Key Points
-
•
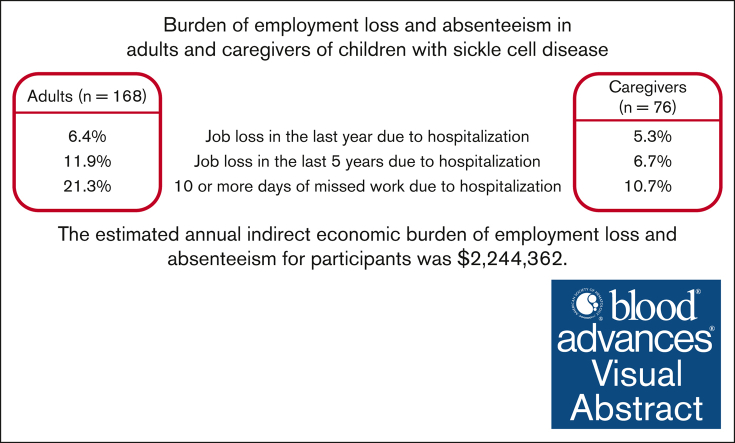
Adults and caregivers of children with sickle cell disease have high rates of employment loss and absenteeism related to hospitalization.
-
•
Not living with a partner is associated with increased employment loss and missed work for families affected by sickle cell disease.
Visual Abstract
Abstract
Sickle cell disease (SCD) is a genetic disorder affecting 100 000 people with an estimated annual medical cost of $3 billion in the United States; however, the economic impact on patients is not well described. We aimed to examine the indirect economic burden and test the hypothesis that socioeconomic status and greater social vulnerability risks are associated with increased absenteeism and employment loss. We surveyed adults and caregivers of children with SCD at 5 US centers from 2014 to 2021. Logistic regression models were used to examine the associations of employment loss and missed days of work with demographics and social determinants. Indirect costs were estimated by multiplying the self-reported missed days of work and job loss by 2022 average wages by the state of the participating institution. Of the 244 participants, 10.3% reported employment loss in the last 5 years, and 17.5% reported missing 10 or more days of work. Adults had 3 times more employment loss compared with caregivers of children with SCD (OR, 3.18; 95% CI, 1.12-9.01) but fewer missed days of work (OR, 0.24; 95% CI, 0.11-0.0.51). Participants who did not live with a partner reported increased employment loss (OR, 4.70; 95% CI, 1.04-21.17) and more missed days of work (OR, 4.58; 95% CI, 1.04-20.15). The estimated annual indirect economic burden was $2 266 873 ($9290 per participant). Adults with SCD and caregivers of children with SCD commonly report employment loss and missed days of work as important risk factors. The high indirect economic burden suggests that future economic evaluations of SCD should include SCD-related indirect economic burden.
Introduction
Sickle cell disease (SCD), a hereditary disorder of the hemoglobin structure within red blood cells, affects >100 000 Americans,1 and leads to debilitating pain episodes, disability, and early mortality.2 As the vast majority of individuals with SCD are Black/African Americans,1 this compounds other existing health and socioeconomic disparities. The direct economic costs of SCD care have been studied extensively.3, 4, 5, 6, 7 The average annual medical costs are ∼$10 000 for a child and $34 000 for an adult with SCD,3 with an estimated lifetime cost of $1.6 million per person.4 Given the complexities of SCD, procedures as simple as blood transfusions have significantly increased associated costs,5,8 and costs exponentially increase as individuals develop end organ damage.7
Despite the extensive interest in direct health care costs, little is known about their full economic impact on people with SCD. The projected lifetime income of a person with SCD is $500 000 lower than that of matched individuals.9 There are many ways in which SCD can impact personal productivity10; over half of the people with SCD report a reduction in work hours and school achievement related to their disease,11 and studies have shown that vaso-occlusive crises (VOCs) significantly impact work productivity.12 However, the effect of SCD on employment remain poorly understood. The unemployment rates in adults with SCD vary from 25% to 60%.13 More individuals in the United States report a negative impact of SCD on their employment/schooling compared with other high- and middle-income countries,14 and employment status in SCD is associated with decreased health care use.15,16 The indirect costs associated with SCD have been studied largely in single-center studies, are often model-based, and are usually limited to adults and children.17 Empirical studies on the productivity costs of families affected by SCD in the United States are currently lacking.18 It is critical to understand not only the burden of loss of work productivity for families affected by SCD but also the predictors of absenteeism and employment loss to allow targeted interventions to improve financial health in those most at risk for hardship.
Our study aimed to test the hypothesis that greater social vulnerability risks (eg, lower education, not living with a partner, and difficulty paying bills) are associated with increased absenteeism and employment loss. We also characterized the prevalence and economic burden of work absenteeism and employment loss in adults and caregivers of children with SCD and the indirect economic costs at multiple institutions across the United States.
