Abstract
Background and purpose:
Isolated posterior cerebral artery occlusions (iPCAO) were underrepresented in pivotal randomized clinical trial (RCTs) of endovascular thrombectomy (EVT) in ischemic stroke, and the benefit of EVT in this population is still indeterminate. We performed a systematic review and a meta-analysis to compare the safety and efficacy of EVT compared to best medical management (BMM) in patients with iPCAO.
Methods:
We searched Medline/PubMed, Embase, Web of Science, and the Cochrane databases up to May 2023 for eligible studies reporting outcomes of patients with iPCAO treated with EVT or BMM. We pooled odds ratios (ORs) with corresponding 95% confidence intervals (CI) using a random-effects model.
Results:
Seven studies involving 2560 patients were included. EVT was associated with significantly higher likelihood of early neurological improvement (OR, 2.31 [95% CI, 1.38–2.91]; p < 0.00001) and visual field normalization (OR, 3.08 [95% CI, 1.76–5.38]; p < 0.0001) compared to BMM. Rates of good functional outcomes (mRS 0–2) were comparable between the two arms (OR, 0.88 [95% CI, 0.70–1.10]; p = 0.26). Symptomatic intracranial hemorrhage (sICH) was comparable between the two groups (OR, 1.94 [95% CI, 0.96–3.93]; p = 0.07). Mortality was also similar between the two groups (OR, 1.36; [95% CI, 0.77–2.42]; p = 0.29).
Conclusions:
In patients with iPCAO, EVT was associated with visual and early neurological improvement but with a strong trend toward increased sICH. Survival and functional outcomes may be slightly poorer. The role of EVT in iPCAO remains uncertain.
Keywords: Posterior cerebral artery, ischemic stroke, thrombectomy, meta-analysis
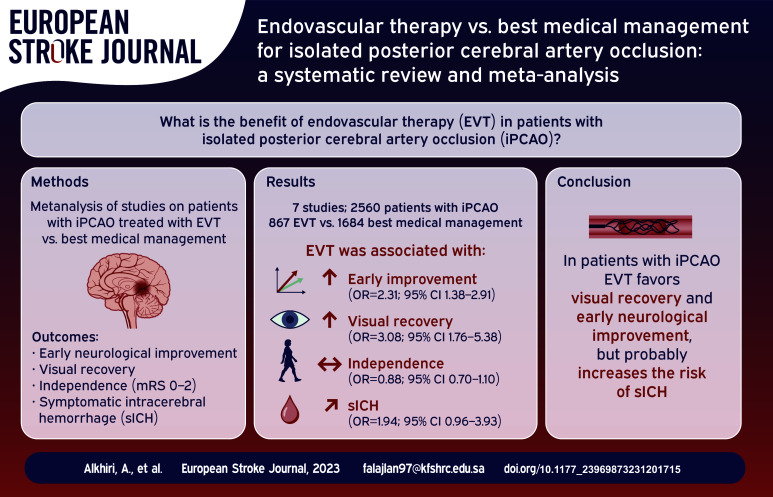
Graphical abstract.
Introduction
Isolated posterior cerebral artery occlusions (iPCAO) account for approximately 5% to 10% of all ischemic strokes. 1 Patients with PCA occlusion may experience a variety of visual manifestations, including visual field defects such as homonymous hemianopia and less commonly visual cognitive impairments such as optic ataxia and achromatopsia. 2 In addition to the visual manifestations, PCA strokes may lead to neuropsychological symptoms, sensory loss and motor impairments.2,3 Despite that most of ischemic strokes of the PCA territory carry a mild to moderate symptomatic course, 4 they can result in disabling symptoms and contribute to functional dependence. 5
The optimal approach in managing patients presenting with PCA is uncertain. 6 Recommendations from international guidelines advocate for acute revascularization therapy using intravenous thrombolysis in this population.7,8 Pivotal randomized control trials (RCTs) of endovascular thrombectomy (EVT) in acute ischemic stroke were primarily involving patients with large vessel occlusion of the anterior circulation and basilar artery, whereas patients with PCA were underrepresented. Hence, the benefit of EVT in this population is still indeterminate.2,9,10 More recently, reports of EVT utility in PCA have evolved through including larger cohorts and addressing more representative measures to determine the outcomes in this specific group.6,9
Therefore, we performed a systematic review and a meta-analysis to assess the safety and efficacy of EVT compared to best medical management (BMM) in patients with isolated PCA occlusion (iPCAO).
