Abstract
Objectives. To assess COVID-19 and influenza vaccination rates across Indiana’s 92 counties and identify county-level factors associated with vaccination.
Methods. We analyzed county-level data on adult COVID-19 vaccination from the Indiana vaccine registry and 2021 adult influenza vaccination from the Centers for Disease Control and Prevention. We used multiple linear regression (MLR) to determine county-level predictors of vaccinations.
Results. COVID-19 vaccination ranged from 31.2% to 87.6% (mean = 58.0%); influenza vaccination ranged from 33.7% to 53.1% (mean = 42.9%). In MLR, COVID-19 vaccination was significantly associated with primary care providers per capita (b = 0.04; 95% confidence interval [CI] = 0.02, 0.05), median household income (b = 0.23; 95% CI = 0.12, 0.34), percentage Medicare enrollees with a mammogram (b = 0.29; 95% CI = 0.08, 0.51), percentage uninsured (b = −1.22; 95% CI = −1.57, −0.87), percentage African American (b = 0.31; 95% CI = 0.19, 0.42), percentage female (b = −0.97; 95% CI = −1.79, ‒0.15), and percentage who smoke (b = −0.75; 95% CI = −1.26, −0.23). Influenza vaccination was significantly associated with percentage uninsured (b = 0.71; 95% CI = 0.22, 1.21), percentage African American (b = −0.07; 95% CI = −0.13, −0.01), percentage Hispanic (b = −0.28; 95% CI = −0.40, −0.17), percentage who smoke (b = −0.85; 95% CI = −1.06, −0.64), and percentage who completed high school (b = 0.54; 95% CI = 0.21, 0.87). The MLR models explained 86.7% (COVID-19) and 70.2% (influenza) of the variance.
Conclusions. Factors associated with COVID-19 and influenza vaccinations varied. Variables reflecting access to care (e.g., insurance) and higher risk of severe disease (e.g., smoking) are notable. Programs to improve access and target high-risk populations may improve vaccination rates. (Am J Public Health. 2024;114(4):415–423. https://doi.org/10.2105/AJPH.2023.307553)
The COVID-19 pandemic, caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),1 represents an unprecedented public health crisis in modern times. While initial pandemic hotspots centered in densely populated urban areas, infections in rural areas began to rise as the pandemic progressed.2 This rise in rural infections highlighted rural disparities in access to health care as well as differences in health beliefs, resistance to preventive health behaviors (e.g., mask wearing and social distancing), and higher vaccine hesitancy and lower vaccine confidence.3 Vaccine hesitancy, which involves distrust or concern about vaccination, is predictive of, but distinct from, vaccine uptake.4,5 Rural‒urban differences in vaccine hesitancy, confidence, and health beliefs are being seen both with new COVID-19 vaccines and more established adult vaccinations, including human papillomavirus and influenza.6,7 Nationally, there is a significant urban– rural vaccination coverage disparity. This disparity encompasses different age ranges, including child, adolescent, and adult vaccination, and different vaccines, ranging from influenza to pneumococcal to human papillomavirus.6,8–10
Addressing these disparities must begin with an understanding of the unique context of rural areas. Furthermore, effective interventions must account for the “triad” of local culture, geographic location, and economics of the region.11 For example, in addition to higher vaccine hesitancy rates,12,13 rural residents also face more logistical barriers such as access to, and quality of, health care.14 Importantly, rural individuals’ health care providers play a crucial role in vaccination. Interventions that partner with clinics and health care providers show more vaccine improvement than interventions without these components.15 In addition, rural individuals must depend more on traditional clinical settings (e.g., their provider’s office) for vaccination versus their urban counterparts with more access to alternative vaccine sites (e.g., pharmacies, health fairs), which may contribute to disparities in uptake.7 Most relevant interventions have focused on improving provider communication,16 practice-based strategies (e.g., provider prompts, standing orders),17,18 and shifting individual attitudes and intent.19 Although these approaches have shown some success, the typical effect size is small to moderate, and these approaches have not often targeted those who live in rural areas. In sum, continued work is needed to investigate rural‒urban disparities in vaccination and identify factors associated with these disparities within specific geographic areas, especially during a complex vaccine rollout like the COVID-19 vaccine.
Therefore, this study aimed to assess existing differences among adults in both COVID-19 and influenza vaccinations by county in Indiana and determine what county-level factors are associated with those vaccination rates. We chose to focus on these 2 vaccines as they both involve respiratory viruses, both have generated greater hesitancy than other adult vaccines, and both are routinely recommended for all adults.
METHODS
In this study, we examined COVID-19 and influenza vaccination rates across Indiana’s 92 counties among adults aged 18 years and older from December 2020 through March 2022. We extracted the data for COVID-19 vaccinations from the Indiana State Department of Health, Children and Hoosier Immunization Registry Program (CHIRP). We extracted influenza rates from the Centers for Disease Control and Prevention (CDC) US Influenza Surveillance Dashboard (FluVaxView),20 which reports weekly national influenza vaccination data by county.
