Key Points
Question
Is initiation of attention-deficit/hyperactivity disorder (ADHD) medication associated with a reduced mortality risk in individuals with ADHD?
Findings
In this observational, target trial emulation analysis that included 148 578 individuals diagnosed with ADHD in Sweden, initial dispensation of ADHD medication was significantly associated with lower all-cause (hazard ratio [HR], 0.79) and unnatural-cause (HR, 0.75) mortality, whereas the association with natural-cause mortality was not significant (HR, 0.86).
Meaning
Among individuals diagnosed with ADHD, medication initiation was significantly associated with lower mortality, in particular for unnatural causes.
Abstract
Importance
Attention-deficit/hyperactivity disorder (ADHD) is associated with increased risks of adverse health outcomes including premature death, but it is unclear whether ADHD pharmacotherapy influences the mortality risk.
Objective
To investigate whether initiation of ADHD pharmacotherapy was associated with reduced mortality risk in individuals with ADHD.
Design, Setting, and Participants
In an observational nationwide cohort study in Sweden applying the target trial emulation framework, we identified individuals aged 6 through 64 years with an incident diagnosis of ADHD from 2007 through 2018 and no ADHD medication dispensation prior to diagnosis. Follow-up started from ADHD diagnosis until death, emigration, 2 years after ADHD diagnosis, or December 31, 2020, whichever came first.
Exposures
ADHD medication initiation was defined as dispensing of medication within 3 months of diagnosis.
Main Outcomes and Measures
We assessed all-cause mortality within 2 years of ADHD diagnosis, as well as natural-cause (eg, physical conditions) and unnatural-cause mortality (eg, unintentional injuries, suicide, and accidental poisonings).
Results
Of 148 578 individuals with ADHD (61 356 females [41.3%]), 84 204 (56.7%) initiated ADHD medication. The median age at diagnosis was 17.4 years (IQR, 11.6-29.1 years). The 2-year mortality risk was lower in the initiation treatment strategy group (39.1 per 10 000 individuals) than in the noninitiation treatment strategy group (48.1 per 10 000 individuals), with a risk difference of −8.9 per 10 000 individuals (95% CI, −17.3 to −0.6). ADHD medication initiation was associated with significantly lower rate of all-cause mortality (hazard ratio [HR], 0.79; 95% CI, 0.70 to 0.88) and unnatural-cause mortality (2-year mortality risk, 25.9 per 10 000 individuals vs 33.3 per 10 000 individuals; risk difference, −7.4 per 10 000 individuals; 95% CI, −14.2 to −0.5; HR, 0.75; 95% CI, 0.66 to 0.86), but not natural-cause mortality (2-year mortality risk, 13.1 per 10 000 individuals vs 14.7 per 10 000 individuals; risk difference, −1.6 per 10 000 individuals; 95% CI, −6.4 to 3.2; HR, 0.86; 95% CI, 0.71 to 1.05).
Conclusions and Relevance
Among individuals diagnosed with ADHD, medication initiation was associated with significantly lower all-cause mortality, particularly for death due to unnatural causes.
This cohort study investigates whether the initiation of medication to treat patients with attention-deficit/hyperactivity disorder (ADHD) was associated with mortality.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is the most prevalent neurodevelopmental condition, affecting 5.9% of youths and 2.5% of adults worldwide, according to the 2021 World Federation of ADHD International Consensus Statement.1 In the US, the prevalence of ADHD is estimated to be 9.8% among children and adolescents2 and 4.4% among adults.3 The disorder is associated with a broad range of psychiatric and physical comorbidities, as well as adverse functional outcomes.4,5,6,7 Furthermore, individuals with ADHD have a 2-fold increased risk of premature death compared with those without it, mainly due to unnatural causes.8
Pharmacological treatment, including stimulant and nonstimulant medications, is recommended for both children and adults diagnosed with ADHD, alongside nonpharmacological treatment.9 Randomized controlled trials have demonstrated that ADHD medications are effective in reducing core ADHD symptoms. Pharmacoepidemiological studies have also shown reduced risks of negative outcomes, including injuries, traffic collisions, and criminality, which would be expected to decrease the mortality rate.10 However, there are concerns regarding the cardiovascular safety of ADHD medications, especially following long-term use, which could increase the mortality rate.11,12
To date, 3 studies have examined the association between ADHD medication and mortality with mixed results.13,14,15 These studies had important limitations, including a small number of deaths,13,14 indication bias (eg, starting methylphenidate in patients with depression or other debilitating conditions in their latest phase of life),15 no consideration of time-varying exposure,13,14,15 and absence of a control group.14 Importantly, no study has rigorously examined the association in adults with ADHD, which is a critical knowledge gap, given the increasing number of diagnoses and prescriptions for adults.1,16 Adults with ADHD have a higher prevalence of somatic comorbidities, including cardiovascular diseases17,18 and other conditions,5 compared with children and youths. Therefore, there is a need for population-based studies with long-term follow-up to investigate the association between ADHD medication use and mortality across the lifespan.
Using the Swedish national registers, we investigated whether initiation of ADHD medication was associated with mortality in children, youths, and adults with ADHD, using the target trial emulation approach to avoid key biases in pharmacoepidemiological studies.19
Methods
This study was approved by the Swedish Ethical Review Authority (reference number 2020-06540). Informed consent is not required for pseudoanonymized register-based research according to the Swedish law.
Study Cohort
Data were obtained from multiple Swedish national registries (eMethods in Supplement 1). We identified all individuals aged 6 through 64 years residing in Sweden with an incident diagnosis of ADHD (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10], F90) from January 1, 2007, through December 31, 2018. In Sweden, those displaying ADHD symptoms undergo a thorough neuropsychiatric assessment before receiving a specialist diagnosis. To obtain a cohort naive to medication before cohort entry, we only included individuals without any ADHD medication dispensation for at least 18 months before the diagnosis (Figure 1). We followed up the cohort from diagnosis of ADHD (baseline) until death, emigration, 2 years after baseline, or December 31, 2020, whichever came first. In a sensitivity analysis, we extended the maximum follow-up to 5 years. In this cohort, we used the target trial emulation approach19 to evaluate the effect of ADHD medication initiation on risk of all-cause and cause-specific mortality. Table 1 summarizes the protocol of the target trial (eMethods in Supplement 1).
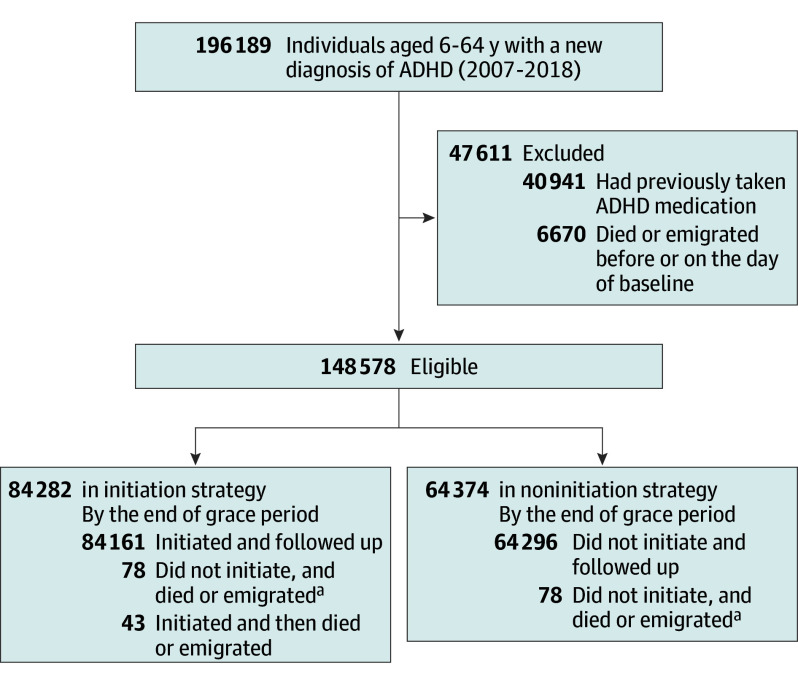
Figure 1. Flowchart of the Cohort Selection.
aThe 78 individuals who died or emigrated during the grace period contributed to both treatment strategies to avoid immortal-time bias.
