Abstract
Background and Objective
One in five preschool children are overweight/obese, and increased weight status over time increases the risks of poorer future health. Motor skill competence may be a protective factor, giving children the ability to participate in health-enhancing physical activity. Yet, we do not know when the relationship between motor competence and weight status first emerges or whether it is evident across the body mass index (BMI) spectrum. This study examined the association between motor skill competence and BMI in a multi-country sample of 5545 preschoolers (54.36 ± 9.15 months of age; 50.5% boys) from eight countries.
Methods
Quantile regression analyses were used to explore the associations between motor skill competence (assessed using the Test of Gross Motor Development, Second/Third Edition) and quantiles of BMI (15th; 50th; 85th; and 97th percentiles), adjusted for sex, age in months, and country.
Results
Negative associations of locomotor skills, ball skills, and overall motor skill competence with BMI percentiles (p < 0.005) were seen, which became stronger at the higher end of the BMI distribution (97th percentile). Regardless of sex, for each raw score point increase in locomotor skills, ball skills, and overall motor skill competence scores, BMI is reduced by 8.9%, 6.8%, and 5.1%, respectively, for those preschoolers at the 97th BMI percentile onwards.
Conclusions
Public health policies should position motor skill competence as critical for children’s obesity prevention from early childhood onwards. Robust longitudinal and experimental designs are encouraged to explore a possible causal pathway between motor skill competence and BMI from early childhood.
1. Background
Childhood obesity is a serious public health concern, with adverse consequences for health and well-being. In 2016, the number of boys and girls aged 5–19 years with obesity, as measured by the body mass index (BMI), were estimated to be approximately 74 and 50 million, respectively [1]. According to the World Health Organization, 39 million under 5-year-old individuals were overweight or obese in 2020 [2]. This represents serious implications for future generations, as early childhood is a critical time for the development of obesity, with BMI trajectories being established by 5 years of age [3, 4], and obesity in childhood extending into adolescence and adulthood [5].
A conceptual model described by Stodden et al. [6] suggested that healthy (or risky) weight status might be partially the consequence of a positive (or negative) spiral of physical activity (PA) engagement driven by motor competence (MC), a latent concept that reflects the degree of proficient performance in motor skills, the underlying mechanisms, and PA engagement. This model suggests that during early childhood, a positive relationship between MC and PA might lead to a healthy weight status, providing the basis for a positive trajectory of health for children and across the life course. Moreover, an age-appropriate level of MC is critical not only for a healthy BMI [7], but also for developing and maintaining adequate physical fitness levels [8, 9], executive functions and academic achievement [10, 11], psychological, emotional and social outcomes [11], and PA [12].
In 2010, Lubans et al. [13] provided early evidence of a consistent inverse association between MC and weight status. Recently, Barnett et al. [14] examined longitudinal and experimental evidence for MC and health outcomes. In this review, bidirectional relationships were explored, as it is not only plausible that children who are less active will have less opportunity to develop their MC, but also that children who are heavier may find it challenging to engage in certain physical activities and therefore, over time their MC would be lower. Authors of this review reported that nine studies investigated the pathway from weight status to MC, and five studies investigated the reverse pathway. However, only a single study comprised children in the preschool years (age 5 years). The results highlighted a strong bi-directional inverse association between children’s MC and weight status. However, neither of these reviews could quantify the strength of the relationship between MC and BMI, determine when it first occurred, or identify if the relationship was present across the BMI spectrum. In addition, the use of different protocols for MC assessment have made synthesis challenging.
Early childhood is a pivotal period for children to build foundational movement capacities in order to then progress to context-specific PA application in middle childhood, adolescence, and adulthood [15]. Optimal early child development is the basis of adult health and well-being. It is also a critical component of the United Nations Sustainable Development Goals, and it is essential to enable everyone to reach their full human potential [16]. Therefore, it is critical to focus specifically on the MC-BMI association in the preschool years (age 3–5 years), a crucial period for the development of MC. Thus, this study examined the association between MC and BMI in a pooled data of preschoolers from eight countries, in which similar assessment protocols were followed. We hypothesize that even at preschool ages, a negative association between MC and BMI is observed and that this association was likely to be more present for those with unhealthy BMI. In the current review, we situate BMI as the outcome variable and MC as the predictor, although we acknowledge the potential reciprocal relationship.
2. Methods
2.1. Data Sources and Participants
This study represents a large multicenter collaboration between motor development researchers from different countries. The targeted age range was 3–5 years, aligning with the preschool age range in most countries. From December 2020 up to mid-September 2021, possible collaborators who had used the Test of Gross Motor Development (TGMD, Second or Third Edition) in preschoolers between 2010 and 2020, before the COVID-19 lockdown, were identified. The TGMD is commonly used among preschool children [17], and scores derived from it show good-to-excellent support for a valid and reliable assessment in children and adolescents [18, 19].
Methods to identify collaborators included: (i) an extensive search on international databases (Web of Science, PubMed, and Scopus) of the fundamental movement skills or MC literature in preschool years and (ii) from a list of participants’ contacts of the International Motor Development Research Consortium (https://www.i-mdrc.com), to identify the relevant sources of information. Additionally, bibliographic references of the studies identified in the databases were also searched to make the search more sensitive. A total of 39 possible collaborators from 28 different countries (Australia, Belgium, Brazil, Canada, Chile, China, Colombia, England, Finland, Germany, Greece, Indonesia, Iran, Ireland, Italy, Macedonia, Malaysia, Mozambique, Netherlands, New Zealand, Norway, Portugal, Spain, South Korea, South Africa, Turkey, USA, and Wales) were identified.
