Abstract
Maternal diet influences breast milk nutritional profile; however, it is unclear which nutrients and contaminants are particularly responsive to short- and long-term changes in maternal intake, and the impact of specific exclusion diets, such as vegan or vegetarian. This study systematically reviewed the literature on the effects of maternal nutrient intake, including exclusion diets, on both the nutrient and contaminant content of breast milk. The electronic databases, PubMed, CENTRAL, Web of Science and CINALH were systematically searched until 4 June 2023, with additionally searches of reference lists (PROSPERO, CRD42020221577). The quality of the studies was examined using Cochrane Risk of Bias tool and Newcastle–Ottawa scale. Eighty-eight studies (n 6577) met the search criteria. Due to high heterogeneity, meta-analysis was not possible. There was strong evidence of response to maternal intakes for DHA and EPA, vitamins A, E and K, iodine and Se in breast milk composition, some evidence of response for α-linolenic acid, B vitamins, vitamin C and D, ovalbumin, tyrosine and contaminants, and insufficient evidence to identify the effects arachidonic acid, Cu, Fe, Zn and choline. The paucity of evidence and high heterogeneity among studies reflects the need for more high-quality trials. However, this review identified the importance of maternal intake in the nutritional content of breast milk for a wide range of nutrients and supports the recommendation for supplementation of DHA and vitamin B12 for those on restrictive diets.
Keywords: Lactating mothers, Human milk, Milk banks, n-3 PUFA, Nutrients, Vegan, Vegetarian
Appropriate nutrition is fundamental for newborns, especially preterm infants, where their materno-fetal nutrients supply have been prematurely terminated(1). Breast milk provides nutrients, hormones, enzymes and immunological factors that are essential for infant development. Maternal breast milk is the first choice for feeding neonates; however, if mothers are unable to provide sufficient, donor human milk is the recommended alternative(2). The nutritional composition of human milk varies widely, not only over lactation, but also between individuals and populations(3–5). Factors that have been shown to affect the nutritional composition include maternal lifestyle and dietary habits(6). It is therefore essential to identify which nutrients in breast milk are responsive to maternal diet in order to inform and update nutritional guidance for lactating mothers, milk donors and milk banks.
The impact of maternal diet on breast milk composition has been widely investigated; however, the results have been equivocal, with some studies showing positive effects whereas others have not. Systematic reviews in 2016(6) and 2017(7) report a positive association between oily fish consumption and higher levels of the n-3 PUFA, DHA (22:6n-3) and EPA (20:5n-3), and other fatty acids, such as the n-6 PUFA, linoleic acid (LA, 18:3n-6), and oleic acid (18:1n-9) in breast milk(6). There was also evidence demonstrating a positive association between dietary vitamin C, B1 and vitamin A, D, E and K, with breast milk levels. The effects of dietary vitamin and/or mineral supplementation were reported in two systematic reviews(8,9), where the results were mixed, although there was some indication that vitamin supplementation had a greater effect on breast milk levels than mineral supplementation, with the strongest evidence seen for vitamin A, D, B1, B2, B12 and C.
Restricted diets, such vegan or vegetarian, can provide lower levels of nutrients, such as DHA, which may consequently affect the nutritional content of breast milk. In a 2020 systematic review by Karzc and Krόlak-Olejnik, the effects of vegan or vegetarian diets on breast milk composition were explored(8). Thirteen studies were summarised, and the authors identified that although milk from mothers following vegan, vegetarian and non-vegetarian diets was generally comparable in nutritional content, there were lower levels of some nutrients, particularly of DHA and vitamin B12, in the milk from vegan mothers and, therefore, recommended supplementation with these nutrients to enhance the nutritional content of the milk.
DHA, the long-chain n-6 PUFA and arachidonic acid (ARA, 20:4n-6) are essential for the development of optimal brain, visual and immune system functions(10). In addition to those following vegan diets, lactating women may limit their consumption of fish, where DHA and EPA are highly enriched, due to concerns over the presence of heavy metal contaminants, such as methylmercury(11) and their effects on breast milk composition. This review also investigated the effects of dietary exposure to contaminants including heavy metals (As, B, Pb and Hg) and polychlorinated biphenyls (PCB) on breast milk levels.
The aim of this review is to extend the scope of previous systematic reviews and provide an up-to-date summary of the effects of short-term and long-term changes in maternal nutrient intake, including restrictive diets, and on breast milk nutritional composition. It is hoped that the results may be used to guide future research and inform nutritional guidance for lactating mothers, milk donors and milk banks.
Methodology
This review was designed and undertaken following the protocols for Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA)(12). Study selection, assessment of eligibility, extraction of data and statistical analysis were performed according to a predefined protocol registered with the PROSPERO International prospective register of systematic reviews (ID: CRD42020221577).
Search strategy
The search was performed on four different databases: PubMed, CENTRAL, Web of Science and CINALH following the PRISMA(12) statement for systematic reviews. Additionally, three systematic reviews(6,8,9) were screened and articles meeting the selection criteria were also included. The review was designed upon the participants/population, intervention, comparison and outcome (PICO) model, with population being ‘lactating mothers’ or ‘human milk donors’; intervention, ‘experimental’ or ‘observation’ studies; comparison, ‘maternal dietary intake’ and outcome, ‘micronutrients’, ‘macronutrients’ and ‘contaminants’ breast milk content. The search was conducted on human studies and exclusively on lactating women. Publication types included were randomised controlled trials (RCT), experimental studies and observational studies. Limitations were applied to exclude conference papers, editorials, letters, commentary, and short survey, and grey literature was not searched. The search was run in English language up to 4 June 2023, with no time limitation. Online Supplementary Table S1 shows the search strategy.
Selection criteria
The selection criteria were based on the participants/population, intervention, comparison and outcome framework(13). The participants/population were healthy, non-micronutrient-deficient, lactating women, as defined by investigators. The participants/population were breast-feeding or expressing breast milk within the first 12 months postpartum, and the exclusion criteria were participants/populations with predisposition to malnutrition, micronutrient deficiency as defined by investigators, any severe medical conditions or disorders including, HIV 1 or 2, hepatitis B or C, human T-lymphotropic virus type I or II, or syphilis, recreational drug users, smokers, or users of nicotine replacement therapy. The intervention was dietary supplementation for RCT and experimental studies, and assessment of dietary intake for observational studies. The comparison was to the control group or differences in relative levels of intake. The outcome was the differences in breast milk nutrient/contaminant level by maternal intake.
Data extraction
Two reviewers independently screened all titles and abstracts (CF and MS), according to the inclusion and exclusion criteria. Disagreements were resolved by discussion and where necessary involving a third reviewer (SCD). If the title or abstract appeared to meet the eligibility criteria or they could not determine its eligibility, the full texts of the articles were obtained. Full-text screenings and quality assessments for each of the included papers were also conducted by the two reviewers independently (CF and MS), and any discrepancies were discussed with a third author (SCD) until a decision on whether or not to include the paper in the review was reached. Rayyan software was used for handling and managing extracted studies that were found in the databases, and duplicates were removed(14).
Quality assessment and risk of bias
The quality assessment of the studies was performed by using the Cochrane Risk of Bias tool (ROB2_IRPG_beta_v7)(15,16) for RCT and the Newcastle–Ottawa scale for the non-randomised cohort and case–control studies(17). The ROB2_IRPG_beta_v7 assessment tool contains five domains: randomisation process, deviations from intended interventions, missing outcome data, measurement of the outcome and selection of the reported result. An algorithm calculates the risk of bias for each domain as well as the overall risk, classifying it within three categories, high risk, low risk or some concerns. The Newcastle–Ottawa scale is comprised of eight items covering three domains: selection (including representativeness and source of sample), comparability (including study design and considerations in analysis) and exposure (for cohort studies, the exposure domain is instead the ‘outcome’ domain). Each paper can be assigned a score of 9 stars and was rated as either ‘good’, ‘fair’ or ‘poor’. The quality of each study was rated using the following scoring algorithms: ≥ 7 points were considered as ‘good’, 3–6 points were considered as ‘fair’ and ≤ 2 points was considered as ‘poor’ quality.
Statistical analysis
Information was extracted on author, type of study, geographical area, characteristics and number of participants, evaluated nutrients, type of supplement when intervention, breast milk extraction method, aim and outcome of the study, and most relevant findings. Among the examined nutrients in breast milk, results are reported for heavy metals, iodine, Fe, Cu, n-3 and n-6 PUFA, ovalbumin, persistent organic pollutants, protein, retinol, Se, vitamin A, B vitamins, vitamin B, vitamin C, vitamin D, vitamin E, vitamin K and Zn. A random effect meta-analysis was conducted with RevMan 5.4, Cochrane’s online review-writing platform on fatty acids (DHA, EPA and ARA), vitamins A, D and E, iodine and Se; however, due to high heterogeneity, it was decided not to publish the meta-analysis results. In the final summary, the overall certainty of the evidence was rated by the authors as either (1) very low, (2) low, (3) moderate or (4) high, following the Grading of Recommendations Assessment, Development and Evaluation system(18).
Results
Description of the identified studies
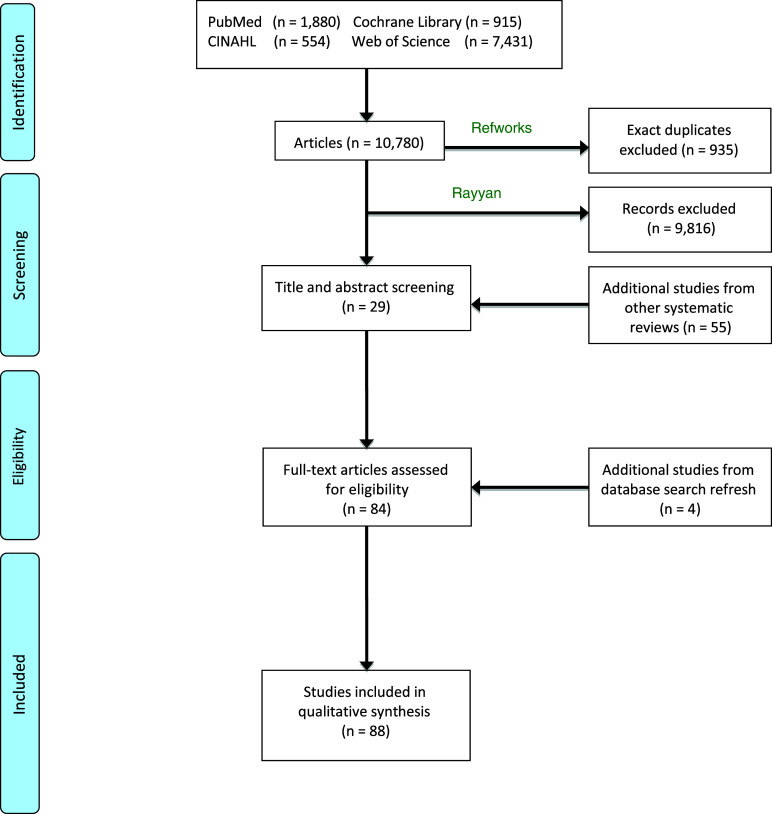
The initial search identified 10 780 articles across four databases: PUBMED, CENTRAL, CINAHL and Web of Science; Fig. 1 shows the article selection procedure (PRISMA flow chart): 10 702 articles were excluded, 935 because they were duplicates, and 9816 after abstract and title screening. Fifty-nine additional articles were identified from reference lists.
Fig. 1.
PRISMA 2009 flow diagram. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097. For more information, visit www.prisma-statement.org.
In total, eighty-eight articles were included in the final review, fifty-four experimental studies and thirty-four observational, comprising a total of 6577 participants. Twenty-nine articles examined fatty acids, thirty-one examined vitamins, twenty-three examined minerals, amino acids and proteins, and five examined contaminants (heavy metals: As, B, Pb and Hg) and PCB. For the rest of the nutrients, there were less than five studies each. The breakdown per nutrient is shown in online Supplementary Table S2.
Breast milk extraction
The breast milk collection details are summarised in Tables 1–4. The other studies either analysed samples taken over the day or did not specify the time of collection.
Table 1.
