Abstract
Rurality has served as a key concept in popular and scientific understandings of the US overdose crisis, with White, rural, and low-income areas thought to be most heavily affected. However, we observe that overdose trends have risen nearly uniformly across the urban-rural designations employed in most research, implying that their importance has likely been overstated or incorrectly conceptualized. Nevertheless, urbanicity/rurality does serve as a key axis to understand inequalities in overdose mortality when assessed with more nuanced modalities--employing a more granular analysis of geography at the sub-county level, and intersecting rurality sociodemographic indices such as race/ethnicity. Using national overdose data from 1999–2021, we illustrate the intersectional importance of rurality for overdose surveillance. Finally, we offer recommendations for integrating these insights into drug overdose surveillance moving forward.
Introduction
“Years ago, the worst of the crack epidemic was seen publicly: drive-by shootings, car jackings, gang graffiti and lines of street dealers. Public mayhem sparked public outrage, and media reports about crack remained constant for more than a decade.
Addiction to opiate painkillers, however, has spawned little of that. Crime plunged as overdose deaths rose, in fact. Most of the victims were white and that further concealed the scourge. It spread through Appalachia, and if there’s one part of the country that we’re used to ignoring, it’s Appalachia. Then it spread to the rest of white America--middle-and upper-middle class suburbs, rural towns. These families were aghast and ashamed. Their loved ones were now stealing, shooting up in library bathrooms, and dying with needles in their arms. So these families kept silent, hid it from public view.”
– Prepared statement by Sam Quinones, 2018, Senate Hearing 115–714, Hearing of the Committee on Health, Education, Labor, and Pensions (The Opioid Crisis: An Examination of How We Got Here and How We Move Forward, 2018)
The above excerpt from a U.S. senate hearing highlights the dominant narrative of opioid overdose that has circulated widely among the American public: namely, that the crisis has affected mainly “rural” and “Appalachian” populations and those in small towns who are “hidden” from public view (Talbot, 2017). This common narrative both shifts focus onto rural areas and otherizes and exoticizes both the “rural” and the “urban,” stymying a structural understanding of the problem and obscuring potential interventions. While this narrative has achieved widespread prominence in public health discourse, it overstates the importance of urban-rural designations in overdose epidemiology and mischaracterizes, and ignores, important spatial and geographic drivers of opioid overdose in the United States.
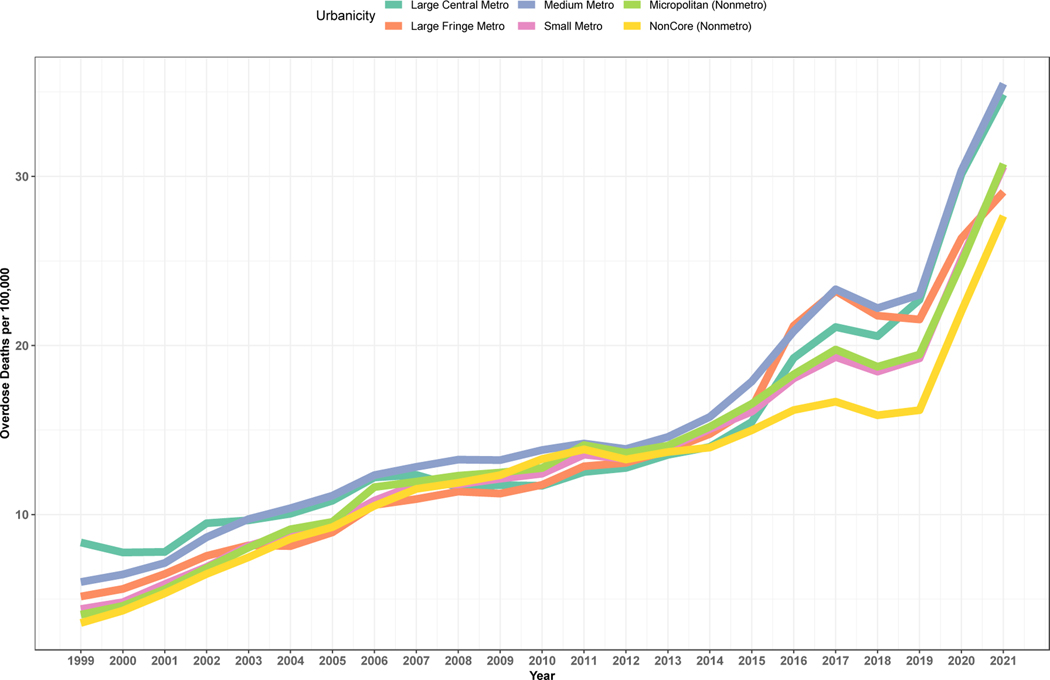
Urban-rural designations are powerful categories in scientific, political, and popular discourses concerning the overdose epidemic and public health more broadly. In the U.S., the focus on rural-urban distinctions when it comes to opioids distracts from key patterns now shaping the course of the ongoing overdose epidemic. Mapping opioid overdose deaths by urban-rural categories, race/ethnicity, and income level shows that urban-rural designations are less meaningful in determining overdose than imagined in popular narratives (Figure 1). The urban-rural categories used in U.S. national data sets, through which overdose studies are often filtered, show that overdose has risen nearly uniformly across each designated spatial category.
