Abstract
Evidence linking traffic noise to insulin resistance and diabetes is limited and unanswered questions remain regarding the potential effect modification by neighborhood socioeconomic status (nSES). We aimed to assess socioeconomic inequalities in noise exposure, whether road and aircraft noise exposures were associated with insulin resistance or diabetes, and whether nSES modified these relationships. Among the Community of Mine Study in San Diego County, road and aircraft noise exposure at enrollment was calculated based on the static (participant’s administrative boundary, and circular buffer around participant homes), and dynamic (mobility data by global positioning system, GPS) spatio-temporal aggregation methods. Associations of noise with insulin resistance (HOMA-IR) or type 2 diabetes (T2DM) were quantified using generalized estimating equation models adjusted for sex, age, ethnicity, individual income, and air pollution (nitrogen dioxide) exposure. Additive interaction between noise and nSES was assessed. Among 573 participants (mean age 58.7 y), participants living in low nSES were exposed to higher levels of aircraft and road noise using noise level at the census tract, circular buffer, or Kernel Density Estimation (KDE) of GPS data. Participants exposed to road noise greater or equal to the median (53 dB(A)) at the census tract and living in low nSES had an increased level of insulin resistance (β = 0.15, 95%CI: −0.04, 0.34) and higher odds of T2DM (Odds Ratio = 2.34, 95%CI: 1.12, 4.90). A positive additive interaction was found as participants living in low nSES had higher odds of T2DM. The impact of noise exposure on insulin resistance and T2DM differs substantially by nSES. Public health benefits of reducing exposure to road or aircraft noise would be larger in individuals living in low nSES.
Keywords: Transportation noise, Glucose regulation, Cardiometabolic health, Environmental justice, Activity space, Inequalities, Health disparities, Social determinants of health
1. Introduction
Noise pollution is increasingly recognized as an important environmental determinant of population health (Hammer et al., 2014; Münzel et al., 2014). Environmental noise, including transportation noise (noise from roads, railways, and aircraft), not only leads to hearing loss, auditory fatigue, or sleep disturbance, but also contributes to a higher incidence of cardiovascular diseases (CVDs) such as ischemic heart disease, myocardial infarction, or stroke (Münzel et al., 2014). In October 2018, the World Health Organization (WHO) published the Environmental Noise Guidelines for the European Region, and concluded high-quality evidence exists for the association between road traffic noise and ischemic heart disease (Kempen et al., 2018). In Europe, long-term exposure to environmental noise is estimated to cause 12,000 premature deaths and 48,000 new cases of ischemic heart disease per year (European Environment Agency, 2020). Recent studies indicate that noise exposure may also contribute to hypertension (Sivakumaran et al., 2022; Dimakopoulou et al., 2017), hyperglycemia (Li et al., 2021; Dreger et al., 2019; Taylor, 2014), and metabolic syndrome (Huang et al., 2020; Yu et al., 2020; Li et al., 2021). Despite consensus of environmental noise as an important cardiovascular risk factor, there is a need for more research on these relationships across diverse populations with further investigation into the unequal burden of noise regarding social groups (Münzel et al., 2014; Dreger et al., 2019).
Exposure to noise and related health impacts may constitute an important environmental justice issue where noise could be classified as a neighborhood level social determinant of health. Some communities could be more exposed and more vulnerable than others. Individuals with low socioeconomic status (SES) have access to lower quality housing and more often live near environmental hazards such as roads with high traffic density (Taylor, 2014). In the European region, it has been observed that social deprivation is associated with higher environmental noise exposure, however studies are scarce and methodologically inconsistent (Dreger et al., 2019). In the US, social inequalities in noise exposures have been identified; two studies found that noise levels are higher for census block groups with higher percentages of socially vulnerable populations (Casey et al., 2017; Simon et al., 2022). Better exposure assessment methods are needed to characterize the double burden of noise exposure and low SES in the US and how it may contribute to health inequities. In this context, we will use three ways to assess noise exposure: two static approaches, based on the participant’s census-tract and circular buffer around participant’s home, and one dynamic approach considering a participant’s activity space defined by their daily mobility. Dynamic exposure assessment can greatly improve the accuracy of exposure assessment by incorporating where an individual goes and how much time they spend there (Jankowska et al., 2021).
In 2022, in the US, approximately 37.3 million people had diabetes (11.3% of the US population), and approximately 90–95% of them had type 2 diabetes (T2DM) (National Diabetes Statistics Report | Diabetes | CDC [Internet], 2022). As the prevalence of diabetes continues to rise, associated CVDs can also be expected to rise through traditional cardiovascular risk factors (including obesity, hypertension, and dyslipidemia) and direct effects of diabetes on CVDs (Leon and Maddox, 2015). A wide variety of environmental exposures have been linked to TD2M, such as walkability, green space, air pollution, or noise (Dendup et al., 2018). The quality of evidence on the adverse effects of noise exposure on T2DM has recently increased (Münzel et al., 2021; Zare Sakhvidi et al., 2018; Vienneau et al., 2019). Since the 2018 WHO evaluation, seven new prospective studies conducted in Europe and Canada consistently found that road traffic noise increased the risk of T2DM (Clark et al., 2017; Eze et al., 2017a; Ohlwein et al., 2019; Jørgensen et al., 2019; Shin et al., 2020; Thacher et al., 2021; Klompmaker et al., 2019). To our knowledge, only one epidemiological study evaluated the association between transportation noise and insulin resistance, an important underlying condition of T2DM, and found no adverse effects of road noise exposure (Pedersen et al., 2019). Evidence linking transportation noise to insulin resistance or T2DM remains scarce, and no prior studies assessed diverse US populations or used dynamic assessment (using GPS data to consider daily mobility).
Using data from the Community of Mine Study, a study involving an ethnically diverse population in San Diego, CA, we aim to evaluate: (i) whether socioeconomic inequalities in transportation noise exposure exist, according to three ways of assessing noise exposure (static, using census tract and buffer; and dynamic, using GPS data), (ii) whether static or dynamic noise exposure is associated with insulin resistance or T2DM, and (iii) whether neighborhood socioeconomic status (nSES) is an effect modifier in the relationship between transportation noise exposure and insulin resistance or T2DM.
2. Material and methods
2.1. Study population
The Community of Mine Study was an observational study conducted from 2014 to 2017 in San Diego County, California. The full protocol and inclusion criteria have been described elsewhere (Jankowska et al., 2019). Briefly, this study includes 602 adults aged 35–80 years old living for at least 6 months in study census block groups, selected to maximize environmental variation. The main objective of the Community of Mine Study is to advance methods of cancer risk exposure assessment by measuring participant access and exposure to various environments by integrating Geographical Information System (GIS) data. Participants wore GPS and accelerometer sensors for up to two weeks. They attended a clinical visit (after 1 week of sensor wear and before the 2nd week of sensor wear) where blood pressure, height, weight, and hip/waist circumference were recorded, and blood and urine samples were collected. Fasting plasma insulin and fasting plasma glucose were measured. Demographic characteristics (e.g., age, sex, race/ethnicity) were collected via self-report survey. Study ethics approval was obtained from the University of California San Diego Institutional Review Board (protocol #140510). Signed informed consent was obtained from all participants.