Initial contact was undertaken through e-mail to: (a) the corresponding author of each study and (b) possible collaborators identified through international networks that could have microdata on the specific age range. This first contact invited collaborators to participate in the study and to provide their data for analysis. Subsequently, a second e-mail was sent to the corresponding author and to the last author (when available) of the studies who did not respond to the first e-mail sent in the previous step.
From those 39 possible collaborators, responses were obtained from 34 contacts (response rate = 87.2%). From the 34 responders, data sets of 16 could not be incorporated into the study because (a) there was no local ethics approval for data sharing; (b) the sample size was less than 100 participants; (c) the age range was inappropriate; and (d) there was a lack of strict adherence to the TGMD protocol (i.e., did not administer the entire protocol). Thus, this study pooled data from 18 collaborators from eight different countries (Australia, Belgium, Brazil, China, England, Italy, Spain, and USA), located in three of the six World Health Organization regions (East Asia and Pacific, Europe and Central Asia, and Latin America and the Caribbean), and comprising two country-specific income levels, according to the World Bank (high and upper-middle) [20].
Data from each of the collaborators were inserted into a template Excel file comprising the following information: age in months; sex; BMI; individual skill scores; locomotor, ball skills subscale scores, and total scores. Then, data were shared, and securely stored in a cloud store administered by Coventry University (UK). Data sets from the same country were merged to facilitate the analysis, thereby operationalizing a country-specific condition as a unit of clustering. The pooled data included 5545 preschoolers, both boys and girls aged 3–5 years. A flow diagram presenting details about the datasets included is shown in Fig. 1.
Fig. 1.
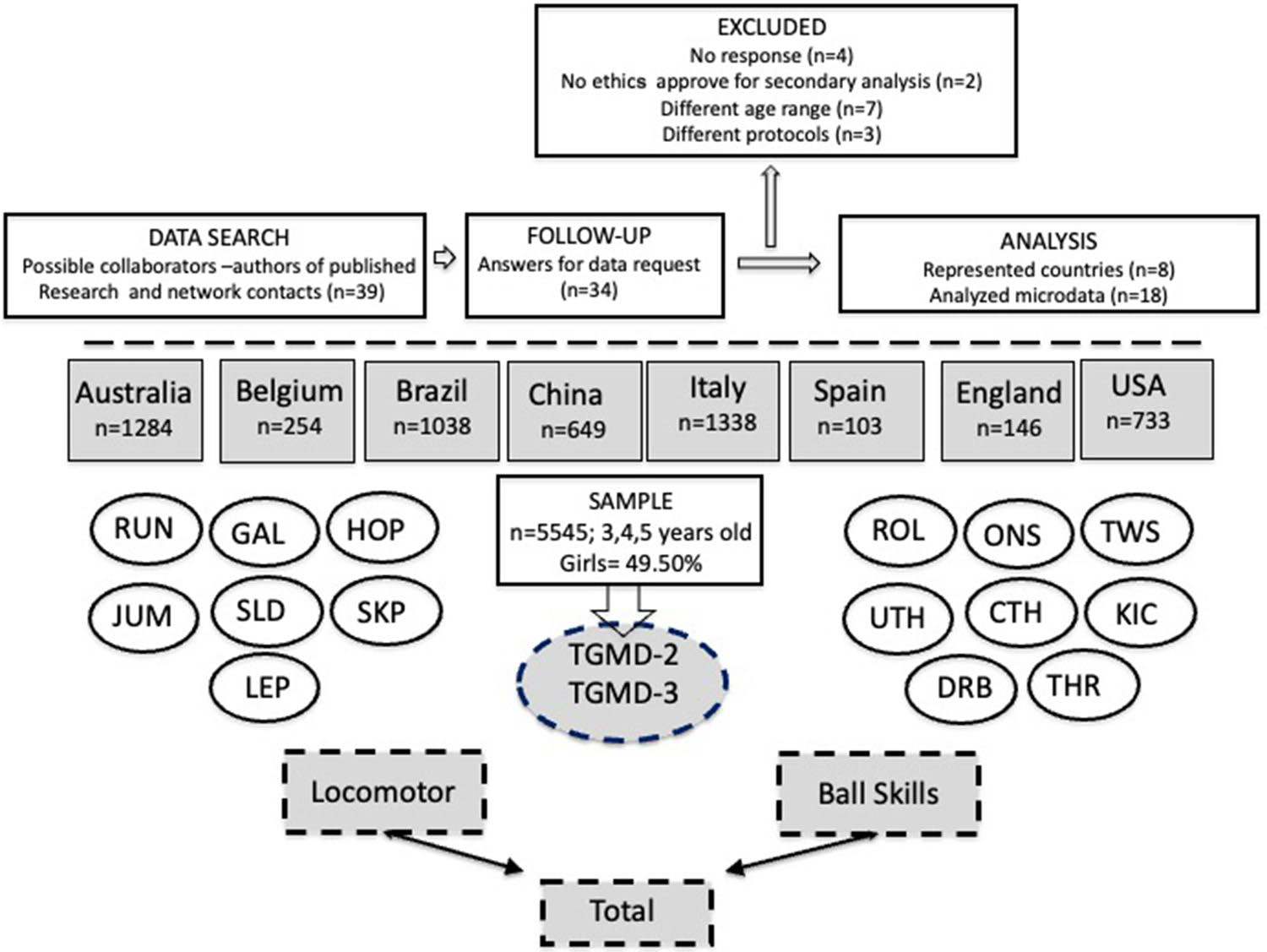
Flowchart of procedures for data acquisition and variables of the study. CTH catch, DRB dribble, GAL gallop, HOP hop, JUM jump, KIC kick, LEP leap, ONS one hand strike, ROL roll, RUN run, SKP skip, SLD slide, TGMD Test of Gross Motor Development, THR throw, TWS two-hand strike, UHT underhand throw
The smallest country samples were from England (n = 146) and Spain (n = 103), while the largest samples were from Australia (n = 1284) and Italy (n = 1338). Almost all the countries have data from varying locations, with the exception of Spain and England. Three participating countries (Brazil, China, and USA) provided information from both the Second and Third Editions of the TGMD protocol. Detailed information is available in Table 1 of the Electronic Supplementary Material (ESM).