Figure 1: Drug overdose mortality per 100,000 population from 1999–2021, subdivided by six categories of urbanicity.
Records describing drug-related overdose were accessed through CDC WONDER[defined as underlying cause of death ICD-10 codes for drug-related accidental (X40-X44), intentional (X60–64), assault-related (X85), and undetermined intent (Y10-Y14)]. Urban-rural classification shown by 2013 NCHS Urban-Rural Classification Scheme for Counties. This figure highlights that trends in overdose show little variation by category of urbanicity; increases are observed across all six categories of urbanicity.
Background
Urban-rural categorizations inform narratives concerning opioid overdose and also impact funding dollars for research and health care. Some grants from the U.S. National Institute for Drug Abuse, for instance, require that applicants use a database to ensure that their proposed study locations are rural, despite the fact that counties typically contain both rural and urban parts (U.S. Department of Health and Human Services, 2002). Researchers have illustrated damaging consequences that can occur when poor geographic proxies are used, for instance, filtering rural places out of eligibility for rural health clinic funding because they are within counties designated as urban (Bennett et al., 2019). While risks of drug overdose are global in scope, and interventions aimed at reducing drug-related morbidity and mortality, such as the movement for harm reduction, are international, categories such as “rural” and “urban” are defined differently within nation-states, making translation of findings difficult. Here we focus on U.S.-based categories of rural and urban to characterize the problem, but reference existing international research efforts in our recommendations.
Previous research has identified conceptual and methodological problems with spatial categories; in this analysis, we extend and apply these concepts to the study of opioid overdose. Methodological problems pointed out in previous research include the dynamic nature of geographic context, including spatial uncertainty regarding areas that exert influence over a person, and temporal uncertainty as to the timing and duration of influences (Kwan, 2012). In lay terms, people move around, to different degrees, for various lengths of time, and it is difficult to measure how and to what extent these dynamic movements shape health outcomes. In a review of commonly used rural taxonomies, Hart et al (2005) point out that county-level data both over-bounds and under-bounds space, and discuss the reasons why researchers often must fall back on them, including data availability, a lack of understanding by policymakers and legislators about variability and diversity across rural areas, and the political expediency of lumping people together rather than dividing them in data sets (Hart et al., 2005). Moreover, people’s perceptions of rurality may not fit the categories assigned to them: Onega et al (2019) showed significant discordance between residents’ self-reported rurality and zip code-derived categories, while Castle & Tak (2021) showed high discordance in self-reported rurality amongst pharmacists, raising questions about how the perception of one’s rurality may affect health-related behaviors as well as the provision of health care (Castle & Tak, 2021; Onega et al., 2019). Despite their many pitfalls and inadequacies, urban-rural categories are deployed in diverse ways as researchers attempt to understand how geography impacts health.
When it comes to research on drugs, Cano et al (2023) recently published a systematic review of county-level predictors of drug overdose mortality in the U.S., and found mixed results, with both positive and negative associations between rurality and overdose mortality across studies (Cano et al., 2023). They conclude, in corroboration with our analysis here, that their findings “emphasize sub-population variation in county-level risk factors for drug overdose mortality.” Despite the poor quality of county-level analyses in understanding ecologies and geographies of overdose risk, evidence reveals that there are meaningful geographic differences that shape risks of overdose, highlighting the need for better epidemiological and sociological tools to comprehend and address these differences. Some alternative classification schemes and relatively more nuanced conceptualizations of rurality exist, and Bennett et al suggest creating rural indices on a continuous scale by taking multiple factors into account, a good recommendation that we expand on below (Bennett et al., 2019). Unfortunately data related to drug overdose in the United States thus far have been limited from a geographic standpoint.
Within the U.S., the Centers for Disease Control and Prevention make overdose-related mortality data available according to a six-level urban-rural classification scheme developed by the National Center for Health Statistics in order to study associations between urbanization level of residence and health outcomes, depicted in the figures below (Ingram & Franco, 2006). There are disadvantages to characterizing U.S. opioid overdose patterns solely via these categories. The most important disadvantage, highlighted below, is the misleading narrative that overdose is mainly a rural problem, and, due to a social imaginary that associates rurality with whiteness, overdose has been misrepresented as primarily a White problem as well. In our analysis of existing data, we argue that rural and urban categories in available data sets can easily lead public health efforts astray when it comes to characterizing and preventing drug overdose.
Adding temporal variability to investigations of opioid overdose has been crucial, and epidemiologists have described four “waves” of U.S. opioid overdose epidemic since the turn of the 21st century (Ciccarone, 2019). The first was dominated by overdoses attributed to prescription opioid medications, beginning in 1996 with the FDA approval of OxyContin for moderate to severe chronic pain. The second was characterized by heroin as its use began to rise in the mid-2000s. The third started after 2013 when illicitly manufactured synthetic fentanyl entered the drug supply. Finally, the fourth is characterized by polysubstance use of illicit fentanyl, methamphetamine, and novel synthetic substances in various drug classes (Ciccarone, 2021). These waves have been distinct but overlapping and intertwined; each successive wave reshaped and fundamentally altered the opioid overdose epidemic, shifting the landscape of overdose risk in important ways. Nonetheless, this knowledge has not led to a critical examination of urban/rural distinctions in overdose risk. One pitfall of a focus on rural opioid use is that both popular media outlets and public health researchers have been slow to recognize that since 2015, the opioid epidemic has become more concentrated in urban areas. Across geographic location, opioid overdose has been and continues to be shaped by complex factors of social inequality, racism, policing, and disparities in court sentencing not reducible to false dichotomies and urban/rural divisions.