Responsivity of breast milk fatty acid content to maternal diet
| Ref | Participants Risk of bias |
Study | Ethnicity | Breast milk collection timing | Effects on breast milk PUFA content |
|---|---|---|---|---|---|
| Experimental studies | |||||
| Argaw, 2020 | Healthy lactating women 6–12 months PP Ethiopia RCT Some concerns |
215 mg DHA and 285 mg EPA per d (n 72) or placebo (control maize oil without DHA or EPA, n 82) for 6 months | African | Not provided | Supplementation increased BM DHA, by 39 % (95 % CI 20·6, 57·5 %, P < 0·001) and EPA by 36 % (95 % CI 16·0, 56·4 % P < 0·001) compared with controls |
| Boris, 2004 | Healthy lactating women enrolled at 30 weeks GA Denmark RCT Some concerns |
Fish oil supplementation (900 mg DHA and 300 mg EPA per d) until delivery (n 12), or further 30 d (n 11), or placebo (olive oil, n 13) | Danish women supposedly White Caucasian | Morning milk from one breast only | BM DHA levels 2·1, 3·6 and 2·8 times higher at 4, 16 and 30 d, respectively, in extended supplementation group v. control group (all P < 0·001) |
| Craig-Schmidt, 1984 | Healthy lactating women 2 months PP USA RCT Some concerns |
BM samples (n 8). Participants provided with a two 5 d diets with an intervening 2 d period. Diets for the two periods were identical except that source of hydrogenated fats were used in the first period and non-hydrogenated fats is the second period | Not provided | Milk samples collected after first nursing of the day by manual expression for both breasts | BM myristic acid (14:0), palmitic acid (16:0) and palmitoleic acid (16:1n-7), all significantly lower following diets with hydrogenated v. non-hydrogenated fats, whereas elaidic acid (18:1 trans-9) and oleic acid (18:1n-9) were significantly higher |
| Fougere, 2021 | Healthy lactating women, < 72 h PP France RCT Low risk of bias |
1·2 g DHA per d (n 196) or placebo (maize oil and soyabean oil, (n 193) for 14 d | Not provided | Not provided | After 14 d, significantly higher levels of BM mean (sd) DHA and EPA in supplemented (DHA: 0·95 % (0·44 %); EPA: 0·08 %, (0·05 %)) v. control (DHA: 0·34 %, (0·20 %); EPA: 0·07 %, (0·07 %)), both P < 0·0001 |
| Hawkes, 2002 | Healthy lactating women 3 d PP Australia RCT Some concerns |
300 mg DHA and 70 mg EPA per d (n 26), or 600 mg DHA and 140 mg EPA per d (n 28), or placebo (sunflower oil, n 27) for 4 weeks | Not provided | Hand-expressed morning milk | Mean (sd) BM DHA content increased in a linear manner in response to dietary DHA (placebo DHA: 0·26 %, (0·08 %); LoDHA: 0·39 %, (0·09 %); HiDHA: 0·66 %, (0·18 %); all P < 0·05). BM EPA only significantly increased in HiDHA group (placebo EPA: 0·11 %, (0·02 %); LoDHA: 0·11 %, (0·02 %); HiDHA: 0·14 %, (0·03 %); P < 0·05). No significant effects on ARA |
| Lauritzen2002 | Healthy lactating women 4 months PP Denmark RCT Some concerns |
BM samples (n 12). Lactating women were given fish oil (2–8 g) for breakfast and delivered 6–12 BM samples during the following 24 h | Not provided | Morning milk, after first feeding | Mean (sd) BM DHA of the fish-eating mothers was 0·57 %, (0·28 %) and non-fish-eating mothers was 0·42 %, (0·15 %); P = 0·05. Fish oil supplementation resulted in a 2-fold increase in BM DHA levels, peaked after 10 h and lasted for 24 h |
| Mazurier, 2017 | Lactating mothers 1–4 months PP France RCT Low risk of bias |
All groups received 350 mg DHA and 210 mg EPA per d but varied in ALA and LA content. n 19–22 per group, with 15 d washout period followed by 15 d supplementation | White Caucasian | Human milk collected at the first infant feeding of the morning | Significant dose response following in ALA (P < 0·003), but no significant effects on LA. No significant differences in DHA or EPA between groups. ARA content significantly increased only in intermediate ALA and LA dose, and n-3 PUFA-enriched rapeseed oil group |
| Mellies, 1979 | Overweight and normal weight lactating women 1 month PP USA RCT Some concerns |
BM samples (n 14), 2 weeks baseline nutrition history collected by a nutritionist, mothers randomly assigned to one diet followed by the other; diet 1: cholesterol-poor phytosterol-rich, PUFA-rich (PUFA:SFA ratio 1·8); diet 2: cholesterol-rich, phytosterol-poor, PUFA-poor (PUFA:SFA ratio 0·12) | Not provided | Samples collected at the beginning or end of the second nursing period of the day, through manual expression or breast pump | Mean (s em) for baseline diet v. diet 1 v. diet 2; milk cholesterol (mg/g milk fat) 2·4 (0·4) v. 2·4 (0·1) v. 2·5(0·2): milk phytosterols (mg/g milk fat) 0·17 (0·03) v. 2·2 (0·3) v. 0·7 (0·1); total milk fat, 3·58 (0·56) v. 2·69 (0·16) v. 2·66 (0·16) (P < 0·001) |
| Nasser, 2010 | Healthy lactating women between 2 and 6 months PP, vegetarian excluded Canada RCT Some concerns |
BM samples (n 14), low-fat diet or high-fat diet for 4 d in randomised order | Not provided | Milk collected on the last 2 d of each 4-d period between 1 and 14.00 using a manual breast pump | Significant differences in mean (sem) BM composition in low fat v. high-fat diet for lauric acid (12:0) 5·38 (1·16) v. 3·98 (0·37) (P = 0·01), palmitoleic acid (16:1n-7) 1·95 (0·29) v. 1·31 (0·23) (P = 0·046), ALA 1·22 (0·04) v. 0·69 (0·06) (P = 0·01), ARA 0·34 (0·01) v. 0·30 (0·02) (P = 0·02) |
| Park, 1999 | Healthy lactating women between 1 and 26 months PP USA RCT Some concerns |
Three-week crossover study. Week 1, minimal rumenic acid (18:2 cis-9, trans-11) foods (depletion), then either high-fat dairy food or low-fat dairy food intake for 1 week, then crossover (n 8 per group). BM samples (n 16), and dietary records during last 3 d of each period and FFQ | Not provided | Not provided | Significantly higher BM (mean (sem), μmol/g lipid) in high-fat dairy v. low-fat dairy groups for: rumenic acid (13·5 (1·1) v. 8·2 (0·4)), myristic acid (264·7 (34·2) v. 195·2 (11·0)), palmitic acid (707·0 (51·5) v. (511·3 (16·4)), stearic acid (1055·0 (103·4) v. 874·3 (33·3)), oleic acid (1055·0 (103·4) v. (874·3 (33·3)) and significantly lower ALA (10·7 (3·6) v. 17·6 (1·1)), all P < 0·05) |
| Smithers, 2010 | Mothers of preterm infants born 33 weeks GA Australia RCT Low risk of bias |
900 mg DHA, 195 mg EPA, and 54 mg ARA per d, (n 69) or placebo (soyabean oil, n 74) for 2 weeks | 98 % Caucasian | Not provided | DHA significantly higher in supplemented (M = 1·0 % sd = 0·4 %) v. placebo (M = 0·3 % sd = 0·1 %) groups, (P < 0·05). No significant differences in EPA or ARA between groups |
| Storck lindholm, 2012 | Obese and normal-weight lactating women after delivery Sweden Obs/RCT Some concerns |
Control group (BMI < 25 kg/m2, n 26), Group O (BMI > 30 kg/m2, n 25) and Group I (BMI > 30 kg/m2, n 25) were given dietary advice (e.g. eat fish 2–3 times a week) and increase physical activity. BM measured 3 and 10 d, 1 and 2 months | White Caucasian | Not provided | Group O had low fish intake and at baseline had the lowest BM ALA, EPA and DHA (all P < 0·01), which was continued across subsequent samples. The ARA: EPA + DHA ratio was significantly higher in Group O across repeated samples (P < 0·01), compared with the other groups. Group I levels approached those seen in control group |
| Valentine, 2013 | Milk donors mean lactational age 19 weeks USA RCT Some concerns |
1 g DHA/d (n 69), or placebo (soyabean oil, n 74) for 14 d | Not provided | Not provided | Supplementation significantly increased DHA content when expressed as mol wt%, but not in absolute amounts. No significant effect of supplementation on EPA or ARA content |
| Valenzuela, 2015 | Lactating women at delivery and 6 months PP Chile RCT Some concerns |
10·1 g ALA per d (chia oil, n 19) or untreated control group (n 21) for 9 months | Hispanic | Not provided | Significant increase in ALA and significant decrease in LA following supplementation v. control at all time points (all P < 0·05). DHA significantly increased in first 3 months (P < 0·05), then no effect, no change in EPA or ARA v. control at any time point. |
| Yang, 2022 | Healthy lactating women between 30 and 50 d PP China RCT Some concerns |
200 mg DHA per d (n 77) or placebo (n 60) for 8 weeks | Asian | Breast milk samples collected between 07.30 and 09.00 | Absolute GLA (18:3n-6), ARA and DHA significantly decreased over the study in control group (P < 0·001, P = 0·001 and P < 0·037, respectively), whereas GLA and DHA were maintained in supplemented group, although there was a significant decrease in ARA (P = 0·03). DHA content was significantly higher in supplemented v. control group at the end (P = 0·012. Similar trends were found when expressed as relative content |
| Observational studies | |||||
| Aitchison, 1977 | Healthy lactating women between 4 and 6 months PP USA Obs Fair Quality 6 |
BM samples (n 11), recorded food intake for 1 week and saved duplicated food portions consumed on 3 d | Not provided | Experiment 1: five subjects took morning and evening milk samples. Experiment 2: six additional subjects collected morning milk only |
Correlation coefficient (P) between PUFA to SFA ratio in maternal diet and milk (% of total FA): 0·46 considering diet and milk in the same evening; 0·43 (P < 0·05) considering milk in the next morning In nine of eleven subjects, fluctuation of percent total trans acids in the milk appeared to follow dietary trans changes after a 12–36-h lag period |
| Antonakou, 2013 | Healthy lactating women 1 month PP Greece Obs Fair Quality 6 |
BM samples 1-month PP (n 64), 3-month PP (n 39), 6-month PP (n 24). Three-day dietary record at 1st, 3rd and 6th month PP | Caucasian | Morning milk collected after at least 2 h after previous breast-feeding | BM fat ranged from 26·3 and 30·2 g/l (P < 0·05). Strong positive effect found during first month lactation between mother’s PUFA intakes and BM PUFA concentration, r = 0·25, P < 0·05; n-3 fatty acids, r = 0·26, P < 0·05; DHA r = 0·27, P < 0·05 and LA, r = 0·26, P < 0·05, while MUFA intake was strongly correlated with concentration of PUFA, r = 0·29, P < 0·05; n-6, r = 0·27, P < 0·05 and LA,, r = 0·25, P < 0·05 |
| Bzikowska, 2019 | Healthy lactating women 1 month PP Poland Obs Fair quality 6 |
BM samples (n 32) and dietary information 3-d dietary record and FFQ | Not provided | Foremilk and hindmilk collected from four time periods: 06.00–12.00, 12.00–18.00, 18.00–00.00 and 00.00–06.00 | Significant positive correlation between fatty fish consumption and DHA (τb = 0·25, P = 0·049), EPA (τb = 0·27, P = 0·03) and ALA (τb = 0·28, P = 0·02). ALA positively correlated with intakes of linseed oil (τb = 0·3, P = 0·01), coconut oil (τb = 0·29, P = 0·02) and milk (τb = 0·26, P = 0·04). EPA positively correlated with pork consumption (τb 0·29, P = 0·02) |
| Daud, 2013 | Healthy lactating women between 15 d and 6 months PP Malaysia Obs Fair Quality 6 |
BM samples (n 101). Participants provided a 1-year period FFQ. Sub-experiment, BM samples (n 18). Participants provided a 3-d FFQ | Asian | Not provided | The most abundant BM trans-fatty acid was linoelaidic acid (mean = 1·44%, sem = 0·60 % fatty acids), which was also the most consumed (mean = 0·07 sem = 0·01, g/100 g of food). Ten food items had an effect on the total BM trans-fatty acids (buns, chicken burgers, cheeseburgers, shortening, powdered milk, sweetened milk blended oil mayonnaise, maize oil and ice cream). No association between consumption and BM trans-fatty acid levels |
| De la Presa-Owens, 1996 | Healthy lactating women < 1 PP Spain Obs Poor Quality 2 |
BM samples (n 40), dietary questionnaire | Not provided | Not provided | Lower BM LA observed between mothers consuming olive oil (n 15) or sunflower (n 6) as the preferred source of fat (P < 0·001). Significant differences in BM DHA and EPA between mothers reporting high, low or no fish consumption (P < 0·001) |
| Freitas, 2019 | Healthy lactating women < 3 PP Brazil Obs Fair quality 2 |
Diet quality assessed through a semi-structured questionnaire (n 106) | Most participants black/multiracial (82 %) | Sample collected after the first breast-feeding of the morning | Long-chain n-3 and n-6 PUFA not analysed separately. Total fruits and whole fruits, r = −0·302, r = 0·283, respectively, both P < 0·05 |
| Juber, 2017 | Healthy new mothers > 1 week PP USA Obs Fair quality 7 |
BM at baseline (n 84), subject received analysis of BM DHA and dietary recommendations (n 60) had second sample at 1 month | 99 % White Caucasian | Not provided | Those reporting taking DHA supplements (n 43) had higher levels than those who did not (0·23 % v. 0·15 %, P < 0·0001). In second sample, median breast milk DHA content increased from 0·19 % to 0·22 % (P < 0·01) |
| Liu, 2015 | Healthy lactating women 22–25 d PP China Obs Good quality 8 |
Dietary intake of lactating women assessed with 24-h dietary recall questionnaire (n 514) | Asian | Morning milk, manual expression between 09.00 and 11.00 | Significant negative correlation between dietary ALA and BM GLA (18:3n-6, r2 = −0·201, P = 0·03) and adrenic acid (22:4n-6, r2 = −0·197, P = 0·03), and dietary LA and BM DGLA (20:3n-6, r2 = −0·182, P = 0·03) |
| Makela, 2013 | Overweight and normal-weight lactating women 3 months PP Finland Obs Good quality 8 |
BM samples (n 100), self-administrated dietary record of the day before milk samples collection every day for 1 week | Not provided | Morning milk, manual expression | Mean (sd) BM from overweight v. normal weight women: SFA (46·3 % (4·4) v. 43·6 % (6·0), P = 0·012), n-3 PUFA (2·2 % (0·79) v. 2·7 % (1·1), P = 0·010), ratio of unsaturated to saturated FA (1·1 (0·2) v. 1·3 (0·4), P = 0·008). Pearson’s correlation coefficient between the high-fat dairy products and breast milk SFA: 0·21 (0·04). |
| Olafsdottir, 2006 | Healthy lactating women between 2 and 4 months PP Iceland Obs Fair quality 6 |
BM samples (n 77), 24-h recalls and food questionnaire on fish consumption and dietary habits. Two groups: women consuming (n 18) v. not consuming cod liver oil (n 59) | Not provided | Collection of four times per d | Proportion of PUFA in the diet is significantly higher among women consuming cod liver oil. It also gives higher % of DHA, EPA and DPA n-3 in BM. Correlation coefficient between maternal diet and milk FA composition (% of total FA): maternal PUFA: SFA and milk ALA, 0·336 (P = 0·003): maternal PUFA and milk ALA, 0·432 (P < 0·001): maternal PUFA and milk EPA, 0·302 (P = 0·008): maternal protein and milk EPA, 0·362 (P = 0·001): maternal protein and milk DPA, 0·373 (P = 0·001): maternal protein and milk DHA, 0·346 (P = 0·002) |
| Perrin, 2019 | Healthy lactating women ≥ 2 weeks PP USA Obs Good quality 7 |
Single BM sample from vegan lactating women (n 26), vegetarian lactating women (n 22) and omnivore lactating women (n 26) | Not provided | Sample collected in the morning during first and second breast-feeding of the day and at least 2 h since previous breast-feeding in a dimly lit room to protect light-sensitive nutrients | Vegan, vegetarian and omnivores median (IQR) unsaturated fatty acids were 66·0 % (6·5 %), 57·8 % (9·8 %) and 56·2 % (8·5 %), respectively (P < 0·001). Total n-3 PUFA were 2·29 % (0·77 %) for vegans 1·55 % (0·56 %) for vegetarians and 1·46 % (0·94) for omnivores (P < 0·001), with significant difference driven by higher ALA (P < 0·001). Ratio of LA to ALA was significantly lower (P < 0·001) in BM vegans 9·3 % (2·1 %) compared with vegetarians 12·2 % (4·9 %) and omnivores 12·7 % (6·2 %). No significant differences in DHA, but over 80 % had levels below 0·30 %. Reports of n-3 PUFA supplement and seafood consumption were limited |
| Sanders, 1978 | Vegan and omnivore healthy lactating women between 2 and 6 months PP UK Obs Fair Quality 6 |
BM samples (n 8) | Caucasian | Sample collected at the start of the morning | BM of vegans contained lower proportions of 16:0, 16:1, 18:0 and 20:4 n-3 and higher proportions of 18:2 n-6 (P < 0·05) |
| Sanders, 1992 | Healthy lactating mothers < 14 weeks PP UK Obs Fair quality 6 |
Milk samples from (n 45); (n 19 vegans, n 5 vegetarians and n 21 omnivores); 3-d food dietary | White vegetarians and vegan, Indian vegetarians and Whit e omnivores | Not provided | In comparisons to omnivores, vegan’s BM contains higher proportion of SCFA (C10–C14) and lower proportion of medium-chain FA (C16–C18); (P < 0·01). Same proportion of ARA is in all groups, and proportion of BM DHA is lower in vegans than in omnivores and vegetarians (P < 0·01). The n-6/n-3 FA ratio was higher in the vegan group than in the others |
| Scopesi, 2001 | Healthy lactating women < 1 month PP Italy Obs Fair quality 6 |
BM samples (n 34) 1 d PP, 4 d PP, 14 d PP, 21 d PP and 28 d PP. Dietary questionnaire referred to the day prior milk extraction for sampling |
Not provided | Not provided | Pearson’s correlation coefficient between maternal dietary intake and corresponding BM concentrations (% of total FA): SFA, 0·60 (P < 0·01) in transitional milk; MUFA, 0·63 (P < 0·01) in transitional milk; PUFA, 0·65 (P < 0·01) in mature milk |
RCT, randomised control trial; BM, breast milk; PP, postpartum; AM, ante meridiem ; PM, post meridiem; M, median; GA, gestational age; Obs, observational study; ALA, α-linolenic acid; ARA, arachidonic acid; ALA, α-linolenic; LA, linoleic acid; DGLA, dihomo-γ-linolenic acid; DTA, docosatetraenoic acid; GLA, γ-linolenic acid.
Table 4.