Measures
Vaccination data
The Indiana CHIRP database is a secure, Web-based immunization registry program that permanently stores immunization records. CHIRP provided county-level data on the number of first and second doses of Pfizer and Moderna COVID-19 vaccinations given as well as single-dose Johnson & Johnson vaccination, consistent with vaccine recommendations at the time of data collection, from December 2020 through March 2022. While CHIRP was designed to track pediatric vaccinations, the state uses CHIRP to track all COVID-19 vaccinations, regardless of age. These data are publicly available through a data request with the Indiana State Department of Health. In addition, CHIRP also provided information on county-level vaccination rates by age group, race/ethnicity, and sex. All data were aggregate, and no individual-level data were available.
Because CHIRP does not track influenza vaccinations for adults, we obtained county-level influenza vaccination in 2021 from the FluVaxView database, administered by the CDC.20 From the database, we downloaded a comma-separated values‒format report, and we extracted influenza vaccination rates by using the Federal Information Processing Standard codes—unique codes assigned to identify each county in the United States. We used codes 18001 through 18183 to filter down to only Indiana counties.
County-level data
We derived county-level population estimates from the US Census to determine COVID-19 vaccination rates. We derived county-specific socio-demographic and health data from the County Health Rankings Report, a program supported by the Robert Wood Johnson Foundation and the University of Wisconsin Population Health Institute.21 Lastly, because we aimed to investigate county-level factors associated with vaccination rates, we gathered information on number of primary care providers per 100 000 individuals, as reported by the County Health Rankings Report, and the existence of a community paramedicine program that incorporates vaccination services. Information on community paramedicine programs was available, by request, from the Indiana Department of Homeland Security. Recently, the Department of Homeland Security released updated information on these programs.22 The latter practice has increased in use across the country to improve vaccination rates23–29 and was therefore included as a potential predictor variable.
Statistical Analyses
Descriptive statistics were presented using mean ±SD and median (minimum‒ maximum) and reported for all county-level variables and COVID-19 and influenza vaccination rates at the county level. COVID-19 vaccination rates were calculated by determining the percentage of individuals in each county aged 18 years and older who received either their second dose of the Pfizer or Moderna COVID-19 vaccinations or a single dose of the Johnson & Johnson COVID-19 vaccination.
We modeled county-level vaccination rates by using linear regression weighted by the total adult population of each county. We conducted model selection by using forward, backward, and stepwise selection to determine the best multiple linear regression model for each vaccination rate. The forward and stepwise selection methods used a .05 significance level for entry criterion, and the backward and stepwise selection methods used a .05 significance level for staying in the model. We selected the best model based on the adjusted R2 value. We examined tolerance values for variables in each final model to ensure issues with multicollinearity were negligible, and we assessed residuals for normality. The full model for each vaccination rate is reported along with the selected reduced model. Estimated model coefficients and associated 95% confidence intervals (CIs) are reported. The squared semipartial correlation coefficient for each variable is also reported as a measure of effect size. We considered a P value less than .05 to be statistically significant. We conducted statistical analyses with SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
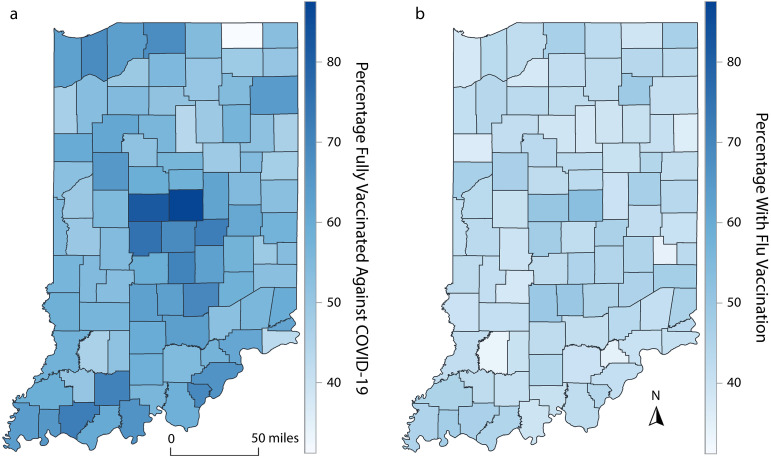
The mean COVID-19 vaccination rate across the 92 counties in Indiana was 58% and ranged from 31.2% to 87.6% (Table 1). The mean influenza vaccination rate was 42.9% and ranged from 33.7% to 53.1%. Figure 1 displays the variability in COVID-19 (panel a) and influenza (panel b) vaccination rates across Indiana counties with darker color indicating a higher vaccination rate.
