Abstract
Background
Non-alcoholic fatty liver disease (NAFLD) is characterized by hepatic steatosis. It is the leading cause of liver-related mortality, end-stage liver disease, and the need for liver transplantation. This study aimed to assess the level of awareness regarding NAFLD among the adult population in Jazan, Saudi Arabia, and to explore the determinants of the awareness level.
Method
This descriptive cross-sectional study was conducted among the general population of Jazan, Saudi Arabia, under the supervision of Jazan University, excluding those with end-stage liver failure. An online self-administered questionnaire, adopted from the literature, was sent through different social media platforms. A total of 1,034 people participated in this study. The chi-square test and multiple linear regression were used to identify the predictors of NAFLD awareness.
Results
Fifty-three percent of the participants were aware of NAFLD. The mean score of the participants' awareness was 22.7 ± 4.9 out of 40 points. Employed (95% confidence interval (CI): -1.9, -0.03; p = 0.044) and private business individuals (95% CI: -3.5, -1.1; p < 0.001) had a lower awareness level than students. The higher income level was associated with greater awareness (95% CI: 0.36, 2.4; p = 0.008). Those who had never heard of NAFLD had nearly twice as much awareness (95% CI: -3.0, -0.67; p = 0.002).
Conclusions
Nearly half the study participants displayed good awareness of NAFLD. However, efforts must focus on awareness campaigns, encouraging health-seeking behaviors, and targeted screening for early detection and treatment, especially in at-risk populations, since many participants were unaware of NAFLD.
Keywords: jazan, awareness, middle east, liver disease, nafld
Introduction
Non-alcoholic fatty liver disease (NAFLD) represents a complex spectrum of liver disorders characterized by hepatic steatosis and excessive fat accumulation within the liver without secondary causes, such as heavy alcohol consumption. This spectrum ranges from non-alcoholic fatty liver (NAFL), which tends to be relatively benign, to a more severe and potentially progressive form known as non-alcoholic steatohepatitis (NASH). Left unaddressed, NAFLD can lead to fibrosis and cirrhosis, which pose significant threats to public health [1,2].
NAFLD is distinctly categorized into two types. The first type is closely associated with metabolic syndrome. The prevailing understanding implicates insulin resistance as the primary underlying mechanism [3-5]. Individuals with NAFLD often exhibit one or more components of metabolic syndrome, such as systemic hypertension, dyslipidemia, insulin resistance, or overt diabetes [6].
NAFLD has surged globally, affecting approximately 30.05% of the world's population [7]. It is the leading cause of liver-related mortality [8] and end-stage liver disease [9], often necessitating liver transplantation [10]. Escalating epidemics of obesity and type-2 diabetes mellitus have fueled the rise in NAFLD [11,12]. The Middle East has witnessed a notable increase in NAFLD prevalence in recent years, from 36.53% in 1990 to 42.62% in 2019 [7]. A systematic review reported an NAFLD prevalence of 16.8% in Saudi Arabia [13]. In particular, the obesity rates in Saudi Arabia exceed the global average, contributing to a higher prevalence of NAFLD in the region [14].
Despite the growing global significance of NAFLD, awareness of this condition remains dismally low. In the United States, NAFLD awareness is only 4.4%, representing a glaring discrepancy compared to the awareness levels of other liver-related disorders, such as viral hepatitis [15]. European countries exhibited similarly low awareness rates [16]. One study found that only 2.4% of the individuals diagnosed with NAFLD were aware of their condition [17].
However, the importance of raising awareness of NAFLD cannot be overstated. Elevated awareness is a pivotal step toward increasing treatment uptake, facilitating informed decisions, and promoting crucial behavioral changes, such as lifestyle modifications. Beyond its clinical implications, NAFLD has a significant economic impact and diminishes the overall health-related quality of life of affected individuals [18].
This study aimed to assess the level of NAFLD awareness among the adult population in Jazan, Saudi Arabia, and to identify the factors influencing this awareness.