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies were adhered to for the current study [21]. Ethics committees in their respective countries approved all the main studies, ensuring the written informed consents from all parents/guardians were provided for the original study, and took responsibility for permission for sharing data for the secondary analysis (detailed information is provided in Table 1 of the ESM).
2.2. Independent Variable
Data on MC were shared by each country contact and included the assessment protocol. For this, the TGMD-2 [22] and the TGMD-3 [23] were used. The TGMD evaluates gross motor performance in children aged 3–10 years and consists of a protocol to assess process-oriented fundamental movement skills during childhood, including in preschool children. The TGMD includes a comprehensive battery of gross motor skills comprising both locomotor and ball skills. It can be used to identify children who are significantly behind their peers in gross motor skills, to plan programs to improve MC in those children showing delays, and to assess changes as a function of increasing age, experience, instruction, or intervention [22–24].
The TGMD-2 consists of a two-factor test, with six locomotor skills (run, gallop, hop, leap, horizontal jump, and slide) and six object control skills (two-hand strike, dribble, catch, kick, overhand throw, and underhand roll). The TGMD-3 test also consists of two factors, but with 13 total skills, six locomotor skills (run, gallop, hop, skip, horizontal jump, and slide), and seven ball skills (one-hand strike, two-hand strike, dribble, catch, kick, overhand throw, and underhand throw). Research examining the criterion validity of the TGMD-3 and the TGMD-2 showed nearly perfect correlations between performance on the locomotor, ball skills, and total TGMD scores (all r = 0.98) [23].
According to the procedures, children practiced each skill once and then had to perform each skill twice. For each trial, a child receives a score of “1” if the performance criteria for that skill (e.g., stepping with foot opposite the throwing arm) is performed correctly and a score of “0” if the criterion is performed incorrectly. The locomotor and ball skills scores are based on the presence (one) or absence (zero) of each performance criterion. The raw scores are summed to create a locomotor and ball skills subscale score. The overall MC score is created by the sum of these two subscale scores. In all but one of the original projects, each collaborator’s team video recorded all the skills trials and were later assessed by trained assessors who did not administer the tests and had prior experience coding this assessment. The exception is for Belgian children, who were assessed live by trained administrators (not through video recording) [25]. All collaborators who participated in the project have ample experience in motor development research and significant experience in using, analyzing, and interpreting motor skill assessments like the TGMD. Evidence of TGMD assessment reliability was previously presented in the main original studies from Spain, Italy, Brazil, Australia, USA, Iran, and Belgium [25–34]. Feedback results to all parents of all participants were provided.
2.3. Outcome
In all studies, data collectors measured a child’s height (without shoes, to the nearest 0.1 cm, using wall-mounted stadiometers) and weight (to the nearest 0.1 kg, using research-grade scales). Shoes and heavy outwear/jackets were removed for these measurements. BMI was calculated as kg/m2. Children were classified according to the World Health Organization child growth standards for children younger than 5 years [35], and for children that were 5 years and above at the date of measurement [36] as underweight (15th percentile), normal weight (15th ≥ 85th percentile), overweight (≥ 85th percentile), and obese (≥ 97th percentile). The median value (50th percentile) was also calculated to characterize the continuum of BMI distribution. BMI continuous values were used as the outcome variable in the regression models.
2.4. Statistical Analysis
All analyses were performed in Stata 17.0. Data from countries were pooled into a single dataset for analyses, which was performed for the whole sample. No imputation of information was performed, and missing data, corresponding to 3.3% of the total sample, were excluded for analysis (detailed information in Table 1 of the ESM). Then, data were stratified by age and sex. BMI categories were used to describe the sample.
