Abstract
Background. Mental health is declining in health care workers.
Objectives. To provide a comprehensive assessment of intervention literature focused on the support and treatment of mental health within the health care workforce.
Search Methods. We searched online databases (e.g., Medline, PsycINFO).
Selection Criteria. We selected manuscripts published before March 2022 that evaluated the target population (e.g., nurses), mental health outcomes (e.g., burnout, depression), and intervention category (e.g., mindfulness).
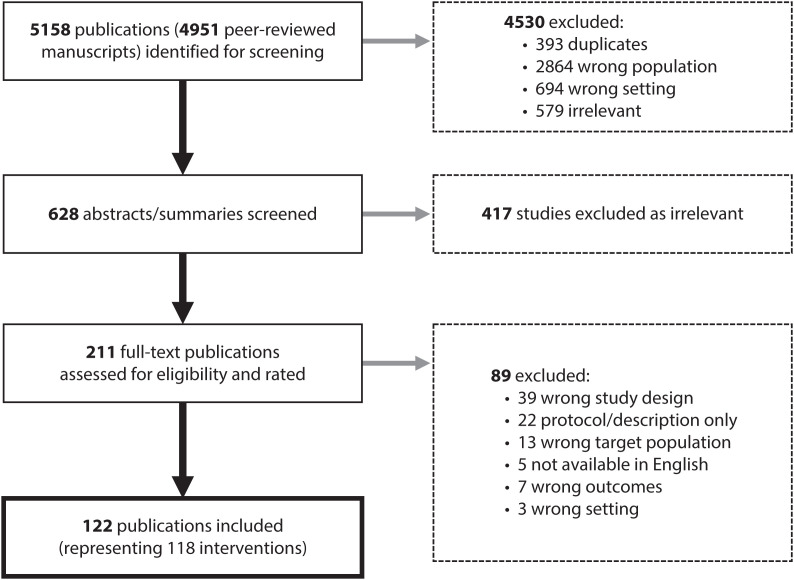
Data Collection and Analysis. Of 5158 publications screened, 118 interventions were included. We extracted relevant statistics and information.
Main Results. Twenty (17%) earned study quality ratings indicating design, analysis, and implementation strengths. Randomized controlled trials were used by 52 studies (44%). Thirty-eight percent were conducted in the United States (n = 45). Ninety (76%) reported significant changes, and 46 (39%) reported measurable effect sizes. Multiple interventions significantly reduced stress (n = 29; 24%), anxiety (n = 20; 17%), emotional exhaustion or compassion fatigue (n = 16; 14%), burnout (n = 15; 13%), and depression (n = 15; 13%).
Authors’ Conclusions. Targeted, well-designed mental health interventions can improve outcomes among health care workers.
Public Health Implications. Targeted health care‒focused interventions to address workers’ mental health could improve outcomes within this important and vulnerable workforce. (Am J Public Health. 2024;114(S2):S213–S226. https://doi.org/10.2105/AJPH.2023.307556)
PLAIN-LANGUAGE SUMMARY
We searched research publications to locate interventions that aimed to improve mental health among health care workers, such as nurses and medical doctors. The interventions were designed to offer support, such as training or counseling, to health care workers who were having symptoms of poor mental health, such as burnout, stress, or anxiety. We screened 5158 science journal articles and found 118 different interventions that had been offered to health care workers. Each article was evaluated to rate the degree to which they used accepted scientific methods of research. Most studies used strong research designs and contained valuable information about methods to improve mental health among health care workers. More than one third of the interventions were conducted in the United States, and most of the others were conducted in in Canada or Europe. Several interventions were successful in improving symptoms of stress, burnout, anxiety, and depression among health care workers.
Since 2020, mental health in the workplace has ranked among the most critical areas of research and practice by major organizations worldwide.1,2 In any given year, mental health issues create an economic burden in the United States of $225 billion attributable to costs associated with medical care and lost productivity.3 In the general workforce, mental health issues (e.g., distress, burnout) and mental illnesses (e.g., anxiety, depression) are associated with increased absenteeism and presenteeism (i.e., lost productivity or reduced performance), turnover, and increased rates of short- and long-term disability.4–6
Within the health care sector, the consequences of poor worker mental health have never been more troubling. Before COVID-19, more than 50% of clinicians reported experiencing some level of burnout because of challenges associated with short staffing, long hours, high job demands, and compassion fatigue.7–9 This number rose to 76% within the first year of the pandemic.10 Benefits surrounding mental illness (i.e., diagnosable psychological disorders classified within the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM-5; Washington, DC: American Psychiatric Association; 2013]) have grown substantially, with many organizations now offering funding for psychological services.11 Those who invest in mental health support and intervention see an estimated return on investment (ROI) of $4 per dollar invested.12
The purpose of this systematic review is to provide information from evidence-based literature describing mental health interventions that have been evaluated within health care populations and to evaluate the quality of those interventions. The target audience for implementation of this review is academicians and practitioners in public health, health care administrators, leaders, and safety and human resources professionals.
METHODS
For this review, we considered all relevant peer-reviewed and gray literature describing workplace mental health interventions targeting health care workers. We defined 3 key operational definitions by the following search terms (* indicates truncation, which allows for inclusion of all terms that begin with a specified string of characters):
-
•
Target population: physician, nurse, doctor, surgeon, provider, clinician, resident, “first responder,” “health care worker,” “healthcare worker,” “care provider,” “home care worker,” “homecare worker,” “home health aide,” “hospice worker,” “health aide”
-
•
Mental health: depress*, burnout, anx*, fatigue, stress, distress, strain, satisfaction, “quality of life,” well-being/wellbeing/“well being”/“well-being,” “mental health”
-
•
Intervention: intervention, program, training, computer-based, online, resource, app, program, “peer support,” “support group,” “social support,” “supervisor support,” policy, redesign, “work redesign,” “organization level,” “individual level,” “system level”
Key terms were made intentionally broad to include all medical professions, intervention types, and health care settings. Articles were gathered and initially screened for relevance by a senior research associate with advanced expertise in systematic review methodology (LA). The following sources were searched to identify potentially relevant publications, using an OR/AND search strategy combining the terms listed previously:
-
•
Ovid MEDLINE ALL
-
•
PsycINFO
-
•
PubMed
-
•
National Institute for Health and Care Excellence
-
•
Agency for Healthcare Research and Quality Project Database
-
•
Patient-Centered Outcomes Research Institute Project Database
-
•
National Institute for Occupational Safety and Health Project Database
-
•
Effective Healthcare Program
-
•
Google Scholar and DuckDuckGo
The initial search placed no restrictions on language, location, or time, searching all peer-reviewed and gray literature up to March 2022. We considered all studies employing either a pre‒post or post-only design to evaluate an intervention (broadly defined), including randomized controlled trials, quasi-experimental studies, qualitative post hoc evaluations, case studies, and program descriptions that included a data collection component. We mined systematic reviews and meta-analyses in health care mental health for additional references.13–29
We imported all relevant literature into Zotero30 and Covidence31 (systematic review software). Articles were rated by at least 2 senior researchers (WKA, JD, LA). In the first screening phase, articles were rated for inclusion or exclusion based on titles and abstracts (scale: Yes, No, Maybe). Second, a full-text review was conducted for articles rated as “Yes” or “Maybe” during the abstract review phase. Full publications were reviewed in depth to determine whether they met inclusion criteria: (1) recruited health care workers (broadly defined), (2) measured 1 or more mental health‒related outcomes, and (3) introduced a mental health‒focused intervention (e.g., resource, tool, exercise, policy, program, training) of some form. Exclusion criteria were (1) the intervention was not specific to mental health (e.g., job performance, patient care skills training), (2) the sample did not include at least 1 type of medical personnel, and (3) the full publication was not available in English.
Included articles underwent a quality rating process using a slightly adapted version of the validated Downs and Black (D&B) measure.32 The final D&B measure consisted of 25 items to rate articles’ study quality, external validity, internal validity—bias, internal validity—confounding, and power. A final item was added to the rating process to assess the raters’ confidence (1 = not at all confident; 4 = very confident) that the true intervention effect lies close to the authors’ estimate of the effect. This item was derived from the GRADE rating protocol.33
We analyzed level of agreement (percentage) and interrater reliability (IRR; Cohen’s κ)34,35 to assess whether raters met the desired threshold of 80% agreement at each phase of the process. Initial IRR (Cohen’s κ) was 0.79 during abstract review, 0.76 during full-text review, and 0.42 for the D&B study quality rating assessment (initial % agreement = 85%; R2 = 0.76). Following completion of the D&B rating and analysis phase, the team discussed points of disagreement, reconsidered the literature quality, and produced a revised consensus used in the final data tables (revised D&B IRR = 0.84).
RESULTS
The search yielded 5158 publications (4951 peer-reviewed) for preliminary screening (single-reviewer). After removing duplicates and irrelevant publications (e.g., patient-focused, nonwork setting), 628 abstracts were screened for inclusion, and 211 articles underwent full-text review (Figure 1).