TABLE 1—
Summary Statistics for County-Level Demographic and Health Care Variables: Indiana
| Variable | Mean ± SD | Median (Min‒Max) |
| Total primary care providers per 100 000 individualsa | 124.0 ± 63.3 | 116.5 (18.8–321.9) |
| Median household income, $b | 60 637.4 ± 10 163.5 | 59 269 (42 504–96 359) |
| % of the county that is ruralc | 54.5 ± 26.9 | 53.6 (0.6–100) |
| % of Medicare enrollees with influenza vaccinea | 50.5 ± 6.6 | 52.0 (31.0–62.0) |
| % of Medicare enrollees with mammography screeninga,d | 42.7 ± 5.0 | 43.0 (31.0–54.0) |
| % of all county residents | ||
| Uninsureda | 10.4 ± 2.7 | 10.0 (6.0–27.9) |
| Food insecurea | 12.5 ± 1.9 | 12.5 (7.5–16.6) |
| Aged ≥ 65 yearsb | 18.6 ± 2.3 | 18.8 (12.2–25.7) |
| African Americanb | 3.0 ± 4.5 | 0.9 (0.2–28.7) |
| Hispanicb | 4.5 ± 3.8 | 3.1 (1.3–20.0) |
| Femaleb | 50.1 ± 1.2 | 50.2 (45.3–52.9) |
| % of adult county residents | ||
| Smokea | 22.0 ± 2.4 | 22.3 (12.5–26.9) |
| Obesitya | 36.0 ± 2.3 | 36.2 (26.3–39.8) |
| Unemployedb | 6.7 ± 1.3 | 6.5 (3.8–11.1) |
| Completed high schoole | 88.6 ± 4.4 | 89.2 (61.1–97.1) |
| Fully vaccinated against COVID-19 | 58.0 ± 8.4 | 57.1 (31.2–87.6) |
| Vaccinated against influenzaf | 42.9 ± 3.5 | 42.5 (33.7–53.1) |
Note. n = 92.
Data from 2019.
Data from 2020.
Data from 2010.
Defined as the percentage of female Medicare enrollees aged 65–74 years that received annual mammography screening.
Data from 2016–2020.
Data from 2021.
FIGURE 1—
Heatmap of Vaccination Rates by Indiana County for (a) COVID-19 (December 2020‒March 2022) and (b) Influenza (2021)
County-Level Factors and COVID-19 Vaccination
Although the univariable regression results between county factors and COVID-19 or influenza vaccination (Table A, available as a supplement to the online version of this article at https://ajph.org) were generally similar, differences were evident in the multiple linear regression models (Table 2). The final selected model for COVID-19 vaccination, which was obtained by both forward and stepwise selection, contained 7 explanatory variables with an adjusted R2 = 0.867. The unit of the outcome of the model is percentage with COVID-19 vaccination with a 0-to-100 range. Based on this model, 1 additional primary care provider per 100 000 individuals was associated with an increase of 0.04 (b = 0.04; 95% CI = 0.02, 0.05) in the percentage with COVID-19 vaccination after adjusting for other factors in the model. An increase in median household income of $1000 is associated with an increase in the percentage with COVID-19 vaccination of 0.23 (b = 0.23; 95% CI = 0.12, 0.34). All other explanatory variables are in percentages; thus, interpretations are similar for each.
TABLE 2—
Association of County-Level Factors and COVID-19 (December 2020‒March 2022) or Influenza (2021) Vaccination: Indiana
| Variable | COVID-19 (Forward/Stepwise) | Influenza (Backward) | ||
| b (95% CI) | Effect Size | b (95% CI) | Effect Size | |
| Total primary care providers per 100 000 individuals | 0.04 (0.02, 0.05) | 0.040 | … | … |
| Median household income (thousands) | 0.23 (0.12, 0.34) | 0.027 | … | … |
| % of Medicare enrollees with mammography screening | 0.29 (0.08, 0.51) | 0.011 | … | … |
| % of all county residents | ||||
| Uninsured | −1.22 (−1.57, −0.87) | 0.071 | 0.71 (0.22, 1.21) | 0.027 |
| African American | 0.31 (0.19, 0.42) | 0.041 | −0.07 (−0.13, −0.01) | 0.016 |
| Female | −0.97 (−1.79, −0.15) | 0.008 | … | … |
| Hispanic | … | … | −0.28 (−0.40, −0.17) | 0.079 |
| % of adult county residents | ||||
| Smoke | −0.75 (−1.26, −0.23) | 0.012 | −0.85 (−1.06, −0.64) | 0.216 |
| Completed high school | … | … | 0.54 (0.21, 0.87) | 0.035 |
| Adjusted R2 | 0.867 | 0.702 | ||
Note. CI = confidence interval. This table shows multiple linear regression results—selected reduced models.