Methods
This project included data from the Mid-South CDRN, established in 201419 and funded by the Patient-Centered Outcomes Research Institute, and a multisite feasibility randomized controlled trial.20 This study was approved by the Institutional Review Boards of all participating sites, and informed consent was obtained from all participants.
Setting and procedure
We surveyed adults aged 18 years and older with SCD and caregivers of children with SCD between 0-16 years old. The following 5 SCD centers across the Unites States participated in questions regarding employment loss and absenteeism: Lurie Children’s Hospital of Chicago, University of Tennessee Health Science Center, University of San Francisco, The Ohio State University, and Vanderbilt University. Three institutions (Lurie Children’s Hospital of Chicago, University of Tennessee Health Science Center, and University of California San Francisco) were surveyed between October 2014 and March 2016, and 2 institutions (The Ohio State University and Vanderbilt University) were surveyed between 2018 and 2022. The inclusion criteria for survey participants in both studies included being over the age of 18 years, being able to read and speak English, having a diagnosis of SCD (all genotypes included) or being parents/caregivers of a child with SCD, and receiving care at one of the contributing centers. Individuals with SCD and their caregivers were recruited by research personnel during clinic visits or via clinic flyers. Participants completed the surveys on electronic tablets or paper-and-pencil, with members of the research team present if they had questions or required assistance. Participants were compensated for their time with a gift card upon survey completion.
Surveys
The surveys were designed in collaboration with various stakeholders, including individuals with SCD. Question domains included sociodemographic variables, social support systems, and employment loss. The full survey are described in detail elsewhere.21, 22, 23 Participants were asked 2 questions about whether they had lost their jobs due to needing hospitalization: (1) employment loss in the last year and (2) employment loss in the last 5 years. They were also asked how many days of work they had missed in the last year because of hospitalization. Of note, the question did not specify whether the hospitalization was due to SCD or another illness. Given the small available sample, survey results from the 2 studies were pooled together; the studies had similar inclusion criteria, and all included questions had identical wording. The demographics of the included adults were reviewed and were found to be similar (supplemental Table 1). All institutions were geographically remote from each other, making the likelihood of repeated survey participation low.
Statistical analysis
The study data were collected, deidentified, and managed using the REDCap electronic data capture tools. Surveys were excluded if participants did not answer basic demographic information (age and gender) or any questions regarding absenteeism or employment loss. We reported descriptive statistics (mean, standard deviation, and distribution) for the demographics of the sample, frequency of job loss, and number of missed days due to hospitalization.
Bivariate associations among employment loss in the last year, employment loss in the last 5 years, and the number of missed days due to hospitalization were explored with demographics and social determinants of health using univariable logistic regression models. Participants who reported “Not applicable” to these questions were excluded from the statistical test. Models were created for all participants, and separate models were created for adults with SCD and caregivers of children with SCD to understand whether the risk factors differed between these 2 groups. Notably, race/ethnicity was not studied because most participants reported being Black/African American (Table 1). Sex was not studied in the caregiver model, as sex reported is that of the patient (or child of the caregiver) and was thought unlikely to be related to employment loss. We also created multivariable logistic regression models, including all studied variables as predictors, for all participants. Given the large proportion of participants reporting “not applicable,” multivariable analyses for the adult and caregiver subgroups were not performed due to small sample size. Analyses were performed using Stata version 17.0 and SAS version 9.4.
Table 1.
Sociodemographic information of adults and caregivers of children with SCD
| Total | Adults |
Children∗ |
Combined |
|
|---|---|---|---|---|
| 168 (68.9%) | 76 (31.1%) | 244 | ||
| Age of patient in years, mean (SD) | 33.2 (12.1) | 8.1 (4.7) | 25.4 (15.6) | |
| Sex of patient | Male | 64 (38.1%) | 40 (52.6%) | 107 (42.6%) |
| Female | 102 (60.7%) | 36 (47.4%) | 135 (56.6%) | |
| Other | 2 (1.2%) | 0 (0%) | 2 (0.8%) | |
| Race | Black/African American | 165 (98.2%) | 71 (93.4%) | 236 (96.7%) |
| Highest degree or level of school | High school graduate or less | 70 (42.4%) | 28 (54.9%) | 98 (45.4%) |
| Some college or beyond | 92 (55.8%) | 13 (25.5%) | 105 (48.6%) | |
| Prefer not to answer | 3 (1.8%) | 10 (19.6%) | 13 (6%) | |
| Relationship status | Married/living together | 51 (30.4%) | 12 (15.8%) | 63 (25.8%) |
| Unmarried | 108 (64.3%) | 50 (65.8%) | 158 (64.8%) | |
| Prefer not to say | 9 (5.4%) | 14 (18.4%) | 23 (8.4%) | |
| Difficulty paying monthly bills | Not very/not at all | 67 (39.9%) | 38 (50%) | 105 (43.0%) |
| Somewhat/very | 98 (58.3%) | 38 (50%) | 136 (55.7%) | |
| Prefer not to say | 3 (1.8%) | 0 (0) | 3 (1.2%) | |
| Site | Chicago | 14 (8.3%) | 76 (100%) | 90 (36.9%) |
| OSU | 25 (14.9%) | 0 | 25 (10.2%) | |
| UCSF | 51 (30.4%) | 0 | 51 (20.9%) | |
| VUMC | 32 (19%) | 0 | 32 (13.1%) | |
| UTHSC | 46 (27.4%) | 0 | 46 (18.8%) | |
Data obtained from caregivers of children with SCD.