2.2. Outcomes
We focused on two main outcomes: insulin resistance and T2DM. Insulin resistance was assessed using the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) (Matthews et al., 1985). The HOMA-IR index was calculated according to the formula: fasting plasma insulin (mlU/L) × fasting plasma glucose (mg/dL)/22.5. T2DM was defined by a fasting blood glucose level greater than or equal to 126 mg/dL. In supplementary analysis, we defined T2DM by the use of antidiabetic treatment or by self-reported diabetes.
2.3. Noise exposure
Annual average noise levels from aircraft and road were estimated for the year 2016. The national transportation noise inventory was developed using a 24-hr equivalent sound level (Leq, denoted by LAeq) noise metric. The results are A-weighted noise levels that represent the approximate average noise energy due to transportation noise sources over the 24-h period at the defined receptors. The U.S. Department of Transportation conducted the noise computations by implementing the Aircraft Environmental Design Tool version 2b (AEDT; version 2b) developed by Federal Aircraft Administration (FAA) and the acoustic algorithms from the Traffic Noise Model 2.5 (TNM) proposed by the Federal Highway Administration (FHWA) (Volpe National Transportation Systems Center, 2020). Airports with an average of 1 or more jet departures per day are included in the analysis resulting in the modeling of operations at 685 airports (airports with exclusively military operations were excluded) across the US (6 airports in study area). Average Annual Daily Traffic (AADT) values, obtained from FHWA’s Highway Performance Monitoring System, are used in conjunction with vehicle types and speed to compute road noise using TNM’s acoustical algorithms. The transportation noise map (a raster dataset) was generated utilizing traffic data, and aircraft flight operation data along with simplifying assumptions–namely, atmospheric absorption for aircraft noise, non-homogenous atmospheric effects in road traffic noise modeling and TNM’s default temperature and humidity levels (68 degrees F, 50% relative humidity), acoustically soft ground, average pavement material and texture of the road, and distribution of average annual daily traffic data across 24h. The aircraft and road noise rasters are shown in Figure S1 and more information on noise modeling is available in supplementary data.
2.4. Static and dynamic noise exposures
Three different approaches were used to assess exposure to aircraft and road traffic noise: two static approaches and one dynamic approach considering activity space (Fig. 1).
Fig. 1.
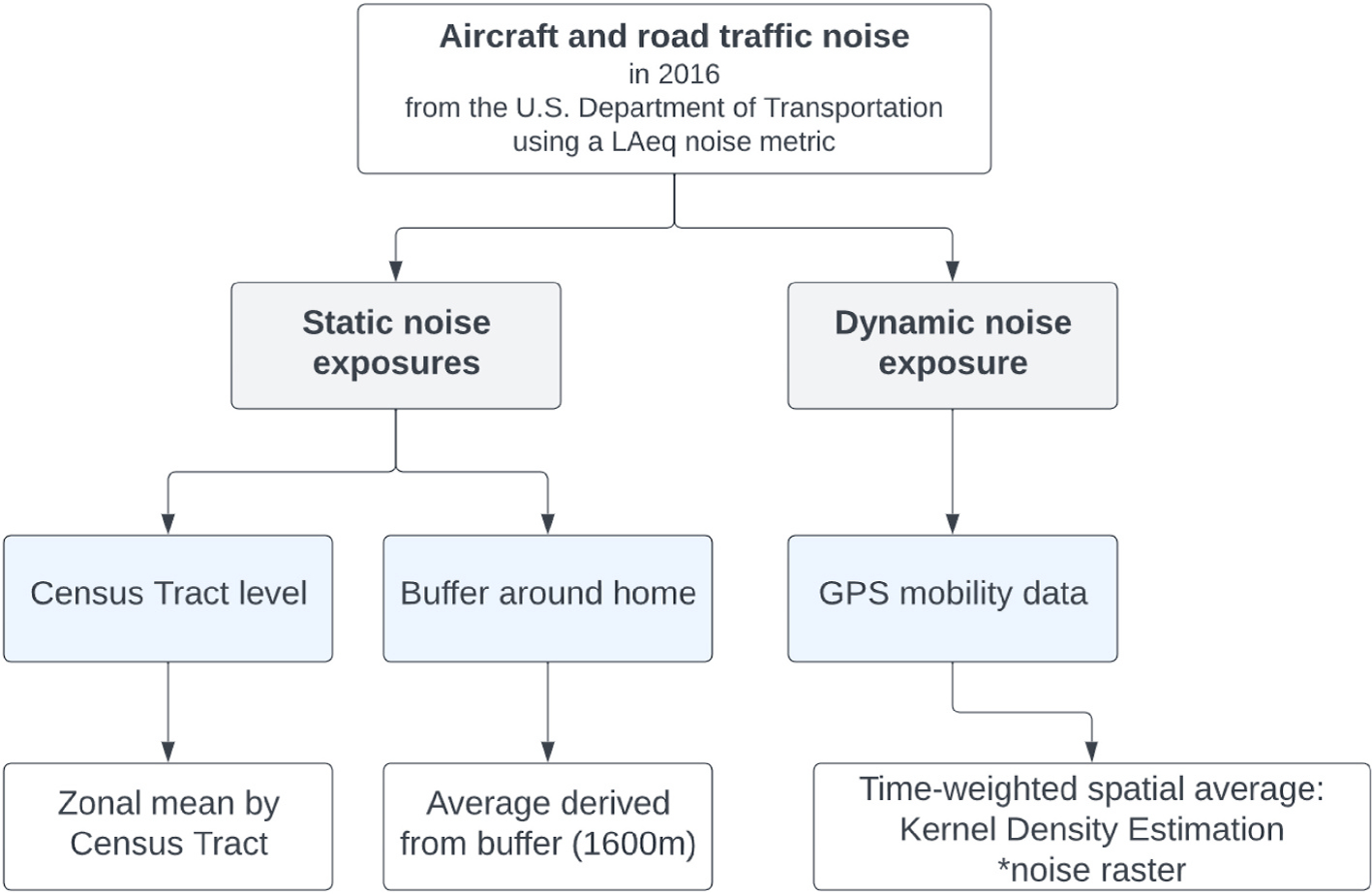
Three ways to assess exposure to aircraft and road traffic noise.
2.4.1. Static noise exposure
Static measures of noise exposure were assessed in two ways. First, we used an administrative boundary method at the census tract aggregation level, a unit of US census geography based on population (about 4000 people). We calculated the zonal mean noise exposure by census tract. These exposures were assigned to participant’s census tract based on their home address at enrollment. These analyses were performed using the zonal statistics function in ArcGIS Pro (version 2.8.0). Second, we calculated the average noise exposure value using a circular buffer with a radius of 1600m around the participant’s home (Figure S2 a. and b.). For both methods (average at census tract or using a circular buffer), we used static road noise as a continuous variable and a dichotomized variable (using the median of 53.4 for census tract and 54.8 dB(A) for buffer in this sample, in San Diego County). We used static aircraft noise as a dichotomized variable. We classified participants with static aircraft noise in their census tract or buffer around their home as exposed to aircraft noise, vs. participants not exposed (without aircraft noise).
