Abstract
Poor sleep during adolescence is a public health concern that may be especially important to address among youth in juvenile correctional facilities, who tend to experience greater mental health challenges, substance use disorders, and traumatic stress exposure. However, evidence for addressing sleep in correctional settings is limited. Using de-identified composite clinical cases, this paper describes challenges and opportunities for addressing sleep disorders (i.e. insomnia) and promoting sleep health (i.e. improving duration, regularity, and behaviors) among adolescents in long-term juvenile correctional facilities. These clinical cases highlight common presenting problems and underscore the need for integrated sleep and mental health interventions as well as adaptations to enhance feasibility and efficacy of behavioral sleep treatment and sleep health promotion in juvenile correctional contexts. We conclude by summarizing clinical, research, and policy implications for addressing adolescent sleep problems and promoting sleep health and well-being in these contexts.
Keywords: adolescent, behavioral interventions, circadian rhythm sleep–wake disorders, insomnia, juvenile correctional facilities, substance use, trauma
Statement of Significance.
Adolescents living in correctional facilities are at increased risk for sleep disorders and poor sleep health due to intrinsic (e.g. mental health challenges and traumatic stress exposure) and environmental factors (e.g. overnight checks, time in isolation, and legal and family separation-related stress). Sleep is modifiable and linked to overall well-being, yet very little research exists on the extent and evidence-based management of sleep disorders among adolescents residing in correctional facilities. To begin to address these knowledge gaps, this paper presents clinical case examples highlighting the need for integrated sleep and mental health treatments, as well as broader clinical practice, research, and policy changes, to effectively address sleep disorders and promote sleep health among youth in long-term correctional settings.
Introduction
On any given day, more than 30 000 youth sleep in juvenile detention or long-term correctional facilities [1]. Attention to the poor sleeping conditions in juvenile correctional facilities has been an ongoing concern with the need for more research and evidence-based approaches to support overall youth health and well-being [2]. Poor sleep health (e.g. short sleep duration and irregular/variable timing) [3] has been identified as a public health concern, particularly during adolescence [4–6]. Adolescents are at increased risk for poor sleep health due to a combination of biological, social, and environmental changes during this developmental period. Biologically, a delay in circadian timing and slowing of homeostatic sleep pressure occur with puberty, making it challenging to adhere to school start times that are too early for adolescents to obtain sufficient sleep [6, 7]. Social and environmental factors, such as greater involvement in school and/or extracurricular activities, as well as increased independence around sleep routines, bedtime, and electronics usage, contribute to poor adolescent sleep health [6, 7].
Indeed, according to the Centers for Disease Control, more than 50% of middle and high school students in the United States obtain insufficient sleep on school nights [8], or less than the 8–10 hours per day recommended for adolescents [9]. In addition, up to 40% of youth experience symptoms of insomnia (i.e. difficulty falling/staying asleep) and circadian rhythm sleep–wake phase disorders (i.e. delayed or irregular sleep schedules and daytime sleepiness) [4, 8, 10]. Addressing poor sleep health and sleep disorders in adolescents is crucial for promoting optimal psychosocial development. For example, insufficient sleep and variable sleep timing are associated with emotional dysregulation, worsening mental health symptoms [11, 12], substance use [5], and cardiometabolic problems, including obesity, hypertension, and diabetes [13]. Adolescent insomnia symptoms have additionally been linked bidirectionally with life stress and mood concerns [14], while sleep disturbances are prospectively associated with adolescent suicidal thoughts and behaviors [15, 16]. There is also evidence for bidirectional associations between short sleep duration and risk-taking and/or delinquent behaviors in adolescents [17, 18], which could further increase risk of youth incarceration.
Given the linkages between sleep and overall well-being, poor sleep health and sleep disorders may be particularly important to consider when treating youth in juvenile correctional facilities. Compared to the general population, incarcerated youth are more likely to experience mental health symptoms, substance use disorders, physical health concerns, and stressful life events [19], which can increase risk for insomnia and poor sleep health [6, 7, 14]. Epidemiologic data suggest that about 70% of incarcerated youth have at least one psychiatric disorder [20, 21], almost half meet criteria for a substance use disorder, and up to 75% may have co-occurring psychiatric disorders [22]. Unfortunately, the sleep needs of youth in alternative care settings have been largely ignored in the scientific literature, with limited information about the prevalence, assessment, and management of sleep difficulties among youth in juvenile correctional facilities.
Recently, two small studies [23, 24] described poor adolescent sleep health, insomnia symptoms, and circadian dysregulation in correctional settings, as well as sleep-disrupting environmental features of these facilities (e.g. light and noise), underscoring the need to improve youth sleep in these contexts. A 2019 National Commission on Correctional Health Care Policy Statement on Adolescent Sleep Hygiene [2] also highlights the clinical, systemic, and policy changes needed to effectively promote sleep health among incarcerated youth. Overall, however, limited guidance exists to support clinicians can incorporate evidence-based practices into the care of incarcerated youth given the significant systemic challenges that exist in these facilities [25].
The overall goal of this paper is to describe challenges and opportunities for treating sleep disorders and improving sleep health among adolescents in juvenile correctional facilities. This manuscript draws upon available research as well as the authors’ direct clinical experiences treating adolescent sleep and traumatic stress (ARD, LRF, SH, SZ, and AAW) including among youth in long-term correctional facilities, where authors and adolescent psychiatrists BRR and JS have worked for over 10 years. To stimulate future treatment research and support practicing clinicians, this manuscript is organized around de-identified, composite clinical case examples that highlight common presenting sleep concerns among youth in correctional settings. Throughout the case discussions, we reference relevant research on psychosocial and psychotropic interventions to address adolescent sleep disorders and promote sleep health. We conclude by discussing challenges and potential clinical practice, research, and policy-level opportunities to improve youth sleep in juvenile correctional facilities.
Case Examples
Clinical context
The following cases are drawn from clinical practice (BRR and JS) in a long-term, residential, therapeutic program for post-adjudicated youth. Treatment in this program is focused on rehabilitation and informed by dialectical behavioral therapy (DBT) [26] principles. The treatment program includes individual, group, and family therapy. Length of stay ranges between 5 and 10 months and most of the adolescents present with high rates of trauma and adverse childhood experiences (ACEs). The program’s patient population is comprised of mostly black, Latino, or Indigenous youth with multiple layers of added sociopolitical stress, including racism, poverty, and more frequent community violence exposure, consistent with the experiences of most legal system-impacted youth in the United States. [27–30]. Overrepresentation of black, Latino, and Indigenous youth in the juvenile legal system is well documented and national efforts to mitigate disproportionate contact have been in place for over three decades [31].
Youth in this program typically go into their rooms at 9 pm and are expected to be asleep at 10 pm. The wake time is set at 6 am and followed by hygiene and breakfast. Some independent time in their room is available outside of programming, usually in the afternoon, which may provide opportunities for youth to nap. However, it is important to note that an individual sleep space may not always be available to youth in correctional settings. According to findings from a survey of youth in residential placement, while 36% of the youth sleep in a private room, most youth must share their room with one or more residents. Up to 17% of youth may sleep in a room with 10 or more residents [32].
All youth are screened for mental health needs in detention and then again when they are transferred to the long-term correctional facility. Youth may raise concerns about their sleep at any point during their stay, which may prompt their therapist to refer them for a full psychiatric evaluation, which includes reviewing prior sleep practices, screening for sleep disorders, and administration of the Epworth Sleepiness Scale [33] for measurement of general level of daytime sleepiness. Furthermore, sleep logs are completed by correctional staff for 5–7 days to record sleep onset, middle-of-the-night awakenings, and daytime naps.