ADHD indicates attention-deficit/hyperactivity disorder.
Table 1. Protocol of a Target Trial on ADHD Medication on Mortality in Individuals With ADHD and Emulation Using Observational Data.
| Protocol component | Target randomized trial | Emulation using observational data |
|---|---|---|
| Eligibility criteria |
|
|
| Treatment strategies |
|
|
| Assignment procedures | Eligible individuals are randomly assigned to either strategy at baseline and are aware of the assigned strategy | Randomization is emulated by cloning eligible individuals and assigning each copy to 1 treatment strategy |
| Follow-up period | Follow-up starts at treatment assignment and ends at death, loss to follow-up (emigration), or administrative end of follow-up (December 31, 2020, or 2 years after baseline), whichever occurs first | Same as the target trial |
| Outcomes | All-cause and cause-specific mortality within 2 years after baseline | Same as the target trial |
| Causal contrasts of interest | Effect of adhering to the treatment strategies (per protocol) during follow-up | Observational analogue of the per-protocol effect |
| Analysis plan | Effect estimates are calculated from an inverse probability-weighted, pooled-logistic regression model, with censoring at deviation from the protocol and adjustment for baseline and postbaseline covariates | Same as the target trial, except that the analyses are conducted in an expanded data set that includes copies of each eligible individual |
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
Measurements
Exposure
We identified all 6 medications licensed for ADHD treatment in Sweden (methylphenidate, amphetamine, dexamphetamine, lisdexamfetamine, atomoxetine, and guanfacine) during the 2007-2020 period (eTable 1 in Supplement 1). The exposure was initiation of medication, defined as dispensation of any ADHD medication within 3 months of diagnosis (ie, grace period).20
Outcomes
The main outcomes were all-cause and cause-specific mortality during a 2-year follow-up period. Specific causes of death were categorized into natural (eg, physical conditions; ICD-10 codes, A00-R99 and U07) and unnatural causes (eg, suicide, accidental injuries, accidental poisoning, and other external injuries; ICD-10 codes, S00-T98 and V01-Y98) according to the underlying cause of death.21 We also examined specific unnatural causes including suicide, accidental injuries, and accidental poisoning (eTable 2 in Supplement 1). Accidental poisoning involves unintentional exposure to harmful substances, whereas suicide entails deliberate self-harm with the intent to end one’s life. In sensitivity analysis and subgroup analysis, the 5-year mortality and sex- and age-specific associations were also assessed.
Covariates
Baseline covariates included age at ADHD diagnosis; calendar year of baseline; sex; birth country; highest educational level; diagnosis of mental disorders (ie, anxiety disorder, autism spectrum disorder, bipolar disorder, conduct disorder, depressive disorder, eating disorder, intellectual disability, personality disorder, schizophrenia, alcohol use disorder, tobacco use disorder, and drug use disorder); physical diseases (ie, cardiovascular disease, epilepsy, type 2 diabetes, hyperlipidemia); suicide attempt and external injuries (eTable 3 in Supplement 1); dispensation of other psychotropic medications (Anatomical Therapeutic Chemical [ATC] codes, antipsychotics [N05A]; anxiolytics, hypnotics, and sedatives [N05B, N05C]; antidepressants [N06A]; antiepileptic drugs [N03A]; antiaddiction drugs [N07B]; and opioid [N02A]); and number of outpatient visits and hospitalizations for psychiatric and nonpsychiatric reasons (eMethods in Supplement 1). Time-varying covariates included the above mentioned diagnoses, dispensations, any outpatient visit or hospitalization for psychiatric and nonpsychiatric reasons in the previous month.
Statistical Analyses
The 2 treatment strategies considered in our main analysis were initiating ADHD medication within 3 months after diagnosis and continuing the prescribed medication vs not initiating ADHD medication during the follow-up. We therefore estimated the observational analogs of per-protocol effects.22 We focused on the effect of sustained treatment with ADHD medication because deviations from the initially assigned treatment strategies were common. We implemented a 3-step approach comprising cloning, censoring, and inverse-probability weighting (eMethods in Supplement 1)19,23 to compare the mortality rate between the 2 treatment strategies. First, in the cloning step, we created a data set with 2 copies (clones) of each eligible individual and assigned each of the copies to 1 of the treatment strategies at the start of follow-up. Second, in the censoring step, we assessed whether copies had adhered to their assigned treatment strategy at monthly intervals. For example, participants assigned to the initiation group were censored at the third month if they did not redeem any dispensation of ADHD medication during the grace period or were censored at the month when they discontinued ADHD medication treatment or switched to another ADHD medication after the grace period. In contrast, participants assigned to the noninitiation group were censored at the month when they redeemed an ADHD medication dispensation. Finally, in the weighting step, each individual received time-varying inverse probability weights of remaining uncensored at each month24 to adjust for potential selection bias induced by this artificial censoring. To estimate the weights, we fitted a pooled logistic regression model for each treatment strategy separately, including an indicator for time (with cubic splines) and the above mentioned time-fixed and time-varying covariates. Model coefficients for remaining uncensored in each treatment strategy are shown in eTable 4 in Supplement 1.
To evaluate whether the weighting step achieved a good covariate balance between groups, we calculated the standardized mean differences (SMDs) for all confounders at the end of the grace period. We fitted an inverse probability weighted discrete-time hazard model using pooled logistic regression.25 In this model, the outcome was regressed on treatment and time, providing an approximation of the hazard ratio (HR). When analyzing cause-specific mortality, we treated the competing event as a censoring event to estimate the cause-specific HRs rather than fitting competing risk models (eMethods in Supplement 1). To estimate the mortality risk at each month, we conducted an outcome regression with treatment, time, and treatment-time interaction as independent variables. We used a nonparametric bootstrap with 500 samples to compute the 95% CIs.
We further performed stratified analyses by age (children and youths [6-24 years], adults [≥25 years]) and by sex. Additionally, we extended the follow-up period from 2 years to 5 years to examine longer-term associations.
To test the robustness of our findings, we conducted 5 sensitivity analyses. First, we used a 2-week interval to more precisely model the time-varying censoring weights. Second, we compared 2 less restricted treatment strategies: initiating ADHD medication within 3 months after diagnosis vs not initiating ADHD medication during the grace period, irrespective of deviations from the assigned treatment strategies after the grace period. Third, we calculated the hazard without excluding competing events by estimating a cause-specific cumulative incidence as absolute risk based on the subdistribution function and related subdistribution HRs. This approach allows the change in risk for competing events among those who initiated treatment to also change the risk for the outcome of interest.26 Fourth, we emulated a head-to-head trial comparing the effectiveness of stimulants with nonstimulants on all-cause mortality. Finally, we conducted a case-crossover analysis27 to address unmeasured confounding using a different design based on alternative assumptions than the main analysis. All individuals who died during the follow-up were included in this analysis, and the exposure status at the time of the death (case period) was compared with the exposure status at other times before death (control periods) within individual, with adjustment for time-varying covariates (eMethods in Supplement 1). This method controls for all time-invariant confounders within individual (even unmeasured, eg, genetic factors) by design because each case serves as its own control.