FIGURE 1—
PRISMA Figure Depicting the Articles Examined and Included in the Systematic Review
Note. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
One hundred twenty-two publications (describing 118 interventions) met inclusion criteria. All included publications were peer-reviewed articles.
Study quality, assessed by the D&B criteria, had a maximum of 25 points available; the 3 highest rated36–38 received 22 points. Seventeen publications earned D&B quality ratings between 20 and 21 (14%).39–55 Forty-eight (41%) were rated between 15 and 1956–103; the remaining 42% were rated 14 or below.104–153 Overall, 13 articles (11%) received the highest confidence rating (4) while 19 (16%) received a rating of 3.5 (Table 1).
TABLE 1—
Number of Mental Health Intervention Articles Meeting Quality and Confidence Ratings by Ranges
| No. of Articles (%, Rounded) | |
| Quality ratinga (D&B) | |
| 20–22 | 20 (17) |
| 15–19 | 48 (41) |
| 6–14 | 50 (42) |
| Confidence ratingb | |
| 4 | 13 (11) |
| 3.5 | 19 (16) |
| 3 | 24 (20) |
| 2.5 | 22 (19) |
| 2 | 26 (23) |
| 1.5 | 8 (7) |
| 1 | 6 (5) |
Note. D&B = Downs and Black.32 Larger number = better rating.
Quality rating assessed study quality, external validity, internal validity—bias, internal validity—confounding, and power.
Confidence rating assessed raters’ confidence that the true intervention effect lies close to the authors’ estimate of the effect. Ratings calculated as a mean of two raters.
Study Design
Most interventions employed a randomized controlled (n = 552; 44%) trial or quasi-experimental design (n = 50; 42%), defined as either (1) a single-group study design (no comparison group) with 2 data collection timepoints or (2) a multigroup study with a single timepoint for data collection (postintervention only).
Setting
Evaluations were conducted in a hospital setting (n = 85; 72%), online (n = 15; 13%), at a nonhospital facility (n = 10; 8%), or miscellaneous (e.g., multiple; telephone, mail, unspecified; n = 8; 7%). Programs were typically implemented and accessed during work hours. Studies were conducted in 25 countries. Most interventions were conducted in the United States (n = 45; 38%), Italy, and Canada (n = 9 each; 8%).
Sample Sizes
The number of participants in the 118 interventions ranged from 11 to 1575. Forty-six (38%) had fewer than 50 participants (with 7 having fewer than 20); 27 (23%) had between 51 and 100 participants, and 27 (23%) had between 101 and 249 participants. Eighteen interventions (15%) had 250 or more participants; including 4 (3%) with 1000 or more (Table A, available as a supplement to the online version of this article at https://ajph.org).
Health Care Worker Occupation
Nurses were recruited to the interventions most frequently (n = 78; 66%), followed by physicians (n = 41; 35%). Twenty-two (19%) did not provide specific demographics on job titles.
Intervention Category
From the 118 interventions, 7 categories emerged:
-
1.
coping skills development (e.g., resilience-building, help-seeking, responding to stressors),
-
2.
mindfulness (e.g., mindfulness and similar practices such as directed meditation),
-
3.
health literacy and anti-stigma (e.g., mental health or general health-related awareness, stigma reduction),
-
4.
peer support (e.g., focus on teams, relationship building, or support between coworkers),
-
5.
organizational and system level (e.g., focus on policies, cultural change, and large-scale resources),
-
6.
reflection and relaxation (e.g., writing or artistic exercises, creativity, and conveying gratitude), and
-
7.
medical (e.g., medical, including pharmaceutical, treatment).
Thirty-one (26%) of the intervention methods fit into multiple categories. The number and percentage of categories is shown in Table 2 (see note).
TABLE 2—
Number of Mental Health Interventions by Intervention and Prevention Category
| No. of Interventions (%) | |
| Intervention category | |
| Coping skills development | 38 (32) |
| Health literacy and anti-stigma | 25 (21) |
| Mindfulness | 33 (28) |
| Peer support | 16 (14) |
| Organizational and system level | 11 (9) |
| Reflection and relaxation | 25 (21) |
| Medical | 4 (4) |
| Prevention category | |
| Primary | 20 (17) |
| Primary/secondary | 44 (37) |
| Secondary | 40 (33) |
| Secondary/tertiary | 13 (11) |
| Tertiary | 1 (1) |
Note. Thirty-one intervention methods fit within 2 or more intervention categories. These 31 interventions are counted multiple times within this table, leading to a total of 152.
Prevention Category
Workplace mental health interventions are often categorized as primary, secondary, or tertiary prevention. Primary interventions are designed to prevent illness, injury, and disease before they occur.154 Secondary interventions, often considered “early interventions,” are designed to treat an existing illness or injury, slow its progression, and help the individual recover. Tertiary interventions are designed to help people manage the long-term, and often complex, health problems associated with an injury or illness that has progressed to a point that is debilitating.
Most articles did not specify which prevention category they were targeting. To assess this factor, an expert in mental health interventions (JD) coded the literature into prevention categories. Some interventions are categorized as hybrid format, both primary and secondary or secondary and tertiary, because of the dual purpose of the intervention (e.g., an intervention focused on both preventing and reducing symptoms). Twenty interventions provided primary, 40 secondary, and one tertiary prevention. The number and percentage of categories are shown in Table 2.
Individual Versus Organizational Interventions
We coded interventions as organizational (e.g., changes to the work environment to support employee mental health), individual (e.g., education or training on coping or self-help strategies to prevent or reduce mental health symptoms), or a combination of the 2. Individual interventions predominated (n = 98; 83%), while only 8 interventions (7%) were coded as organizational and 12 (10%) judged to address both.
Mental Health Outcomes
Table 3 lists the mental health‒related outcomes measured across the intervention articles. The most common mental health outcomes were stress (n = 48; 41%), burnout (n = 40; 34%), and anxiety, depression, and emotional exhaustion or compassion fatigue (each had an n = 31; 26%); this is consistent with the most frequently identified mental health issues reported by health care professionals before and during the COVID-19 pandemic (2020–2022).9,12
TABLE 3—
Mental Health Outcomes Targeted by Interventions
| Outcomes | No. of Interventions | No. With Significant Changesa | No. With Effect Sizesb | Effect Size, No. | ||
| Large | Medium | Small | ||||
| General health and well-being | ||||||
| Sleep/exhaustion | 12 | 7 | 3 | 0 | 2 | 1 |
| Mental health | 14 | 5c | 4c | 2c | 1c | 1 |
| General health | 12 | 8c | 4 | 2 | 1 | 1 |
| Affect | 10 | 7 | 6 | 2 | 4 | 0 |
| Well-being | 13c | 10c | 7 | 4 | 1 | 2 |
| Quality of life | 11 | 8 | 7 | 4 | 2 | 1 |
| Somatization | 3 | 2 | 0 | 0 | 0 | 0 |
| Stress and strain | ||||||
| Stress | 48 | 29 | 14 | 5 | 6 | 3 |
| Distress | 14 | 9 | 4 | 3 | 0 | 1 |
| Posttraumatic stress disorder | 6 | 2 | 1 | 1 | 0 | 0 |
| Strain | 5 | 3 | 2 | 1 | 0 | 1 |
| Depression | 31 | 15 | 8 | 4 | 3 | 1 |
| Anxiety | 32 | 20c | 12c | 6c | 2 | 4 |
| Burnout and compassion fatigue | ||||||
| Burnout | 40 | 15 | 6 | 2 | 3 | 1 |
| Emotional exhaustion or compassion fatigue | 30 | 16 | 11 | 4 | 2 | 5 |
| Emotions and attitudes | ||||||
| Psychosocial functioning | 5 | 2 | 1 | 1 | 0 | 0 |
| Happiness | 2 | 1 | 0 | 0 | 0 | 0 |
| Anger | 2 | 1 | 0 | 0 | 0 | 0 |
| Mental health stigma | 2 | 2 | 0 | 0 | 0 | 0 |
| Resilience and coping | ||||||
| Social support | 15 | 8 | 2 | 1 | 0 | 1 |
| Coping | 10 | 1 | 1 | 0 | 1 | 0 |
| Demands | 6 | 1 | 1 | 0 | 1 | 0 |
| Support seeking | 5 | 2 | 0 | 0 | 0 | 0 |
| Drinking behaviors | 6 | 3 | 0 | 0 | 0 | 0 |
| Work‒life balance | 7 | 3 | 2 | 0 | 1 | 1 |
| Resilience | 7 | 6 | 4 | 1 | 2 | 1 |
| Mindfulness | ||||||
| Mindfulness | 13 | 8 | 6 | 2 | 3 | 1 |
| Self-compassion | 7 | 5 | 4 | 0 | 2 | 2 |
| Psychological flexibility | 4 | 2 | 1 | 0 | 1 | 0 |
| Awareness | 2 | 2 | 0 | 0 | 0 | 0 |
| Self-efficacy and self-esteem | ||||||
| Confidence | 10 | 7 | 3 | 1 | 1 | 1 |
| Self-efficacy | 8 | 5 | 2 | 1 | 1 | 0 |
| Inadequacy | 1 | 1 | 0 | 0 | 0 | 0 |
| Civility and relationships | ||||||
| Trust | 1 | 1 | 1 | 1 | 0 | 0 |
| Civility/incivility | 5 | 5 | 2 | 1 | 0 | 1 |
| Empathy | 2 | 2 | 2 | 0 | 2 | 0 |
| Respect | 2 | 2 | 1 | 1 | 0 | 0 |
Number of interventions with at least 1 significant change in a measure over time from baseline to follow-up or in rare cases from postintervention to a subsequent follow-up.