Methods
Search strategy and inclusion criteria
We performed this systematic review and meta-analysis in accordance with the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines, 11 and the study protocol was registered with PROSPERO (CRD42023437870). We searched Medline/PubMed, Embase, Web of Science, and the Cochrane databases up to May 2023 for English language literature reporting outcomes of patients with iPCAO stroke treated with EVT or medical therapy. The inclusion criteria was as follows; (1) RCTs or observational studies of adult patients with iPCAO; (2) reported head-to head comparisons between endovascular thrombectomy and best medical therapy; and (3) with a minimum of 15 patients. Case reports and studies of secondary occluded PCA were excluded.
A tailored search to each database was done using different combinations of possible keywords and medical subject heading term. Keywords and medical subject heading terms included stroke, thrombectomy, posterior cerebral artery and others. Complete search strategy is provided in the Supplemental Material.
Data extraction
Two authors independently extracted the data, which was subsequently evaluated by a third author. The extracted data included demographics and baseline characteristics such as: age, sex, number of patients, premorbid modified Rankin scale (mRS), initial National Institutes of Health Stroke Scale (NIHSS), and occlusion site.
Outcomes
Efficacy outcomes include early neurological improvement (ENI) defined as a decrease in NIHSS by ⩾2 points 6 or ⩾4 points,2,10,12 visual field normalization, functional independence at 90-days (mRS score 0–2), and excellent functional outcome (mRS score 0–1). Safety outcomes include symptomatic intracerebral hemorrhage (sICH), as defined by each study, and 90-day mortality rate.
Statistical analysis
All data were analyzed using RevMan (Review Manager) version 5.4 (Cochrane Collaboration). A random-effects model was used to compute odds ratios (ORs) and their corresponding 95% confidence intervals (CIs) of crude events rates reported by each study. A 95% confidence level and p < 0.05 as a borderline were set for statistical significance. Heterogeneity was assessed using the P values of the chi-square test and Higgins index (I2), 13 in which a p < 0.05 or I2 values greater than 50% were considered significant. A forest plot was produced for each outcome. Since our review included less than 10 articles, assessment of publication bias using Egger’s test or meta-regression was not applicable.14,15
Quality assessment
Two independent authors performed the quality assessment of the included studies using the Newcastle-Ottawa quality assessment scale (NOS) for cohort and case-control studies. 16 Conflicts in assessment were resolved through discussion with a third author. Scoring stars of 7–9, 5–6, and 0–4 indicate good, moderate, and poor quality respectively.
Result
Search results and study characteristics
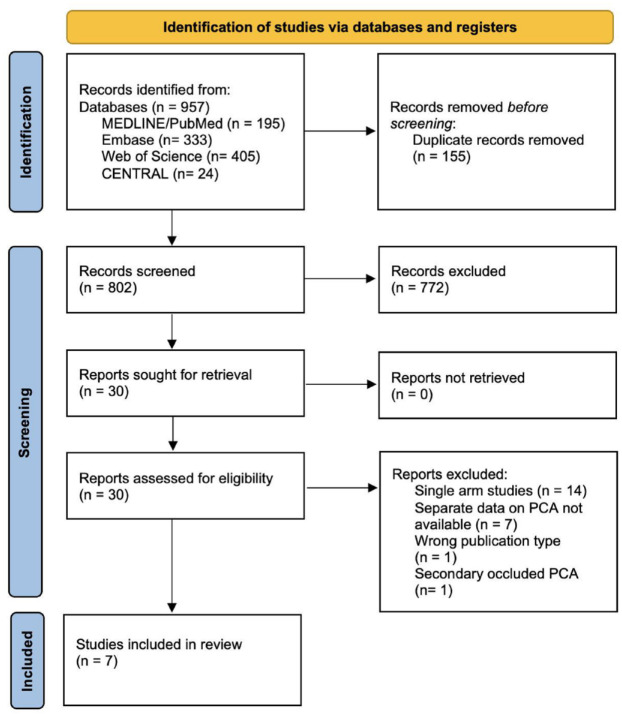
After eliminating 155 duplicate records, 802 articles were retrieved for further screening. Seven hundred seventy-two records were excluded through the title and abstract screening stage, followed by excluding another 20 articles through full-text screening (Figure 1). Thereby, seven studies2,3,6,9,10,12,17 with a total of 2560 patients were deemed to satisfy our inclusion criteria and were included in this meta-analysis.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram summarizing literature search strategy.