Economic burden estimation
Income estimates were obtained via the 2021 Current Population Survey Annual Social and Economic Supplements conducted by the US Census Bureau, which includes pretax wages and fringe benefits.24 Annual salaries were calculated based on educational attainment–matched national averages. Daily wages were determined by assuming 240 workdays per year, after excluding weekends and leave.25 For participants who did not answer educational attainment, the US average annual income26 was used to estimate the income loss. Absenteeism costs were estimated by multiplying the number of reported days of work missed due to hospitalization in the last year by the estimated daily wage. Employment loss costs were estimated by including all participants who reported employment losses in the last 1 or 5 years and multiplying the number of participants by their estimated wage. Because we did not ask how long the participants were out of work, we reported this as an annual potential earning loss.
Results
Demographics
A total of 268 participants were surveyed: 171 adults with SCD and 76 caregivers of children with SCD. A total of 25 participants (9.3%) were excluded from the analysis because they did not answer basic demographic data (age and sex) or did not answer any of the employment questions, leaving 244 participants analyzed. The average age of the adults was 33.2 years (SD: 12.1) and the average age of the children was 8.1 years (SD: 4.7), with 38.1% of adults and 52.6% of children being male (Table 1). Notably, caregivers only reported the sex of their child; thus, the sex of the caregiver filling out the survey was not known. Caregivers reported lower education levels on average than adults with SCD. There were similar rates of participating adults and caregivers who reported not living with a partner (64.3% adults vs 65.8% caregivers).
Two institutions participating in the study collected data regarding employment from 57 adults with SCD (supplemental Table 2). A total of 48.3% of the adults with SCD surveyed reported current employment; 20.7% reported that they were out of work and only 1.7% reported being unable to work or disabled.
Employment loss and absenteeism are prevalent in families affected by SCD
In total, 6% (n = 13) reported employment loss in the last year, and 10.3% (n = 25) reported employment loss in the last 5 years due to emergency room visits or hospitalization (Table 2). Adults had a much higher rate of employment loss in the last 5 years than caregivers of children with SCD: 11.9% vs 6.7%, respectively. A total of 22.1% (n = 48) reported missing 5 or more days of work in the last year due to hospitalization. Twice as many adults with SCD missed 10 or more days compared with caregivers of children: 21.3% vs 10.7%, respectively.
Table 2.
Employment loss and absenteeism as reported by adults and caregivers of children with SCD
| Adults | Children∗ | Combined | |
|---|---|---|---|
| In the last year, have you lost job because you had to go to the emergency room or hospital? | |||
| Yes | 9 (6.4%) | 4 (5.3%) | c13 (6%) |
| No | 59 (42.1%) | 56 (74.7%) | 115 (53.5%) |
| N/A | 72 (51.4%) | 15 (20%) | 87 (40.5%) |
| In the last 5 years, have you lost job because you had to go to the emergency room or hospital? | |||
| Yes | 20 (11.9%) | 5 (6.7%) | 25 (10.3%) |
| No | 68 (40.5%) | 54 (72%) | 122 (50.2%) |
| N/A | 80 (47.6%) | 16 (21.3%) | 96 (39.5%) |
| How many days of work in the last year were missed because of hospitalization(s)? | |||
| 0-2 days | 13 (9.1%) | 23 (30.7%) | 26 (16.6%) |
| 3-5 days | 8 (5.6%) | 8 (10.7%) | 16 (7.4%) |
| 6-10 days | 3 (2.1%) | 7 (9.3%) | 10 (4.6%) |
| 10 or more days | 30 (21.3%) | 8 (10.7%) | 38 (17.5%) |
| N/A | 88 (62%) | 29 (38.7%) | 117 (53.9%) |
Data obtained from caregivers of children with SCD.
