Abstract
Physical activity and exercise (PAE) improve quality of life and reduce the effects of chronic diseases. Primary care physicians (PCPs) play an important role to encourage PAE in patients. We aim to assess PCPs' current PAE consultation practices and their enablers/barriers in daily clinical practice. We had 64 PCPs (age [35.3 ± 4.7] y, 47 women) that completed self-administered questionnaires on PAE consultation practices, training, and confidence levels. PCPs (n = 42) also completed the International Physical Activity Questionnaire-Short Form to assess their physical activity (PA) levels. We conducted correlation, one-way analysis of variance and a linear regression to assess the associations between enablers, barriers and PA levels to PAE consultation practices. On average, PCPs consulted on PAE in 49.7% of their daily clinical appointments. Majority of PCPs (70%) strongly agreed that more PAE knowledge were needed to increase consultation practices. Top three barriers related (p < 0.001) to practices were lack of PAE education (r = 0.47), patients’ preference of pharmaceutical interventions (r = 0.45) and lack of continuing education in PAE for PCPs (r = 0.37). Physically active PCPs (health-enhancing PA levels, n = 6) gave significantly more daily consultations in PAE, 73.2% ± 21.9%, compared to inactive PCPs (n = 13), 37.4% ± 22.8% (p = 0.013). In our regression output, PCPs who had higher PA levels consulted more on PAE daily (R2 = 0.38, p < 0.001) while controlling for age. Conclusion, PCPs require more knowledge on PAE and need be physically active themselves to increase PAE consultation for patients in their daily practice. Medical education should consider including more PA and exercise topics that may benefit both physicians and their patients.
Keywords: Physical activity and exercise, Primary care physicians, Consultations, Exercise prescription, Medicine
List of abbreviation
- PAE
Physical activity and exercise
- PCPs
Primary care physicians
- IPAQ-SF
International Physical Activity Questionnaire – Short Form
- PA
Physical activity
- ANOVA
Analysis of Variance
- HEPA
Health-enhancing physical activity
- EP
Exercise prescription
- METs
Metabolic equivalents
- WHO
World Health Organisation
- ACSM
American College of Sports Medicine
- EIM
Exercise is Medicine
- FITT
Frequency, intensity, time (duration) and type
- EIMM
Exercise is Medicine in Malaysia
1. Introduction
Physical activity and exercise (PAE) are essential components of healthy living and have a profound impact on physical and mental health.1,2 The evidence from the scientific and medical literature regarding insufficient physical activity (PA) or being physically inactive is considered a public health problem with a wide range of harmful effects.3,4 From managing hypertension5 to improving our immune system,6 adequate PA is key to good health and well-being. The World Health Organisation (WHO) reported that worldwide, more than a quarter of adult (28%) over aged 18 years are physically inactive.7 Physically inactive is defined as having less than 150 min of moderate-intensity or 75 min of vigorous-intensity of PA per week. It is estimated that around 5 million deaths per year could be averted if the global population were more physically active.7
Primary care physicians (PCPs) are the first-line health care professionals that people meet to diagnose and treat their illnesses and diseases. A PCP is defined as a medical doctor who provides screening, diagnosis, preventive services, patient education, and monitoring outcomes such as follow-ups for stable chronic diseases.8 On the other hand, physicians in hospital settings are prioritised to specialise in specific medical areas, have inadequate time to provide PAE counselling and may present discouraging attitudes towards providing PAE counselling.9 Nonetheless, the advice given by medical doctors is a powerful motivator for patients and PAE advice may have more weight and influence when delivered by them. As an encouragement for physicians to prescribe exercise, American College of Sports Medicine (ACSM) started the Exercise is Medicine (EIM) initiative to increase exercise in patients and subsequently improve health and wellness.10 Physical inactivity is considered as a “vital sign” to be assessed in medical primary care alongside other clinical measures such as blood pressure and weight status.11 Hence, PCPs are encouraged to routinely assess PA levels in their patients and prescribe PAE to reduce and manage chronic conditions.12 The PA counselling during patient consultation would cover the two Exercise Vital Sign (EVS) questions – (i) How many days per week do you engage in moderate to vigorous intensity exercises? and (ii) On average, how many minutes per day do you engage in exercise at this level?10 The EVS questions easily inform if the recommended minimum 150 min/week of moderate-intensity PA and/or 75 min/week of vigorous-intensity PA was achieved.13,14 This is an efficient and simple way for PCPs to monitor and consult their patients on their PA levels. Yet, we know little about PCPs' practice on giving PAE counselling for patients in a university-based, teaching-hospital. Furthermore, with the changes in health and medical care due to the Covid-19 pandemic, we are also uncertain about the challenges faced by PCPs in providing PAE consultations when factoring in new norms such as avoiding crowds, individual distancing and many more, due to the Covid-19 pandemic. Thus, we aim to assess the current PAE consultation practices of PCPs along with the challenges and enablers they experienced in a university-based, medical-teaching setting in Malaysia. We also analysed the influence of PCPs’ individual PA levels in relation to their practice of PAE consultations with patients.