PCA: posterior cerebral artery.
In total, The EVT group consisted of 867 patients and the BMM group included 1684 patients. Bridging IVT was administered in 400 (46.1%) patients before EVT, whereas 1050 (62.4%) of the BMM cohort received IVT. Table 1 summarizes the baseline characteristics of the included studies. Baseline NIHSS scores ranged from 7 to 10 and the median age of included patients ranged from 62 to 83.8 years. Patients’ characteristics stratified by treatment arm are provided in Supplemental Table S1.
Table 1.
Characteristics of the included studies.
| Study ID | Study design | Occlusion site, N (%) | No. of patients (% female) |
Baseline NIHSS, Median (IQR) |
IVT, N (%) |
ENI definition | sICH definition | |||
|---|---|---|---|---|---|---|---|---|---|---|
| EVT | BMM | EVT | BMM | EVT | BMM | |||||
| Cunha et al. 2 | Single-center retrospective cohort | P1: 19 (50%), P2: 16 (42.1%), P3: 3 (7.89%) | 25 (36.0) | 13 (46.2) | 10 (6–14.5) | 8 (5.5–10.0) | 14 (56) | 13 (100) | A minimum four-point score improvement compared to admission NIHSS. | ECASS II |
| Herweh et al. 10 | Multicenter retrospective cohort | P1: 62 (47.69%), distal to P1: 68 (52.3%) | 23 (39.1) | 107 (47.7) | 9 (1–20) | 7 (1–38) | 5 (21.7) | 44 (41.1) | An improvement in NIHSS scores of at least 4 points or reaching 0 points. | Heidelberg Bleeding Classification |
| Maulucci et al. 17 | Multicenter retrospective cohort | P1: 107 (39.9%), P2: 161 (60.1%) | 119 (35.3) | 149 (45.6) | 7 (5–13) | 5 (3–8) | 69 (57.98) | 149 (100) | – | ECASS II |
| Meyer et al. 12 | Multicenter retrospective case-control | P2: 199 (81.9%), P3: 44 (18.1%), fetal variant 15 (6.2%), bilateral 8 (3.3%) | 143 (44.8) | 100 (50.0) | 7 (4–11) | 5 (2–10) | 57 (39.9) | 56 (56.0) | An improvement in NIHSS scores of at least 4 points or reaching 0 points. | ECASS II |
| Nguyen et al. 6 | Multicenter retrospective cohort | P1: 421 (41.2%), P2: 503 (49.2%), P3 (includes 3 P4): 73 (7.1%), fetal PCA: 14 (1.4%), bilateral: 12 (1.2%) | 378 (42.9) | 645 (42.2) | 8 (5–12) | 5 (2–9) | 152 (40.2) | 287 (45.5) | A ⩾ 2-point decrease in (NIHSS) at 24 h or at hospital discharge. | SITS-MOST |
| Sabben et al. 9 | Multicenter retrospective cohort | P1: 188 (25%), P2: 564 (75%) | 167 (47.3) | 585 (42.7) | 8 (5–11) | 6 (3–10) | 90 (53.9) | 467 (79.8) | – | ECASS II |
| Strambo et al. 3 | Single-center retrospective cohort | P1: 34 (32.1%; n = 3 fetal), P2: 72 (67.9%; n = 4 fetal) | 21 (61.9) | 85 (43.5) | 7 (5–8.3) | 7 (4–12.0) | 13 (61.9) | 34 (40) | – | ECASS II |
iPCAO: isolated posterior cerebral artery occlusion; EVT: endovascular thrombectomy; BMM: best medical management; IVT: intravenous thrombolysis; NIHSS: National Institutes of Health Stroke Scale; ENI: early neurological improvement; ECASS II: European Cooperative Acute Stroke Study-II; SITS-MOST: Safe Implementation of Thrombolysis in Stroke-Monitoring Study.
Quality assessment
Among included cohort studies, Cunha et al. 2 and Herweh et al. 10 scored 7 points, whereas a score of 9 was determined for the other studies.3,6,9,17 (Supplemental Table S2) Meyer et al. 12 scored 8 points using the NOS for case-control studies (Supplemental Table S3). Therefore, all studies were classified as good quality.
