Abstract
Objective
To test the hypothesis that healthy weight status and adherence to American Academy of Pediatrics (AAP) guidelines for diet and physical activity would extend to greater executive function (EF) at age 24 months.
Study design
Parents of 24-month-old children from the STRONG Kids 2 cohort study (n = 352) completed the Behavioral Rating Inventory of Executive Function for Preschoolers (BRIEF-P) and reported physical activities, diet, and screen time. Toddlers met AAP guidelines if they consumed at least 5 servings of fruits and vegetables, were physically active, refrained from sugar-sweetened beverages, and limited daily screen time to <60 minutes. Relationships between EF, 24-month weight status, and meeting AAP guidelines were tested independent of child sex, ethnicity, socioeconomic status, weight status at birth, and maternal pregnancy weight status.
Results
Weight-for-length z-score had no effect on EF. Toddlers meeting the screen time guideline had greater EF (β, −0.125; 95% CI, 0.234 to −0.008), inhibitory self-control (β, −0.142; 95% CI, −0.248 to −0.029), and emergent meta-cognition (β, −0.111; 95% CI, −0.221 to 0.002), indicated by lower BRIEF-P scores. Those with more minutes of screen time had poorer overall EF (β, 0.257; 95% CI, 0.118–0.384), inhibitory self-control (β, 0.231; 95% CI, 0.099–0.354), cognitive flexibility (β, 0.217; 95% CI, 0.082–0.342), and emergent metacognition (β, 0.257; 95% CI, 0.120–0.381). Daily physical activity was associated with greater emergent metacognition (β, −0.116; 95% CI, −0.225 to −0.005).
Conclusions
Meeting AAP guidelines for physical activity and screen time was related to greater EF in a demographically homogenous sample of toddlers. Future randomized control trials and more diverse samples are needed to confirm the directionality of this relationship.
Clinical trial registration
Executive function (EF), defined as neurocognitive processes pertinent to the regulation of goal-directed behaviors,1 is linked to overweight and obesity in childhood.2 Low EF is implicated in lower academic success as early as preschool age,3 as well as in poorer physical health (including overweight), financial instability, criminal offenses, and substance dependence in adulthood.4 Inhibitory control is a domain of EF that allows one to regulate behavior, attention, thoughts, and emotions1 and has been heavily studied in regard to weight status. This is likely due to its role in the regulation of energy intake and subsequently, prevention of excess weight gain.2 Indeed, several longitudinal studies have observed poor performance on various aspects of inhibitory control in preschool ages to be predictive of body mass index (BMI) z-scores throughout childhood.5,6 Few studies have explored the relationship between early-life weight status in multiple EF domains that are thought to develop rapidly over early childhood, such as working memory (which allows individuals to hold on to information for application to problem-solving situations) and cognitive flexibility (which allows for switching of perspective or focus)1; however, children with higher weight status as young as 5–9 years exhibit poorer EF in these domains.7,8 By advancing our understanding of the relationship of weight status with these important predictors of success across the lifespan, we add to the understanding of the possible impact of obesity on cognitive development.
Because the prevalence of overweight and obesity tends to rise with age,9 it is also important to consider how habits of diet and play that emerge around toddlerhood could influence EFs directly and indirectly through their effects on weight status. The American Academy of Pediatrics (AAP) provides evidence-based guidelines for the prevention of childhood obesity in the form of the Bright Futures initiative, which encourages (1) 5 or more servings of fruits and vegetables per day; (2) reduced or eliminated intake of sugar-sweetened beverages (SSB); (3) less than 1 hour of screen time daily; and (4) participation in daily physical activity or at least 60 minutes of moderate-to-vigorous physical activity daily.10 Emerging evidence in older children suggests that adherence to these guidelines positively impacts cognitive function. Specifically, the amount of screen time11,12 and physical activity,13 as well as various aspects of diet quality,14 have been linked to EF in school-aged and adolescent children, although not independently of weight status. A better understanding of the interrelationships among these factors in toddlerhood is needed, as that stage marks a sensitive period of cognitive development15 and rapid brain growth.16
The primary aim of the present analysis was to examine how toddler weight status is related to EF. A secondary aim was to address the possible direct and indirect (through weight status) relationships among adherence to childhood obesity prevention guidelines, health behaviors, and better EF at 24 months of age (24-moa). A sub-aim of these analyses was to explore the impact of additional early-life factors, delivery mode, and feeding mode at 3 months of age (3-moa) as covariates of the relationship between weight status and EF. Determining the relationships among weight status, health behaviors, obesity prevention guidelines, and EF in toddlers could inform interventions aimed at improving adherence to guidelines.
Methods
Data were obtained for mothers and 24-moa dyads enrolled in the STRONG Kids 2 birth cohort study (ClinicalTrials.gov: NCT03341858).17 This study was approved by the University of Illinois Institutional Review Board (13 448). Women were recruited during their third trimester of pregnancy between May 2013 and January 2017 from the Francis Nelson Center in conjunction with Carle Foundation Hospital (Champaign, IL), Christie Clinic (Champaign, IL), Decatur Memorial Hospital (Decatur, IL), Provena United Samaritans Medical Center, and Danville Polyclinic (Danville, IL) at prenatal visits or birthing classes provided by the sites. For birthing classes, recruitment was conducted by STRONG Kids research staff. For prenatal visits, recruitment materials were distributed by trained clinic or hospital staff. In addition, participants were recruited through local newsletters and other media outlets in the Champaign-Urbana, Danville, and Decatur areas.
Interested mothers were contacted by trained research staff to schedule a meeting during their next prenatal visit to discuss further details of the study and to confirm or decline enrollment. In either case, mothers were provided with a $15 gift card for their time. Online informed consent forms were completed by all participant parents or guardians. Infants with birth conditions that affect feeding or who were born prematurely (<37 weeks) or with a low birth weight (<2.5 kg) were excluded from the cohort study. After using these exclusionary criteria and addressing missing data a final sample of 356 children was retained for analyses (see the EF Measurement section and Figure 1; available at www.jpeds.com).
Figure 1.
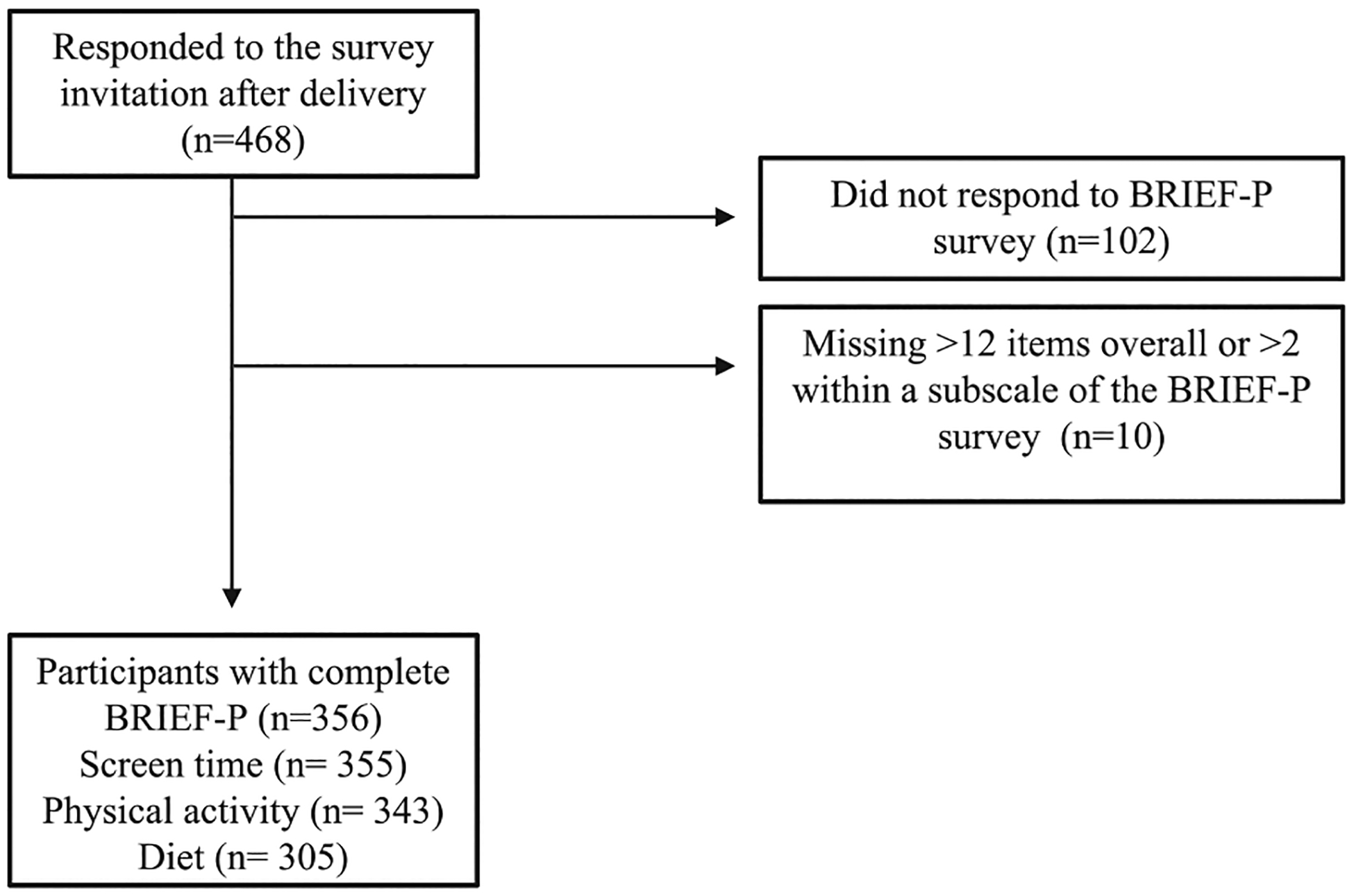
Study recruitment and data analysis flow.