In our commentary, we apply a critical analysis of rurality to the study of drug-related morbidity and mortality in the U.S., in the interest of improving future public health research and interventions to reduce overdose. First, we highlight the reification of the concept of rurality, furthering insights from broad critiques of rurality and applying this analysis to research on opioids. Then, we use available national data with the six geographic categories described above to demonstrate some of the ways that public health research can reproduce oversimplified narratives about both rurality and overdose, leading to the erasure of racially marginalized persons from narratives about the opioid epidemic as well as from narratives about rurality. By superimposing additional data on race/ethnicity and income level, we illustrate how intersectional analyses and interdisciplinary methods offer a better understanding of geographic factors impacting overdose, and further. Finally, we state what we see as top priorities for future research into geographic factors impacting overdose. We identify existing research that provides a nuanced analysis of place and describe the impact that interdisciplinary research can have in rapidly assessing geographic risk and producing effective interventions to reduce drug-related harms.
Rurality Revisited
In our analysis, the problem is not simply that rural and urban categories are imperfectly measured. Rather, rurality and urbanicity are cultural constructs that have taken on a larger-than-life quality when it comes to opioids; a sustained focus on imagined attributes of rural and urban places detracts from, rather than contributes to, understanding risks of overdose. Here, we briefly review the narrative ways in which research and media approaches to overdose have come to reify rurality.
The prevailing narrative of the opioid epidemic is that it mostly has affected White rural populations, supported by some academic research highlighting a higher rate of overdose increase in rural-designated counties early in the epidemic (Ciccarone, 2019). While trends have since shifted, during these years, both central metropolitan and rural areas likely experienced similar absolute rates of increase in drug overdose (Rossen et al., 2013). However, focus was narrowed onto the greater percentage increase in overdose in rural populations: Paulozzi & Xi (2008) described for the years 1999–2004 a 371% increase in drug-related poisonings in counties classified as rural versus a 52% increase in counties classified as urban, while Rossen et al (2013) described a percentage increase of 394% in rural areas from 1999 to 2009 compared to an increase of 279% in urban areas (Paulozzi & Xi, 2008; Rossen et al., 2013). At the time, opioid prescriptions were disproportionately provided to White patients in lower income areas (consistent with well-documented class and race biases of physician interpretation of pain levels and opioid treatment non-compliance) where urban and rural neighborhood/regional overdose deaths were likewise concentrated (Friedman et al., 2019). In retrospect, these data fit the first “wave” of opioid overdose patterns described above. During this time, prescription opioids were responsible for the majority of opioid overdose deaths, and prescribing was driven by intensive lobbying and scientific racketeering practices by big pharmaceutical producers of analgesic medications (Hoffman, 2022).
Popular discourse and media coverage contributed to a sustained focus on rurality. Researchers and journalists described a “new” kind of drug epidemic caused by White rural economic decline and the amorphous, empirically inaccurate concept of “deaths of despair” being higher among White populations (K. D. Brown, 2013; Case & Deaton, 2015). Studies and stories focusing exclusively on rural populations or areas such as Appalachia or the Midwest may have contributed to the popular notion that the epidemic was rural in nature (Keyes et al., 2014). Rural populations were found to be more likely to graduate from unproblematic prescription opioid use to opioid use disorder compared to those living in urban areas, and researchers hypothesized that this may have been due to “prescription drug abuse” being “indigenous” and “socially acceptable” in certain rural areas (Cicero et al., 2007). Additional hypotheses for rural prescription opioid misuse rates included the influence of “rural family structure” and the structural stressors of modern rural living (Keyes et al., 2014). Mischaracterizing the crisis as rural has thus led to causal inferences about a “culture of rurality.” Such inferences are evocative of misleading and debunked “culture of poverty” narratives of the 1960s such as the ‘Moynihan Report,’ which argued that the primary cause of persistent Black poverty was due to “the tangle of pathology” inherent to Black culture in the United States (Benjamin, 2017; Steinberg, 2015).
When the second wave of the epidemic hit, heroin overtook prescription opioids as a leading cause of opioid overdose. Cicero et al. (2014) described the rise in heroin use by White individuals in small urban, suburban, and rural areas as the “changing face of heroin use in the United States” (Cicero et al., 2014). It became clear that it was not only opioid prescription use rising across these geographic areas. This rapid transition calls into question accounts focusing discussions on rural cultural norms of prescription misuse.