Our study followed the Reporting of Studies Conducted Using Observational Routinely Collected Health Data–Pharmacoepidemiological Research (RECORD-PE) guideline.28 Data management was performed using SAS, version 9.4 (SAS Institute Inc). Statistical analyses were conducted with R, version 4.0.5 (R Foundation for Statistical Computing). A 2-sided P value <.05 was considered statistically significant.
Results
We identified 148 578 eligible individuals with incident ADHD diagnosis (61 356 females [41.3%]; 87 222 males [58.7%]; Table 2 and Figure 1). The median age at baseline was 17.4 years (interquartile range, 11.6-29.1 years). A total of 632 individuals died during the 2-year follow-up, and 1402 died during the 5-year follow-up. The primary causes of death are listed in eTable 2 in Supplement 1, with more than half of the deaths due to unnatural causes (66.7%).
Table 2. Characteristics of the Study Cohort at Baseline and at the End of 3-Month Grace Period (Before and After Weighting).
| Characteristics | Total cohort (N = 148 578)a | Before weightingb | After weightingb | |||||
|---|---|---|---|---|---|---|---|---|
| Initiation (n = 84 161) |
Noninitiation (n = 64 296) | SMD | Initiation (n = 148 221.8) | Noninitiation (n = 158 223.7) | SMD | |||
| Age at baseline, median (IQR), y | 17.4 (11.6-29.1) | 16.4 (11.5-27.8) | 19.1 (11.9-30.6) | 0.14 | 16.6 (11.6-28.2) | 17.8 (11.3-28.5) | 0.02 | |
| Sex, No. (%) | ||||||||
| Female | 61 356 (41.3) | 34 596 (41.1) | 26 721 (41.6) | 0.01 | 61 968.0 (41.8) | 65 186.7 (41.2) | 0.01 | |
| Male | 87 222 (58.7) | 49 565 (58.9) | 37 575 (58.4) | 86 253.8 (58.2) | 93 037.0 (58.8) | |||
| Year of diagnosis, No. (%) | ||||||||
| 2007 | 4771 (3.2) | 2119 (2.5) | 2645 (4.1) | 0.14 | 4143.1 (2.8) | 5216.7 (3.3) | 0.05 | |
| 2008 | 6500 (4.4) | 3080 (3.7) | 3414 (5.3) | 5797.7 (3.9) | 7064.6 (4.5) | |||
| 2009 | 7961 (5.4) | 4212 (5.0) | 3745 (5.8) | 7433.3 (5.0) | 8547.4 (5.4) | |||
| 2010 | 9842 (6.6) | 5516 (6.6) | 4315 (6.7) | 9511.2 (6.4) | 10 611.3 (6.7) | |||
| 2011 | 11 552 (7.8) | 6765 (8.0) | 4773 (7.4) | 11 363.8 (7.7) | 12 125.3 (7.7) | |||
| 2012 | 12 709 (8.6) | 7279 (8.6) | 5415 (8.4) | 12 502.5 (8.4) | 13 510.3 (8.5) | |||
| 2013 | 13 272 (8.9) | 7624 (9.1) | 5640 (8.8) | 13 275.7 (9.0) | 14 053.7 (8.9) | |||
| 2014 | 14 463 (9.7) | 8382 (10.0) | 6066 (9.4) | 14 764.2 (10.0) | 15 184.6 (9.6) | |||
| 2015 | 15 707 (10.6) | 9193 (10.9) | 6505 (10.1) | 16 156.5 (10.9) | 16 493.4 (10.4) | |||
| 2016 | 16 508 (11.1) | 9337 (11.1) | 7159 (11.1) | 16 827.3 (11.4) | 17 785.3 (11.2) | |||
| 2017 | 17 223 (11.6) | 9926 (11.8) | 7290 (11.3) | 17 705.5 (11.9) | 18 290.1 (11.6) | |||
| 2018 | 18 070 (12.2) | 10 728 (12.7) | 7329 (11.4) | 18 741.0 (12.6) | 19 340.9 (12.2) | |||
| Birth country, No. (%) | ||||||||
| Sweden | 136 951 (92.2) | 78 101 (92.8) | 58 752 (91.4) | 0.05 | 137 051.8 (92.5) | 146 119.8 (92.4) | <0.01 | |
| Otherc | 11 627 (7.8) | 6060 (7.2) | 5544 (8.6) | 11 170.0 (7.5) | 12 103.9 (7.6) | |||
| Educational level at baseline, No. (%)d | ||||||||
| Primary or lower secondary | 24 783 (16.7) | 12 753 (15.2) | 12 010 (18.7) | 0.11 | 23 697.5 (16.0) | 26 401.1 (16.7) | 0.02 | |
| Upper secondary | 75 253 (50.6) | 42 936 (51.0) | 32 262 (50.2) | 75 071.6 (50.6) | 79 839.7 (50.5) | |||
| Postsecondary or postgraduate | 47 341 (31.9) | 27 920 (33.2) | 19 395 (30.2) | 48 399.9 (32.7) | 50 784.9 (32.1) | |||
| Unknown | 1201 (0.8) | 552 (0.7) | 629 (1.0) | 1052.8 (0.7) | 1198.0 (0.8) | |||
| Comorbidities at baseline, No. (%) | ||||||||
| Accidental injuries | 85 994 (57.9) | 48 966 (58.2) | 36 943 (57.5) | 0.01 | 86 189.0 (58.1) | 91 416.2 (57.8) | 0.01 | |
| Depressive disorder | 28 353 (19.1) | 15 092 (17.9) | 13 220 (20.6) | 0.07 | 27 507.9 (18.6) | 30 045.7 (19.0) | 0.01 | |
| Nonalcohol drug use disorder | 12 906 (8.7) | 6207 (7.4) | 6651 (10.3) | 0.1 | 11 907.2 (8.0) | 13 602.0 (8.6) | 0.02 | |
| Suicide attempt history | 12 453 (8.4) | 6332 (7.5) | 6083 (9.5) | 0.07 | 11 723.8 (7.9) | 13 171.2 (8.3) | 0.02 | |
| Alcohol use disorder | 12 347 (8.3) | 6138 (7.3) | 6170 (9.6) | 0.08 | 11 476.9 (7.7) | 12 921.8 (8.2) | 0.02 | |
| Anxiety disorders | 11 940 (8.0) | 6028 (7.2) | 5896 (9.2) | 0.07 | 11 300.2 (7.6) | 12 473.3 (7.9) | 0.01 | |
| Personality disorders | 7231 (4.9) | 3394 (4.0) | 3823 (5.9) | 0.09 | 6580.2 (4.4) | 7569.4 (4.8) | 0.02 | |
| Bipolar disorder | 5137 (3.5) | 2546 (3.0) | 2582 (4.0) | 0.05 | 4710.8 (3.2) | 5372.9 (3.4) | 0.01 | |
| Cardiovascular disease | 5000 (3.4) | 2232 (2.7) | 2752 (4.3) | 0.09 | 4317.9 (2.9) | 5284.2 (3.3) | 0.02 | |
| Autism spectrum disorder | 4765 (3.2) | 2279 (2.7) | 2484 (3.9) | 0.06 | 4314.4 (2.9) | 4720.2 (3.0) | <0.01 | |
| Epilepsy | 3119 (2.1) | 1321 (1.6) | 1793 (2.8) | 0.08 | 2682.2 (1.8) | 3291.7 (2.1) | 0.02 | |