2.4.2. Dynamic noise exposure
To calculate dynamic noise exposure, we used GPS data. Participants were asked to wear a GT3X + ActiGraph accelerometer (ActiGraph, LLC; Pensacola, FL) and Qstarz GPS device (Qstarz International Co. Ltd, Taipei, Taiwan) on a belt around the waist for 14 days. Data was cleaned (GPS noise points with speed >130 km/h and delta elevation >1000m between points were imputed to bookend non-noise points) and processed through the Personal Activity and Location Measurement System (PALMS) and aggregated to the minute level (Carlson et al., 2015). Missing GPS data was imputed per a previously validated algorithm (Meseck et al., 2016). Only valid wear days were included, defined as having at least 600 min of matched wear-time accelerometer data (>90 min of consecutive zeros with a 2-min threshold defined as non-wear) and GPS data (after imputation). Participants wore devices for an average (minimum − maximum) of 11.8 valid days. Most participants wore GPS devices in 2016 or 2017 (61%), and for participants wearing GPS devices in 2015 (35%) or 2014 (4%), we assumed that the 2016 noise exposure was consistent with the previous two years.
To capture the spatio-temporality of exposure, we used one of the most common time-weighted spatial averaging approaches, Kernel Density Estimation (KDE), as detailed previously (Jankowska et al., 2023). All valid-wear GPS points for the entire participant’s wear time were used to create a time-weighted activity space using the KDE model (Figure S2 c. and d.). To account for variation in amount of time participants wore devices, we normalized the time-weighted density measure values for each participant on a scale of 0–1 where the greatest amount of time spent by a participant in a location was equal to 1, and the least equal to 0 (Jankowska et al., 2021). The time-weighted activity space was then multiplied by noise layer. The average noise across the entire time-weighted activity space was calculated to derive a total exposure measure that accounts for locations visited and the time spent in all locations (Figure S2 e. and f.). These dynamic measurements of noise exposure are unitless and cannot be interpreted in dB.
2.5. Neighborhood socioeconomic status - nSES
Neighborhood socioeconomic status was evaluated by the median household income at the census tract level and assigned to participants based on their home address. We used data from the American Community Survey (ACS) for the period 2011–2015. We dichotomized the neighborhood income using the distribution median. Low neighborhood socioeconomic status (nSES) was defined as neighborhood with a median household income below $63,269 (vs. high nSES).
2.6. Covariates
Covariates included age, sex, ethnicity (Hispanic/Latino vs. non-Hispanic), individual income (categorized into 3 categories: less then 30k, 30k – 55k, more than 55k), and nitrogen dioxide (NO2) concentration. We used an inverse distance weighting approach to calculate yearly averages of air pollution across the study area for years 2014–2017 based on daily observations of NO2 in ug/m3 from eight Environmental Protection Agency Air Quality System (EPA AQS) monitoring stations in San Diego County. NO2 exposure was measured using the average pollution (for years 2014–2017) value for a 1600m buffer around the participant’s home. A directed acyclic graph was used to select the covariates.
2.7. Statistical analyses
We first examined Spearman correlations between each of the noise exposures.
2.7.1. Association between noise exposure and insulin resistance or diabetes
To evaluate the association between road or aircraft noise exposure and insulin resistance or T2DM, we performed Generalized Estimating Equation (GEE) models with exchangeable matrix, accounting for participants clustering within zip code. We chose to account for clustering by zip code because of the small number of participants in census tract. We used gaussian distribution for insulin resistance and binomial distribution and log-link function for T2DM. We performed models separately for static and dynamic exposures. The GEE models were adjusted for age, sex, ethnicity, individual income, and NO2 concentration. We checked for the potential presence of multicollinearity in our models by calculating the Variance Inflation Factor (VIF). We used natural cubic splines to explore potential deviation from linearity.
2.7.2. Potential effect modification by nSES
First, we assessed the interaction between noise exposure and nSES. We plotted the marginal effects between noise level and insulin resistance or T2DM according to nSES to look at a potential difference in dose-effect relationship. Then, to identify the subgroups of individuals in which a potential intervention on noise exposure is likely to be the most effective, we calculated the relative excess risk due to interaction (RERI). RERI gives a qualitative assessment of additive interaction and is define as follow: RERIOR=OR11 − OR10 − OR01 + 1 (VanderWeele and Knol, 2014; Knol et al., 2011). For example, OR11 corresponds to the Odds Ratio among participants exposed to high levels of noise and living in low nSES. The direction, and not magnitude, of RERI is needed to understand the public health relevance of interaction identifying which subgroups of nSES would benefit most from intervention when resources are limited. A RERI >0 implies the public health consequences of an intervention on noise exposure would be larger in the low nSES group, while RERI <0 implies the public health consequences of an intervention on noise exposure would be larger in the high nSES group (VanderWeele and Knol, 2014). Analyses were performed with RStudio Version 3.6.5.
3. Results
3.1. Population sample
Among the 602 participants, we restricted the population to participants with HOMA-IR and T2DM data (N = 598). Participants with missing information on covariates (income and NO2) were excluded (n = 25). For the dynamic noise analyses, participants without GPS data (n = 3) and extreme noise values (n = 3) were also excluded. Among 573 participants included (95% of original sample), 318 were female (58.3%) and 239 identified as Hispanic/Latino (41.7%). The mean age was 58.7 years (SD 11.0). In comparison to participants living in high-income neighborhood (i.e., neighborhood median income ≥$63,269), participants living in low nSES were younger (median age: 57.5 vs. 59.9 years), more often women (56.3 vs 54.7%), more often Hispanic/Latino (54.6 vs. 29.1%) and had lower individual incomes (Table 1). Surprisingly, the level of NO2 was lower among participants living in low nSES. Participants living in low nSES also had higher levels of insulin resistance (HOMA-IR median: 2.23 vs 1.84) and higher prevalence of T2DM (11.3 vs 5.9% according to blood glucose level, and 16.5 vs 11.1% according to self-reported or medication). Fig. 2 displays the spatial distribution of static road and aircraft noise exposures over San Diego County in 2016 and shows important variability across census tracts. For all participants, the median exposure to road traffic at the census tract was 53.4 dB(A). For participants exposed to aircraft noise level at census tract level, the median exposure was 47 dB(A). After conversion in Lden indicator (Brink et al., 2018), this corresponds to 56.7 dB and 50.6 dB, respectively, knowing that the 2018 WHO noise guidelines for protecting health are 53 dB for road noise and 45 dB for aircraft noise using Lden indicator (Kempen et al., 2018).
Table 1.
