Abstract
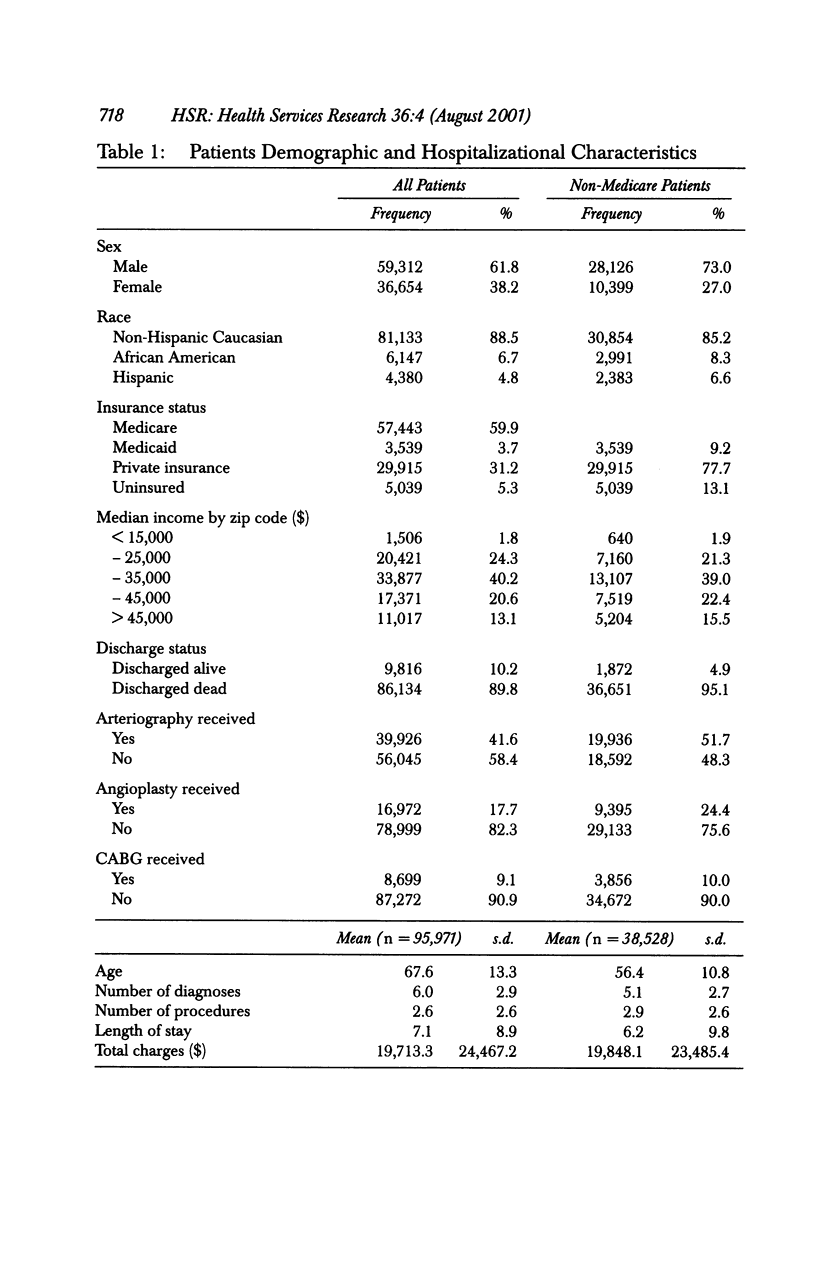
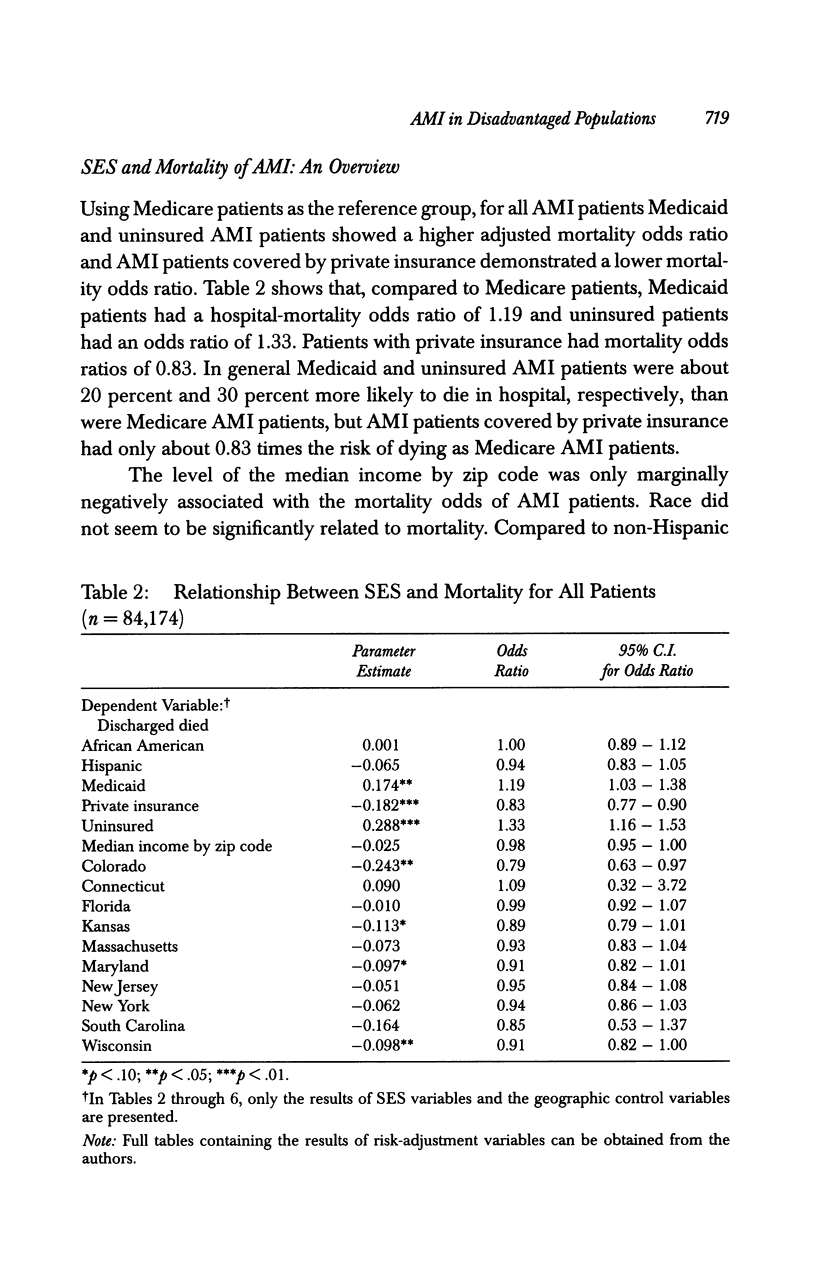
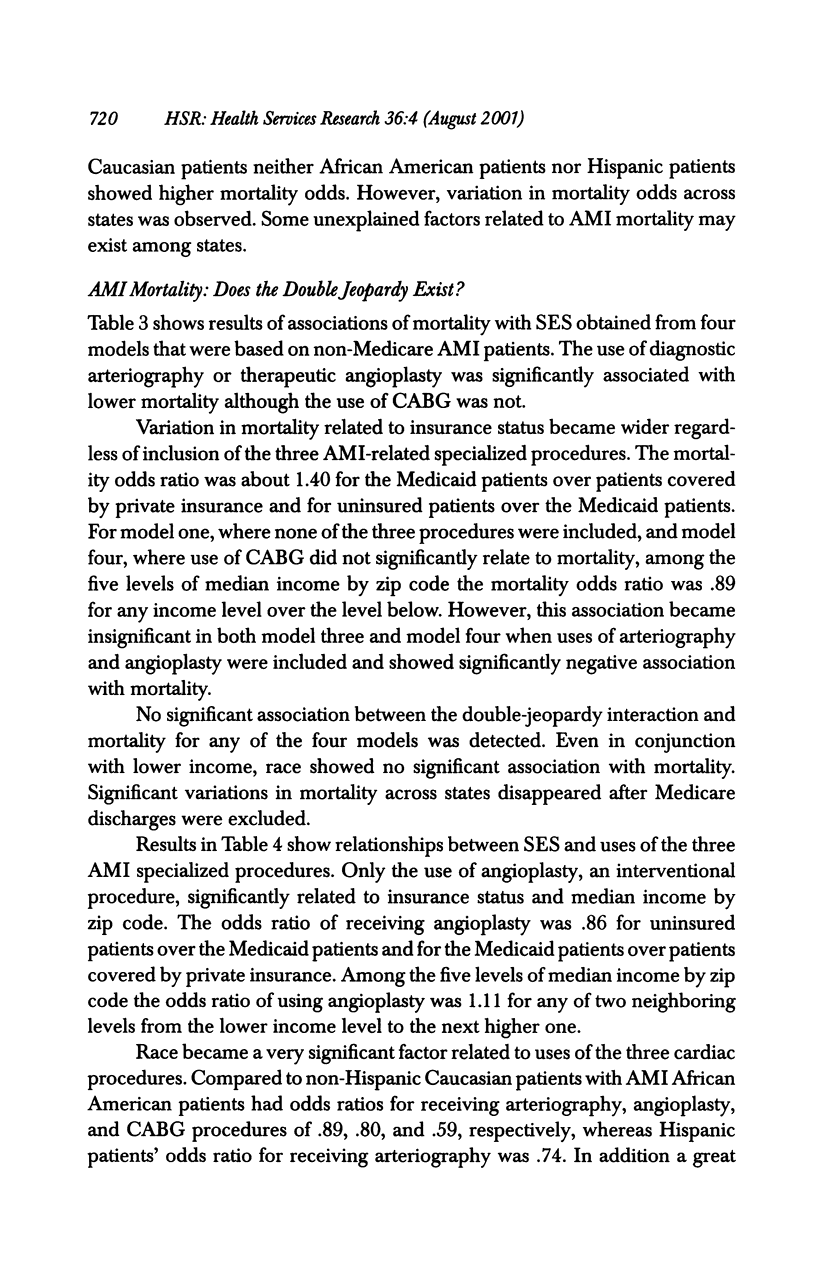
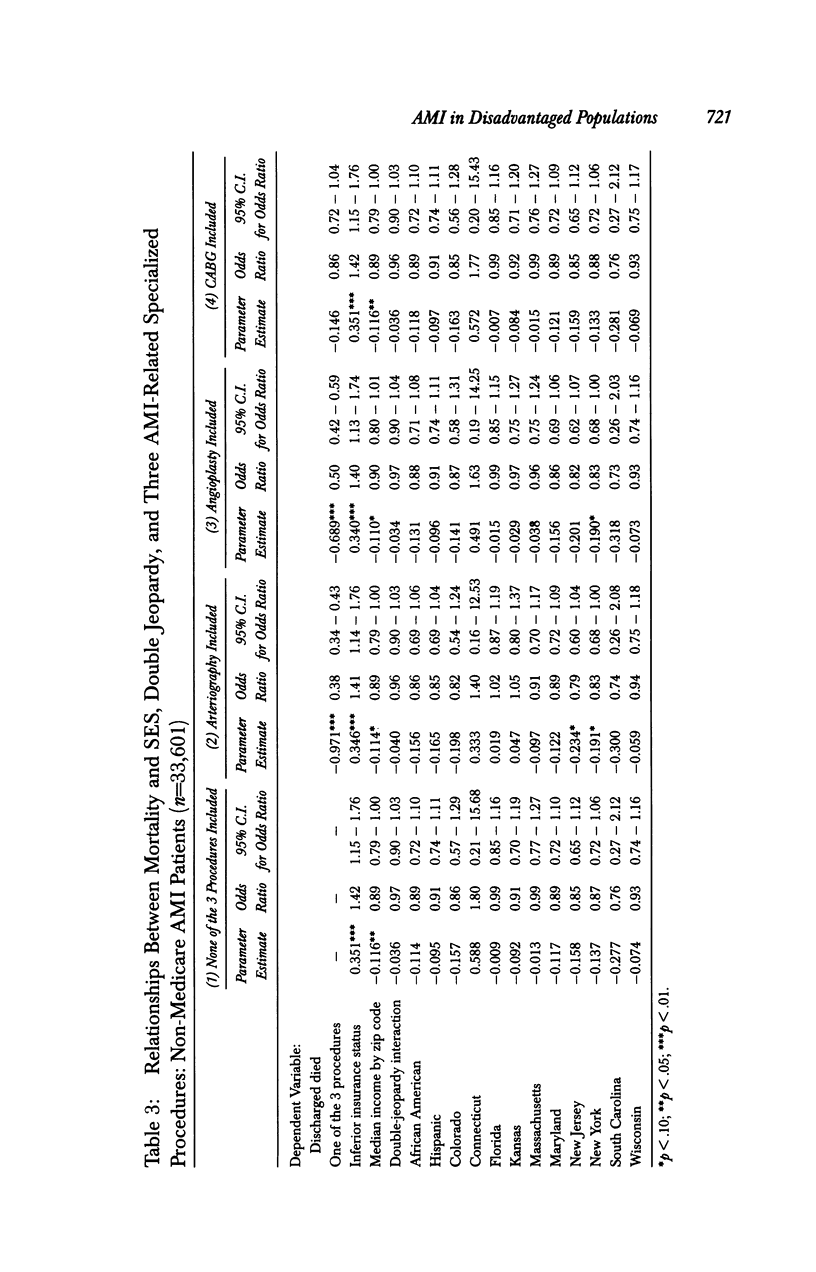
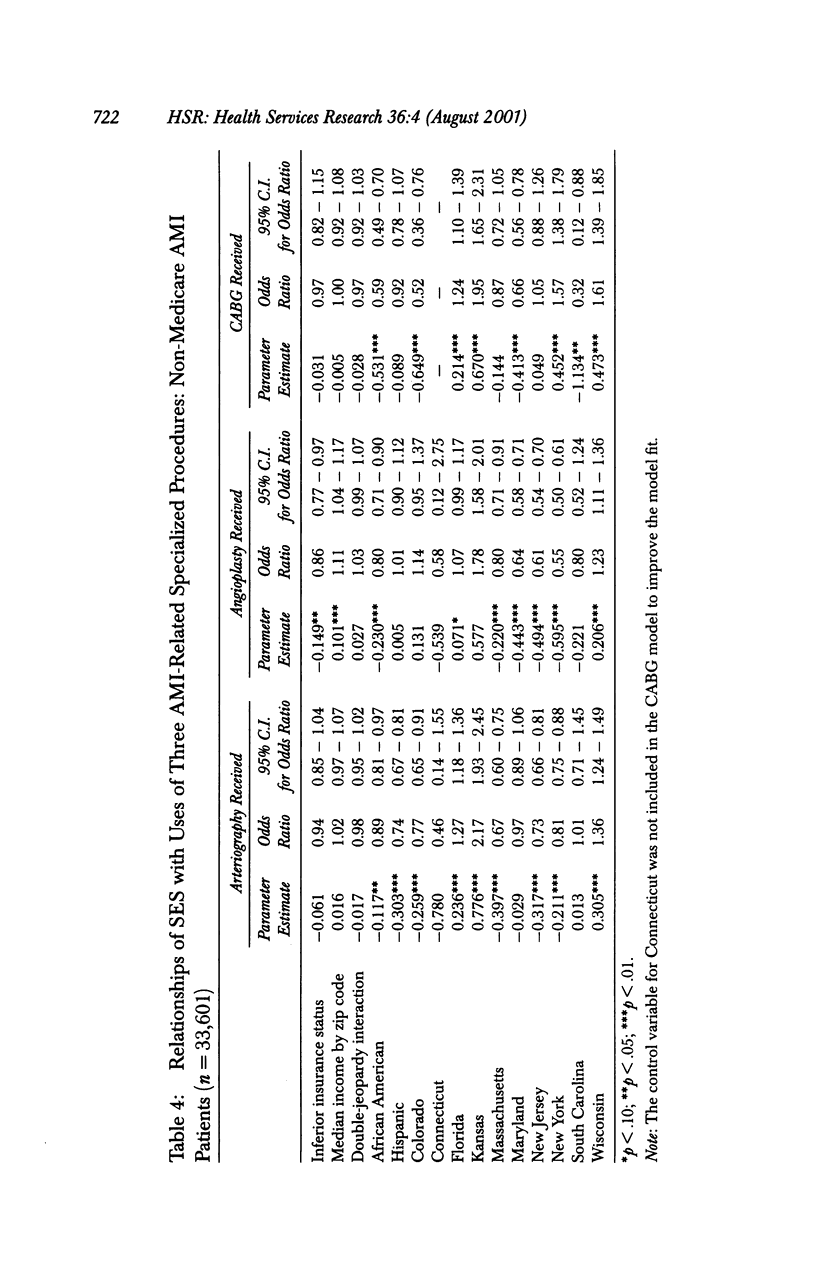
OBJECTIVE: To examine the relationship of patients' socioeconomic status (SES) as measured by race, health insurance status, and median income by zip code to in-hospital mortality of acute myocardial infarction (AMI), paying special attention to patients with multiple unfavorable socioeconomic risk factors. DATA SOURCES/STUDY SETTING: The data set was abstracted from patient-level hospital discharges in the Nationwide Inpatient Sample, Release 3, 1994. A total of 95,971 AMI discharges in 11 states were extracted. STUDY DESIGN: The risk adjustment methodology was adapted from the California Hospital Outcomes Project. Risk factors included demographic and clinical characteristics. Patients in double jeopardy had inferior insurance status and lived in poorer neighborhoods. PRINCIPAL FINDINGS: Compared with patients with health care coverage under Medicare and private insurance uninsured AMI patients had the highest risk-adjusted mortality odds and Medicaid AMI patients had the second highest odds. Probably because of the modest association of median income by zip code areas with mortality odds, the double jeopardy phenomenon was not