Materials and methods
This study represents a descriptive cross-sectional investigation undertaken within the geographic confines of the Jazan region, situated in the southwestern expanse of Saudi Arabia, contiguous with the Red Sea, encompassing an approximate population of 1.5 million residents. The study included the population of Jazan aged 18 years or above who possessed basic literacy skills and had social media platforms. Individuals with end-stage liver failure were excluded.
The sample size was determined using the following formula:
n = z²p(1-p)/d²,
where Z corresponds to a 95% confidence level, p denotes the anticipated population proportion, and d denotes the 5% margin of error. In addition, a 10% nonresponse rate was factored in, yielding a minimum sample size of 440 participants.
Data collection
A preliminary pilot study involving a selected group of participants was conducted to assess the questionnaire's clarity and understanding. Participant feedback from the preliminary phase was incorporated into the final survey. The survey tool was disseminated to participants through Google Forms, Facebook, and WhatsApp, employing convenience sampling.
The questionnaire comprised two principal sections. The first segment collected demographic data, including age, gender, nationality, employment status, educational qualifications, and monthly income. The second section featured the validated questionnaire derived from previous studies [19] that explored the participants’ NAFLD knowledge, including prior liver disease diagnoses among respondents or their close relatives. Moreover, it delved into the participants' awareness of NAFLD, including their comprehension of the risk factors, diagnostic methodologies, treatment modalities, associated symptoms, and potential complications arising from this condition. Furthermore, the participants' perceptions toward NAFLD curability, preventability, and potentially life-threatening effects were assessed.
A structured scoring system was implemented to assess NAFLD awareness. Correct, incorrect, and neutral responses were assigned scores of 2, 0, and 1, respectively. Subsequently, a cumulative awareness score was computed for each participant, resulting in scores ranging from 0 to 40 points. Higher scores indicated greater levels of awareness.
The normality of the data distribution was examined using the Kolmogorov-Smirnov test. To categorize awareness data, the median score was employed as a delineating threshold, bifurcating participants into those classified as "aware" (those scoring greater than or equal to the median) and those designated as "not aware" (those scoring less than the median). Categorical data were presented using frequency and percentage. To identify the factors associated with NAFLD awareness, multiple linear regression analysis was performed. The statistical significance of the study was set at p < 0.05.
Ethical considerations
Ethical approval was obtained from the Jazan Health Ethics Committee (IRB No.: REC-44/05/404). Each participant was provided with a comprehensive explanation of the study's objectives. Written informed consent was obtained from all participants, affirming their voluntary participation in the study. The ethical preference for participant withdrawal at any point was emphasized. The anonymity and confidentiality of participants' identities and responses were maintained.
Results
In this study, 1,034 participants were enrolled, primarily within the 18-24-year age group (48.5%). Most participants were female (72.9%), of Saudi nationality (96.7%), and possessed a bachelor's degree (61.1%). The predominant occupational category was students (38.4%), with the majority reporting a monthly income below 5000 Saudi Riyals (58.7%). Notably, a substantial proportion of participants (62.3%) indicated no prior awareness of NAFLD, with 14.3% reporting educational curricula as their primary source of information on NAFLD (Table 1).
Table 1. Sociodemographic characteristics of the study participants.