Responsivity of breast milk contaminant levels in response to maternal diet
| Ref | Participants Risk of bias |
Study | Ethnicity | Breast milk collection timing | Effects on breast milk content |
|---|---|---|---|---|---|
| Observational studies | |||||
| Castro, 2014 | Lactating mothers Chile, 2–4 months PP Obs Fair quality 7 |
Participants from Arica (n 24) and southern Santiago (n 11) completed questionnaires on health status, food habits and breast-feeding practices. BM As, B, Cd, caesium, Ca, Fe, Pb, Li, Mn, Se, U, V and Zn measured | Not provided | BM collected during the morning | No difference in essential and toxic element levels between groups, except B (P < 0·001) and Li (P < 0·05), which were higher in Arica. Caesium was higher in Santiago samples (P < 0·05). Pb positively associated with Fe and Zn (r = 0·60, r = 0·61, respectively, both P < 0·05), but inversely associated with Ca (r = −0·61, P < 0·05). As associated with Fe (r = 0·6, P < 0·05), and B and Ca (r = 0·54, P < 0·05) |
| Dewailly, 1994 | Lactating healthy Inuit women < 3 d PP Artic Quebec Obs Poor quality 2 |
Inuit (n 109) participants. Seven PCB and chlorinated pesticides determined in BM and compared with Quebec Caucasian women. | Inuit | Not provided | Mean levels of the different analysed PCB were 3–7 times higher in BM from Inuit v. Caucasian women. Seafood consumption was extremely high for Inuit women, at 300 g/d compared with 12 g/d for Caucasian women |
| Gundacker, 2002 | Healthy lactating mothers < 1 month PP Austria Obs Good quality 8 |
Urban (n 59) and rural (n 47) participants completed questionnaire about dietary habits, smoking, living area and dental filings. | Not provided | Not provided | Low Hg and Pb concentrations were far below currently recommended safety limits (Hg: mean = 1·59 g/l, sd = 1·21 g/l, n 116; Pb: mean = 1·63 g/l, sd = 1·66 g/l, n 138). Hg was significantly associated with area of residence, prematurity, cereal consumption and vitamin supplementation, whereas for Pb it was area of residence, fish consumption and smoking, all P < 0·05 |
| Leotsinidis, 2005 | Healthy lactating mothers 3 d PP Greece Obs Fair quality 6 |
BM samples collected (n 180) to measure Cd and Pb at 3 and 14 d PP, FFQ | Not provided | Morning milk 2 h after previous breast-feeding | Mean (sd) values of colostrum samples: Cd, 0·190 (0·150) µg/l; Pb, 0·48 (0·60) µg/l. Higher BM lead in samples from urban areas, dietary habits seem to play a role in metal levels in human milk |
| Ursinyova, 2018 | Healthy lactating mothers 6 weeks PP Slovakia Obs Good quality 7 |
n 142 participants asked about dietary habits, including frequency and amount of fish consumption per d | Not provided | Hand expression, no information on timing | Total Hg mean = 0·376 µg/l, sd = 0·475 µg/l, with no difference between fish and non-fish eaters. Negative association between BM total Hg and freshwater fish consumption (β = −0·193, P = 0·017) |
Obs, observational study; PP, postpartum; BM, breast milk; PCB, polychlorinated biphenyls.
Ethnicity
The articles included in this review involved African, Arabic, Asian, Australian, European and Hispanic participants, as summarised in Tables 1–4.
Main results
Fatty acids
Twenty-nine publications on fatty acids were included, fifteen experimental studies(19–33), and fourteen observational studies(34–47) and are summarised in Table 1.
Of the experimental studies, three were rated low risk of bias(22,25,29) and twelve were identified having some concerns(19–21,23,24,26–29,31–33). For the observational studies, three were of good quality(41,42,44), nine were fair quality(34–36,39,40,43,45–47) and two were poor quality(38,39).
PUFA
Nine experimental studies were identified with DHA and EPA, and participants were supplemented with DHA in the range of 200 to 1200 mg/d, and EPA between 70 and 300 mg/d(19,20,22–25,29,31,33). DHA and EPA supplementation was consistently shown to increase DHA and EPA breast milk levels, and this was in a dose-dependent manner. Two RCT investigated the effects of maternal α-linolenic acid (ALA) and LA maternal supplementation on breast milk, and ALA maternal intake was similarly show to increase breast milk ALA levels(25,32). The observational studies also reported a significant positive correlation between maternal consumption of fatty fish intake and breast milk DHA, EPA and ALA(36,38,40,43,44). The effect of vegan, vegetarian or omnivore diet patterns on breast milk fatty acids fat composition was investigated in three observational studies(44–46). DHA levels were either significantly lower in vegans than omnivores or vegetarians(46) or low across all groups(44). The LA to ALA ratio was significantly lower in breast milk from vegan participants compared with vegetarians and omnivores(44). In comparison to omnivores, breast milk from vegans contains a higher proportion of SCFA (C10–C14) and lower proportion of medium-chain fatty acid (C16–C18). For ARA, only one study was identified, and in this experimental study participants were supplemented with 54 mg ARA per d for 2 weeks and no relationship was identified between maternal intake and breast milk levels(29).
Others fatty acids
Trans-fatty acids, SFA and hydrogenated fats consumption and their content in breast milk were investigated in four studies(21,34,37,42). The consumption of hydrogenated vegetable oils with high content of trans-fatty acid increased the trans-fatty acids concentration in breast milk after a 12–36-h lag period.
Lipid-soluble vitamins (A, D, E and K)
Vitamin A
Eight publications were included for vitamin A, which were all experimental studies(48–55). One was low risk of bias(52), four presented some concerns(48,51,53,54) and three were high risk of bias(49,50,55), with the results summarised in Table 2.
Table 2.
Responsivity of breast milk vitamin content to maternal diet
| Ref | Participants Risk of bias |
Study | Ethnicity | Breast milk collection timing | Effects on breast milk vitamin content |
|---|---|---|---|---|---|
| Vitamin A | |||||
| Experimental studies | |||||
| Bahl, 2002 | Healthy women 18–42 d PP Ghana, India and Peru RCT Some concerns |
Single dose (60 mg) retinyl palmitate (n 322) or control (soyabean oil, n 309). Milk retinol levels at 0, 2, 6 and 9 months | Hispanic, Indian and African | Usually collected between 09.00 and 12.00 | Significantly higher retinol in treatment group at 2 months only (difference in means 7·1 nmol/g fat, 91 % CI 3·4, 10·8, P < 0·05) |
| Basu, 2003 | Healthy lactating women after delivery India RCT High Risk of bias |
Single dose (209 μmol, 200 000 μg) retinol within 24 h of delivery (n 139), and untreated control group (n 132). Milk retinol levels at 0 and 24 h, and 1–6 months | Asian | Colostrum collected by manual breast pump, no information in the collection timing | Treatment group had significantly higher retinol levels up to 4 months (P < 0·01) |
| Canfield, 2001 | Lactating women 7 months PP Honduras RCT Some concerns |
90 mg β-carotene as red palm oil (n 32), β-carotene supplements (n 36) or placebo (n 18). Six doses over 10 d. Milk retinol, lutein, β-cryptoxanthin, lycopene, α- and β-carotene at 0 and 10 d | Hispanic | Mid-morning collection by manual expression | No significant difference in retinol, but palm oil supplementation led to greater increases in lutein, lycopene, α- and β-carotene v. control. Increases in β-carotene concentrations were greater for the palm oil group (2·5-fold, P < 0·0001) than for the β-carotene concentrations supplement group (1·6-fold, P < 0·006) relative to placebo |
| Canfield, 1998 | Healthy lactating women < 6 months PP USA RCT High Risk of bias |
Participants received a single dose of 60 mg (group 1, n 6) or 210 mg (group 2, n 6) of β-carotene. Milk retinol. α-Tocopherol and carotenoids were monitored for 8 d | Not provided | Mid-afternoon | Data show that a single 60 mg supplement of β-carotene sustained elevated β-carotene concentrations in milk for > 1 week in healthy mothers but did not affect concentrations of other carotenoids, retinol and α-tocopherol β-Carotene concentration in BM group 1 v. group 2, mean (se): 36·1(5·5) nmol/g lipid v. 50·4 (16·8) nmol/g lipid. α-Carotene concentration in BM group 1 v. group 2, mean (se): 10·4 (2·4) nmol/g lipid v. 14·0 (5·0) nmol/g lipid Lycopene concentration in BM group 1 v. group 2, mean (s e): 18·7 (3·4) nmol/g lipid v. 34·7 (5·6) nmol/g lipid (P < 0·05) |
| Ding, 2021 | Healthy lactating women 30–45 d PP China RCT Low risk of bias |
Supplementation for 2 months with 1800 μg vitamin A and 600 μg vitamin D (n 117), or placebo (n 128) | Asian | BM collected between 07.30 and 09.00 through breast pump | After 2 months vitamin A in supplemented group was M = 1 (sd = 0·5) µmol/l v. control group M = 0·8 (sd = 0·5) µmol/l, P < 0·05. |
| Gossage, 2002 | Healthy lactating women < 32 d PP USA RCT Some concerns |
Subjects (n 21) received 30 mg/d of β-carotene or placebo from day 4 to day 32 PP. BM samples analysed for concentrations of carotenoids, α-tocopherol, and retinol. Eight diet records and eight BM samples | Two African American, two Hispanic and 17 European American | Not provided | No significant effects of β-carotene supplementation on BM concentrations of lutein, β-cryptoxanthin, lycopene or α-carotene. Milk concentrations for all four carotenoids decreased over time (P < 0·01 for all). Milk concentration in retinol andα- tocopherol were unaffected by supplementation and decreased over time (P < 0·0050. Mean (sd) retinol concentration were 4944 (539) µmol/l initially and 2079 (207) µmol/l at the end of the study. α-Tocopherol concentrations were 31 (4·6) µmol/l initially and 9·4 (1·2) µmol/l at the end of the study |
| Grilo, 2016 | Healthy puerperal women 24 h PP Brazil RCT Some concerns |
Single dose (60 mg, 200 000 μg) retinyl palmitate after first colostrum collection (n 30), and untreated control group (n 27). Milk retinol and α-tocopherol levels at 0 and 24 h and 30 d | Not provided | Collection after an overnight fast from 08.00 until 12.00 | Intervention significantly increased retinol levels at 24 h (+157 %, P < 0·001); however, retinol levels of both groups did not differ at 30 d. After supplementation, colostrum α-tocopherol decreased significantly (–16·4 %, P < 0·05), but no significant difference in α-tocopherol levels between groups at 30 d. |
| Johnson, 1997 | Healthy lactating women < 8 months PP USA RCT High Risk of bias |
Subjects given either placebo (n 4) or naturally occurring β-carotene (64 mg all-trans BC and 69 mg 9-cis BC; n 8) for 8 d | Not provided | Not provided | For supplemented group, significant increase in concentration observed at day 3 (P < 0·001) and steadily increased to six times the baseline level by the end of the supplementation period (day 8, P < 0·001). After 1 month, BM concentration of all-trans BC decreased but was still significantly higher than day 1 (P < 0·022). |
| B vitamins | |||||
| Experimental studies | |||||
| Chang, 2002 | Healthy lactating women < 1 month PP USA RCT High risk of bias |
Four groups of lactating mothers (n 47) receiving 2·5, 4, 7·5 and 10 mg/d of PN-HCl, 24 h dietary record. | Not provided | Not provided | BM vitamin B6 responsive to maternal supplementation from 1–6 months PP. Mean BM B6 significantly lower for women supplemented with 2·5 mg PN-HCl/d than for those supplemented with 4·0, 7·5 or 10·0 mg/d. Mean (sem) range from 1–6 months for groups supplemented with 2·5 mg/d (891 (29·9) to 1·316 (74·8) nmol/l), 4 mg/d (1184 (40·8) to 1944 (74·8)), 7·5 mg/d (1·752 (86·7) to 2278 (86·7)), and 10 mg/d (1704·3 (38·9) to 2338·1 (104·7) nmol/l). |
| Hampel, 2017 | Healthy lactating women 2–4 months PP Bangladesh RCT Low risk of bias |
3-d supplementation study (n 18). Day 1: fasting no supplement, day 2: one time the US Canadian RDA for vitamins, day 3: Twice US Canadian RDA for vitamins. BM vitamin A, B1, B2, B3, B6, B12 and E measured | Not provided | Breast milk collected at each feeding through a breast pump form the same breast for 24 h | BM vitamin A, B1, B2 and B6 significantly increased in BM-supplemented group, median increases > 180 % (B2 and B6) and 120–130 % for B1 and A. B3 and E levels significantly lower on days supplements were consumed (P < 0·05). No significant effect of supplementation for B12 |
| Nail, 1980 | Healthy lactating women at parturition USA RCT Some concerns |
Two groups, one (n 7) received vitamin B1 and B2 supplementation (B1 1·7 mg/d, B2 2·0 mg/d), second group (n 5) received no supplementation. BM samples after 1 and 6 weeks supplementation | Not provided | Not provided | BM mean (sd) B1 of both groups after 1 and 6 weeks, respectively were: non-supplemented 138 (18) µg/l and 220 (27) µg/l; and supplemented 133 (27) µg/l and 238 (21) µg/l. There were significant increases in B1 both groups (P < 0·05). BM mean (sd) B2 of both groups after 1 and 6 weeks, respectively, were non-supplemented 367 (128) µg/l and 485 (123) µg/l and supplemented 880 (168) µg/l and 710 (187) µg/l |
| Styslinger, 1985 | Healthy lactating women 2–3 months PP USA RCT High risk of bias |
0, 2·5, 10·0 or 20·0 mg pyridoxine-HCl for three consecutive days in addition to dietary sources (n 6). BM samples at baseline and 3 d | Not provided | Not provided | Significant positive correlation (r = 0·80, P < 0·001) between supplemental intake and vitamin B6 content |
| Thomas, 1979 | Healthy lactating women 1 week PP USA RCT High risk of bias |
No supplement (n 7), or multivitamin and multimineral supplement (n 10), containing 4 mg vitamin B6. BM measured for 3 d periods at 1 and 6 weeks | Caucasian | Milk samples expressed four times a day at 4 h interval | Vitamin B6 differed significantly (P < 0·05) at 5–7 d. At 43–45 d, content significantly increased (P < 0·05) in supplemented group. Content in supplemented group remained constant at 43–45 d, and the difference between groups at 43–45 d was not significant |
| Thomas, 1979 | Healthy lactating women 1 week PP USA RCT High risk of bias |
Non-supplement (n 7) and multivitamin and multimineral supplement (n 10), containing 8 μg of vitamin B12. BM measured for 3 d periods at 1 and 6 weeks | Caucasian | Milk samples expressed four times a day at 4 h interval | No significant differences between the groups at 5–7 d. Decline in both groups at 43–45 d. However, levels in non-supplemented group were significantly lower than both the 5 to 7 d levels. Mean (sd) values for non-supplemented were 1·22 (0·41) µg/l at 5–7 d and 0·61 (0·17) µg/l at 43–45 d, (P < 0·05), and supplemented group at 43–45 d PP; and supplemented were 1·65 (0·63) µg/l at 5–7 d, 1·10 (0·57) µg/l, (P < 0·05). |
| Vitamin C | |||||
| Experimental studies | |||||