observed. However, compared to patients who had two favorable SES attributes, patients who carried two unfavorable SES attributes had much higher mortality risk, more comorbidities, longer length of stay, and higher total hospital charges, while they received fewer AMI specialized procedures. Race did not seem to be a significant factor after adjustment for other SES attributes. CONCLUSIONS: SES is significantly related to the mortality of AMI patients. The disadvantaged patients receive fewer specialized procedures, possibly because of their higher levels of severity and financial barriers. The variation in mortality between patients who had favorable and unfavorable SES becomes wider when multiple socioeconomic risks are borne by the latter.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bearden D., Allman R., McDonald R., Miller S., Pressel S., Petrovitch H. Age, race, and gender variation in the utilization of coronary artery bypass surgery and angioplasty in SHEP. SHEP Cooperative Research Group. Systolic Hypertension in the Elderly Program. J Am Geriatr Soc. 1994 Nov;42(11):1143–1149. doi: 10.1111/j.1532-5415.1994.tb06979.x. [DOI] [PubMed] [Google Scholar]
- Belgrave L. L., Wykle M. L., Choi J. M. Health, double jeopardy, and culture: the use of institutionalization by African-Americans. Gerontologist. 1993 Jun;33(3):379–385. doi: 10.1093/geront/33.3.379. [DOI] [PubMed] [Google Scholar]