A 1-percentage-point increase in Medicare enrollees with mammography screening was associated with an increase of 0.29 in the percentage with COVID-19 vaccination (b = 0.29; 95% CI = 0.08, 0.51); a 1-percentage-point increase of uninsured residents was associated with a decrease of 1.22 in the percentage with COVID-19 vaccination (b = −1.22; 95% CI = ‒1.57, −0.87); a 1-percentage-point increase of African American residents was associated with an increase of 0.31 in the percentage with COVID-19 vaccination (b = 0.31; 95% CI = 0.19, 0.42); a 1-percentage-point increase of female residents was associated with a decrease of 0.97 in the percentage with COVID-19 vaccination (b = −0.97; 95% CI = ‒1.79, −0.15); and a 1-percentage-point increase of adult smokers was associated with a decrease of 0.75 in the percentage with COVID-19 vaccination (b = −0.75; 95% CI = ‒1.26, −0.23).
The percentage of uninsured residents had the largest effect size with 7.1% of the total variation in COVID-19 vaccination rates being explained by this covariate. Overall, this model explained 86.7% of the variation in COVID-19 vaccination rates across Indiana counties.
County-Level Factors and Influenza Vaccination
The final multiple linear regression model for influenza vaccination rates contained 5 explanatory variables, was obtained by backward selection, and provided an adjusted R2 = 0.702 (Table 2). Similar to the COVID-19 model, the unit of outcome was the percentage. Based on this model, a 1-percentage-point increase of uninsured residents (b = 0.71; 95% CI = 0.22, 1.21) and adults who completed high school (b = 0.54; 95% CI = 0.21, 0.87) was associated with a higher influenza vaccination rate, whereas a 1-percentage-point increase of African American residents (b = −0.07; 95% CI = ‒0.13, −0.01), Hispanic residents (b = −0.28; 95% CI = ‒0.40, −0.17), and adults who smoke (b = −0.85; 95% CI = ‒1.06, −0.64) was associated with a lower influenza vaccination rate.
The percentage of adults who smoke had the largest effect size with 21.6% of the total variation in influenza vaccination rates being explained by this covariate. Overall, this model explained 70.2% of the variation in influenza vaccination rates across Indiana counties. For each vaccination rate, the full model with all candidate variables for model selection is presented in Table B (available as a supplement to the online version of this article at https://ajph.org).
In sum, different county-level factors were associated with COVID-19 vaccination rates and influenza vaccination rates. Greater access to health care (e.g., primary care providers per capita, percentage of uninsured residents, household income, percentage of Medicare enrollees with mammography screening) was associated with COVID-19 vaccination rates, as were the percentage of residents who were African American or female, or who smoked. For influenza vaccination, mostly demographic factors (i.e., percentage Hispanic, percentage African American, percentage who completed high school) had a significant association. The percentages of uninsured residents and African American residents were associated with both but were in opposite directions for each vaccine. Percentage of adults in the county who smoke was the only variable that was significant for each vaccine in the same direction (a higher percentage of smokers was associated with lower vaccination rates).
DISCUSSION
In this study, we examined county-level factors associated with adult influenza and COVID-19 vaccination rates. While both vaccinations are recommended for adults, adjusted models showed that county-level factors associated with each vaccination varied greatly. Specifically, the reduced model for COVID-19 vaccination explained a slightly higher percentage of the variance (86.7%) than the model for influenza vaccination (70.2%). This may reflect greater polarization surrounding COVID-19 vaccination, leading to a greater influence of sociodemographic factors with COVID-19 vaccination as compared with influenza vaccination. Of note were variables reflecting access to care (e.g., number of primary care providers per capita), which were significant for COVID-19 vaccination rates but not for influenza vaccination rates.
One finding of interest was that the percentage of uninsured residents in the county was associated with each vaccination, but in opposite directions. Higher COVID-19 vaccination rates were associated with a decrease in the percentage of uninsured residents, whereas higher influenza vaccination rates were associated with an increase in uninsured residents, although this effect size was small (0.016). In addition, the number of primary care providers per capita was associated with COVID-19 vaccination rates but was not significant for influenza.
People wishing to obtain the COVID-19 vaccine should have faced fewer barriers than perhaps any other vaccination in recent decades. A combination of federal, state, and local programs including Operation Warp Speed,30 the American Rescue Plan Act of 2021,31 and Section 317 of the Public Health Service Act,32 among others, eliminated copays for the vaccine and ensured it was available at community locations beyond traditional health care provider offices. Therefore, structural barriers for COVID-19 vaccination should have been minimal.