Measures
Demographics.
Caregivers responded to a survey that provided their highest level of education, maternal prepregnancy height and weight, childbirth mode, child’s birth weight and length, child’s ethnicity/race, and household income at 24-moa. Mother’s level of education and household income were used to compute composite socioeconomic status (SES) scores, which were divided into low, medium, and high SES. Some caregivers failed to disclose socioeconomic (n = 32), ethnicity (n = 16), prepregnancy weight (n = 13), birth weight (n = 7), and delivery mode (n = 1). There was no significant difference in child sex (mean difference, 0.03; 95% CI, −0.14 to 0.07), ethnicity (mean difference, 0.07; 95% CI, −0.16 to 0.03), 24-moa Weight-for-length z-score (WFLZ) (mean difference, 0.02; 95% CI, −0.21 to 0.24), age (mean difference, 0.01; 95% CI, −0.04 to 0.03), and 6-week high SES (mean difference <0.00; 95% CI, −0.10 to 0.10) or low SES (mean difference, 0.02; 95% CI, −0.04 to 0.08) between families lost to follow-up by 24-moa.
Anthropometrics.
All 24-moa measurements were obtained during home visits by trained research personnel. After requesting that shoes and any excess, heavy clothing be removed, the average of 2 measurements of height and weight obtained with a portable stadiometer (Seca 213) and a digital scale (HealthOmeter 349KLX), respectively, were recorded. WFLZ was computed using the World Health Organization’s child growth standards. Children were classified as obese (≥3.0), overweight (≥2.0), normal weight (−2.0 to <2.0), and underweight (<−2.0) based on established criteria.18 Maternal prepregnancy height and weight were self-reported and BMI was used to classify mothers as underweight (BMI <18.5 kg/m2), normal weight (18.5≤ BMI <25), overweight (25≤ BMI <30), or obese (BMI ≥30). Twenty-three participants at 24-moa had missing height and weight measurements.
EF.
Parents completed the Behavioral Rating Inventory of EF for Preschoolers (BRIEF-P),19 which consists of 63 questions on a single-rating scale of frequency—never (1), sometimes (2), or often (3)—of everyday behaviors at home or daycare. A lower score is indicative of better EF—that is, the child exhibits lower frequency of behavioral problems related to EF. Scoring was completed based on recommendations from the survey authors. In brief, the responses were aggregated to compute 5 clinical subscales representing various dimensions of EF (Inhibit, Shift, Emotional Control, Working Memory, and Plan/Organize). According to the scoring recommendations, clinical scales consisting of 3 broader indices were then created: Inhibitory Self-Control (composed of Inhibit and Emotional Control scales), Cognitive Flexibility of Shift and Emotional Control, Emergent Metacognition of Working Memory, and Plan/Organize, along with Overall Executive Function (composed of all 5 scales).
In adherence to the BRIEF-P manual instructions, toddlers missing >12 items overall or >2 items on a scale were excluded from the analyses, and the remaining missing values (0.5%) on this survey were imputed with the response “never,” at the guideline provided by the BRIEF-P manual. Survey results were assessed for validity using Negativity and Inconsistency indices.19 Raw index scores were converted to T-scores and percentiles as instructed in the BRIEF-P manual for descriptive purposes. Raw scores are used in all analyses, as several of our toddlers fell just below 24-moa (n = 183; minimum age, 23.41 months).20 Age was not associated with any BRIEF-P index and thus was not included as a covariate in the models.
Physical Activity.
Parents reported the number of days per week that their child participated in various physical activities for at least 15 minutes using the Sports, Play, and Active Recreation for Kids (SPARK) survey.21 Total activities reported were summed and used to determine weekly physical activity. Those reporting 1 activity per day were classified as meeting the AAP guideline for toddlers to engage in active play every day. In this case, it was assumed that if at least 7 activities were reported in a week, the child was participating in at least 1 activity per day. Thirteen participants failed to complete the SPARK survey.
Screen Time.
The Common Sense Media Survey was used by parents to report their child’s screen time.22 This survey consists of both ratings and open-ended questions to determine the frequency and duration of various types of media, respectively. Minutes of media use that involved screens (ie, TV, DVD, shows on a computer or cellphone, games on a console, computer, cellphone, handheld device, and other uses of apps and computers) were summed to determine total screen time. Outlier values for screen time, as determined by those 3 SD above the mean (2075 minutes/day), were winsorized to the next highest value within 3 SD (685 minutes/day). Those reporting no more than 60 minutes of screen time were classified as meeting the AAP guideline for screen time. One participant failed to complete the Common Sense Media Survey.
Dietary Intake.
At 3-moa, mothers completed survey items on feeding mode (ie, exclusive breastfeeding, formula feeding, or both) from the CDC Survey on Infant Feeding Practices Study II.23 At 24-moa, parents completed the NutritionQuest Child Block Food Frequency Questionnaire (FFQ) for Ages 2–7, consisting of 90 questions pertaining to the child’s usual eating habits in the previous 6 months. Food lists developed by NutritionQuest were obtained from National Health and Nutrition Examination Survey II dietary recall data, which provided approximate daily servings of fruits and vegetables and kcal from sugary beverages.24 Children above (1602 kcal) or below (396 kcal) 2 SD of the mean for total kcal were considered outliers (n = 7) and were excluded, based on typical energy intake of ~1470 kcal for age 2–5 years.25 Children who consumed at least 5 servings of fruits and vegetables were classified as meeting the AAP guideline for fruit and vegetable servings. The AAP recommends limited consumption of sugary beverages10; thus, children who did not consume any energy from sugary beverages were classified as meeting the guideline. Fifty-one participants failed to complete the FFQ, and 8 did not complete the CDC Survey on Infant Feeding Practices Study II.
Statistical Analyses
A path analysis with the structural equation modeling technique was performed with MPlus version 8.4 to assess the direct and indirect relationships between AAP guidelines and heath behaviors with EF (Figures 2 and 3). Direct effects were tested to examine AAP guidelines and continuous health behavior relationships with BRIEF-P indices. Indirect effects were tested to explore the possible mediating effect of WFLZ at 24-moa on the relationships of AAP guidelines and continuous health behaviors with BRIEF-P indices. All path coefficients were freely estimated in the models. A threshold of P = .05 was considered significant. P values were corrected for multiple comparisons using a Benjamini–Hochberg procedure with a false discovery rate of 0.1 to determine significance after correction. Because individual testing was the primary interest of this study (ie, to determine relationships between individual components of EF with specific AAP guidelines or continuous health behaviors), P values were considered the primary indicator for hypothesis testing.26 The full information maximum likelihood approach was used to handle missing data. Unlike traditional maximum likelihood estimation, which requires complete data, this method uses all observed variables for each case, allowing computation of parameter estimates even in the presence of missing data. The full information maximum likelihood approach has been shown to produce unbiased parameter estimates and standard errors when data are at least missing at random.27 Selection of the covariates—child sex, SES, birth WFLZ, ethnicity, and maternal pre-pregnancy weight status—was based on a priori expected association with EF and WFLZ at 24-moa.10,19,20 The independent-samples t-test and ANOVA were used to examine these relations in our sample. These analyses and descriptive statistics were conducted in SPSS 28.0 (IBM). Direct and indirect effects were tested using a bootstrap estimation approach with 5000 samples. Bootstrap SEs and CIs of the direct and indirect effects were calculated. Post hoc power analysis revealed that our model was sufficiently powered (95.4%) to detect an effect on overall EF, based on number of predictors included in the model (n = 10), observed R2 of 6.7%, probability level of .05, and sample size of 356.28,29 Additionally, post hoc power analyses were performed to evaluate the sufficiency of meeting the guideline for fruits and vegetable consumption and 24-moa WFLZ groups owing to their uneven group sizes.30
Figure 2.