Larger household size and not living with a partner were associated with employment loss and absenteeism
Bivariate logistic regression models for patient characteristics and employment loss are shown in Table 3. Notably, because of the low number of caregivers reporting job loss (<5), the regression models could not be fitted for caregivers and were not used. A larger household size was associated with lower rates of employment loss in the last year (odds ratio [OR], 0.65; P = .046). Employment loss in the last 5 years was more likely for adults than for caregivers of children (OR, 3.18; P = .031). Not living with a partner was also associated with a higher rate of employment loss in the last 5 years in the combined model (OR, 4.70; P = .044).
Table 3.
Logistic regression models for employment loss in the last 1 and 5 years
| Employment loss in last 1 year | |||||
|---|---|---|---|---|---|
| Combined (Adults & caregivers) | Odds Ratio | 95% CI | Unadjusted P-value | Adjusted P-value | |
| Participant type | Adult (≥ 18 y/o) | 2.14 | (0.62, 7.33) | .228 | .571 |
| Education | Some college or more | 0.50 | (0.12, 2.06) | .337 | .177 |
| Household size | By one unit increase | 0.65 | (0.43, 0.99) | .046∗ | .235 |
| Children in home | By one unit increase | 0.71 | (0.44, 1.15) | .162 | |
| Relationship status | Not living with a partner | 1.69 | (0.35, 8.21) | .516 | .317 |
| Bills | Somewhat or very difficult | 0.73 | (0.23, 2.31) | .593 | .992 |
| Adults | |||||
| Age | 0.97 | (0.90, 1.04) | .355 | ||
| Sex | Male | 1.00 | (0.23, 1.42) | .233 | |
| Education | Some college or more | 0.50 | (0.11, 2.31) | .377 | |
| Household size | 0.57 | (0.30, 1.09) | .089 | ||
| Children in home | 0.58 | (0.25, 1.34) | .201 | ||
| Relationship status | Not living with a partner | 2.56 | (0.29, 22.59) | .397 | |
| Bills | Somewhat or very difficult | 0.34 | (0.08, 1.49) | .152 | |
| Employment loss in last 5 years | |||||
|---|---|---|---|---|---|
| Combined | |||||
| Participant type | Adult (≥ 18 y/o) | 3.18 | (1.12, 9.01) | .030∗ | .061 |
| Education | Some college or more | 1.04 | (0.41, 2.62) | .932 | .375 |
| Household size | 0.93 | (0.72, 1.19) | .544 | .670 | |
| Children in home | 0.91 | (0.68, 1.22) | .526 | ||
| Relationship status | Not living with a partner | 4.70 | (1.04, 21.17) | .044∗ | .051 |
| Bills | Somewhat or very difficult | 1.48 | (0.60, 3.65) | .390 | .504 |
| Adults | |||||
| Age | 0.97 | (0.92, 1.02) | .224 | ||
| Sex | Male | 0.94 | (0.35, 2.56) | .375 | |
| Education | Some college or more | 0.76 | (0.28, 2.07) | .587 | |
| Household size | 1.03 | (0.74, 1.43) | .866 | ||
| Children in home | 0.88 | (0.57, 1.36) | .565 | ||
| Relationship status | Not living with a partner | 4.49 | (0.95, 21.27) | .059 | |
| Bills | Somewhat or very difficult | 1.31 | (0.46, 3.74) | .616 | |
Unadjusted P-value with univariate logistic regression analysis for all participants and adult participants. Adjusted multivariable logistic regression analysis for all participants.
: statistically significant (P < .05).
Bivariate logistic regression models among patient characteristics and number of days missed at work are shown in Table 4. Adults had significantly lower missed day rates than caregivers (OR, 0.24; P < .005). A larger household size was associated with more frequent missed days (OR, 1.26; P = .049). Caregivers of children who did not live with a partner reported missing more days of work (OR, 4.58; P = .044).
Table 4.