Factors impacting adolescent sleep before, during, and after incarceration
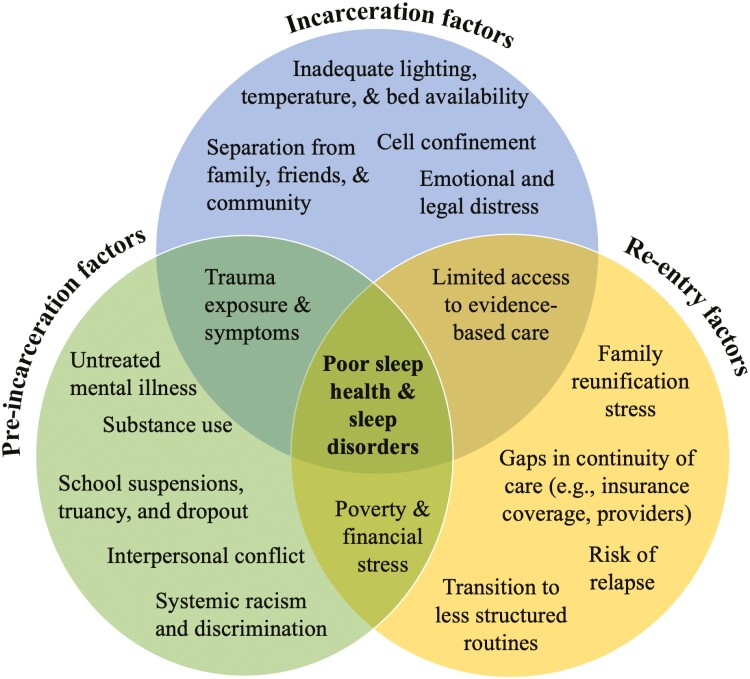
Many intrinsic and environmental factors likely impact the etiology and maintenance of sleep disorders and/or poor sleep health among adolescents living in long- and short-term correctional facilities. Figure 1 depicts the factors at multiple socio-ecological [34] levels (i.e. in the adolescent’s home, school, correctional setting, and neighborhood) that may impact adolescent sleep before, during, and after incarceration. As described in the following clinical cases, prior to incarceration, youth in correctional settings may have experienced interrelated factors, such as poverty, housing instability, interpersonal conflict at home and school, and trauma and mental health concerns, all of which can contribute to poor sleep health (e.g. inconsistent or irregular bedtimes, insufficient sleep) and behavioral sleep disorder symptoms (e.g. difficulty falling/staying sleep) [18, 35–39].
Figure 1.
Socio-ecological factors contributing to poor sleep health and sleep disorders in adolescents at pre-incarceration, during incarceration, and at reentry
Many of these factors, particularly trauma and mental health concerns [38, 40], may continue to impact adolescent sleep upon transition to a correctional facility. Incarceration factors (Figure 1), including lack of access to previously used coping and/or sleep-promoting strategies, such as substances [41] and/or technology devices [42], may exacerbate existing insomnia symptoms or circadian rhythm dysregulation [23]. Some may also experience well-founded distress related to family safety or age-appropriate preoccupation about missing out on major milestones at home, such as birthdays, birth of their children, death of a grandparent, etc. Furthermore, ongoing legal or custodial stressors may ebb and flow throughout their stay and contribute to nighttime ruminations and stressors. These include distress about their existing charges, upcoming court dates, program extensions (including additional charges, lack of progress/investment in treatment plan, familial disengagement), and child protective custody involvement. Thus, youth may find it particularly difficult to tolerate quiet time when in correctional settings, especially when they are not used to a quiet environment that may naturally promote self-reflection of worries and fears in the context of stressful environments (i.e. incarceration).
Physical aspects of incarceration may additionally disrupt or worsen adolescent sleep in these contexts (Figure 1). Youth may also struggle with comfort as living spaces (e.g. individual or group cells) are not the same as home with limited freedom and flexibility, lack of temperature control, difference in bedding and sheets, and low access to healthy coping mechanisms such as going for a walk, unrestricted outdoor activity or friendships. Lack of control over ambient noise or light from peers and staff may further affect sleep [23]. These factors may be further amplified when placed in seclusion (e.g. solitary confinement), another unique circumstance in the carceral system. When youth are physically aggressive or are significantly out of adherence with programming, they may be placed in seclusion where, for safety purposes, there is no furniture. The only place they may rest is on a concrete platform. There are often no windows or exposure to external light–dark cues coupled together with no scheduled, structured programming while they are in their cells, which could significantly exacerbate insomnia symptoms and contribute to circadian rhythm dysregulation. As seclusion practices can also adversely affect psychological and physical health and even increase the risk of death in youth, reducing seclusion in correctional settings has been a priority for over a decade [43].
Factors influencing sleep before and during incarceration must be taken into consideration when providing care for sleep difficulties in correctional settings and when planning for discharge/reentry. Potential factors that could worsen or maintain poor sleep health and/or sleep disorders during the reentry process are shown in Figure 1. Although these factors have yet to be studied in relation to adolescent sleep, available research indicates these factors are linked to worse youth mental health and risk of recidivism after reentry [44], which theoretically may impact sleep [17, 18]. reentry factors may include family reunification stress [45], less structured routines, gaps in continuity of care (e.g. insurance coverage and provider changes), and limited access to evidence-based mental health care more broadly [27, 32], the latter of which is also relevant during incarceration [25]. We further describe pre-incarceration, incarceration-related, and reentry factors in the context of each case, as well as relevant treatment considerations.
Case example 1
Justin is a 17-year-old cisgender male who presented with difficulty initiating sleep. He spent about 5 months in pretrial detention before being evaluated by the psychiatry team at a long-term post-adjudication program which offers individual sleeping rooms. He initially reported that his sleep concerns began upon admission to the detention center, however, upon further assessment, he reported that he has experienced problems with sleep onset and maintenance “since [he] can remember,” eventually developing a sleep pattern of staying up until 3 am and waking up “whenever,” which usually ranged from noon to 3 pm. He tried melatonin and Trazodone prior to detainment with initial improvement in sleep onset, but both medications eventually stopped working after a few weeks.
While in detention he reported that he would lay down at 9 pm when all youth are required to go into their rooms. He stated that would lay down in bed soon after going into his room to get extra sleep, even though he was not yet tired. He estimated that it took him 3–4 hours to fall asleep. He reported that he did not like being alone with his thoughts, as he often felt guilt for how his situation had impacted his family. He endorsed irritability, particularly when he felt disrespected by others, whether by peers, and adults. These feelings would last for an hour, and he believed that if he were more rested, he would not have as much difficulty tolerating them. On review of symptoms, he denied mania, depression, or anxiety symptoms. He had witnessed several community violence events and reported intermittent intrusive reminders though he denied further post-traumatic stress disorder (PTSD) symptoms, including nightmares. He denied taking long naps but does tend to go into his room and nap almost daily, typically falling asleep at least a few times per week.
Case conceptualization.
This clinical case represents a very common presentation among youth in this long-term residential correctional setting, who tend to experience mental health symptoms co-occurring with transdiagnostic sleep challenges, including insomnia symptoms (i.e. prolonged sleep onset latency), and a delayed circadian rhythm, especially during the transition into the correctional placement. Clinical care requires a careful balance of acknowledging the patient’s more acute sleep concerns while also evaluating and attending to the chronicity of their sleep disturbances. Contextualizing current sleep issues within longer-term struggles can empower youth to understand that addressing their concerns will require a comprehensive approach that accounts for the different layers and complexities of their lives.
Relevant to Justin’s case, significant unstructured time and a delayed sleep phase prior to admission likely contributed to his prolonged sleep onset latency, while his history of trauma exposure and guilt over his admission to a detention center may have led to worsening bedtime hyperarousal and more severe insomnia symptoms. As in Justin’s case, many youth report nighttime ruminations and traumatic memories during independent evening time, which may, in turn, trigger physical and emotional dysregulation that impacts sleep [40]. Even when youth do not meet full PTSD criteria, traumatic stress symptoms may hamper their perceived safety and ability to regulate their emotions and impulse control [46, 47], disrupting sleep.