Number of studies that included effect sizes.
Two intervention methods in 3 studies produced 2 differences, and 2 of those produced 2 effect-size results. Effect sizes were defined as follows: Cohen’s d: small = 0.2; medium = 0.5; large = 0.8; ŋ2 or partial ŋ2: small = 0.01; medium = 0.06; large = 0.14; R2: small = 0.00; medium = 0.03; large = 0.14; and Δ: small = 0.2; medium = 0.5; large = 0.8. Details are noted in Table A (available as a supplement to the online version of this article at https://ajph.org).
Statistically Significant Changes and Effect Sizes
Statistically significant improvements were reported by 90 (76%) of the interventions. Measures of the effect size were reported, or in some cases calculated by the authors using reported data and an effect size calculator,155 by 46 interventions (39%). Effect sizes were calculated with Cohen’s d (small = 0.2; medium = 0.5; large = 0.8),156 η-squared (ŋ2) or partial ŋ2 (small = 0.01; medium = 0.06; large = 0.14),157 the correlation statistic R2 (small = 0.00; medium = 0.03; large = 0.14),156,157 and delta (Δ; small = 0.2; medium = 0.5; large = 0.8).158 See Table 3 for effect sizes by outcome.
Overall, several interventions reported significant changes in key outcome measures: stress (29 interventions; 14 effect sizes, 5 large), anxiety (20 interventions; 12 effect sizes, 6 large), depression (15 interventions; 8 effect sizes; 4 large), emotional exhaustion or compassion fatigue (16 interventions; 11 effect sizes, 4 large), and burnout (15 interventions; 6 effect sizes, 2 large). In addition, multiple interventions improved most measures in the category of general health and well-being. See Table 3 and Table B (available as a supplement to the online version of this article at https://ajph.org).
Time Commitment for Participants
Many (n = 90; 76%) of the publications noted the amount of time spent on the intervention at work by the participants (listed in Table A). The range was 0 (conducted outside work time) to 50 hours; 55 interventions (47%) required 10 or fewer hours.
DISCUSSION
The 118 interventions (122 publications) described in this review focused on outcomes related to general mental health and well-being, as well as mental health issues and illnesses, including depression, anxiety, psychological strain, stress, burnout, and compassion fatigue. Findings suggest that targeted, well-designed mental health‒focused interventions have the potential to lead to significant improvements in mental health outcomes among health care workers.
Interventions That Improved Outcome Measures
Of the 118 interventions included in this review, 97 were associated with significant reductions in mental health outcome measures highly relevant to the health care sector (i.e., stress: n = 29; anxiety: n = 20]; emotional exhaustion or compassion fatigue: n = 16; burnout: n = 16; and depression: n = 15). Randomized controlled trial designs were used in several of these studies, showing improvement in stress (n = 17), emotional exhaustion or compassion fatigue (n = 10), depression (n = 9), anxiety (n = 9), and burnout (n = 7). Importantly, nearly one fourth (n = 27; 23%) of the observed improvements in mental health outcome measures met the criteria for a large effect size, and 12 (30%) of the 40 interventions rated 18 (D&B) or better produced large effect-size changes in outcome measures including all of the 5 highly relevant outcomes, indicating that the changes reported by participants were large enough to be meaningful in the real world.156 By participating in interventions associated with large effect sizes in mental health outcomes, health care workers may experience real, perceptible improvements in their mental health.
Interventions that incorporated mindfulness and coping skills development using formal therapeutic approaches (e.g., acceptance and commitment therapy [ACT], cognitive behavioral therapy [CBT]) tended to result in the most significant changes in measures of mental health outcomes. Though there were proportionately fewer, relaxation and reflection interventions with techniques that varied much more widely (e.g., art therapy, expressive writing, yoga) were also associated with positive changes in mental health outcome measures. Mindfulness, coping skills development, and relaxation and reflection interventions repeatedly influenced measures of burnout, stress, depression, emotional exhaustion, and general well-being (Table A).
Interventions that incorporated multiple foci (e.g., increased awareness of mental health and training for workers on how to improve coping skills) were also associated with improvements in mental health outcome measures. For instance, interventions focused solely on education and awareness related to health literacy and anti-stigma rarely resulted in changes to mental health outcome measures. Instead, they tended to be associated with improvement in more general outcomes, such as improved confidence and reduced mental health stigma. However, when combined with other intervention strategies, such as coping skills development, reflection and relaxation, and peer support, interventions using health literacy and anti-stigma strategies were associated with improvements in mental health measures. Although there were few interventions that employed medical intervention methods (e.g., cannabidiol therapy, transcranial magnetic stimulation), these intervention strategies were also associated with significant reductions in measures of anxiety and depression, indicating significant promise.
Several interventions reported multiple outcome measure changes with large effect sizes: Civility, Respect, and Engagement at Work (CREW; 7 outcomes); Stress Management and Resiliency Training (SMART; 5 outcomes); MINDBODYSTRONG and Brief Mindfulness-Based Stress Reduction (MBSR; 4 each); and Mindfulness-Based Resilience Training (MBRT), Acupressure and Emotional Freedom Techniques (EFT), expressive writing, and enhancing resilience (3 each). Considering specific mental health outcomes, 9 interventions produced large effect size changes for measures of stress, strain, or distress (i.e., gratitude journaling, ACT+CBT, repetitive transcranial magnetic stimulation (RTMS), Acupressure and EFT, SMART, MINDBODYSTRONG, reflective debriefing, enhancing resilience, ACT); 5 produced large effect-size changes in anxiety measures (Acupressure and EFT, SMART, MINDBODYSTRONG, stretch-release and cognitive relaxation, Life and Death—The Same Preparation), and in burnout and emotional exhaustion or compassion fatigue measures (MBRT, Mental Health Promotion, Acupressure and EFT, Promote Professionalism and Mental Health, MBSR); and 4 resulted in large changes in depression (RTMS, expressive writing, MINDBODYSTRONG, enhancing resilience). All but 3 of these interventions were designed as randomized controlled trials, and 5 of the interventions listed for stress, 2 for anxiety, 1 for depression, and 4 for emotional exhaustion or compassion fatigue and burnout carry D&B ratings of 18 or more.
Among the most highly rated studies (D&B quality ratings), interventions that focused on coping skills development and mindfulness had the most studies (n = 26; 22% each) to demonstrate improvements in mental health outcome measures. Coping skills development interventions were also associated with the highest number of large intervention effect sizes (n = 6) among the 5 key outcome measures, and mindfulness was associated with 4. Following coping skills development interventions was “reflection and relaxation” (n = 20; 17%; 4 large effect sizes in key outcome measures). The most impactful coping skills development interventions were SMART (7 outcome measures improved, 7 with effect sizes, 5 large; D&B rating = 20; though a quasi-experimental design) and Acupressure and EFT (3 outcomes, 3 with effect sizes, all large; D&B = 19; randomized controlled trial), and the most impactful mindfulness interventions were Mindfulness-Based Cognitive Therapy for Life (6 outcomes, 6 with effect sizes, 1 large; D&B = 21; randomized controlled trial) and ACT+CBT (4 outcomes, 4 with effect sizes, 2 large; D&B = 19; randomized controlled trial).
Interventions that targeted peer support or organizational- and system-level improvements tended to produce mixed findings. Some peer-focused interventions demonstrated medium or large effect size results on multiple work outcome measures (e.g., turnover intentions, job satisfaction) and personal outcomes (e.g., affect; see CREW), but not on mental health outcomes. Others only had small to medium effect-size changes on mental health, but none on work. Patterns of results were similar for organizational- and system-level interventions unless combined with individual intervention strategies, which tended to be associated with mental health improvements—as was the case with multifocused interventions incorporating peer support strategies.
It is important to acknowledge that a statistically significant improvement in a mental health outcome does not necessarily translate to a significant, recognizable, or universal improvement in health for all participants. Organizations must recognize that intervention “effectiveness” will vary among workers depending on outcomes of interest, individual differences, and the status of employees’ mental health at the onset of the intervention.
Study Quality
Most reviewed evaluations had high study quality ratings; 20 earned a high-quality rating (greater than 19 on a 25-point scale), and another 48 earned relatively high ratings (15‒19) for a total of 58% of the interventions, based on research methods and design elements, indicating design and implementation strengths. Among the 118 interventions, there were 52 randomized controlled trials and 50 quasi-experimental designs. Thus, 44% of the evaluations used the most robust design methods used in field research, while an additional 42% used strong designs but without the strength of randomization to avoid biases. Similarly, 32 (27%) earned the authors’ confidence ratings of 3.5 or higher on a 4-point scale. Findings associated with higher-quality studies, such as those that are adequately powered and used more rigorous evaluation methods (e.g., randomized controlled trials), are more likely to be reflective of true, and potentially replicable, benefits of their associated interventions.