Since 2016, researchers have shown, the geographic pattern of drug overdose death rates has reversed, and the contribution of prescription opioids to overall opioid overdose deaths has simultaneously lessened (Hedegaard et al., 2019). In retrospect, “rural” or “non-urban” overdose death rates rose faster than urban overdose death rates for only a short period, and this trend quickly reversed (Hedegaard et al., 2019). In the meantime, the rising rates of overdose in urban areas, and the consistently and disproportionately high overdose rates among Native American individuals, received relatively little attention in either public health research or popular discourse (Friedman et al., 2023; Friedman & Hansen, 2021). Far from ignoring Appalachia, as Quinones claimed in his congressional address, research and media narratives have been focused on “rural America,” and in the process, have missed the ways that opioid-related harms continue to be shaped by structural racism.
Beyond Rural/Urban Divides
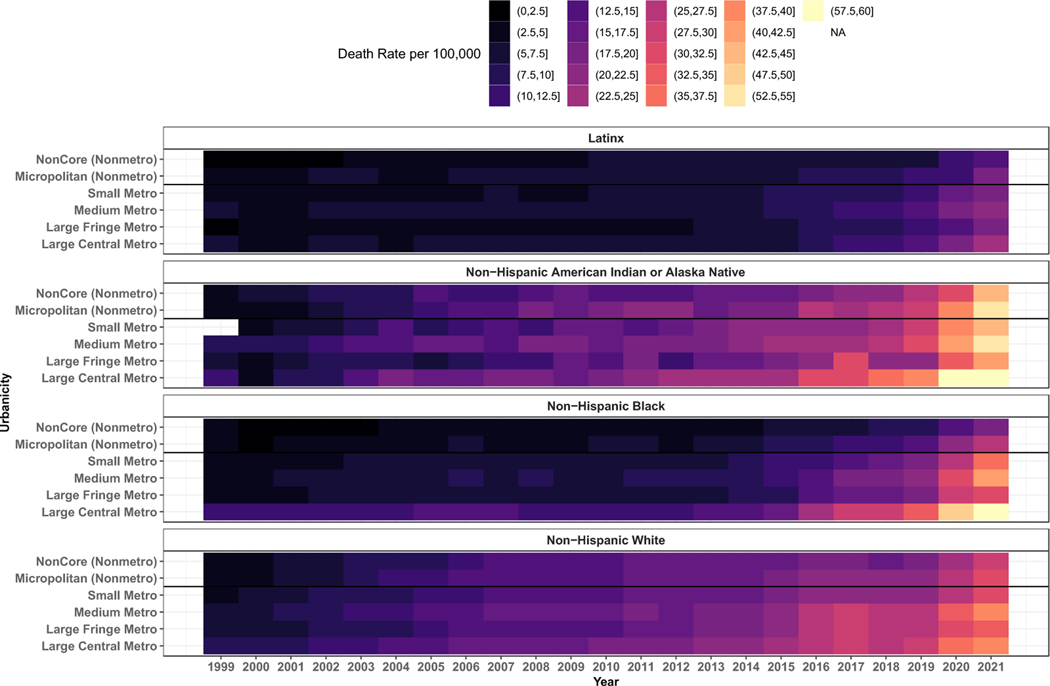
Several patterns emerge when drug-related overdose mortality rates from 1999–2021 are subdivided by race/ethnicity, income level, and urban-rural classification, using the 2013 NCHS Urban-Rural Classification Scheme for Counties (Figure 1, Figure 2). First, overdose rates are more stratified by race/ethnicity and income level than county population size. From 1999–2021, overdose rates have been consistently highest amongst non-Hispanic, American Indian or Alaska Natives. This high overdose rate is consistent across geographic location and county population size. Amongst non-Hispanic White individuals, overdose rates were initially higher than amongst non-Hispanic Black individuals, but in 2020, that trend reversed. Amongst White individuals, overdose rates have risen across both urban and rural counties, but since 2013, overdose rates have been higher within large central metro counties. Graphing each of the six categories of county designation, constructed using 2010 census-based data on U.S. counties that define four metropolitan and two nonmetropolitan levels, shows little variation in overdose rates by county type, while there has been a significant increase in overdose rates across all county types.
Figure 2 : Drug overdose mortality per 100,000 people by race/ethnicity and type of drug involved, 1999–2021.
Drug overdose mortality definitions are described in figure 1 caption. Race and ethnicity were used as defined in the WONDER and NCHS databases. Racial and ethnic groups were defined first by ethnicity (Hispanic or Latino) and subsequently by race (non-Hispanic American Indian or Alaska Native, non-Hispanic Black, and non-Hispanic White). This figure highlights that during the study period, overdose increased significantly and at rates that were more impacted by race/ethnicity than by level of urbanicity. All urban and rural-designated counties showed worsening rates of overdose in each racial/ethnic category between the years 1999–2021.