Additional individual and environmental factors during incarceration may have contributed to Justin’s sleep concerns. In our clinical practice, youth tend to nap outside of programming due to boredom or avoidance (i.e. chaotic unit environment, interpersonal conflict, emotional dysregulation, and fear of behavioral outbursts resulting in sanctions), or, as in Justin’s case, due to daytime sleepiness following short overnight sleep duration. Preferences and expectations such as the desire to fall asleep within minutes of laying down, disliking middle of the night awakenings despite immediate return to sleep, the impact of daytime sleepiness on mood and cognition and lack of awareness about the impact of naps and other factors on nighttime sleep can result in inconsistent subjective report of sleep–wake times compared to staff-reported sleep logs [23, 24]. This inconsistency can ignite tension or disagreement between youth and clinical staff regarding the need for medications. Data collection via sleep log may also disrupt sleep when lights shine into rooms during security checks [23].
Treatment considerations.
In Justin’s case, his assessment revealed a discrepancy between his reported prolonged sleep onset latency and staff-identified fall-asleep time, which was noted to be closer to lights out. This often occurs in clinical practice and may require sleep logs to be documented by both youth and staff, in line with guidance on including multiple reporters (e.g. caregiver and youth) when evaluating behavioral sleep problems [48]. Nonetheless, his reported symptoms of negative bedtime emotions and a prolonged sleep onset latency were consistent with insomnia disorder. As described above, a history of a delayed sleep phase and traumatic experiences likely played a role in the manifestation of these symptoms.
Although elements from Cognitive Behavioral Therapy for Insomnia (CBT-I) could be useful, such as stimulus control and sleep restriction or compression [48, 49], aspects of correctional facilities limit the feasibility of these strategies. There is little personal space in cells, and youth have few alternative locations where they might be able to engage in stimulus control activities. In our practice, some youth cite reluctance to read out of bed due to inadequate back support in the swivel stools in their rooms. Other youth may not be allowed to have any extra items (i.e. books and journals) to help them stay busy if they are not sleepy, due to safety concerns. Sleep restriction or compression is also challenging without many options for remaining out of bed, as all overhead lights are typically turned off at bedtime. Furthermore, once youth do fall asleep they may awake due to loud noises (i.e. doors locking) or light exposure [23].
For Justin’s case, it was important to incorporate psychoeducation about the impact of trauma on mental health and sleep, as well as validation of his current subjective experience of insomnia symptoms and the accompanying challenges. Validation is an important and, in our perspective, an underutilized tool in children’s mental health. Invalidation of subjective symptoms will likely result in lower patient-clinician rapport. In addition, treatment included selected behavioral techniques, such as restricting daytime naps and remaining out of bed at bedtime as much as was allowed until he was sleepy, to address his insomnia symptoms and circadian rhythm delays. Justin was also asked to engage in relaxation strategies once he was sleepy enough to get in bed, and to practice these strategies during the day to facilitate generalization. His treatment included ongoing collaboration with his therapist to monitor and adjust his sleep schedule in the context of addressing other psychosocial needs. Of note, even when clinicians and youth collaborate in implementing a plan to address sleep problems, there may be implementation challenges. Such challenges include high staff turnover, consistent short-staffing, and the use of a correctional rather than therapeutic approach to caring for youth, and few mental health clinicians available to oversee sleep plan implementation. Justin’s care required collaboration with facilities staff to ensure he could remain out of bed until sleepy and avoid naps during the day to increase sleep pressure at bedtime.
Justin did not always express agreement with this treatment plan and often dismissed the use of behavioral and relaxation techniques. However, with a consistent approach from his psychiatrist, therapist, and correctional staff, he eventually embraced these practices. His therapist also worked on strengthening his ability to practice DBT-based concepts [26], as this is the therapeutic approach used across the correctional facility, including acceptance of developmentally and contextually expected sleep difficulties and reducing cognitive distortions impacting his sleep. Eventually, his bedtime hyperarousal and sleep onset latency improved, and he was able to maintain an earlier, more consistent sleep schedule. Overall, this was accomplished through the combination of psychoeducation, validation of current struggles and past experiences, selected behavioral sleep techniques, and providing support around acceptance.
Clinical case example 2
Mercedes is a 14-year-old cisgender female who presented with irritability and depressed mood. Pertinent social history includes victimization in sex trafficking, a highly traumatic experience for youth [50]. Both before and after victimization, Mercedes also experienced intermittent houselessness, and was “couch surfing” at different friends’ homes, which impacted her sleep. She spent over 6 months in juvenile detention prior to being transferred to the long-term correctional treatment center. Her difficulties with sleep began years prior to her current incarceration, and she would often use cannabis or benzodiazepines to try to “relax,” clear her mind, and fall asleep. She reported that she stays busy to cope with distressful feelings during the daytime, avoiding quiet or alone times. In addition to serving her time in the forensic residential program, she has been participating in forensic interviews with authorities and other preparatory activities as she may need to testify in court, possibly against one of her perpetrators. She endorsed frequent reeexperiencing symptoms, including nightmares, hypervigilance, significant psychological distress with reminders of trauma, and a negative view of the world and her future. Nighttime is particularly difficult as she would ruminate about the trauma and the impending legal proceedings, along with other stressors. During her time in the correctional facility, she typically fell asleep by 11 pm, but reported a high level of discomfort for 30–60 minutes prior to falling asleep. Mercedes indicated that she would like to fall asleep as quickly as possible. She also hoped to receive a sleep medication, and did not believe any other medications were needed. She reported being open to meeting with a therapist but indicated that she did not want to share details about her nightmares and prior victimization experiences.
Case conceptualization.
This case exemplifies a common clinical scenario we see in juvenile correctional facilities, which is that some youth do not wish to initiate first-line medications, in this case, an anti-depressant to treat PTSD, even when symptoms are clinically elevated and impacting both their sleep and daily functioning. Psychiatric medication hesitancy and/or refusal may arise from personal belief about mental illness and medications or parental disagreement about the youth’s mental health treatment needs. As in the case of Mercedes, youth may also be more comfortable using sedating substances to help them sleep [41], which could make them more open to using sleep medications rather than those intended to treat mental health concerns.
Prior to incarceration, Mercedes experienced a significant number of ACEs, including sex trafficking, that impacts mental health and are associated with risk of further victimization, adolescent delinquency, and increased sleep disorder symptoms [38, 50, 51]. With higher ACEs than the general population, youth impacted by the legal system require comprehensive mental health interventions that are not always accessible in correctional settings. Relevant to Mercedes, nightmares, shorter and more frequent rapid eye movement sleep periods, and overall poorer sleep quality have been linked with exposure to trauma or a diagnosis of PTSD [52, 53]. Evidence suggests that sleep abnormalities may precede the development of PTSD or even predict its development or severity [54].
Before incarceration, Mercedes also consumed cannabis to cope with her trauma-related sleep disturbances, which may have contributed to worsening sleep when she transitioned to detention. Cannabis withdrawal is known to exacerbate mood symptoms, while cannabis cessation or acute involuntary abstinence can worsen sleep quality [55]. Cannabis is the most widely used recreational drug among adolescents with 37% of US high school students reporting lifetime use of cannabis and 22% having used it in the past month [56]. Many individuals use cannabis to improve their mood and sleep; however, its effects tend to be short-term. Chronic cannabis use has been shown to worsen mental health symptoms and can result in higher rates of affective and psychotic disorders [57].
In addition to these pre-incarceration and incarceration transition-related factors, Mercedes’ experience of preparing for possible testimony against her abuser was a significant source of stress during incarceration. This preparation likely heightened her overall emotional and psychological distress. As a result, she may have had increased traumatic reeexperiencing and nightmares, contributing to her hyperarousal and prolonged sleep onset latency at bedtime.
Treatment considerations.