Data normality and homogeneity tests were conducted. Sex differences were examined using the independent t-test and Cohen’s d effect size [37]. Quantile regression [38, 39] was used to estimate the changes in BMI (outcome variable) as a function of change in MC (locomotor, ball skills, and overall MC), sex, and age (exposures). This procedure was based on the minimization of weighted absolute deviations (L_1 method) to estimate conditional quantile (percentile) functions [40]. For the median (quantile = 0.5), symmetric weights were used, and for all other percentiles (e.g., 15th, 85th, and 97th) asymmetric weights were employed. In contrast, classical ordinary least-square regression (also known as the L_2 method) estimates conditional mean functions. Unlike regular linear regression, quantile regression is not limited to explaining the mean of the dependent variable. It can be employed to explain the determinants of the dependent variable at any point of the distribution, estimating the conditional median of the target-dependent variable.
For this study, three quantile regression models were created to explore possible associations. First, a model comprising sex, age in months, and locomotor skills scores as independent variables, and percentiles of BMI (15th, 50th, 85th, and 97th) as the dependent variable was created. Subsequently, models for ball skills scores and overall MC scores were created. All the three models were adjusted for the country from where the data were collected.
3. Results
The final dataset included 5545 preschoolers from eight countries. Preschoolers were of a similar age (54.36 ± 9.15 months), and equivalent representativeness between boys and girls was achieved (50.5% boys). Different weight status profiles, according to BMI, were seen for children in all age groups (by years). Differences between sexes within ages were seen for ball skills and for overall MC scores, with boys outperforming girls (Table 1).
Table 1.
Participants characteristics
| Age | 3 years M (SD) | d | 4 years M (SD) | d | 5 years M (SD) | d | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Sex | Boys (n = 690) | Girls (n = 649) | Boys (n = 1107) | Girls (n = 1230) | Boys (n = 1004) | Girls (n = 865) | |||
|
| |||||||||
| LOC | 15.31 (8.70) | 14.95 (8.70) | 0.04 | 24.39 (10.54) | 24.52 (10.75) | 0.08 | 26.05 (9.26) | 26.85 (9.00) | 0.09 |
| BALT, | 15.18 (8.52) | 13.03 (7.90)* | 0.26 | 23.41 (10.31) | 21.21 (10.28)* | 0.37 | 26.29 (9.68) | 22.46 (8.75)* | 0.41 |
| Overall | 30.49(15.41) | 27.98 (14.85)* | 0.17 | 47.80(19.07) | 45.72 (19.03)* | 0.16 | 52.34 (16.49) | 49.31 (15.40)* | 0.19 |
| BMI | 16.28 (1.86) | 16.12 (2.04) | 0.08 | 16.17(2.05) | 16.20 (2.06) | 0.01 | 16.51 (2.28) | 16.35 (2.56) | 0.07 |
| N (%) of children in WHO categories for BMI | |||||||||
| Under | 56 (8.1%) | 53 (8.3%) | 79 (7.1%) | 71 (5.80%) | 49 (4.9%) | 56 (6.5%) | |||
| Normal | 415 (60.2%) | 421 (64.8%) | 703 (63.5%) | 839 (68.2%) | 580 (57.8%) | 563 (65.0%) | |||
| Over | 141 (20.4%) | 116(17.9%) | 203 (18.3%) | 200 (16.3%) | 235 (23.4%) | 160 (18.5%) | |||
| Obese | 78 (11.3%) | 59 (9.1%) | 122 (11.0%) | 120 (9.8%) | 140(13.9%) | 86 (10.0%) | |||
BALL ball skills, BMI body mass index, d Cohen's effect size, LOC locomotor skill score, M mean. Over overweight. Overall overall motor competence score, SD standard deviation. Under underweight, WHO World Health Organization
Studenťs t test for paired samples of sex comparation; significant difference;
p < 0.001
The quantile regression estimating the effects of MC on changes in BMI are presented in Table 2. The results showed negative and statistically significant associations of locomotor skills, ball skills, and overall MC with BMI percentiles (p < 0.005), which became stronger at the higher end of the BMI distribution (97th). The results indicated that at this point, for each increase in the locomotor skills subscale score by one point, BMI is reduced by 8.9% (p < 0.001). Moreover, at the 97th BMI percentile, the coefficient for the association indicates that for each increase in the ball skill subscale score, BMI is reduced by 6.8% (p < 0.001). For the overall MC scores, the negative association with the BMI percentile was also stronger at the higher end of the distribution, showing a 5.1% reduction in BMI, when one raw score point of the overall MC score is increased. The results also showed an association between sex and BMI in favor of boys, but for those at the end of the BMI distribution (97th), whereas no association between sex and BMI was observed for the three models. Finally, a positive association with age and BMI was observed (i.e., older children tended to have higher BMI) once they were above the 50th percentile (median). The R2 values indicated that the three models could better explain the variance in BMI for those children classified at the 97th percentile of the BMI distribution.
Table 2.