The findings associated with lower-quality study designs may still be valid and reliable, but it is more challenging to determine whether findings, or a lack thereof, were attributable to chance, inadequate power, or confounding variables. For instance, some of the evaluations lacked rigorous designs, used underpowered sample sizes (few reported power analyses), did not use control groups or intent-to-treat analytic strategies, and did not explore the long-term duration of the intervention effects. Most evaluations (62%) relied on 100 or fewer participants, with 39% using 50 or fewer participants. Only 15% recruited more than 250 participants. These methodological challenges make it unclear whether nonsignificant outcomes were the result of underpowered samples or ineffective interventions.
Availability and Cost
Cost-related justifications or ROI calculations were rare among the evaluated interventions. Of the 6 that included a measure of ROI, 4 saw significant improvements in worker attendance (e.g., absences). When implementing intervention programs, organizations should aim to weigh the ratio of costs to benefits associated with intervention participation.
Nearly one third (32%) of the interventions are described in sufficient detail to enable implementation or are available from the intervention authors. Of those that were not adequately described, several were in-person programs and others were system-wide interventions that required tailored individual efforts for implementation within a specific system. The 37 interventions for which websites, guides, or other source materials are publicly available are identified in Table A.
When planning or selecting an intervention, organizations should (1) select for the specific health outcomes they are trying to improve (e.g., stress reduction, general well-being), (2) consider through what mechanisms their chosen intervention will initiate those improvements (e.g., knowledge gain, better access to work support), and (3) identify who will most benefit from them. To truly assess impact, it is important to continue postintervention measurement over time, as appropriate. For instance, if a health care system is investigating the impact of a counseling program on depression, symptoms may take many weeks or months to improve or resolve. Therefore, the extent to which an intervention will be “effective” can be dependent on its duration, the outcomes of interest, and how and when they are being measured.
Limitations and Future Directions
Only articles published up to March 2022 were reviewed, potentially omitting important research conducted during the COVID-19 pandemic. This review focused solely on mental health interventions conducted within the health care sector. As a result, there are effective mental health interventions applied in other industry sectors that were excluded. Finally, despite the promising nature of this literature, the efficacy of many of these programs remains largely undetermined because of small sample sizes or insufficient evaluation methods. Most interventions focused on the individual, highlighting an important gap in organization-focused mental health intervention research within health care. While this literature has not yet reached the point of providing a “1-stop shop” for health care workers’ mental health programs, the growing breadth of the literature is very promising, as is the current prioritization of these issues at organizational, national, and policy levels.
ACKNOWLEDGMENTS
Funding for this project, “Assimilate Evidence-Based Interventions, Best Practices, and Current Resources on Healthcare Worker Mental Health [Contract # 500455-20/PO 2021-0294],” was provided by the US Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health (NIOSH) through the American Rescue Plan. This work was also partly supported by the Oregon Institute of Occupational Health Sciences at OHSU via funds from the Division of Consumer and Business Services of the State of Oregon (ORS 656.630).
We received excellent, clear, and prompt guidance from NIOSH program officer Thomas R. Cunningham as we conducted this systematic review.
CONFLICTS OF INTEREST
OHSU and W. K. Anger have a financial interest in Northwest Education, Training and Assessment, a company that may have a commercial interest in the results of this research and technology. This potential conflict of interest has been reviewed and managed by OHSU.
HUMAN PARTICIPANT PROTECTION
This research was based on publicly accessible research publications; no human participants were involved in this systematic review.
REFERENCES
- 1.Kelloway EK , Dimoff JK , Gilbert S. Mental health in the workplace. Annu Rev Organ Psychol Organ Behav. 2023;10(1):363–387. 10.1146/annurev-orgpsych-120920-050527 [DOI] [Google Scholar]
- 2.Staglin G. Getting mental health back on the world’s agenda. Forbes. January 26, 2022. Available at: https://www.forbes.com/sites/onemind/2022/01/26/getting-mental-health-back-on-the-worlds-agenda. Accessed June 9, 2022.
- 3.Open Minds. The U.S. mental health market: $225.1 billion in spending in 2019: an OPEN MINDS market intelligence report. 2020. Available at: https://openminds.com/intelligence-report/the-u-s-mental-health-market-225-1-billion-in-spending-in-2019-an-open-minds-market-intelligence-report. Accessed May 26, 2022.
- 4.Dewa CS , Goering P , Goering P , Lin E , Paterson M. Depression-related short-term disability in an employed population. J Occup Environ Med. 2002;44(7):628–633. 10.1097/00043764-200207000-00007 [DOI] [PubMed] [Google Scholar]
- 5.Dewa CS , Loong D , Bonato S , Thanh NX , Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14(1):325. 10.1186/1472-6963-14-325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dewa CS , McDaid D. Investing in the mental health of the labor force: epidemiological and economic impact of mental health disabilities in the workplace. In: Schultz IZ , Rogers ES , eds. Work Accommodation and Retention in Mental Health. New York, NY: Springer; 2011:33‒51. 10.1007/978-1-4419-0428-7_2 [DOI] [Google Scholar]
- 7.Fiabane E , Giorgi I , Sguazzin C , Argentero P. Work engagement and occupational stress in nurses and other healthcare workers: the role of organisational and personal factors. J Clin Nurs. 2013;22(17-18):2614–2624. 10.1111/jocn.12084 [DOI] [PubMed] [Google Scholar]
- 8.Johnson & Johnson Foundation. The mental health of healthcare workers in COVID-19. Available at: https://mhanational.org/mental-health-healthcare-workers-covid-19. Accessed November 17, 2023.
- 9.Li Y , Scherer N , Felix L , Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLoS ONE. 2021;16(3):e0246454. 10.1371/journal.pone.0246454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Institute for Health Care Management Foundation. Physician burnout & moral injury: the hidden health care crisis. March 22, 2021. Available at: https://nihcm.org/publications/physician-burnout-suicide-the-hidden-health-care-crisis. Accessed June 9, 2022. [Google Scholar]
- 11.Miller MW , Wolf EJ , Kilpatrick D , et al. The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychol Trauma. 2013;5(6):501–512. 10.1037/a0029730 [DOI] [Google Scholar]
- 12.National Safety Council. Prioritizing employee mental health. June 1, 2022. Available at: https://www.nsc.org/workplace/safety-topics/employee-mental-health. Accessed June 1, 2022.
- 13.Bresesti I , Folgori L , De Bartolo P. Interventions to reduce occupational stress and burn out within neonatal intensive care units: a systematic review. Occup Environ Med. 2020;77(8): 515–519. 10.1136/oemed-2019-106256 [DOI] [PubMed] [Google Scholar]
- 14.Cocchiara RA , Peruzzo M , Mannocci A , et al. The use of yoga to manage stress and burnout in healthcare workers: a systematic review. J Clin Med. 2019;8(3):284. 10.3390/jcm8030284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drissi N , Ouhbi S , Marques G , de la Torre Diez I , Ghogho M , Janati Idrissi MA. A systematic literature review on e-mental health solutions to assist health care workers during COVID-19. Telemed J E Health. 2021;27(6):594–602. 10.1089/tmj.2020.0287 [DOI] [PubMed] [Google Scholar]
- 16.Hooper JJ , Saulsman L , Hall T , Waters F. Addressing the psychological impact of COVID-19 on healthcare workers: learning from a systematic review of early interventions for frontline responders. BMJ Open. 2021;11(5):e044134. 10.1136/bmjopen-2020-044134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marine A , Ruotsalainen J , Serra C , Verbeek J. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. 2006;(4): CD002892. [DOI] [PubMed] [Google Scholar]
- 18.Nicolakakis N , Lafantaisie M , Letellier MC , et al. Are organizational interventions effective in protecting healthcare worker mental health during epidemics/pandemics? A systematic literature review. Int J Environ Res Public Health. 2022; 19(15):9653. 10.3390/ijerph19159653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nikunlaakso R , Selander K , Oksanen T , Laitinen J. Interventions to reduce the risk of mental health problems in health and social care workplaces: a scoping review. J Psychiatr Res. 2022; 152:57–69. 10.1016/j.jpsychires.2022.06.004 [DOI] [PubMed] [Google Scholar]
- 20.Phillips CS , Becker H. Systematic review: expressive arts interventions to address psychosocial stress in healthcare workers. J Adv Nurs. 2019; 75(11):2285–2298. 10.1111/jan.14043 [DOI] [PubMed] [Google Scholar]
- 21.Pollock A , Campbell P , Cheyne J , et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. 2020;11(11):CD013779. 10.1002/14651858.CD013779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pospos S , Young IT , Downs N , et al. Web-based tools and mobile applications to mitigate burnout, depression, and suicidality among healthcare students and professionals: a systematic review. Acad Psychiatry. 2018;42(1):109–120. 10.1007/s40596-017-0868-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rao D , Elshafei A , Nguyen M , Hatzenbuehler ML , Frey S , Go VF. A systematic review of multi-level stigma interventions: state of the science and future directions. BMC Med. 2019;17(1):41. 10.1186/s12916-018-1244-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruotsalainen J , Serra C , Marine A , Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health. 2008;34(3): 169–178. 10.5271/sjweh.1240 [DOI] [PubMed] [Google Scholar]
- 25.Ruotsalainen JH , Verbeek JH , Marine A , Serra C. Preventing occupational stress in healthcare workers [update in Cochrane Database Syst Rev. 2023;5(5):CD002892]. Cochrane Database Syst Rev. 2015;(4):CD002892. 10.1002/14651858.CD002892.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schoonover KL , Hall-Flavin D , Whitford K , Lussier M , Essary A , Lapid MI. Impact of poetry on empathy and professional burnout of health-care workers: a systematic review. J Palliat Care. 2020;35(2):127–132. 10.1177/0825859719865545 [DOI] [PubMed] [Google Scholar]
- 27.Yarker J , Lewis R , Sinclair A , Michlig G , Munir F. Meta-synthesis of qualitative research on the barriers and facilitators to implementing workplace mental health interventions. SSM-Ment Health (Lond). 2022;2:100148. 10.1016/j.ssmmh.2022.100148 [DOI] [Google Scholar]
- 28.Zace D , Hoxhaj I , Orfino A , Viteritti AM , Janiri L , Di Pietro ML. Interventions to address mental health issues in healthcare workers during infectious disease outbreaks: a systematic review. J Psychiatr Res. 2021;136:319‒333. 10.1016/j.jpsychires.2021.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X , Sun F , Wang Y , Zhu Z. Establishment of a psychological intervention mechanism for healthcare workers facing public health emergencies in the context of the COVID-19 outbreak. Int J Health Plann Manage. 2021; 36(6):2424‒2429. 10.1002/hpm.3306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Corporation for Digital Scholarship. Zotero. 2016. Available at: https://www.zotero.org/download. Accessed November 11, 2017.