Outcomes of interest
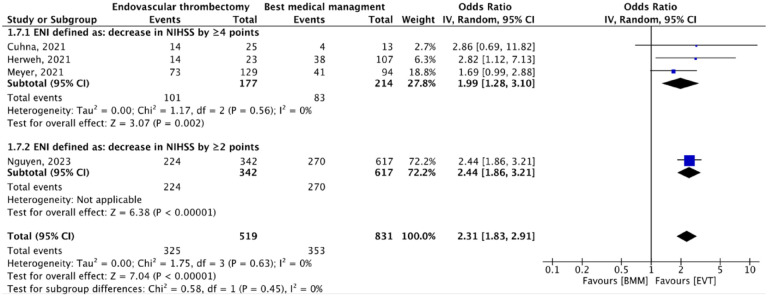
ENI
Four studies2,6,10,12 involving 1350 patients reported data on ENI. ENI was significantly higher in the EVT group compared to BMM group (OR, 2.31 [95% CI, 1.38–2.91]; p < 0.00001), with no between-study heterogeneity (I2 = 0%; p = 0.63). This remained significant across different ENI definitions, with no significant subgroup differences (p = 0.45) (Figure 2).
Figure 2.
Rates of early neurological improvements for patient groups treated with either endovascular thrombectomy or best medical management.
BMM: best medical management; EVT: endovascular thrombectomy; ENI: early neurological improvement; NIHSS: National Institutes of Health Stroke Scale; CI: confidence interval; IV: inverse variance.
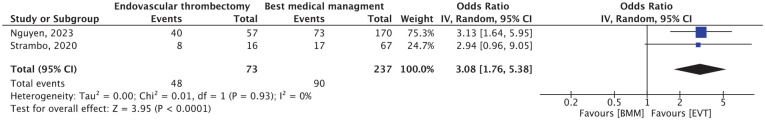
Visual field normalization
Only two studies3,6 involving 310 patients reported data on visual field normalization. Complete resolution of visual field deficits was significantly higher in in the EVT group compared to BMM group (OR, 3.08 [95% CI, 1.76–5.38]; p < 0.0001), with no between-study heterogeneity (I2 = 0%; p = 0.93) (Figure 3).
Figure 3.
Rates for visual field normalization for patient groups treated with either endovascular thrombectomy or best medical management.
BMM: best medical management; EVT: endovascular thrombectomy; CI: confidence interval; IV: inverse variance.
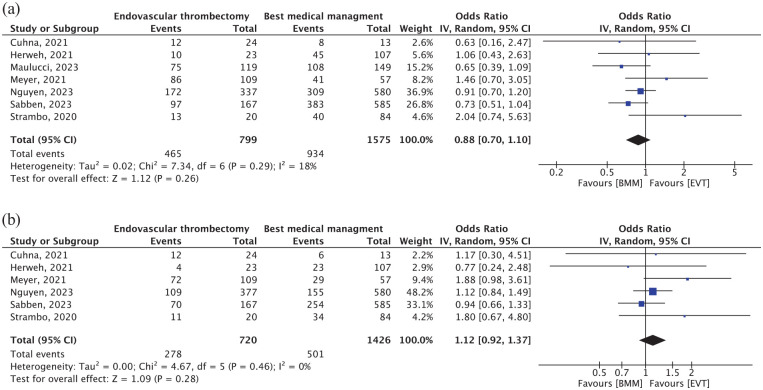
Functional outcomes
Seven studies2,3,6,9,10,12,17 involving 2374 patients reported on functional independence (mRS 0–2) at 90-days. The rate of mRS 0–2 was comparable between the two arms (OR, 0.88 [95% CI, 0.70–1.10]; p = 0.26) with no significant between-study heterogeneity (I2 = 18%; p = 0.29) (Figure 4(a)). Moreover, six studies2,3,6,9,10,12 involving 2146 patients reported rates of 90-day excellent functional outcome (mRS 0–1). The pooled rates of excellent functional outcomes were similar in both groups (OR, 1.12 [95% CI, 0.92–1.37]; p = 0.28), with no between-study heterogeneity (I2 = 0%; p = 0.46) (Figure 4(b)).
Figure 4.