Association between MC and BMI percentiles, considering sex and age in months
| Locomotor skills | Ball skills | Overall MC | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||||
| BMI percentile | Value | Std. Error | 95% CI | Pr (>|t|) | BMI percentile | Value | Std. Error | 95% CI | Pr (>|t|) | BMI percentile | Value | Std. Error | 95% CI | Pr (>|t|) |
|
| ||||||||||||||
| 0.15 | R2 = 0.016 | R2 = 0.020 | R2 = 0.019 | |||||||||||
| Cons | 14.939 | 0.181 | 14.584; 15.295 | 0.001 | Cons | 14.870 | 0.221 | 14.434; 15.304 | 0.001 | Cons | 14.896 | 0.175 | 14.551; 15.240 | 0.001 |
| Sex | −0.150 | 0.056 | −0.262; −0.040 | 0.008* | Sex | −0.192 | 0.064 | −0.318; −0.066 | 0.003* | Sex | −0.177 | 0.068 | −0.311; −0.041 | 0.010* |
| Age | 0.004 | 0.004 | −0.003; 0.011 | 0.308 | Age | 0.007 | 0.004 | −0.009; 0.016 | 0.079 | Age | 0.008 | 0.003 | 0.001; 0.014 | 0.022* |
| Locom | −0.009 | 0.004 | −0.017; −0.001 | 0.030* | Ball | −0.018 | 0.003 | −0.024; −0.010 | <0.001* | Overall | −0.009 | 0.002 | −0.013; −0.005 | <0.001* |
| 0.50 | R2 = 0.009 | R2 = 0.011 | R2 = 0.011 | |||||||||||
| Cons | 15.998 | 0.179 | 15.647; 16.349 | 0.001 | Cons | 15.972 | 0.149 | 15.679; 16.265 | 0.001 | Cons | 15.920 | 0.215 | 15.497; 16.341 | 0.001 |
| Sex | −0.140 | 0.048 | −0.236; −0.045 | 0004* | Sex | −0.220 | 0.066 | −0.349; −0.092 | <0.001* | Sex | −0.185 | 0.061 | −0.307; −0.064 | 0.003* |
| Age | 0.008 | 0.003 | 0.002; 0.014 | 0.007* | Age | 0.010 | 0.003 | 0.003; 0.016 | 0.004* | Age | 0.012 | 0.004 | 0.005; 0.019 | <0.001* |
| Locom | −0.014 | 0.003 | −0.020; −0.008 | <0.001* | Ball | −0.018 | 0.003 | −0.025; −0.011 | <0.001 | Overall | −0.010 | 0.002 | −0.015; −0.005 | <0.001* |
| 0.85 | R2 = 0.025 | R2 = 0.027 | R2 = 0.032 | |||||||||||
| Cons | 16.683 | 0.245 | 16.201; 17.165 | 0.001 | Cons | 16.516 | 0.290 | 15.945; 17.086 | 0.001 | Cons | 16.540 | 0.262 | 16.024; 17.055 | 0.001 |
| Sex | −0.069 | 0.140 | −0.343; 0.205 | 0.622 | Sex | −0.2512 | 0.086 | −0.421; −0.080 | 0.004* | Sex | −0.188 | 0.103 | −0.390; 0.014 | 0.069 |
| Age | 0.034 | 0.005 | 0.024; 0.044 | <0.001* | Age | 0.035 | 0.005 | 0.025; 0.045 | <0.001* | Age | 0.043 | 0.006 | 0.032; 0.053 | <0.001* |
| Locom | −0.049 | 0.006 | −0.061; −0.036 | <0.001* | Ball | −0.052 | 0.008 | −0.068; −0.035 | <0.001* | Overall | −0.035 | 0.004 | −0.041; −0.027 | <0.001* |
| 0.97 | R2 = 0.170 | R2 = 0.163 | R2 = 0.171 | |||||||||||
| Cons | 16.922 | 0.779 | 15.393; 18.450 | 0.001 | Cons | 16.777 | 0.761 | 15.283; 18.270 | 0.001 | Cons | 16.920 | 0.860 | 15.234; 18.607 | 0.001 |
| Sex | 0.078 | 0.226 | −0.367; 0.520 | 0.736 | Sex | −0.247 | 0.207 | −0.652; 0.159 | 0.233 | Sex | −0.123 | 0.276 | −0.665; 0.418 | 0.655 |
| Age | 0.079 | 0.016 | 0.045; 0.110 | <0.001* | Age | 0.072 | 0.013 | 0.046; 0.098 | <0.001* | Age | 0.081 | 0.015 | 0.052; 0.111 | <0.001* |
| Locom | −0.089 | 0.013 | −0.116; −0.0062 | <0.001* | Ball | −0.068 | 0.015 | −0.098; −0.039 | <0.001* | Overall | −0.051 | 0.007 | −0.065; −0.037 | <0.001* |
BMI body mass index, CI confidence interval, Cons Constant, MC motor competence, PR Probability of t-distribution, R2 pseudo R2, Std. Error standard error Analyses are adjusted by country
Pr(>t) < 0.05
The quantile regression models between MC and BMI for the whole sample (Panel A), and stratified by age in years (Panels B, C, and D) are presented in Fig. 2. The graphs show that there is a generally negative effect of MC scores on BMI, especially at the end of the BMI distribution (85th and 97th percentiles), for the three age groups. Detailed information is available in Table 2 of the ESM.
Fig. 2.