Furthermore, research shows that structural inequities (e.g., health insurance, lack of access to primary care) are associated with influenza vaccination rates.33 Thus, the findings from this study that structural inequities were associated with COVID-19 vaccination rates, but not influenza vaccination rates, were surprising and point to the need for more research. One possible explanation is the unique way in which the COVID-19 vaccine was rolled out, which involved different dates when people were eligible (based on age, for instance), the need to sign up for vaccination online, and difficulties, particularly early on, in finding available appointments, all of which may have increased logistical barriers.
Another finding of interest was the association between each vaccination and county-level racial/ethnic distribution. The percentage of Hispanic residents in the county was associated with influenza vaccination but not COVID-19 vaccination. Furthermore, the percentage of African American residents in a county was negatively associated with influenza vaccination but positively associated with COVID-19 vaccination.
Similar differences across the 2 types of vaccination were demonstrated in other studies. Adult COVID-19 vaccination rates were not significantly different between non-Hispanic Black, Hispanic, and non-Hispanic White adults at the end of 2021,34 whereas non-Hispanic White adults had higher influenza vaccination rates than either non-Hispanic Black and Hispanic adults during the same timeframe.35 One possible explanation for the differing associations for the 2 vaccinations is that there was significant outreach to the Hispanic and Latinx community to promote vaccine equity for COVID-19 vaccination, and similar efforts have not been implemented for influenza vaccination. Specifically, 1 systematic review found that in the 2021 calendar year, there were coordinated efforts to understand the nuances of vaccine hesitancy, access issues, and structural inequities experienced by Latinx communities with regard to the COVID-19 vaccination.36 Furthermore, disparities in influenza vaccination persist, even among Hispanic adults who report a recent medical checkup, suggesting that missed opportunities for vaccination occurred at these clinic visits.37
Lastly, an additional study found racial/ethnic disparities for influenza vaccination among adults aged 50 years and older with lower vaccination rates for Hispanics and non-Hispanic Black adults compared with non-Hispanic White adults.38 However, there was not a disparity for those aged 18 to 49 years, when controlling for patient characteristics. Given these results, it is possible the differing findings by Hispanic population may be better explained if we controlled for individual patient characteristics. However, this was not possible with our county-level aggregate data, and future research should explore these racial/ethnic disparities while taking individual patient characteristics into account.
We found that smoking was strongly negatively associated with vaccination rates for both COVID-19 and influenza. While this may seem counterintuitive, given that smoking is a risk factor for severe COVID-19 disease,39 it is consistent with the literature. Research has consistently shown that preventive health behaviors cluster together, and people who engage in one healthy (or unhealthy) behavior, are more likely to engage in another.40 Likewise, research has shown that people who smoke are less likely to receive routine preventive services, which may reduce the opportunity to get vaccinated.41 Another study, conducted before the COVID-19 pandemic, showed lower rates of influenza and pneumococcal vaccination among smokers,42 and the authors highlighted the importance of providers facilitating smoking cessation and promoting vaccinations for people who smoke. As we continue to see hospitalizations and deaths from COVID-19 and seasonal influenza, it is important to raise awareness of the factors associated with severe disease and improve public health messaging to target groups who are disproportionately affected and should be targeted for vaccination efforts.
Finally, while the percentage of the county that was rural was significantly associated with both COVID-19 and influenza vaccination in univariable linear regression analyses, these associations were no longer significant when other variables were included in the model. This is consistent with other recent research that has found no rural‒urban differences in influenza vaccination rates using data from the Behavioral Risk Factor Surveillance System.43 It is possible that the rural‒urban differences were accounted for with other county-level factors, including income or smoking status. Indeed, another study examining rural‒urban differences in COVID-19 vaccination rates found that the differences were explained by a combination of educational attainment, health care infrastructure, and political ideology.44 Reasons for rural‒urban disparities across a multitude of health indicators are multifaceted and are likely a complex combination of access, infrastructure, attitudes, and beliefs.
Strengths and Limitations
In this study, we examined county-level factors associated with adult influenza and COVID-19 vaccination uptake. While it had numerous strengths, including using a population-based data set and incorporating county-level variables, results should be interpreted in light of several limitations. First, the data are cross-sectional, and a causal relationship between county-level variables and vaccination rates cannot be established. Second, the data are aggregate and are subject to ecological fallacy (i.e., erroneously inferring characteristics to an individual based on characteristics of a group). Third, this cross-sectional study cannot determine the sequence of events between exposure and outcome, which may lead to temporal ambiguity.
Fourth, this study focused only on Indiana, and, therefore, the findings may not be applicable to other states or jurisdictions. Indiana, as a state, has more non-Hispanic White residents and fewer Hispanic or non-Hispanic Black residents than the overall United States.45 Furthermore, per-capita income tends to be lower, resulting in higher percentages of people living in poverty.45 Indiana also has a higher percentage of its population living in rural areas46 and fewer primary care providers.47 As these factors emerged as having a significant relationship with vaccination rates, our findings may generalize most to other Midwestern states. Additional research is needed to identify how these findings may differ in other regions.