- Berger A. K., Schulman K. A., Gersh B. J., Pirzada S., Breall J. A., Johnson A. E., Every N. R. Primary coronary angioplasty vs thrombolysis for the management of acute myocardial infarction in elderly patients. JAMA. 1999 Jul 28;282(4):341–348. doi: 10.1001/jama.282.4.341. [DOI] [PubMed] [Google Scholar]
- Berk M. L., Schur C. L. Access to care: how much difference does Medicaid make? Health Aff (Millwood) 1998 May-Jun;17(3):169–180. doi: 10.1377/hlthaff.17.3.169. [DOI] [PubMed] [Google Scholar]
- Bloomberg L., Meyers J., Braverman M. T. The importance of social interaction: a new perspective on social epidemiology, social risk factors, and health. Health Educ Q. 1994 Winter;21(4):447-63, discussion 465-9. doi: 10.1177/109019819402100407. [DOI] [PubMed] [Google Scholar]
- Claudio L., Tulton L., Doucette J., Landrigan P. J. Socioeconomic factors and asthma hospitalization rates in New York City. J Asthma. 1999 Jun;36(4):343–350. doi: 10.3109/02770909909068227. [DOI] [PubMed] [Google Scholar]
- Crawford S. L., McGraw S. A., Smith K. W., McKinlay J. B., Pierson J. E. Do blacks and whites differ in their use of health care for symptoms of coronary heart disease? Am J Public Health. 1994 Jun;84(6):957–964. doi: 10.2105/ajph.84.