Forest plots of (a) rates of favorable functional outcome (mRS score of 0–2) at 3 months and (b) rates of excellent functional outcome (mRS score of 0–1) at 3 months.
BMM: best medical management; EVT: endovascular thrombectomy; mRS: modified Rankin Scale; CI: confidence interval; IV: inverse variance.
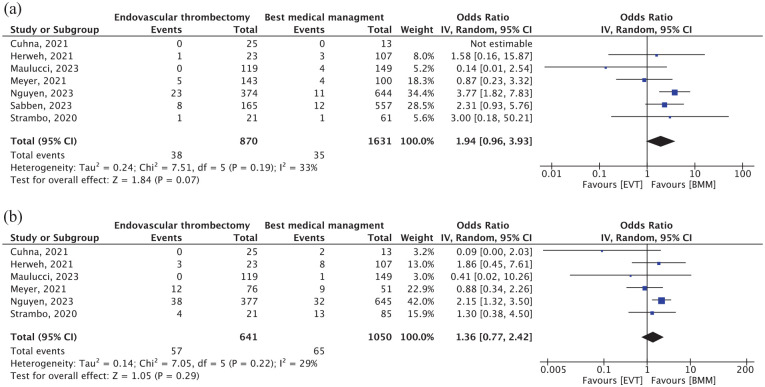
SICH and mortality
For sICH, data were available for 2501 patients from all seven studies.2,3,6,9,10,12,17 sICH was observed in 4.37% patients treated with mechanical thrombectomy as compared to 2.15% patients treated with best medical therapy (OR, 1.94 [95% CI, 0.96–3.93]; p = 0.07), with no significant between-study heterogeneity (I2 = 33%; p = 0.19). In the same context, six studies2,3,6,10,12,17 involving 1691 patients reported on 90-day mortality. Their pooled analysis showed no significant difference between the two arms (OR, 1.36; [95% CI, 0.77–2.42]; p = 0.29), with no significant between-study heterogeneity (I2 = 29%; p = 0.22) (Figure 5(b)).
Figure 5.
Forest plots of (a) symptomatic intracranial hemorrhage rates and (b) mortality rates at 3 months.
BMM: best medical management; EVT: endovascular thrombectomy; CI: confidence interval; IV: inverse variance.
EVT versus IVT
Five studies2,3,6,10,17 reported direct comparisons between EVT with or without IVT versus IVT alone. EVT was associated with significantly higher likelihood of early neurological improvement compared to IVT (OR, 1.75 [95% CI, 1.29–2.37]; p = 0.0003) (Supplemental Figure S1) without statistically significant added risk of sICH (OR, 1.93 [95% CI, 0.84–4.39]; p = 0.12) or mortality (OR, 1.14 [95% CI, 0.49–2.62]; p = 0.77) (Supplemental Figure S3).
Discussion
This systematic review and meta-analysis based on seven clinical studies, including 867 patients in the EVT group and 1684 patients in the BMM group, shows that EVT for patients with iPCAO may be safe and associated with favorable early outcomes when compared to BMM. In four studies,2,6,10,12 EVT was associated with significantly higher likelihood of ENI, and two studies3,6 found that EVT led to significantly more visual field normalization compared to BMM. However, rates of good functional outcomes (mRS 0–2) were comparable between the two groups. Rates of sICH and mortality were also similar between the two groups.
In our meta-analysis, the baseline NIHSS was ranging from 7 to 10. This highlights the fact that the NIHSS is weighted toward anterior circulation stroke and tends to underestimate stroke severity in posterior circulation stroke.18–20 As shown in the TOAST trial and other studies, the mean NIHSS scores in posterior circulation strokes were 3–5 points lower than those in anterior circulation strokes.21–23 This might explain why 15% of patients with posterior circulation stroke with NIHSS scores ⩽4 had death or disability at 3 months as a direct consequence of their stroke. 20 Accordingly, this suggests that an NIHSS score ⩽4 does not reliably predict an excellent outcome in the posterior circulation strokes. Currently in daily clinical practice, substantial restraint remains in providing EVT to patients with mild deficits, particularly patients who are eligible for IVT. 24 However, typical symptoms of infarcts in the territory of the PCA, such as hemianopia, may be associated with substantial restrictions in quality of life. 6
Our meta-analysis showed that ENI was more frequent in EVT group, but this treatment effect on ENI is more likely to be seen on patients with higher baseline NIHSS. Thus, ENI is observed in patients presented with high NIHSS scores and might not be an appropriate outcome to evaluate EVT effect in patients presented with low, but disabling NIHSS scores caused by iPCAO.