Fifth, influenza and COVID-19 vaccinations have differing numbers of vaccinations to be considered fully vaccinated. While we examined recommended series completion at the time of data collection (1 dose of influenza vaccine and 2 doses of COVID-19 vaccine), it is possible that there are differing barriers to receiving 1 influenza vaccination than there are to completing 2 COVID-19 vaccinations. Lastly, because CHIRP does not track adult influenza vaccination, we used 2 different data sources to examine the 2 vaccination rates. Therefore, it is possible that the 2 data sources differ in their accuracy and reporting. Results of this study should be interpreted with caution, and further studies are needed to understand the complex association between the systems-level factors we examined and vaccination rates.
Conclusions
In this study, we explored county-level factors associated with rates of vaccination for 2 adult vaccines: COVID-19 and influenza. While both of these vaccines protect against respiratory viruses and are recommended for all adults, the factors associated with uptake of each varied. Variables reflecting access to care (e.g., number of primary care providers per capita, median household income) were significant for COVID-19 vaccination rates but not influenza vaccination rates. In addition, the percentage of uninsured residents in the county was significant for both vaccines, but in opposite directions. The rate was negatively associated with COVID-19 vaccination and positively associated with influenza vaccination. The polarization surrounding COVID-19 vaccination may have led to a greater influence of sociodemographic factors with COVID-19 vaccination as compared with influenza vaccination. Further research, including patient-level data, is needed to better understand these associations and develop effective interventions to address county-level factors and improve vaccine uptake.
ACKNOWLEDGMENTS
This project was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. M. L. Kasting was supported by grants KL2TR002530 (B. Tucker Edmonds, principal investigator [PI]) and UL1TR002529 (S. Moe and S. Wiehe, co-PIs) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award.
Findings from this study were presented at the American Public Health Association 2023 Annual Meeting and Expo in Atlanta, GA.
Note. The opinions expressed in this article are those of the authors and do not necessarily represent those of Merck Sharp & Dohme Corp. The funding agencies had no role in designing the study, interpreting the data, writing the article, or making the decision to submit the article for publication.
CONFLICTS OF INTEREST
G. D. Zimet has served as an external advisory board member for Pfizer and Moderna, and as a consultant to Merck. G. D. Zimet, K. J. Head, and M. L. Kasting have received investigator-initiated research funding from Merck administered through Indiana University and Purdue University, respectively.
HUMAN PARTICIPANT PROTECTION
This study was reviewed by the institutional review board at Purdue University and was determined not to be human participant research.
See also Bednarczyk, p. 359.
REFERENCES
- 1. World Health Organization . WHO timeline—COVID-19. April 2020. . Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed January 27, 2024.
- 2.Paul R , Arif AA , Adeyemi O , Ghosh S , Han D. Progression of COVID-19 from urban to rural areas in the United States: a spatiotemporal analysis of prevalence rates. J Rural Health. 2020;36(4): 591–601. 10.1111/jrh.12486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kasting ML , Head KJ , Hartsock JA , Sturm L , Zimet GD. Public perceptions of the effectiveness of recommended non-pharmaceutical intervention behaviors to mitigate the spread of SARS-CoV-2. PLoS One. 2020;15(11):e0241662. 10.1371/journal.pone.0241662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larson HJ , Gakidou E , Murray CJL. The vaccine-hesitant moment. N Engl J Med. 2022;387(1): 58–65. 10.1056/NEJMra2106441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldwin AS , Tiro JA , Zimet GD. Broad perspectives in understanding vaccine hesitancy and vaccine confidence: an introduction to the special issue. J Behav Med. 2023;46(1-2):1–8. 10.1007/s10865-023-00397-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhai Y , Santibanez TA , Kahn KE , Srivastav A , Walker TY , Singleton JA. Rural, urban, and suburban differences in influenza vaccination coverage among children. Vaccine. 2020;38(48):7596–7602. 10.1016/j.vaccine.2020.10.030 [DOI] [PubMed] [Google Scholar]
- 7.Bennett KJ , Pumkam C , Probst JC. Rural‒urban differences in the location of influenza vaccine administration. Vaccine. 2011;29(35):5970–5977. 10.1016/j.vaccine.2011.06.038 [DOI] [PubMed] [Google Scholar]
- 8. Center for Medicare and Medicaid Services Office of Minority Health . Data snapshot August 2020. : Annual influenza vaccination disparities in Medicare beneficiaries. Available at: https://www.cms.gov/files/document/data-snapshot-annual-influenza-vaccination.pdf . Accessed February 8, 2021.