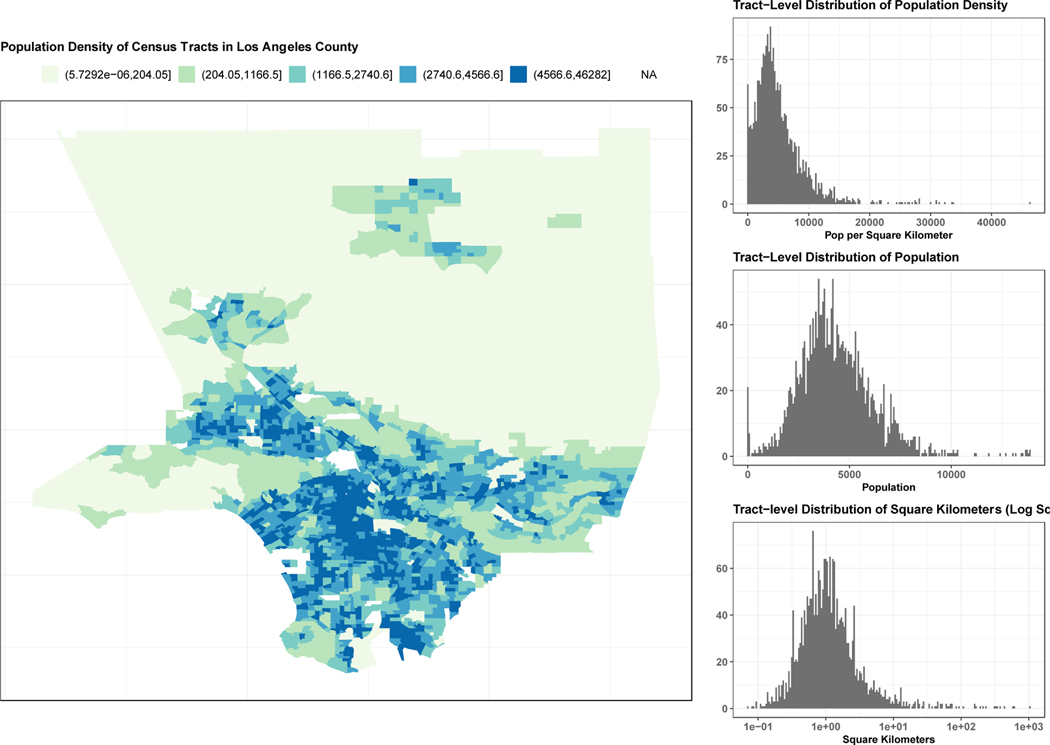
Important variations in overdose rates exist within large urban areas. However, differences within a given county are missing in representations using the six categories of metropolitan/non-metropolitan available from the CDC data. Urban counties such as Los Angeles have large geographic areas of low population density, equivalent to a small rural county. L.A. has more than 2,000 census tracks that vary considerably by rurality/urbanicity and other characteristics, illustrated below (Figure 3). Moreover, counties classified as “rural” often have a county center more densely populated than the surrounding municipalities. These distinctions are missed because the area is classified as a uniform large central metro area. As we will discuss below, interventions tailored to specific geographic needs are missed when such differences are erased. Given that overdose rates mapped here show more intra-county variability than inter-county variability, intersectional analyses are needed that include important social categories such as race/ethnicity, gender, and income level.
Figure 3: Population Density of Census Tracts in Los Angeles County in 2020.
This figure illustrates the wide range of census tract level population densities that can be observed within LA County. The histograms on the right display the population density by tract (population per sq. km), the overall populations by tract (population), and the areas of the tract (log-sq. km). The map shows population density for all tracts in Los Angeles County, excluding islands. Population data were drawn from the 2020 US census.
Complex interplays between public health categories and dynamic phenomena, including geographic displacement, incarceration, access to clinical/public health services (prescriptions, naloxone, low-threshold treatment), and housing status, are missed by static designations of county residency. Since displacement and incarceration shape the potential harms of drug use, effective public health intervention design requires more sophisticated surveillance tools and improved community engagement with people with lived experience. There is an urgent need to craft an agenda for drug overdose monitoring, prevention, and harm reduction.
Moreover, categorical designations including “rural” and “urban,” along with categories of race/ethnicity, can reify socially constructed difference. There is nothing intrinsic about rurality or urbanicity that determines risk of overdose. Yet associations found between rurality and overdose often attract distorted causal explanations. Rural/urban designations serve as poor proxies for meaningful causal factors such as social and political processes and structures that segregate individuals into or out of spaces of care or punishment. These geographic categories are not being used by researchers to produce intentionally misleading results; rather, they are shortcuts understandably utilized given the absence of more precise data and meaningful analytic tools, signaling the need for new ways to describe geographic factors affecting health outcomes.
An Agenda for Future Research: Describing Significant Geographic Drivers
Overdose data analyses deploying overly simplistic rural-urban categorizations result in incomplete and potentially misleading overdose narratives. These narratives have a long half-life in public health imaginations and in popular discourse. We urgently need effective public health surveillance tools that comprehend geographic differences in a timely manner without falling back on these inadequate categories as lone geographic variables. Here we suggest several steps public health researchers can take to build toward a robust surveillance and prevention toolkit.
First, researchers should pursue rigorous analyses of geographic difference that examine overdose data deploying rural-urban categories as only one factor, mapping additional categories simultaneously including race/ethnicity, gender, economic disadvantage (Pear et al., 2019), and social vulnerability (Joudrey et al., 2022), to obtain a more nuanced picture of a given place. Such analyses will provide a more accurate depiction of difference and similarity in overdose rates, provide insight into intra-county variability, and can further direct attempts to do root cause analysis.