SR: Saudi Riyals
| Characteristic | n | (%) |
| Age (years) | ||
| 18-24 | 502 | 48.5% |
| 25-34 | 283 | 27.4% |
| 35-44 | 162 | 15.7% |
| 45-54 | 69 | 6.7% |
| 55-64 | 15 | 1.5% |
| 65 and above | 3 | 0.3% |
| Gender | ||
| Female | 754 | 72.9% |
| Male | 280 | 27.1% |
| Nationality | ||
| Non-Saudi | 34 | 3.3% |
| Saudi | 1,000 | 96.7% |
| Level of education | ||
| Primary | 6 | 0.6% |
| Intermediate | 25 | 2.4% |
| Secondary | 232 | 22.4% |
| Bachelor's | 632 | 61.1% |
| Others | 139 | 13.4% |
| Occupation | ||
| Employed | 239 | 23.1% |
| Private business | 79 | 7.6% |
| Housewife | 116 | 11.2% |
| Student | 397 | 38.4% |
| Retired | 203 | 19.6% |
| Income level | ||
| Less than 5000 SR | 607 | 58.7% |
| 5000-10,000 SR | 222 | 21.5% |
| 10,000-15,000 SR | 135 | 13.1% |
| More than 15,000 SR | 70 | 6.8% |
| Source of information | ||
| Friends/relatives | 55 | 5.3% |
| From my curriculum | 148 | 14.3% |
| From my doctor | 31 | 3% |
| Social media | 99 | 9.6% |
| Others | 57 | 5.5% |
| I have never heard about it before | 644 | 62.3% |
It was ascertained that 9.4% of the participants had either a personal diagnosis of NAFLD or were acquainted with it through a relative’s diagnosis. Notably, 77% of the respondents acknowledged NAFLD's potential to induce hepatic inflammation, whereas 50% were ignorant regarding its presenting symptoms. In addition, 47% identified obesity as a prevalent risk factor, with 39% recognizing end-stage liver disease as a potential complication. Of the participants, 42% perceived NAFLD as preventable, 50% believed it was curable, and 53% considered it a life-threatening condition (Table 2).
Table 2. Awareness regarding NAFLD among the adult population of Jazan.
NAFLD: non-alcoholic fatty liver disease, BMI: body mass index, CT: computed tomography, MR: magnetic resonance, USG: ultrasound sonography
| Characteristic | N = 1,0341 |
| Have you or someone you know ever been diagnosed with NAFLD? | |
| Yes* | 97 (9.4%) |
| No | 732 (71%) |
| I don’t remember | 205 (20%) |
| NAFLD is characterized by the accumulation of……… | |
| Fats in heart | 8 (0.8%) |
| Fats in the liver* | 639 (62%) |
| I don’t know | 359 (35%) |
| Oil in liver | 28 (2.7%) |
| Do you think NAFLD can only occur if it runs in the family? | |
| Agree | 174 (17%) |
| Disagree* | 352 (34%) |
| I don’t know | 508 (49%) |
| Do you think healthy eating habits can prevent NAFLD? | |
| Agree* | 708 (68%) |
| Disagree | 76 (7.4%) |
| I don’t know | 250 (24%) |
| People with low blood pressure are at higher risk of NAFLD. | |
| Agree | 244 (24%) |
| Disagree* | 151 (15%) |
| I don’t know | 639 (62%) |
| Diabetes is related to NAFLD | |
| Agree* | 362 (35%) |
| Disagree | 131 (13%) |
| I don’t know | 541 (52%) |
| Only adults are prone to the development of NAFLD. | |
| Agree | 291 (28%) |
| Disagree* | 208 (20%) |
| I don’t know | 535 (52%) |
| How many stages can occur in NAFLD disease? | |
| 2 | 70 (6.8%) |
| 3 | 171 (17%) |
| 4* | 119 (12%) |
| I don’t know | 674 (65%) |