- 31. Veritas Health Innovation. Covidence Systematic Review Software. Available at: https://www.covidence.org . Accessed March 8, 2021. . [Google Scholar]
- 32.Downs SH , Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6): 377–384. 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guyatt GH , Oxman AD , Vist GE , et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37–46. 10.1177/001316446002000104 [DOI] [Google Scholar]
- 35.Prieto L , Lamarca R , Casado A , Alonso J. The evaluation of agreement on continuous variables by the intraclass correlation coefficient. J Epidemiol Community Health. 1997;51(5): 579–581. 10.1136/jech.51.5.579-a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheng ST , Tsui PK , Lam JHM. Improving mental health in health care practitioners: randomized controlled trial of a gratitude intervention. J Consult Clin Psychol. 2015;83(1):177–186. 10.1037/a0037895 [DOI] [PubMed] [Google Scholar]
- 37.Clemow LP , Pickering TG , Davidson KW , et al. Stress management in the workplace for employees with hypertension: a randomized controlled trial. Transl Behav Med. 2018;8(5): 761–770. 10.1093/tbm/iby018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maatouk I , Müller A , Angerer P , et al. Healthy ageing at work—efficacy of group interventions on the mental health of nurses aged 45 and older: results of a randomised, controlled trial. PLoS One. 2018;13(1):e0191000. 10.1371/journal.pone.0191000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alexander GK , Rollins K , Walker D , Wong L , Pennings J. Yoga for self-care and burnout prevention among nurses. Workplace Health Saf. 2015;63(10):462–470. 10.1177/2165079915596102 [DOI] [PubMed] [Google Scholar]
- 40.Barrett K , Stewart I. A preliminary comparison of the efficacy of online acceptance and commitment therapy (ACT) and cognitive behavioural therapy (CBT) stress management interventions for social and healthcare workers. Health Soc Care Community. 2021;29(1): 113–126. 10.1111/hsc.13074 [DOI] [PubMed] [Google Scholar]
- 41.Crippa JAS , Zuardi AW , Guimaraes FS , et al. Efficacy and safety of cannabidiol plus standard care vs standard care alone for the treatment of emotional exhaustion and burnout among frontline health care workers during the COVID-19 pandemic: a randomized clinical trial. JAMA Netw Open. 2021;4(8):e2120603. 10.1001/jamanetworkopen.2021.20603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Errazuriz A , Schmidt K , Undurraga EA , et al. Effects of mindfulness-based stress reduction on psychological distress in health workers: a three-arm parallel randomized controlled trial. J Psychiatr Res. 2022;145:284–293. 10.1016/j.jpsychires.2020.11.011 [DOI] [PubMed] [Google Scholar]
- 43.Gärtner FR , Nieuwenhuijsen K , Ketelaar SM , van Dijk FJH , Sluiter JK. The Mental Vitality @ Work Study: effectiveness of a mental module for workers’ health surveillance for nurses and allied health care professionals on their help-seeking behavior. J Occup Environ Med. 2013;55(10):1219–1229. 10.1097/JOM.0b013e31829f310a [DOI] [PubMed] [Google Scholar]
- 44.Gupta S , Kumar M , Rozatkar AR , et al. Feasibility and effectiveness of telecounseling on the psychological problems of frontline healthcare workers amidst COVID-19: a randomized controlled trial from central India. Indian J Psychol Med. 2021;43(4):343–350. 10.1177/02537176211024537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hammer LB , Johnson RC , Crain TL , et al. Intervention effects on safety compliance and citizenship behaviors: evidence from the work, family, and health study. J Appl Psychol. 2016; 101(2):190–208. 10.1037/apl0000047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hersch RK , Cook RF , Deitz DK , et al. Reducing nurses’ stress: a randomized controlled trial of a web-based stress management program for nurses. Appl Nurs Res. 2016;32:18–25. 10.1016/j.apnr.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kozasa EH , Lacerda SS , Polissici MA , et al. An intervention to increase situational awareness and the culture of mutual care (Foco) and its effects during COVID-19 pandemic: a randomized controlled trial and qualitative analysis. Front Psychiatry. 2020;11(101545006):570786. 10.3389/fpsyt.2020.570786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mache S , Bernburg M , Baresi L , Groneberg D. Mental health promotion for junior physicians working in emergency medicine: evaluation of a pilot study. Eur J Emerg Med. 2018;25(3): 191–198. 10.1097/MEJ.0000000000000434 [DOI] [PubMed] [Google Scholar]
- 49.Maunder RG , Lancee WJ , Mae R , et al. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv Res. 2010;10(1):72. 10.1186/1472-6963-10-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mistretta EG , Davis MC , Temkit M , Lorenz C , Darby B , Stonnington CM. Resilience training for work-related stress among health care workers: results of a randomized clinical trial comparing in-person and smartphone-delivered interventions. J Occup Environ Med. 2018;60(6):559–568. 10.1097/JOM.0000000000001285 [DOI] [PubMed] [Google Scholar]
- 51.Moll SE , Patten S , Stuart H , MacDermid JC , Kirsh B. Beyond silence: a randomized, parallel-group trial exploring the impact of workplace mental health literacy training with healthcare employees. Can J Psychiatry. 2018;63(12):826–833. 10.1177/0706743718766051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Olson R , Wright RR , Elliot DL , et al. The COMPASS pilot study: A Total Worker HealthTM intervention for home care workers. J Occup Environ Med. 2015;57(4):406–416. 10.1097/JOM.0000000000000374 [DOI] [PubMed] [Google Scholar]
- 53.Ozgundondu B , Gok Metin Z. Effects of progressive muscle relaxation combined with music on stress, fatigue, and coping styles among intensive care nurses. Intensive Crit Care Nurs. 2019; 54:54–63. 10.1016/j.iccn.2019.07.007 [DOI] [PubMed] [Google Scholar]
- 54.Peterson U , Bergstrom G , Samuelsson M , Asberg M , Nygren A. Reflecting peer-support groups in the prevention of stress and burnout: randomized controlled trial. J Adv Nurs. 2008; 63(5):506–516. 10.1111/j.1365-2648.2008.04743.x [DOI] [PubMed] [Google Scholar]
- 55.Strauss C , Gu J , Montero-Marin J , Whittington A , Chapman C , Kuyken W. Reducing stress and promoting well-being in healthcare workers using mindfulness-based cognitive therapy for life. Int J Clin Health Psychol. 2021;21(2):100227. 10.1016/j.ijchp.2021.100227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Adair KC , Rodriguez-Homs LG , Masoud S , Mosca PJ , Sexton JB. Gratitude at work: prospective cohort study of a web-based, single-exposure well-being intervention for health care workers. J Med Internet Res. 2020;22(5): e15562. 10.2196/15562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Axisa C , Nash L , Kelly P , Willcock S. Burnout and distress in Australian physician trainees: evaluation of a wellbeing workshop. Australas Psychiatry. 2019;27(3):255–261. 10.1177/1039856219833793 [DOI] [PubMed] [Google Scholar]
- 58.Bartels-Velthuis AA , van den Brink E , Koster F , Hoenders HJR. The Interpersonal Mindfulness Program for health care professionals: a feasibility study. Mindfulness (NY). 2020;11(11): 2629‒2638. 10.1007/s12671-020-01477-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bormann JE , Becker S , Gershwin M , et al. Relationship of frequent mantram repetition to emotional and spiritual well-being in healthcare workers. J Contin Educ Nurs. 2006;37(5): 218–224. 10.3928/00220124-20060901-02 [DOI] [PubMed] [Google Scholar]
- 60.Brooks DM , Bradt J , Eyre L , Hunt A , Dileo C. Creative approaches for reducing burnout in medical personnel. Arts Psychother. 2010;37(3): 255–263. 10.1016/j.aip.2010.05.001 [DOI] [Google Scholar]
- 61.Browning ED , Cruz JS. Reflective debriefing: a social work intervention addressing moral distress among ICU nurses. J Soc Work End Life Palliat Care. 2018;14(1):44–72. 10.1080/15524256.2018.1437588 [DOI] [PubMed] [Google Scholar]