Secondly, public health surveillance efforts should develop means to incorporate insights from qualitative social scientists with expertise in local geographic contexts more rapidly. Social scientists embedded in settings where drug use is prevalent can immediately observe changes in illicit drug supplies and effects of public health interventions that are typically only captured retrospectively in epidemiological surveillance through rises in overdose deaths. As social scientists observe and interact with people using drugs, they generate data about the ways that drug use, drug treatment, and overdose prevention are made meaningful, effective, or ineffective (Messac et al., 2013). Such data can help to identify overdose drivers by observing dynamic geographic factors such as economic displacement in situ. Immediate effects of drug supply changes, or of public health interventional strategies aimed at curtailing harms, can be understood more rapidly if epidemiological studies are designed with the help of timely social scientific observations.
Third, community engaged research approaches that collaborate or partner with people with lived and living experience and community organizations, should be prioritized and supported. Community based participatory research (CBPR) and community driven research (CDR) orientations are especially important for the timely and nuanced assessment of local issues and can help fill important knowledge gaps on emergent risks (G. Brown et al., 2019; Damon et al., 2017; Hayashi et al., 2012; Jozaghi et al., 2018).
Social scientists working in collaboration with organizations of directly impacted people (including people who use drugs, and communities most impacted by geographic displacement and incarceration) are well situated to offer potential explanations into the root causes of overdose. Simon et al (2022), for example, describes how the American national drug users union can generate information about spatialized risks of overdose by quickly integrating insights from 30 chapters and affiliate groups located across the U.S., and can also widely disseminate relevant public health information via weekly national virtual presentations. The authors focus on the implementation of methadone take-home doses at the beginning of the COVID-19 pandemic, aptly describing uneven implementation and barriers faced by clinic directors in specific locations, as well as the risks of revoking take-home doses, all of which are locally and regionally specific issues but with implications for federal public health policy and interventions aimed at increasing health care access. Recent studies by Brothers et al (2023), Figgatt et al (2021), and Meyerson et al (2022) are additional examples of community-driven work responding to issues faced by directly impacted people during COVID-19, with the goal of shaping nimble public health interventions.
These approaches reveal geographic and regional variability in the issues individuals and communities faced, and such approaches could be extended to addressing urgent issues with geographic specificity. While researchers have limited geographic scope, directly impacted community leaders and community organizations are already working in geographically specific areas and are intimately connected with the risks their communities face. Further collaborations and partnerships should be supported. Engaging with community members in multiple locations can expose which issues are regionally specific and which are signs of larger geographic trends.
Finally, accurate and timely public health surveillance data, in combination with social science observations of spatially contingent overdose risks, can produce a significantly improved, more geographically specific public health response to overdose. Small area estimates of overdose are appropriate for counties with larger populations and can inform a more nuanced understanding of overdose risk in large metropolitan areas with mixed rural components, especially. The recent spread of xylazine in the drug supply in Puerto Rico and the east coast of the U.S., for example, is an urgent public health matter that can be studied with the collaboration of ethnographic researchers located in regional sites and quantitative researchers using larger data sets on drug-related overdose (see Friedman et al., 2022). In terms of incarceration and displacement, richer understandings of the exceedingly high risk of overdose for people leaving jails and prisons has been crucial for defining the need for health care and harm reduction services (Green et al., 2018; Ranapurwala et al., 2018). Combining these data with qualitative data examining root causes and specific localized needs could lead to even more effective, nuanced approaches to preventing overdose, including increased provision of medications for opioid use disorder (MOUD) (Stopka et al., 2022)and access to harm reduction services in communities heavily impacted by incarceration (Krawczyk et al., 2022; Wakeman & Rich, 2015; Weizman et al., 2023) and approaches that address displacement itself such as through decarceration and access to housing. Overall, combining social scientific predictive capacity and root cause analysis with public health scalability and epidemiological monitoring capability can generate nimble and responsive public health interventions to reduce overdose.
Conclusion
Public health urgently needs more precise and nuanced modalities for assessing geographic factors that affect overdose risk. Oversimplified designations of “rural” and “urban” have for too long limited rather than enhanced our understanding of place. The notion of a mostly rural and hidden opioid epidemic, while narratively appealing, has misled the public and distracted researchers, delaying recognition of emerging trends in overdose. If researchers prioritize assessing risk by mapping geographic variables alongside other categories, and incorporate spatial insights from social science regarding root causes of overdose, we can create more responsive and effective interventions to reduce overdose.