2. Methods
We recruited PCPs (n = 64) from the Family Medicine Department, Hospital Universiti Sains Malaysia (Hospital USM), Kubang Kerian, Malaysia. The PCPs attend to daily clinics that consists of walk-in patients and follow-up appointments of patients with stable chronic diseases. Hospital USM is a typical public, university-level, teaching-hospital and is equipped with a rehabilitation department. However, university-qualified exercise scientists or trainers are not part of Hospital USM treatment team and there are no physical activity facilities like gymnasiums or exercise centres for primary care treatment purposes. PCPs were recruited via department emails and internal communication groups.
Ethical approval was provided by the Human Research Ethics Committee, Universiti Sains Malaysia (USM/JEPem/20040211). All participants provided written informed consent.
Building on previous studies,15, 16, 17 four construct sections on (i) demographics and current PAE consultation practices, (ii) knowledge of PAE and readiness to consult, (iii) barriers of PAE consultation and (iv) self-reported PA levels (International Physical Activity Questionnaire – Short Form, IPAQ-SF) were obtained via an online survey using QuestionPro, www.questionpro.com. The questionnaire used is attached as Supplementary 1. We sent reminder emails to PCPs to complete their survey and after two email reminders, non-completions were considered as drop-outs. Complimentary coffee vouchers were provided as a token of appreciation for five randomly selected participants.
The PAE practices and confidence levels of PCPs were assessed based on a sliding scale from a minimum of 0% (zero practice/confidence level) to maximum 100% (full practice/confidence level). Barriers on PAE consultations were reported using a 5-point Likert scale from 1 as “strongly disagree” to 5 as “strongly agree”. PCPs’ practice of giving PAE consultations is defined as the self-reported percentage of PAE consultation provided in a regular day of their total medical appointments.
For statistical computations, we used IBM SPSS Statistics 26.0 to analyse the data. Descriptive statistics for categorical and continuous variables were reported in percentages and means with standard deviations. The association of practice to confidence levels, barriers, and PA levels were analysed using Pearson's correlation. To identify the relation of different PCPs' PA level to PAE consultation practice, we used a one-way ANOVA to detect the differences of practice between inactive, minimally active and health-enhancing physically active (HEPA) PCPs from the IPAQ-SF categories. From the significantly correlated variables to PAE practice, we conducted linear regression analyses to adjust for confounders and checked assumptions in the models. Statistically significant values were set at less than 0.05.
3. Results
A total of 64 PCPs completed the online survey regarding their current PAE counselling and exercise prescription (EP) in clinical practices. PCPs characteristics are provided in Table 1. There were incomplete IPAQ-SF by 22 PCPs despite two reminders through email.
Table 1.
Background of participants, current clinical practices, perceived PAE knowledge and self-reported physical activity levels, n = 64.
| Variables | Mean ± SD/Numbers | Percentage | Range |
|---|---|---|---|
| Age (years) | 35.3 ± 4.7 | – | 30–54 |
| Gender (M/F) | 17/47 | 26.6/73.4 | – |
| Nationality (Malaysian/non-Malaysian) | 63/1 | 98.4/1.6 | – |
| Highest professional education | |||
| Bachelor medical degree | 53 | 82.8 | – |
| Master medical graduate | 10 | 15.6 | – |
| Doctoral graduate | 1 | 1.6 | – |
| Years of medical practice | 8.6 ± 4.1 | – | 4–20 |
| < 5 | 11 | 17.2 | – |
| 5–10 | 39 | 60.9 | – |
| 11–15 | 5 | 7.8 | – |
| 16–20 | 7 | 10.9 | – |
| Average patients per day | 21.7 ± 9.9 | – | 1–50 |
| Average clinical time (min/patient) | 16.6 ± 6.4 | – | 5–38 |
| Recommend clinical time (min/patient) | 14.8 ± 5.9 | – | 5–30 |
| Any formal education/training in PAE and EP (Yes/No) | 16/48 | 25/75 | – |
| Any difference between physical activity and exercise? (Yes/No/Not sure) | 59/0/4 | 92.2/0/6.3 | – |
| Know the differences between exercise counselling and exercise prescription before this study (Yes/No) | 42/22 | 65.6/34.4 | – |
| – | |||
| – | |||
| IPAQ-SF categories, n = 42 (METs/week) | |||
| Inactive (< 600) | 13 | 20.3 | – |
| Minimally active (600–2999) | 23 | 35.9 | – |
| HEPA (>3000) | 6 | 9.4 | – |
| Total METs (MET-min/week) | 1 301.2 ± 1 345.3 | – | 80–5 358 |
| Sedentary time (h/day) | 6.5 ± 3.1 | – | 1–15 |
PAE, physical activity and exercise; SD, standard deviation: EP, exercise prescription; IPAQ-SF, International Physical Activity Questionnaire-Short form; METs, metabolic equivalents; HEPA, health enhancing physical activity..