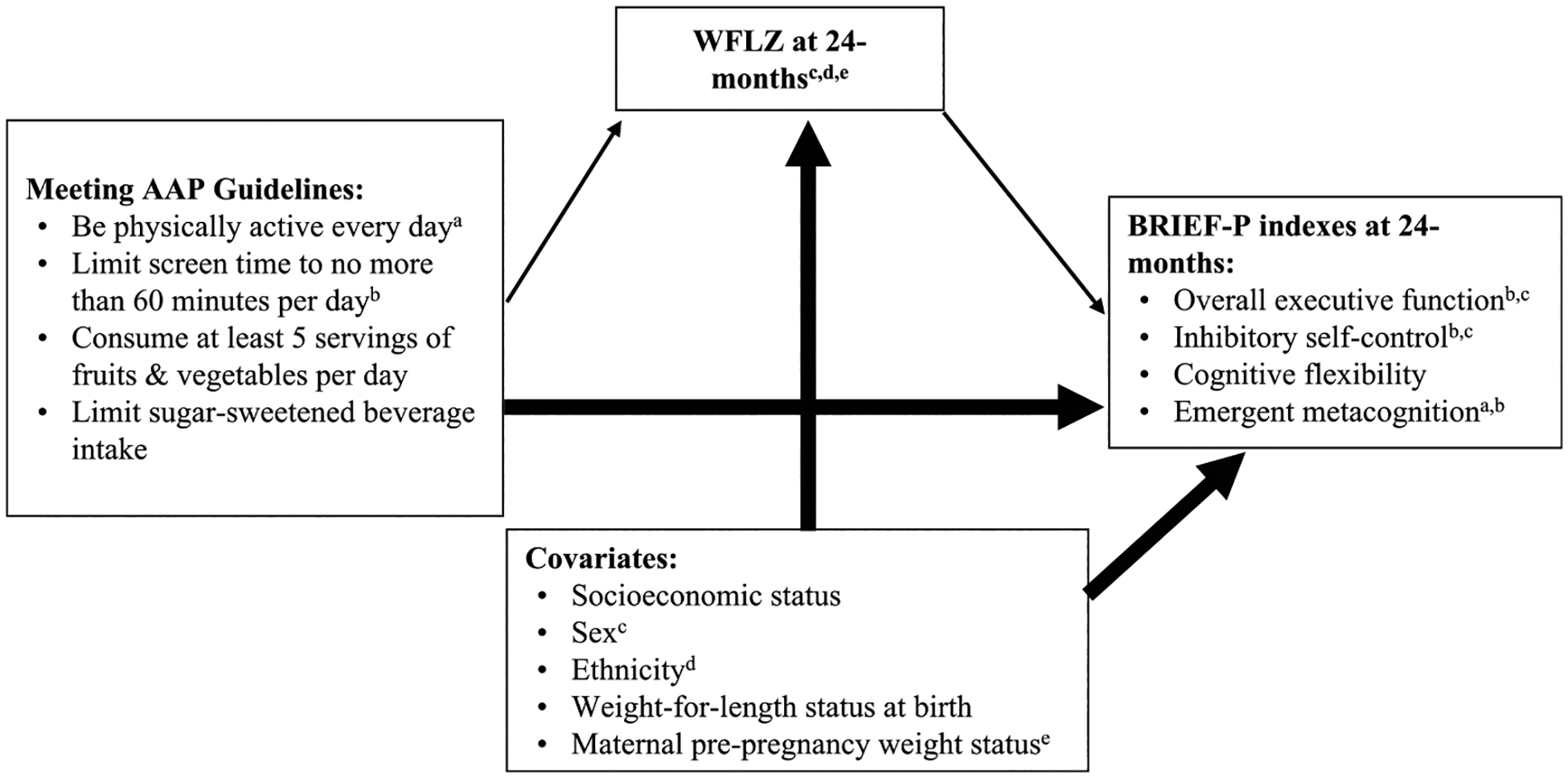
Path model A. Direct and indirect effects (through weight status) of AAP guidelines for physical activity, screen time, and fruit, vegetable, and SSB intakes on EF.
Figure 3.
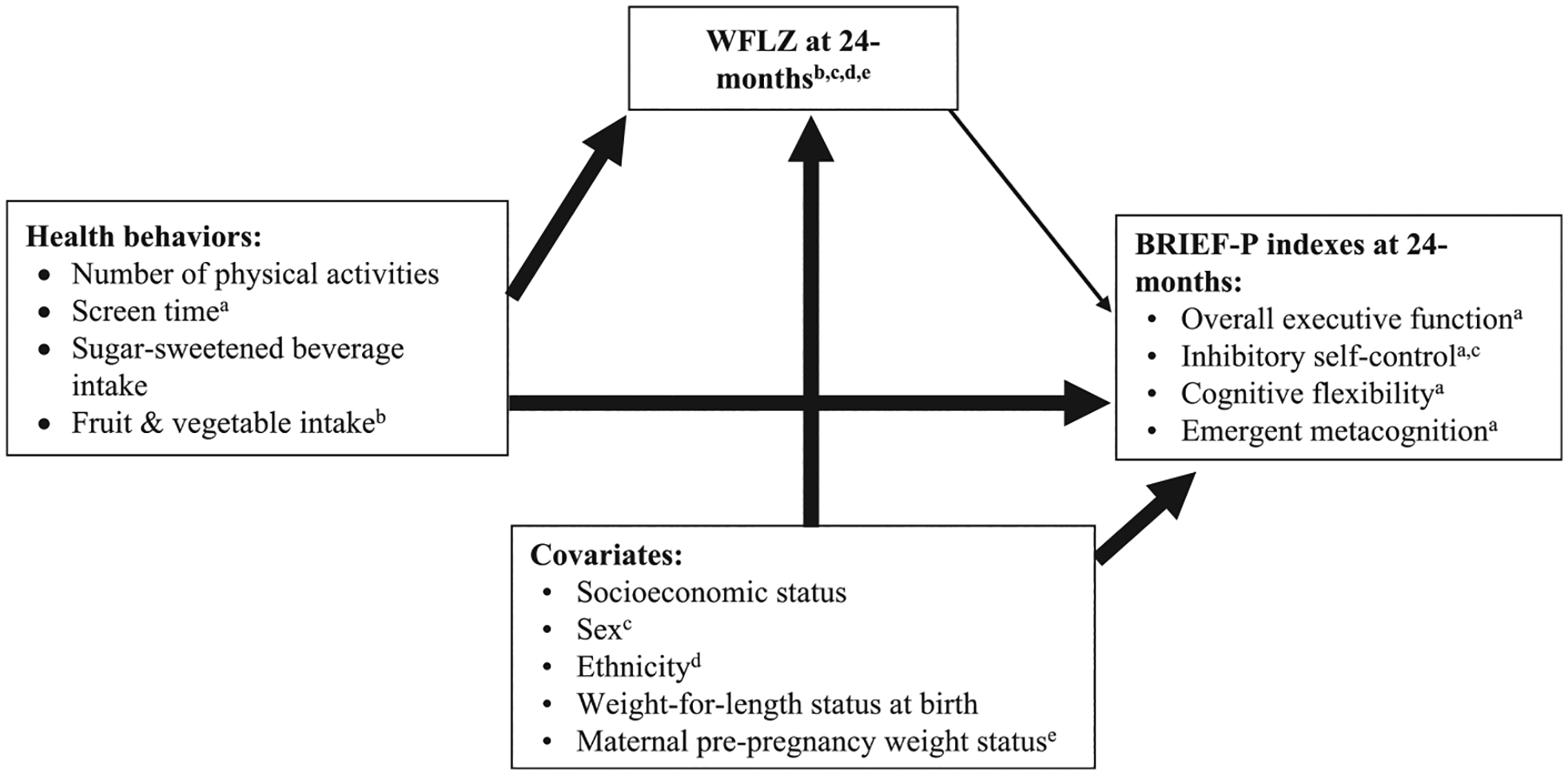
Path model B. Direct and indirect effects (through weight status) of physical activity, screen time, and fruit, vegetable, and SSB intakes on EF.
Results
Participant recruitment and data analysis flow can be found in Figure 1. Demographic data, weight status, and EF percentiles standardized for age and sex are presented in Table I. Adherence to AAP guidelines can be found in Table II. Eight percent of toddlers met none of the guidelines, 25% met 1 guideline, 38% met 2 guidelines, 28% met 3 guidelines, and 1% met all 4 AAP guidelines. Note that EF scores were all below the 50th percentile for frequency of problematic behaviors related to poorer EF (Table I). Toddlers of mothers with obesity or overweight prior to conception had higher WFLZ at 24-moa (mean difference, 0.73; 95% CI, 0.39 to 1.07) and toddlers who had a higher WFLZ at birth (≥2.0) exhibit higher WFLZ at 24-moa (mean difference, 0.82; 95% CI, −1.63 to 0.01). The t-test showed no significant difference in EF by any covariate or in WFLZ at 24-mo by 3-moa feeding mode, delivery mode, ethnicity, or SES in this sample (Table III; available at www.jpeds.com). Sex, ethnicity, SES, WFLZ at birth, and maternal pregnancy weight status were included as covariates in subsequent analyses.
Table I.
Maternal and child characteristics and demographics
| Characteristics | Total N | Values |
|---|---|---|
| Child sex, n (%) | 356 | |
| Male | 177 (49.7) | |
| Female | 179 (50.3) | |
| Child race, n (%) | 340 | |
| Caucasian | 255 (75.7) | |
| Asian | 18 (5.3) | |
| Black | 18 (5.3) | |
| American Indian or Alaskan Native | 1 (0.3) | |
| Multiple races | 45 (13.4) | |
| SES, n (%) | 324 | |
| Low | 15 (4.6) | |
| Medium | 121 (37.3) | |
| High | 188 (58.0) | |
| Child age, mo, mean ± SE | 356 | 24.1 (0.03) |
| Delivery mode, n (%) | 355 | |
| Cesarean | 83 (23.4) | |
| Vaginal | 272 (76.6) | |
| Feeding mode at 3-moa, n (%) | 348 | |
| Exclusively breastfed | 238 (68.4) | |
| Mixed feeding | 61 (17.5) | |
| Exclusively formula-fed | 49 (14.1) | |
| Child WFLZ* | ||
| Birth weight category, n (%) | 349 | |
| Underweight | 36 (10.3) | |
| Normal weight | 299 (85.7) | |
| Overweight | 14 (4.0) | |
| 24-month weight category, n (%) | 333 | |
| Underweight | 12 (3.6) | |
| Normal weight | 254 (76.3) | |
| Overweight | 67 (20.1) | |
| Maternal prepregnancy weight status, n (%) | 343 | |
| Normal weight | 168(49.0) | |
| Overweight | 85 (24.8) | |
| Obese | 90 (26.2) | |
| Standardized EF scores†, mean (SE) | 356 | |
| Overall EF | 47.2 (1.7) | |
| Inhibitory self-control | 45.1 (1.5) | |
| Cognitive flexibility | 44.1 (1.5) | |
| Working memory | 47.8 (1.8) | |
| Raw EF scores‡, mean (SE) | 356 | |
| Overall EF | 91.3 (1.0) | |
| Inhibitory self-control | 38.4 (0.4) | |
| Cognitive flexibility | 29.3 (0.3) | |
| Working memory | 38.8 (0.5) |
WFLZ characterized by weight category using the following World Health Organization standard cutoffs: <−2.0, underweight; −2.0 to <2.0, normal weight; ≥2.0 to <3.0, overweight; ≥3.0, obese.