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale W., Vijayakumar S., Lawlor E. F., Merrell K. Prostate cancer, race, and socioeconomic status: inadequate adjustment for social factors in assessing racial differences. Prostate. 1996 Nov;29(5):271–281. doi: 10.1002/(SICI)1097-0045(199611)29:5<271::AID-PROS1>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Ebell M. H., Smith M., Kruse J. A., Drader-Wilcox J., Novak J. Effect of race on survival following in-hospital cardiopulmonary resuscitation. J Fam Pract. 1995 Jun;40(6):571–577. [PubMed] [Google Scholar]
- Ell K., Haywood L. J., Sobel E., deGuzman M., Blumfield D., Ning J. P. Acute chest pain in African Americans: factors in the delay in seeking emergency care. Am J Public Health. 1994 Jun;84(6):965–970. doi: 10.2105/ajph.84.6.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold M. Beyond coverage and supply: measuring access to healthcare in today's market. Health Serv Res. 1998 Aug;33(3 Pt 2):625–684. [PMC free article] [PubMed] [Google Scholar]
- Haywood L. J., Ell K., deGuman M., Norris S., Blumfield D., Sobel E. Chest pain admissions: characteristics of black, Latino, and white patients in low- and mid-socioeconomic strata. J Natl Med Assoc. 1993 Oct;85(10):749–757. [PMC free article] [PubMed] [Google Scholar]
- Jaglal S. B., Goel V. Social inequity in risk of coronary artery disease in Ontario. Can J Cardiol. 1994 May;10(4):439–443. [PubMed] [Google Scholar]