Logistic regression models for absenteeism
| Missed days | |||||
|---|---|---|---|---|---|
| Combined (Adults & Caregivers) | Odds Ratio | 95% CI | Unadjusted P-value | Adjusted P-value | |
| Participant type | Adult (> 18 y/o) | 0.24 | (0.11, 0.51) | < .005∗ | .005∗ |
| Education | Some college or more | 0.51 | (0.22, 1.17) | .110 | .089 |
| Household size | 1.26 | (1.00, 1.58) | .049∗ | .986 | |
| Children in home | 1.19 | (0.93, 1.53) | .176 | ||
| Relationship status | Not living with a partner | 1.88 | (0.71, 4.96) | .202 | .115 |
| Bills | Somewhat or very difficult | 1.15 | (0.55, 2.39) | .717 | .290 |
| Adults | |||||
| Age | 1.01 | (0.97, 1.06) | .68 | ||
| Sex | Male | 0.62 | (0.21, 1.79) | .375 | |
| Education | Some college or more | 0.65 | (0.23, 1.88) | .428 | |
| Household size | 0.92 | (0.64, 1.31) | .626 | ||
| Children in home | 0.93 | (0.61, 1.40) | .714 | ||
| Relationship status | Not living with a partner | 1.53 | (0.37, 6.38) | .556 | |
| Bills | Somewhat or very difficult | 1.80 | (0.60, 5.38) | .294 | |
| Caregivers | |||||
| Age | 1.03 | (0.91, 1.17) | .628 | ||
| Education | Some college or more | 2.56 | (0.54, 12.10) | .237 | |
| Household size/ | 1.22 | (0.83, 1.80) | .306 | ||
| Children in home | 0.94 | (0.63, 1.38) | .739 | ||
| Relationship status | Not living with a partner | 4.58 | (1.04, 20.15) | .044∗ | |
| Bills | Somewhat or very difficult | 0.88 | (0.29, 2.63) | .817 | |
Unadjusted P-value with univariate logistic regression analysis for all participants and adult participants. Adjusted multivariable logistic regression analysis for all participants.
: statistically significant (P < .05).
In multivariable analysis (Table 3), adults were statistically less likely to report missed days of work (OR, 0.21; P = .005). Not living with a partner approached statistical significance as a predictor of employment loss in the last 5 years (OR, 4.88; P = .051).
The indirect economic burden of absenteeism and employment loss was ∼$2 266 873 annually
By using the number of days participants reported missing work due to SCD in the last year multiplied by the average wage of the corresponding educational attainment (supplemental Table 3), we estimated that participants reported a total of $144 726, ranging from $0 to $4811 with mean of $586 per participant, in lost wages due to missed days of work. Employment loss is estimated to cost $2 122 147 annually in lost wages, yielding a total annual indirect economic burden of $2 266 873. Importantly, this only represents lost wages for participants who reported working in the last 5 years and excludes participants who were not working due to disability or other reasons.
Discussion
In this study, we illustrated that employment loss and absenteeism due to hospitalization represent a common problem for adults with SCD and caregivers of children with SCD at multiple institutions across the United States. More than 10% of the participants reported employment loss in the last 5 years due to hospitalization, and >20% reported missing >5 days of work in the last year due to hospitalization. Our participants reported a total of $2 266 873 per year of missed income due to employment loss and absenteeism, or $9290 per participant annually. This economic burden represents nearly the entirety of the average annual medical costs for a child and one-third of an adult’s expected direct health care costs.3 Importantly, participants were only asked to report employment loss due to hospitalization and unrelated to other causes (eg, home management of vaso-occlusive pain episodes and medical appointments). Participants from 2 institutions demonstrated that unemployment rates are much higher for families impacted by SCD than for the general population27; 20.7% of participants reported being out of work, compared with 4.7% of families that included an unemployed person in the United States. SCD has many impacts that may make maintaining employment significantly challenging, including the need for frequent appointments, home management of vaso-occlusive pain episodes,28 cognitive deficits,13 and chronic disability.29 Simultaneously, employment loss and absenteeism increase financial burdens on families, which are already high, given the high cost of medical care for SCD. Given the significant direct and indirect economic burden of SCD, these costs should be considered when assessing the value of new curative therapies that may have a high upfront cost but could significantly alter patients’ ongoing health and productivity. If our per-participant estimated cost is extrapolated to >100 000 Americans living with SCD,1 absenteeism and employment represent >$900 million of lost wages, a large-scale loss of productivity, and economic growth that demands action. Notably, this disproportionately affects 2 groups that already struggle with economic disenfranchisement: people who are Black, given the demographics of SCD, and women who are more likely to be caregivers for family members.30
Employment challenges impact adults with SCD and caregivers of children with SCD differently. Although adults were more likely to report employment loss in the last 5 years, caregivers and adults had different levels of missed days of work due to hospitalization. Although both lead to decreased earnings and financial hardships, our results suggest that adults and caregivers need separate support to improve their employment stability. Individuals living with a partner had significantly lower rates of employment loss for the total sample and missed days of work for caregivers. Notably, no other social determinants of health (including age, education, and ability to pay bills) were associated with employment loss or missed workdays, suggesting that this is a challenge for families impacted by SCD from various backgrounds. Increased household size was associated with less employment loss but more missed days of work, suggesting a need for further study on how social support systems impact employment in families affected by SCD.