| What is the most commonly presented symptom of NAFLD? | |
| Fatigue and lethargy* | 194 (19%) |
| Headache | 24 (2.3%) |
| Nausea and vomiting | 297 (29%) |
| I don’t know | 519 (50%) |
| Which methods are helpful for doctors to diagnose NAFLD? | |
| Blood tests | 63 (6.1%) |
| BMI | 45 (4.4%) |
| Imaging techniques | 94 (9.1%) |
| All of these* | 477 (46%) |
| I don’t know | 355 (34%) |
| What is the standard method for definite diagnosis of NAFLD? | |
| CT | 70 (6.8%) |
| Liver biopsy* | 330 (32%) |
| MR | 75 (7.3%) |
| USG | 47 (4.5%) |
| I don’t know | 512 (50%) |
| What is the standard method for definite treatment of NAFLD? | |
| Angioplasty | 50 (4.8%) |
| Laparoscopy | 127 (12%) |
| Surgical intervention | 157 (15%) |
| None* | 81 (7.8%) |
| I don’t know | 619 (60%) |
| NAFLD can cause... in the liver | |
| Inflammation* | 795 (77%) |
| Injury | 341 (33%) |
| Swelling | 691 (67%) |
| What can be the associated complications of NAFLD? | |
| Liver cancer* | 106 (10%) |
| End-stage liver disease* | 406 (39%) |
| Brain tumor | 15 (1.5%) |
| Cardiovascular disease | 73 (7.1%) |
| Skeletal dysfunction | 12 (1.2%) |
| I don’t know | 422 (41%) |
| What are the common risk factors associated with NAFLD? | |
| Obesity* | 483 (47%) |
| Metabolic disorders* | 416 (40%) |
| Diabetes mellitus* | 316 (31%) |
| Parkinson’s disease | 111 (11%) |
| Dermatitis | 117 (11%) |
| I don’t know | 460 (44%) |
| Do you think NAFLD can be prevented? | |
| Yes* | 431 (42%) |
| No | 94 (9.1%) |
| I don’t know | 509 (49%) |
| Do you think NAFLD can be cured? | |
| Yes* | 521 (50%) |
| No | 85 (8.2%) |
| I don’t know | 428 (41%) |
| Can NAFLD be life-threatening? | |
| Yes* | 551 (53%) |
| No | 72 (7.0%) |
| I don’t know | 411 (40%) |
| 1n (%), *correct answer | |
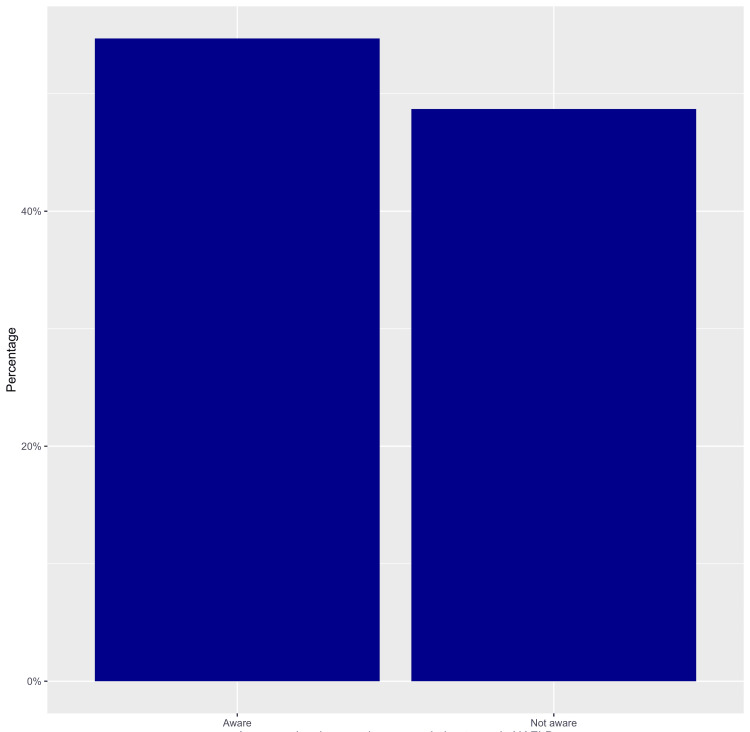
The mean awareness score was 22.7 ± 4.9 out of a maximum attainable score of 40, with a median score of 22. Notably, 52.9% of the participants were categorized as "aware" of NAFLD, while 47.1% fell into the "not aware" category (Figure 1).
Figure 1. Awareness level of NAFLD among the adult population of Jazan.
Distinct patterns emerged when assessing the determinants of NAFLD awareness among the study participants. Employed individuals exhibited a 0.97-point decrease in awareness levels compared to students (95% CI: -1.9, -0.03, p = 0.044), while participants engaged in private business demonstrated a substantially greater decrement, with a 2.3-fold reduction in awareness compared to students (95% CI: -3.5, -1.1; p < 0.001). Furthermore, participants within the income bracket of 10,000-15,000 Saudi Riyals exhibited 1.4 times higher awareness than those with incomes below 5,000 Saudi Riyals (95% CI:0.36, 2.4; p = 0.008). Notably, participants with no prior exposure to information about NAFLD were found to possess nearly half the level of awareness as those who had received information from friends or relatives (95% CI: -3.0, -0.67; p = 0.002) (Table 3).