- 62.Chen SF , Fang YW , Wang MH , Wang TF. Effects of an adaptive education program on the learning, mental health and work intentions of new graduate nurses. Int J Environ Res Public Health. 2021;18(11):5891. 10.3390/ijerph18115891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chesak SS , Bhagra A , Cutshall S , et al. Authentic connections groups: a pilot test of an intervention aimed at enhancing resilience among nurse leader mothers. Worldviews Evid Based Nurs. 2020;17(1):39–48. 10.1111/wvn.12420 [DOI] [PubMed] [Google Scholar]
- 64.Dincer B , Inangil D. The effect of emotional freedom techniques on nurses’ stress, anxiety, and burnout levels during the COVID-19 pandemic: a randomized controlled trial. Explore (N Y). 2021;17(2):109–114. 10.1016/j.explore.2020.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ducar DM , Penberthy JK , Schorling JB , Leavell VA , Calland JF. Mindfulness for healthcare providers fosters professional quality of life and mindful attention among emergency medical technicians. Explore (N Y). 2020;16(1):61–68. 10.1016/j.explore.2019.07.015 [DOI] [PubMed] [Google Scholar]
- 66.Duchemin AM , Steinberg BA , Marks DR , Vanover K , Klatt M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: effects on salivary α-amylase levels. J Occup Environ Med. 2015;57(4):393–399. 10.1097/JOM.0000000000000371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dyrbye LN , West CP , Richards ML , Ross HJ , Satele D , Shanafelt TD. A randomized, controlled study of an online intervention to promote job satisfaction and well-being among physicians. Burn Res. 2016;3(3):69–75. 10.1016/j.burn.2016.06.002 [DOI] [Google Scholar]
- 68.Dyrbye LN , Shanafelt TD , Gill PR , Satele DV , West CP. Effect of a professional coaching intervention on the well-being and distress of physicians: a pilot randomized clinical trial. JAMA Intern Med. 2019;179(10):1406–1414. 10.1001/jamainternmed.2019.2425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Edmonds C , Lockwood GM , Bezjak A , Nyhof-Young J. Alleviating emotional exhaustion in oncology nurses: an evaluation of Wellspring’s “Care for the Professional Caregiver Program.” J Cancer Educ. 2012;27(1):27‒36. 10.1007/s13187-011-0278-z [DOI] [PubMed] [Google Scholar]
- 70.Ghawadra SF , Lim Abdullah K , Choo WY , Danaee M , Phang CK. The effect of mindfulness-based training on stress, anxiety, depression and job satisfaction among ward nurses: a randomized control trial. J Nurs Manag. 2020;28(5):1088–1097. 10.1111/jonm.13049 [DOI] [PubMed] [Google Scholar]
- 71.Glass N , Hanson GC , Anger WK , et al. Computer-based training (CBT) intervention reduces workplace violence and harassment for homecare workers. Am J Ind Med. 2017;60(7): 635–643. 10.1002/ajim.22728 [DOI] [PubMed] [Google Scholar]
- 72.Gunasingam N , Burns K , Edwards J , Dinh M , Walton M. Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgrad Med J. 2015;91(1074):182–187. 10.1136/postgradmedj-2014-132847 [DOI] [PubMed] [Google Scholar]
- 73.Guo YF , Lam L , Plummer V , Cross W , Zhang JPA. WeChat-based “Three Good Things” positive psychotherapy for the improvement of job performance and self-efficacy in nurses with burnout symptoms: a randomized controlled trial. J Nurs Manag. 2020;28(3):480–487. 10.1111/jonm.12927 [DOI] [PubMed] [Google Scholar]
- 74.Holt J , Del Mar C. Reducing occupational psychological distress: a randomized controlled trial of a mailed intervention. Health Educ Res. 2006;21(4):501–507. 10.1093/her/cyh076 [DOI] [PubMed] [Google Scholar]
- 75.Hsu MF , Wang C , Tzou SJ , Pan TC , Tang PL. Effects of Zentangle art workplace health promotion activities on rural healthcare workers. Public Health. 2021;196:217‒222. 10.1016/j.puhe.2021.05.033 [DOI] [PubMed] [Google Scholar]
- 76.Kersemaekers WM , Vreeling K , Verweij H , et al. Effectiveness and feasibility of a mindful leadership course for medical specialists: a pilot study. BMC Med Educ. 2020;20(1):34. 10.1186/s12909-020-1948-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ketelaar SM , Nieuwenhuijsen K , Gärtner FR , Bolier L , Smeets O , Sluiter JK. Effect of an e-mental health approach to workers’ health surveillance versus control group on work functioning of hospital employees: a cluster-RCT. PLoS One. 2013;8(9):e72546. 10.1371/journal.pone.0072546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim YI , Kim SM , Kim H , Han DH. The effect of high-frequency repetitive transcranial magnetic stimulation on occupational stress among health care workers: a pilot study. Psychiatry Investig. 2016;13(6):622–629. 10.4306/pi.2016.13.6.622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.La Torre G , Raffone A , Peruzzo M , et al. Yoga and mindfulness as a tool for influencing affectivity, anxiety, mental health, and stress among healthcare workers: results of a single-arm clinical trial. J Clin Med. 2020;9(4):1037. 10.3390/jcm9041037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lavoie-Tremblay M , Bourbonnais R , Viens C , Vezina M , Durand PJ , Rochette L. Improving the psychosocial work environment. J Adv Nurs. 2005;49(6):655–664. 10.1111/j.1365-2648.2004.03339.x [DOI] [PubMed] [Google Scholar]
- 81.Leary S , Weingart K , Topp R , Bormann J. The effect of mantram repetition on burnout and stress among VA staff. Workplace Health Saf. 2018;66(3):120–128. 10.1177/2165079917697215 [DOI] [PubMed] [Google Scholar]
- 82.Leiter MP , Laschinger HKS , Day A , Oore DG. The impact of civility interventions on employee social behavior, distress, and attitudes. J Appl Psychol. 2011;96(6):1258–1274. 10.1037/a0024442 [DOI] [PubMed] [Google Scholar]
- 83.Lin L , He G , Yan J , Gu C , Xie J. The effects of a modified mindfulness-based stress reduction program for nurses: a randomized controlled trial. Workplace Health Saf. 2019;67(3):111–122. 10.1177/2165079918801633 [DOI] [PubMed] [Google Scholar]
- 84.Linzer M , Poplau S , Grossman E , et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) study. J Gen Intern Med. 2015;30(8): 1105–1111. 10.1007/s11606-015-3235-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mache S , Baresi L , Bernburg M , Vitzthum K , Groneberg D. Being prepared to work in gynecology medicine: evaluation of an intervention to promote junior gynecologists professionalism, mental health and job satisfaction. Arch Gynecol Obstet. 2017;295(1):153–162. 10.1007/s00404-016-4223-6 [DOI] [PubMed] [Google Scholar]
- 86.Mackenzie CS , Poulin PA , Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl Nurs Res. 2006;19(2):105–109. 10.1016/j.apnr.2005.08.002 [DOI] [PubMed] [Google Scholar]
- 87.Mahdizadeh M , Jaberi AA , Bonabi TN. Massage therapy in management of occupational stress in emergency medical services staffs: a randomized controlled trial. Int J Ther Massage Bodywork. 2019;12(1):16–22. 10.3822/ijtmb.v12i1.421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Matsugaki R , Kuhara S , Saeki S , et al. Effectiveness of workplace exercise supervised by a physical therapist among nurses conducting shift work: a randomized controlled trial. J Occup Health. 2017;59(4):327–335. 10.1539/joh.16-0125-OA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McGonagle AK , Schwab L , Yahanda N , et al. Coaching for primary care physician well-being: a randomized trial and follow-up analysis. J Occup Health Psychol. 2020;25(5):297–314. 10.1037/ocp0000180 [DOI] [PubMed] [Google Scholar]
- 90.Medisauskaite A , Kamau C. Reducing burnout and anxiety among doctors: randomized controlled trial. Psychiatry Res. 2019;274:383–390. 10.1016/j.psychres.2019.02.075 [DOI] [PubMed] [Google Scholar]
- 91.Mellins CA , Mayer LES , Glasofer DR , et al. Supporting the well-being of health care providers during the COVID-19 pandemic: the CopeColumbia response. Gen Hosp Psychiatry. 2020;67:62‒69. 10.1016/j.genhosppsych.2020.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nepper MJ , McAtee JR , Chai W. Effect of a workplace weight-loss program for overweight and obese healthcare workers. Am J Health Promot. 2021;35(3):352–361. 10.1177/0890117120960393 [DOI] [PubMed] [Google Scholar]
- 93.O’Brien WH , Singh R , Horan K , Moeller MT , Wasson R , Jex SM. Group-based acceptance and commitment therapy for nurses and nurse aides working in long-term care residential settings. J Altern Complement Med. 2019;25(7): 753–761. 10.1089/acm.2019.0087 [DOI] [PubMed] [Google Scholar]