The proportion of patients experiencing visual field normalization in our study were similar to that of the PLATO Study. 6 Complete resolution of visual field deficits is likely to be one of the key surrogate outcomes for posterior cerebral artery occlusions as an improvement by as little as 2 points on the NIHSS can be a clinically meaningful event in patients who present with homonymous hemianopia.6,25
As mRS primarily focuses on physical disabilities, in PCA strokes the mRS score may underestimate the functional impact at 3 months. In addition to the visual field defects, PCA stroke usually results in symptoms related to cognitive dysfunctions such as memory loss, loss of visuospatial skills, and impaired executive functioning. Thus, mRS assessment may not adequately capture the extent of cognitive impairments in PCA stroke patients. 26
Distal and medium vessels occlusion are longer, have more tortuous access route and have thinner arterial walls; and therefore are considered to pose a potentially higher risk of dissection, perforation, and vasospasm with endovascular intervention. 27 In the current meta-analysis, sICH was observed in 4.37% of those receiving EVT and 2.15% of patients receiving BMM; however, this difference was not statistically significant. The observed rate of sICH in the EVT arm is similar to the rate seen in the HERMES and AURORA studies (4.4% and 5.3%, respectively).28,29
Our results have implications for clinical practice and future research. First, in order to provide evidence-based recommendations further high-quality evidence for the safety and efficacy of EVT for acute stroke in patients with iPCAO is recommended. Second, future studies need to assess systematically the EVT safety and best EVT technique (i.e. first-line aspiration thrombectomy vs first-line stent retriever thrombectomy) in patients with iPCAO as PCA have different anatomical variation and efficient EVT procedures in the posterior circulation might require more carefully selected sized devices to be safely guided to the distal vessel. Third, mRS is often used as an outcome measure in stroke clinical trials, but may not be the best outcome measure for evaluating the specific effects of PCA stroke. The mRS is a global measure of functional disability and may not capture the unique impairments associated with PCA strokes accurately. PCA strokes often present with visual and cognitive impairments, neglect, and higher-level visual processing deficits that may not be adequately captured by the mRS alone. This limitation could result in an underestimation of treatment effects or may not fully reflect the patient’s overall recovery. Assessments such as neuropsychological tests, visual field tests, and quality of life questionnaires may provide a more detailed understanding of the treatment’s effects on various domains affected by PCA stroke. Last, pooling of individual patient data is needed to provide a more valid estimate of EVT efficacy until we have randomized clinical trials data.
Limitations
Several limitations in this review need to be acknowledged. First, included studies are restricted to English-language articles and may have missed some studies published in other languages. Second, there was a variability between studies about the EVT technique (stent retriever, direct aspiration, or both). It is unlikely that this difference has affected our results as recent trials suggest that equal functional outcome of aspiration and stent retriever thrombectomy in all occlusion segments.30,31 However, some studies indicated that aspiration might be more effective and safer for posterior circulation stroke than stent retriever.32–34 Third, outcomes of interest were not reported in all included studies. Four studies out of seven reported data on ENI and only two studies reported data on visual field normalization, which might lead to an under/over estimation of the treatment effect. Fourth, the sICH outcome was not defined in the same manner across studies, which is a source of heterogeneity and limits the sICH analysis. Finally, the lack of individual patient data did not allow us to perform more precise estimation of effect sizes and increased sensitivity to detect smaller yet significant effects.
Conclusions
In patients with iPCAO, EVT was associated with visual and early neurological improvement but with a strong trend toward increased sICH. Survival and functional outcomes may be slightly poorer. The role of EVT in iPCAO remains uncertain.
