study compared results using least squares (LS) multivariate regression with results from IV methods that accounted for additional unmeasured patient characteristics. Primary outcomes were 30-day and one-year mortality, and secondary outcomes included treatment with medications and revascularization procedures. DATA COLLECTION/EXTRACTION METHODS: Medical charts for the initial hospital stay of each AMI patient underwent a comprehensive abstraction, including dates of hospitalization, admitting physician, demographic characteristics, comorbid conditions, severity of clinical presentation, electrocardiographic and other diagnostic test results, contraindications to therapy, and treatments before and after AMI. PRINCIPAL FINDINGS: Patients admitted by cardiologists had fewer comorbid conditions and less severe AMIs. These patients had a 10 percent (95 percent CI: 9.5-10.8 percent) lower absolute mortality rate at one year. After multivariate adjustment with LS regression, the adjusted mortality difference was 2 percent (95 percent CI: 1.4-2.6 percent). Using IV methods to provide additional adjustment for unmeasured differences in risk, we found an even smaller, statistically insignificant association between physician specialty and one-year mortality, relative risk (RR) 0.96 (0.88-1.04). Patients admitted by a cardiologist were also significantly more likely to have a cardiologist consultation within the first day of admission and during the initial hospital stay, and also had a significantly larger share of their physician bills for inpatient treatment from cardiologists. IV analysis of treatments showed that patients treated by cardiologists were more likely to undergo revascularization procedures and to receive thrombolytic therapy, aspirin, and calcium channel-blockers, but less likely to receive beta-blockers. CONCLUSIONS: In a large population of elderly patients with AMI, we found significant treatment differences but no significant incremental mortality benefit associated with treatment by cardiologists.
Full text
PDF





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ayanian J. Z., Guadagnoli E., McNeil B. J., Cleary P. D. Treatment and outcomes of acute myocardial infarction among patients of cardiologists and generalist physicians. Arch Intern Med. 1997 Dec 8;157(22):2570–2576. [PubMed] [Google Scholar]
- Barefoot J. C., Helms M. J., Mark D. B., Blumenthal J. A., Califf R. M., Haney T. L., O'Connor C. M., Siegler I. C., Williams R. B. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol. 1996 Sep 15;78(6):613–617. doi: 10.1016/s0002-9149(96)00380-3. [DOI] [PubMed] [Google Scholar]
- Borowsky S. J., Kravitz R. L., Laouri M., Leake B., Partridge J., Kaushik V., Haywood L. J., Brook R. H. Effect of physician specialty on use of necessary coronary angiography. J Am Coll Cardiol. 1995 Nov 15;26(6):1484–1491. doi: 10.1016/0735-1097(95)00337-1. [DOI] [PubMed] [Google Scholar]
- Brand D. A., Newcomer L. N., Freiburger A., Tian H. Cardiologists' practices compared with practice guidelines: use of beta-blockade after acute myocardial infarction. J Am Coll Cardiol. 1995 Nov 15;26(6):1432–1436. doi: 10.1016/0735-1097(95)00362-2. [DOI] [PubMed] [Google Scholar]
- Donohoe M. T. Comparing generalist and specialty care: discrepancies, deficiencies, and excesses. Arch Intern Med. 1998 Aug 10;158(15):1596–1608. doi: 10.1001/archinte.158.15.1596. [DOI] [PubMed] [Google Scholar]
- Ellerbeck E. F., Jencks S. F., Radford M. J., Kresowik T. F., Craig A. S., Gold J. A., Krumholz H. M., Vogel R. A. Quality of care for Medicare patients with acute myocardial infarction. A four-state pilot study from the Cooperative Cardiovascular Project. JAMA. 1995 May 17;273(19):1509–1514. [PubMed] [Google Scholar]
- Fitzmaurice G. M., Laird N. M. Regression models for mixed discrete and continuous responses with potentially missing values. Biometrics. 1997 Mar;53(1):110–122. [PubMed] [Google Scholar]
- Frances C. D., Go A. S., Dauterman K. W., Deosaransingh K., Jung D. L., Gettner S., Newman J. M., Massie B. M., Browner W. S. Outcome following acute myocardial infarction: are differences among physician specialties the result of quality of care or case mix? Arch Intern Med. 1999 Jul 12;159(13):1429–1436. doi: 10.1001/archinte.159.13.1429. [DOI] [PubMed] [Google Scholar]
- Gibbons R. J., Holmes D. R., Reeder G. S., Bailey K. R., Hopfenspirger M. R., Gersh B. J. Immediate angioplasty compared with the administration of a thrombolytic agent followed by conservative treatment for myocardial infarction. The Mayo Coronary Care Unit and Catheterization Laboratory Groups. N Engl J Med. 1993 Mar 11;328(10):685–691. doi: 10.1056/NEJM199303113281003. [DOI] [PubMed] [Google Scholar]