| Eating disorder | 3053 (2.1) | 1622 (1.9) | 1430 (2.2) | 0.02 | 3009.1 (2.0) | 3172.2 (2.0) | <0.01 | |
| Schizophrenia | 2401 (1.6) | 966 (1.1) | 1423 (2.2) | 0.08 | 1992.8 (1.3) | 2433.2 (1.5) | 0.02 | |
| Conduct disorder | 2271 (1.5) | 1378 (1.6) | 892 (1.4) | 0.02 | 2358.0 (1.6) | 2377.0 (1.5) | 0.01 | |
| Intellectual disability | 2268 (1.5) | 963 (1.1) | 1303 (2.0) | 0.07 | 1894.4 (1.3) | 2258.0 (1.4) | 0.01 | |
| Type 2 diabetes | 1092 (0.7) | 453 (0.5) | 634 (1.0) | 0.05 | 874.9 (0.6) | 1165.6 (0.7) | 0.02 | |
| Dyslipidemia | 570 (0.4) | 253 (0.3) | 315 (0.5) | 0.03 | 492.3 (0.3) | 619.6 (0.4) | 0.01 | |
| Tobacco use disorder | 562 (0.4) | 243 (0.3) | 316 (0.5) | 0.03 | 479.1 (0.3) | 574.8 (0.4) | 0.01 | |
| Psychotropic medication use at baseline, No. (%) | ||||||||
| Antidepressants | 51 568 (34.7) | 27 689 (32.9) | 23 810 (37.0) | 0.09 | 49 970.7 (33.7) | 54 534.2 (34.5) | 0.02 | |
| Anxiolytics, hypnotics, or sedatives | 42 503 (28.6) | 23 152 (27.5) | 19 291 (30.0) | 0.06 | 41 487.2 (28.0) | 44 986.8 (28.4) | 0.01 | |
| Opioidse | 30 541 (20.6) | 16 909 (20.1) | 13 583 (21.1) | 0.03 | 29 664.1 (20.0) | 32 284.7 (20.4) | 0.01 | |
| Antipsychotics | 14 915 (10.0) | 7454 (8.9) | 7420 (11.5) | 0.09 | 13 840.8 (9.3) | 15 529.5 (9.8) | 0.02 | |
| Antiepileptic drugs | 10 786 (7.3) | 5203 (6.2) | 5562 (8.7) | 0.09 | 9854.6 (6.6) | 11 376.7 (7.2) | 0.02 | |
| Antiaddiction drugsf | 7612 (5.1) | 3901 (4.6) | 3682 (5.7) | 0.05 | 7027.0 (4.7) | 8036.1 (5.1) | 0.02 | |
| No. of prior outpatient visits for psychiatry, No. (%) | ||||||||
| 0 | 65 697 (44.2) | 36 280 (43.1) | 29 384 (45.7) | 0.14 | 65 253.9 (44.0) | 71 316.0 (45.1) | 0.03 | |
| 1-4 | 47 624 (32.1) | 29 139 (34.6) | 18 448 (28.7) | 48 998.7 (33.1) | 50 201.7 (31.7) | |||
| 5-9 | 18 185 (12.2) | 9937 (11.8) | 8231 (12.8) | 17 739.5 (12.0) | 18 949.4 (12.0) | |||
| ≥10 | 17 072 (11.5) | 8805 (10.5) | 8233 (12.8) | 16 229.7 (10.9) | 17 756.7 (11.2) | |||
| No. of prior hospitalizations for psychiatry, No. (%) | ||||||||
| 0 | 122 280 (82.3) | 71 764 (85.3) | 50 471 (78.5) | 0.18 | 124 265.3 (83.8) | 131 025.9 (82.8) | 0.03 | |
| 1-2 | 17 072 (11.5) | 8294 (9.9) | 8742 (13.6) | 15 846.7 (10.7) | 17 676.5 (11.2) | |||
| 3-4 | 3946 (2.7) | 1815 (2.2) | 2112 (3.3) | 3516.3 (2.4) | 4101.9 (2.6) | |||
| ≥5 | 5280 (3.6) | 2288 (2.7) | 2971 (4.6) | 4593.5 (3.1) | 5419.4 (3.4) | |||
| No. of prior outpatient visits for nonpsychiatric reason. No. (%) | ||||||||
| 0 | 25 214 (17.0) | 14 108 (16.8) | 11 079 (17.2) | 0.05 | 24 824.9 (16.7) | 26 758.0 (16.9) | 0.01 | |
| 1-4 | 65 021 (43.8) | 37 493 (44.5) | 27 485 (42.7) | 65 506.0 (44.2) | 69 221.2 (43.7) | |||
| 5-9 | 31 921 (21.5) | 18 242 (21.7) | 13 656 (21.2) | 31 997.4 (21.6) | 34 082.2 (21.5) | |||
| ≥10 | 26 422 (17.8) | 14 318 (17.0) | 12 076 (18.8) | 25 893.5 (17.5) | 28 162.3 (17.8) | |||
| No. of prior hospitalizations for nonpsychiatric reason, (No.%) | ||||||||
| 0 | 78 959 (53.1) | 46 359 (55.1) | 32 563 (50.6) | 0.13 | 80 454.5 (54.3) | 84 263.3 (53.3) | 0.03 | |
| 1-2 | 48 693 (32.8) | 27 438 (32.6) | 21 213 (33.0) | 48 472.2 (32.7) | 51 725.0 (32.7) | |||
| 3-4 | 11 737 (7.9) | 6136 (7.3) | 5583 (8.7) | 11 182.5 (7.5) | 12 496.3 (7.9) | |||
| ≥5 | 9189 (6.2) | 4228 (5.0) | 4937 (7.7) | 8112.6 (5.5) | 9739.1 (6.2) | |||
| Time-varying covariates during the previous month, No. (%) | ||||||||
| Depressive disorder | 2475 (1.7) | 1908 (2.3) | 1547 (2.4) | 0.01 | 3506.1 (2.4) | 3483.8 (2.2) | 0.01 | |
| Accidental injuries | 2412 (1.6) | 1099 (1.3) | 929 (1.4) | 0.01 | 2014.0 (1.4) | 2115.8 (1.3) | <0.01 | |
| Other drug use disorder | 1295 (0.9) | 745 (0.9) | 811 (1.3) | 0.04 | 1471.0 (1.0) | 1601.5 (1.0) | <0.01 | |
| Anxiety disorders | 797 (0.5) | 910 (1.1) | 756 (1.2) | 0.01 | 1690.9 (1.1) | 1592.7 (1.0) | 0.01 | |
| Autism spectrum disorder | 765 (0.5) | 2060 (2.4) | 1396 (2.2) | 0.02 | 3543.3 (2.4) | 2955.2 (1.9) | 0.04 | |
| Alcohol use disorder | 730 (0.5) | 419 (0.5) | 417 (0.6) | 0.02 | 793.0 (0.5) | 813.6 (0.5) | <0.01 | |
| Bipolar disorder | 708 (0.5) | 654 (0.8) | 692 (1.1) | 0.03 | 1279.2 (0.9) | 1413.2 (0.9) | <0.01 | |
| Personality disorders | 617 (0.4) | 591 (0.7) | 541 (0.8) | 0.02 | 1133.2 (0.8) | 1089.1 (0.7) | 0.01 | |
| Suicide attempt history | 570 (0.4) | 152 (0.2) | 160 (0.2) | 0.01 | 302.4 (0.2) | 306.1 (0.2) | <0.01 | |
| Cardiovascular disease | 254 (0.2) | 105 (0.1) | 212 (0.3) | 0.04 | 210.1 (0.1) | 377.1 (0.2) | 0.02 | |
| Eating disorder | 254 (0.2) | 170 (0.2) | 191 (0.3) | 0.02 | 315.2 (0.2) | 412.5 (0.3) | 0.01 | |
| Conduct disorder | 248 (0.2) | 420 (0.5) | 167 (0.3) | 0.04 | 651.9 (0.4) | 417.6 (0.3) | 0.03 | |
| Epilepsy | 234 (0.2) | 92 (0.1) | 182 (0.3) | 0.04 | 192.9 (0.1) | 321.4 (0.2) | 0.02 | |