Table 3. Predictors of NAFLD awareness among the adult population of Jazan.
1CI: confidence interval; SR: Saudi Riyals; NAFLD: non-alcoholic fatty liver disease
| Characteristic | Beta | 95% CI1 | p value |
| Nationality | |||
| Non-Saudi | — | — | |
| Saudi | 1.1 | -0.57, 2.7 | 0.2 |
| Occupation | |||
| Student | — | — | |
| Employed | -0.97 | -1.9, -0.03 | 0.044 |
| Housewife | -0.20 | -1.1, 0.74 | 0.7 |
| Private business | -2.3 | -3.5, -1.1 | <0.001 |
| Retired | -0.72 | -1.5, 0.10 | 0.086 |
| Income level | |||
| Less than 5000 SR | — | — | |
| 5000-10,000 SR | 0.11 | -0.72, 0.94 | 0.8 |
| 10,000-15,000 SR | 1.4 | 0.36, 2.4 | 0.008 |
| More than 15,000 SR | 0.21 | -0.99, 1.4 | 0.7 |
| Source of information | |||
| Friends/relatives | — | — | |
| I have not heard about it before | -1.8 | -3.0, -0.67 | 0.002 |
| Social media | -0.77 | -2.2, 0.63 | 0.3 |
| Others | 0.00 | -1.9, 1.9 | >0.9 |
Being Saudi or a student and having a bachelor's degree was associated with higher NAFLD awareness (p < 0.05). An income of less than 5000 Saudi riyals was associated with higher NAFLD awareness (p < 0.05) (Table 4).
Table 4. Relationship between the participants’ sociodemographic characteristics and their awareness level.
1n (%); 2Pearson's chi-squared test; Fisher's exact test; SR: Saudi Riyals
| Awareness level | |||
| Characteristic | Aware, N = 5471 | Not aware, N = 4871 | p value2 |
| Gender | 0.089 | ||
| Female | 411 (75%) | 343 (70%) | |
| Male | 136 (25%) | 144 (30%) | |
| Age (years) | 0.2 | ||
| 18-24 | 278 (51%) | 224 (46%) | |
| 25-34 | 148 (27%) | 135 (28%) | |
| 35-44 | 82 (15%) | 80 (16%) | |
| 45-54 | 28 (5.1%) | 41 (8.4%) | |
| 55-64 | 10 (1.8%) | 5 (1.0%) | |
| 65 and above | 1 (0.2%) | 2 (0.4%) | |
| Nationality | 0.005 | ||
| Non-Saudi | 10 (1.8%) | 24 (4.9%) | |
| Saudi | 537 (98%) | 463 (95%) | |
| Level of education | <0.001 | ||
| Primary | 1 (0.2%) | 5 (1.0%) | |
| Intermediate | 11 (2.0%) | 14 (2.9%) | |
| Secondary | 100 (18%) | 132 (27%) | |
| Bachelors | 380 (69%) | 252 (52%) | |
| Others | 55 (10%) | 84 (17%) | |
| Occupation | <0.001 | ||
| Employed | 126 (23%) | 113 (23%) | |
| Housewife | 59 (11%) | 57 (12%) | |
| Private business | 30 (5.5%) | 49 (10%) | |
| Student | 239 (44%) | 158 (32%) | |
| Retired | 93 (17%) | 110 (23%) | |
| Income level | 0.024 | ||
| Less than 5000 SR | 328 (60%) | 279 (57%) | |
| 5000-10,000 SR | 101 (18%) | 121 (25%) | |
| 10,000-15,000 SR | 83 (15%) | 52 (11%) | |
| More than 15,000 SR | 35 (6.4%) | 35 (7.2%) | |
| Source of information | <0.001 | ||
| From my curriculum | 128 (23%) | 20 (4.1%) | |
| Friends/relatives | 30 (5.5%) | 25 (5.1%) | |
| I have not heard about it before | 282 (52%) | 362 (74%) | |
| Others | 54 (9.9%) | 34 (7.0%) | |
| Social media | 53 (9.7%) | 46 (9.4%) | |
Discussion
NAFLD is a common benign liver disease. However, it can progress to fibrosis in approximately 32% of cases and to cirrhosis in 20% of cases, over a 10-year course [20]. Despite the high prevalence of NAFLD in Saudi Arabia, studies on the awareness of this disease among the general population are few.