We suggest several potential mechanisms for the associations between employment loss and absenteeism. Living with a partner may help decrease the burden of unpaid work at home and childcare, if applicable, which may cause difficulties in completing employment requirements. Nationally, married couples have lower unemployment rates than single-adult households,27 suggesting that this remains true for families with and without SCD. However, living with a partner may also help prevent depression or worsening social stigma, 2 significant concerns for people with SCD.31,32 One study has shown that people with SCD were most likely to receive emotional support from those living with them, as opposed to support outside of the home.33 This support may have a protective factor that is critical to consider, given the burden of employment loss due to SCD. It is critical to note that while healthy relationships may benefit productivity and provide support, toxic or abusive relationships have negative effects on health and well-being, including economic well-being.34
Our data are strengthened by its multi-institutional reach, encompassing findings from 5 SCD centers throughout the United States. Given the regional differences in employment availability and disability patterns, this allows us to make further generalizations about US families impacted by SCD. Although the 2 survey periods that were pooled together were separated by a couple of years, we found no significant difference in the proportion of adults with SCD reporting employment loss or missed days between the 2 survey periods (supplemental Table 1), suggesting that transient economic changes or the COVID-19 pandemic did not change the proportion of employment loss.
There are limitations in our study. First, given the self-reported nature of this survey, recall bias could impact participants’ reports of health care use or employment loss. Second, the survey was also administered in outpatient clinics; therefore, it was limited to individuals who attended outpatient visits and may not represent people who are high inpatient utilizers and are rarely seen in the outpatient setting. Third, many participants reported “not applicable” to job loss (39.5%) or missed work days (53.9%). Based on participants' employment status from 2 institutions, we expect around one-third of participants to report not applicable (out of work, homemaker, retired, or unable to work); however, even for this data, one-quarter of participants reported “prefer not to say.” Due to our small sample size, we were limited to performing bivariate regression analysis. Although there may be confounding in the bivariate analyses, the associations observed in these analyses could be further evaluated in multivariate analyses of larger populations. Finally, caregiver data were obtained from one institution based on the demographics of patients served at the included SCD centers; this may make the data obtained regarding caregivers more difficult to generalize to other centers. Caregivers only reported their child’s sex, not their own, so we were unable to analyze differences in productivity by caregiver sex, given that known sex disparities in caregiving,35 employment loss, and missed days due to caregiving are likely to affect women disproportionately.
Future research is needed to further characterize the productivity loss in paid employment for people with SCD and the impact of SCD on unpaid work (eg, caregiving and household productivity) to characterize the economic impact of SCD on families comprehensively. As women complete three-quarters of unpaid work,36 this would also help characterize sex inequities in the disease burden. The effect of SCD vs non-SCD populations on productivity requires further evaluation to determine the incremental costs attributable to SCD. Although the surveys in this study focused on attitudes regarding outpatient care and barriers to access, not on disease complications and who are actively on treatment and adherent to their regimen, future studies will be critical to further delineate the impact of therapies and complications on the indirect economic burden. Ultimately, the economic burden of SCD is an important consideration in cost analyses for future therapies to determine treatments that would have a positive economic impact on direct health care costs and indirect costs for patients.
Conclusions
Employment loss and absenteeism due to hospitalization represent prevalent issues in families affected by SCD, which lead to significant financial losses of >$2 million annually. The impact of medical care costs compounded by losses of income opportunities perpetuate a vicious cycle of poverty among many patients with SCD and their families. Adults with SCD are more likely to report employment loss, and caregivers of children with SCD report more missed days of work, suggesting different and significant employment challenges for both populations. Not living with a partner was associated with both employment loss and missed days of work, suggesting that this is an important risk factor for health care providers to consider for those who need more financial resources. A larger household size was associated with lower rates of employment loss but more missed workdays, suggesting that social support systems play an important but conflicting role in employment maintenance for families impacted by SCD. Further work is warranted to understand how social support protects against employment loss and potential interventions for those with limited social support.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Acknowledgments
The authors greatly appreciate the input of Jeannie Byrd, Brandi M. Pernell, Patricia Adams-Graves, and Michael DeBaun, in design of the initial survey and collaboration via the Mid-South CDRN.
This work was financially supported by the PCORI grant number CDRN 1501-26498, and the research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number K23HL141447. Gordon is currently supported by the Agency for Healthcare Research and Quality (T32HS029590-01).
Authorship
Contribution: R.D.G., C.J.L., and R.M.C. designed the study; N.Q., J.S.H., A.A.K., A.A.T., M.T., and R.M.S. collected the data; R.D.G. and R.L.W. performed the analysis; R.D.G., C.J.L., and R.M.S. interpreted the results; and all authors reviewed and provided critical input into the final manuscript.
Footnotes
Deidentified data are available upon request from the corresponding author, Rachel D’Amico Gordon (Rachel.Gordon@osumc.edu).
The full-text version of this article contains a data supplement.