- 9.McLaughlin JM , Swerdlow DL , Khan F , et al. Disparities in uptake of 13-valent pneumococcal conjugate vaccine among older adults in the United States. Hum Vaccin Immunother. 2019; 15(4):841–849. 10.1080/21645515.2018.1564434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swiecki-Sikora AL , Henry KA , Kepka D. HPV vaccination coverage among US teens across the rural‒urban continuum. J Rural Health. 2019;35(4): 506–517. 10.1111/jrh.12353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas TL , DiClemente R , Snell S. Overcoming the triad of rural health disparities: how local culture, lack of economic opportunity, and geographic location instigate health disparities. Health Educ J. 2014;73(3):285–294. 10.1177/0017896912471049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santibanez TA , Nguyen KH , Greby SM , et al. Parental vaccine hesitancy and childhood influenza vaccination. Pediatrics. 2020;146(6):e2020007609. 10.1542/peds.2020-007609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khubchandani J , Sharma S , Price JH , Wiblishauser MJ , Sharma M , Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270‒277. 10.1007/s10900-020-00958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Purnell TS , Calhoun EA , Golden SH , et al. Achieving health equity: closing the gaps in health care disparities, interventions, and research. Health Aff (Millwood). 2016;35(8):1410–1415. 10.1377/hlthaff.2016.0158 [DOI] [PubMed] [Google Scholar]
- 15.Brandt HM , Vanderpool RC , Pilar M , Zubizarreta M , Stradtman LR. A narrative review of HPV vaccination interventions in rural US communities. Prev Med. 2021;145:106407. 10.1016/j.ypmed.2020.106407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilkey MB , Dayton AM , Moss JL , et al. Increasing provision of adolescent vaccines in primary care: a randomized controlled trial. Pediatrics. 2014; 134(2):e346–e353. 10.1542/peds.2013-4257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilkey MB , Moss JL , Roberts AJ , Dayton AM , Grimshaw AH , Brewer NT. Comparing in-person and webinar delivery of an immunization quality improvement program: a process evaluation of the adolescent AFIX trial. Implement Sci. 2014; 9(1):21. 10.1186/1748-5908-9-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dixon BE , Kasting ML , Wilson S , Kulkarni A , Zimet GD , Downs SM. Health care providers’ perceptions of use and influence of clinical decision support reminders: qualitative study following a randomized trial to improve HPV vaccination rates. BMC Medical Inform Decis Mak. 2017;17(1): 119. 10.1186/s12911-017-0521-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kennedy A , Sapsis KF , Stokley S , Curtis CR , Gust D. Parental attitudes toward human papillomavirus vaccination: evaluation of an educational intervention, 2008. J Health Commun. 2011;16(3):300–313. 10.1080/10810730.2010.532296 [DOI] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention . FluVaxView Interactive! Available at: https://www.cdc.gov/flu/fluvaxview/index.htm . Accessed January 17, 2023.
- 21. County Health Rankings and Roadmaps . About us. Available at: https://www.countyhealthrankings.org/about-us . Accessed February 9, 2021.
- 22. Indiana Department of Homeland Security . Mobile Integrated Health: Indiana MIH Dashboard. Available at: https://www.in.gov/dhs/ems/mobile-integrated-health/#MIHDash . Accessed October 9, 2023.
- 23.Drennan IR , Dainty KN , Hoogeveen P , et al. Expanding Paramedicine in the Community (EPIC): study protocol for a randomized controlled trial. Trials. 2014;15(1):473. 10.1186/1745-6215-15-473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Meara P , Ruest M , Stirling C. Community paramedicine: higher education as an enabling factor. Australasian J Paramedicine. 2014;11(2):1–9. 10.33151/ajp.11.2.22 [DOI] [Google Scholar]
- 25.Rasku T , Kaunonen M , Thyer E , Paavilainen E , Joronen K. The core components of community paramedicine–integrated care in primary care setting: a scoping review. Scand J Caring Sci. 2019;33(3):508–521. 10.1111/scs.12659 [DOI] [PubMed] [Google Scholar]
- 26.Bigham BL , Kennedy SM , Drennan I , Morrison LJ. Expanding paramedic scope of practice in the community: a systematic review of the literature. Prehosp Emerg Care. 2013;17(3):361–372. 10.3109/10903127.2013.792890 [DOI] [PubMed] [Google Scholar]
- 27.Chan J , Griffith LE , Costa AP , Leyenaar MS , Agarwal G. Community paramedicine: a systematic review of program descriptions and training. CJEM. 2019;21(6):749–761. 10.1017/cem.2019.14 [DOI] [PubMed] [Google Scholar]
- 28.Gregg A , Tutek J , Leatherwood MD , et al. Systematic review of community paramedicine and EMS mobile integrated health care interventions in the United States. Popul Health Manag. 2019;22(3): 213–222. 10.1089/pop.2018.0114 [DOI] [PubMed] [Google Scholar]
- 29.Pang PS , Litzau M , Liao M , et al. Limited data to support improved outcomes after community paramedicine intervention: a systematic review. Am J Emerg Med. 2019;37(5):960–964. 10.1016/j.ajem.2019.02.036 [DOI] [PubMed] [Google Scholar]
- 30.Slaoui M , Hepburn M. Developing safe and effective Covid vaccines—Operation Warp Speed’s strategy and approach. N Engl J Med. 2020; 383(18):1701–1703. 10.1056/NEJMp2027405 [DOI] [PubMed] [Google Scholar]
- 31. Library of Congress . H.R.1319 - American Rescue Plan Act of 2021. 2021. . Available at: https://www.congress.gov/bill/117th-congress/house-bill/1319/text . Accessed March 9, 2023.