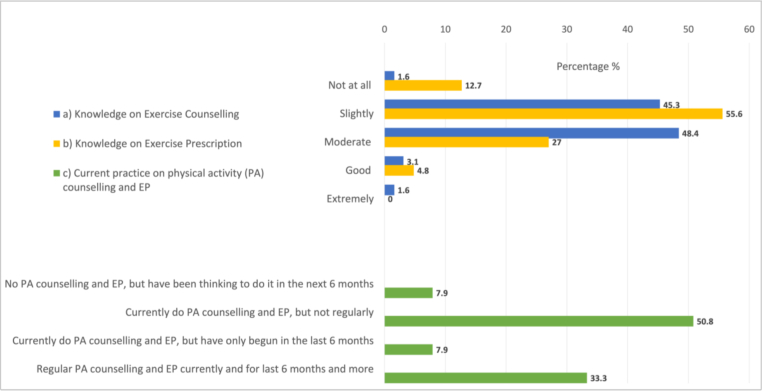
3.1. Knowledge of PAE & counselling in clinics
Majority of PCPs (n = 60, 94%) admitted their PAE knowledge was on “slight” to “moderate” scale that translated to only a-third that consistently gave regular PAE consultations for the past 6 months or more (Fig. 1). Overall readiness to provide PAE consultations showed that 92% of PCPs were already giving PAE advice with different consistencies during their clinical appointments (Fig. 1c). On average, PCPs’ PAE consultation practices were present in about half of their daily appointments (Table 2). Other component of PAE consultation like assessing PAE participation, recommending PA, prescribing exercises and so forth are also provided in Table 2.
Fig. 1.
Participant's self-reported perception on a) their knowledge on exercise counselling, b) their knowledge on exercise prescription (EP) and c) current practice on physical activity (PA) counselling and EP.
Table 2.
Participants’ practice in providing PAE consults to patients as reported based on a 100% sliding scale, n = 64.
| Variables | Mean ± SD | Range |
|---|---|---|
| Include PAE in appointments | 49.7 ± 24.9 | 4–100 |
| Assess PAE participation | 48.8 ± 24.5 | 0–100 |
| Assess physical activity readiness | 46.2 ± 25.9 | 9–100 |
| Recommend physical activity | 57.9 ± 24.3 | 8–100 |
| Prescribe exercise | 32.3 ± 26.2 | 0–91 |
| Provide a referral | 35.9 ± 26.0 | 0–89 |
PAE, physical activity and exercise; SD, standard deviation.
3.2. Confidence level & PAE consultation
Overall, PCPs' average confidence levels to (i) provide information, (ii) assess patient safety and readiness, (iii) give proper advice and instructions, and (iv) make proper referrals are provided in Table 3. PCPs' confidence level in each item were significantly correlated to their PAE consultation practice, with r-values ranging from 0.50 to 0.68 (p < 0.001). Ultimately, PCPs would be inclined to consult more on PAE if they feel that their patients are able to follow their PAE recommendations. This ties in to PCPs ability to assess their patient's readiness and being able to provide proper information and advice on PAE.
Table 3.
Participants’ confidence level on exercise counselling and exercise prescription areas as reported based on a 100% sliding scale (mean ± SD), n = 64 and their correlation values to PAE consultation practice.
| Variables | Mean ± SD | Range | r-value |
|---|---|---|---|
| Able to provide information and advice | 67.4 ± 21.8 | 10–100 | 0.61∗ |
| Able to answer patient's question | 65.1 ± 18.9 | 10–97 | 0.51∗ |
| Able to help patients maintain PAE | 54.8 ± 20.4 | 0–100 | 0.59∗ |
| Able to assess patient safety | 53.7 ± 20.6 | 10–100 | 0.60∗ |
| Able to assess patients' readiness | 57.4 ± 21.2 | 10–100 | 0.62∗ |
| Able to provide advice and instruction | 56.7 ± 21.3 | 10–100 | 0.50∗ |
| Able to make appropriate referrals | 57.0 ± 24.3 | 6–100 | 0.59∗ |
| In your patients' ability to follow PAE recommendation | 51.0 ± 21.1 | 9–88 | 0.68∗ |
SD, standard deviation; PAE, physical activity and exercise.
∗ Significant at p < 0.001 level (2-tailed).