| Byerley, 1985 | Healthy lactating women 11 weeks PP Canada RCT High risk of bias |
Five vitamin C groups (1) 0 mg, 0 mg 1 d + 90 mg per for 2 d, (3) 90 mg for 1 d + 250 mg per d for 2 d, (4) 90 mg for 1 d + 500 mg per d for 2 d, (5) 90 mg for 1 d + 1000 mg per d for 2 d, all n 5 | Not provided | BM collected at each feeding either manually or by use of breast pump | Mean vitamin C ranged from 44 to 158 mg/l but not correlated with intake and not significantly different between groups |
| Daneel Otterbech, 2005 | Healthy lactating women Switzerland and Republic of Ivory Coast 8 mPP RCT High risk of bias |
Five separate studies: 1. Baseline milk ascorbic acid levels European (n 142) and African (n 171) women. 2. 1000 mg ascorbic acid per d for 10 d, European (n 10) and African (n 18) women. 3. European women (n 17), 1000 mg ascorbic acid per d for 5 d, followed for 35 d. 4. African women (n 11), 100 mg ascorbic acid per d for 10 d. 5. 1, 3 or 5 servings of orange juice (100 mg ascorbic acid/serving) per week for six weeks, African women (n 15) |
Caucasian and African | All samples collected between 07.00 and 12.00 | BM vitamin C 50 % lower (P < 0·001) from African women. Supplementation (1000 mg/d for 10 d) increased levels in both African and European women, from 19 to 60 mg/kg (P < 0·001) and 60 to 70 mg/kg (P < 0·03), respectively |
| Thomas, 1979 | Healthy lactating women 1 week PP USA RCT High risk of bias |
Non-supplement (n 7) and multivitamin and multimineral supplement (n 10), containing 90 mg vitamin C from parturition. BM analysed for 3 d periods at 1 and 6 weeks | Caucasian | BM samples expressed four times a day at 4 h intervals | No significant differences in levels between groups at any time points |
| Vitamin D | |||||
| Experimental studies | |||||
| Ala-Houhala, 1988 | Healthy lactating women 8 weeks and 20 weeks PP USA RCT High risk of bias |
Daily supplementation for 8 weeks (Winter) and 15 weeks (Spring) with 2000 μg (n 15) vitamin D, 1000 μg vitamin D (n 15), or no supplementation (n 15) | Not provided | Morning milk | Oral maternal supplementation of vitamin D had no significant effect on milk vitamin D levels, but 25(OH) D levels of mothers receiving either 1000 or 2000 μg (25 or 50 micrograms) vit D/d were significantly higher than those of non-supplemented mothers in February and April |
| Basile, 2006 | Healthy lactating women 1 month PP USA RCT Low risk of bias |
Subjects received (n 12) 2000 μg/d vitamin D or (n 13) 4000 μg/d for 3 months. BM samples collected to measure vitamin D | 16 White and 9 African-American | Not provided | 25 (OH) D increased from 1 to 4 months in both group (mean (sd)): (+11·5 (2·3)) ng/ml for group 2000 (P = 0·002) and (+14·4 (3·0)) ng/ml for group 4000 (P = 0·0008). The 4000 μg/d regimen was more effective in raising BM antirachitic activity than the 2000 μg/d supplementation. Decline in BM was not associated with vitamin D dose (P = 0·73) or maternal 25(OH)D (P = 0·94) |
| Ketha, 2018 | Healthy lactating women < 6 months PP USA RCT Low risk of bias |
Subjects (n 40) received either a single dose 150 000 μg or 5000 μg daily of vitamin D3 for 28 d. BM vitamin D measured at 1, 3, 7, 14 and 28 d. Outcome was the temporal changes in 24,25 (OH)2D3/25(OH)D3 ratio |
Not provided | Not provided | BM vitamin D3 values in the single-dose group were inversely associated with 24,25 (OH)2D3/25(OH)D3 ratio (r2 = 0·14, P < 0·001), but not with daily dosing |
| Niramitmahapanya, 2017 | Healthy lactating women < 6 weeks PP Thailand RCT Low risk of bias |
Subjects received either 800 μg/d vitamin D supplement (n 35) for 6 weeks or a placebo (n 33) | Asian | Not provided | BM vitamin D at baseline mean (sd) supplemented group v. non-supplemented group: 79·86 (18·27) nmol/l v. 88·33 (21·28) nmol/l, (P = 0·183). Vitamin D BM concentration at 6 weeks supplemented group v. non-supplemented group: 97·49 (19·32) nmol/l v. 88·92 (22·42) nmol/l, (P = 0·076) |
| Oberhelman, 2013 | Healthy lactating women < 6 months PP USA RCT Some concerns |
Single dose 150 000 μg cholecalciferol (n 20) or 5000 μg/d cholecalciferol (n 20) for 28 d. BM cholecalciferol and 25(OH)D measured on 0, 1, 3, 7, 14 and 28 d | Not provided | Not provided | BM mean cholecalciferol reached peak of 40 ng/ml at 1 d in single-dose group, whereas in the daily supplemented group levels remained at approximately 8 ng/ml from 3 to 28 d |
| Vitamin E | |||||
| Experimental studies | |||||
| Clemente, 2015 | Healthy lactating women 12 h PP Brazil RCT Low risk of bias |
Non-supplemented control (n 36), single dose 400 μg RRR-α-tocopherol (n 40), or single dose 400 μg all-rac-α-tocopherol synthetic (n 33). BM colostrum α-tocopherol measured 12 h PP and 24 h after supplementation | Not provided | Colostrum collected by manual expression, no information on timing | No change in control group at 24 h, whereas RRR α-tocopherol and all-rac α-tocopherol increased by 57 % and 39 %, respectively (significantly different between control group and α-tocopherol synthetic group and control group and α-tocopherol natural group, P < 0·001); significantly different between α-tocopherol synthetic group and α-tocopherol natural group, P = 0·04) |
| Gaur, 2017 | Healthy lactating mothers < 4–6 weeks PP USA RCT Low risk of bias |
3 groups (n 89), group 1 (n 29) received 45·5 mg all-rac-α-tocopherol acetate, group 2 (n 30) 22·8 mg all-rac-α-tocopherol acetate + 20·1 mg RRR-α-tocopherol, group 3 (n 30) 40·2 mg RRR α-tocopherol for 6 weeks | Not provided | Not provided | In group 3, % of RRR-α-tocopherol increased in BM (mean (sem): 78 % (2·3 %) compared with 82 % (1·7 %) (P < 0·05). In contrast, the % of RRR-α-tocopherol decreased in the group 2 (P < 0·05) and group 1 (P < 0·0001) |
| Kanno, 1989 | Healthy lactating mother 70 d parturition Japan RCT High risk of bias |
d-α-Tocopherol (1·1 g) in a capsule was orally administrated once with ice cream to a mother | Not provided | BM expressed 2–3 times daily with manual pump | The transfer of α-tocopherol into BM reached a maximum value of 414 µmol/100 g after 3 d and then declined to the baseline level after 5 d. The amount of α-tocopherol recovered in BM was 0·11 %. The α-tocopherol equivalent/PUFA ratio (mg/g) was increased from 0·25 to value between 0·7 and 1·7 |
| Pires Medeiros, 2016 | Healthy lactating women < 30 d PP Brazil RCT High risk of bias |
Non-supplemented control (n 51), of single dose 400 μg RRR-α-tocopherol (n 38). BM α-tocopherol measured after delivery, 24 h, 7 and 30 d | Not provided | Samples collected after an overnight fast | BM α-tocopherol increased by 60 %, 24 h after, but not control group (P < 0·001). At 7 d supplemented group levels 35 % higher than control group, but no difference at 30 d |
| De Souca Reboucas, 2019 | Healthy lactating women 30–90 d PP Brazil RCT Some concerns |
Single dose 800 μg (588 mg, RRR-α-tocopherol, (n 39), or non-supplemented control (n 40). BM α-tocopherol measured at supplementation and next day. | Not provided | BM collected manually from a single breast that had not been collected previously | No difference between control and supplemented groups at baseline. One day after supplementation, supplemented group levels significantly increased by 124 % (mean = 15·00 µmol/l, sd = 5·1 µmol/l, P < 0·001), with no change in control group (mean = 6·94 µmol/l, sd = 2·0 µmol/l) |
| Observational studies | |||||
| Antonakou, 2011 | Healthy lactating mothers < 1 month PP Greece Obs Good quality 8 |
BM samples (n 64), 3 d dietary record at 1, 3 and 6 months PP | Not provided | Morning hour BM collection by electric pump | BM mean (sd)α tocopherol was 8·3 (3·4) µmol/l, 8·1 (4·2) µmol/l and 8·5 (4·7) µmol/l at 1, 3 and 6 months PP, respectively; while total tocopherol values were 8·9 (3·6) µmol/l, 8·7 (4·6) µmol/l and 9·5 (5·6) µmol/l, respectively. No significant differences observed between the time points. Mean (sd) maternal vitamin E dietary intake was 7·2 (3·7) mg/d, 6·8 (3·5) mg/d and 10·9 (5·2) mg/d at 1, 3 and 6 months PP, respectively. Though, vitamin E dietary intake was lower than the recommended one. Correlation of dietary intake parameters with the concentration of vitamin E in mature milk at first month of lactation: total fat (% total fat), r = 0·244, P = 0·047, PUFA (% total fat) r = 0·092, P = 0·387; MUFA (% total fat) r = 0·195, P = 0·062 |
| Vitamin K1 | |||||
| Experimental studies | |||||
| Bolisetty, 1998 | Healthy lactating women with preterm births, 28–32 weeks RCT High risk of bias |
2·5 mg phylloquinone (vitamin K1) daily for 2 weeks (n 6). BM phylloquinone measured daily for 14 d | 4 Caucasian and 2 Asian | BM extracted either manually or with electric pump at 5 h intervals | Mean (sd) BM levels increased from baseline: 3 (2·3) ng/ml to 22·6 (16·3) ng/ml, (P < 0·05) after the first dose, with continual increase until plateau at 64·2 (31·4) ng/ml after sixth day |
| Greer, 1997 | Healthy lactating mothers < 3 d PP USA RCT Low risk of bias |
2 groups: either 5 mg of phylloquinone (n 11) or placebo (n 11), daily supplementation for 12 weeks. Placebo was glucose. BM collected after 2 weeks, 6 weeks and 12 weeks supplementation |
Not provided | Not provided | Mean (sd) BM vitamin K supplemented v. placebo: 1·10 (0·75) ng/ml v. 0·69 (0·39) ng/ml at baseline; 76·53 (26·98) ng/ml v. 1·17 (0·70) ng/ml after 2 weeks (P < 0·01); 75·27 (46·23) ng/ml v. 1·14 (0·46) ng/ml after 6 weeks (P < 0·01) |
| Von Kries, 1987 | 1 lactating mother Germany < 5 weeks PP RCT High risk of bias |
Single dose of 0·5 mg, 1 mg and 3 mg vit K1 (n 1 per group). Dose response (0·1 mg, 0·5 mg, 1 mg and 3 mg) measured over 24 h (n 1). Single dose study measured BM vitamin K1 over 50 h, and dose–response study measured over 24 h | Not provided | Complete expression of both breasts using an electric pump | 0·5 mg, 1 mg and 3 mg produced increases in milk levels, peaking at 12–24 h. Dose–response relationship observed, with the lowest dose (0·1 mg) producing 2-fold increase in vitamin K1 content. 100 µg dose of vitamin K1 raised BM vitamin K1 from 2·5 to 4·9 ng/ml after 16 h, this then declined to 1·9 ng/ml after 24 h |
PP, postpartum; RCT, randomised control trial; BM, breast milk; AM, ante meridiem; PM, post meridiem; M, median; Obs, observational study.
Maternal β-carotene supplementation increased β-carotene concentration in breast milk without impacting retinol, α-tocopherol or other carotenoid breast milk content. A similar effect is observed with retinol, lactating mothers supplemented with retinol produce a higher retinol concentration breast milk without affecting other carotenoids. The supplements in the experimental studies varied from 30 mg of β-carotene daily to 60 mg of retinyl palmitate or β-carotene single dose and 90 mg β-carotene as red palm oil in six doses over 10 d.
Vitamin D
Five publications were included for vitamin D, all experimental studies(56–60) Three were low risk of bias(57–59), one with concerns(60) and one rated high risk of bias(56), with the results summarised in Table 2. One study reported that daily maternal supplementation had no significant effect on vitamin D breast milk concentration(56). The other four studies reported that a single large dose supplementation was more effective in raising breast milk vitamin D concentration than a smaller daily supplementation(57–60). The supplements in the experimental studies varied from 50 µg per d to 3750 µg single dose.
Vitamin E
Six studies were included for vitamin E, with five experimental(61–65) and one observational(66), and are summarised in Table 2. Among the experimental studies, two were low risk(61,63), one was rated with some concerns(62) and two were high risk of bias(64,65), whereas the observational study was considered good quality(66).
Maternal intake of vitamin E (α-tocopherol) was shown to influence breast milk vitamin E concentration. The supplements in the experimental studies ranged from 40 mg/d to 536 mg in a single dose.
Vitamin K
Three experimental studies measuring vitamin K were included(67–69), as summarised in Table 2. One was low risk of bias(68), and two were considered high risk of bias(67,69). The three studies reported that supplementing lactating mothers with vitamin K produced an increase in hind milk, foremilk and total breast milk vitamin K concentration, with a peak 12–24 h after supplementation. Vitamin K supplements varied from 0·5 to 5 mg per d for a period of 1 d up to 12 weeks.
Water-Soluble vitamins
B vitamins
Five experimental studies were included(70–74), one was rated as low risk of bias(71), one presented some concerns(72) and three were high risk of bias(70,73,74), and are summarised in Table 2. Two studies investigated vitamins B1 and B2 (71,72), four investigated vitamin B6 (70,71,73,74) and one investigated vitamin B12 (74). The effects of maternal vitamin B1 intake on breast milk levels showed mixed results(71,72). When the maternal supplementation was 1·7 mg/d for 6 weeks from parturition, there was no significant impact on vitamin B1 breast milk concentration(72), whereas a supplement of 5 mg and then 10 mg over 2 d increased vitamin B1 content of breast milk.
Maternal vitamin B2 and B6 supplementation increased the breast milk vitamin B2 and B6 concentrations, respectively, in the first few postpartum weeks(70–72). Maternal supplementations were 2 mg per d for vitamin B2 and ranged from 4 mg to 20 mg per d for vitamin B6 and lasted between 3 d and 6 weeks. Although, vitamin B6 maternal intake positively impacts breast milk concentration in the first few weeks postpartum, the effects of vitamin B6 supplementation were shown to decrease after 40 d(74).
Vitamin B12 maternal supplementation did not show a significant effect on breast milk content at 1 week postpartum; however, a daily 8 μg intake was shown to prevent its decline in breast milk over lactation(74).
Vitamin C
Three experimental studies were included on vitamin C(74–76), all were rated high risk of bias, as summarised in Table 2. Overall, vitamin C in breast milk was only shown to be responsive to maternal intake following high-dose supplementation, that is, 1000 mg per d for 4 months(76). Supplementation at lower doses, for example, 90 mg/d of vitamin C given to lactating mothers for 6 weeks, showed no difference in breast milk composition(74,75)
Minerals (iodine, iron, copper, zinc and selenium)
Iodine
Four studies(77–80)were identified investigating iodine content, three were experimental(77–79) and one observational(80), as summarised in Table 3. Of the experimental studies, two were rated as low risk of bias(78,79), and one high risk of bias(77), whereas the observational study was rated of good quality(80).
Table 3.