| Schizophrenia | 215 (0.1) | 93 (0.1) | 160 (0.2) | 0.03 | 197.7 (0.1) | 281.7 (0.2) | 0.01 | |
| Intellectual disability | 188 (0.1) | 273 (0.3) | 218 (0.3) | <0.01 | 500.9 (0.3) | 404.8 (0.3) | 0.02 | |
| Type 2 diabetes | 64 (<0.1) | 18 (<0.1) | 46 (0.1) | 0.02 | 40.2 (<0.1) | 80.1 (0.1) | 0.01 | |
| Tobacco use disorder | 16 (<0.1) | 9 (<0.1) | 17 (<0.1) | 0.01 | 19.3 (<0.1) | 36.9 (<0.1) | 0.01 | |
| Dyslipidemia | 14 (<0.1) | 13 (<0.1) | 14 (<0.1) | <0.01 | 26.0 (<0.1) | 32.8 (<0.1) | <0.01 | |
| Antidepressants | 6103 (4.1) | 4239 (5.0) | 3776 (5.9) | 0.04 | 7753.8 (5.2) | 8518.7 (5.4) | 0.01 | |
| Anxiolytics, hypnotics, or sedatives | 3033 (2.0) | 2077 (2.5) | 1443 (2.2) | 0.01 | 3614.5 (2.4) | 3230.8 (2.0) | 0.03 | |
| Opioids | 2441 (1.6) | 1182 (1.4) | 1119 (1.7) | 0.03 | 2150.1 (1.5) | 2489.0 (1.6) | 0.01 | |
| Antipsychotics | 1829 (1.2) | 1309 (1.6) | 1280 (2.0) | 0.03 | 2478.1 (1.7) | 2612.9 (1.7) | <0.01 | |
| Antiepileptic drugs | 1134 (0.8) | 689 (0.8) | 936 (1.5) | 0.06 | 1377.1 (0.9) | 1928.6 (1.2) | 0.03 | |
| Antiaddiction drugs | 418 (0.3) | 265 (0.3) | 213 (0.3) | <0.01 | 493.2 (0.3) | 439.5 (0.3) | 0.01 | |
| Any outpatient visit for psychiatry | 145 666 (98.0) | 23 607 (28.0) | 9961 (15.5) | 0.31 | 38 536.7 (26.0) | 23 667.8 (15.0) | 0.28 | |
| Any hospitalizations for psychiatry | 5258 (3.5) | 665 (0.8) | 769 (1.2) | 0.04 | 1331.2 (0.9) | 1430.8 (0.9) | <0.01 | |
| Any outpatient visit for nonpsychiatric reason | 12 428 (8.4) | 4236 (5.0) | 3574 (5.6) | 0.02 | 7702.1 (5.2) | 8040.5 (5.1) | 0.01 | |
| Any hospitalizations for nonpsychiatric reason | 2472 (1.7) | 479 (0.6) | 547 (0.9) | 0.03 | 930.0 (0.6) | 1090.5 (0.7) | 0.01 | |
Abbreviation: SMD, standardized mean difference.
Assessed at baseline.
Assessed at the end of the grace period when each individual’s treatment strategy was completely determined. The n denotes the absolute number of individuals before or after applying the inverse probability weighting.
Including all countries other than Sweden, the information was extracted from Statistics Sweden.
For those younger than 25 years, educational level was replaced by parents’ highest educational level.
Refers to prescribed opioids in the prescription drug register.
Including drugs used in nicotine dependence, drugs used in alcohol dependence, and drugs used in opioid dependence.
Within 3 months of an ADHD diagnosis, 84 204 individuals (56.7%) initiated and 64 296 (43.3%) did not initiate ADHD medication treatment. The remaining 78 individuals who died or emigrated during the grace period contributed to both treatment strategies to avoid immortal-time bias. The characteristics in each treatment strategy at the end of the grace period before and after weighting are shown in Table 2. The inverse probability weighting showed a balance of the covariates (SMD <0.1),29 except for any outpatient visit for psychiatric reason (SMD = 0.28), which was further adjusted in the outcome regression models.
The crude 2-year mortality rate was lower among those who initiated ADHD medication (17.3 per 10 000 individuals) compared with those who did not initiate medication (31.8 per 10 000). The adjusted cumulative incidence curve of all-cause mortality is shown in eFigure 1 in Supplement 1. During the 2-year follow-up period, ADHD medication initiation was associated with statistically significantly lower rate of all-cause (weighted 2-year mortality risk, 39.1 vs 48.1 per 10 000; risk difference, −8.9 per 10 000; 95% CI, −17.3 to −0.6; HR, 0.79; 95% CI, 0.70 to 0.88) and unnatural-cause mortality (2-year mortality risk, 25.9 vs 33.3 per 10 000; risk difference,−7.4 per 10 000; 95% CI, −14.2 to −0.5; HR, 0.75; 95% CI, 0.66 to 0.86), but not for natural-cause mortality (2-year mortality risk, 13.1 vs 14.7 per 10 000; risk difference, −1.6 per 10 000; 95% CI, −6.4 to 3.2; HR, 0.86; 95% CI, 0.71 to 1.05; Figure 2). In the analyses of specific unnatural causes of death, a significantly lower risk, following ADHD medication initiation, in death due to accidental poisoning, was observed (2-year mortality risk, 6.0 vs 12.1 per 10 000; risk difference, −6.0 per 10 000; 95% CI, −9.8 to −2.3; HR, 0.47; 95% CI, 0.36 to 0.60).
Figure 2. Association Between ADHD Medication Initiation and 2-Year Mortality Among Individuals With ADHD.
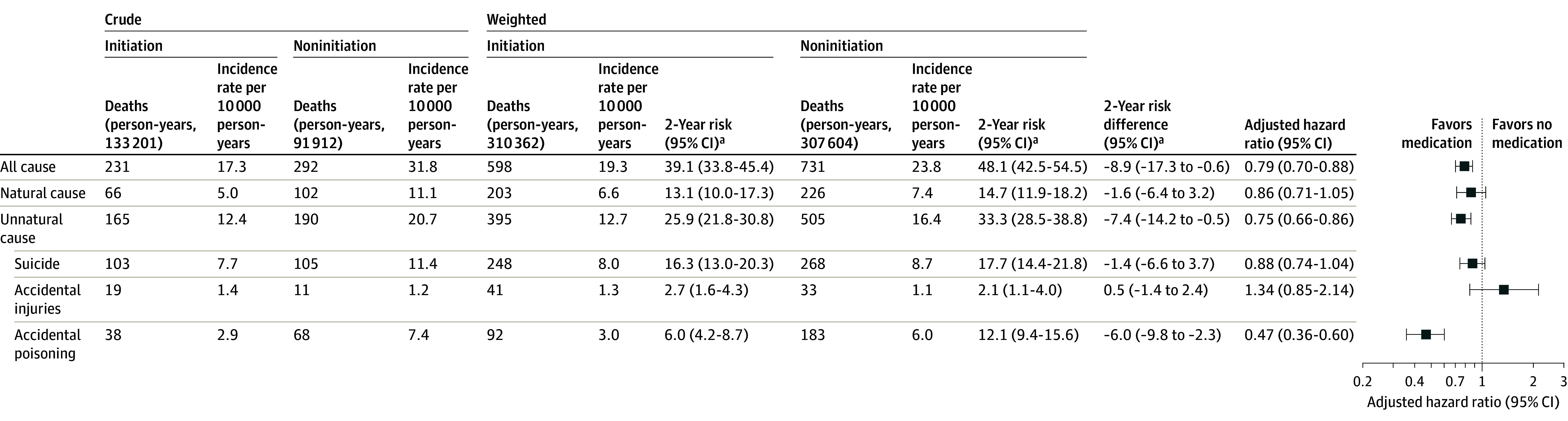
Natural-cause mortality among those diagnosed with attention-deficit/hyperactivity disorder (ADHD) included death from somatic diseases and medical conditions (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10], A00-R99, U07) and unnatural-cause mortality included death from suicide, accidental injuries, accidental poisoning, and other external injuries (ICD-10 codes, S00-T98, V01-Y98).
aTwo-year absolute risk and 2-year risk difference were calculated per 10 000 individuals.