Mercedes’ case reflects insomnia due to her underlying untreated PTSD, as her trauma symptoms and nightmares likely significantly contribute to her hyperarousal at bedtime and prolonged sleep onset latency. Trauma-focused psychotherapies are the first-line treatment for adolescent PTSD. Trauma-focused cognitive behavioral therapy (TF-CBT) is the most studied, with some evidence that this approach improves nightmares in adolescents with PTSD [58]. TF-CBT has also been adapted to address the needs of commercially sexually exploited youth [59], while therapist implementation strategies and outcomes among adjudicated youth have been evaluated in residential treatment facilities [60]. Despite evidence of effectiveness, treatment response varies [61], and some intrusive symptoms may fail to improve especially when co-occurring with substance use disorders, and exposure to ongoing dysregulating environments and situations [62]. In addition, implementing trauma-focused therapies in youth correctional facilities is challenging for a variety of reasons. Logistically, a high staff turnover rate makes it difficult to maintain a well-trained clinician base, although web-based training is available [59]. Importantly, treating trauma during a potentially traumatizing condition (incarceration and court proceedings) poses a greater challenge. Youth in correctional settings are at high risk of experiencing abuse during incarceration [63]. Trauma-focused therapies require a high level of therapeutic alliance between therapist and client, which can be difficult to foster with clinicians working in a system not generally trusted by youth and families.
As sleep concerns are Mercedes’ identified treatment priority, we would recommend considering treatment with prazosin to improve her PTSD-related nightmares and to promote rapport-building trust, while also engaging her in collaborative, patient-centered approaches to address her sleep and mental health symptoms. Small studies and case reports support the use of prazosin (dose range 1–15 mg at bedtime) [64, 65] along with TF-CBT [66], although the American Academy of Sleep Medicine recently downgraded their prazosin recommendations due to negative studies in adults [67]. Unfortunately, given the limited options available for treatment, and lack of placebo trials in this unique age group [64, 65], it may be an option to consider.
Initially offering psychoeducation to Mercedes about the impacts of trauma on her mental health and sleep could also help build rapport until Mercedes is ready to address her PTSD symptoms through TF-CBT. During treatment, her therapist must be aware of the additional stressors related to legal procedures and should consider offering supportive sessions before and after any court hearings. In addition, collaborating with other clinicians and correctional staff to implement trauma-informed care, particularly during potentially re-traumatizing court proceedings, could also help engage Mercedes in treatment. Education regarding the use of cannabis to self-medicate these symptoms is another priority along with connecting Mercedes to substance use treatment and support, especially after discharge for relapse prevention. Communicating these strategies and information to her caregivers is of utmost importance so they can support her ongoing healing in the community.
To further address Mercedes’ sleep and in anticipation of subsequent TF-CBT treatment, her therapist could incorporate approaches from CBT-I (e.g. sleep restriction or compression) which have been found to benefit adult PSTD symptoms [68]. However, little guidance exists around when and how to adapt CBT-I [69] for adolescents in correctional settings, as previously discussed in the context of Justin’s case. An additional consideration would be imagery rehearsal therapy, which has been found to reduce PTSD-related nightmares in adolescents [70], with one study examining this approach among adjudicated youth [71]. This approach may not be possible in the context of Mercedes’ low perceived safety while incarcerated, ongoing stress, and possible re-traumatization with court proceedings. When treating cases like Mercedes, who have extensive trauma histories and multiple incarcerations, clinicians must be able to support youths’ ability to develop and utilize practices that are internally accessible to them, which may also benefit sleep.
In working with cases similar to that of Mercedes and Justin, author B.R.R. has taken an approach informed by both DBT [26] and evidence-based behavioral sleep strategies [48, 49, 72] to support youths’ distress tolerance and ability to regulate their emotions, particularly in the evening. This approach involves creating a nightly, five-step bedtime routine with strategies to promote feelings of safety, regulate strong emotions, and create more positive associations with bedtime. Given these youths’ experiences of stress, racism, family separation, and other sleep-disrupting factors, strategies should promote cultural pride and connection to their communities outside of the correctional setting. Ideally, a total of five steps or strategies are selected, with youth using their own hands and fingers to map out a plan, to ensure youth can recall the plan without any written materials, which are often not allowed in their rooms.
Table 1 provides an example of this five-step routine implemented with youth in long-term correctional facilities. Clinicians in practice could use this routine in conjunction with psychoeducation to promote sleep health, or could pair it with additional behavioral strategies, such as sleep restriction or compression, to address youth with insomnia symptoms. Although this approach has not been studied, it provides an example of how some evidence-based strategies for both mental health and sleep problems could be adapted and integrated in this context. Clinical use of this approach demonstrates that youth tend to be responsive to these conversations during psychiatric visits, and other clinical staff can then follow up on the plan, progress and support adjustments to continue building sleep promotion.
Table 1.
Example Five-step Bedtime Routine Informed by DBT and Evidence-Based Sleep Health Promotion Strategies to Support Youth Sleeping in Long-Term Correctional Facilities
| Step number and activity | Links to evidence-based strategies | Additional clinical considerations |
|---|---|---|
| 1. Youth are invited to observe how their body feels upon entering their room at night. They are instructed to consider a brief movement-based practice to relieve any remaining tension or inner discomfort. Movement practices offered can include physical activity such as jumping jacks, jump rope, and squats or dance. 2. Youth are guided to incorporate stretches or yoga-like movements paired with deep breathing to help their physical bodies begin to slow down cardiovascular activity and physical hyperarousal. 3. Youth are invited to engage in a cognitive- and emotion-based processing activity, which can include journaling, coloring, drawing, or writing songs. 4. Youth are invited to use mindfulness-based activities or other strategies to promote relaxation (e.g., humming their favorite lullaby/song, praying, or visualizing a positive and safe experience). 5. Youth are encouraged to begin breathing practices to support their transition to sleep. |
• Positive bedtime/wind-down routine can benefit sleep [72, 73]. • Use of mindfulness and physical activity can distress tolerance and emotion regulation [26]. • Cognitive and emotional processing and relaxation strategies can reduce hyperarousal [26, 48, 49]. |
• Youth on medications or medical conditions that could result in autonomic irregularities, such as clonidine, prazosin, or postural orthostatic tachycardia syndrome should be medically assessed before engaging in movement practices. • External tools (e.g. journals, pens, and pencils) may not be available to the youth. It may be necessary to work with youth to develop their own ideas for promoting reflection, emotional regulation, and positive emotions. • Practicing these skills in session can support youth engagement and buy-in to these practices. Clinicians can guide youth through progressive muscle relaxation or short breath practice, if skilled at doing so. |
Opportunities to Improve Sleep in Youth Correctional Facilities
As demonstrated in the clinical cases presented here, there is an urgent need to better address sleep in juvenile correctional and residential settings, as well as significant challenges in these contexts. Table 2 summarizes opportunities to address these challenges through clinical practice, research, and policy-level actions, which we describe further here.
Table 2.