- Grines C. L., Browne K. F., Marco J., Rothbaum D., Stone G. W., O'Keefe J., Overlie P., Donohue B., Chelliah N., Timmis G. C. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med. 1993 Mar 11;328(10):673–679. doi: 10.1056/NEJM199303113281001. [DOI] [PubMed] [Google Scholar]
- Gustafsson F., Køber L., Torp-Pedersen C., Hildebrandt P., Ottesen M. M., Sonne B., Carlsen J. Long-term prognosis after acute myocardial infarction in patients with a history of arterial hypertension. TRACE study group. Eur Heart J. 1998 Apr;19(4):588–594. doi: 10.1053/euhj.1997.0822. [DOI] [PubMed] [Google Scholar]
- Jollis J. G., DeLong E. R., Peterson E. D., Muhlbaier L. H., Fortin D. F., Califf R. M., Mark D. B. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med. 1996 Dec 19;335(25):1880–1887. doi: 10.1056/NEJM199612193352505. [DOI] [PubMed] [Google Scholar]
- Krumholz H. M., Radford M. J., Ellerbeck E. F., Hennen J., Meehan T. P., Petrillo M., Wang Y., Kresowik T. F., Jencks S. F. Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries. Patterns of use and outcomes. Circulation. 1995 Nov 15;92(10):2841–2847. doi: 10.1161/01.cir.92.10.2841. [DOI] [PubMed] [Google Scholar]
- Krumholz H. M., Radford M. J., Wang Y., Chen J., Heiat A., Marciniak T. A. National use and effectiveness of beta-blockers for the treatment of elderly patients after acute myocardial infarction: National Cooperative Cardiovascular Project. JAMA. 1998 Aug 19;280(7):623–629. doi: 10.1001/jama.280.7.623. [DOI] [PubMed] [Google Scholar]
- Latini R., Maggioni A. P., Flather M., Sleight P., Tognoni G. ACE inhibitor use in patients with myocardial infarction. Summary of evidence from clinical trials. Circulation. 1995 Nov 15;92(10):3132–3137. doi: 10.1161/01.cir.92.10.3132. [DOI] [PubMed] [Google Scholar]
- Marciniak T. A., Ellerbeck E. F., Radford M. J., Kresowik T. F., Gold J. A., Krumholz H. M., Kiefe C. I., Allman R. M., Vogel R. A., Jencks S. F. Improving the quality of care for Medicare patients with acute myocardial infarction: results from the Cooperative Cardiovascular Project. JAMA. 1998 May 6;279(17):1351–1357. doi: 10.1001/jama.279.17.1351. [DOI] [PubMed] [Google Scholar]
- McClellan M., McNeil B. J., Newhouse J. P. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. 1994 Sep 21;272(11):859–866. [PubMed] [Google Scholar]
- Meng X. L. The EM algorithm and medical studies: a historical link. Stat Methods Med Res. 1997 Mar;6(1):3–23. doi: 10.1177/096228029700600102. [DOI] [PubMed] [Google Scholar]
- Michels K. B., Yusuf S. Does PTCA in acute myocardial infarction affect mortality and reinfarction rates? A quantitative overview (meta-analysis) of the randomized clinical trials. Circulation. 1995 Jan 15;91(2):476–485. doi: 10.1161/01.cir.91.2.476. [DOI] [PubMed] [Google Scholar]
- Miettinen H., Lehto S., Salomaa V., Mähönen M., Niemelä M., Haffner S. M., Pyörälä K., Tuomilehto J. Impact of diabetes on mortality after the first myocardial infarction. The FINMONICA Myocardial Infarction Register Study Group. Diabetes Care. 1998 Jan;21(1):69–75. doi: 10.2337/diacare.21.1.69. [DOI] [PubMed] [Google Scholar]
- Newhouse J. P., McClellan M. Econometrics in outcomes research: the use of instrumental variables. Annu Rev Public Health. 1998;19:17–34. doi: 10.1146/annurev.publhealth.19.1.17. [DOI] [PubMed] [Google Scholar]
- Normand S. T., Glickman M. E., Sharma R. G., McNeil B. J. Using admission characteristics to predict short-term mortality from myocardial infarction in elderly patients. Results from the Cooperative Cardiovascular Project. JAMA. 1996 May 1;275(17):1322–1328. [PubMed] [Google Scholar]
- Pfeffer M. A., Braunwald E., Moyé L. A., Basta L., Brown E. J., Jr, Cuddy T. E., Davis B. R., Geltman E. M., Goldman S., Flaker G. C. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med. 1992 Sep 3;327(10):669–677. doi: 10.1056/NEJM199209033271001. [DOI] [PubMed] [Google Scholar]
- Rubin D. B. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997 Oct 15;127(8 Pt 2):757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Ryan T. J., Anderson J. L., Antman E. M., Braniff B. A., Brooks N. H., Califf R. M., Hillis L. D., Hiratzka L. F., Rapaport E., Riegel B. J. ACC/AHA guidelines for the management of patients with acute myocardial infarction: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation. 1996 Nov 1;94(9):2341–2350. doi: 10.1161/01.cir.94.9.2341. [DOI] [PubMed] [Google Scholar]
- Vaccarino V., Krumholz H. M., Berkman L. F., Horwitz R. I. Sex differences in mortality after myocardial infarction. Is there evidence for an increased risk for women? Circulation. 1995 Mar 15;91(6):1861–1871. doi: 10.1161/01.cir.91.6.1861. [DOI] [PubMed] [Google Scholar]