- 32.National Vaccine Advisory Committee. Protecting the public’s health: critical functions of the Section 317 Immunization Program—a report of the National Vaccine Advisory Committee. Public Health Rep. 2013;128(2):78–95. 10.1177/003335491312800203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brewer LI , Ommerborn MJ , Nguyen AL , Clark CR. Structural inequities in seasonal influenza vaccination rates. BMC Public Health. 2021;21(1): 1166. 10.1186/s12889-021-11179-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kriss JL , Hung MC , Srivastav A , et al. COVID-19 vaccination coverage, by race and ethnicity—National Immunization Survey Adult COVID Module, United States, December 2020‒November 2021. MMWR Morb Mortal Wkly Rep. 2022; 71(23):757–763. 10.15585/mmwr.mm7123a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Centers for Disease Control and Prevention . Flu vaccination coverage, United States, 2021–22 influenza season. 2022. . Available at: https://www.cdc.gov/flu/fluvaxview/coverage-2022estimates.htm . Accessed March 9, 2023.
- 36.Demeke J , Ramos SR , McFadden SM , et al. Strategies that promote equity in COVID-19 vaccine uptake for Latinx communities: a review. J Racial Ethn Health Disparities. 2023;10(3):1349–1357. 10.1007/s40615-022-01320-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Black CL , O’Halloran A , Hung MC , et al. Vital signs: Influenza hospitalizations and vaccination coverage by race and ethnicity—United States, 2009‒10 through 2021‒22 influenza seasons. MMWR Morb Mortal Wkly Rep. 2022;71(43):1366–1373. 10.15585/mmwr.mm7143e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lu D , Qiao Y , Brown NE , Wang J. Racial and ethnic disparities in influenza vaccination among adults with chronic medical conditions vary by age in the United States. PLoS One. 2017;12(1): e0169679. 10.1371/journal.pone.0169679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Poudel R , Daniels LB , DeFilippis AP , et al. Smoking is associated with increased risk of cardiovascular events, disease severity, and mortality among patients hospitalized for SARS-CoV-2 infections. PLoS One. 2022;17(7):e0270763. 10.1371/journal.pone.0270763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fortenberry JD , Costa FM , Jessor R , Donovan JE. Contraceptive behavior and adolescent lifestyles: a structural modeling approach. J Res Adolesc. 1997;7(3):307–329. 10.1207/s15327795jra0703_4 [DOI] [PubMed] [Google Scholar]
- 41.Vander Weg MW , Howren M , Cai X. Use of routine clinical preventive services among daily smokers, non-daily smokers, former smokers, and never-smokers. Nicotine Tob Res. 2012;14(2): 123–130. 10.1093/ntr/ntr141 [DOI] [PubMed] [Google Scholar]
- 42.Pearson WS , Dube SR , Ford ES , Mokdad AH. Influenza and pneumococcal vaccination rates among smokers: data from the 2006 Behavioral Risk Factor Surveillance System. Prev Med. 2009; 48(2):180–183. 10.1016/j.ypmed.2008.11.001 [DOI] [PubMed] [Google Scholar]
- 43.Alalwan AA. Influenza vaccine utilization: a comparison between urban and rural counties in Florida. Vaccines (Basel). 2022;10(5):669. 10.3390/vaccines10050669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun Y , Monnat SM. Rural‒urban and within-rural differences in COVID-19 vaccination rates. J Rural Health. 2022;38(4):916–922. 10.1111/jrh.12625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. US Census Bureau . QuickFacts: United States; Indiana. Available at: https://www.census.gov/quickfacts/fact/table/US,IN/PST045222 . Accessed April 24, 2023.
- 46. Iowa State University . Urban percentage of the population for states, historical. Available at: https://www.icip.iastate.edu/tables/population/urban-pct-states . Accessed April 24, 2023.
- 47. County Health Rankings & Roadmaps . Explore health rankings: Indiana—primary care physicians. Available at: https://www.countyhealthrankings.org/explore-health-rankings/indiana?year=2023&measure=Primary+Care+Physicians . Accessed April 24, 2023.