Distribution of participant characteristics and noise exposures according to neighborhood socioeconomic status (N = 573).
| n, (%) | Participants living in low nSES (n = 284) | Participants living in high nSES (n = 289) | p-valuec |
|---|---|---|---|
|
| |||
| Sociodemographic characteristics | |||
| Female | 160 (56.3) | 158 (54.7) | 0.7 |
| Agea | 57.5 (11.1) | 59.9 (10.9) | 0.009 |
| Hispanic/Latino | 155 (54.6) | 84 (29.1) | <.0001 |
| Income | <.0001 | ||
| $30k or less | 115 (40.5) | 45 (15.6) | |
| $30k to $55k | 84 (29.6) | 50 (17.3) | |
| $55k+ | 85 (29.9) | 194 (67.1) | |
| Cardiometabolic health | |||
| HOMA-IRb | 2.23 (1.40–4.25) | 1.84 (1.15–3.21) | <.0001 |
| T2DM (blood glucose level ≥126 mg/dL) | 32 (11.3) | 17 (5.9) | 0.02 |
| T2DM (self-reported or medication) | 47 (16.5) | 32 (11.1) | 0.06 |
| Environmental exposuresb | |||
| NO2 (μg/m3) | 10.7 (9.7–11.5) | 11.1 (10.0–11.7) | 0.006 |
| Road noise | |||
| Static exposure dB(A) | |||
| Census tract | 53.7 (52.6–55.7) | 53.1 (52.3–56.0) | 0.02 |
| Buffer | 55.1 (53.6–55.6) | 54.6 (52.7–55.6) | 0.001 |
| Dynamic exposure (N = 568) | |||
| KDE | 0.15 (0.09–0.22) | 0.12 (0.08–0.19) | 0.02 |
| Aircraft noise | |||
| Static exposure dB(A) | |||
| Census Tract (n = 235)d | 48.2 (46.5–51.0) | 46.4 (45.5–47.8) | <.0001 |
| Buffer (n = 316)d | 48.1 (46.4–50.4) | 46.5 (45.8–48.3) | <.0001 |
| Dynamic exposure (N = 570) | |||
| KDE | 0.13 (0.06–0.38) | 0.08 (0.04–0.23) | <.0001 |
nSES: Neighborhood Socioeconomic Status; HOMA-IR: Homeostatic Model Assessment of Insulin Resistance; T2DM: Type 2 Diabetes Mellitus.
mean (SD).
median (interquartile range).
Student or Wilcoxon test for quantitative variable. Chi-square for qualitative variable.
Noise exposure level among participants exposed to aircraft noise in their census tract or buffer around their home.
Fig. 2.
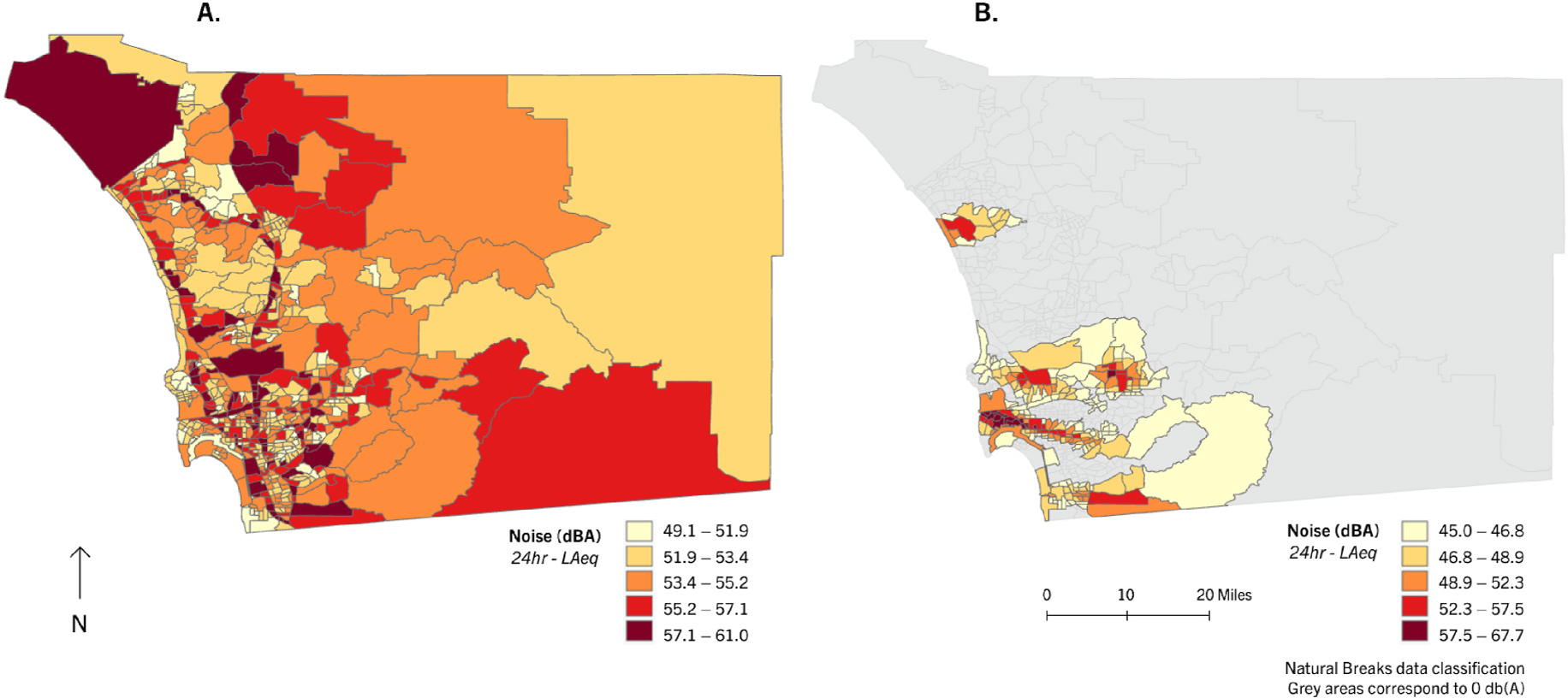
Spatial distribution of static road noise exposure (A) and aviation noise exposure (B), by Census Tract in San Diego County, in 2016.
Figure S3 illustrates Spearman correlations between noise values obtained by different noise exposure assessment methods (administrative boundary, buffer, or KDE). Noise values from static methods (administrative boundary and buffer) tended to have high correlations with each other (p = 0.53 for road noise, p = 0.77 for aircraft noise). Higher correlations were observed between the three assessment methods for aircraft noise than for road noise.
3.2. Socioeconomic inequalities in transportation noise exposure
Participants living in low nSES were exposed to higher levels of static road noise and aircraft noise exposures calculated at census tract level, in comparison to participants living in high-income neighborhood (53.7 vs 53.1 dBA, 48.2 vs 46.4 dBA, respectively) (Table 1). Using home buffer (1600m), participants living in low nSES were also exposed to higher levels of road and aircraft noise (55.1 vs 54.6 dBA, 48.1 vs 46.5 dBA, respectively). These findings are consistent when considering spatio-temporal mobility of participants (using GPS data). Participants living in low nSES were exposed to higher levels of dynamic road and aircraft noise (0.15 vs 0.12, 0.13 vs 0.08, respectively).
3.3. Transportation noise exposure, insulin resistance and diabetes
For all participants, higher static exposure to road noise at census tract level was associated with higher odds of T2DM (OR 1.10, 95%CI: 0.96, 1.27) (Table 2). For insulin resistance, we found a β (95%CI) of 0.02 (−0.02, 0.05). For dynamic aircraft noise (KDE exposure), we observed an OR (95%CI) of 1.52 (0.92, 2.50) for T2DM. In the whole sample, no associations were found between insulin resistance and TD2M (except for static road noise at census tract level) and static or dynamic noise exposures. We did not find evidence of deviation from linearity except for dynamic road noise and T2DM (Figure S4).