Data are average percentile scores standardized for sex and age (SE). Lower than 50th percentile indicates reporting fewer problems related to EF relative to the BRIEF-P standard population mean.
Data are average raw scores (SE) used in analyses.
Table II.
Adherence to AAP guidelines (%) and mean participant physical activities, screen time, and fruit, vegetable, and SSB intakes
| Measures | N | Reported frequency, mean (SE) | Guidelines | % adherence (n) |
|---|---|---|---|---|
| Physical activities, n/wk | 343 | 10.8 (0.5) | Physically active every day | 75.5 (259) |
| Screen time, min/d | 355 | 98.2 (6.4) | No more than 60 minutes of screen time daily | 54.1 (192) |
| Fruits and vegetables, servings/d | 305 | 2.8 (0.1) | At least 5 servings of fruits and vegetables daily | 3.9 (12) |
| SSB, kcal/d | 305 | 11.5 (1.7)* | Limit SSB | 68.9 (210) |
Includes only those who reported any SSB intake (n = 95).
Table III.
Means of the BRIEF-P indices and WFLZ at 24-moa by sex, ethnicity, SES, WFLZ at birth, maternal prepregnancy weight status, delivery mode, and feeding mode at 3-moa
| Variables | Overall EF | Cognitive flexibility | Inhibitory self-control | Emergent metacognition | WFLZ at 24-moa |
|---|---|---|---|---|---|
| Sex | |||||
| Females (n) | 89.67 ± 1.34 (87.06–92.25) | 28.93 ± 0.44 (28.10–29.80) | 37.60 ± 0.59 (36.44–38.75) | 38.14 ± 0.65 (36.86–39.40) | 0.55 ± 0.10 (0.35–0.74) |
| Males (n) | 93.03 ± 1.38 (90.32–95.74) | 29.71 ± 0.44 (28.86–30.59) | 39.25 ± 0.62 (38.01–40.45) | 39.53 ± 0.67 (38.19–40.82) | 0.81 ± 0.11 (0.59–1.04) |
| P value | .078 | .215 | .057 | .137 | .084 |
| Ethnicity | |||||
| Caucasian (n) | 90.91 ± 1.12 (88.72–93.11) | 29.13 ± 0.36 (28.44–29.82) | 38.28 ± 0.50 (37.32–39.25) | 38.67 ± 0.56 (37.60–39.78) | 0.73 ± 0.86 (0.57–0.90) |
| Other (n) | 90.82 ± 1.90 (87.26–94.61) | 29.48 ± 0.66 (28.19–30.82) | 37.95 ± 0.90 (36.22–39.75) | 38.44 ± 0.90 (36.68–40.20) | 0.38 ± 0.16 (0.06–0.70) |
| P value | .970 | .622 | .755 | .818 | .054 |
| SES* | |||||
| Low (n) | 99.40 ± 5.96 (86.63–112.17) | 31.93 ± 2.02 (27.60–36.27) | 42.00 ± 2.69 (36.24–47.76) | 41.93 ± 2.74 (36.07–47.80) | 0.67 ± 0.29 (0.05–1.29) |
| Medium (n) | 90.57 ± 1.68 (87.24–93.90) | 28.81 ± 0.53 (27.77–29.85) | 38.08 ± 0.76 (36.59–39.58) | 38.80 ± 0.82 (37.17–40.43) | 0.61 ± 0.14 (0.34–0.88) |
| High (n) | 91.66 ± 1.27 (89.15–94.17) | 29.59 ± 0.42 (28.75–30.42) | 38.59 ± 0.58 (37.44–39.73) | 38.80 ± 0.62 (37.58–40.01) | 0.71 ± 0.10 (0.51–0.92) |
| P value† | .206 | .127 | .219 | .403 | .839 |
| WFLZ at birth | |||||
| <2.0 (n) | 91.43 ± 5.80 (80.59–103.08) | 28.93 ± 1.52 (26.06–32.07) | 37.43 ± 2.32 (32.92–42.07) | 39.43 ± 2.98 (33.80–45.36) | −0.08 ± 0.41 (−0.87–0.74) |
| ≥2.0 (n) | 91.11 ± 0.99 (89.20–93.06 | 29.29 ± 0.32 (28.66–29.93) | 38.35 ± 0.45 (37.48–39.23) | 38.71 ± 0.48 (37.78–39.66) | 0.74 ± 0.08 (0.59–0.89) |
| P value | .956 | .815 | .688 | .809 | .040 |
| Maternal prepregnancy weight status | |||||
| Healthy weight (n) | 93.14 ± 2.06 (89.06–97.23) | 29.34 ± 0.62 (28.11–30.58) | 39.39 ± 0.93 (37.60–41.22) | 39.89 ± 1.02 (37.85–41.88) | 0.49 ± 0.09 (0.32–0.66) |
| Overweight or obese (n) | 89.44 ± 1.10 (88.27–92.63) | 29.19 ± 0.37 (28.48–29.91) | 37.98 ± 0.50 (37.01–38.96) | 38.37 ± 0.53 (37.33–39.42) | 1.22 ±0.15 (0.91–1.51) |
| P value | .242 | .827 | .175 | .182 | <.001 |
| Delivery mode | |||||
| Vaginal (n) | 91.22 ± 1.08 (89.16–93.37) | 29.29 ± 0.35 (28.61–29.98) | 38.32 ± 0.48 (37.41–39.28) | 38.83 ± 0.53 (37.83–39.89) | −0.65 ± 0.09 (0.49–0.83) |
| Cesarean (n) | 92.05 ± 2.07 (87.86–96.00) | 29.51 ± 0.65 (28.22–30.77) | 38.90 ± 0.91 (37.18–40.70) | 38.98 ± 1.01 (37.83–39.89) | 0.76 ± 0.16 (0.43–1.08) |
| P value | .726 | .761 | .572 | .896 | .584 |
| Feeding mode at 3-moa | |||||
| Exclusively breastfed (n) | 91.20 ± 1.11 (89.10–93.40) | 29.31 ± 0.36 (28.62–30.04) | 38.23 ± 0.50 (37.27–39.27) | 38.79 ± 0.56 (37.72–39.91) | 0.63 ± 0.09 (0.45–0.81) |
| Mixed- or formula-fed (n) | 90.88 ± 1.74 (87.47–94.40) | 29.19 ± 0.59 (28.07–30.38) | 38.47 ± 0.77 (36.95–39.99) | 38.51 ± 0.85 (36.89–40.20) | 0.72 + 0.13 (0.45–0.99) |
| P value | .871 | .854 | .783 | .780 | .589 |
All values are reported as mean ± SE (95% CI). All statistics were from an independent-samples t-test with SE, 95% CIs, and P values calculated using the bootstrap with 5000 samples unless noted otherwise. Bold type denotes a significant result (P < .05).
SES is a composite score of mother’s level of education and household income, which was divided into low, medium, and high SES.
Represents P value for between-group difference by ANOVA.
Model A Results: Adherence to AAP Guidelines and EF
Adherence to guidelines was not associated with WFLZ. Toddlers adhering to the screen time guideline had significantly greater emergent metacognition (β, −0.111; 95% CI, −0.221 to 0.002), inhibitory self-control (β, −0.142; 95% CI, −0.248 to −0.029), and overall EF abilities (β, −0.125; 95% CI, −0.234 to −0.008), indicated by lower BRIEF-P scores. Those who met the guideline of daily physical activity had greater emergent metacognition (β, −0.116; 95% CI, −0.225 to −0.005). Those meeting the guideline to limit SSB had numerically greater emergent metacognition (β, −0.118; 95% CI, −0.240 to 0.001), inhibitory self-control (β, −0.107; 95% CI, −0.232 to 0.020), and overall EF (β, −0.113; 95% CI, −0.237 to −0.010), although the differences were not statistically significant. There was no significant difference in BRIEF-P indices for those meeting the guideline for fruit and vegetable intake. WFLZ at 24-moa was not associated with any BRIEF-P index, nor did it have any mediating effects on the relationships between AAP guidelines and BRIEF-P (Table IV; available at www.jpeds.com). AAP guidelines and covariates explained 10.9% of the variance in WFLZ at 24-moa. AAP guidelines, WFLZ, and covariates explained 6.7%, 6.8%, and 6.8% of the variance in overall EF, inhibitory self-control, and emergent metacognition, respectively. Male children (β, −0.127; 95% CI, −0.237 to −0.023), children of Caucasian ethnicity (β, 0.125; 95% CI, 0.007 to 0.242), and mothers with overweight or obesity prior to pregnancy (β, 0.232; 95% CI, 0.121 to 0.351) had higher WFLZ at 24-moa. Males also had poorer inhibitory self-control (β, −0.117; 95% CI, −0.223 to −0.018). Correction for multiple comparisons abrogated all significant relationships with EF and WFLZ in the model (Table IV).