Citations
- Benjamin R. (2017). Cultura Obscura: Race, Power, and “Culture Talk” in the Health Sciences. American Journal of Law & Medicine, 43(2–3), 225–238. 10.1177/0098858817723661 [DOI] [PubMed] [Google Scholar]
- Bennett KJ, Borders TF, Holmes GM, Kozhimannil KB, & Ziller E. (2019). What Is Rural? Challenges And Implications Of Definitions That Inadequately Encompass Rural People And Places. Health Affairs, 38(12), 1985–1992. 10.1377/hlthaff.2019.00910 [DOI] [PubMed] [Google Scholar]
- Brown G, Crawford S, Perry G-E, Byrne J, Dunne J, Reeders D, Corry A, Dicka J, Morgan H, & Jones S. (2019). Achieving meaningful participation of people who use drugs and their peer organizations in a strategic research partnership. Harm Reduction Journal, 16(1), 37. 10.1186/s12954-019-0306-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KD (2013, July 1). Heroin abuse problems plague rural Mass. Towns—The Boston Globe. BostonGlobe.Com. https://www.bostonglobe.com/lifestyle/health-wellness/2013/06/30/heroin/C1li7rwcJgz7MtSwKtEjUP/story.html [Google Scholar]
- Cano M, Oh S, Osborn P, Olowolaju SA, Sanchez A, Kim Y, & Moreno AC (2023). County-level predictors of US drug overdose mortality: A systematic review. Drug and Alcohol Dependence, 242, 109714. 10.1016/j.drugalcdep.2022.109714 [DOI] [PubMed] [Google Scholar]
- Case A, & Deaton A. (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences of the United States of America, 112(49), 15078–15083. 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle ME, & Tak CR (2021). Self-reported vs RUCA rural-urban classification among North Carolina pharmacists. Pharmacy Practice, 19(3), 2406. 10.18549/PharmPract.2021.3.2406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D. (2019). The Triple Wave Epidemic: Supply and Demand Drivers of the US Opioid Overdose Crisis. The International Journal on Drug Policy, 71, 183–188. 10.1016/j.drugpo.2019.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D. (2021). The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Current Opinion in Psychiatry, 34(4), 344–350. 10.1097/YCO.0000000000000717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, & Kurtz SP (2014). The Changing Face of Heroin Use in the United States: A Retrospective Analysis of the Past 50 Years. JAMA Psychiatry, 71(7), 821–826. 10.1001/jamapsychiatry.2014.366 [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Surratt H, Inciardi JA, & Munoz A. (2007). Relationship between therapeutic use and abuse of opioid analgesics in rural, suburban, and urban locations in the United States. Pharmacoepidemiology and Drug Safety, 16(8), 827–840. 10.1002/pds.1452 [DOI] [PubMed] [Google Scholar]
- Damon W, Callon C, Wiebe L, Small W, Kerr T, & McNeil R. (2017). Community-based participatory research in a heavily researched inner city neighbourhood: Perspectives of people who use drugs on their experiences as peer researchers. Social Science & Medicine (1982), 176, 85–92. 10.1016/j.socscimed.2017.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, & Hansen H. (2021). Black and Native Overdose Mortality Overtook that of White Individuals During the COVID-19 Pandemic (p. 2021.11.02.21265668). medRxiv. 10.1101/2021.11.02.21265668 [DOI]
- Friedman J, Hansen H, & Gone JP (2023). Deaths of despair and Indigenous data genocide. Lancet (London, England), 401(10379), 874–876. 10.1016/S0140-6736(22)02404-7 [DOI] [PubMed] [Google Scholar]
- Friedman J, Kim D, Schneberk T, Bourgois P, Shin M, Celious A, & Schriger DL (2019). Assessment of Racial/Ethnic and Income Disparities in the Prescription of Opioids and Other Controlled Medications in California. JAMA Internal Medicine, 179(4), 469–476. 10.1001/jamainternmed.2018.6721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Montero F, Bourgois P, Wahbi R, Dye D, Goodman-Meza D, & Shover C. (2022). Xylazine spreads across the US: A growing component of the increasingly synthetic and polysubstance overdose crisis. Drug and Alcohol Dependence, 233, 109380. 10.1016/j.drugalcdep.2022.109380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TC, Clarke J, Brinkley-Rubinstein L, Marshall BDL, Alexander-Scott N, Boss R, & Rich JD (2018). Postincarceration Fatal Overdoses After Implementing Medications for Addiction Treatment in a Statewide Correctional System. JAMA Psychiatry, 75(4), 405–407. 10.1001/jamapsychiatry.2017.4614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart LG, Larson EH, & Lishner DM (2005). Rural Definitions for Health Policy and Research. American Journal of Public Health, 95(7), 1149–1155. 10.2105/AJPH.2004.042432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi K, Fairbairn N, Suwannawong P, Kaplan K, Wood E, & Kerr T. (2012). Collective empowerment while creating knowledge: A description of a community-based participatory research project with drug users in Bangkok, Thailand. Substance Use & Misuse, 47(5), 502–510. 10.3109/10826084.2012.644110 [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Minino A, & Warner M. (2019). Urban–rural Differences in Drug Overdose Death Rates, by Sex, Age, and Type of Drugs Involved, 2017. 345, 8. [PubMed] [Google Scholar]