Challenges, Opportunities, and Implications for Improving Sleep Among Youth in Juvenile Correctional Facilities
| Challenges | Clinical and research opportunities | Systems-level and policy implications |
|---|---|---|
| Inflexible bedtimes with sleep schedules that may be too early for adolescents | • Adjust sleep schedules to better align with adolescent circadian timing and homeostatic sleep pressure | • Advocate for guideline recommendations for juvenile correctional facilities management to include circadian timing information |
| Lack of sleep health promotion and access to evidence-based behavioral sleep treatments | • Design, implement, and evaluate easily accessible curriculums to support sleep health education in individual and group modalities for youth, families, and staff. • Promote youth-staff communication about available tools to support healthy sleep. • Adapt and evaluate behavioral sleep treatment programs for implementation in correctional facilities using participatory and health equity-informed methods. |
• Approach funders and other organizations to raise awareness about and increase funding mechanisms for sleep health promotion and intervention with justice-involved youth. |
| Lack of sleep training for correctional and residential facility staff | • Provide continuing education that includes assessment and promotion of sleep health. • Create facility-wide clinician workgroups to engage in case consultation and ensure that youths’ needs are addressed in evidence-based, culturally humble, and prevention-focused methods |
• Require sleep health training for all staff and clinicians in correctional facilities. • Advocate for state, national, and professional organization guidelines to guide systematic approaches to routine screening for sleep and sleep health promotion activities in correctional and residential facilities. |
| Overreliance on medication to address sleep disturbances | • Create consistency in the way that sleep disturbances are assessed, monitored, and treated. • Provide continuing education for physicians that focuses on evidence-based assessment and treatment of adolescent sleep disturbances. • Evaluate the integration of selected pharmacological and non-pharmacological approaches to treat sleep disturbances. |
• Establish national guidelines specific to both pharmacological and non-pharmacological methods to treat sleep and circadian challenges among youth with co-occurring sleep and mental health problems. |
| Impacts of co-occurring sleep and mental health problems, especially PTSD and substance use, both prior to and during correctional and residential placements. | • Identify, monitor, and treat co-occurring conditions that exacerbate sleep disturbance, including substance use withdrawal symptoms and their effects on sleep during correctional facility stay. • Provide psychoeducation to youth and clinicians about the impacts of recreational substance use to cope with sleep problems and offer alternative coping strategies. |
• Institute facility-wide, non-punitive, and trauma-informed longitudinal assessment of substance use history and withdrawal, and care of mental health conditions. • Increase training opportunities for clinical providers to build and advance expertise in adolescent sleep, mental health, and substance use treatment. • Integrate more Licensed Chemical Dependency Counselors into juvenile correctional and residential facilities. |
| Gaps in continuity of care and family engagement | • Inform youth, including families about the sleep and health practices used during incarceration to promote continuity. • Assess for social determinants of health that may impact youth’s ability to maintain learned healthy sleep behaviors upon discharge. • Communicate with outpatient services, providers, and primary care about discharge planning and continuity of care. |
• Implement policies and procedures that encourage family engagement and outpatient provider communication. |
| Seclusion and limited opportunities for sunlight and outdoor activity | • Provide opportunities for outdoor activities (preferred) or adequately timed lightboxes, even when there are no national requirements. • Adhere to guidance (e.g. First Act of 2018) on limiting the use of restrictive measures like seclusion. • Provide opportunities for exercise as regular practice and allow youth to use rooms to exercise if they need to, as some youth have higher needs for daily energy expenditure. |
• Promote policies requiring access to at least one hour of outdoor activity to promote overall physical, emotional, and sleep health. • Advocate for state and national guidelines that limit the use and length of seclusion. |
Identifying and addressing modifiable environmental determinants of sleep in juvenile correctional settings could both prevent the onset of sleep problems and promote overall sleep health. Importantly, instituting sustainable practices is crucial to address both clinical and systemic barriers. One approach is to implement routine sleep schedules and a structured environment that promote consistency but are more aligned with adolescent circadian rhythms [6, 7]. Although research evaluating the potential benefits of these and other environmental changes (e.g. minimizing noise from overnight checks) is needed, advocacy efforts could use guidance on later adolescent school start times from the American Academy of Pediatrics and other organizations [74] to support similar guideline development and changes in correctional facilities (e.g. waketimes no earlier than 8:30 am).
Providing access to evidence-based sleep health education could additionally empower adolescents to adopt healthy sleep practices even after they return home or to the community. Group-based sleep health education [75] for youth in correctional settings could also offer an opportunity to promote youth-staff communication about strategies that may be supportive and available to them. For example, youth may have accessible strategies that other youth could benefit from, such as dance, singing, or prayer. These strategies can be shared in the unit to promote collective health.
Cognitive and behavioral approaches are the first-line treatments for poor sleep health, insomnia, and circadian rhythm problems in youth, but have yet to be rigorously evaluated with adolescents in juvenile correctional facilities. Adapting and evaluating evidence-based treatments including group-based psychoeducation, CBT-I [49], IRT [70], and modularized approaches, such as the transdiagnostic intervention for sleep and circadian dysfunction [76] (TranS-C), are crucial steps for future research and case practice. Trans-C may be especially beneficial for justice-involved youth, as the intervention was designed to address various sleep and circadian problems that co-occur with mental health conditions, with evidence of effectiveness with adolescents [73]. Ideally, justice-involved adolescents, their families, and correctional facility staff and clinicians should be engaged as collaborators in treatment adaptation and evaluation research to ensure acceptability, appropriateness, and feasibility of these approaches [77].
Implementing behavioral approaches to treat sleep could also reduce overreliance on psychotropic medication in correctional settings. There are no Food and Drug Administration-approved medications for youth behavioral sleep disorders. While melatonin is often used due to generally accepted efficacy versus safety profile relative to other agents, it is not Food and Drug Administration-regulated, with variation in its strength and purity within and across brands [78]. Furthermore, studies in general adolescent populations are limited and absent in youth residing in correctional facilities [79]. Developing facility-wide guidelines about the use of medications, including melatonin, can create consistency among clinicians, staff, and youth regarding what to expect for the treatment of insomnia. Pairing these guidelines with the behavioral sleep strategies mentioned above can inform youth and staff about when medications may be used.
To support the integration of evidence-based sleep services in juvenile correctional settings, facilities should also consider integrating sleep screening tools [80] and questionnaires [81] into routine evaluations and when monitoring progress, particularly when treating co-occurring conditions such as PTSD and substance use. Continuing medical education focused on management of adolescent sleep and mental health disturbances should also be offered to clinicians in correctional settings, particularly as sleep medicine education is limited in most clinical training programs [82, 83]. Training clinical and correctional staff in socioemotional learning practices to promote stress management and overall well-being could also reduce interpersonal conflict between youth and staff around bed and wake times, creating more positive associations around sleep for youth. Avenues for making clinical and systems-level changes in correctional facilities to support these practices could include establishing clinician workgroups dedicated to case consultation and training around integrated sleep and mental health care (Table 1).
More broadly, youth in the carceral system must have access to evidence-based and trauma-informed mental health care. An overall lack of behavioral health clinicians and limited financial resources to support advanced sleep and mental health training are significant barriers that warrant future attention and advocacy efforts. Given the common co-occurring conditions in the case examples we presented, in addition to access to behavioral sleep treatment, access to trauma-focused therapies and interventions for substance use disorders may address underlying symptoms bidirectionally linked with sleep [84]. Licensed Chemical Dependency Counselors may be a critical resource in supporting these efforts as they can help youth identify and address the role that substance use plays in their lives. Staff at every level should receive training in trauma-informed care and restorative justice practices to improve facility climate.
Improving family engagement in the care of incarcerated youth is a national priority [63] that can benefit both sleep and mental health. Maintaining family and community connections can support youths’ transition into detention and placement [64]. Practices that improve family engagement and increase family-centered care can improve child safety, family or kin placements and help build the family’s problem-solving skills [65]. Effective treatments for adolescent trauma (e.g. TF-CBT) and substance use (e.g. multisystemic therapy, and functional family therapy) often involve family-based strategies or treatment of a caregiver or guardian in parallel [63], which may present logistical challenges for families of incarcerated youth. Efforts to engage family members in both treatment and discharge planning are necessary to support continuity of sleep and mental health care (Table 2).
Lastly, the impact of the use of punitive and restrictive measures in youth correctional settings on sleep and overall health and development must be taken into consideration. Seclusion not only impairs the youth’s ability to experience the daily social, emotional, and cognitive stimulation needed for healthy development, but it will also impair physical movement, daily routines, access to healthcare, among other factors that can impact their sleep. Clinicians should be aware that the First Step Act of 2018 prohibits solitary confinement of youth, except when used temporarily to mitigate behavior that may result in serious and immediate harm to others [85]. At the same time, there is substantial subjectivity in determination of what behavior requires seclusion and for how long [86]. There is also no national requirement for outdoor activity for youth in correctional facilities, but what is legal or legally required does not always clearly correlate with what is best for youths’ health. Although data are limited, exposure to sunlight and nature are both correlated with healthy sleep and mental health [66, 67]. Our clinical consensus is that youth in correctional facilities should have access to at least one hour of outdoor activity to promote overall physical and mental well-being.