In subgroup analyses (Figure 3), we found ADHD medication initiation was significantly associated with lower rate of all-cause and unnatural-cause mortality in children and youths (6-24 years old), adults (25-64 years), and in males. In the study cohort, females with ADHD had lower mortality risk for both natural (5.9 per 10 000) and unnatural causes (9.3 per 10 000) than males (8.5 per 10 000 for natural cause and 20.2 per 10 000 for unnatural cause), and ADHD medication initiation was only associated with lower rate of natural-cause mortality in females (2-year mortality risk, 8.5 vs 12.9 per 10 000; risk difference, −4.4 per 10 000; 95% CI, −10.8 to 1.9; HR, 0.64; 95% CI, 0.45 to 0.90). When extending the follow-up to 5 years, the associations attenuated for most outcomes but remained statistically significant for unnatural-cause mortality (5-year mortality risk, 66.5 vs 70.5 per 10 000; risk difference, −4.0 per 10 000; 95% CI, −17.2 to 9.2; HR, 0.89; 95% CI, 0.81 to 0.97; eTable 5 in Supplement 1).
Figure 3. Association Between ADHD Medication Initiation and 2-Year Mortality Among Individuals With ADHD Stratified by Age and Sex.
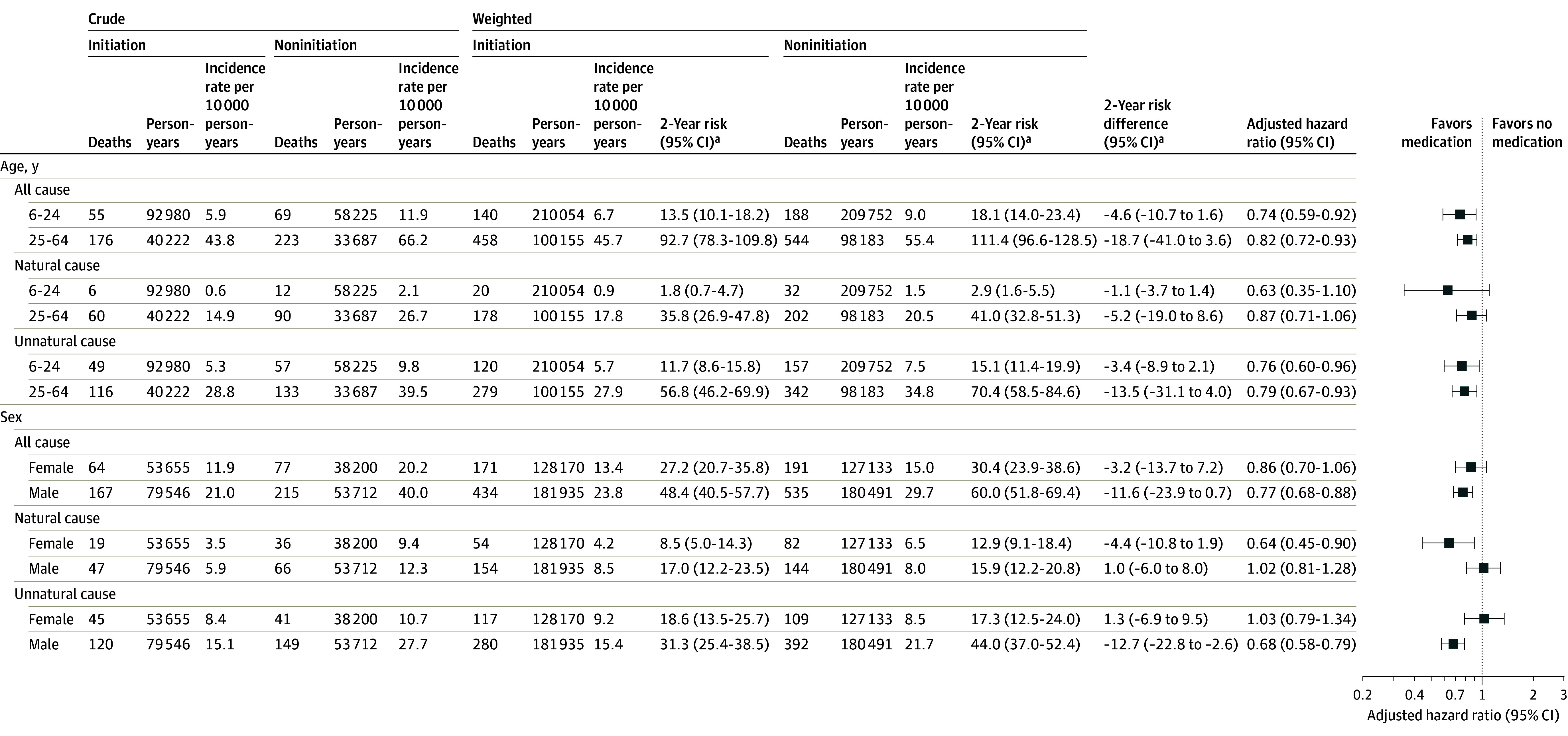
Natural-cause mortality among those diagnosed with attention-deficit/hyperactivity disorder (ADHD) included death from somatic diseases and medical conditions (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] codes, A00-R99, U07) and unnatural-cause mortality included suicide, accidental injuries, accidental poisoning, and other external injuries (ICD-10 codes, S00-T98, V01-Y98).
aTwo-year absolute risk and 2-year risk difference were calculated per 10 000 individuals.
In sensitivity analysis, we found similar results when using 2 weeks as a time interval for analyses requiring adherence to the treatment strategies during the entire follow-up period (eTable 6 in Supplement 1) and when ignoring deviations from the assigned treatment strategies after the grace period (HR for all-cause mortality was 0.82 compared with 0.79 from the main analysis; eTable 7 in Supplement 1). A different approach addressing competing risks yielded comparable results as well (eTable 8 in Supplement 1). Although most ADHD medication initiators (91.9%) started with stimulants, initiation of stimulants vs nonstimulants showed no significant difference in terms of the all-cause mortality rate (eTable 9 in Supplement 1). In the case-crossover analysis, ADHD medication use was associated with significantly lower risk of all-cause mortality (OR, 0.70; 95% CI, 0.57-0.88) and unnatural-cause mortality (OR, 0.66; 95% CI, 0.51-0.85), but not with the risk of natural-cause mortality (OR, 0.81; 95% CI, 0.53-1.24; eTable 10 in Supplement 1).
Discussion
In this population-based study of 148 578 individuals with ADHD, initiation of ADHD medication, compared with noninitiation, was significantly associated with lower mortality at 2 years after diagnosis, especially for unnatural-cause mortality.