Responsivity of breast milk mineral, amino acid and protein content to maternal diet
| Ref | Participants Risk of Bias |
Study | Ethnicity | Breast milk collection timing | Effects on breast milk content |
|---|---|---|---|---|---|
| Iodine | |||||
| Experimental studies | |||||
| Leung, 2012 | Healthy lactating women over 3 months PP USA RCT High risk of bias |
600 µg oral potassium iodide (456 µg iodine) after overnight fast (n 16). Iodine measured in BM at baseline and hourly for 8 h after intake and dietary iodine recorded | Not provided | Not provided | Following supplementation, there was a significant median increase in BM iodine levels (280·5 μg/l; IQR 71·5–338·0) above baseline (P < 0·01); the median peak iodine was 354 μg/l (IQR 315–495) |
| Mulrine, 2010 | Healthy lactating women after delivery New Zealand RCT Low risk of bias |
Placebo (n 56), 75 µg iodine/d (n 27) or 150 µg iodine per d (n 26) for 24 weeks. BM iodine measured at 1, 4, 8, 12, 16, 20 and 24 weeks | Most likely White Caucasian | All BM samples collected from 09.00 and 12.00 | Iodine decreased by 40 % over 24 weeks in placebo group (P < 0·001) but was 1·3 times higher in 75 µg supplemented group (P = 0·003) and 1·7 times higher in 150 µg supplemented group (P < 0·001) |
| Nazeri, 2016 | Healthy lactating mothers 3–5 d PP Iran RCT Low risk of bias |
Either 150 µg iodine/d (n 42), or no supplementation, but recommendation to used only iodised salt for cooking (control) (n 42). Iodine measured at 0, 7, 10, 14 and 30 d | Persian | Manual expression but no information on timing | At baseline: Median (IQR) 176·0 µg/l (133·7–218·7 µg/l) in supplemented group and 215 µg/l (168·5–315·5 µg/l) in control group, (P = 0·027). d7:191·0 µg/l (105·0–245·0) in supplemented group and 176·0 µg/l (140·0–286·0 µg/l) in control; d10:217·0 µg/l (148·7–339·0 µg/l) in supplemented group and 162·0 µg/l (120·0–206·5 µg/l) in control; d14:242·0 µg/l (156·2–355·7 µg/l) supplemented group and 160·0 µg/l (115·2–199·2 µg/l) in control; d30:210·0 µg/l (100·0–286·0 µg/l) supplemented group and 142·0 µg/l (92·2–197·2 µg/l) in control |
| Observational study | |||||
| Ureta-Velasco | Milk donors Spain Obs Good quality 8 |
BM iodine level from milk donors (n 113) measured and analysed together with five dietary records | Caucasian | Not provided | Iodine positively correlated with total iodine intake (rho = 0·0499, P < 0·001), but not iodine intake from food only (rho = 0·046, P = 0·628). Iodine positively correlated with consumption of > three dairy products per d |
| Se | |||||
| Experimental studies | |||||
| Dodge, 1999 | Healthy lactating women from delivery New Zeeland RCT Some concerns |
50 µg Se per d (n 12), or placebo (n 10) during pregnancy and lactation for 3 months. | Caucasian | First morning milk was collected using a breast pump | Se increased by 37 % (P = 0·003) following supplementation, glutathione activity was unchanged. Supplementation increased PUFA levels by 41 %; (placebo: mean = 9·7, sd = 1·24, v. supplemented: mean = 13·70, sd = 1·02), including LA and ARA, all P ≤ 0·05. SFA levels were correspondingly decreased by 11 % (placebo: mean = 50·1, sd 2·0, v. supplemented: mean = 44·4, sd = 1·6 g/100, P ≤ 0·04). Fatty acid values all expressed as g/100 g fatty acids |
| Dylewski, 2002 | Healthy lactating women 3 months PP USA RCT High risk of bias |
20 µg Se per d for 3 months (n 23). Dietary data and milk at 3 and 6 months | Not provided | Not provided | BM mean (sd) Se dietary intake was 111 (40) µg/d and did not change over the study. Supplementation significantly increased levels by 41 % from 3 (23 (7) ng/ml) to 6 months (32 (14) ng/ml), P ≤ 0·01 |
| Trafikowska, 1996 | Healthy lactating women 3–4 weeks PP Poland RCT High risk of bias |
Subjects (n 16) supplemented with 200 µg/d Se in the form of yeast-rich-Se for 3 months | Not provided | Not provided | After 1 month of Se supplementation, the Se concentration in milk increased significantly (P < 0·001) by 73 % to a plateau of 14–16 ng/ml |
| Trafikowska, 1998 | Healthy lactating women 3–5 weeks PP Poland RCT High risk of bias |
3 groups; group 1 (n 24) supplemented with 200 µg/d Se (yeast-rich Se, group 2 (n 30) supplemented with 200 µg/d selenite mixed with baker’s yeast, group 3 (n 13) supplemented with plain brewer’s yeast without Se. Supplementation lasted 3 months | Not provided | BM collected by manual expression prior to the first morning feeding | Baseline BM (sd) Se 8·9 (2·8) µg/l. In the control group, it remained constant during the 3-month period. Group 1 and 2; BM Se increased significantly reaching a plateau of 14–16 µg/l after 1 month of supplementation. The difference was significantly higher than controls in the yeast-rich Se (P < 0·001) and the selenite-Se-supplemented group (P < 0·01) |
| Observational studies | |||||
| Bianchi, 1999 | Healthy lactating mothers < 210 d PP Brazil Obs Fair quality 6 |
BM from (n 30) mothers, 24-h recall FFQ. BM collected at 7 d and 270 d. BM Se analysed | Nor provided | Not provided | No significant correlation between BM Se and maternal BMI (r2 = −0·0654, P = 0·7351); Se intake (r2 = −0·103, P = 0·594) and stage of lactation (r2 = −0·2981, P = 0·1095) |
| Valent, 2011 | Healthy lactating mothers 3 months PP Italy Obs Good quality 8 |
BM from (n 100) mothers, semi-structured dietary questionnaires. BM Se analysed. | Not provided | Milk collected at any time | BM Se significantly correlated with current fresh fish consumption, r = 0·21, P = 0·04. No significant correlation between intake of multivitamin supplements during pregnancy and Se in BM (mean 10·9 (3·3) ng/g, median 9·6 v. mean 12·3 (2·9) ng/g. median 11·4 for women who did not consume supplement, P = 0·11) |
| Zn/Cu/Fe | |||||
| Choi, 2016 | Healthy women 5–15 d PP Korea Obs Good quality 9 |
n 79 participants completed 3 d dietary record. | Asian | Not provided | Mean (sd) Fe significantly higher in BM from those taking daily Fe supplements (7·36 (9·10) mg/ml, n 64) v. those not (2·83 (6·36) mg/l, n 15), (P = 0·002). No significant difference from those taking daily Zn supplementation (0·36 (0·18) mg/l, n 64) v. those not (0·40 (0·17) mg/l, n 15). No significant difference from those taking daily Cu supplementation (0·69 (0·27) mg/l, n 64) v. those not (0·70 (0·22) mg/l, n 15) |
| Leotsinidis, 2005 | Healthy lactating mothers 3 d PP Greece Obs Fair quality 5 |
BM samples collected (n 180) to measure Cd, Cu, Fe, Pb, Mn and Zn at 3 and 14 d PP, FFQ | Not provided | Morning BM 2 h after previous breast-feeding | Mean (sd) values of colostrum samples: Cd, 0·190 (0·150) µg/l; Cu, 381 (132) µg/l; Fe, 544 (348) µg/l; Pb, 0·48 (0·60) µg/l; Mn, 4·79 (3,23) µg/l; Zn, 4905 (1725) µg/l. All metals with exception of Cu were found in lower concentrations in transitory milk |
| Vuori, 1980 | Healthy lactating mothers 6–8 weeks PP Finland Obs Fair quality 6 |
BM samples collected to measure Fe and Zn at 6–8 weeks PP and 17–22 weeks PP, 7 d FFQ n 15 |
Not provided | BM collected at beginning and end of each breast-feeding | Correlation coefficient (r) between enery intake (Kcal) and BM minerals (mg): Fe, 0·478 (P < 0·01) and Zn, 0·554 (P < 0·01) |
| Fe | |||||
| Experimental studies | |||||
| Yalcin, 2009 | Healthy lactating women 2 weeks PP Turkey RCT Low risk of bias |
Placebo (n 23) or 80 mg/d Fe (n 24) for 16 weeks. BM Fe and Zn at baseline, and Fe at 2 and 16 weeks | Turkish | Collection in morning before feeding infant, 2 h after previous breast-feeding | Fe supplementation to non-anaemic women did not change BM Fe content. BM mean (sd) supplemented Fe concentration was 579 (219) µg/l in week 2 and 372 (163) µg/l in week 16; whereas placebo 512 (178) µg/l week 2, and 385 (207) µg/l, in week 16 |
| Tyrosine | |||||
| Experimental studies | |||||
| Downlati, 2014 | Healthy lactating women from 2 to 24 months PP Canada RCT Some concerns |
Single dose 0, 2, 5 and 10 g oral tyrosine (n 24). Free and total tyrosine measured before and 2, 4 and 6 h after supplementation | Not provided | Not provided | Significant rise only in free tyrosine. 10 g of tyrosine group had significantly higher free tyrosine concentration compared with other groups (P < 0·001). Peak free tyrosine in BM after 10 g dose occurred at 4 h, whereas for the 2 g and 5 g tyrosine doses, maximum free tyrosine levels occurred at 6 h |
| Protein, amino acids, ovalbumin | |||||
| Experimental studies | |||||
| Forsum, 1980 | Healthy lactating women 13–20 weeks PP Sweden RCT Some concerns |
4 d of low protein diet, 1 d wash out and then 4 d of high-protein diet (n 3) | Not provided | Milk collected before and after each nursing by hand expression or manual pump | Mean (sd) protein content in BM (g/d) for low protein diet v. high protein diet: true protein 7·31 (0·74) v. 8·83 (0·44) (P < 0·05); lactoferrin (g/24 h), 2·52 (0·17) v. 3·01 (0·36); α-lactalbumin (g/24 h) 1·50 (0·20) v. 1·75 (0·12); lactose (g/24 h), 58·1 (13·2) v. 63·5 (5·6). Differences in lactoferrin, α-lactalbumin and lactose between the two groups not significant |
| Metcalfe, 2016 | Healthy lactating women first 6 weeks PP Australia RCT High Risk of Bias |
Groups comprised high-egg diet (> 4 eggs per week, n 40), low-egg diet (1–3 egg per week, n 44), and egg-free diet (n 36). BM measured at 2, 4 and 6 weeks. | 85 % Caucasian | BM collected between 2 and 6 h after previous breast-feeding | Mean egg consumption associated with ovalbumin concentration, whereby each additional egg ingested per week led to 25 % increase in ovalbumin levels (95 % CI 5, 48 %, P = 0·01). Ovalbumin significantly higher in high egg group compared with egg-free group. One third of women had no ovalbumin detected |
| Palmer, 2016 | Healthy lactating women 11–14 weeks PP Australia RCT Some concerns |
Groups comprised, no egg, one raw egg, half a cooked egg and one cooked egg (all n 41). BM samples collected every 2 h for 8 h. | Not provided | Not provided | Direct dose–response between amount of cooked egg ingested and peak of ovalbumin in BM (no egg 0·05 ng/ml (95 % CI 0·01, 0·1), half a cooked egg 2·24 ng/ml (95 % CI 0·57, 3·91), one cooked egg 3·16 ng/ml (95 % CI 1·41, 4·91), P < 0·05. No difference between raw and cooked eggs. No ovalbumin detected in BM of 24 % of women |
| Observational studies | |||||
| Rana, 1986 | Healthy lactating women 4–6 weeks PP England Obs Poor quality 2 |
Group 1 followed vegan diet for a year, no medication, no contraceptives (n 14), group 2, control (n 14) omnivore diet. FFQ 7 consecutive d | Not provided | Not provided | Mean taurine concentration in the vegan BM 35 mg/l was significantly lower than in BM of omnivores (55 mg/l) (P < 0·01) |
| Choline | |||||
| Observational studies | |||||
| Perrin, 2020 | Healthy lactating women > 2 weeks PP USA Obs Fair quality 7 |
FFQ to classify as non-vegetarian, vegetarian or vegan (n 74). Single BM sample measured free choline, PC and GPC. | Not provided | Samples collected in morning during first or second breast-feeding of day and last 2 h after previous breast-feeding | Wide range in free choline (4–301 mg/l), with no significant differences between groups. Significantly higher GPC in vegan (mean = 62·7 mg/l, sd = 25·3 mg/l) than vegetarian (mean = 47·7 mg/l, sd = 21·2 mg/l) and non-vegetarian (mean = 42·4 mg/l, sd = 14·2 mg/l), P = 0·005. Significantly lower PC in vegan (mean = 32·5 %, sd = 18·3 %) than vegetarian (M = 46·1 %, sd = 18·3 %) and non-vegetarian (Mean = 44·8 %, sd = 15·7 %), P = 0·01. |
RCT, randomised control trial; PP, postpartum; BM, breast milk, obs, observational study; IQR, interquartile range; GPC; glycerol-phosphocholine; PC, phosphocholine.
Maternal iodine supplementation increased breast milk iodine content and prevented a decline over lactation. Supplementation varied between 75 μg and 150 μg/d or a single 450 μg dose. The observational study found a positive correlation between breast milk iodine content and the consumption of at least three dairy products per d(80).
Selenium
Six publications(81–86) were included on Se, four RCT(82–85) and two observation studies(81,86), as summarised in Table 3. Among the experimental studies, one presented some concerns(82), and three were rated high risk of bias(83–85). The two observational studies were good quality(86) and fair quality(81). Maternal Se supplementation increased breast milk Se concentration. The experimental studies supplements varied from 20 μg/d, 50 μg/d and 200 μg/d for 3 months. One study(82)reported that maternal Se supplementation (50 μg per d) increased breast milk PUFA levels by 41 % (including LA and ARA) and decreased the levels of SFA by 11 %.
Iron, copper and zinc
One experimental study was included for Fe, which was rated low risk of bias(87). Three observational studies were included, which measured Cu, Fe and Zn(88–90). One was rated good quality(88), and two were fair quality(89,90), summarised in Table 3.
Cu, Fe and Zn maternal intake in healthy non-deficient lactating women was not shown to impact breast milk composition in the observational studies. Furthermore, in the experimental study, Fe supplementation at 80 mg/d for 4 months did not increase breast milk Fe levels(87).
Protein, ovalbumin, choline and tyrosine
Protein (amino acids)
Two publications were included(91,92), one experimental study, which was rated as presenting concerns(91), and one observational study(92), which was rated as poor quality. Results are summarised in Table 3. There was no significant difference in the breast milk true protein, lacto-ferrin, α-lacto-albumin and lactose content between lactating women consuming a low or a high protein diet for 4 d(91). However, breast milk from vegans was shown to have a lower taurine concentration than that from omnivores(92)
Ovalbumin
Two experimental studies(93,94) were included, one was rated as some concerns(94) and the other high risk(93), summarised in Table 3. A direct dose response between the number of cooked eggs ingested and the ovalbumin concentration in breast milk was identified.
Choline
One observational study rated fair quality(95) was included for choline, and the results are summarised in Table 3. The study reported differences in breast milk choline forms for vegans, as they had a greater mean concentration and distribution of choline derived from glycerophosphocholine than vegetarian and omnivores. Also, there was a lower mean percentage of choline from phosphocholine in vegan breast milk compared with vegetarian and omnivores.
Tyrosine
One experimental study, rated with some concerns, was included on tyrosine(96). Results are summarised in Table 3. The study reported that lactating women supplemented with tyrosine had a higher breast milk total tyrosine concentration. The supplementation was a single dose of 10 g of tyrosine.
Contaminants
Five observational studies were included(89,97–100). One on Hg, which was rated good quality(100), one on Hg and Pb, which was rated good quality(99),one on As, B and Li, rated as fair quality(97), one on Pb and Cd, rated as fair quality(89), and one on PCB, rated as poor quality(98). The results are summarised in Table 4.
Heavy metals (arsenic, boron, cadmium, lead, lithium and mercury)
Maternal intake of freshwater fish was shown to be negatively associated with breast milk Hg levels, whereas maternal consumption of cereals was associated with higher breast milk Hg levels(100).
One study identified a significant association between fish consumption and breast milk Pb levels(99). The other studies show that environment can have a bigger impact on the presence of contaminants in breast milk than dietary habits(89,97).
Polychlorinated biphenyls
The reviewed study reported Inuit breast milk samples (300 g/d seafood intake) had a content in total 2,3,7-tetrachlorodibenzo-p-dioxinequivalents (TEQ) for PCB 3·5 times higher than Caucasian breast milk samples (12 g/d seafood intake)(98).
Overall summary
Table 5 provides an overall summary of the results of this systematic review and provides ratings of the overall quality of the evidence by the authors using the GRADE system for each nutrient and contaminant(18). The table also summarises the doses of supplementation provided in the experimental studies, and where relevant European Food Safety Authority recommended intake levels are provided for comparison, as well as toxicity information on contaminant levels(101).
Table 5.