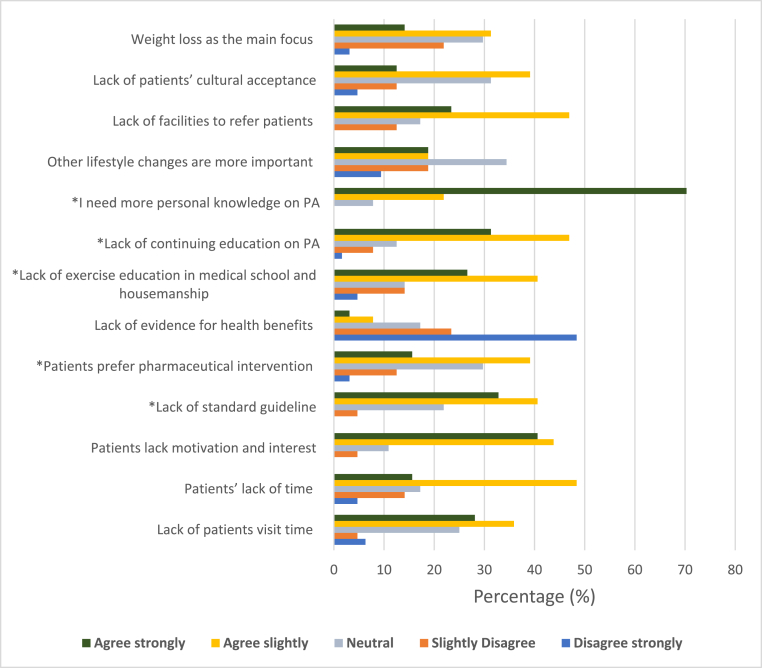
3.3. Barriers & PAE consultation
The key barriers that were significantly correlated (p < 0.001) to PAE practice as reported by PCPs and mostly were at a moderate strength of association whereby weak association is considered when r is less than 0.30. Barriers associated to PAE practice were (i) the lack of exercise education (r = 0.47), (ii) patients prefer pharmaceutical interventions (r = 0.45), (iii) lack of continuing education on PAE in medical school and housemanship (r = 0.37), iv) lack of standard guidelines to consult on PAE (r = 0.32, p < 0.05) and v) PCPs’ need more personal knowledge on PAE (r = 0.25, p < 0.05). The rest of the barrier items in Fig. 2 were not significantly linked to PAE practice. Overall, we found that physicians tend to recommend physical activities that were familiar to them and most recommended activities for their patients were brisk walk, jogging, cycling and strength training. When relating PAE to diseases, PCPs were most comfortable consulting on PAE for diabetes (non-insulin therapies, 17.3%), hypertension (16.7%) and obesity (16.1%). On the other hand, PCPs were least comfortable talking about PAE to patients when it is related to cancer (20.1%), osteoporosis (16.4%) and respiratory diseases (14.0%).
Fig. 2.
Barriers on exercise counselling and exercise prescription as reported by primary care physicians.
3.4. Relation of PCPs’ PA levels & PAE consultations
PCPs’ PA levels of inactive, minimally active and HEPA were significantly different to their practice on recommending PAE (p = 0.013) (Table 4). From the Bonferroni analysis, the HEPA group significantly provided nearly twice the amount of PAE consultations in their daily clinics compared to the inactive PCPs.
Table 4.
One-way analyses of variance (p = 0.013) in the daily practice of recommending PAE to patients in a 100% scalea and self-reported PA levels of PCPs.
| Self-report PA level | Mean ± SD (%) | 95% confidence interval |
|---|---|---|
| Inactive (n = 13) | 37.4 ± 22.8b | 23.6–51.1 |
| Minimally active (n = 23) | 50.7 ± 23.9 | 40.4–61.0 |
| HEPA active (n = 6) | 73.2 ± 21.9 | 50.2–96.2 |
PAE, physical activity and exercise; PA, physical activity, PCPs, primary care physicians; SD, standard deviation; HEPA, health-enhancing physical activity.
100 % represents every patient seen in daily clinical appointments where PCP had consulted about PAE.
Significantly different means when compared with HEPA level PCPs.
In the regression model adjusted for age, the overall model showed that total metabolic equivalents (METs) of PA conducted by PCPs significantly (p < 0.001) predicted up to 38% of PAE consultation practice (Table 5). The predicted PAE consultation practice equation is presented as, PAE practice = 0.006∗Total METs + 2.8 ∗ Age – 56.2.
Table 5.
Linear regression model (R2 = 0.38, p < 0.001) on the contribution of PA levels (total metabolic equivalents, METs, MET-min/week) on PAE consultation practices of PCPs, adjusted for age.
| Variables | β ± SE | p-value | 95% confidence interval |
|---|---|---|---|
| Total METs (MET-min/week) | 0.006 ± 0.003 | 0.032 | 0.001–0.011 |
| Age (year) | 2.8 ± 0.8 | 0.002 | 1.15–4.47 |
| Constant | −56.2 ± 28.4 | 0.055 | −133.8 – 1.31 |
PA, physical activity; METs, metabolic equivalents; PAE, physical activity and exercise; PCPs, primary care physicians; SE, standard error.