Conclusions
Healthy sleep is important and foundational for caring for young people, especially incarcerated youth who have layers of vulnerability influencing their sleep. Promoting sleep health, addressing sleep disorders, and avoiding the misuse and/or overreliance on medications among justice-involved youth requires dedicated research, clinical practice, and policy-level changes. These changes are not easy to implement and require intentional support from institutional leadership to ensure that adequate resources (i.e. sleep and behavioral health training) and procedural changes are established to promote both clinical and correctional staff to implement and sustain these practices. State or even national policy changes that address basic human needs and adolescent development, such as requiring minimum outdoor activity and access to the least-restrictive treatment options may be areas of focus for clinician advocates treating this population. Collaboration with youth and families impacted by the legal system should also be considered as new practices and procedures are implemented. Ultimately, by recognizing and overcoming the barriers to sleep associated with juvenile correctional settings, we can work towards improving the health of adolescents. Perhaps most importantly, given the negative effects of incarceration on sleep and overall youth health and development, efforts to minimize rates and length of incarceration, and offer community-based, prevention, and family-centered approaches must continue to be prioritized.
Acknowledgments
We thank the adolescents in juvenile correctional and residential facilities that we have worked with, as well as their families. We also thank the clinical and correctional staff who care deeply about the youth they serve.
This paper is part of the Sleep and Circadian Health in the Justice System Collection.
The authors have no conflicts of interest to disclose. Portions of this work were presented by the authors at the 2021 American Psychiatric Association Annual Meeting (virtual).
Contributor Information
Barbara Robles-Ramamurthy, Department of Psychiatry and Behavioral Sciences, University of Texas Health San Antonio, San Antonio, TX, USA.
Saadia Zaki, Department of Psychiatry and Behavioral Sciences, University of Texas Health San Antonio, San Antonio, TX, USA.
Jessica F Sandoval, Department of Psychiatry and Behavioral Sciences, University of Texas Health San Antonio, San Antonio, TX, USA.
Anish R Dube, Department of Psychiatry, Charles R. Drew University College of Medicine and Science, Los Angeles, CA, USA.
Steven Hlozek, Department of Internal Medicine, University of Texas Health San Antonio, San Antonio, TX, USA.
Lisa R Fortuna, Department of Psychiatry and Neurosciences, University of California Riverside, School of Medicine, Riverside, CA, USA.
Ariel A Williamson, Ballmer Institute for Children’s Behavioral Health, University of Oregon, Portland, OR, USA.
Funding
None.
Author Contributions
Barbara Robles-Ramamurthy (Conceptualization [Lead], Data curation [Lead], Methodology [Lead], Resources [Lead], Supervision [Lead], Writing—original draft [Equal], Writing—review & editing [Equal]), Saadia Zaki (Conceptualization [Supporting], Data curation [Supporting], Writing—original draft [Supporting]), Jessica Sandoval (Conceptualization [Supporting], Methodology [Supporting], Writing—original draft [Supporting]), Anish Dube (Conceptualization [Supporting], Supervision [Supporting], Writing—review & editing [Supporting]), Steven Hlozek (Data curation [Supporting], Writing—original draft [Supporting]), Lisa Fortuna (Conceptualization [Equal], Supervision [Equal], Writing—original draft [Equal], Writing—review & editing [Equal]), and Ariel Williamson (Conceptualization [Equal], Resources [Equal], Writing—original draft [Equal], Writing—review & editing [Lead]).
Disclosure Statement
References
- 1. Puzzanchera C, Hockenberry S, and Sickmund, M.. Youth and the Juvenile Justice System: 2022 National Report. https://ojjdp.ojp.gov/library/publications/youth-and-juvenile-justice-system-2022-national-report. Accessed December 1, 2023,2022.
- 2. National Commission on Correctional Health Care. Position Statement: Adolescent Sleep Hygiene. https://www.ncchc.org/wp-content/uploads/Adolescent-Sleep-Hygiene-2019-1.pdf. Accessed September 23, 2023, 2019.
- 3. Meltzer LJ, Williamson AA, Mindell JA.. Pediatric sleep health: it matters, and so does how we define it. Sleep Med Rev. 2021;57:101425. doi: 10.1016/j.smrv.2021.101425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, Liao D, Bixler EO.. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep Med. 2014;15(1):91–95. doi: 10.1016/j.sleep.2013.08.787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Owens JA, Dearth-Wesley T, Lewin D, Gioia G, Whitaker RC.. Self-regulation and sleep duration, sleepiness, and chronotype in adolescents. Pediatrics. 2016;138(6):e20161406–e20161406. doi: 10.1542/peds.2016-1406 [DOI] [PubMed] [Google Scholar]
- 6. Carskadon MA. Sleep in adolescents: the perfect storm. Pediatr Clin North Am. 2011;58(3):637–647. doi: 10.1016/j.pcl.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crowley SJ, Wolfson AR, Tarokh L, Carskadon MA.. An update on adolescent sleep: new evidence informing the perfect storm model. J Adolesc. 2018;67:55–65. doi: 10.1016/j.adolescence.2018.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wheaton AG, Jones SE, Cooper AC, Croft JB.. Short sleep duration among middle school and high school students—United States, 2015. Morb Mortal Wkly Rep. 2018;67(3):85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. doi: 10.5664/jcsm.5866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Academy of Sleep Medicine. International Classification of Sleep Disorders, Third Edition- Text Revision. Darien, IL: American Academy of Sleep Medicine; 2023. [Google Scholar]
- 11. Clinkinbeard SS, Simi P, Evans MK, Anderson AL.. Sleep and delinquency: does the amount of sleep matter? J Youth Adolesc. 2011;40:916–930. doi: 10.1007/s10964-010-9594-6 [DOI] [PubMed] [Google Scholar]
- 12. Becker SP, Sidol CA, Van Dyk TR, Epstein JN, Beebe DW.. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: a systematic review. Sleep Med Rev. 2017;34:94–121. doi: 10.1016/j.smrv.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Matricciani L, Paquet C, Galland B, Short M, Olds T.. Children’s sleep and health: a meta-review. Sleep Med Rev. 2019;46:136–150. doi: 10.1016/j.smrv.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 14. Yang Y, Liu X, Liu Z-Z, Tein J-Y, Jia C-X.. Life stress, insomnia, and anxiety/depressive symptoms in adolescents: a three-wave longitudinal study. J Affect Disord. 2023;322:91–98. doi: 10.1016/j.jad.2022.11.002 [DOI] [PubMed] [Google Scholar]
- 15. Bernert R, Horn M, Iwata N, Joiner T.. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudianl evaluation of young adults at high suicide risk. J Clin Psychiatry. 2017;78(6):e678–e687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Goldstein TR, Bridge JA, Brent DA.. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76(1):84–91. doi: 10.1037/0022-006X.76.1.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Short MA, Weber N.. Sleep duration and risk-taking in adolescents: a systematic review and meta-analysis. Sleep Med Rev. 2018;41:185–196. doi: 10.1016/j.smrv.2018.03.006 [DOI] [PubMed] [Google Scholar]
- 18. Kim J, Son H.. Adolescent delinquent behavior and sleep deficiency: a test of multiple mechanisms using sibling comparison designs. Eur Child Adolesc Psychiatry. 2023;32(1):167–176. doi: 10.1007/s00787-022-02054-y [DOI] [PubMed] [Google Scholar]
- 19. Dewa LH, Hassan L, Shaw JJ, Senior J.. Trouble sleeping inside: a cross-sectional study of the prevalence and associated risk factors of insomnia in adult prison populations in England. Sleep Med. 2017;32:129–136. doi: 10.1016/j.sleep.2016.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Colins O, Vermeiren R, Vreugdenhil C, van den Brink W, Doreleijers T, Broekaert E.. Psychiatric disorders in detained male adolescents: a systematic literature review. Can J Psychiat. 2010;55(4):255–263. doi: 10.1177/070674371005500409 [DOI] [PubMed] [Google Scholar]
- 21. Underwood LA, Washington A.. Mental illness and juvenile offenders. Int J Environ Res Public Health. 2016;13(2):228. doi: 10.3390/ijerph13020228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA.. Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry. 2002;59(12):1133–1143. doi: 10.1001/archpsyc.59.12.1133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adornetti JP, Woodard KN, Nogales JM, et al. Sleep and circadian health in juvenile justice systems: a descriptive analysis. Sleep Health. 2023;9(6):876–881. doi: 10.1016/j.sleh.2023.08.009 [DOI] [PubMed] [Google Scholar]
- 24. Levenson JC, London S, Ekas D, et al. Sleep among Adolescents in Juvenile Detention. Sleep. 2022;45.A218. [Google Scholar]
- 25. Blackaby J, Byrne J, Bellass S, Canvin K, Foy R.. Interventions to improve the implementation of evidence-based healthcare in prisons: a scoping review. Health Justice. 2023;11(1):1–12. doi: 10.1186/s40352-022-00200-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Linehan MM, Wilks CR.. The course and evolution of dialectical behavior therapy. Am J Psychother. 2015;69(2):97–110. doi: 10.1176/appi.psychotherapy.2015.69.2.97 [DOI] [PubMed] [Google Scholar]
- 27. Anoshiravani A. Addressing the unmet health needs of justice system-involved youth. Lancet Public Health. 2020;5(2):e83. doi: 10.1016/S2468-2667(19)30251-8 [DOI] [PubMed] [Google Scholar]
- 28. Borschmann R, Janca E, Carter A, et al. The health of adolescents in detention: a global scoping review. Lancet Public Health. 2020;5(2):e114–e126. doi: 10.1016/S2468-2667(19)30217-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jones MS, Pierce H.. Early exposure to adverse childhood experiences and youth delinquent behavior in fragile families. Youth Soc. 2021;53(5):841–867. doi: 10.1177/0044118x20908759 [DOI] [Google Scholar]
- 30. Lacey C. Racial Disparities and the Juvenile Justice System: A Legacy of Trauma.. National Center for Child Traumatic Stress. 2013. https://www.nctsn.org/sites/default/files/resources//racial_disparities_and_juvenile_justice_system_legacy_of_trauma.pdf. Accessed April 14, 2023.