- Hoffman J. (2022, March 3). Sacklers and Purdue Pharma Reach New Deal With States Over Opioids. The New York Times. https://www.nytimes.com/2022/03/03/health/sacklers-purdue-oxycontin-settlement.html
- Ingram D, & Franco S. (2006). NCHS Urban-Rural Classification Scheme Methodology. Centers for Disease Control and Prevention. https://wonder.cdc.gov/wonder/help/cmf/urbanization-methodology.html [Google Scholar]
- Joudrey PJ, Kolak M, Lin Q, Paykin S, Anguiano V, & Wang EA (2022). Assessment of Community-Level Vulnerability and Access to Medications for Opioid Use Disorder. JAMA Network Open, 5(4), e227028. 10.1001/jamanetworkopen.2022.7028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jozaghi E, Greer AM, Lampkin H, & Buxton JA (2018). Activism and scientific research: 20 years of community action by the Vancouver area network of drug users. Substance Abuse Treatment, Prevention, and Policy, 13(1), 18. 10.1186/s13011-018-0158-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Cerdá M, Brady JE, Havens JR, & Galea S. (2014). Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health, 104(2), e52–59. 10.2105/AJPH.2013.301709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk N, Bandara S, Merritt S, Shah H, Duncan A, McEntee B, Schiff M, Ahmad NJ, Whaley S, Latimore A, & Saloner B. (2022). Jail-based treatment for opioid use disorder in the era of bail reform: A qualitative study of barriers and facilitators to implementation of a state-wide medication treatment initiative. Addiction Science & Clinical Practice, 17(1), Article 1. 10.1186/s13722-022-00313-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan M-P (2012). The Uncertain Geographic Context Problem. Annals of the Association of American Geographers, 102(5), 958–968. 10.1080/00045608.2012.687349 [DOI] [Google Scholar]
- Messac L, Ciccarone D, Draine J, & Bourgois P. (2013). The good-enough science-and-politics of anthropological collaboration with evidence-based clinical research: Four ethnographic case studies. Social Science & Medicine (1982), 99, 176–186. 10.1016/j.socscimed.2013.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onega T, Weiss JE, Alford-Teaster J, Goodrich M, Eliassen MS, & Kim SJ (2019). Concordance of Rural-Urban Self-identity and ZIP Code-derived Rural-Urban Commuting Area (RUCA) Designation. The Journal of Rural Health : Official Journal of the American Rural Health Association and the National Rural Health Care Association, 10.1111/jrh.12364. 10.1111/jrh.12364 [DOI] [PMC free article] [PubMed]
- Paulozzi LJ, & Xi Y. (2008). Recent changes in drug poisoning mortality in the United States by urban–rural status and by drug type. Pharmacoepidemiology and Drug Safety, 17(10), 997–1005. 10.1002/pds.1626 [DOI] [PubMed] [Google Scholar]
- Pear VA, Ponicki WR, Gaidus A, Keyes KM, Martins SS, Fink DS, Rivera-Aguirre A, Gruenewald PJ, & Cerdá M. (2019). Urban-rural variation in the socioeconomic determinants of opioid overdose. Drug and Alcohol Dependence, 195, 66–73. 10.1016/j.drugalcdep.2018.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranapurwala SI, Shanahan ME, Alexandridis AA, Proescholdbell SK, Naumann RB, Edwards D, & Marshall SW (2018). Opioid Overdose Mortality Among Former North Carolina Inmates: 2000–2015. American Journal of Public Health, 108(9), 1207–1213. 10.2105/AJPH.2018.304514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen LM, Khan D, & Warner M. (2013). Trends and Geographic Patterns in Drug-Poisoning Death Rates in the U.S., 1999–2009. American Journal of Preventive Medicine, 45(6), e19–e25. 10.1016/j.amepre.2013.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg S. (2015, June 24). The Moynihan Report at Fifty. Boston Review. https://www.bostonreview.net/articles/stephen-steinberg-moynihan-report-black-families-nathan-glazer/ [Google Scholar]
- Stopka TJ, Rottapel RE, Ferguson WJ, Pivovarova E, Toro-Mejias LD, Friedmann PD, & Evans EA (2022). Medication for opioid use disorder treatment continuity post-release from jail: A qualitative study with community-based treatment providers. International Journal of Drug Policy, 110, 103803. 10.1016/j.drugpo.2022.103803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot M. (2017, May 29). The Addicts Next Door. The New Yorker. https://www.newyorker.com/magazine/2017/06/05/the-addicts-next-door
- The Opioid Crisis: An Examination of How We Got here and How We Move Forward. (2018). https://www.govinfo.gov/content/pkg/CHRG-115shrg28300/html/CHRG-115shrg28300.htm
- U.S. Department of Health and Human Services. (2002, 2023). Am I Rural? Tool - Rural Health Information Hub. Rural Health Information Hub. https://www.ruralhealthinfo.org/am-i-rural [Google Scholar]
- Wakeman SE, & Rich JD (2015). Addiction Treatment Within U.S. Correctional Facilities: Bridging the Gap between Current Practice and Evidence-Based Care. Journal of Addictive Diseases, 34(2–3), Article 2–3. 10.1080/10550887.2015.1059217 [DOI] [PubMed] [Google Scholar]
- Weizman SR, El-Sabawi T, Brown S, Pulice T, & LaBelle R. (2023). To Save Lives, Prioritize Treatment For Opioid Use Disorder In Correctional Facilities. Health Affairs Forefront. 10.1377/forefront.20220615.871779 [DOI]