4. Discussion
PCPs practice, confidence, and barriers in PAE counselling and EP within a teaching-hospital setting are encouraging with most PCPs (92%) have included PAE counselling at various consistencies for their patients. On average, PCPs conducted PAE counselling up to 49.7% for their patients on a daily basis. Overall, confidence levels of PCPs to provide PAE counselling and EP were considered at moderate levels with ranges between 50% and 67% while key barriers reported by PCPS were the (i) lack of exercise education, (ii) patient's preference for pharmaceutical interventions, and (iii) lack of continuing education during medical school and housemanship. The most prominent component that would encourage more PAE consultations with patients would be the PCPs personal PA level, whereby highly active PCPs would advised more on PAE for their patients compared to inactive PCPs. These findings largely reaffirms that the PCPs that are physically active and have adequate training in PAE would be those that would provide PAE consultations to their patients.
4.1. Practice of PAE counselling in clinics
PCPs are in the ideal position to provide PAE counselling to patients as part of their medical role to prevent and manage chronic diseases. In our study, PCPs agreed with the importance of PAE toward patients’ health. Although our PCPs have a high level of readiness to give PAE counselling and EP to patients, only a third reported giving regular PAE counselling in the past six months and more. This however seems to be better than other settings where most of their physicians failed to include practice PAE counselling and prescribe exercise in their regular clinic routine.18 Yet, regular PAE consultations by physicians are critical to further strengthen behaviour changes in PA and sedentarism for health.19 With regular PAE counselling by physicians over a three year behavioural therapy intervention, patients with type 2 diabetes successfully sustained increases in PA and decreased sedentary time.20 Generally, PCPs that have longer consultations time with patients would equate to better opportunities to incorporate PAE counselling as compared to other physicians.9
In our study, PCPs on average takes about 16.6 min per patient consultation in their daily clinical work. The time was slightly lower than an average of 18.2 min per patient consultation,21 and was within the range of 10–20 min recommendation based on the personal communication with the Head of Family Medicine Department, Hospital USM. From the total clinical consultation time, PCPs need only 2–4 min to ask the two EVS questions at each visit and this was effective to promote PA in patients.18 Regular EVS questioning showed that it helps physician to monitor their PAE counselling and also reduce patients’ risk of diseases.18 This would also be a great way to start conversations about the duration, intensity and type of exercise required for health and fitness.
The National Strategic Plan for Active Living was published to encourage Malaysians to stay active. According to the Ministry of Health (2018), one strategy planned was integrating PAE and non-communicable diseases prevention into primary healthcare system. However, we find that most PCPs only provide PAE counselling to about 49.7% of their patients that they see in daily practice. This is discouraging as physician's advice on exercise is important for patients to adopt regular exercise. Hence, a medical doctor is the most influential source of information to promote PA adoption for patients. This is evident as physician counselling on PAE is one of the strategies to promote health and make positive behaviour changes in patients in the overall larger population.10 When patients seek professional guidance to treat their illness, it is highly indicative that they desire to change their behaviour.22 In addition, having professional advice and reminders to be more physically active may make a significant difference.12
4.2. Physician's knowledge, confidence and practice towards PAE counselling in practice
While we know that PCPs are strong influencers to PA adoption in patients, we know little on the factors that encourage Malaysian PCPs to provide PAE consultations. Although almost all PCPs may mention PAE to their patients, the majority of PCPs still do not provide specific guidance and written prescription to their patients. The lack of PAE knowledge was a significantly key barrier to PAE counselling. The FITT (frequency, intensity, time [duration] and type) framework on EP can be integrated into PCP professional practice alongside scientific and medical concepts.23 It is an important component to encourage PA assessment and promotion by increasing physicians’ knowledge and experience with PAE and counselling behaviour.24
PCPs who had previous educational training in PAE are more able and confident to provide EP to patients. From EIM in Malaysia (EIMM), there is a simple and effective action guide for PCP to improve the practice in prescribing PAE to their patients with the appropriate ‘dosage’ of FITT within the limited consultation time.25 When applied effectively, EIMM mechanism may help to lower cost in health care and also provide resources to PCPs and exercise professionals to develop a healthier community.26 Our study found that only 25% of physicians reported that they had some sort of formal training in PAE and EP. Subsequently, they had greater confidence and were able to include PAE, provide information and advise patients in their clinical practice. Fowles and colleagues found that trained physicians with PAE education included more exercise counselling (51%) than untrained physicians (39%).17 Continuous education session on PAE may help physicians change behaviour to provide exercise counselling in their clinical practice.
4.3. Barriers towards clinical practice of PAE counselling and prescription
Generally, physicians encounter numerous barriers when attempting to provide PA to patients.14 Alahmed and Lobelo presented that inadequate consultation time, lack of exercise professional's referral service and poor PAE knowledge are key reasons to why physicians do not counsel patients about PAE in their busy clinical setting.27 Similarly, we found that lack of exercise education was reported as the biggest barrier where nearly three-quaters of PCPs strongly agreed that this prevent them from practicing exercise counselling and prescription for their patients.