Supplemental Material
Supplemental material, sj-pdf-1-eso-10.1177_23969873231201715 for Endovascular therapy versus best medical management for isolated posterior cerebral artery occlusion: A systematic review and meta-analysis by Ahmed Alkhiri, Aser F Alamri, Abdullah R Alharbi, Ahmed A Almaghrabi, Nayef Alansari, Abdulelah A Niaz, Basil A Alghamdi, Amrou Sarraj, Adel Alhazzani and Fahad S Al-Ajlan in European Stroke Journal
Supplemental material, sj-pdf-2-eso-10.1177_23969873231201715 for Endovascular therapy versus best medical management for isolated posterior cerebral artery occlusion: A systematic review and meta-analysis by Ahmed Alkhiri, Aser F Alamri, Abdullah R Alharbi, Ahmed A Almaghrabi, Nayef Alansari, Abdulelah A Niaz, Basil A Alghamdi, Amrou Sarraj, Adel Alhazzani and Fahad S Al-Ajlan in European Stroke Journal
Acknowledgments
None.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Not applicable.
Informed consent: Not applicable.
Guarantor: Ahmed Alkhiri (AA).
Contributorship: Conceptualization: AA, FA, and AH; Literature search: NA and AN, Data curation and methodology: AF, AR, AAA, NA, AN, and BA; Formal analysis: AA; Writing – original draft: FA, AA, AF, AR, AAA, NA, AN, and BA; Writing – review & editing: FA, AS, and AH.
ORCID iDs: Ahmed Alkhiri  https://orcid.org/0000-0002-4241-2316
https://orcid.org/0000-0002-4241-2316
Fahad S Al-Ajlan  https://orcid.org/0000-0002-0501-479X
https://orcid.org/0000-0002-0501-479X
Supplemental material: Supplemental material for this article is available online.
References
- 1. Ntaios G, Spengos K, Vemmou AM, et al. Long-term outcome in posterior cerebral artery stroke. Eur J Neurol 2011; 18: 1074–1080. [DOI] [PubMed] [Google Scholar]
- 2. Cunha B, Baptista M, Pamplona J, et al. Acute treatment of isolated posterior cerebral artery occlusion: single center experience. J Stroke Cerebrovasc Dis 2022; 31: 106239. [DOI] [PubMed] [Google Scholar]
- 3. Strambo D, Bartolini B, Beaud V, et al. Thrombectomy and thrombolysis of isolated posterior cerebral artery occlusion: cognitive, visual, and disability outcomes. Stroke 2020; 51: 254–261. [DOI] [PubMed] [Google Scholar]
- 4. Brandt T, Steinke W, Thie A, et al. Posterior cerebral artery territory infarcts: clinical features, infarct topography, causes and outcome. Multicenter results and a review of the literature. Cerebrovasc Dis 2000; 10: 170–182. [DOI] [PubMed] [Google Scholar]
- 5. Ng YS, Stein J, Salles SS, et al. Clinical characteristics and rehabilitation outcomes of patients with posterior cerebral artery stroke. Arch Phys Med Rehabil 2005; 86: 2138–2143. [DOI] [PubMed] [Google Scholar]
- 6. Nguyen TN, Qureshi MM, Strambo D, et al. Endovascular versus medical management of posterior cerebral artery occlusion stroke: the Plato study. Stroke 2023; 54: 1708–1717. [DOI] [PubMed] [Google Scholar]
- 7. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018; 49: e46–e99. [DOI] [PubMed] [Google Scholar]
- 8. Berge E, Whiteley W, Audebert H, et al. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur Stroke J 2021; 6: I–LXII. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sabben C, Charbonneau F, Delvoye F, et al. Endovascular therapy or medical management alone for isolated posterior cerebral artery occlusion: a multicenter study. Stroke 2023; 54: 928–937. [DOI] [PubMed] [Google Scholar]
- 10. Herweh C, Abdalkader M, Nguyen TN, et al. Mechanical thrombectomy in isolated occlusion of the proximal posterior cerebral artery. Front Neurol 2021; 12: 697348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 2021; 134: 178–189. [DOI] [PubMed] [Google Scholar]
- 12. Meyer L, Stracke CP, Jungi N, et al. Thrombectomy for primary distal posterior cerebral artery occlusion stroke. JAMA Neurol 2021; 78: 434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315(7109): 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peters JL, Sutton AJ, Jones DR, et al. Comparison of two methods to detect publication bias in meta-analysis. JAMA 2006; 295: 676–680. [DOI] [PubMed] [Google Scholar]