Therefore, the current study aimed to assess the awareness of NAFLD among the population of Jazan. Employed and private business workers were significantly more aware of NAFLD than those who belonged to other occupations (p = 0.044 and 0.001, respectively).
There was a significant correlation between the awareness level and Saudi nationality (p = 0.005). This could be attributed to the high socioeconomic levels and educational privileges among the original Saudi residents compared to non-Saudis who are mostly marginalized or illiterate workers.
The sources of information for most participants were their curriculum (14.3%) and social media (9.6%), which are similar to those of a study on Mexican women where their information sources on NAFLD were mostly family and media [21].
In the present study, 53% of the respondents were aware of NAFLD. By contrast, a similar study by Aljahdli et al. in 2021 on the Saudi population in Jeddah reported an overall awareness of 33% among the study participants [22]. This difference could be attributed to differences between the study samples, improvements in health education programs, and the growing use of smartphones and social communication platforms in Saudi Arabia.
In the current study, 71% of the participants reported that they or their relatives had never been diagnosed with NAFLD, and approximately 48% had a low level of awareness about the disease. Another Asian community-based study conducted in 2020 in Singapore revealed that 71.2% of the participants had heard about NAFLD; a more recent study reported awareness at 75% [23,24].
Despite both being Asian countries and developed economies, the Singaporean population had a better awareness of NAFLD than the Saudi population. Both communities appreciate the fact that NAFLD can be dangerous and life-threatening (53% in Saudi Arabia and 68.8% in Singapore) [23].
Nevertheless, most of our study participants indicated that the disease could be prevented (42%) and cured (50%), compared with 2% and 1%, respectively, in the Brooklyn population [20]. When asked about the familial nature of the disease, 17% of our participants agreed that NAFLD runs in the family, compared to 70% of the United States population who indicated that it is hereditary. A study from a different continent concluded that approximately 84% of the United States population was unaware of NAFLD and the conditions that could predispose them to it. When asked about the risk factors for NAFLD, 44% of our participants indicated their ignorance, compared to 83% of the Brooklyn-USA residents [20]. Interestingly, 49% of the South Korean population was aware of NAFLD, and less than half were aware of its risk factors [25].
Limitations and strengths of the current study
The present study provides significant findings regarding the awareness of NAFLD and its risk factors among people in the Jazan region of Saudi Arabia. However, it also has some limitations. One of the main drawbacks of this study is the use of an online self-administered questionnaire, which may result in a high frequency of missed data and inaccurate answers compared to an interview-based questionnaire. Moreover, only those with good Internet access could have been included in this study. Second, most study respondents and participants were young students, causing an indirect selection bias that could have affected the conclusion. We hope that these limitations will be addressed in future survey-based observational studies.
The strengths of this study include the use of a validated Arabic-translated questionnaire. Furthermore, the sample was adequate and representative of the entire population and the results and conclusions represent an excellent addition to the medical literature. Finally, the present study will undoubtedly enrich the epidemiological data regarding the awareness of NAFLD and its risk factors among the Saudi population.
Recommendations
Based on the outcomes of this study, we recommend strategic planning of awareness campaigns about NAFLD among residents of Jazan and other Saudi areas, in addition to conducting more nationwide surveys to establish awareness levels among the Saudi population and assess their health-seeking behaviors.