There is currently a wide range of evidence to suggest that the physician's encouragement on PA, combined with multi-professional approaches, may be an effective way of achieve long-term adherence of a physically activity lifestyle.14 Physicians may not be familiar and are limited in exercise and sports knowledge especially when it is reported that less than 4 h (29%) and no lessons (57.8%) on PAE in health promotion topics were taught in medical schools.28 Yet, Pugh and his colleagues found that medical students reported they were aware of the benefits of PA in disease management but lack the confidence to give EP to patients due to their lack of knowledge in current PA guideline.29 Thus, 93% of them do not have the confidence to prescribe exercise to patient who needed it the most.29
Our result found that, 75% of PCPs admitted to not having any formal training or education regarding PAE. Majority of medical education institutes did not provide any PA education-related courses in medical education. In our study, 34.4% of participants reported that they do not know the difference between exercise counselling and EP before this study. Most of the PCPs acquired their PAE knowledge from self-reading (42.7%). Hence, multi-institutional medical education research and education centres may consider including a larger component of PAE topics to ensure physician's clinical competence and enhance patient care when counselling about PAE.
4.4. PCP's self-report PA level
The average PA level among PCPs in our study were 1301 METs-min/week and was much higher than the 464 METs-min/week as reported in a study among family physicians in South India.30 Our PCPs also more frequently inquired and advised patients on PA compared to the doctors in the South India, 49.7% versus 25%, respectively.30 It seems that physically active physicians may be an ideal role model and would impart the importance of PA to their patients as well.
PCPs who are inactive are less likely to provide PA counselling than their active counterparts. We saw the pattern of increased PA consultations that corresponded to the categories of inactive, minimally active and HEPA PCPs. Lobelo and de Quevedo found that same positive association between PCPs PA habits and providing PAE counselling to patients in their review.31 Out of the 24 studies analysed in their review, 19 studies showed a significant positive correlation of physician's PA levels to the practice of counselling for PA in patients.31 In five out of six studies listed with self-reported PA levels, physically active physicians had significantly 1.4 to 5.7 odds-ratio of counselling their patients on PA.31 Taken together, these results suggest that physically active PCPs are more likely to advise their patients to be as active as them. Thus, getting PCPs to be physically active may be a critical component in increasing PAE patient consultations other than PAE education for PCPs. Theoretically, when PCPs understand the components of PAE and are conducting PAE regularly themselves, they would then be able to connect and advise their patients better through their own personal experience to be more physically active.
4.5. Changes of practices in PAE counselling due to Covid-19 pandemic situations
In the face of this novel coronavirus pandemic, the WHO, department for Disease Control and Prevention, and public health advisory organizations are encouraging individuals to begin or continue to engage in PA regularly to maintain physical and mental health and wellbeing when not contraindicated and abiding to public health and community safety guidelines.1 It is important to know that regular exercises will simultaneously strengthen both our mental health and immune system. PA is one of the major steps in managing the Covid-19 threat in a healthy way.32
In UK, clinicians continued prescribing exercise base on FITT principle to help patients maintain PA levels during the COVID-19 outbreak showed significant physical health benefits.33 PCPs in this study captured the current PAE consultation practices after the Covid-19 pandemic. PCPs mentioned of continued PAE counselling albeit with slight adaptations due to this Covid-19 situation. Most PCPs advised patients to modify indoor exercises by using equipment that can be easily obtained and used at home. Additional, PCPs touched on types and exercise duration along with advice to avoid crowded areas and staying at home if any Covid-19 symptoms appear. PCPs shared that they need to put in more effort to increase patient's motivation to conduct PAE as patients become less motivated to workout at home which leads them to be more sedentary and reduces PA levels. Yet, it was still critical that PCPs advise patients on PA as there is a priming effect34 when provided by physicians.
4.6. Strength and limitation of this study
Our study has several strengths. First, we had a good response from the pool of 108 active PCPs in the teaching hospital setting in Hospital USM where 64 PCPs participated our study. Second, we managed to replicate two key studies in this area and able to attain initial insights of PAE practices and barriers in Malaysian PCPs within a teaching-hospital setting. Despite the strengths, we acknowledge several weaknesses such as this is a cross-sectional study and are limited in providing inferential insights to the factors related to PAE consultations in PCPs. Also, another limitation would be that PCPs provided self-reported level of PAE practice that may be subjected to reporting or information biases. Future studies may involve patient's input on the extent of PAE consultations received in clinical consultations from PCPs. However, by keeping participants anonymous in their responses, we hope to have limit biases related to self-reporting. Lastly, the study is conducted in one of the several teaching-hospitals in the country and is not representative of the other PCP practices in Malaysia.
5. Conclusion
In summary, PCPs that are physically active were more likely to have a higher PAE consultation rate with their patients. PCPs reported a strong barrier of insufficient technical knowledge on PAE to provide adequate consultations. Further research is required to examine the effectiveness of PAE education for PCPs on physician recommendations and PA counselling and EP towards patients and their clinical outcomes. It would be helpful to expand the scope of the study to other teaching-hospitals and even public hospitals in the country. Coordination between PCPs, exercise physiologists, university-qualified exercise science graduates and government agencies are required to assist and lead in developing the best practices around physical PA activity assessment and promotion that will benefit patients and their health.