- Jones C. P., LaVeist T. A., Lillie-Blanton M. "Race" in the epidemiologic literature: an examination of the American Journal of Epidemiology, 1921-1990. Am J Epidemiol. 1991 Nov 15;134(10):1079–1084. doi: 10.1093/oxfordjournals.aje.a116011. [DOI] [PubMed] [Google Scholar]
- Kahn K. L., Pearson M. L., Harrison E. R., Desmond K. A., Rogers W. H., Rubenstein L. V., Brook R. H., Keeler E. B. Health care for black and poor hospitalized Medicare patients. JAMA. 1994 Apr 20;271(15):1169–1174. [PubMed] [Google Scholar]
- Kravitz R. L. Ethnic differences in use of cardiovascular procedures: new insights and new challenges. Ann Intern Med. 1999 Feb 2;130(3):231–233. doi: 10.7326/0003-4819-130-3-199902020-00028. [DOI] [PubMed] [Google Scholar]
- Laouri M., Kravitz R. L., French W. J., Yang I., Milliken J. C., Hilborne L., Wachsner R., Brook R. H. Underuse of coronary revascularization procedures: application of a clinical method. J Am Coll Cardiol. 1997 Apr;29(5):891–897. doi: 10.1016/s0735-1097(96)00434-2. [DOI] [PubMed] [Google Scholar]
- Lillie-Blanton M., Parsons P. E., Gayle H., Dievler A. Racial differences in health: not just black and white, but shades of gray. Annu Rev Public Health. 1996;17:411–448. doi: 10.1146/annurev.pu.17.050196.002211. [DOI] [PubMed] [Google Scholar]