Conclusions
More than half of the study participants have good knowledge about NAFLD, yet around 47.1% have low awareness levels, which necessitate establishing awareness programs and enhancing health-seeking behaviors in addition to screening at-risk populations for early diagnosis and treatment of this prevalent disease. The predictors of awareness among our participants were private businesses and high income level. There were no differences in the awareness level between males and females and between the different age groups. Nevertheless, there was a statistically significant difference in awareness level according to nationality, educational level, occupation, and level of income.
Acknowledgments
We would like to extend our gratitude to the Station of Medical Essentials (SOME) Institution for their invaluable contribution in analyzing the data presented in this study.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Bushra I. Maashi, Abdulrahman Kulaybi, Njoud AL Alhadi , Asmaa S. Almalki, Hamad Majrabi , Bushra A. Alfaifi, Alfadl A. Abdulfattah, Erwa Eltayib. Elmakki, Ayoub Salami, Fouad I. Hakami
Acquisition, analysis, or interpretation of data: Bushra I. Maashi, Abdulrahman Kulaybi, Njoud AL Alhadi , Asmaa S. Almalki, Hamad Majrabi , Bushra A. Alfaifi, Alfadl A. Abdulfattah, Erwa Eltayib. Elmakki, Ayoub Salami, Fouad I. Hakami
Drafting of the manuscript: Bushra I. Maashi, Abdulrahman Kulaybi, Njoud AL Alhadi , Asmaa S. Almalki, Hamad Majrabi , Bushra A. Alfaifi, Alfadl A. Abdulfattah, Erwa Eltayib. Elmakki, Ayoub Salami, Fouad I. Hakami
Critical review of the manuscript for important intellectual content: Bushra I. Maashi, Abdulrahman Kulaybi, Njoud AL Alhadi , Asmaa S. Almalki, Hamad Majrabi , Bushra A. Alfaifi, Alfadl A. Abdulfattah, Erwa Eltayib. Elmakki, Ayoub Salami, Fouad I. Hakami
Supervision: Alfadl A. Abdulfattah, Erwa Eltayib. Elmakki
Human Ethics
Consent was obtained or waived by all participants in this study. Jazan Health Ethics Committee issued approval IRB No.: REC-44/05/404. Each participant was provided with a comprehensive explanation of the study's objectives. Written informed consent was obtained from all participants, affirming their voluntary participation in the study. The ethical preference for participant withdrawal at any point was emphasized. The anonymity and confidentiality of participants' identities and responses were maintained.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Nonalcoholic fatty liver disease review: diagnosis, treatment, and outcomes. Ahmed A, Wong RJ, Harrison SA. Clin Gastroenterol Hepatol. 2015;13:2062–2070. doi: 10.1016/j.cgh.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 2.Pathogenesis of nonalcoholic steatohepatitis. Machado MV, Diehl AM. Gastroenterology. 2016;150:1769–1777. doi: 10.1053/j.gastro.2016.02.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Etiopathogenesis of nonalcoholic steatohepatitis. Chitturi S, Farrell GC. Semin Liver Dis. 2001;21:27–41. doi: 10.1055/s-2001-12927. [DOI] [PubMed] [Google Scholar]
- 4.Impaired mitochondrial function in microvesicular steatosis. Effects of drugs, ethanol, hormones and cytokines. Fromenty B, Pessayre D. J Hepatol. 1997;26:43–53. doi: 10.1016/s0168-8278(97)80496-5. [DOI] [PubMed] [Google Scholar]
- 5.Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. Pouwels S, Sakran N, Graham Y, et al. BMC Endocr Disord. 2022;22:63. doi: 10.1186/s12902-022-00980-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Dixon JB, Bhathal PS, O'Brien PE. Gastroenterology. 2001;121:91–100. doi: 10.1053/gast.2001.25540. [DOI] [PubMed] [Google Scholar]
- 7.The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. Hepatology. 2023;77:1335–1347. doi: 10.1097/HEP.0000000000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Changes in the global burden of chronic liver diseases from 2012 to 2017: the growing impact of NAFLD. Paik JM, Golabi P, Younossi Y, Mishra A, Younossi ZM. Hepatology. 2020;72:1605–1616. doi: 10.1002/hep.31173. [DOI] [PubMed] [Google Scholar]