Submission statement
This manuscript is based on AKL bachelor's degree thesis, supervised by VPST. While this manuscript is being reviewed for this journal, the manuscript is not be submitted elsewhere for review and publication. All authors have read and agreed with manuscript content.
Ethics approval statement
Ethical approval provided by the Human Research Ethics Committee, Universiti Sains Malaysia (USM/JEPem/20040211). All participants provided written informed consent.
Availability of data and material
Data and material are not openly available. If required, it can be obtained by contacting the Corresponding Author.
Authors' contributions
Ann Kee Lee: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. Rosediani Bt Muhamad: Conceptualization, Methodology, Writing – review & editing. Vina Phei Sean Tan: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Visualization, Writing – review & editing.
Conflict of interest
None of authors have any conflicts and interest regarding this manuscript submission.
Acknowledgement
We acknowledge the contribution from participants to be part of this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.smhs.2023.11.002.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Laddu D.R., Lavie C.J., Phillips S.A., Arena R. Physical activity for immunity protection: inoculating populations with healthy living medicine in preparation for the next pandemic. Prog Cardiovasc Dis. 2021;64:102–104. doi: 10.1016/j.pcad.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.da Silveira M.P., da Silva Fagundes K.K., Bizuti M.R., Starck É., Rossi R.C., de Resende e Silva D.T. Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature. Clin Exp Med. 2021;21(1):15–28. doi: 10.1007/s10238-020-00650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saad H.A., Low P.K., Jamaluddin R., Chee H.P. Level of physical activity and its associated factors among primary healthcare Workers in Perak, Malaysia. Int J Environ Res Publ Health. 2020;17(16):5947. doi: 10.3390/IJERPH17165947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson W.R., Sallis R., Joy E., Jaworski C.A., Stuhr R.M., Trilk J.L. Exercise is medicine. Am J Lifestyle Med. 2020;14(5):511–523. doi: 10.1177/1559827620912192/ASSET/IMAGES/10.1177_1559827620912192-IMG2.PNG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alpsoy Ş. Exercise and hypertension. Adv Exp Med Biol. 2020;1228:153–167. doi: 10.1007/978-981-15-1792-1_10/COVER. [DOI] [PubMed] [Google Scholar]
- 6.Sharif K., Watad A., Bragazzi N.L., Lichtbroun M., Amital H., Shoenfeld Y. Physical activity and autoimmune diseases: get moving and manage the disease. Autoimmun Rev. 2018;17(1):53–72. doi: 10.1016/J.AUTREV.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Guidelines on physical activity and sedentary behaviour. World Health Organization. 2022. https://apps.who.int/iris/handle/10665/336656 [PubMed]
- 8.Katon W., von Korff M., Lin E., Simon G. Rethinking practitioner roles in chronic illness: the specialist, primary care physician, and the practice nurse. Gen Hosp Psychiatr. 2001;23(3):138–144. doi: 10.1016/S0163-8343(01)00136-0. [DOI] [PubMed] [Google Scholar]
- 9.Osinaike J., Hartley S.E. Physical activity counselling among junior doctors in the UK: a qualitative study. Health Educ J. 2021;80(5):584–595. doi: 10.1177/0017896921999074. [DOI] [Google Scholar]
- 10.Sallis R. Exercise is medicine: a call to action for physicians to assess and prescribe exercise. Phys Sportsmed. 2015;43(1):22–26. doi: 10.1080/00913847.2015.1001938. [DOI] [PubMed] [Google Scholar]
- 11.AlHajri S.A., Alyafei A. Physical activity vital sign, the need for incorporation into the clinical practice: narrative review. J Comm Med Public Health. 2022;6(2):238. doi: 10.29011/2577-2228.100238. [DOI] [Google Scholar]
- 12.Beni Yonis O., Saadeh R., Chamseddin Z., Alananzeh H. Exercise counselling by primary care physicians in Jordan—a preliminary study. J Prim Care Community Health. 2020;11 doi: 10.1177/21501327209469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Golightly Y.M., Allen K.D., Ambrose K.R., et al. Physical activity as a vital sign: a systematic review. Pre Chronic Dis. 2019;14 doi: 10.5888/PCD14.170030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shuval K., Leonard T., Drope Jeffrey, et al. Physical activity counseling in primary care: insights from public health and behavioral economics. CA Cancer J Clin. 2017;67(3):233–244. doi: 10.3322/CAAC.21394. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien M.W., Shields C.A., Oh P.I., Fowles J.R. Health care provider confidence and exercise prescription practices of exercise is medicine Canada workshop attendees. Appl Physiol Nutr Metabol. 2017;42(4):384–390. doi: 10.1139/apnm-2016-0413. [DOI] [PubMed] [Google Scholar]