- Moore K. Socioeconomic status as quarantine: unfortunate consequences of the inability to afford health care. Outcomes Manag Nurs Pract. 1997 Oct-Dec;1(1):41–48. [PubMed] [Google Scholar]
- Mueller K. J., Patil K., Boilesen E. The role of uninsurance and race in healthcare utilization by rural minorities. Health Serv Res. 1998 Aug;33(3 Pt 1):597–610. [PMC free article] [PubMed] [Google Scholar]
- Norris S. L., deGuzman M., Sobel E., Brooks S., Haywood L. J. Risk factors and mortality among black, Caucasian, and Latina women with acute myocardial infarction. Am Heart J. 1993 Dec;126(6):1312–1319. doi: 10.1016/0002-8703(93)90528-h. [DOI] [PubMed] [Google Scholar]
- Pappas G., Hadden W. C., Kozak L. J., Fisher G. F. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997 May;87(5):811–816. doi: 10.2105/ajph.87.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkleby M. A., Kraemer H. C., Ahn D. K., Varady A. N. Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the Third National Health and Nutrition Examination Survey, 1988-1994. JAMA. 1998 Jul 22;280(4):356–362. doi: 10.1001/jama.280.4.356. [DOI] [PubMed] [Google Scholar]
- Young G. J., Cohen B. B. Inequities in hospital care, the Massachusetts experience. Inquiry. 1991 Fall;28(3):255–262. [PubMed] [Google Scholar]
- Zhang J., Yu K. F. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998 Nov 18;280(19):1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]