- 31. Robles-Ramamurthy B, Watson C.. Examining racial disparities in juvenile justice. J Am Acad Psychiatry Law. 2019;47(1):48–52. doi: 10.29158/JAAPL.003828-19 [DOI] [PubMed] [Google Scholar]
- 32. Sedlak A, McPherson KS.. Survey of Youth in Residential Placement: Youth’s Needs and Services., MD: Westat; Rockville; 2010. [Google Scholar]
- 33. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540 [DOI] [PubMed] [Google Scholar]
- 34. Bronfenbrenner U. Ecological Systems Theory. London, UK: Jessica Kingsley Publishers; 1992. [Google Scholar]
- 35. Ireland JL, Culpin V.. The relationship between sleeping problems and aggression, anger, and impulsivity in a population of juvenile and young offenders. J Adolesc Health. 2006;38(6):649–655. doi: 10.1016/j.jadohealth.2005.05.027 [DOI] [PubMed] [Google Scholar]
- 36. Bagley EJ, Kelly RJ, Buckhalt JA, El-Sheikh M.. What keeps low-ses children from sleeping well: the role of presleep worries and sleep environment. Sleep Med. 2015;16(4):496–502. doi: 10.1016/j.sleep.2014.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Black LI, Zablotsky B.. Chronic school absenteeism among children with selected developmental disabilities: national health interview survey, 2014-2016. National Health Statistics Reports. Natl Health Stat Report. 2018;118:1–7. [PubMed] [Google Scholar]
- 38. Brown SM, Rodriguez KE, Smith AD, Ricker A, Williamson AA.. Associations between childhood maltreatment and behavioral sleep disturbances across the lifespan: a systematic review. Sleep Med Rev. 2022;64:101621. doi: 10.1016/j.smrv.2022.101621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Philbrook LE, Saini EK, Fuller-Rowell TE, Buckhalt JA, El-Sheikh M.. Socioeconomic status and sleep in adolescence: the role of family chaos. J Fam Psychol. 2020;34(5):577–586. doi: 10.1037/fam0000636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Brown TH, Garcia E.. Trauma-related sleep disturbance in youth. Curr Opin Psychol. 2020;34:128–132. doi: 10.1016/j.copsyc.2020.01.004 [DOI] [PubMed] [Google Scholar]
- 41. Goodhines PA, Wedel AV, Dobani F, Zaso MJ, Gellis LA, Park A.. Cannabis use for sleep aid among high school students: concurrent and prospective associations with substance use and sleep problems. Addict Behav. 2022;134:107427. doi: 10.1016/j.addbeh.2022.107427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Daniels A, Pillion M, Rullo B, et al. Technology use as a sleep-onset aid: are adolescents using apps to distract themselves from negative thoughts? Sleep Adv. 2023;4(1):zpac047. doi: 10.1093/sleepadvances/zpac047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Substance Abuse Mental Health Services Administration. Promoting Alternatives to the Use of Seclusion and Restraint—Issue Brief #1. 2010. A National Strategy to Prevent Seclusion and Restraint in Behavioral Health Services. 2010. https://www.samhsa.gov/sites/default/files/topics/trauma_and_violence/seclusion-restraints-1.pdf. Accessed December 1, 2023.
- 44. Aalsma MC, White LM, Lau KS, Perkins A, Monahan P, Grisso T.. Behavioral health care needs, detention-based care, and criminal recidivism at community reentry from juvenile detention: a multisite survival curve analysis. Am J Public Health. 2015;105(7):1372–1378. doi: 10.2105/AJPH.2014.302529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mowen TJ, Boman JH.. A developmental perspective on reentry: understanding the causes and consequences of family conflict and peer delinquency during adolescence and emerging adulthood. J Youth Adolesc. 2018;47:275–289. doi: 10.1007/s10964-017-0794-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cohen JA, Scheeringa MS.. Post-traumatic stress disorder diagnosis in children: challenges and promises. Dialogues Clin Neurosci. 2009;11(1):91–99. doi: 10.31887/DCNS.2009.11.1/jacohen [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cruz D, Lichten M, Berg K, George P.. Developmental trauma: conceptual framework, associated risks and comorbidities, and evaluation and treatment. Front Psychiatry. 2022;13:800687. doi: 10.3389/fpsyt.2022.800687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Meltzer LJ, McLaughlin Crabtree V.. Pediatric Sleep Problems: A Clinician’s Guide to Behavioral Interventions. Washington, DC: American Psychological Association; 2015. [Google Scholar]
- 49. Dewald-Kaufmann J, de Bruin E, Michael G.. Cognitive behavioral therapy for insomnia (CBT-i) in school-aged children and adolescents. Sleep Med Clin. 2019;14(2):155–165. doi: 10.1016/j.jsmc.2019.02.002 [DOI] [PubMed] [Google Scholar]
- 50. Cole J, Sprang G, Lee R, Cohen J.. The trauma of commercial sexual exploitation of youth: a comparison of CSE victims to sexual abuse victims in a clinical sample. J Interpers Violence. 2016;31(1):122–146. doi: 10.1177/0886260514555133 [DOI] [PubMed] [Google Scholar]
- 51. Hambrick EP, Rubens SL, Brawner TW, Taussig HN.. Do sleep problems mediate the link between adverse childhood experiences and delinquency in preadolescent children in foster care? J Child Psychol Psychiatry. 2018;59(2):140–149. doi: 10.1111/jcpp.12802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kovachy B, O’Hara R, Hawkins N, et al. Sleep disturbance in pediatric PTSD: current findings and future directions. J Clin Sleep Med. 2013;9(5):501–510. doi: 10.5664/jcsm.2678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Baddam SK, Olvera RL, Canapari CA, Crowley MJ, Williamson DE.. Childhood trauma and stressful life events are independently associated with sleep disturbances in adolescents. Behav Sci. 2019;9(10):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pace-Schott EF, Germain A, Milad MR.. Sleep and REM sleep disturbance in the pathophysiology of PTSD: the role of extinction memory. BiolMood Anxiety Disord. 2015;5:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sullivan RM, Wallace AL, Stinson EA, et al. Assessment of withdrawal, mood, and sleep inventories after monitored 3-week abstinence in cannabis-using adolescents and young adults. Cannabis Cannabinoid Res. 2022;7(5):690–699. doi: 10.1089/can.2021.0074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Jones CM, Clayton HB, Deputy NP, et al. Prescription opioid misuse and use of alcohol and other substances among high school students—youth risk behavior survey, United States, 2019. MMWR Suppl. 2020;69(1):38–46. doi: 10.15585/mmwr.su6901a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hser Y-I, Mooney LJ, Huang D, et al. Reductions in cannabis use are associated with improvements in anxiety, depression, and sleep quality, but not quality of life. J Subst Abuse Treat. 2017;81:53–58. doi: 10.1016/j.jsat.2017.