Table 2.
Association between noise exposure and diabetes and insulin resistance for all participants.
| Insulin resistance β (95%CI) | T2DM OR (95%CI) | |
|---|---|---|
|
| ||
| Road noise | ||
| Static exposure (N = 573) | ||
| Census Tract | ||
| Continuous* | 0.02 (−0.02, 0.05) | 1.10 (0.96, 1.27) |
| ≥53 dB(A) | 0.04 (−0.10, 0.17) | 1.36 (0.75, 2.46) |
| Buffer around home | ||
| Continuous* | − 0.01 (−0.06, 0.03) | 1.02 (0.84, 1.24) |
| ≥55 dB(A) | − 0.06 (−0.19, 0.07) | 1.02 (0.55, 1.88) |
| Dynamic exposure (N = 566) KDE | ||
| Continuous* | − 0.15 (−0.83, 0.53) | 0.41 (0.07, 2.49) |
| ≥ median | − 0.10 (−0.24, 0.03) | 1.23 (0.64, 2.38) |
| Aircraft noise | ||
| Static exposure (N = 573) | ||
| Census Tract | ||
| ≥45 dB(A) | − 0.03 (−0.16, 0.10) | 1.18 (0.65, 2.16) |
| Buffer around home | ||
| ≥45 dB(A) | − 0.07 (−0.20, 0.06) | 1.58 (0.85, 2.93) |
| Dynamic exposure (N = 567) | ||
| KDE | ||
| Continuous* | − 0.07 (−0.30, 0.17) | 2.22 (0.91, 5.38) |
| ≥ median | − 0.06 (−0.19, 0.07) | 1.52 (0.92, 2.50) |
T2DM: Type 2 Diabetes Mellitus; OR: Odds Ratio; CI: Confidence Interval. Models were adjusted for sex, age, ethnicity, individual income and NO2. This paper has been recommended for acceptance by Dr. Payam Dadvand.. The median of dynamic road and aircraft noise exposure was 0.13 and 0.10, respectively..
3.4. Role of neighborhood socioeconomic status
We identified statistical interactions between road noise exposure at census tract and nSES both for insulin resistance and T2DM (p-value of interaction: 0.09 and 0.02, respectively). We found an interaction of 0.15 between dynamic aircraft noise exposure (KDE exposure) and T2DM. However, we did not identify interactions between noise exposures derived from buffers around participant homes and nSES.
When we stratified the analyses according to the median income of neighborhood of residence (≥$63269 vs <$63269), we found a strong exposure-response relationships between noise exposure and insulin resistance and T2DM, only for participants living in low nSES (Fig. 3 and Figure S5). Participants exposed to road noise exposure greater or equal to 53 dB(A) in their census tract and living in low nSES had increased level of HOMA-IR (β 0.15, 95%CI: −0.04, 0.34) and higher odds of T2DM (OR 2.34, 95%CI: 1.12, 4.90) (Table 3), in comparison to participants exposed to road noise exposure lower than 53 dB(A) and living in high-income neighborhood. Participants exposed to high levels of road noise around their homes and living in low nSES also had higher odds of T2DM (OR 2.08, 95%CI: 0.95, 4.59) (Table S1). Moreover, participants exposed to dynamic aircraft noise (KDE exposure) above the median and living in low nSES had higher odds of T2DM (OR 2.21, 95% CI: 1.09, 4.49) (Table 4).
Fig. 3.
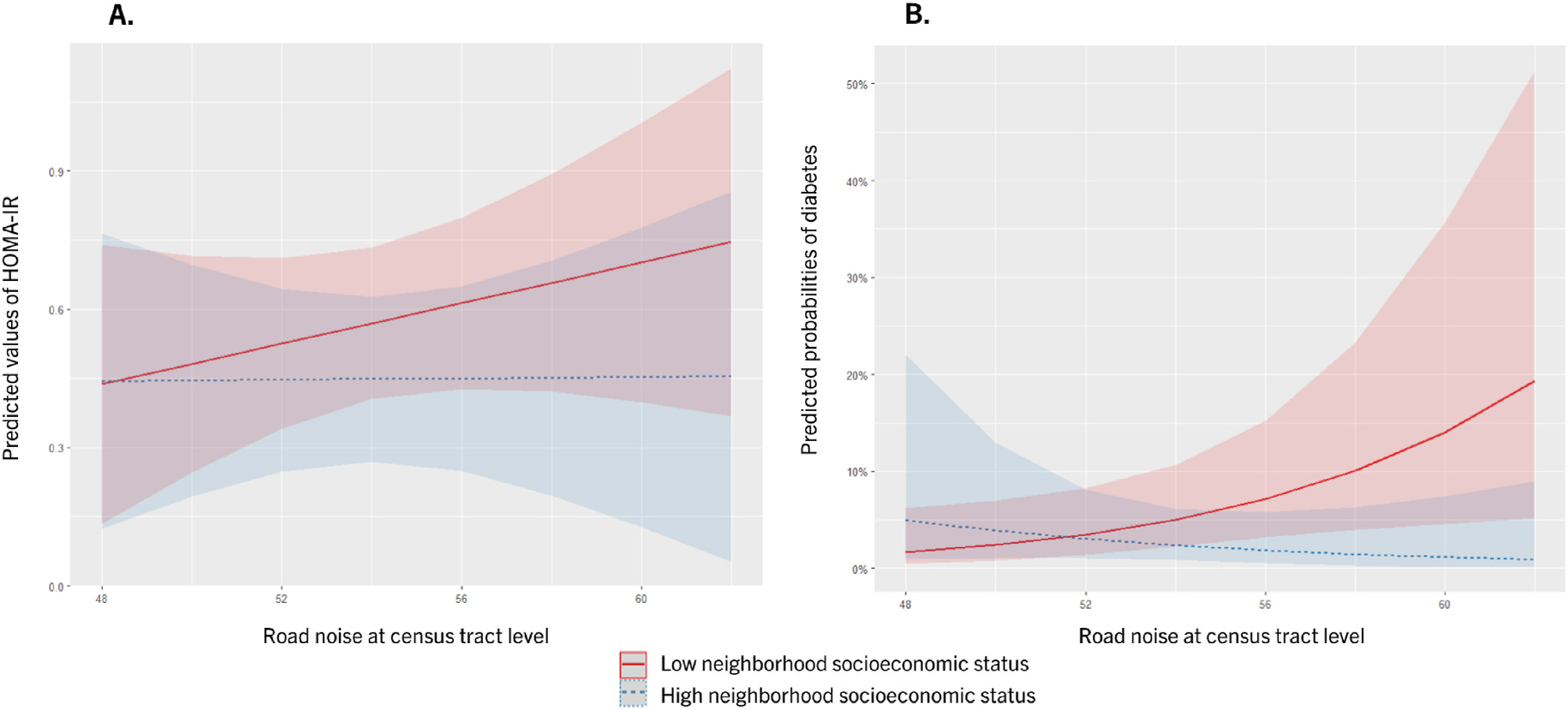
Marginal effects for relationships between static road noise at census tract level and insulin resistance (A) and T2DM (B), according to neighborhood socioeconomic status (adjusted for age, ethnicity, individual income and NO2).