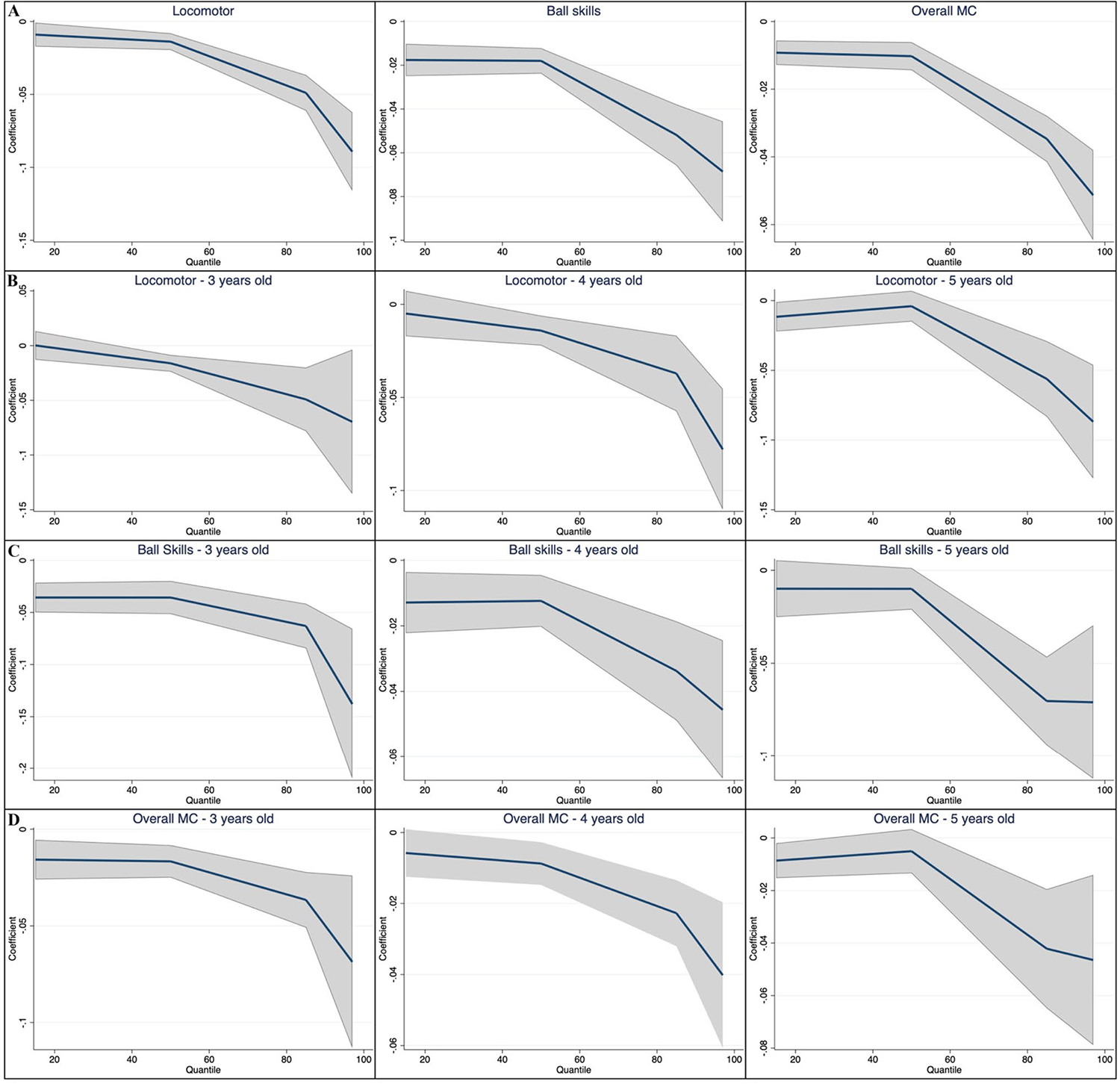
Coefficients and 95% confidence intervals of quantile regression models between motor competence (MC) and body mass index for the whole sample (A), and stratified by age in years (B–D)
4. Discussion
This is the first study to analyze the association between MC and BMI across the whole spectrum of its distribution in a large multi-country sample of preschoolers. The key findings from the quantile regression demonstrated a negative association between overall MC (and its domains) and BMI. Importantly, this relationship is markedly strengthened at the higher end of the BMI distribution (85th and 97th). Although we acknowledge the potential reciprocal relationship, in the current study, when situating BMI as the outcome variable and MC as the predictor, our results suggest that developing MC could potentially have a larger impact in preschoolers who are overweight and obese.
Children classified as obese at a young age are of concern, as overweight/obese young children rarely change to normal weight as a consequence of the growth process [41]. Therefore, the evidence reported in the current study is important as it shows that at a young age, weight status is different according to MC levels. Our multi-country crosscultural sample of preschoolers, assessed using the same standardized protocol, might suggest that even at early ages, facilitating the development of MC may be an important intervention strategy to consider. This is because, based on the theoretical background, we could speculate that the development of MC at early ages could assist preschoolers to be more physically active, thereby starting them on a positive spiral of engagement, which may positively assist their weight status in the long term [6, 42].