- 94.Procaccia R , Segre G , Tamanza G , Manzoni GM. Benefits of expressive writing on healthcare workers’ psychological adjustment during the COVID-19 pandemic. Front Psychol. 2021; 12(101550902):624176. 10.3389/fpsyg.2021.624176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Salyers MP , Garabrant JM , Luther L , et al. A comparative effectiveness trial to reduce burnout and improve quality of care. Adm Policy Ment Health. 2019;46(2):238–254. 10.1007/s10488-018-0908-4 [DOI] [PubMed] [Google Scholar]
- 96.Sampson M , Melnyk BM , Hoying J. The MINDBODYSTRONG intervention for new nurse residents: 6-month effects on mental health outcomes, healthy lifestyle behaviors, and job satisfaction. Worldviews Evid Based Nurs. 2020; 17(1):16–23. 10.1111/wvn.12411 [DOI] [PubMed] [Google Scholar]
- 97.Stansfeld SA , Kerry S , Chandola T , et al. Pilot study of a cluster randomised trial of a guided e-learning health promotion intervention for managers based on management standards for the improvement of employee well-being and reduction of sickness absence: GEM Study. BMJ Open. 2015;5(10):e007981. 10.1136/bmjopen-2015-007981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Uchiyama A , Odagiri Y , Ohya Y , Takamiya T , Inoue S , Shimomitsu T. Effect on mental health of a participatory intervention to improve psychosocial work environment: a cluster randomized controlled trial among nurses. J Occup Health. 2013;55(3):173–183. 10.1539/joh.12-0228-OA [DOI] [PubMed] [Google Scholar]
- 99.Watanabe N , Horikoshi M , Shinmei I , et al. Brief mindfulness-based stress management program for a better mental state in working populations—Happy Nurse Project: a randomized controlled trial. J Affect Disord. 2019;251: 186–194. 10.1016/j.jad.2019.03.067 [DOI] [PubMed] [Google Scholar]
- 100.Waters CS , Frude N , Flaxman PE , Boyd J. Acceptance and commitment therapy (ACT) for clinically distressed health care workers: waitlist-controlled evaluation of an ACT workshop in a routine practice setting. Br J Clin Psychol. 2018;57(1):82–98. 10.1111/bjc.12155 [DOI] [PubMed] [Google Scholar]
- 101.Werneburg BL , Jenkins SM , Friend JL , et al. Improving resiliency in healthcare employees. Am J Health Behav. 2018;42(1):39–50. 10.5993/AJHB.42.1.4 [DOI] [PubMed] [Google Scholar]
- 102.West CP , Dyrbye LN , Rabatin JT , et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527–533. 10.1001/jamainternmed.2013.14387 [DOI] [PubMed] [Google Scholar]
- 103.Yung PMB , Fung MY , Chan TMF , Lau BWK. Relaxation training methods for nurse managers in Hong Kong: a controlled study. Int J Ment Health Nurs. 2004;13(4):255–261. 10.1111/j.1445-8330.2004.00342.x [DOI] [PubMed] [Google Scholar]
- 104.Aiello A , Young-Eun Khayeri M , Raja S , et al. Resilience training for hospital workers in anticipation of an influenza pandemic. J Contin Educ Health Prof. 2011;31(1):15–20. 10.1002/chp.20096 [DOI] [PubMed] [Google Scholar]
- 105.Beneria A , Arnedo M , Contreras S , et al. Impact of simulation-based teamwork training on COVID-19 distress in healthcare professionals. BMC Med Educ. 2020;20(1):515. 10.1186/s12909-020-02427-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bennion MR , Baker F , Burrell J. An unguided web-based resilience training programme for NHS keyworkers during the COVID-19 pandemic: a usability study. J Technol Behav Sci. 2022;7(2):125–129. 10.1007/s41347-021-00225-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bottaccioli F , Carosella A , Cardone R , et al. Brief training of psychoneuroendocrinoimmunology-based meditation (PNEIMED) reduces stress symptom ratings and improves control on salivary cortisol secretion under basal and stimulated conditions. Explore (N Y). 2014;10(3):170–179. 10.1016/j.explore.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 108.Buselli R , Baldanzi S , Corsi M , et al. Psychological care of health workers during the COVID-19 outbreak in Italy: preliminary report of an occupational health department (AOUP) responsible for monitoring hospital staff condition. Sustainability. 2020;12(12):5039. 10.3390/su12125039 [DOI] [Google Scholar]
- 109.Cheng W , Zhang F , Liu Z , et al. A psychological health support scheme for medical teams in COVID-19 outbreak and its effectiveness. Gen Psychiatr. 2020;33(5):e100288. 10.1136/gpsych-2020-100288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cohen-Katz J , Wiley SD , Capuano T , Baker DM , Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout, part II: a quantitative and qualitative study. Holist Nurs Pract. 2005;19(1):26–35. 10.1097/00004650-200501000-00008 [DOI] [PubMed] [Google Scholar]
- 111.Cordoza M , Ulrich RS , Manulik BJ , et al. Impact of nurses taking daily work breaks in a hospital garden on burnout. Am J Crit Care. 2018;27(6): 508–512. 10.4037/ajcc2018131 [DOI] [PubMed] [Google Scholar]
- 112.Dalmasso G , Di Prinzio RR , Gilardi F , et al. Effectiveness of psychological support to healthcare workers by the occupational health service: a pilot experience. Healthcare (Basel). 2021;9(6):732. 10.3390/healthcare9060732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dukhanin V , Edrees HH , Connors CA , Kang E , Norvell M , Wu AW. Case: a second victim support program in pediatrics: successes and challenges to implementation. J Pediatr Nurs. 2018;41:54‒59. 10.1016/j.pedn.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 114.Etingen B , Martinez RN , Smith BM , et al. Developing an animal-assisted support program for healthcare employees. BMC Health Serv Res. 2020;20(1):714. 10.1186/s12913-020-05586-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gabbe SG , Webb LE , Moore DE , Mandel LS , Melville JL , Spickard WA. Can mentors prevent and reduce burnout in new chairs of departments of obstetrics and gynecology: results from a prospective, randomized pilot study. Am J Obstet Gynecol. 2008;198(6):653.e1–653.e7. 10.1016/j.ajog.2007.11.004 [DOI] [PubMed] [Google Scholar]
- 116.Gaupp R , Walter M , Bader K , Benoy C , Lang UE. A two-day acceptance and commitment therapy (ACT) workshop increases presence and work functioning in healthcare workers. Front Psychiatry. 2020;11:861. 10.3389/fpsyt.2020.00861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Geoffroy PA , Le Goanvic V , Sabbagh O , et al. Psychological support system for hospital workers during the Covid-19 outbreak: rapid design and implementation of the Covid-Psy Hotline. Front Psychiatry. 2020;11:511. 10.3389/fpsyt.2020.00511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Giordano F , Scarlata E , Baroni M , et al. Receptive music therapy to reduce stress and improve wellbeing in Italian clinical staff involved in COVID-19 pandemic: a preliminary study. Arts Psychother. 2020;70:101688. 10.1016/j.aip.2020.101688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Giordano F , Cipolla A , Ungar M. Building resilience for healthcare professionals working in an Italian red zone during the COVID-19 outbreak: a pilot study. Stress Health. 2022;38(2): 234–248. 10.1002/smi.3085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gray M , Monti K , Katz C , Klipstein K , Lim S. A “Mental health PPE” model of proactive mental health support for frontline health care workers during the COVID-19 pandemic. Psychiatry Res. 2021;299:113878. 10.1016/j.psychres.2021.113878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Haraway DL , Haraway WM. Analysis of the effect of conflict-management and resolution training on employee stress at a healthcare organization. Hosp Top. 2005;83(4):11–17. 10.3200/HTPS.83.4.11-18 [DOI] [PubMed] [Google Scholar]
- 122.Heyen JM , Weigl N , Muller M , et al. Multimodule web-based COVID-19 Anxiety and Stress Resilience Training (COAST): single-cohort feasibility study with first responders. JMIR Form Res. 2021;5(6):e28055. 10.2196/28055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Houchens N , L Sivils S , Koester E , Ratz D , Ridenour J , Saint S. Fueling leadership in yourself: a leadership development program for all types of health-care workers. Leadersh Health Serv (Bradf Engl). 2021; epub ahead of print May 10, 2021. 10.1108/LHS-06-2020-0037 [DOI] [PubMed] [Google Scholar]