Table IV.
Path model A: Standardized regression coefficients of the direct and indirect effects of adherence to AAP guidelines on BRIEF-P indices, with WFLZ at 24-moa as a mediator variable
| Variables | Point estimate (95% CI) | SE | P value | Adjusted P value* |
|---|---|---|---|---|
| Direct path from guidelines to WFLZ | ||||
| Physically active every day | −0.005 (−0.116 to 0.106) | 0.057 | .94 | 1.0 |
| No more than 60 minutes of screen time | −0.055 (−0.166 to 0.053) | 0.057 | .33 | .637 |
| At least 5 servings of fruits and vegetables | 0.096 (−0.032 to 0.219) | 0.065 | .14 | .392 |
| Limit SSB | 0.107 (−0.028 to 0.234) | 0.066 | .11 | .411 |
| Direct path from WFLZ to BRIEF-P indices | ||||
| Overall EF | −0.003 (−0.123 to 0.112) | 0.06 | .96 | 1.0 |
| Cognitive flexibility | −0.033 (−0.152 to 0.086) | 0.061 | .58 | .902 |
| Inhibitory self-control | 0.006 (−0.116 to 0.124) | 0.060 | .93 | 1.0 |
| Emergent metacognition | 0.011 (−0.108 to 0.123) | 0.059 | .86 | 1.0 |
| Effects of guidelines on overall EF | ||||
| Physically active every day | ||||
| Total | −0.082 (−0.190 to 0.029) | 0.056 | .14 | .413 |
| Direct | −0.082 (−0.190 to 0.029) | 0.056 | .14 | .436 |
| Indirect | 0.00002 (−0.007 to 0.008) | 0.003 | .997 | .997 |
| No more than 60 min of screen time | ||||
| Total | −0.125 (−0.233 to −0.008) | 0.057 | .03 | .56 |
| Direct | −0.125 (−0.234 to −0.008) | 0.057 | .03 | .42 |
| Indirect | 0.0002 (−0.009 to 0.010) | 0.005 | .97 | 1.0 |
| At least 5 servings of fruits and vegetables | ||||
| Total | −0.053 (−0.154 to 0.046) | 0.051 | .30 | .622 |
| Direct | −0.053 (−0.156 to 0.047) | 0.052 | .31 | .62 |
| Indirect | −0.0003 (−0.016 to 0.014) | 0.007 | .97 | 1.0 |
| Limit SSB | ||||
| Total | −0.114 (−0.237 to 0.010) | 0.064 | .08 | .373 |
| Direct | −0.113 (−0.237 to 0.010) | 0.065 | .08 | .407 |
| Indirect | −0.003 (−0.017 to 0.014) | 0.008 | .97 | 1.0 |
| Effects of guidelines on cognitive flexibility | ||||
| Physically active every day | ||||
| Total | −0.044 (−0.155 to 0.065) | 0.056 | .43 | .753 |
| Direct | −0.044 (−0.155 to 0.065) | 0.056 | .43 | .730 |
| Indirect | 0.0002 (−0.008 to 0.009) | 0.004 | .97 | 1.0 |
| No more than 60 min of screen time | ||||
| Total | −0.090 (−0.202 to 0.027) | 0.059 | .12 | .395 |
| Direct | −0.092 (−0.205 to 0.026) | 0.059 | .12 | .420 |
| Indirect | 0.002 (−0.007 to 0.014) | 0.005 | .71 | 1.0 |
| At least 5 servings of fruits and vegetables | ||||
| Total | −0.056 (−0.148 to 0.034) | 0.047 | .23 | .56 |
| Direct | −0.053 (−0.148 to 0.040) | 0.048 | .27 | .630 |
| Indirect | −0.003 (−0.020 to 0.011) | 0.007 | .66 | .999 |
| Limit SSB | ||||
| Total | −0.090 (−0.226 to 0.046) | 0.069 | .19 | .507 |
| Direct | −0.086 (−0.224 to 0.051) | 0.070 | .22 | .560 |
| Indirect | −0.004 (−0.023 to 0.010) | 0.008 | .66 | .973 |
| Effect of guidelines on inhibitory self-control | ||||
| Physically active every day | ||||
| Total | −0.044 (−0.153 to 0.071) | 0.057 | .44 | .725 |
| Direct | −0.044 (−0.154 to 0.071) | 0.058 | .44 | .704 |
| Indirect | −0.00003 (−0.007 to 0.008) | 0.004 | .99 | 1.0 |
| No more than 60 min of screen time | ||||
| Total | −0.143 (−0.248 to −0.029) | 0.056 | .01 | .560 |
| Direct | −0.142 (−0.248 to −0.029) | 0.056 | .01 | .280 |
| Indirect | −0.0003 (−0.010 to 0.010) | 0.005 | .95 | 1.0 |
| At least 5 servings of fruits and vegetables | ||||
| Total | −0.047 (−0.146 to 0.049) | 0.050 | .35 | .632 |
| Direct | −0.047 (−0.148 to 0.051) | 0.051 | .35 | .653 |
| Indirect | 0.001 (−0.014 to 0.016) | 0.007 | .94 | 1.0 |
| Limit SSB | ||||
| Total | −0.107 (−0.231 to 0.019) | 0.064 | .10 | .400 |
| Direct | −0.107 (−0.232 to 0.020) | 0.065 | .10 | .431 |
| Indirect | 0.001 (−0.017 to 0.016) | 0.008 | .94 | 1.0 |
| Effects of guidelines on emergent metacognition | ||||
| Physically active every day | ||||
| Total | −0.116 (−0.224 to −0.004) | 0.056 | .04 | .448 |
| Direct | −0.116 (−0.225 to −0.005) | 0.056 | .04 | .373 |
| Indirect | 0.001 (−0.008 to 0.007) | 0.004 | .99 | 1.0 |
| No more than 60 min of screen time | ||||
| Total | −0.112 (−0.222 to 0.002) | 0.057 | .047 | .376 |
| Direct | −0.111 (−0.221 to 0.002) | 0.057 | .049 | .343 |
| Indirect | −0.001 (−0.010 to 0.010) | 0.005 | .90 | 1.0 |
| At least 5 servings of fruits and vegetables | ||||
| Total | −0.053 (−0.148 to 0.045) | 0.049 | .28 | .627 |
| Direct | −0.054 (−0.150 to 0.046) | 0.050 | .28 | .603 |
| Indirect | 0.001 (−0.013 to 0.016) | 0.007 | .88 | 1.0 |
| Limit SSB | ||||
| Total | −0.117 (−0.239 to 0.003) | 0.062 | .06 | .373 |
| Direct | −0.118 (−0.240 to 0.001) | 0.063 | .06 | .336 |
| Indirect | 0.001 (−0.015 to 0.016) | 0.007 | .88 | 1.0 |
Statistics in bold type denote a significant result (P < .05) before correction for multiple comparisons. Covariates included in the model were child sex, SES, ethnicity, WFLZ at birth, and maternal prepregnancy weight status.
P values are corrected for multiple comparisons using a Benjamini–Hochberg procedure with a false discovery rate of 0.1 to determine significance after correction.
Model B Results: Associations of Physical Activity, Screen Time, and Diet with EF
Toddlers consuming more servings of fruits and vegetables had significantly higher WFLZ at 24-moa (β, 0.131; 95% CI, 0.006–0.252). Although not statistically significant, toddlers with more screen time had higher WFLZ (β, 0.116; 95% CI, −0.012 to 0.233). Screen time was significantly associated with each BRIEF-P index, such that toddlers with more screen time had poorer overall EF (β, 0.257; 95% CI, 0.118–0.384), inhibitory self-control (β, 0.231; 95% CI, 0.099–0.354), cognitive flexibility (β, 0.217; 95% CI, 0.082–0.342), and emergent metacognition (β, 0.257; 95% CI, 0.120–0.381). Intake of SSB, consumption of fruit or vegetables, and physical activity were not associated with any BRIEF-P index. SSB and number of physical activities also were not associated with WLZ at 24-moa (Table V; available at www.jpeds.com). WFLZ at 24-moa had no effect on any BRIEF-P index, nor did it have any mediating effect on the relationships between health behaviors and BRIEF-P. Health behaviors, WFLZ, and covariates explained 8.1%, 7.9%, 5.8%, and 7.7% of the variance in overall EF, inhibitory self-control, cognitive flexibility, and emergent metacognition, respectively, and health behaviors and covariates explained 11.7% of the variance in WFLZ at 24-moa. Male children (β, −0.120; 95% CI, −0.230 to −0.021), children of Caucasian ethnicity (β, 0.121; 95% CI, 0.005–0.240), and mothers with overweight or obesity prior to pregnancy (β, 0.213; 95% CI, 0.101–0.329) had higher WFLZ at 24-moa. Males also had poorer inhibitory self-control (β, −0.106; 95% CI, −0.209 to −0.007). After correction for multiple comparisons, all effects remained significant in the model except for the direct association between fruit and vegetable servings with higher WFLZ at 24-moa (Table V).