ADHD medication may reduce the risk of unnatural-cause mortality by alleviating the core symptoms of ADHD and its psychiatric comorbidities, leading to improved impulse control and decision-making, ultimately reducing the occurrence of fatal events, in particular among those due to accidental poisoning. Previous studies have reported improvements in comorbid psychiatric symptoms when ADHD is effectively treated.30 For instance, early and optimal treatment of ADHD may alter the trajectory of psychiatric morbidity by preventing the onset of comorbidities such as mood, anxiety, or substance use disorders.31,32 There is also evidence showing that ADHD medications were associated with lower risk of accidents, substance use, and criminality,10 which in turn could lead to lower rates of unnatural deaths. No statistically significant association between the use of ADHD medication and death by suicide was observed, although the magnitude of the association (HR, 0.88; 95% CI, 0.74-1.04) aligns with some previous pharmacoepidemiology studies examining the relationship between ADHD medication and suicide-related outcomes.10 Previous research has suggested that stimulant medication may reduce the risk of suicidal behavior in individuals with ADHD via both the direct improvement of ADHD symptoms and indirect reduction of risks associated with conditions like depression or substance use disorder.33,34 However, to what extent these findings extend to death by suicide requires further studies with a larger sample size.
In contrast to the extensive literature on psychiatric and behavioral outcomes associated with ADHD medication, the impact of ADHD medication on physical comorbidities is less well understood. There is evidence that stimulants contribute to lower rates of smoking in adults, which could improve overall health.35 Additionally, methylphenidate is associated with improvement in lifestyle, self-regulation, and enhancement of executive function,36 which could contribute to the reduction of natural mortality risks associated with ADHD. However, there are also concerns regarding the cardiovascular safety of stimulants.11 The results of the current study were reassuring because ADHD medication was not associated with increased risk of natural-cause mortality and, if anything, was associated with a reduced risk of natural-cause mortality in females. Nevertheless, future studies with larger sample sizes are warranted to confirm the relationship between ADHD medication use and natural-cause morbidity and mortality.
When considering sex-stratified associations, the initiation of ADHD medication was associated with a lower risk of all-cause and unnatural-cause mortality in males. In females, the only observed statistically significant association was between initiation of ADHD medication and natural-cause mortality. Notably, females had a higher median age at baseline in our study, suggesting delayed ADHD diagnosis compared with males, and previous studies have also reported distinct patterns of psychiatric and physical comorbidities (eg, females with ADHD have higher rates than males of depression, sleep disorder, atrial fibrillation, and asthma).5,37 Nevertheless, it is important to consider the difference in sample size and lower mortality rates in females when interpreting the results. Collectively, these findings underscore the need for further exploration of any sex difference in the relationship between ADHD treatment and mortality to inform targeted interventions aimed at optimizing outcomes for both males and females with ADHD.
It is important to note that this study focused on individuals aged 6 through 64 years at baseline. During the follow-up period, the absolute incidence of all-cause and cause-specific mortality was relatively small in magnitude. The interpretation of these findings should be made with caution, considering the limited number of events observed within this study population. However, the magnitude of the risk of mortality is comparable with the risk related to other common medical conditions. Indeed, ADHD is associated with a 2-fold increased risk of premature death,8 which is as high as the risk of mortality associated with type 2 diabetes.38 Because premature mortality is a major public health issue and ADHD is a common condition, the appropriate use of ADHD medications may contribute to decreasing the burden of mortality in a substantial number of individuals.
To our knowledge, this study is the first target trial emulation study using real-world data in ADHD research. Additional strengths are the long follow-up time, validated measures on exposure and outcome in a nationwide sample, and a broad age range that enabled the exploration of the association in both children and adults.
Limitations
Several limitations should be considered. First, due to the observational nature, these results cannot conclusively establish causal effects of ADHD medication treatment on mortality risk because unmeasured confounders, such as lifestyle factors, could contribute to the associations. It is also crucial to recognize that the treatment for ADHD involves more than just taking medication; it often includes various aspects of care, including social engagement and support. These nonmedication components may also affect the treatment outcomes. Therefore, the observed lower mortality may not be entirely accounted for by the medication per se. Second, given the potential for type I error resulting from multiple comparisons regarding cause-specific mortality and subgroup analyses, findings from these analyses should be interpreted as exploratory in nature rather than as definitive conclusions. Third, we cannot rule out exposure misclassification, because some individuals may not have consistently adhered to their prescribed medication, leading to potential underestimation of the true effects. Fourth, misclassification of death due to suicide and accidental poisoning cannot be ruled out because sometimes the intent may not be definitely determined.
Conclusions
In this target trial emulation study using national register data, medication initiation among individuals diagnosed with ADHD was associated with significantly lower mortality, in particular for death due to unnatural causes.
eMethods
eTable 1. Anatomical Therapeutic Chemical (ATC) codes for ADHD medication from the Prescribed Drug Register
eTable 2. The number and proportion of causes of death during a 5-year follow-up period
eTable 3. International Classification of Diseases Tenth Revisions (ICD-10) codes from the Swedish National Patient Register
eTable 4. Model coefficients for remaining uncensored in each treatment group
eTable 5. Association between ADHD medication initiation and 5-year mortality among individuals with ADHD
eTable 6. Association between ADHD medication initiation and 2-year mortality among individuals with ADHD using a 2-week interval
eTable 7. Association between ADHD medication initiation and 2-year mortality among individuals with ADHD without accounting for deviations from the assigned treatment strategies after the grace period.
eTable 8. Association between ADHD medication initiation and 2-year all-cause mortality among individuals with ADHD, without excluding competing events by using the subdistribution function
eTable 9. Association of stimulants versus non-stimulants with 2-year all-cause mortality among individuals with ADHD
eTable 10. Case-crossover analysis of the association between ADHD medication use and mortality
eFigure 1. Cumulative incidence curves of all-cause mortality
eReferences
Data Sharing Statement
References
- 1.Faraone SV, Banaschewski T, Coghill D, et al. The World Federation of ADHD International Consensus Statement: 208 evidence-based conclusions about the disorder. Neurosci Biobehav Rev. 2021;128:789-818. doi: 10.1016/j.neubiorev.2021.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bitsko RH, Claussen AH, Lichstein J, et al. Mental health surveillance among children—United States, 2013–2019. MMWR Suppl. 2022;71(2):1-42. doi: 10.15585/mmwr.su7102a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716-723. doi: 10.1176/ajp.2006.163.4.716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arrondo G, Solmi M, Dragioti E, et al. Associations between mental and physical conditions in children and adolescents: an umbrella review. Neurosci Biobehav Rev. 2022;137:104662. doi: 10.1016/j.neubiorev.2022.104662 [DOI] [PubMed] [Google Scholar]
- 5.Du Rietz E, Brikell I, Butwicka A, et al. Mapping phenotypic and aetiological associations between ADHD and physical conditions in adulthood in Sweden: a genetically informed register study. Lancet Psychiatry. 2021;8(9):774-783. doi: 10.1016/S2215-0366(21)00171-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartman CA, Larsson H, Vos M, et al. Anxiety, mood, and substance use disorders in adult men and women with and without attention-deficit/hyperactivity disorder: a substantive and methodological overview. Neurosci Biobehav Rev. 2023;151:105209. doi: 10.1016/j.neubiorev.2023.105209 [DOI] [PubMed] [Google Scholar]