- 16. Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 2014; 14: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Maulucci F, Disanto G, Bianco G, et al. Endovascular therapy outcome in isolated posterior cerebral artery occlusion strokes: a multicenter analysis of the Swiss Stroke Registry. Eur Stroke J 2023; 8: 575–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kasner SE. Clinical interpretation and use of stroke scales. Lancet Neurol 2006; 5: 603–612. [DOI] [PubMed] [Google Scholar]
- 19. Sato S, Toyoda K, Uehara T, et al. Baseline NIH stroke scale score predicting outcome in anterior and posterior circulation strokes. Neurology 2008; 70: 2371–2377. [DOI] [PubMed] [Google Scholar]
- 20. Inoa V, Aron AW, Staff I, et al. Lower NIH stroke scale scores are required to accurately predict a good prognosis in posterior circulation stroke. Cerebrovasc Dis 2014; 37: 251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Libman RB, Kwiatkowski TG, Hansen MD, et al. Differences between anterior and posterior circulation stroke in toast. Cerebrovasc Dis 2001; 11: 311–316. [DOI] [PubMed] [Google Scholar]
- 22. Förster A, Gass A, Kern R, et al. Thrombolysis in posterior circulation stroke: stroke subtypes and patterns, complications and outcome. Cerebrovasc Dis 2011; 32: 349–353. [DOI] [PubMed] [Google Scholar]
- 23. Sarikaya H, Arnold M, Engelter ST, et al. Outcomes of intravenous thrombolysis in posterior versus anterior circulation stroke. Stroke 2011; 42: 2498–2502. [DOI] [PubMed] [Google Scholar]
- 24. Seners P, Perrin C, Lapergue B, et al. Bridging therapy or iv thrombolysis in minor stroke with large vessel occlusion. Ann Neurol 2020; 88: 160–169. [DOI] [PubMed] [Google Scholar]
- 25. Darsaut TE, Collins J, Raymond J. Patients may be right: clinical research should be designed in their best medical interest. Neurochir 2023; 69: 101391. [DOI] [PubMed] [Google Scholar]
- 26. Markus HS, van der Worp HB, Rothwell PM. Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. Lancet Neurol 2013; 12: 989–998. [DOI] [PubMed] [Google Scholar]
- 27. Saver JL, Chapot R, Agid R, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke 2020; 51: 2872–2884. [DOI] [PubMed] [Google Scholar]
- 28. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 29. Jovin TG, Nogueira RG, Lansberg MG, et al. Thrombectomy for anterior circulation stroke beyond 6 h from time last known well (Aurora): a systematic review and individual patient data meta-analysis. Lancet 2022; 399: 249–258. [DOI] [PubMed] [Google Scholar]
- 30. Lapergue B, Blanc R, Gory B, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA 2017; 318: 443–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Turk AS, Siddiqui A, Fifi JT, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet 2019; 393: 998–1008. [DOI] [PubMed] [Google Scholar]
- 32. Bernsen MLE, Bruggeman AAE, Brouwer J, et al. Aspiration versus stent retriever thrombectomy for posterior circulation stroke. Stroke 2022; 53: 749–757. [DOI] [PubMed] [Google Scholar]
- 33. Guo X, Xiong Y, Huang X, et al. Aspiration versus stent retriever for posterior circulation stroke: a meta-analysis. CNS Neurosci Ther 2023; 29: 525–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ye G, Wen X, Wang H, et al. First-line contact aspiration versus first-line stent retriever for acute posterior circulation strokes: an updated meta-analysis. J Neurointerv Surg 2022; 14: 457–463. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-eso-10.1177_23969873231201715 for Endovascular therapy versus best medical management for isolated posterior cerebral artery occlusion: A systematic review and meta-analysis by Ahmed Alkhiri, Aser F Alamri, Abdullah R Alharbi, Ahmed A Almaghrabi, Nayef Alansari, Abdulelah A Niaz, Basil A Alghamdi, Amrou Sarraj, Adel Alhazzani and Fahad S Al-Ajlan in European Stroke Journal
Supplemental material, sj-pdf-2-eso-10.1177_23969873231201715 for Endovascular therapy versus best medical management for isolated posterior cerebral artery occlusion: A systematic review and meta-analysis by Ahmed Alkhiri, Aser F Alamri, Abdullah R Alharbi, Ahmed A Almaghrabi, Nayef Alansari, Abdulelah A Niaz, Basil A Alghamdi, Amrou Sarraj, Adel Alhazzani and Fahad S Al-Ajlan in European Stroke Journal