- 16.Smock C., Alemagno S. Understanding health care provider barriers to hospital affiliated medical fitness center facility referral: a questionnaire survey and semi structured interviews. BMC Health Serv Res. 2017;17(1):1–6. doi: 10.1186/S12913-017-2474-Y/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fowles J.R., O'Brien M.W., Solmundson K., Oh P.I., Shields C.A. Exercise is Medicine Canada physical activity counselling and exercise prescription training improves counselling, prescription, and referral practices among physicians across Canada. Appl Physiol Nutr Metabol. 2018;43(5):535–539. doi: 10.1139/APNM-2017-0763. [DOI] [PubMed] [Google Scholar]
- 18.Thornton J.S., Frémont P., Khan K., et al. Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the Canadian Academy of Sport and Exercise Medicine. Br J Sports Med. 2016;50(18):1109–1114. doi: 10.1136/BJSPORTS-2016-096291. [DOI] [PubMed] [Google Scholar]
- 19.Lavie C.J., Ozemek C., Carbone S., Katzmarzyk P.T., Blair S.N. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019;124(5):799–815. doi: 10.1161/CIRCRESAHA.118.312669. [DOI] [PubMed] [Google Scholar]
- 20.Balducci S., D'Errico V., Haxhi J., et al. Effect of a behavioral intervention strategy on sustained change in physical activity and sedentary behavior in patients with type 2 diabetes: the IDES_2 randomized clinical trial. JAMA. 2019;321(9):880–890. doi: 10.1001/jama.2019.0922. [DOI] [PubMed] [Google Scholar]
- 21.Ahmad B.A., Khairatul K., Farnaza A. An assessment of patient waiting and consultation time in a primary healthcare clinic. Malays Fam Physician. 2017;12(1):14–21. [PMC free article] [PubMed] [Google Scholar]
- 22.Falskog F., Landsem A.M., Meland E., Bjorvatn B., Hjelle O.P., Mildestvedt T. Patients want their doctors' help to increase physical activity: a cross sectional study in general practice. Scand J Prim Health Care. 2021;39(2):131–138. doi: 10.1080/02813432.2021.1910670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wattanapisit A., Poomiphak Na, Nongkhai M., et al. What elements of sport and exercise science should primary care physicians learn? An interdisciplinary discussion. Front Med. 2021;8:1262. doi: 10.3389/fmed.2021.704403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pojednic R.M., Polak R., Arnstein F., Kennedy M.A., Bantham A., Phillips E.M. Practice patterns, counseling and promotion of physical activity by sports medicine physicians. J Sci Med Sport. 2017;20:123–127. doi: 10.1016/j.jsams.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 25.What we do - Exercise is Medicine Malaysia. 2022. https://www.eimm.org.my/what-we-do/
- 26.About - Exercise is Medicine Malaysia. 2022. https://www.eimm.org.my/about/
- 27.Alahmed Z., Lobelo F. Correlates of physical activity counselling provided by physicians: a cross-sectional study in Eastern Province, Saudi Arabia. PLoS One. 2019;14(7) doi: 10.1371/JOURNAL.PONE.0220396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Brien S., Prihodova L., Heffron M., Wright P. Physical activity counselling in Ireland: a survey of doctors' knowledge, attitudes and self-reported practice. BMJ Open Sport Exerc Med. 2019;5(1) doi: 10.1136/BMJSEM-2019-000572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pugh G., O'Halloran P., Blakey L., Leaver H., Angioi M. Integrating physical activity promotion into UK medical school curricula: testing the feasibility of an educational tool developed by the Faculty of Sports and Exercise Medicine. BMJ Open Sport Exerc Med. 2020;6(1) doi: 10.1136/BMJSEM-2019-000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patra L., Mini G.K., Mathews E., Thankappan K.R. Doctors' self-reported physical activity, their counselling practices and their correlates in urban Trivandrum, South India: should a full-service doctor be a physically active doctor? Br J Sports Med. 2015;49(6):413–416. doi: 10.1136/BJSPORTS-2012-091995. [DOI] [PubMed] [Google Scholar]
- 31.Lobelo F., de Quevedo I.G. The evidence in support of physicians and health care providers as physical activity role models. Am J Lifestyle Med. 2014;10(1):36–52. doi: 10.1177/155982761352012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aktug Z.B., Demir N.A. An exercise prescription for COVID-19 pandemic. Pakistan J Med Sci. 2020;36(7):1732–1736. doi: 10.12669/PJMS.36.7.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahmed I. COVID-19 – does exercise prescription and maximal oxygen uptake (VO2 max) have a role in risk-stratifying patients? Clin Med. 2020;20(3):282–284. doi: 10.7861/CLINMED.2020-0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kreuter M.W., Chheda S.G., Bull F.C. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9(5):426–433. doi: 10.1001/ARCHFAMI.9.5.426. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and material are not openly available. If required, it can be obtained by contacting the Corresponding Author.