- 7.Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. J Pediatr Psychol. 2007;32(6):643-654. doi: 10.1093/jpepsy/jsl054 [DOI] [PubMed] [Google Scholar]
- 8.Catalá-López F, Hutton B, Page MJ, et al. Mortality in persons with autism spectrum disorder or attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. JAMA Pediatr. 2022;176(4):e216401. doi: 10.1001/jamapediatrics.2021.6401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cortese S. Pharmacologic treatment of attention deficit-hyperactivity disorder. N Engl J Med. 2020;383(11):1050-1056. doi: 10.1056/NEJMra1917069 [DOI] [PubMed] [Google Scholar]
- 10.Chang Z, Ghirardi L, Quinn PD, Asherson P, D’Onofrio BM, Larsson H. Risks and benefits of attention-deficit/hyperactivity disorder medication on behavioral and neuropsychiatric outcomes: a qualitative review of pharmacoepidemiology studies using linked prescription databases. Biol Psychiatry. 2019;86(5):335-343. doi: 10.1016/j.biopsych.2019.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang L, Yao H, Li L, et al. Risk of cardiovascular diseases associated with medications used in attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(11):e2243597. doi: 10.1001/jamanetworkopen.2022.43597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang L, Li L, Andell P, et al. Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen VCH, Chan HL, Wu SI, et al. Methylphenidate and mortality in children with attention-deficit hyperactivity disorder: population-based cohort study. Br J Psychiatry. 2020;220(2):1-9. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy S, Cranswick N, Potts L, Taylor E, Wong IC. Mortality associated with attention-deficit hyperactivity disorder (ADHD) drug treatment: a retrospective cohort study of children, adolescents and young adults using the general practice research database. Drug Saf. 2009;32(11):1089-1096. doi: 10.2165/11317630-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 15.Stricker B, Cheung K, Verhamme K. General practice database on mortality in adults on methylphenidate: cohort study. BMJ Open. 2022;12(8):e057303. doi: 10.1136/bmjopen-2021-057303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Volkow ND, Swanson JM. Clinical practice: adult attention deficit-hyperactivity disorder. N Engl J Med. 2013;369(20):1935-1944. doi: 10.1056/NEJMcp1212625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L, Chang Z, Sun J, et al. Attention-deficit/hyperactivity disorder as a risk factor for cardiovascular diseases: a nationwide population-based cohort study. World Psychiatry. 2022;21(3):452-459. doi: 10.1002/wps.21020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li L, Yao H, Zhang L, et al. Attention-deficit/hyperactivity disorder is associated with increased risk of cardiovascular diseases: a systematic review and meta-analysis. JCPP Adv. 2023;3(3):e12158. doi: 10.1002/jcv2.12158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hernán MA, Wang W, Leaf DE. Target trial emulation: a framework for causal inference from observational data. JAMA. 2022;328(24):2446-2447. doi: 10.1001/jama.2022.21383 [DOI] [PubMed] [Google Scholar]
- 20.Khan MU, Aslani P. A review of measures used to examine medication adherence in people with ADHD at initiation, implementation and discontinuation of pharmacotherapy. Res Social Adm Pharm. 2020;16(3):277-289. doi: 10.1016/j.sapharm.2019.06.001 [DOI] [PubMed] [Google Scholar]
- 21.Sun S, Kuja-Halkola R, Faraone SV, et al. Association of psychiatric comorbidity with the risk of premature death among children and adults with attention-deficit/hyperactivity disorder. JAMA Psychiatry. 2019;76(11):1141-1149. doi: 10.1001/jamapsychiatry.2019.1944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matthews AA, Szummer K, Dahabreh IJ, et al. Comparing effect estimates in randomized trials and observational studies from the same population: an application to percutaneous coronary intervention. J Am Heart Assoc. 2021;10(11):e020357. doi: 10.1161/JAHA.120.020357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maringe C, Benitez Majano S, Exarchakou A, et al. Reflection on modern methods: trial emulation in the presence of immortal-time bias. assessing the benefit of major surgery for elderly lung cancer patients using observational data. Int J Epidemiol. 2020;49(5):1719-1729. doi: 10.1093/ije/dyaa057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656-664. doi: 10.1093/aje/kwn164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cain LE, Cole SR. Inverse probability-of-censoring weights for the correction of time-varying noncompliance in the effect of randomized highly active antiretroviral therapy on incident AIDS or death. Stat Med. 2009;28(12):1725-1738. doi: 10.1002/sim.3585 [DOI] [PubMed] [Google Scholar]
- 26.Young JG, Stensrud MJ, Tchetgen Tchetgen EJ, Hernán MA. A causal framework for classical statistical estimands in failure-time settings with competing events. Stat Med. 2020;39(8):1199-1236. doi: 10.1002/sim.8471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hallas J, Pottegård A. Use of self-controlled designs in pharmacoepidemiology. J Intern Med. 2014;275(6):581-589. doi: 10.1111/joim.12186 [DOI] [PubMed] [Google Scholar]
- 28.Langan SM, Schmidt SA, Wing K, et al. The reporting of studies conducted using observational routinely collected health data statement for pharmacoepidemiology (RECORD-PE). BMJ. 2018;363:k3532. doi: 10.1136/bmj.k3532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang Z, Kim HJ, Lonjon G, Zhu Y; written on behalf of AME Big-Data Clinical Trial Collaborative Group . Balance diagnostics after propensity score matching. Ann Transl Med. 2019;7(1):16. doi: 10.21037/atm.2018.12.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017;17(1):302. doi: 10.1186/s12888-017-1463-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Biederman J, Monuteaux MC, Spencer T, Wilens TE, Faraone SV. Do stimulants protect against psychiatric disorders in youth with ADHD? a 10-year follow-up study. Pediatrics. 2009;124(1):71-78. doi: 10.1542/peds.2008-3347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics. 1999;104(2):e20. doi: 10.1542/peds.104.2.e20 [DOI] [PubMed] [Google Scholar]
- 33.Chang Z, D’Onofrio BM, Quinn PD, Lichtenstein P, Larsson H. Medication for attention-deficit/hyperactivity disorder and risk for depression: a nationwide longitudinal cohort study. Biol Psychiatry. 2016;80(12):916-922. doi: 10.1016/j.biopsych.2016.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liang SHY, Yang YH, Kuo TY, et al. Suicide risk reduction in youths with attention-deficit/hyperactivity disorder prescribed methylphenidate: a Taiwan nationwide population-based cohort study. Res Dev Disabil. 2018;72:96-105. doi: 10.1016/j.ridd.2017.10.023 [DOI] [PubMed] [Google Scholar]
- 35.Schoenfelder EN, Faraone SV, Kollins SH. Stimulant treatment of ADHD and cigarette smoking: a meta-analysis. Pediatrics. 2014;133(6):1070-1080. doi: 10.1542/peds.2014-0179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Storebø OJ, Ramstad E, Krogh HB, et al. Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD). Cochrane Database Syst Rev. 2015;2015(11):CD009885. doi: 10.1002/14651858.CD009885.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ottosen C, Larsen JT, Faraone SV, et al. Sex differences in comorbidity patterns of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2019;58(4):412-422.e3. doi: 10.1016/j.jaac.2018.07.910 [DOI] [PubMed] [Google Scholar]
- 38.Xu G, You D, Wong L, et al. Risk of all-cause and CHD mortality in women versus men with type 2 diabetes: a systematic review and meta-analysis. Eur J Endocrinol. 2019;180(4):243-255. doi: 10.1530/EJE-18-0792 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eTable 1. Anatomical Therapeutic Chemical (ATC) codes for ADHD medication from the Prescribed Drug Register
eTable 2. The number and proportion of causes of death during a 5-year follow-up period
eTable 3. International Classification of Diseases Tenth Revisions (ICD-10) codes from the Swedish National Patient Register
eTable 4. Model coefficients for remaining uncensored in each treatment group
eTable 5. Association between ADHD medication initiation and 5-year mortality among individuals with ADHD
eTable 6. Association between ADHD medication initiation and 2-year mortality among individuals with ADHD using a 2-week interval
eTable 7. Association between ADHD medication initiation and 2-year mortality among individuals with ADHD without accounting for deviations from the assigned treatment strategies after the grace period.
eTable 8. Association between ADHD medication initiation and 2-year all-cause mortality among individuals with ADHD, without excluding competing events by using the subdistribution function
eTable 9. Association of stimulants versus non-stimulants with 2-year all-cause mortality among individuals with ADHD
eTable 10. Case-crossover analysis of the association between ADHD medication use and mortality
eFigure 1. Cumulative incidence curves of all-cause mortality
eReferences
Data Sharing Statement