Table V.
Path model B: Standardized regression coefficients of the direct and indirect effects of health behaviors on BRIEF-P indices, with WFLZ at 24-moa as a mediator variable
| Variables | Point estimate (95% CI) | SE | P value | Adjusted P value* |
|---|---|---|---|---|
| Direct path from health behaviors to WFLZ | ||||
| Number of physical activities | −0.024 (−0.148 to 0.086) | 0.060 | .69 | .991 |
| Screen time | 0.116 (−0.012 to 0.233) | 0.062 | .06 | .336 |
| Fruit and vegetable servings | 0.131 (0.006–0.252) | 0.062 | .04 | .249 |
| SSB kcal | −0.091 (−0.229 to 0.014) | 0.062 | .14 | .713 |
| Direct path from WFLZ to BRIEF-P indices | ||||
| Overall EF | −0.032 (−0.154 to 0.088) | 0.062 | .60 | 1.0 |
| Cognitive flexibility | −0.061 (−0.179 to 0.059) | 0.061 | .32 | .943 |
| Inhibitory self-control | −0.015 (−0.139 to 0.110) | 0.062 | .82 | .937 |
| Emergent metacognition | −0.021 (−0.143 to 0.096) | 0.061 | .73 | .973 |
| Effects of health behaviors on overall EF | ||||
| Number of physical activities | ||||
| Total | −0.028 (−0.168 to 0.088) | 0.065 | .67 | .987 |
| Direct | −0.029 (−0.170 to 0.088) | 0.065 | .66 | .999 |
| Indirect | 0.001 (−0.008 to 0.012) | 0.005 | .17 | .680 |
| Screen time | ||||
| Total | 0.254 (0.114–0.378) | 0.067 | <.001 | .008 |
| Direct | 0.257 (0.118–0.384) | 0.067 | <.001 | .056 |
| Indirect | −0.004 (−0.023 to 0.011) | 0.008 | .65 | 1.0 |
| Fruit and vegetable servings | ||||
| Total | −0.067 (−0.179 to 0.056) | 0.059 | .26 | .971 |
| Direct | −0.063 (−0.179 to 0.063) | 0.061 | .30 | .988 |
| Indirect | −0.004 (−0.026 to 0.013) | 0.009 | .65 | 1.0 |
| SSB kcal | ||||
| Total | −0.045 (−0.169 to 0.125) | 0.075 | .54 | 1.0 |
| Direct | −0.048 (−0.172 to 0.125) | 0.075 | .52 | 1.0 |
| Indirect | 0.003 (−0.009 to 0.022) | 0.008 | .70 | .98 |
| Effects of health behaviors on cognitive flexibility | ||||
| Number of physical activities | ||||
| Total | −0.035 (−0.171 to 0.075) | 0.063 | .57 | 1.0 |
| Direct | −0.037 (−0.175 to 0.075) | 0.063 | .56 | 1.0 |
| Indirect | 0.001 (−0.009 to 0.014) | 0.005 | .78 | .929 |
| Screen time | ||||
| Total | 0.210 (0.076–0.336) | 0.067 | .002 | .014 |
| Direct | 0.217 (0.082–0.342) | 0.067 | .001 | .028 |
| Indirect | −0.007 (−0.026 to 0.008) | 0.009 | .41 | .998 |
| Fruit and vegetable servings | ||||
| Total | −0.031 (−0.142 to 0.090) | 0.060 | .60 | 1.0 |
| Direct | −0.024 (−0.139 to 0.100) | 0.061 | .70 | .956 |
| Indirect | −0.008 (−0.030 to 0.008) | 0.010 | .40 | 1.0 |
| SSB kcal | ||||
| Total | −0.031 (−0.144 to 0.126) | 0.068 | .65 | 1.0 |
| Direct | −0.037 (−0.151 to 0.123) | 0.068 | .59 | 1.0 |
| Indirect | 0.006 (−0.006 to 0.028) | 0.008 | .51 | 1.0 |
| Effects of health behaviors on inhibitory self-control | ||||
| Number of physical activities | ||||
| Total | −0.005 (−0.133 to 0.101) | 0.059 | .93 | .93 |
| Direct | −0.005 (−0.134 to 0.101) | 0.059 | .93 | .964 |
| Indirect | 0.0004 (−0.008 to 0.011) | 0.004 | .93 | .947 |
| Screen time | ||||
| Total | 0.229 (0.098–0.351) | 0.064 | <.001 | .019 |
| Direct | 0.231 (0.099–0.354) | 0.064 | <.001 | .014 |
| Indirect | −0.002 (−0.020 to 0.015) | 0.008 | .84 | .922 |
| Fruit and vegetable servings | ||||
| Total | −0.088 (−0.200 to 0.032) | 0.059 | .14 | .653 |
| Direct | −0.086 (−0.202 to 0.039) | 0.061 | .16 | .689 |
| Indirect | −0.002 (−0.021 to 0.016) | 0.009 | .83 | .93 |
| SSB kcal | ||||
| Total | −0.025 (−0.162 to 0.163) | 0.082 | .76 | .946 |
| Direct | −0.027 (−0.166 to 0.166) | 0.083 | .75 | .977 |
| Indirect | 0.001 (−0.011 to 0.019) | 0.007 | .86 | .926 |
| Effects of health behaviors on emergent metacognition | ||||
| Number of physical activities | ||||
| Total | −0.039 (−0.181 to 0.072) | 0.065 | .54 | 1.0 |
| Direct | −0.040 (−0.183 to 0.074) | 0.065 | .54 | 1.0 |
| Indirect | 0.001 (−0.008 to 0.011) | 0.004 | .91 | .962 |
| Screen time | ||||
| Total | 0.255 (0.118–0.012) | 0.066 | <.001 | .011 |
| Direct | 0.257 (0.120–0.381) | 0.067 | <.001 | .009 |
| Indirect | −0.002 (−0.021 to 0.012) | 0.008 | .76 | .925 |
| Fruit and vegetable servings | ||||
| Total | −0.062 (−0.171 to 0.062) | 0.058 | .29 | 1.0 |
| Direct | −0.059 (−0.172 to 0.067) | 0.059 | .32 | .996 |
| Indirect | −0.003 (−0.172 to 0.014) | 0.009 | .76 | .967 |
| SSB kcal | ||||
| Total | −0.059 (−0.172 to 0.094) | 0.068 | .38 | 1.0 |
| Direct | −0.061 (−0.175 to 0.092) | 0.068 | .37 | 1.0 |
| Indirect | 0.002 (−0.010 to 0.020) | 0.007 | .79 | .922 |
Statistics in bold type denote a significant result (P < .05). Covariates included in the model were child sex, SES, ethnicity, WFLZ at birth, and maternal prepregnancy weight status.
P values are corrected for multiple comparisons using a Benjamini–Hochberg procedure with a false discovery rate of 0.1 to determine significance after correction.
Discussion
The current study expands on prior findings of poorer EFs linked to higher weight status2,5,7,8 and factors influencing weight regulation in older children,2,11–14 by addressing these relationships in a large cohort of toddlers for each EF domain individually and as a composite score. The results suggest that associations between health behaviors and EFs may precede observed relationships between EFs and weight status. Toddlers meeting the guideline to limit screen time to no more than 1 hour per day had better inhibitory self-control and emergent metacognition, as well as overall EF. Lower total screen time also was predictive of higher overall EF and each domain of EF. Meeting the guideline to be physically active every d was associated with greater emergent metacognition. Although associations specific to meeting guidelines was abrogated on correction for multiple comparisons, this should be interpreted with caution, owing to the interest in individual testing of relationships between EFs and guidelines. Alternatively, this result may be simply a further indicator (aside from effect sizes) of the weaker association of EFs with guidelines compared with continuous variables, which had greater variability. Overall, these findings suggest that obesity risk factors are relevant, and that adherence to guidelines for daily physical activity and screen time limitations may be advantageous not only for weight regulation, but also for cognitive development.
Although much of the work surrounding EFs and weight status has focused on the causal relationship of the former on the latter, this relationship is likely to be birectional. Indeed, up-regulation of inflammatory cytokines and other obesity-associated biomarkers may have consequences for brain growth and development.31,32 A study of 9- to 11-year-olds showed that the relationship between increased BMI and lower EF was mediated by cortical thickness of the prefrontal cortex, the maturation of which has been linked to EF development.33 Despite these previous observations in older children, there was no association between weight status and any domain of EF in the current sample of toddlers; however, a high proportion of the current sample was of healthy weight at 24-moa. Post hoc power analyses revealed low power (17%) to detect an effect on overall EF, based on a Cohen d value of 0.110.
Therefore, our results may indicate that the relationship between greater weight status and EF emerges later in childhood; toddlers must rely heavily on their caregiver for dietary intake, but this reliance tends to decrease throughout childhood as they naturally become more independent. In this sample, toddlers of mothers with overweight or obesity prior to conception had higher WFLZ at 24-moa. Although noncausal, this may suggest a role for caregiver weight status on weight management in early childhood and may be a reflection of the relevance of family-wide interventions for promoting optimal health behaviors in young children. Longitudinal work in this area could elucidate the age at which relationships between EF and weight status emerge, and whether parent weight status and behaviors continue to track with child weight status throughout early life.