Synthesis of the nutrients in breast milk responsive to maternal diet
| Nutrients | Number of articles | Relevance | Quality of evidence | Observations |
|---|---|---|---|---|
| PUFA/SFA | ||||
| DHA | 29 (15 exp, 14 obs) | Essential for optimal brain and visual system development | High quality | DHA levels in BM proportional to maternal dietary DHA intake Maternal diet quality affects the fatty acid composition of breast milk. Lower DHA and long-chain fatty acids proportion in vegan BM For RCT, supplementation ranged from 200 mg to 1200 mg/d EFSA adequate DHA intake: 100–200 mg/d |
| EPA | Important for cardiovascular function and precursor of bioactive mediators with anti-inflammatory and pro-resolving properties | High quality | EPA levels in BM less proportional to maternal dietary EPA intake Effect of maternal EPA supplementation on BM concentration is more modest than DHA For RCT, supplementation ranged from 70 mg to 300 mg/d EFSA adequate EPA intake: 100–200 mg/d |
|
| ALA | Precursor of longer-chain n-3 PUFA and may have independent roles | Low quality | BM ALA content correlated with intake of rapeseed and soyabean oils; seeds and nuts such as flaxseed, chia and walnuts and some green leafy vegetables (kale and spinach) For RCT, supplementation was 10·1 g/d EFSA adequate intake: 0·5 % Energy intake of ALA |
|
| ARA | Essential for brain development and immune system function | Low quality | No effect observed in studies, but very low doses provided Same proportion of ARA in omnivores and vegans’ BM For RCT, supplementation was 54 mg/d EFSA adequate intake: Not available |
|
| SFA/TFA | High quality | Total trans acids (TFA) in the milk appeared to follow dietary trans changes after a 12–36 h lag period. No association between TFA consumption and BM TFA level Overweight women’s BM compared with normal-weight women’s BM contained higher amount of SFA, lower ratio of unsaturated to saturated FA than those of normal weight EFSA adequate intake: not applicable |
||
| Vitamins | ||||
| A | 8 exp | Optimum visual, growth, immune system and cognitive development | High quality | Vitamin A level in BM is responsive to maternal intake Higher deficiency risks in developing countries For RCT, supplementation was either 30 mg/d, 54 mg/d or 60 mg single dose EFSA average requirement: 1020 µg RE/d |
| B1, B2 and B9 | 6 (5 exp, 1 obs) | B1 deficiency can cause gastrointestinal symptoms, cardiac failure, and lactic. B2 deficiency can cause anaemia and cataracts can develop if riboflavin deficiency is severe and prolonged B5 deficiency may include symptoms such as fatigue, insomnia, depression, irritability and vomiting B9 plays an essential role in the development of a baby’s brain and spinal cord during pregnancy. |
Very low quality | Thiamine supplementation did not significantly affect the thiamine concentration in BM Riboflavin supplementations seem to have a positive impact on BM riboflavin concentration No evidence found on folic acid and pantothenic acid For RCT, vitamin B1 supplementation was 1·7 mg/d For RCTs, vitamin B2 supplementation was 2 mg/d EFSA average requirement vitamin B1:0·072 mg/MJ Thiamin requirement is related to energy requirement and therefore expressed in mg/MJ. Values expressed in mg/d can be calculated based on the energy requirement of the group considered (EFSA NDA Panel, 2013) EFSA adequate requirement vitamin B2:1·7 mg/d EFSA adequate intake vitamin B5:7 mg/d EFSA adequate requirement vitamin B9:380 µg DFE/d |
| B6 | Essential for brain development | Moderate quality | Vitamin B6 supplementation seems to impact vitamin B6 breast milk concentration positively For RCT, Vitamin B6 supplementation ranged from 2·5 to 20 mg/d EFSA average requirement: 1·4 mg/d |
|
| B12 | Essential for brain development | Moderate quality | Maternal vitamin B12 supplementation may prevent declines in BM content For RCT, Vitamin B12 supplementation was 8 µg/d EFSA adequate intake: 5 µg/d |
|
| C | 3 exp | Essential for collagen formation, and role in immune system and nervous system function | Moderate quality | BM vitamin C levels responsive to maternal supplementation only when lactating mothers have low intake. Overall, vitamin C levels appear responsive to intake, but levels are regulated, as response to a highest dose of vitamin C was modest in European women in contrast with the 3-fold increase in African women. For RCT, Vitamin C supplementation ranged from 90 mg/d to 1000 mg/d EFSA average requirement: 140 mg/d |
| D | 5 exp | Essential for Ca absorption and skeletal growth, deficiency can cause nutritional rickets | Moderate quality | BM vitamin D levels responsive to maternal supplementation. Higher effect when high unique dose supplementation (150 000 μg) For RCT, vitamin D supplementation ranged from 50 µg/d to 3750 µg single dose EFSA adequate intake: 15 µg/d |
| E | 6 (5 exp, 1 obs) | Deficiency can compromise immune system and affect lung development. Premature infants are more susceptible to deficiency and can cause thrombocytosis, haemolytic anaemia and interventricular haemorrhage | High quality | Dose–response relationship, and supplementation effects are confirmed for α-tocopherol Milk total tocopherol found to be associated only with mother’s total fat and saturated fat dietary intake An increase in PUFA content may increase peroxidation and therefore increase vitamin E requirements. For RCT, Vitamin E supplementation ranged from 40 mg to 536 mg single dose EFSA adequate intake: 11 mg/d |
| K1 | 3 exp | Deficiency can lead to classical haemorrhagic disease of newborn with bleeding in the first week of life |
Low quality | Dose–response relationship, and supplementation effects are confirmed For RCT, vitamin K supplementation ranged from 0·5 mg/d to 5 mg/d EFSA adequate intake: 70 µg/d |
| Minerals and others | ||||
| Iodine | 4 (1 exp, 3 obs) | Deficiency can damage the developing brain and increase mortality | High quality | Dose–response relationship, and supplementation effects are confirmed Supplementation effects are immediate (peak 6 h after supplementation) For RCTs, iodine supplementation ranged from 75 µg/d to 150 µg/d. One study administrated 450 µg as a single dose EFSA adequate intake: 200 µg/d |
| Se | 6 (4 exp, 2 obs) | Deficiency associated with increased respiratory morbidity | Low quality | BM Se significantly correlated to current fresh fish consumption, no significant correlation between intake of multivitamin supplements during pregnancy and Se in BM Se maternal supplementation seems to increase Se levels in BM and prevent decline with advancing lactation and also appeared to increase the BM concentration of PUFA (especially LA) and decrease BM SFA. For RCT, Se supplementation ranged from 20 µg/d to 200 µg/d EFSA adequate intake: 85 µg/d |
| Fe | 4 (1 exp, 3 obs,) | Fe deficiency anaemia is associated with long-lasting neurofunctional effects and can affect sleep pattern | Low quality | Fe supplementation to non-anaemic women did not change BM Fe content or prevent a decline. For RCT, Fe supplementation was from 80 mg/d EFSA average requirement: 7 mg/d |
| Zn and Cu | 3 obs | Zn deficiency can lead to cutaneous signs, diarrhoea and alopecia. Cu deficiency can cause bone lesions |
Low quality | Dietary intake of Zn, Cu and Fe did not affect BM Zn, Cu and Fe concentrations. All metals with exception of Cu were found in lower concentrations in transitory milk. EFSA adequate intake Cu: 1·5 mg/d EFSA average requirement: Zn: 2·4 mg/d |
| Ovalbumin | 2 exp | Exposure to ovalbumin may reduce egg allergy development | Moderate quality | Direct dose–response between the amount of cooked egg ingested and the BM ovalbumin For RCT, egg intake ranged from no egg to > 4 eggs/week EFSA adequate intake: Not available |
| Protein and amino acids | 2 (1 exp, 1 obs) | Maternal protein consumption may impact the BM nitrogen content. BM nitrogen is used by beneficial bacteria present in the infant’s digestive system. Taurine has an important role in intestinal fat absorption, hepatic function, and auditory and visual development in preterm and low birth weight infant |
Low quality | Output of lactoferrin, α-lactalbumin and serum albumin seem to be higher when a high protein diet is consumed; however, differences are not significant compared with low protein diet consumption. Mean taurine concentration in the vegan BM 35 mg/dl was significantly lower than in BM of omnivores. EFSA average requirement: Zn: 15 mg/d from 0 to 6 months PP and 10 g/d after 6 months PP |
| Tyrosine | 1 exp | Tyrosine deficiency may increase risk postpartum depression | Low quality | Rise in free, but not total tyrosine, supplementation effects immediate (peak 6 h after supplementation) For RCT, tyrosine supplementation ranged from 2 to 10 g single dose EFSA adequate intake/average requirement: not available |
| Choline | 1 obs | Needed for growth and development, and role in membrane and signalling functions | Low quality | No significant effects by maternal diet pattern. EFSA adequate intake: 520 mg/d |
| Contaminants | ||||
| As, Cd, Pb, Hg | 4 obs | Heavy metals disrupt cellular events including growth can induce cancer | Moderate quality | Factors significantly related to metal levels in BM were area of residence (Hg, Pb), prematurity (Hg), fish consumption (Pb) and cereals (Hg), vitamin supplementation (Hg) and smoking (Pb, Cu). BM Pb positively associated with Fe and Zn but inversely associated with Ca. As in BM associated with Fe and B with Ca. No significant differences were found in BM between fish and non-fish eaters for THg concentrations. Negative association was found between THg concentrations in BM and freshwater fish consumption PTWI (JEFCA): no appropriate safety guidelines for As and Pb; Cd PTWI, 2·5 µg/kg bw/week; Inorganic Hg (IHg), 4 µg/kg bw/weeks. Total Hg (MeHg), 1·6 µg/kg bw/week |
| PCB | 1 obs | PCB can induce skin and liver damage | Moderate quality | Levels were three times higher for very high seafood consumers (300 g/d in average) than for low seafood consumers (12 g/d in average) EFSA tolerable intake: 2 picograms per kg bw |
Based on GRADE rating system.
Obs, observational study; exp, experimental study (randomised control trial); ALA, α-linolenic acid; ARA, arachidonic acid; BM, breast milk, FA, fatty acid; PP, postpartum; DFE, dietary folate equivalent; EFSA, European Food Safety Authority; THg, total Hg; PCB, polychlorinated biphenyls; PTWI, provisional tolerable monthly intake; bw, body weight; JEFCA, joint FAO/WHO Expert Committee on Food Additives; RE, retinol equivalent.
Discussion
This study systematically reviewed the literature investigating the relationship between maternal intake and the levels of macronutrients, micronutrients and contaminants (heavy metals and PCB) in breast milk, for women without nutrient deficiencies. Due to the high heterogeneity between studies, it was not possible to undertake a meta-analysis, and so the results have been summarised with a narrative synthesis. The main findings were that there was strong evidence of response to maternal intakes of DHA, EPA, vitamins A, E and K, iodine and Se in breast milk composition, some evidence of response for ALA, B vitamins, vitamin C and D, ovalbumin, tyrosine and some contaminants, and insufficient evidence to determine the effects of ARA, Cu, Fe, Zn and choline. However, it should be noted that only a high dose of vitamin C was shown to produce an increase in breast milk vitamin C content, and although ARA intake was not found to affect breast milk ARA content, the supplemental dose used in this study was too low to allow definitive conclusions. Although maternal intake of Fe, Cu, Zn and total choline levels was not shown to affect their levels in breast milk, these findings are based on a limited number of studies, and so there remains uncertainty for these nutrients.
Maternal intake of DHA, EPA, ALA, B vitamins, and vitamins A, E, and K, iodine, Se, ovalbumin, and tyrosine was shown to affect their breast milk levels; however, the strength of evidence and quality of studies underpinning this evidence were highly variable. The relationship between DHA and EPA intake and breast milk levels has been extensively investigated, and the results across the experimental and observational studies show clear and consistent results that maternal intake influences their levels in breast milk(19,20,22–25,29–33,35,36,38,40,43–47). With vitamin A, there was a much greater heterogeneity in experimental study design, particularly around the type of intervention and the dose and duration of supplementation; however, of the nine RCT, eight identified a positive relationship between intake and breast milk levels(48–52,54,55). There have been fewer studies with B vitamins, and these are highly heterogeneous in study design, but overall, the results support the importance of maternal intake in influencing their levels in breast milk. Since the completion of this review, a relevant study has been published exploring the relationship between diet and nutritional status and the nutritional composition of donor milk(102). Their results are consistent with our findings of a dose–response relationship between DHA intake and milk DHA content, and associations between maternal intake and milk levels of vitamins B1, B2, B6, C, and D. However, further high-quality studies are still needed, particularly for B12, to explore the effects of dose and also interactions between B vitamins(70–74).
Studies of the effects of vitamin D intake are potentially confounded by seasonal effects, as breast milk concentrations of vitamin D and 25-hydroxyvitamin D have been shown to have significant seasonal variations(103). Five experimental studies were identified that investigated the effects of maternal vitamin D supplementation on breast milk levels(56–60). Overall, the strongest effects were identified with the higher doses of supplementation, and importantly supplementation was shown to alleviate seasonal declines. It may therefore be advisable to recommend vitamin D supplementation in circumstances where endogenous synthesis is limited.
In all five experimental studies, maternal vitamin E supplementation increased breast milk α-tocopherol levels; however, two studies directly compared natural (RRR α-tocopherol) and synthetic (all-racemic α-tocopherol) sources(61,63). Synthetic α-tocopherol is an equimolar mix of its eight stereoisomers, as the three chiral carbons of α-tocopherol can be in either an R or an S orientation, whereas in nature only one of these isomers (RRR) is found(104). Clemente and co-workers found that supplementation with both forms increased vitamin E concentrations in breast milk (colostrum); however, the RRR form was more efficient in increasing the levels(61). Gaur and co-workers reported that supplementation with RRR increased the percentage of RRR α-tocopherol isomers in breast milk, whereas supplementation with all-racemic α-tocopherol decreased the percentage of RRR stereoisomers and increased the non-RRR-α-tocopherol stereoisomers, such as 2S-α-tocopherol(63). Since the relative effects and potencies of these different forms of α-tocopherol on health outcomes are not well understood(104), it may be prudent at this time to recommend the RRR form of α-tocopherol, where supplementation is advised.
Three experimental studies were identified for vitamin K, and although a wide range of supplementation protocols were employed, a consistent dose–response relationship was identified between maternal vitamin K intake and breast milk levels(67–69). Three experimental and one observational studies were identified that explored the relationship between maternal intake of iodine and breast milk levels, and a consistent relationship was identified across all studies(77–80). With Se four experimental studies were identified, and they all showed that maternal supplementation increases breast milk levels(82–84); however, the observational studies were discordant, with one identifying a significant association between fish intake and breast milk Se levels(86), whereas the other did not identify any significant associations(81).
No clear relationship between nutrient intake and breast milk levels was identified for Cu, Fe and Zn; however, this is based on a limited number of studies(87–90). The only experimental study reported that Fe supplementation of non-anaemic women did not increase breast milk Fe levels(87), whereas although one observational study found that breast milk Fe concentration was significantly higher from those reporting taking daily Fe supplements(88), the other did not identify an association between Cu, Fe and Zn intake and breast milk levels(89). Albeit with this paucity of evidence, these results are consistent with previous observations that breast milk Cu, Fe and Zn concentrations are not associated with maternal mineral status(105).
Overall, the observations from the present review are consistent with the results of previous systematic reviews in this area(6–9), with the exception of vitamin C, where we did not identify a clear relationship between maternal intake and breast milk levels. This dissonance between may be based on differences in the study selection criteria between systematic reviews, as the present review only included studies on non-deficient populations. In the present review, three experimental studies were identified for vitamin C(74–76). All three studies were based on small numbers of participants, with a range of different supplemental dosing regimens administered. A relationship between maternal intake and breast milk content was only identified in one trail, which provided vitamin C at high doses, that is, 1000 mg per d(76). It may therefore be hypothesised that in non-deficient populations, breast milk vitamin C levels are only responsive to higher levels of maternal supplementation; however, this needs further investigation.
It is important to highlight that in most of the reviewed experimental publications, the nutrient doses were higher than the EFSA adequate intake or average requirements(101). For instance, in all nine reviewed experimental studies, DHA and EPA supplementation was shown to increase breast milk DHA and EPA levels, and this was in a dose-dependent manner(19,20,22–25,29,31,33). The highest dose of DHA provided was 1·2 g for 14 d. The levels of supplementation provided were also higher than EFSA recommendations for vitamins A, B6, B12, E and K(101).