In the review by Barnett et al. [14], which focused on longitudinal and experimental studies, overall evidence for a negative association between BMI and MC was reported, though this evidence was not quantified. Moreover, only one of the studies included in that review targeted preschoolaged children [43]. This specific study reported that a higher BMI at 5 years of age contributed to declines in the MC level (as measured by the Bruininks-Oseretsky Test of Motor Proficiency Short Form) [44]) of 668 children, though no support for the reverse causality pathway was observed (i.e., poor MC at 5 years of age did not predict a BMI increase at 10 years of age) [43]. This longitudinal study used a different assessment of motor skill compared to the current study (i.e., concerning skill outcome, product, as compared to the skill, process), but this does not fully explain why the study did not find an association. An explanation might be that skill level was not differentiated enough in this specific 5-year-old sample to be able to determine subsequent weight status. It could also be argued that in young children, the relationship between MC and BMI/weight status is not as evident as in older children because the development of overweight/obesity takes time, during which a disbalance between energy uptake and energy expenditure continues, which is why large samples are needed with enough children across the weight status and skill continuums. The present study addresses this point by virtue of its multi-center approach of pooled data.
Of course, it is not possible to establish direction or causality in a cross-sectional study. It is also likely that being of a larger weight impacts a child’s ability to learn and develop movement skills successfully [45]. The aforementioned systematic review by Barnett et al. [14] also investigated the reciprocal pathway (i.e., weight status to MC), providing support for a negative association. Hence, this relationship is likely to be reciprocal, supporting the model proposed by Stodden et al. [6]. Indeed, excessive body weight is a clear barrier to MC development, as overweight/obese children may have challenges participating in some physical activities and sports, particularly those involving locomotor skills such as running, which need to propel the body through space [46].
In older children and adolescents, two studies that explored the bi-directional relationship between MC and indicators of obesity were located. The findings support a longitudinal association for the pathway from MC to weight status. For example, in a 7-year longitudinal study with children and adolescents (aged 6–13 years), Lima et al. [47] reported that children with higher MC (measured as motor coordination with the Körperkoordinationstest für Kinder) at baseline had a lower risk of having higher body fatness (βboys = − 0.45, 95% confidence interval − 0.52 to − 0.38; βgirls = − 0.35, 95% confidence interval − 0.42 to − 0.28). In adolescents aged 12–13 years, when assessing the pathway from MC to BMI, a moderate-to-high negative correlation across a 2-year period was reported, emphasizing poorer MC (measured with the Körperkoordinationstest für Kinder), as a significant predictor of body fat over time (B = − 0.05, p = 0.05), even after adjusting for potential confounders [48]. In the first study, Lima et al. [47] does not state whether baseline BMI was adjusted for, but in the second study by Chagas et al. [48], weight and height were adjusted for, indicating the possibility that our associations in the preschool years may continue as children develop, potentially impacting them into the future. It should be noted though that measures of MC in both studies were restricted to motor coordination.
Our results also showed an important finding according to MC domains. A negative association was seen for both locomotor and ball skills, that was markedly stronger at the 97th percentile of BMI, suggesting 8.9% and 6.8% reductions in BMI for each score unit increase in locomotor and ball skills, respectively. Although locomotor and ball skills are reasonably correlated (r = 0.84–0.96) [49], they should be differentiated, given their distinctive differences in the timing of acquisition and their independent importance towards predicting health behaviors [14, 42]. Moreover, when considering age groups (Table 3 of the ESM), consistent negative associations for MC and its domains with BMI were seen at the 85th and 97th percentiles of the BMI distribution, reinforcing the main results for the whole sample.
It is challenging to compare our results stratified by age because in general, studies that investigate preschoolers tend to use one single sample, and differences according to age are not necessarily highlighted. Slaton et al. [50], in a statewide sample of 588 US preschoolers, showed that ball skills, but not locomotor skills related positively to attaining global PA guidelines. From a developmental perspective, locomotor skill mastery is achieved before ball skills [51]. At these young ages, children are expected to have sufficient proficiency in locomotor skills such as running, galloping, and jumping, allowing them to engage in activities in which these specific skills are required because a significant part of their body is in motion. For those children who are overweight or obese, the excess mass may hamper movement from a mechanical point of view. However, there is evidence that later in life, PA and ball skills are positively associated [52]. In fact, it is expected that as they grow, children should have the motor proficiency necessary to be engaged in more intense-level recreational and sports activities, which theoretically could have a positive impact on BMI. Nonetheless, extrapolations on the role of PA in the analyzed associations are merely theoretical, as PA data were not available.
Our results clearly show an inverse association between MC and BMI. Although the cross-sectional evidence cannot establish causality, our results could suggest that improving both locomotor and ball skills in overweight/obese children could be a promising intervention strategy to promote PA, and consequently, a healthy BMI. However, this would need to be tested in trials that also measure PA, as in this scenario, PA engagement is posed as the possible mechanism to improve MC, thereby impacting weight status. From a clinical point of view, and when considering children at the obese end of the spectrum, the observed reductions in BMI of around 5.1% for overall MC, or of approximately 8.9% and 6.8% when considering locomotor and ball skills mastery, respectively, are tremendously relevant. For instance, total MC scores vary substantially (i.e., from 0 to 100 in the TGMD-3), with higher values representing better performance. Thus, in a hypothetical linear scenario, for those children at higher BMI percentiles, the margin of BMI reductions that could potentially be achieved through developing MC (considering the increased PA levels as a potential mechanism) could be extremely significant.