Although a priori covariates were implemented for regression analyses, we also explored other early-life associations with EF in an effort to promote the generalizability of our results, regardless of diet and delivery mode during infancy. Comparing groups who were exclusively breastfed to those who were formula-fed or mixed-fed at 3-moa revealed no significant differences in any domain of EF. In contrast, a recent study reported that each month of exclusive breastfeeding was associated with a decreased risk of clinically defined working memory deficit in 6-year-olds, even after adjusting for SES, among other factors; however, no relationship was found for inhibition or overall EF.34 It is possible that the relationship between breastfeeding and EF is not observable until the child is older (6 years vs 2 years). On the other hand, previous work in a large sample of infants (n = 11 134) suggested that the negative relationship of delivery via cesarean with cognitive outcomes may be rescued by age 3 years.35 Consistent with this work, our results showed no relationship between infant delivery mode and EF. The present study sample demonstrated an especially high proportion of exclusively breastfed infants at 3-moa (68%) and vaginally delivered infants (77%), whereas only 40% of infants aged <6 months are exclusively breastfed worldwide,36 and ~68% of children in the US are delivered vaginally.37 Considering this and the cross-sectional nature of the present study, longitudinal analyses exploring relationships of early-life feeding and delivery mode with EFs throughout childhood in a more diverse sample are needed.
Many parents and guardians in this sample reported toddler SSB intake, screen time, and physical activities in meeting AAP guidelines similar to previous findings in a national, cross-sectional analysis of the 2008 Feeding Infants and Toddlers Study (FITS) of >600 2-year-olds (defined as age 24–35.9 months). In the FITS, ~70% of the toddlers did not meet the recommended 5 servings of fruits and vegetables per day, ~55% consumed SSB on a daily basis, ~20% exceeded 2 hours of screen time per day, and only 30% engaged in active play outside for at least 1 hour per day.38 Our current sample yielded an especially low adherence rate (5%) for consumption of 5 servings of fruits and vegetables per day. Surprisingly, post hoc power analyses indicated that the power to detect a significant difference between those meeting and not meeting the guideline for fruits and vegetables for overall EF was likely sufficient (74.4%), based on a Cohen d of 0.301. However, no significant relationships were found between EFs and fruits and vegetable guideline or intake. Regardless, it is still possible that low adherence and lack of variability in the current sample impacted these findings, possibly owing to imprecise assessment in serving sizes for toddlers, given that the Block FFQ Ages 2–7 does not inquire about food serving sizes (only beverages). Furthermore, as young children tend to meet recommendations for daily fruit servings but not for vegetable servings (and especially nonstarchy vegetables),39 a less crude analysis of diet quality is likely required to detect an effect and should be considered in future analyses.
Even on inquiry of beverage portions, SSB also was not related to EFs, even though those meeting the guideline for SSB exhibited trend toward better EF. Many parents reported no intake of SSB, and those who did report intake of SBB reported very little (11.5 kcal/day). Recent NHANES data suggest that males and females aged 2–5 years consumed 65 kcal and 59 kcal from SSB daily, respectively, an average that is likely skewed by the older ages, because intake of SSB tends to increase across childhood age groups. Even for children aged 6–11 years, the daily kcal from SSB almost doubles, to 133 kcal in males and 104 kcal in females.40 Therefore, considering our highly educated sample of families and the young age of our sample, it is possible that these kcal estimations of SSB are fairly accurate but are not necessarily generalizable. Regardless of study limitations, the lack of relationship between diet and EF was surprising, given the evidence in older children showing relationships between SSB, fruit and vegetable intake, and diet quality (of which these are a hallmarks) and EF.14
Limiting screen time to no more than 60 minutes per day was not associated with cognitive flexibility, and the relationships with the other indices were not as strong as those with the continuous screen time variable. Although noncausal, this may indicate that more than 60 minutes of screen time by toddlers negatively impacted EF. Because the emotional control subscale overlaps for cognitive flexibility and inhibitory self-control, the lack of association between limiting screen time and cognitive flexibility also may indicate greater influence of the inhibition subscale in the relationship between screen time and inhibitory self-control (composed of inhibit and emotional control subscales). Mechanisms for the relationship between screen time and EFs are unclear, however. Nathanson and Fries proposed two mechanisms: one dependent on the specific content, some of which may alter the child’s perception of the social world (eg, fast-paced, fantasy television that requires and rewards inefficient information processing),12 and the other involves the indirect effect of screen time on EF through other behaviors. In fact, screen time has been negatively correlated with both physical activity and sleep time in toddlerhood.12,41
Our results showing greater working memory in toddlers who were more physically active supports observations that physical activity interventions can improve EF in school-aged children;13,38,42 however, these findings are novel in suggesting that this relationship begins in toddlerhood and may be specific to emergent metacognition. Physical activity has numerous health benefits relevant to development, including the up-regulation of important neurodevelopmental growth factors.43 In fact, magnetic resonance imaging studies comparing school-aged children, characterized by their fitness level and/or involvement in a physical activity intervention, exhibited functional44 and structural changes,45 respectively, in areas of the brain associated with EF, along with better performance on cognitive control tasks.
This sample of toddlers was a highly homogenous demographic representation, and future studies should aim to recruit a more ethnically and socioeconomically diverse sample. Given the greater risk for high screen use, obesity, low physical activity, and poor diet in children of non-Caucasian ethnicities/races and lower SES,46,47 this is especially important to address in future studies. Another limitation of the present study was the methods of assessment for physical activity and diet. Measurement of physical activity was through parental report of number of activities engaged in for at least 15 minutes per week. As a result, actual time spent doing physical activity could not be determined, and the actual AAP Bright Futures guideline for 60 minutes of moderate-to-vigorous physical activity per day could not be determined. Diet was assessed through FFQ, which introduces bias related to assumption of serving sizes and reliance on parent memory of diet over the last 6 months. Future work should aim to collect time spent doing physical activities and more precise measures of SSB, fruit, and vegetable intake.
Toddlers with less screen use who meet the AAP guidelines for both screen time and physical activity exhibited better EF, suggesting a potential role of these health behaviors in cognitive development. Based on observations in older children, these study results suggest that relationships between more sedentary and less active play with poorer EF emerges earlier in life compared with weight status. However, owing to the aforementioned limitations and the cross-sectional study design, these results should be interpreted with caution. In addition, a majority (67%) of toddlers met multiple guidelines, suggesting that health behaviors in toddlerhood tend to coincide. Future studies should explore interactions and coincidence of health behaviors, as well as their effects on EF development. Exploring the interplay of these factors and growth trajectories over time could be foundational to the understanding of their impact on early-life cognitive development. Regardless of limitations, this work is among the few studies to explore multiple EF domain relationships with weight status and health behaviors in a large sample of toddlers, emphasizing the need for future, robust studies to determine the significance of building healthy habits from a young age to promote early EF development.
Acknowledgments
This study was a subanalysis of the STRONG Kids 2 birth cohort study, which is funded by grants from the National Dairy Council (to S.D. and B.F.), the Gerber Foundation, (to S.D.), the Christopher Family Foundation (to S.D. and K.B.), and the National Institutes of Health (R01 DK107561, to S.D.) and Hatch Act funding from the US Department of Agriculture (USDA; ILLU 793-330, to B.F. and K.B.). A.M. was supported by a USDA National Needs fellowship (2017-09548) to the Division of Nutritional Sciences. The authors declare no conflicts of interest.
We thank the STRONG Kids 2 Team, Kelly Bost, Sharon Donovan, Soo-Yeun Lee, Brent McBride, Margarita Teran-Garcia, and Barbara H. Fiese, as well as the STRONG Kids 2 research assistants and participants.
Glossary
- 3-moa
3 months of age
- 24-moa
24 months of age
- AAP
American Academy of Pediatrics
- BMI
Body mass index
- BRIEF-P
Behavioral Rating Inventory of Executive Function for Preschoolers
- EF
Executive function
- FFQ
Food Frequency Questionnaire
- FITS
Feeding Infants and Toddlers Study
- SES
Socioeconomic status
- SPARK
Sports, Play, and Active Recreation for Kids
- SSB
Sugar-sweetened beverages
- WFLZ
Weight-for-length z-score
Footnotes
Portions of this study were presented as a poster during the American Academy for Nutrition meeting, June 7–10, 2021, virtual.
Data Statement
Data sharing statement available at www.jpeds.com.