Table 3.
Neighborhood socioeconomic status as effect modifier in the relationships between static road noise exposure at census tract level and insulin resistance and type 2 diabetes mellitus (N = 573).
| Insulin resistance | n | β | (95%CI) | |
|---|---|---|---|---|
|
| ||||
| Static road noise exposure at census tract level | Neighborhood SES | |||
|
| ||||
| <53 dB(A) | ≥ median income | 152 | Ref. | |
| ≥53 dB(A) | ≥ median income | 137 | − 0.08 | (−0.27, 0.11) |
| <53 dB(A) | < median income | 128 | 0.01 | (−0.18, 0.19) |
| ≥53 dB(A) | < median income | 156 | 0.15 | (−0.04, 0.34) |
| Diabetes | OR | (95%CI) | ||
| Static road noise exposure at census tract level | Neighborhood SES | |||
|
| ||||
| <53 dB(A) | ≥ median income | 152 | Ref. | |
| ≥53 dB(A) | ≥ median income | 137 | 0.48 | (0.17, 1.39) |
| <53 dB(A) | < median income | 128 | 1.01 | (0.42, 2.44) |
| ≥53 dB(A) | < median income | 156 | 2.34 | (1.12, 4.90) |
| Measure of interaction on additive scale | ||||
| RERI | 1.85 | (0.32, 3.37) | ||
Models adjusted for sex, age, ethnicity, individual income, and NO2. SES: socioeconomic status; RERI: relative excess risk due to interaction.
Table 4.
Neighborhood socioeconomic status as effect modifier in the relationships between dynamic aircraft noise exposure (KDE exposure) and type 2 diabetes mellitus (N = 555).
| Diabetes | n | OR | (95%CI) | |
|---|---|---|---|---|
|
| ||||
| Dynamic aircraft noise exposure (KDE) | Neighborhood SES | |||
|
| ||||
| < median | ≥ median income | 161 | Ref. | |
| ≥ median | ≥ median income | 123 | 0.70 | (0.26, 1.84) |
| < median | < median income | 123 | 1.30 | (0.58, 2.91) |
| ≥ median | < median income | 157 | 2.21 | (1.09, 4.49) |
| Measure of interaction on additive scale | ||||
| RERI | 1.22 | (−0.14, 2.58) | ||
Models adjusted for sex, age, ethnicity, individual income and NO2. SES: socioeconomic status; RERI: relative excess risk due to interaction.
Per one unit increase.
For T2DM, we found a positive additive interaction with a RERI of 1.85 (95% CI: 0.32, 3.37) for static road noise exposure assessed at census tract level, and a RERI of 1.22 (95% CI: −0.14, 2.58) for dynamic aircraft noise exposure assessed by KDE (Tables 3 and 4) indicating that the public health consequences of an intervention on road or aircraft noise would be larger for participants living in low nSES. However, no additive interactions were observed using noise exposure derived from buffer around home (Table S1).
Same results were found when diabetes was assessed according to declared diabetes and antidiabetic treatment, with no significant association when the whole sample was considered (Table S2). A significant multiplicative interaction was also found between road noise at census tract level and from buffer, and nSES (p-value of interaction: 0.006 and 0.065, respectively). Participants living in low nSES had higher odds of T2DM when exposed to high levels of road noise in their census tract or around their home (OR 2.07, 95%CI: 1.05, 4.07; OR 1.53, 95%CI: 0.75, 3.09, respectively) in comparison to participants living in high nSES (OR 0.45, 95%CI: 0.18, 1.10; OR 0.53, 95%CI: 0.26, 1.11, respectively). Moreover, using this definition of diabetes we also found positive additive interactions when assessing road noise at census tract level or from buffer with RERI of 1.11 (95% CI: 0.48, 1.74) and 0.83 (95% CI: 0.10, 1.56), respectively (Table S3).
4. Discussion
Using data from the Community of Mine Study, we found major socioeconomic inequalities in transportation noise exposure and cardiometabolic impacts in San Diego County, CA. Participants living in low neighborhood SES were exposed to higher levels of road and aircraft noise, regardless of the method of exposure assessment: static methods (average at census tract or average for a 1600m buffer around the participant’s home) or our dynamic method (KDE exposure using GPS point data). Moreover, nSES was found to be a major effect modifier in the relationship between noise pollution and T2DM or insulin resistance. Participants exposed to static road noise exposure greater or equal to 53 dB(A) in their census tract and living in low nSES had increased insulin resistance and T2DM risk. Participants exposed to dynamic aircraft noise (KDE exposure) above the median and living in low nSES also had higher risk of T2DM. We found positive additive interactions indicating that health benefits of an intervention on road and aircraft noise would be larger in participants living in low nSES.
Epidemiologic evidence linking transportation noise to insulin resistance and T2DM remains scarce for diverse US populations, and there is a need to better understand the nature of interactions between other associated social and environmental determinants. In this study, we found an association between road and aircraft noise exposure and T2DM only among participants living in low nSES, even after adjustment for air pollution. Even if there is little evidence of confounding, air pollution may confound the association between environmental noise and health outcomes (Eminson et al., 2021). These findings are consistent regardless of the definition of diabetes used (blood glucose level, or self-reported diabetes and medication) or the methods of noise assessment (census tract, buffer around home, or GPS data). Our results are in line with several longitudinal studies in Europe and Canada looking at the impact of noise exposure on T2DM (Clark et al., 2017; Shin et al., 2020; Thacher et al., 2021; Eze et al., 2017b). In the two most recent studies, long-term exposure to road traffic noise was found to be associated with an increased risk of T2DM among 914,607 persons in Toronto and among 3,563,991 persons in Denmark (Shin et al., 2020; Thacher et al., 2021). Recent studies reported an association between noise exposure and an increased risk of metabolic syndrome (Huang et al., 2020; Yu et al., 2020; Li et al., 2021). In the Sacramento area of California, noise pollution was found to increase the risk of developing metabolic syndrome among elderly Mexican-Americans (Yu et al., 2020). In our study, we found that participants exposed to high level of road noise exposure and living in low nSES had increased insulin resistance, a key contributor to T2DM, and a relationship few have investigated thus far in an ethnically diverse cohort.