With regard to specific restrictive diets, breast milk from vegan mothers contained low DHA levels(44), and in one study this was significantly lower than breast milk from vegetarian and omnivore mothers(46). The choline composition profile was also reported to be lower in breast milk from vegan mothers(95), and taurine was also found to be lower in breast milk from vegan mothers(92). Although the present review did not identify any studies that compared vitamin B12 content between mothers following vegan, vegetarian and non-vegetarian diets, vitamin B12 content was shown responsive to maternal intake. Therefore, our results support the previous recommendations in the systematic review by Karzc and Krόlak-Olejnik, that mothers following a vegan diet should consider supplementation with preformed DHA and vitamin B12, as maternal levels of intake of these nutrients may be low(8). Furthermore, as vegan and vegetarian diets become more popular, there is an urgent need to conduct further high-quality studies in this area, so lactating mothers and milk bank donors can be provided with specific nutritional recommendations.
With regard to the effects of intake of contaminants such as heavy metals and PCB, and breast milk levels, all studies reviewed were observational in nature, and it should be noted that any observed effects may therefore be confounded by environmental factors in addition to dietary intake(89,97). However, two studies reported a negative relationship between freshwater fish consumption and breast milk Hg content, and a positive relationship was found with cereals and vitamin supplements consumption(99,100). A positive relationship was reported between maternal fish consumption (especially large fish species) and PCB content in breast milk, although the fish intake was extremely high (300 g/d)(98). Overall, the number of studies published in this area is limited, with very few publications focusing on dietary sources; however, the overall presence of contaminants in breast milk appears below toxicity levels. Furthermore, based on these observations, fish intake was not identified as a potential source of elevated Hg in breast milk.
A strength of this systematic review is the extensive scope of nutrients and contaminants that have been considered, and recommendations in some areas are possible. Furthermore, our results have identified areas where there is a lack of high-quality evidence, particularly around the effects of ARA, Cu, Fe and Zn supplementation on breast milk content. The relationship between contaminant intake and breast milk levels also requires more comprehensive analysis, to delineate the effects of dietary intake from wider environmental exposures. A further strength is that this review considered studies undertaken in populations from a wide variety of countries and ethnicities, where healthy non-micronutrient-deficient lactating women were considered. Publications from developing countries were not included, unless it was clearly specified that the participants did not have a nutrient deficiency. However, as many publications on B vitamins were excluded during the selection process, as they were reporting on either deficient or low-income populations, we could not include any studies on vitamin B5 or folic acid.
Breast milk is a highly dynamic fluid, and the nutritional content has been shown to be affected by physiological factors in addition to nutritional intake, such as stage of lactation(106) and circadian rhythm(107). Due to the variability in study reporting and high degree of design heterogeneity, it was not possible to draw specific conclusions about the effects of these factors in our analysis. Furthermore, other uncontrolled covariates that have been shown to influence the target compounds in breast milk and that were not analysed in the review, such as environment, obesity or genotype. For example, biosynthesis of DHA is influenced by genotype, as variations in SNP, particularly the fatty acid desaturase (FADS) gene cluster, affect PUFA levels. SNP within this cluster impact on expression of FAD genes across a wide range of tissues are associated with variations of n-6 and n-3 PUFA levels, such that those with the minor FADS allele have higher levels of LA and lower levels of ARA and DHA in serum phospholipids, plasma phospholipids and breast milk compared with carriers of the major allele(108–110). Importantly, it has been shown that only women with the major allele appear to increase breast milk DHA by consuming fish or fish oil(110).
It should also be highlighted that the observational studies employed a wide variety of tools to assess dietary intake, and these have varying levels of precision, and there was also very little information across the publications as to how the supplements were ingested, and therefore absorbed, as it has been demonstrated that lipid-soluble nutrients are better absorbed when ingested with a fat meal(111). These aspects should be considered in the design of future studies and also when providing nutritional advice to lactating mothers and breast milk donors. Our review limited the contaminants list to heavy metals and PCB; however, other ingredients should be further investigated. This is the case of non-nutritive sweeteners that were recently found in breast milk from lactating women in the USA(112).
In conclusion, the present systematic review assessed the available literature on quantitative associations between maternal diet and breast milk composition. Maternal intake, particularly DHA, EPA, ALA, and vitamins A, D, E, B6, B12 and K, ovalbumin and tyrosine were found to be responsive to maternal diet, whereas there is insufficient evidence to ascertain the effects of intake on breast milk ARA, vitamin C, Fe, Zn, Cu and choline. Although these results provide information that can be used to help inform nutritional guidelines for lactating mothers and breast milk donors, further high-quality research is needed to inform nutrient intake recommendations. At present, the recommendation for lactating women and milk donors should adopt a healthy and diversified diet, such as the Mediterranean diet, and consider supplementation with nutrients such as DHA and vitamins B12 and D when their diets are restricted or limited by external factors.
Supporting information
Falize et al. supplementary material
Acknowledgements
No funding was received for this work.
S. C. D. formulated the research question, C. F., Y. M. J. and S. C. D. designed the study protocol, C. F. and M. S. carried out data collection and quality assessment, and C. F. carried out interpretation of results and lead on the formulation the manuscript. C. F., Y. M. J. and S. C. D. critically reviewed the manuscript content, S. C. D. had primary responsibility for the final content of the manuscript, and all authors read and approved the final manuscript.
There are no conflicts of interest.
This research does not include studies on human subjects, human data or tissue, or animals.
All data are available upon request from the corresponding author.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114523002775
References
- 1. De Rooy L, Hamdallah H & Dyall SC (2017) Extremely preterm infants receiving standard care receive very low levels of arachidonic and docosahexaenoic acids. Clin Nutr 36, 1593–1600. [DOI] [PubMed] [Google Scholar]
- 2. Weaver G, Bertino E, Gebauer C, et al. (2019) Recommendations for the establishment and operation of human milk banks in Europe: a consensus statement from the European Milk Bank Association (EMBA). Front Pediatr 7, 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brenna JT, Varamini B, Jensen RG, et al. (2007) Docosahexaenoic and arachidonic acid concentrations in human breast milk worldwide. Am J Clin Nutr 85, 1457–1464. [DOI] [PubMed] [Google Scholar]
- 4. Emmett PM & Rogers IS (1997) Properties of human milk and their relationship with maternal nutrition. Early Hum Dev 49, S7–28. [DOI] [PubMed] [Google Scholar]
- 5. Floris LM, Stahl B, Abrahamse-Berkeveld M, et al. (2020) Human milk fatty acid profile across lactational stages after term and preterm delivery: a pooled data analysis. Prostaglandins Leukot Essent Fatty Acids 156, 102023. [DOI] [PubMed] [Google Scholar]
- 6. Bravi F, Wiens F, Decarli A, et al. (2016) Impact of maternal nutrition on breast-milk composition: a systematic review. Am J Clin Nutr 104, 646–662. [DOI] [PubMed] [Google Scholar]
- 7. Keikha M, Bahreynian M, Saleki M, et al. (2017) Macro- and micronutrients of human milk composition: are they related to maternal diet? A comprehensive systematic review. Breastfeed Med 12, 517–527. [DOI] [PubMed] [Google Scholar]
- 8. Karcz K & Krolak-Olejnik B (2021) Vegan or vegetarian diet and breast milk composition – a systematic review. Crit Rev Food Sci Nutr 61, 1081–1098. [DOI] [PubMed] [Google Scholar]
- 9. Keikha M, Shayan-Moghadam R, Bahreynian M, et al. (2021) Nutritional supplements and mother’s milk composition: a systematic review of interventional studies. Int Breastfeeding J 16, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dyall SC (2015) Long-chain n-3 fatty acids and the brain: a review of the independent and shared effects of EPA, DPA and DHA. Front Aging Neurosci 7, 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grandjean P, Jørgensen PJ & Weihe P (1994) Human milk as a source of methylmercury exposure in infants. Environ Health Perspect 102, 74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Page MJ, Moher D, Bossuyt PM, et al. (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372, n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cochrane M, Watson PM, Timpson H, et al. (2019) Systematic review of the methods used in economic evaluations of targeted physical activity and sedentary behaviour interventions. Soc Sci Med 232, 156–167. [DOI] [PubMed] [Google Scholar]
- 14. Ouzzani M, Hammady H, Fedorowicz Z, et al. (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5, 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cumpston M, Li T, Page MJ, et al. (2019) Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 10, ED000142. [DOI] [PMC free article] [PubMed]
- 16. Sterne JAC, Savovic J, Page MJ, et al. (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898. [DOI] [PubMed] [Google Scholar]
- 17. Lo CK, Mertz D & Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guyatt GH, Oxman AD, Vist GE, et al. (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Argaw A, Bouckaert KP, Wondafrash M, et al. (2021) Effect of fish-oil supplementation on breastmilk long-chain polyunsaturated fatty acid concentration: a randomized controlled trial in rural Ethiopia. Eur J Clin Nutr 75, 809–816. [DOI] [PubMed] [Google Scholar]
- 20. Boris J, Jensen B, Salvig JD, et al. (2004) A randomized controlled trial of the effect of fish oil supplementation in late pregnancy and early lactation on the n-3 fatty acid content in human breast milk. Lipids 39, 1191–1196. [DOI] [PubMed] [Google Scholar]
- 21. Craig-Schmidt MC, Weete JD, Faircloth SA, et al. (1984) The effect of hydrogenated fat in the diet of nursing mothers on lipid composition and prostaglandin content of human milk. Am J Clin Nutr 39, 778–786. [DOI] [PubMed] [Google Scholar]
- 22. Fougere H, Bilodeau JF, Lavoie PM, et al. (2021) Docosahexaenoic acid-rich algae oil supplementation on breast milk fatty acid profile of mothers who delivered prematurely: a randomized clinical trial. Sci Rep 11, 21492. [DOI] [PMC free article] [PubMed]
- 23. Hawkes JS, Bryan DL, Makrides M, et al. (2002) A randomized trial of supplementation with docosahexaenoic acid-rich tuna oil and its effects on the human milk cytokines interleukin 1 beta, interleukin 6, and tumor necrosis factor alpha. Am J Clin Nutr 75, 754–760. [DOI] [PubMed] [Google Scholar]
- 24. Lauritzen L, Jorgensen MH, Hansen HS, et al. (2002) Fluctuations in human milk long-chain PUFA levels in relation to dietary fish intake. Lipids 37, 237–244. [DOI] [PubMed] [Google Scholar]
- 25. Mazurier E, Rigourd V, Perez P, et al. (2017) Effects of maternal supplementation with n-3 precursors on human milk composition. J Hum Lact 33, 319–328. [DOI] [PubMed] [Google Scholar]
- 26. Mellies MJ, Ishikawa TT, Gartside PS, et al. (1979) Effects of varying maternal dietary fatty acids in lactating women and their infants. Am J Clin Nutr 32, 299–303. [DOI] [PubMed] [Google Scholar]
- 27. Nasser R, Stephen AM, Goh YK, et al. (2010) The effect of a controlled manipulation of maternal dietary fat intake on medium and long chain fatty acids in human breast milk in Saskatoon, Canada. Int Breastfeed J 5, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Park Y, McGuire MK, Behr R, et al. (1999) High-fat dairy product consumption increases delta 9c,11t-18:2 (rumenic acid) and total lipid concentrations of human milk. Lipids 34, 543–549. [DOI] [PubMed] [Google Scholar]
- 29. Smithers LG, Markrides M & Gibson RA (2010) Human milk fatty acids from lactating mothers of preterm infants: a study revealing wide intra- and inter-individual variation. Prostaglandins, Leukotrienes Essent Fatty Acids 83, 9–13. [DOI] [PubMed] [Google Scholar]
- 30. Storck Lindholm E, Strandvik B, Altman D, et al. (2013) Different fatty acid pattern in breast milk of obese compared to normal-weight mothers. Prostaglandins, Leukotrienes Essent Fatty Acids 88, 211–217. [DOI] [PubMed] [Google Scholar]
- 31. Valentine CJ, Morrow G, Pennell M, et al. (2013) Randomized controlled trial of docosahexaenoic acid supplementation in midwestern U.S. human milk donors. Breastfeed Med 8, 86–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Valenzuela R, Bascuñán K, Chamorro R, et al. (2015) Modification of docosahexaenoic acid composition of milk from nursing women who received alpha linolenic acid from chia oil during gestation and nursing. Nutrients 7, 6405–6424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yang Y, Li G, Li F, et al. (2022) Impact of DHA from algal oil on the breast milk DHA levels of lactating women: a randomized controlled trial in China. Nutrients 14, 3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Aitchison JM, Dunkley WL, Canolty NL, et al. (1977) Influence of diet on trans fatty acids in human milk. Am J Clin Nutr 30, 2006–2015. [DOI] [PubMed] [Google Scholar]
- 35. Antonakou A, Skenderi KP, Chiou A, et al. (2013) Breast milk fat concentration and fatty acid pattern during the first six months in exclusively breastfeeding Greek women. Eur J Nutr 52, 963–973. [DOI] [PubMed] [Google Scholar]
- 36. Bzikowska-Jura A, Czerwonogrodzka-Senczyna A, Jasińska-Melon E, et al. (2019) The concentration of n-3 fatty acids in human milk is related to their habitual but not current intake. Nutrients 11, 1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Daud AZ, Mohd-Esa N, Azlan A, et al. (2013) The trans fatty acid content in human milk and its association with maternal diet among lactating mothers in Malaysia. Asia Pac J Clin Nutr 22, 431–442. [DOI] [PubMed] [Google Scholar]
- 38. de la Presa-Owens S, Lopez-Sabater MC & Rivero-Urgell M (1996) Fatty acid composition of human milk in Spain. J Pediatr Gastroenterol Nutr 22, 180–185. [DOI] [PubMed] [Google Scholar]
- 39. Freitas RF, Macedo MD, Lessa AD, et al. (2021) Relationship between the diet quality index in nursing mothers and the fatty acid profile of mature breast milk. Rev Paul Pediatr 39, e2019089-e. [DOI] [PMC free article] [PubMed]
- 40. Juber BA, Jackson KH, Johnson KB, et al. (2016) Breast milk DHA levels may increase after informing women: a community-based cohort study from South Dakota USA. Int Breastfeed J 12, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu G, Ding Z, Li X, et al. (2016) Relationship between polyunsaturated fatty acid levels in maternal diets and human milk in the first month post-partum. J Hum Nutr Diet 29, 405–410. [DOI] [PubMed] [Google Scholar]