Supplementary Material
References
- 1.Brousseau DC, Panepinto JA, Nimmer M, Hoffmann RG. The number of people with sickle-cell disease in the United States: national and state estimates. Am J Hematol. 2010;85(1):77–78. doi: 10.1002/ajh.21570. [DOI] [PubMed] [Google Scholar]
- 2.Chaturvedi S, DeBaun MR. Evolution of sickle cell disease from a life-threatening disease of children to a chronic disease of adults: The last 40 years. Am J Hematol. 2016;91(1):5–14. doi: 10.1002/ajh.24235. [DOI] [PubMed] [Google Scholar]
- 3.Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Hartzema AG. The cost of health care for children and adults with sickle cell disease. Am J Hematol. 2009;84(6):323–327. doi: 10.1002/ajh.21408. [DOI] [PubMed] [Google Scholar]
- 4.Johnson KM, Jiao B, Ramsey SD, Bender MA, Devine B, Basu A. Lifetime medical costs attributable to sickle cell disease among nonelderly individuals with commercial insurance. Blood Adv. 2023;7(3):365–374. doi: 10.1182/bloodadvances.2021006281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalpatthi R, Song X, Martinez D, et al. PRO35 economic burden of chronic red blood cell transfusions among patients with sickle cell disease. Value Health. 2020;23:S335. [Google Scholar]
- 6.Shah N, Bhor M, Xie L, et al. Treatment patterns and economic burden of sickle-cell disease patients prescribed hydroxyurea: a retrospective claims-based study. Health Qual Life Outcomes. 2019;17(1):155. doi: 10.1186/s12955-019-1225-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell A, Cong Z, Agodoa I, et al. the economic burden of end-organ damage among medicaid patients with sickle cell disease in the United States: a population-based longitudinal claims study. J Manag Care Spec Pharm. 2020;26(9):1121–1129. doi: 10.18553/jmcp.2020.20009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu P, Gay JC, Lin CJ, Rodeghier M, DeBaun MR, Cronin RM. Economic evaluation of regular transfusions for cerebral infarct recurrence in the Silent Cerebral Infarct Transfusion Trial. Blood Adv. 2021;5(23):5032–5040. doi: 10.1182/bloodadvances.2021004864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lubeck D, Agodoa I, Bhakta N, et al. Estimated life expectancy and income of patients with sickle cell disease compared with those without sickle cell disease. JAMA Netw Open. 2019;2(11) doi: 10.1001/jamanetworkopen.2019.15374. e1915374-e1915374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas VJ, Taylor LM. The psychosocial experience of people with sickle cell disease and its impact on quality of life: qualitative findings from focus groups. Br J Health Psychol. 2002;7(Part 3):345–363. doi: 10.1348/135910702760213724. [DOI] [PubMed] [Google Scholar]
- 11.Osunkwo I, Andemariam B, Minniti CP, et al. Impact of sickle cell disease on patients' daily lives, symptoms reported, and disease management strategies: results from the international Sickle Cell World Assessment Survey (SWAY) Am J Hematol. 2021;96(4):404–417. doi: 10.1002/ajh.26063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rizio AA, Bhor M, Lin X, et al. The relationship between frequency and severity of vaso-occlusive crises and health-related quality of life and work productivity in adults with sickle cell disease. Qual Life Res. 2020;29(6):1533–1547. doi: 10.1007/s11136-019-02412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanger M, Jordan L, Pruthi S, et al. Cognitive deficits are associated with unemployment in adults with sickle cell anemia. J Clin Exp Neuropsychol. 2016;38(6):661–671. doi: 10.1080/13803395.2016.1149153. [DOI] [PubMed] [Google Scholar]
- 14.Osunkwo I, James J, El-Rassi F, et al. Burden of disease, treatment utilization, and the impact on education and employment in patients with sickle cell disease: A comparative analysis of high- and low- to middle-income countries for the international Sickle Cell World Assessment Survey. Am J Hematol. 2022;97(8):1055–1064. doi: 10.1002/ajh.26576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams H, Silva RNS, Cline D, Freiermuth C, Tanabe P. Social and behavioral factors in sickle cell disease: employment predicts decreased health care utilization. J Health Care Poor Underserved. 2018;29(2):814–829. doi: 10.1353/hpu.2018.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Idowu M, Chung TH, Yu K. Association between employment status and hospitalization of patients with sickle cell disease: a retrospective, observational pilot study. Blood. 2018;132(Supplement 1):4930. [Google Scholar]
- 17.Holdford D, Vendetti N, Sop DM, Johnson S, Smith WR. Indirect economic burden of sickle cell disease. Value Health. 2021;24(8):1095–1101. doi: 10.1016/j.jval.2021.02.014. [DOI] [PubMed] [Google Scholar]