We found that differences in noise exposure may contribute to health inequities, as we found higher levels of noise pollution exposure among participants living in low nSES. Our findings are particularly relevant for advancing environmental justice issues and neighborhood-level social determinants of health. First, our study found that participants living in low nSES were most exposed to road and aircraft noise, both with static and dynamic estimates, in comparison to participants living in high-income neighborhoods. This finding contributes to the growing body of evidence suggesting that people in lower socioeconomic strata tend to be more exposed to many environmental stressors such as air pollution (Jbaily et al., 2022; Hajat et al., 2015), but also more susceptible to related health effects than the general population (Son et al., 2019). Second, our study revealed that nSES was a major effect modifier; participants living in low nSES had higher exposure and vulnerability to noise exposure. These findings suggest a possible “double jeopardy” whereby the association between noise exposure and adverse health outcomes is greater for those living in low nSES. One explanation may be the difference in access to high-quality public green spaces and local quiet areas, which are limited in low nSES (Wen et al., 2013); having access to green space and quiet areas can improve soundscape quality and buffer the negative impact of noise (Uebel et al., 2021). Another hypothesis is the potential differences of housing noise insulation (Hajat et al., 2015). We can assume that the houses in low nSES are less insulated and less likely to have double or triple-paned windows, and therefore their residents experience greater exposure to noise, especially during the night. Low-income individuals can also be more susceptible to stressor-linked effects due to a disproportionate burden of other social stressors such as poverty, low quality nutrition, less access to education and healthcare, and racism (Beech et al., 2021). Individual sensitivity to noise exists (manifested by an increased degree of vigilance and physiological reactivity to sound) and high sensitivity to noise can exacerbate stress responses and be associated with poorer health status (Baliatsas et al., 2016). Finally, low-income individuals may also experience higher noise levels in their work environment (Mehlum and Aarhus, 2020) or other occupational hazards, and both exposures may result in a greater adverse effect as shown previously for metabolic syndrome (Li et al., 2021).
Even with the small number of participants who had diabetes and were exposed to high aircraft noise, we were able to identify an association between dynamic aircraft noise exposure and diabetes among participants living in low nSES. This association was found with dynamic aircraft noise exposure (KDE exposure considering participant locations visited and the time spent in all locations), maybe because aircraft noise is concentrated at precise locations and thus the use of GPS data was critical to reduce exposure misclassification. Moreover, it is important to note that airports with exclusively military operations were excluded from aircraft noise assessment. San Diego is home to several Navy, Marine Corps and Coast Guard bases, and the lack of consideration for military jet noise, much louder than other airplanes, may have led to an underestimation of noise exposure and possible exposure misclassification.
Our study had limitations. First, our sample size is relatively small due to the burden and costs of collecting cardiometabolic biomarkers and GPS/accelerometer data. Participants were recruited from San Diego County, limiting the generalization of results. Noise exposures were assessed at a single point in time to capture long-term exposures, as we only have access to 2016 noise exposure. However, participants have lived at the same address for an average of 17 years, limiting the exposure misclassification. We did not consider other environmental noise exposures (noise from railways, maritime, from sites of industrial activity) or co-exposure to occupational noise. Finally, we evaluated noise effect using a LAeq noise metric, A-weighted equivalent continuous sound pressure level, and no nighttime noise penalty was incorporated to evaluate noise exposure. We were not able to evaluate the effect of nocturnal environmental noise on insulin resistance or diabetes, while it may be the most concerning form of noise pollution with influence through sleep disturbances (Thiesse et al., 2018).
5. Conclusions
Our study showed that cross-sectional exposure to higher levels of road and aircraft noise was associated with T2DM among participants living in low nSES in San Diego County. Neighborhood SES was a major effect modifier in the associations between transportation noise and insulin resistance or T2DM, underscoring the need to consider noise pollution and socio-economic status in parallel to understand health inequities. If these findings are confirmed by future studies, we recommend targeting people living in low nSES, especially when resources are limited, for which an intervention reducing transportation noise will have the greatest public health impact.
Supplementary Material
Acknowledgements
We thank the U.S. Department of Transportation Bureau of Transportation Statistics that provides the road and aircraft noise layers for California state. This work was supported by the National Cancer Institute [R01CA228147, R01CA179977]. Exposure data are available upon request.
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2023.122277.
This paper has been recommended for acceptance by Payam Dadvand.
Data availability
Data will be made available on request.
References
- Baliatsas C, van Kamp I, Swart W, Hooiveld M, Yzermans J, 2016. Noise sensitivity: symptoms, health status, illness behavior and co-occurring environmental sensitivities. Environ. Res. 150, 8–13. [DOI] [PubMed] [Google Scholar]
- Beech BM, Ford C, Thorpe RJ, Bruce MA, Norris KC, 2021. Poverty, racism, and the public health crisis in America. Front. Public Health 9:699049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brink M, Schäffer B, Pieren R, Wunderli JM, 2018. Conversion between noise exposure indicators Leq24h, LDay, LEvening, LNight, Ldn and Lden: principles and practical guidance. Int. J. Hyg Environ. Health 221 (1), 54–63. [DOI] [PubMed] [Google Scholar]
- Carlson JA, Jankowska MM, Meseck K, Godbole S, Natarajan L, Raab F, et al. , 2015. Validity of PALMS GPS scoring of active and passive travel compared to SenseCam. Med. Sci. Sports Exerc. 47 (3), 662–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey JA, Morello-Frosch Rachel, Mennitt DJ, Fristrup K, Ogburn EL, James P, 2017. Race/ethnicity, socioeconomic status, residential segregation, and spatial variation in noise exposure in the contiguous United States. Environ. Health Perspect. 125 (7), 077017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark C, Sbihi H, Tamburic L, Brauer M, Frank LD, Davies HW., 2017. Association of long-term exposure to transportation noise and traffic-related air pollution with the incidence of diabetes: a prospective cohort study. Environ. Health Perspect. 125 (8), 087025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dendup T, Feng X, Clingan S, Astell-Burt T, 2018. Environmental risk factors for developing type 2 diabetes mellitus: a systematic review. Int. J. Environ. Res. Publ. Health 15 (1), 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimakopoulou K, Koutentakis K, Papageorgiou I, Kasdagli MI, Haralabidis AS, Sourtzi P, et al. , 2017. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup. Environ. Med. 74 (11), 830–837. [DOI] [PubMed] [Google Scholar]
- Dreger S, Schüle SA, Hilz LK, Bolte G, 2019. Social inequalities in environmental noise exposure: a review of evidence in the WHO European region. Int. J. Environ. Res. Publ. Health 16 (6), 1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eminson K, Chen Y, Fenech B, Rodgers G, Hansell A, 2021. Does air pollution confound associations between environmental noise and cardiometabolic outcomes? - A systematic review. Environmental Research. 12. [DOI] [PubMed] [Google Scholar]
- European Environment Agency, 2020. Environmental noise in Europe (EEA Report No 22/2019; ). [Google Scholar]