- 9.Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Hepatology. 2018;67:123–133. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Wong RJ, Cheung R, Ahmed A. Hepatology. 2014;59:2188–2195. doi: 10.1002/hep.26986. [DOI] [PubMed] [Google Scholar]
- 11.Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Lin X, Xu Y, Pan X, et al. Sci Rep. 2020;10:14790. doi: 10.1038/s41598-020-71908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Components of metabolic syndrome increase the risk of mortality in nonalcoholic fatty liver disease (NAFLD) Golabi P, Otgonsuren M, de Avila L, Sayiner M, Rafiq N, Younossi ZM. Medicine (Baltimore) 2018;97:0. doi: 10.1097/MD.0000000000010214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prevalence, risk factors, and interventions for obesity in Saudi Arabia: a systematic review. Salem V, AlHusseini N, Abdul Razack HI, Naoum A, Sims OT, Alqahtani SA. Obes Rev. 2022;23:0. doi: 10.1111/obr.13448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prevalence of non-alcoholic fatty liver disease (NAFLD) in Saudi Arabia: systematic review and meta-analysis. Alenezi YM, Harris R, Morling J, Card T. Cureus. 2023;15:0. doi: 10.7759/cureus.40308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Poor awareness of liver disease among adults with NAFLD in the United States. Alqahtani SA, Paik JM, Biswas R, Arshad T, Henry L, Younossi ZM. Hepatol Commun. 2021;5:1833–1847. doi: 10.1002/hep4.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.A cross-sectional study of the public health response to non-alcoholic fatty liver disease in Europe. Lazarus JV, Ekstedt M, Marchesini G, et al. J Hepatol. 2020;72:14–24. doi: 10.1016/j.jhep.2019.08.027. [DOI] [PubMed] [Google Scholar]
- 17.Low awareness of nonalcoholic fatty liver disease in a population-based cohort sample: the CARDIA study. Cleveland ER, Ning H, Vos MB, et al. J Gen Intern Med. 2019;34:2772–2778. doi: 10.1007/s11606-019-05340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clinical and economic burden of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Younossi ZM, Henry L, Bush H, Mishra A. Clin Liver Dis. 2018;22:1–10. doi: 10.1016/j.cld.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Awareness of adult population toward non-alcoholic fatty liver disease in Riyadh, Saudi Arabia. Alsubaie A, Mohammad S, Alqarni A, et al. Int J Dev Ctries. 2020;1938:44. [Google Scholar]
- 20.Knowing what's out there: awareness of non-alcoholic fatty liver disease. Ghevariya V, Sandar N, Patel K, Ghevariya N, Shah R, Aron J, Anand S. Front Med (Lausanne) 2014;1:4. doi: 10.3389/fmed.2014.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Awareness, knowledge, and misperceptions related to nonalcoholic fatty liver disease in a community sample of Mexican-origin women: a mixed methods study. Morrill KE, Crocker RM, Hingle MD, Thomson CA, Garcia DO. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.626428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Awareness of non-alcoholic fatty liver disease is low in the general population of Saudi Arabia. Aljahdli ES, Fallatah HI, Alharbi AS, Alwagdani S, Makin M. Int J Med Dev Ctries. 2021;5:899–905. [Google Scholar]
- 23.Perceptions of non-alcoholic fatty liver disease - an Asian community-based study. Goh GB, Kwan C, Lim SY, et al. Gastroenterol Rep (Oxf) 2016;4:131–135. doi: 10.1093/gastro/gov047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Public awareness and knowledge of liver health and diseases in Singapore. Tan CK, Goh GB, Youn J, Yu JC, Singh S. J Gastroenterol Hepatol. 2021;36:2292–2302. doi: 10.1111/jgh.15496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liver diseases in South Korea: a pulse check of the public’s knowledge, awareness, and behaviors. Lee HW, Kim M, Youn J, Singh S, Ahn SH. Yonsei Med J. 2022;63:1088–1098. doi: 10.3349/ymj.2022.0332. [DOI] [PMC free article] [PubMed] [Google Scholar]