- 42. Makela J, Linderborg K, Niinikoski H, et al. (2013) Breast milk fatty acid composition differs between overweight and normal weight women: the STEPS Study. Eur J Nutr 52, 727–735. [DOI] [PubMed] [Google Scholar]
- 43. Olafsdottir AS, Thorsdottir I, Wagner KH, et al. (2006) Polyunsaturated fatty acids in the diet and breast milk of lactating icelandic women with traditional fish and cod liver oil consumption. Ann Nutr Metab 50, 270–276. [DOI] [PubMed] [Google Scholar]
- 44. Perrin MT, Pawlak R, Dean LL, et al. (2019) A cross-sectional study of fatty acids and brain-derived neurotrophic factor (BDNF) in human milk from lactating women following vegan, vegetarian, and omnivore diets. Eur J Nutr 58, 2401–2410. [DOI] [PubMed] [Google Scholar]
- 45. Sanders TA, Ellis FR & Dickerson JW (1978) Studies of vegans: the fatty acid composition of plasma choline phosphoglycerides, erythrocytes, adipose tissue, and breast milk, and some indicators of susceptibility to ischemic heart disease in vegans and omnivore controls. Am J Clin Nutr 31, 805–813. [DOI] [PubMed] [Google Scholar]
- 46. Sanders TA & Reddy S (1992) The influence of a vegetarian diet on the fatty acid composition of human milk and the essential fatty acid status of the infant. J Pediatr 120, S71–7. [DOI] [PubMed] [Google Scholar]
- 47. Scopesi F, Ciangherotti S, Lantieri PB, et al. (2001) Maternal dietary PUFAs intake and human milk content relationships during the first month of lactation. Clin Nutr 20, 393–397. [DOI] [PubMed] [Google Scholar]
- 48. Bahl R, Bhandari N, Wahed MA, et al. (2002) Vitamin A supplementation of women postpartum and of their infants at immunization alters breast milk retinol and infant vitamin A status. J Nutr 132, 3243–3248. [DOI] [PubMed] [Google Scholar]
- 49. Basu S, Sengupta B & Paladhi PK (2003) Single megadose vitamin A supplementation of Indian mothers and morbidity in breastfed young infants. Postgrad Med J 79, 397–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Canfield LM, Giuliano AR, Neilson EM, et al. (1998) Kinetics of the response of milk and serum beta-carotene to daily beta-carotene supplementation in healthy, lactating women. Am J Clin Nutr 67, 276–283. [DOI] [PubMed] [Google Scholar]
- 51. Canfield LM, Kaminsky RG, Taren DL, et al. (2001) Red palm oil in the maternal diet increases provitamin A carotenoids in breastmilk and serum of the mother-infant dyad. Eur J Nutr 40, 30–38. [DOI] [PubMed] [Google Scholar]
- 52. Ding Y, Hu P, Yang Y, et al. (2021) Impact of maternal daily oral low-dose vitamin A supplementation on the mother-infant pair: a randomised placebo-controlled trial in China. Nutrients 13, 2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gossage CP, Deyhim M, Yamini S, et al. (2002) Carotenoid composition of human milk during the first month postpartum and the response to beta-carotene supplementation. Am J Clin Nutr 76, 193–197. [DOI] [PubMed] [Google Scholar]
- 54. Grilo EC, Medeiros WF, Silva AGA, et al. (2016) Maternal supplementation with a megadose of vitamin A reduces colostrum level of α-tocopherol: a randomised controlled trial. J Hum Nutr Diet 29, 652–661. [DOI] [PubMed] [Google Scholar]
- 55. Johnson EJ, Qin J, Krinsky NI, et al. (1997) Beta-carotene isomers in human serum, breast milk and buccal mucosa cells after continuous oral doses of all-trans and 9-cis beta-carotene. J Nutr 127, 1993–1999. [DOI] [PubMed] [Google Scholar]
- 56. Ala-Houhala M, Koskinen T, Parviainen MT, et al. (1988) 25-Hydroxyvitamin D and vitamin D in human milk: effects of supplementation and season. Am J Clin Nutr 48, 1057–1060. [DOI] [PubMed] [Google Scholar]
- 57. Basile LA, Taylor SN, Wagner CL, et al. (2006) The effect of high-dose vitamin D supplementation on serum vitamin D levels and milk calcium concentration in lactating women and their infants. Breastfeed Med 1, 27–35. [DOI] [PubMed] [Google Scholar]
- 58. Ketha H, Thacher TD, Oberhelman SS, et al. (2018) Comparison of the effect of daily v. bolus dose maternal vitamin D(3) supplementation on the 24,25-dihydroxyvitamin D(3) to 25-hydroxyvitamin D(3) ratio. Bone 110, 321–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Niramitmahapanya S, Kaoiean S, Sangtawesin V, et al. (2017) Correlation of 25-hydroxyvitamin D levels in serum v. breastmilk in vitamin D-supplementation breastfeeding women during lactation: randomized double blinded control trial. J Med Assoc Thai 1, S165–S171. [PubMed] [Google Scholar]
- 60. Oberhelman SS, Meekins ME, Fischer PR, et al. (2013) Maternal vitamin D supplementation to improve the vitamin D status of breast-fed infants: a randomized controlled trial. Mayo Clin Proc 88, 1378–1387. [DOI] [PMC free article] [PubMed]
- 61. Clemente HA, Ramalho HM, Lima MS, et al. (2015) Maternal supplementation with natural or synthetic vitamin E and its levels in human colostrum. J Pediatr Gastroenterol Nutr 60, 533–537. [DOI] [PubMed] [Google Scholar]
- 62. de Sousa Rebouças A, Costa Lemos da Silva AG, Freitas de Oliveira A, et al. (2019) Factors associated with increased alpha-tocopherol content in milk in response to maternal supplementation with 800 μg of vitamin E. Nutrients 11, 900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Gaur S, Kuchan MJ, Lai CS, et al. (2017) Supplementation with RRR- or all-rac-alpha-tocopherol differentially affects the α-tocopherol stereoisomer profile in the milk and plasma of lactating women. J Nutr 147, 1301–1307. [DOI] [PubMed] [Google Scholar]
- 64. Kanno C, Kobayashi H & Yamauchi K (1989) Transfer of orally administered α-tocopherol into human milk. J Nutr Sci Vitaminol (Tokyo) 35, 649–653. [DOI] [PubMed]
- 65. Pires Medeiros JF, Ribeiro KD, Lima MS, et al. (2016) α-Tocopherol in breast milk of women with preterm delivery after a single postpartum oral dose of vitamin E. Br J Nutr 115, 1424–1430. [DOI] [PubMed] [Google Scholar]
- 66. Antonakou A, Chiou A, Andrikopoulos NK, et al. (2011) Breast milk tocopherol content during the first six months in exclusively breastfeeding Greek women. Eur J Nutr 50, 195–202. [DOI] [PubMed] [Google Scholar]
- 67. Bolisetty S, Gupta JM, Graham GG, et al. (1998) Vitamin K in preterm breastmilk with maternal supplementation. Acta Paediatr 87, 960–962. [DOI] [PubMed] [Google Scholar]
- 68. Greer FR, Marshall SP, Foley AL, et al. (1997) Improving the vitamin K status of breastfeeding infants with maternal vitamin K supplements. Pediatrics 99, 88–92. [DOI] [PubMed] [Google Scholar]
- 69. von Kries R, Shearer M, McCarthy PT, et al. (1987) Vitamin K1 content of maternal milk: influence of the stage of lactation, lipid composition, and vitamin K1 supplements given to the mother. Pediatr Res 22, 513–517. [DOI] [PubMed] [Google Scholar]
- 70. Chang SJ & Kirksey A (2002) Vitamin B6 status of breast-fed infants in relation to pyridoxine HCl supplementation of mothers. J Nutr Sci Vitaminol (Tokyo) 48, 10–17. [DOI] [PubMed] [Google Scholar]
- 71. Hampel D, Shahab-Ferdows S, Islam MM, et al. (2017) Vitamin concentrations in human milk vary with time within feed, circadian rhythm, and single-dose supplementation. J Nutr 147, 603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Nail PA, Thomas MR & Eakin R (1980) The effect of thiamin and riboflavin supplementation on the level of those vitamins in human breast milk and urine. Am J Clin Nutr 33, 198–204. [DOI] [PubMed] [Google Scholar]
- 73. Styslinger LM & Kirksey A (1985) Effects of different levels of vitamin B-6 supplementation on vitamin B-6 concentrations in human milk and vitamin B-6 intakes of breastfed infants. Am J Clin Nutr 41, 21–31. [DOI] [PubMed] [Google Scholar]
- 74. Thomas MR, Kawamoto J, Sneed SM, et al. (1979) The effects of vitamin C, vitamin B6, and vitamin B12 supplementation on the breast milk and maternal status of well-nourished women. Am J Clin Nutr 32, 1679–1685. [DOI] [PubMed] [Google Scholar]
- 75. Byerley LO & Kirksey A (1985) Effects of different levels of vitamin C intake on the vitamin C concentration in human milk and the vitamin C intakes of breast-fed infants. Am J Clin Nutr 41, 665–671. [DOI] [PubMed] [Google Scholar]
- 76. Daneel-Otterbech S, Davidsson L & Hurrell R (2005) Ascorbic acid supplementation and regular consumption of fresh orange juice increase the ascorbic acid content of human milk: studies in European and African lactating women. Am J Clin Nutr 81, 1088–1093. [DOI] [PubMed] [Google Scholar]
- 77. Leung AM, Braverman LE, He X, et al. (2012) Breastmilk iodine concentrations following acute dietary iodine intake. Thyroid 22, 1176–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Mulrine HM, Skeaff SA, Ferguson EL, et al. (2010) Breast-milk iodine concentration declines over the first 6 mo postpartum in iodine-deficient women. Am J Clin Nutr 92, 849–856. [DOI] [PubMed] [Google Scholar]
- 79. Nazeri P, Mirmiran P, Tahmasebinejad Z, et al. (2017) The Effects of iodine fortified milk on the iodine status of lactating mothers and infants in an area with a successful salt iodization program: a randomized controlled trial. Nutrients 9, 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Ureta-Velasco N, Keller K, Escuder-Vieco D, et al. (2022) Assessment of iodine concentration in human milk from donors: implications for preterm infants. Nutrients 14, 4304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Bianchi ML, Cruz A, Zanetti MA, et al. (1999) Dietary intake of selenium and its concentration in breast milk. Biol Trace Elem Res 70, 273–277. [DOI] [PubMed] [Google Scholar]
- 82. Dodge ML, Wander RC, Butler JA, et al. (1999) Selenium supplementation increases the polyunsaturated fatty acid content of human breast milk. J Trace Elem Exp Med 12, 37–44. [Google Scholar]
- 83. Dylewski ML & Picciano MF (2002) Milk selenium content is enhanced by modest selenium supplementation in extended lactation. J Trace Elem Exp Med 15, 191–199. [Google Scholar]
- 84. Trafikowska U, Sobkowiak E, Butler JA, et al. (1998) Organic and inorganic selenium supplementation to lactating mothers increase the blood and milk Se concentrations and Se intake by breast-fed infants. J Trace Elem Med Biol 12, 77–85. [DOI] [PubMed] [Google Scholar]
- 85. Trafikowska U, Zachara BA, Wiacek M, et al. (1996) Selenium supply and glutathione peroxidase activity in breastfed Polish infants. Acta Paediatr 85, 1143–1145. [DOI] [PubMed] [Google Scholar]
- 86. Valent F, Horvat M, Mazej D, et al. (2011) Maternal diet and selenium concentration in human milk from an Italian population. J Epidemiol 21, 285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Yalçin SS, Baykan A, Yurdakök K, et al. (2009) The factors that affect milk-to-serum ratio for iron during early lactation. J Pediatr Hematol Oncol 31, 85–90. [DOI] [PubMed] [Google Scholar]
- 88. Choi YK, Kim J-M, Lee J-E, et al. (2016) Association of maternal diet with zinc, copper, and iron concentrations in transitional human milk produced by Korean mothers. Clin Nutr Res 5, 15–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Leotsinidis M, Alexopoulos A & Kostopoulou-Farri E (2005) Toxic and essential trace elements in human milk from Greek lactating women: association with dietary habits and other factors. Chemosphere 61, 238–247. [DOI] [PubMed] [Google Scholar]
- 90. Vuori E, Makinen SM, Kara R, et al. (1980) The effects of the dietary intakes of copper, iron, manganese, and zinc on the trace element content of human milk. Am J Clin Nutr 33, 227–231. [DOI] [PubMed] [Google Scholar]
- 91. Forsum E & Lonnerdal B (1980) Effect of protein intake on protein and nitrogen composition of breast milk. Am J Clin Nutr 33, 1809–1813. [DOI] [PubMed] [Google Scholar]
- 92. Rana SK & Sanders TA (1986) Taurine concentrations in the diet, plasma, urine and breast milk of vegans compared with omnivores. Br J Nutr 56, 17–27. [DOI] [PubMed] [Google Scholar]
- 93. Metcalfe JR, Marsh JA, D’Vaz N, et al. (2016) Effects of maternal dietary egg intake during early lactation on human milk ovalbumin concentration: a randomized controlled trial. Clin Exp Allergy 46, 1605–1613. [DOI] [PubMed] [Google Scholar]
- 94. Palmer DJ, Gold MS & Makrides M (2005) Effect of cooked and raw egg consumption on ovalbumin content of human milk: a randomized, double-blind, cross-over trial. Clin Exp Allergy 35, 173–178. [DOI] [PubMed] [Google Scholar]
- 95. Perrin MT, Pawlak R, Allen LH, et al. (2020) Total water-soluble choline concentration does not differ in milk from vegan, vegetarian, and nonvegetarian lactating women. J Nutr 150, 512–517. [DOI] [PubMed] [Google Scholar]
- 96. Dowlati Y, Ravindran AV, Maheux M, et al. (2014) No effect of oral tyrosine on total tyrosine levels in breast milk: implications for dietary supplementation in early postpartum. Arch Womens Ment Health 17, 541–548. [DOI] [PubMed] [Google Scholar]
- 97. Castro F, Harari F, Llanos M, et al. (2014) Maternal-child transfer of essential and toxic elements through breast milk in a mine-waste polluted area. Am J Perinatol 31, 993–1002. [DOI] [PubMed] [Google Scholar]
- 98. Dewailly E, Ryan JJ, Laliberté C, et al. (1994) Exposure of remote maritime populations to coplanar PCBs. Environ Health Perspect 102, 205–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Gundacker C, Pietschnig B, Wittmann KJ, et al. (2002) Lead and mercury in breast milk. Pediatrics 110, 873–878. [DOI] [PubMed] [Google Scholar]
- 100. Ursinyova M, Masanova V, Uhnakova I, et al. (2019) Prenatal and early postnatal exposure to total mercury and methylmercury from low maternal fish consumption. Biol Trace Elem Res 191, 16–26. [DOI] [PubMed] [Google Scholar]
- 101. EFSA (2019) Dietary Reference Values for the EU. www.efsa.europa.eu (accessed May 2023).
- 102. Ureta-Velasco N, Montealegre-Pomar A, Keller K, et al. (2023) Associations of dietary intake and nutrient status with micronutrient and lipid composition in breast milk of donor women. Nutrients 15, 3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Moller UK, Streym S, Jensen LT, et al. (2013) Increased plasma concentrations of vitamin D metabolites and vitamin D binding protein in women using hormonal contraceptives: a cross-sectional study. Nutrients 5, 3470–3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Ranard KM & Erdman JW Jr (2018) Effects of dietary RRR alpha-tocopherol v. all-racemic α -tocopherol on health outcomes. Nutr Rev 76, 141–153. [DOI] [PubMed] [Google Scholar]
- 105. Domellof M, Lonnerdal B, Dewey KG, et al. (2004) Zinc, and copper concentrations in breast milk are independent of maternal mineral status. Am J Clin Nutr 79, 111–115. [DOI] [PubMed] [Google Scholar]
- 106. Ballard O & Morrow AL (2013) Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am 60, 49–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Italianer MF, Naninck EFG, Roelants JA, et al. (2020) Circadian variation in human milk composition, a systematic review. Nutrients 12, 2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Reynolds LM, Howard TD, Ruczinski I, et al. (2018) Tissue-specific impact of FADS cluster variants on FADS1 and FADS2 gene expression. PLoS One 13, e0194610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Schaeffer L, Gohlke H, Muller M, et al. (2006) Common genetic variants of the FADS1 FADS2 gene cluster and their reconstructed haplotypes are associated with the fatty acid composition in phospholipids. Hum Mol Genet 15, 1745–1756. [DOI] [PubMed] [Google Scholar]
- 110. Xie L & Innis SM (2008) Genetic variants of the FADS1 FADS2 gene cluster are associated with altered (n-6) and (n-3) essential fatty acids in plasma and erythrocyte phospholipids in women during pregnancy and in breast milk during lactation. J Nutr 138, 2222–2228. [DOI] [PubMed] [Google Scholar]
- 111. Jeanes YM, Hall WL, Ellard S, et al. (2004) The absorption of vitamin E is influenced by the amount of fat in a meal and the food matrix. Br J Nutr 92, 575–579. [DOI] [PubMed] [Google Scholar]
- 112. Sylvetsky AC, Gardner AL, Bauman V, et al. (2015) Nonnutritive sweeteners in breast milk. J Toxicol Environ Health A 78, 1029–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Falize et al. supplementary material