- Eze IC, Foraster M, Schaffner E, Vienneau D, Héritier H, Rudzik F, et al. , 2017a. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int. J. Epidemiol. 46 (4), 1115–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eze IC, Foraster M, Schaffner E, Vienneau D, Héritier H, Rudzik F, et al. , 2017b. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int. J. Epidemiol. 46 (4), 1115–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A, Hsia C, O’Neill MS, 2015. Socioeconomic disparities and air pollution exposure: a global review. Curr. Environ. Health Rep. 2 (4), 440–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer MS, Swinburn TK, Neitzel RL, 2014. Environmental noise pollution in the United States: developing an effective public health response. Environ. Health Perspect. 122 (2), 115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang T, Chan TC, Huang YJ, Pan WC, 2020. The association between noise exposure and metabolic syndrome: a longitudinal cohort study in taiwan. Int. J. Environ. Res. Publ. Health 17 (12), 4236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankowska MM, Sears DD, Natarajan L, Martinez E, Anderson CAM, Sallis JF, et al. , 2019. Protocol for a cross sectional study of cancer risk, environmental exposures and lifestyle behaviors in a diverse community sample: the Community of Mine study. BMC Publ. Health 19 (1), 186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankowska MM, Yang JA, Luo N, Spoon C, Benmarhnia T, 2021. Accounting for space, time, and behavior using GPS derived dynamic measures of environmental exposure. Health Place, 102706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankowska MM, Yang JA, Luo N, Spoon C, Benmarhnia T, 2023. Accounting for space, time, and behavior using GPS derived dynamic measures of environmental exposure. Health Place 79, 102706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jbaily A, Zhou X, Liu J, Lee TH, Kamareddine L, Verguet S, et al. , 2022. Air pollution exposure disparities across US population and income groups. Nature 601 (7892), 228–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jørgensen JT, Bräuner EV, Backalarz C, Laursen JE, Pedersen TH, Jensen SS, et al. , 2019. Long-term exposure to road traffic noise and incidence of diabetes in the Danish nurse cohort. Environ. Health Perspect. 127 (5), 57006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempen E van, Casas M, Pershagen G, Foraster M, 2018. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int. J. Environ. Res. Publ. Health 15 (2), E379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klompmaker JO, Janssen NAH, Bloemsma LD, Gehring U, Wijga AH, van den Brink C, et al. , 2019. Associations of combined exposures to surrounding green, air pollution, and road traffic noise with cardiometabolic diseases. Environ. Health Perspect. 127 (8), 87003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knol MJ, VanderWeele TJ, Groenwold RHH, Klungel OH, Rovers MM, Grobbee DE, 2011. Estimating measures of interaction on an additive scale for preventive exposures. Eur. J. Epidemiol. 26 (6), 433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon BM, Maddox TM, 2015. Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J. Diabetes 6 (13), 1246–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Ruan W, Yi G, Chen Z, Wang D, 2021. Association of noise exposure with risk of metabolic syndrome: evidence from 44,698 individuals. Diabetes Res. Clin. Pract. 178, 108944. [DOI] [PubMed] [Google Scholar]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC, 1985. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28 (7), 412–419. [DOI] [PubMed] [Google Scholar]
- Mehlum IS, Aarhus L, 2020. Occupational Noise: A Determinant of Social Inequalities in Health. In: Theorell T (Ed.), Handbook of Socioeconomic Determinants of Occupational Health. Handbook Series in Occupational Health Sciences. Springer, Cham. [Google Scholar]
- Meseck K, Jankowska MM, Schipperijn J, Natarajan L, Godbole S, Carlson J, et al. , 2016. Is missing geographic positioning system data in accelerometry studies a problem, and is imputation the solution? Geospatial Health 11 (2), 403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Gori T, Babisch W, Basner M, 2014. Cardiovascular effects of environmental noise exposure. Eur. Heart J. 35 (13), 829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Sørensen M, Daiber A, 2021. Transportation noise pollution and cardiovascular disease. Nat. Rev. Cardiol. 18 (9), 619–636. [DOI] [PubMed] [Google Scholar]
- National Diabetes Statistics Report | Diabetes | CDC; [Internet], 2022. [cited 2022 Oct 5]. https://www.cdc.gov/diabetes/data/statistics-report/index.html. [Google Scholar]
- Ohlwein S, Hennig F, Lucht S, Matthiessen C, Pundt N, Moebus S, et al. , 2019. Indoor and outdoor road traffic noise and incident diabetes mellitus: results from a longitudinal German cohort study. Environ. Epidemiol. Phila. Pa 3 (1), e037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen M, Halldorsson TI, Ketzel M, Grandström C, Raaschou-Nielsen O, Jensen SS, et al. , 2019. Associations between ambient air pollution and noise from road traffic with blood pressure and insulin resistance in children from Denmark. Environ. Epidemiol. 3 (5), e069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin S, Bai L, Oiamo TH, Burnett RT, Weichenthal S, Jerrett M, et al. , 2020. Association between road traffic noise and incidence of diabetes mellitus and hypertension in Toronto, Canada: a population-based cohort study. J. Am. Heart Assoc. 9 (6), e013021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon MC, Hart JE, Levy JI, VoPham T, Malwitz A, Nguyen D, et al. , 2022. Sociodemographic patterns of exposure to civil aircraft noise in the United States. Environ. Health Perspect. 130 (2), 027009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivakumaran K, Ritonja JA, Waseem H, AlShenaibar L, Morgan E, Ahmadi SA, et al. , 2022. Impact of noise exposure on risk of developing stress-related health effects related to the cardiovascular system: a systematic review and meta-analysis. Noise Health 24 (114), 107–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son JY, Liu JC, Bell ML, 2019. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ. Res. Lett. 14 (7), 073004. [Google Scholar]
- Taylor D, 2014. Toxic Communities: Environmental Racism, Industrial Pollution, and Residential Mobility. NYU Press, New York. [Google Scholar]
- Thacher JD, Poulsen AH, Hvidtfeldt UA, Raaschou-Nielsen O, Brandt J, Geels C, et al. , 2021. Long-term exposure to transportation noise and risk for type 2 diabetes in a nationwide cohort study from Denmark. Environ. Health Perspect. 129 (12), 127003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiesse L, Rudzik F, Spiegel K, Leproult R, Pieren R, Wunderli JM, et al. , 2018. Adverse impact of nocturnal transportation noise on glucose regulation in healthy young adults: effect of different noise scenarios. Environ. Int. 121 (Pt 1), 1011–1023. [DOI] [PubMed] [Google Scholar]
- Uebel K, Marselle M, Dean AJ, Rhodes JR, Bonn A, 2021. Urban green space soundscapes and their perceived restorativeness. People Nat. 3 (3), 756–769. [Google Scholar]
- VanderWeele TJ, Knol MJ, 2014. A Tutorial on Interaction. Epidemiol. Methods 3 (1), 33–72. [Google Scholar]
- Vienneau D, Eze I, Probst-Hensch N, Röösli M, 2019. Association between Transportation Noise and Cardio-Metabolic Diseases: an Update of the WHO Meta-Analysis. [Google Scholar]
- Volpe National Transportation Systems Center, 2020. Environmental Measurement and Modeling Division. Environmental Science and Engineering Division. 10.21949/1520433. [DOI] [Google Scholar]
- Wen M, Zhang X, Harris CD, Holt JB, Croft JB, 2013. Spatial disparities in the distribution of parks and green spaces in the USA. Ann. Behav. Med. Publ. Soc. Behav. Med. 45 (Suppl. 1), 18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y, Paul K, Arah OA, Mayeda ER, Wu J, Lee E, et al. , 2020. Air pollution, noise exposure, and metabolic syndrome - a cohort study in elderly Mexican-Americans in Sacramento area. Environ. Int. 134, 105269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zare Sakhvidi MJ, Zare Sakhvidi F, Mehrparvar AH, Foraster M, Dadvand P, 2018. Association between noise exposure and diabetes: a systematic review and meta-analysis. Environ. Res. 166, 647–657. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.