- 18.Baldwin Z, Jiao B, Basu A, et al. Medical and non-medical costs of sickle cell disease and treatments from a US perspective: a systematic review and landscape analysis. Pharmacoecon Open. 2022;6(4):469–481. doi: 10.1007/s41669-022-00330-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenbloom ST, Harris P, Pulley J, et al. The mid-south clinical data research network. J Am Med Inform Assoc. 2014;21(4):627–632. doi: 10.1136/amiajnl-2014-002745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cronin RM, Quaye N, Liu X, et al. A feasibility randomized controlled trial of a mhealth app vs. booklets for patient-facing guidelines. Blood Adv. 2023;7(20):6184–6190. doi: 10.1182/bloodadvances.2023010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cronin RM, Hankins JS, Adams-Graves P, et al. Barriers and facilitators to research participation among adults, and parents of children with sickle cell disease: a trans-regional survey. Am J Hematol. 2016;91(10):E461–E462. doi: 10.1002/ajh.24483. [DOI] [PubMed] [Google Scholar]
- 22.Cronin RM, Hankins JS, Byrd J, et al. Risk factors for hospitalizations and readmissions among individuals with sickle cell disease: results of a U.S. survey study. Hematology. 2019;24(1):189–198. doi: 10.1080/16078454.2018.1549801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cronin RM, Yang M, Hankins JS, et al. Association between hospital admissions and healthcare provider communication for individuals with sickle cell disease. Hematology. 2020;25(1):229–240. doi: 10.1080/16078454.2020.1780737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Semega JK. US Census Bureau; 2023. J. Income in the United States: 2021.https://www.census.gov/library/publications/2022/demo/p60-276.html [Google Scholar]
- 25.Altawalbeh SM, Wateska AR, Nowalk MP, et al. Societal cost of racial pneumococcal disease disparities in US adults aged 50 years or older. Appl Health Econ Health Policy. 2024;22(1):61–71. doi: 10.1007/s40258-023-00854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Bureau of Labor Statistics . 2023. Employment and Wages Data Viewer.https://data.bls.gov/cew/apps/table_maker/v4/table_maker.htm#type=0&year=2022&qtr=A&own=0&ind=10&supp=0 Updated 09/07/2022. [Google Scholar]
- 27.Employment Characteristics of Families- 2022. US Department of Labor; 2023. https://www.bls.gov/news.release/pdf/famee.pdf [Google Scholar]
- 28.Zaidi AU, Glaros AK, Lee S, et al. A systematic literature review of frequency of vaso-occlusive crises in sickle cell disease. Orphanet J Rare Dis. 2021;16(1):460. doi: 10.1186/s13023-021-02096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jiao B, Johnson KM, Ramsey SD, Bender MA, Devine B, Basu A. Long-term survival with sickle cell disease: a nationwide cohort study of Medicare and Medicaid beneficiaries. Blood Adv. 2023;7(13):3276–3283. doi: 10.1182/bloodadvances.2022009202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lorenz-Dant K, Mittelman M. In: Sex and Gender Differences in Alzheimer's Disease. Ferretti MT, Dimech AS, Chadha AS, editors. Academic Press; 2021. Chapter 14 - Sex and gender differences in caregiving patterns and caregivers’ needs; pp. 393–419. [Google Scholar]
- 31.Bediako SM, Lanzkron S, Diener-West M, Onojobi G, Beach MC, Haywood C., Jr. The measure of sickle cell stigma: initial findings from the improving patient outcomes through respect and trust study. J Health Psychol. 2016;21(5):808–820. doi: 10.1177/1359105314539530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hasan SP, Hashmi S, Alhassen M, Lawson W, Castro O. Depression in sickle cell disease. J Natl Med Assoc. 2003;95(7):533–537. [PMC free article] [PubMed] [Google Scholar]
- 33.Desine S, Eskin L, Bonham VL, Koehly LM. Social support networks of adults with sickle cell disease. J Genet Couns. 2021;30(5):1418–1427. doi: 10.1002/jgc4.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Forth A, Sezlik S, Lee S, Ritchie M, Logan J, Ellingwood H. Toxic relationships: the experiences and effects of psychopathy in romantic relationships. Int J Offender Ther Comp Criminol. 2022;66(15):1627–1658. doi: 10.1177/0306624X211049187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacob SA, Bouck J, Daas R, Jackson MD, LaMotte JE, Carroll AE. Understanding caregiver burden with accessing sickle cell care in the Midwest and their perspective on telemedicine. BMC Health Serv Res. 2023;23(1):500. doi: 10.1186/s12913-023-09383-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seedat S, Rondon M. Women's wellbeing and the burden of unpaid work. BMJ. 2021;374:n1972. doi: 10.1136/bmj.n1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.