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lewey JH, Smith CL, Burcham B, Saunders NL, Elfallal D, O’Toole SK.. Comparing the effectiveness of EMDR and TF-CBT for children and adolescents: A meta-analysis. J Child Adolesc Trauma. 2018;11:457–472. doi: 10.1007/s40653-018-0212-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Cohen JA, Mannarino AP, Kinnish K.. Trauma-focused cognitive behavioral therapy for commercially sexually exploited youth. J Child Adolesc Trauma. 2017;10(2):175–185. doi: 10.1007/s40653-015-0073-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Cohen JA, Mannarino AP, Jankowski K, Rosenberg S, Kodya S, Wolford GL.. A randomized implementation study of trauma-focused cognitive behavioral therapy for adjudicated teens in residential treatment facilities. Child Maltreat. 2016;21(2):156–167. doi: 10.1177/1077559515624775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Skar A-MS, Braathu N, Jensen TK, Ormhaug SM.. Predictors of nonresponse and drop-out among children and adolescents receiving TF-CBT: investigation of client-, therapist-, and implementation factors. BMC Health Serv Res. 2022;22(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Villalta L, Smith P, Hickin N, Stringaris A.. Emotion regulation difficulties in traumatized youth: a meta-analysis and conceptual review. Eur Child Adolesc Psychiatry. 2018;27:527–544. doi: 10.1007/s00787-018-1105-4 [DOI] [PubMed] [Google Scholar]
- 63. Dierkhising CB, Lane A, Natsuaki MN.. Victims behind bars: A preliminary study of abuse during juvenile incarceration and post-release social and emotional functioning. Psychol Public Policy, Law. 2014;20(2):181. [Google Scholar]
- 64. Hudson N, Burghart S, Reynoldson J, Grauer D.. Evaluation of low dose prazosin for PTSD-associated nightmares in children and adolescents. Ment Health Clin. 2021;11(2):45–49. doi: 10.9740/mhc.2021.03.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Keeshin BR, Ding Q, Presson AP, Berkowitz SJ, Strawn JR.. Use of prazosin for pediatric PTSD-associated nightmares and sleep disturbances: a retrospective chart review. Neurol Ther. 2017;6:247–257. doi: 10.1007/s40120-017-0078-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Akinsanya A, Marwaha R, Tampi RR.. Prazosin in children and adolescents with posttraumatic stress disorder who have nightmares: a systematic review. J Clin Psychopharmacol. 2017;37(1):84–88. doi: 10.1097/JCP.0000000000000638 [DOI] [PubMed] [Google Scholar]
- 67. Morgenthaler TI, Auerbach S, Casey KR, et al. Position paper for the treatment of nightmare disorder in adults: an American Academy of sleep medicine position paper. J Clin Sleep Med. 2018;14(6):1041–1055. doi: 10.5664/jcsm.7178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ho FY-Y, Chan CS, Tang KN-S.. Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2016;43:90–102. doi: 10.1016/j.cpr.2015.09.005 [DOI] [PubMed] [Google Scholar]
- 69. Crowther ME, Saunders WJ, Sletten TL, Drummond SP, Bei B.. Tailoring cognitive behavioural therapy for insomnia across contexts, conditions, and individuals: what do we know, where do we go? J Sleep Res. 2023;32:e14023. [DOI] [PubMed] [Google Scholar]
- 70. Krakow B. Imagery rehearsal therapy for adolescents. Behavioral Treatments for Sleep Disorders. New York, NY: Elsevier; 2011:333-342. [Google Scholar]
- 71. Krakow B, Sandoval D, Schrader R, et al. Treatment of chronic nightmares in adjudicated adolescent girls in a residential facility. J Adolesc Health. 2001;29(2):94–100. doi: 10.1016/s1054-139x(00)00195-6 [DOI] [PubMed] [Google Scholar]
- 72. Allen SL, Howlett MD, Coulombe JA, Corkum PV.. ABCs of sleeping: a review of the evidence behind pediatric sleep practice recommendations. Sleep Med Rev. 2016;29:1–14. doi: 10.1016/j.smrv.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 73. Dong L, Dolsen MR, Martinez AJ, Notsu H, Harvey AG.. A transdiagnostic sleep and circadian intervention for adolescents: six‐month follow‐up of a randomized controlled trial. J Child Psychol Psychiatry. 2020;61(6):653–661. doi: 10.1111/jcpp.13154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Au R, Carskadon M, Millman R, et al.; Adolescent Sleep Working Group, Committee on Adolescence, Council on School Health,. School start times for adolescents. Pediatrics. 2014;134(3):642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Wolfson AR, Harkins E, Johnson M, Marco C.. Effects of the young adolescent sleep smart program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015;1(3):197–204. doi: 10.1016/j.sleh.2015.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Harvey AG. Treating sleep and circadian problems to promote mental health: perspectives on comorbidity, implementation science and behavior change. Sleep. 2022;45(4). doi: 10.1093/sleep/zsac026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Baumann AA, Cabassa LJ.. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv Res. 2020;20(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Erland LA, Saxena PK.. Melatonin natural health products and supplements: presence of serotonin and significant variability of melatonin content. J Clin Sleep Med. 2017;13(2):275–281. doi: 10.5664/jcsm.6462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Choi K, Lee YJ, Park S, Je NK, Suh HS.. Efficacy of melatonin for chronic insomnia: systematic reviews and meta-analyses. Sleep Med Rev. 2022;66:101692. [DOI] [PubMed] [Google Scholar]
- 80. Owens JA, Dalzell V.. Use of the ‘BEARS’sleep screening tool in a pediatric residents’ continuity clinic: a pilot study. Sleep Med. 2005;6(1):63–69. doi: 10.1016/j.sleep.2004.07.015 [DOI] [PubMed] [Google Scholar]
- 81. Forrest CB, Meltzer LJ, Marcus CL, et al. Development and validation of the promis pediatric sleep disturbance and sleep-related impairment item banks. Sleep. 2018;41(6). doi: 10.1093/sleep/zsy054 [DOI] [PubMed] [Google Scholar]
- 82. Mindell JA, Bartle A, Wahab NA, et al. Sleep education in medical school curriculum: a glimpse across countries. Sleep Med. 2011;12(9):928–931. doi: 10.1016/j.sleep.2011.07.001 [DOI] [PubMed] [Google Scholar]
- 83. Zhou ES, Mazzenga M, Gordillo ML, Meltzer LJ, Long KA.. Sleep education and training among practicing clinical psychologists in the United States and Canada. Behav Sleep Med. 2021;19(6):744–753. doi: 10.1080/15402002.2020.1860990 [DOI] [PubMed] [Google Scholar]
- 84. Liu J, Magielski J, Glenn A, Raine A.. The Bidirectional relationship between sleep and externalizing behavior: a systematic review. Sleep Epidemiol. 2022;2:100039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. First Step Act of 2018, Public Law No. 115-391. 2018.
- 86. Pfleger P. Investigation finds Tenn. juvenile detention center illegally secluded children. Natl Public Radio. 2023. [Google Scholar]