- 124.Katzman JG , Tomedi LE , Everly G , et al. First responder resiliency ECHO: innovative telementoring during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(9):4900. 10.3390/ijerph18094900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lapham SC , Gregory C , McMillan G. Impact of an alcohol misuse intervention for health care workers–1: frequency of binge drinking and desire to reduce alcohol use. Alcohol Alcohol. 2003;38(2):176–182. 10.1093/alcalc/agg047 [DOI] [PubMed] [Google Scholar]
- 126.Los FS , van der Molen HF , de Boer AGEM , Hulshof CTJ , Ketelaar SM , Nieuwenhuijsen K. Workers’ health surveillance targeting mental health: evaluation of a training. Occup Med (Lond). 2022;72(4):244‒247. 10.1093/occmed/kqab165 [DOI] [PubMed] [Google Scholar]
- 127.Luk LA. Assessment of a leadership enhancement program for nursing managers of an acute general hospital in Hong Kong. Open Nurs J. 2018;12(1):133–141. 10.2174/1874434601812010133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Madede T , Sidat M , McAuliffe E , et al. The impact of a supportive supervision intervention on health workers in Niassa, Mozambique: a cluster-controlled trial. Hum Resour Health. 2017;15(1):58. 10.1186/s12960-017-0213-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.McElligott D , Holz MB , Carollo L , et al. A pilot feasibility study of the effects of touch therapy on nurses. J NY State Nurses Assoc. 2003;34(1): 16–24. [PubMed] [Google Scholar]
- 130.Melo CG , Oliver D. Can addressing death anxiety reduce health care workers’ burnout and improve patient care? J Palliat Care. 2011; 27(4):287–295. 10.1177/082585971102700405 [DOI] [PubMed] [Google Scholar]
- 131.Muir KJ , Keim-Malpass J. The emergency resiliency initiative: a pilot mindfulness intervention program. J Holist Nurs. 2020;38(2):205–220. 10.1177/0898010119874971 [DOI] [PubMed] [Google Scholar]
- 132.Muyambi K , Gillam M , Dennis S , Gray R , Martinez L , Jones M. Effect of depression awareness and management training on the attitudes of rural primary health care workers. Aust J Rural Health. 2021;29(3):449–454. 10.1111/ajr.12685 [DOI] [PubMed] [Google Scholar]
- 133.Palumbo MV , Wu G , Shaner-McRae H , Rambur B , McIntosh B. Tai chi for older nurses: a workplace wellness pilot study. Appl Nurs Res. 2012;25(1):54–59. 10.1016/j.apnr.2010.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pan C , Wang H , Chen M , et al. Mindfulness-based intervention for nurses in AIDS care in China: a pilot study. Neuropsychiatr Dis Treat. 2019;15:3131–3141. 10.2147/NDT.S223036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Reilly PM , Buchanan TM , Vafides C , Breakey S , Dykes P. Auricular acupuncture to relieve health care workers’ stress and anxiety: impact on caring. Dimens Crit Care Nurs. 2014;33(3): 151–159. 10.1097/DCC.0000000000000039 [DOI] [PubMed] [Google Scholar]
- 136.Repar PA , Reid S. Creatively caring: effects of arts-based encounters on hospice caregivers in South Africa. J Pain Symptom Manage. 2014;47(5):946–954. 10.1016/j.jpainsymman.2013.10.023 [DOI] [PubMed] [Google Scholar]
- 137.Rich A , Aly A , Cecchinato ME , et al. Evaluation of a novel intervention to reduce burnout in doctors-in-training using self-care and digital wellbeing strategies: a mixed-methods pilot. BMC Med Educ. 2020;20(1):294. 10.1186/s12909-020-02160-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rinaldi A , Tecchio R , Perugino S , De Luca A. The educational intervention “focusing” as a strategy to stress reduction among health care workers: a pilot study in an Italian teaching hospital. Ann Ig. 2019;31(3):236–243. 10.7416/ai.2019.2286 [DOI] [PubMed] [Google Scholar]
- 139.Rippstein-Leuenberger K , Mauthner O , Bryan Sexton J , Schwendimann R. A qualitative analysis of the Three Good Things intervention in healthcare workers. BMJ Open. 2017;7(5): e015826. 10.1136/bmjopen-2017-015826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rodriguez-Vega B , Palao A , Munoz-Sanjose A , et al. Implementation of a mindfulness-based crisis intervention for frontline healthcare workers during the COVID-19 outbreak in a public general hospital in Madrid, Spain. Front Psychiatry. 2020;11:562578. 10.3389/fpsyt.2020.562578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rosen B , Preisman M , Read H , et al. Resilience coaching for healthcare workers: experiences of receiving collegial support during the COVID-19 pandemic. Gen Hosp Psychiatry. 2022;75:83–87. 10.1016/j.genhosppsych.2022.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Schneider A , Wehler M , Weigl M. Effects of work conditions on provider mental well-being and quality of care: a mixed-methods intervention study in the emergency department. BMC Emerg Med. 2019;19(1):1. 10.1186/s12873-018-0218-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Schorch K , Stamm R , Priddy D , Taylor C. A wellness program to decrease pediatric postanesthesia care unit staff compassion fatigue. J Pediatr Health Care. 2021;35(5):526‒541. 10.1016/j.pedhc.2021.04.003 [DOI] [PubMed] [Google Scholar]
- 144.Selamu M , Hanlon C , Medhin G , Thornicroft G , Fekadu A. Burnout among primary healthcare workers during implementation of integrated mental healthcare in rural Ethiopia: a cohort study. Hum Resour Health. 2019;17(1):58. 10.1186/s12960-019-0383-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shapiro SL , Astin JA , Bishop SR , Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag. 2005;12(2):164–176. 10.1037/1072-5245.12.2.164 [DOI] [Google Scholar]
- 146.Sockalingam S , Clarkin C , Serhal E , Pereira C , Crawford A. Responding to health care professionals’ mental health needs during COVID-19 through the rapid implementation of Project ECHO. J Contin Educ Health Prof. 2020;40(3): 211–214. 10.1097/CEH.0000000000000311 [DOI] [PubMed] [Google Scholar]
- 147.Sorensen G , Nagler EM , Hashimoto D , et al. Implementing an integrated health protection/health promotion intervention in the hospital setting: lessons learned from the Be Well, Work Well Study. J Occup Environ Med. 2016; 58(2):185–194. 10.1097/JOM.0000000000000592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tarquinio C , Brennstuhl MJ , Rydberg JA , et al. EMDR in telemental health counseling for healthcare workers caring for COVID-19 patients: a pilot study. Issues Ment Health Nurs. 2021;42(1):3–14. 10.1080/01612840.2020.1818014 [DOI] [PubMed] [Google Scholar]
- 149.Tonarelli A , Cosentino C , Tomasoni C , et al. Expressive writing. A tool to help health workers of palliative care. Acta Biomed. 2018;89(6-S):35–42. 10.23750/abm.v89i6-S.7452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Vajpeyee M , Tiwari S , Jain K , et al. Yoga and music intervention to reduce depression, anxiety, and stress during COVID-19 outbreak on healthcare workers. Int J Soc Psychiatry. 2022; 68(4):798‒807. 10.1177/00207640211006742 [DOI] [PubMed] [Google Scholar]
- 151.Waterman S , Hunter ECM , Cole CL , et al. Training peers to treat Ebola centre workers with anxiety and depression in Sierra Leone. Int J Soc Psychiatry. 2018;64(2):156–165. 10.1177/0020764017752021 [DOI] [PubMed] [Google Scholar]
- 152.White CH , Meier N , Swint C. The implementation of a stress management program for health care workers through a rural occupational health clinic. Workplace Health Saf. 2021;69(4):161–167. 10.1177/2165079920982406 [DOI] [PubMed] [Google Scholar]
- 153.Zingela Z , van Wyk S , Bronkhorst A , Groves C. Developing a healthcare worker psychological preparedness support programme for the COVID-19 outbreak. S Afr J Psychiatr. 2022;28:1665. 10.4102/sajpsychiatry.v28i0.1665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hurrell JJ Jr, Murphy LR. Occupational stress intervention. Am J Ind Med. 1996;29(4):338–341. [DOI] [PubMed] [Google Scholar]
- 155. Becker LA. Effect size calculators . University of Colorado, Colorado Springs. June 9, 2022. . Available at: https://lbecker.uccs.edu . Accessed June 9, 2022. [Google Scholar]
- 156.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York, NY: Routledge; 1988. 10.4324/9780203771587 [DOI] [Google Scholar]
- 157.Ellis PD. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results. Cambridge, England: Cambridge University Press; 2010. 10.1017/CBO9780511761676 [DOI] [Google Scholar]
- 158.Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol Methods. 2009;14(1):43–53. 10.1037/a0014699 [DOI] [PMC free article] [PubMed] [Google Scholar]