References
- 1.Diamond A Executive functions. Annu Rev Psychol 2013;64:135–68. 10.1146/annurev-psych-113011-143750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang J, Matheson BE, Kaye WH, Boutelle KN. Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int J Obes (Lond) 2014;38:494–506. 10.1038/ijo.2013.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blair C, Razza RP. Relating effortful control, executive function, and false belief understanding to emerging math and literacy ability in kindergarten. Child Dev 2007;78:647–63. 10.1111/j.1467-8624.2007.01019.x [DOI] [PubMed] [Google Scholar]
- 4.Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc Natl Acad Sci U S A 2011;108:2693–8. 10.1073/pnas.1010076108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med 2009;163:297–302. 10.1001/archpediatrics.2008.579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graziano PA, Calkins SD, Keane SP. Toddler self-regulation skills predict risk for pediatric obesity. Int J Obes (Lond) 2010;34:633–41. 10.1038/ijo.2009.288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wirt T, Schreiber A, Kesztyüs D, Steinacker JM. Early life cognitive abilities and body weight: cross-sectional study of the association of inhibitory control, cognitive flexibility, and sustained attention with BMI percentiles in primary school children. J Obes 2015;2015:534651. 10.1155/2015/534651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li N, Yolton K, Lanphear BP, Chen A, Kalkwarf HJ, Braun JM. Impact of early-life weight status on cognitive abilities in children. Obesity (Silver Spring) 2018;26:1088–95. 10.1002/oby.22192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016;315:2292–9. 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hagan JF Jr., Shaw JS, Duncan PM, eds. Bright futures: guidelines for health supervision of infants, children, and adolescents. 4th ed. Elk Grove Village (IL): American Academy of Pediatrics; 2017. [Google Scholar]
- 11.Lillard AS, Peterson J. The immediate impact of different types of television on young children’s executive function. Pediatrics 2011;128:644–9. 10.1542/peds.2010-1919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nathanson AI, Fries PT. Television exposure, sleep time, and neuropsychological function among preschoolers. Media Psychol 2014;17:237–61. 10.1080/15213269.2014.915197 [DOI] [Google Scholar]
- 13.Hillman CH, Pontifex MB, Castelli DM, Khan N, Raine LBR, Scudder M, et al. Effects of the FITKids randomized controlled trial on executive control and brain function. Pediatrics 2014;134:e1063–71. 10.1542/peds.2013-3219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen JFW, Gorski MT, Gruber SA, Kurdziel LBF, Rimm EB. The effect of healthy dietary consumption on executive cognitive functioning in children and adolescents: a systematic review. Br J Nutr 2016;116:989–1000. 10.1017/S0007114516002877 [DOI] [PubMed] [Google Scholar]
- 15.Nelson CA 3rd, Zeanah CH, Fox NA, Marshall PJ, Smyke AT, Guthrie D. Cognitive recovery in socially deprived young children: the Bucharest Early Intervention Project. Science 2007;318:1937–40. 10.1126/science.1143921 [DOI] [PubMed] [Google Scholar]
- 16.Knickmeyer RC, Gouttard S, Kang C, Wilber K, Smith J, Hamer R, et al. A structural MRI study of human brain development from birth to 2 Years. J Neurosci 2008;28:12176–82. 10.1523/JNEUROSCI.3479-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fiese BH, Musaad S, Bost KK, McBride B, Lee S, Teran-Garcia M, et al. The STRONG Kids 2 birth cohort study: a cell-to-society approach to dietary habits and weight trajectories across the first 5 years of life. Curr Dev Nutr 2019;3:nzz007. 10.1093/cdn/nzz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Accessed September 6, 2019. https://www.who.int/publications/i/item/924154693X
- 19.Gioia GA, Espy KA, Isquith PK. Behavior Rating Inventory of Executive Function – pre-school version (BRIEF-P). Lutz (FL): Psychological Assessment Resources Inc; 2003. [Google Scholar]
- 20.Iwinski S, Donovan SM, Fiese B, Bost K. The impact of household chaos and dietary intake on executive function in young children. Nutrients 2021;13:4442. 10.3390/nu13124442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mckenzie TL, Sallis JF, Rosengard P. Beyond the stucco tower: design, development, and dissemination of the SPARK physical education programs. Quest 2009;61:114–27. 10.1080/00336297.2009.10483606 [DOI] [Google Scholar]
- 22.Common Sense Media. Zero to eight: children’s media use in America 2013. Accessed September 8, 2019. https://www.commonsensemedia.org/research/zero-to-eight-childrens-media-use-in-america-2013
- 23.Shealy KR, Scanlon KS, Labiner-Wolfe J, Fein SB, Grummer-Strawn LM. Characteristics of breastfeeding practices among US Mothers. Pediatrics 2008;122(Suppl 2):S50–5. 10.1542/peds.2008-1315f [DOI] [PubMed] [Google Scholar]
- 24.NutritionQuest, Assessment & Analysis Services. Questionnaires and screeners. Accessed August 28, 2019. https://www.nutritionquest.com/assessment/list-of-questionnaires-and-screeners/
- 25.US Department of Agriculture, Agricultural Research Service. Nutrient intakes from food and beverages: mean amounts consumed per individual, by gender and age. What We Eat in America, NHANES 2015–2016. 2018. Accessed June 29, 2022. https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/1516/tables_1-36_2015-2016.pdf
- 26.Rubin M When to adjust alpha during multiple testing: a consideration of disjunction, conjunction, and individual testing. Synthese 2021. 10.1007/s11229-021-03276-4 [DOI] [Google Scholar]
- 27.Kane SP. Post. ClinCalc Accessed July 2, 2022. https://clincalc.com/stats/Power.aspx. Updated November 10, 2018.
- 28.Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct Equation Model 2001;8:430–57. [PubMed] [Google Scholar]
- 29.Soper DS. Post-hoc statistical power calculator for multiple regression [Software]. 2022. Accessed June 29, 2022. https://www.danielsoper.com/statcalc
- 30.Cohen J Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 31.Shields GS, Moons WG, Slavich GM. Inflammation, self-regulation, and health: an immunologic model of self-regulatory failure. Perspect Psychol Sci 2017;12:588–612. 10.1177/1745691616689091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ronan L, Alexander-Bloch A, Fletcher PC. Childhood obesity, cortical structure, and executive function in healthy children. Cereb Cortex 2020;30:2519–28. 10.1093/cercor/bhz257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Khalaf SY, O’Neill SM, O’Keeffe LM, Henriksen TB, Kenny LC, Cryan JF, et al. The impact of obstetric mode of delivery on childhood behavior. Soc Psychiatry Psychiatr Epidemiol 2015;50:1557–67. 10.1007/s00127-015-1055-9 [DOI] [PubMed] [Google Scholar]
- 34.Keim SA, Sullivan JA, Sheppard K, Smith K, Ingol T, Boone KM, et al. Feeding infants at the breast or feeding expressed human milk: long-term cognitive, executive function, and eating behavior outcomes at age 6 years. J Pediatr 2021;233:66–73.e1. 10.1016/j.jpeds.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller AL, Lee HJ, Lumeng JC. Obesity-associated biomarkers and executive function in children. Pediatr Res 2015;77:143–7. 10.1038/pr.2014.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.UNICEF/WHO. Global Breast-feeding Scorecard, 2017. Global Breast-feeding Collective. 2017. Tracking progress for breastfeeding policies and programmes. Accessed June 29, 2022. https://www.who.int/publications/m/item/global-breastfeeding-scorecard-2017-tracking-progress-for-breastfeeding-policies-and-programmes
- 37.Centers for Disease Control and Prevention. National Center for Health Statistics. Method of delivery. 2020. Accessed June 29, 2022. https://www.cdc.gov/nchs/fastats/delivery.htm
- 38.Briefel RR, Deming DM, Reidy KC. Parents’ perceptions and adherence to children’s diet and activity recommendations: the 2008 feeding infants and toddlers study. Prev Chronic Dis 2015;12:E159. 10.5888/pcd12.150110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.US Department of Agriculture and US Department of Health and Human Services. Dietary guidelines for Americans, 2020–2025. Accessed June 29, 2022. https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials
- 40.Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened beverage consumption among U.S. youth, 2011–2014. NCHS Data Brief 2017:1–8. [PubMed] [Google Scholar]
- 41.Venetsanou F, Kambas A, Gourgoulis V, Yannakoulia M. Physical activity in pre-school children: trends over time and associations with body mass index and screen time. Ann Hum Biol 2019;46:393–9. 10.1080/03014460.2019.1659414 [DOI] [PubMed] [Google Scholar]
- 42.Álvarez-Bueno C, Pesce C, Cavero-Redondo I, Sánchez-López M, Martínez-Hortelano JA, Martínez-Vizcaíno V. The effect of physical activity interventions on children’s cognition and metacognition: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 2017;56:729–38. 10.1016/j.jaac.2017.06.012 [DOI] [PubMed] [Google Scholar]
- 43.Arvidsson D, Johannesson E, Andersen LB, Karlsson M, Wollmer P, Thorsson O, et al. A longitudinal analysis of the relationships of physical activity and body fat with nerve growth factor and brain-derived neural factor in children. J Phys Act Health 2018;15:620–5. 10.1123/jpah.2017-0483 [DOI] [PubMed] [Google Scholar]
- 44.Chaddock L, Hillman CH, Pontifex MB, Johnson CR, Raine LB, Kramer AF. Childhood aerobic fitness predicts cognitive performance one year later. J Sports Sci 2012;30:421–30. 10.1080/02640414.2011.647706 [DOI] [PubMed] [Google Scholar]
- 45.Chaddock-Heyman L, Erickson KI, Voss MW, Knecht AM, Pontifex MB, Castelli DM, et al. The effects of physical activity on functional MRI activation associated with cognitive control in children: a randomized controlled intervention. Front Hum Neurosci 2013;7:72. 10.3389/fnhum.2013.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Duch H, Fisher EM, Ensari I, Harrington A. Screen time use in children under 3 years old: a systematic review of correlates. Int J Behav Nutr Phys Act 2013;10:102. 10.1186/1479-5868-10-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep 2018;7:130–8. 10.1007/s13679-018-0301-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing statement available at www.jpeds.com.