Our results also showed that for all the age groups (3-year-old, 4-year-old, and 5-year-old children), the association between sex and BMI in favor of boys disappears at the 85th and 97th percentiles of the BMI distribution, meaning that weight status similarly affects boys and girls who are categorized as overweight or obese, even at these young ages. Although biologically girls are more likely to gain weight, this fact occurs during adolescence. In childhood, excessive weight is a multi-factorial condition also determined by genetic, environmental, and lifestyle conditions [53] and in general, commonly affects boys and girls similarly. Finally, older children are likely to exhibit a higher BMI than younger children. In fact, being older and male are consistent predictors of better MC, especially concerning ball skill performance [34], suggesting that sex and age differences in preschoolers’ performance could magnify health risk outcomes, such as BMI. Moreover, as young children are growing (up to the age of 5 years), our results show that the negative association of MC with BMI became more evident for those at the 97th distribution onwards. Based on the vast number of young children who are overweight and obese worldwide, this is a significant public health concern for healthcare systems and individual health and well-being [54].
Promoting children’s healthy development is crucial for the future of our societies. The global burden of child and youth physical inactivity and obesity remains high, and stark inequalities exist. Among girls and in low-income and middle-income countries in particular, physical inactivity and obesity are serious concerns, though these factors affect children in all countries across the globe during the key developmental stages of the preschool years [55]. Understanding additional potential factors that have a positive impact on obesity and physical inactivity early in life, such as children’s MC, are vital to mitigating their lasting effects.
One of the major strengths of this study is its multi-country sample. Prior studies included a wide age range; and were generally restricted to data from developed countries, which may partially justify the moderate-to-high risk of biases or inconsistencies previously reported [14]. Presenting a multi-country view of the association between MC and BMI, combining countries from different regions, and also middle-income countries is an important strength, as the vast majority of children in the world live in low-income and middle-income countries, but they are highly under-represented in the literature base [56]. Moreover, the use of a quantile regression analysis, which is agnostic for data distribution [57] and robust to response outliers, allows modeling of the entire conditional distribution of BMI (which clearly does not show a Gaussian distribution) over the preschool years (Fig. 1 of the ESM).
This study is limited by not having the variable of PA to be able to test the mechanism of the relationship between MC and weight status. Health-related fitness and perceived competence are other important factors within the Stodden et al. [6] model that are not included in our present study. However, it must be noted that attempting to understand and synthesize all the pathways in this model is complex owing to the sheer number of studies, and also the measurement complexities, as highlighted in the Barnett et al. [14] review. Likewise, there is an acknowledged developmental trajectory of both MC and weight status, influenced by a range of factors (e.g., growth and maturation, genetics, movement behaviors, affordances in the physical and social environment), that need to be taken in account in future studies.
It is important to note that in our study, our inclusion criteria were for MC to be assessed using the TGMD, which includes skills that are not as applicable in different cultural contexts. For example, the two-handed strike is more relevant in countries that have sports such as baseball, softball, and cricket. The expertise of the evaluators in scoring the skill criteria is another limitation point to be recognized in terms of the inter-rater reliability between studies that are conducted within different research centers [58]. Although, it is essential to recognize that if we selected a MC assessment for our inclusion criteria that was product oriented (e.g., based on a time rather than movement proficiency), we would have improved the reliability of assessment between studies, but we would have other different limitations (e.g., the Körperkoordinationstest für Kinder does not assess ball skills). Furthermore, the cross-sectional information at different timepoints in each country was used for the analysis and there are differences in the sample size between countries and ages. Additionally, the greatest confidence intervals observed for the associations, especially at the higher end of the BMI distribution, are expected as data present a non-normal distribution, and do not precisely represent the population mean. Nonetheless, the quantile regression method allows an estimation of the conditional percentiles of the outcome variable, in contrast to the method of least squares that estimates the conditional mean.
The current study provides evidence-based information to encourage public policies and recommendations to strengthen MC in the preschool years. We recommend that future large international efforts should be made to investigate longitudinal associations between MC and weight status across early childhood, late childhood, adolescence, and adulthood. We also recommend that representative information on MC be gathered, in order to understand the global interpretation of its impacts on children’s weight status and possible inequalities. For example, gender differences are consistently observed for specific subscales of MC, or for the overall MC, even at this young age group. It is also of great importance to understand and address other social inequalities in MC across contexts, such as income inequalities, that impact on children’s weight status [54].
5. Conclusions
We report a negative association between MC and BMI for preschoolers that is markedly stronger at the higher end of the BMI distribution. Our findings reinforce that public health policies should better position MC as critical for children’s healthy weight status at early childhood. Robust longitudinal and experimental designs are encouraged to explore a possible causal pathway between MC and BMI from early childhood.
Supplementary Material
Key Points.
In preschool age children, there are already significant negative associations between motor skill competence (locomotor, ball, and total scores) and body mass index.
These associations became stronger for preschoolers who are classified as obese, regardless of sex.
Developing preschoolers’ motor skill competence is recommended as part of a comprehensive approach to improving healthy weight status development.
Funding
Funding for the original projects was obtained by the following co-authors: DM, FC and FM were supported by the Fondo Assistenza e Benessere S.M.S (FAB), Fondazione Cassa di Risparmio di Asti, Polo Universitario Asti Studi Superiori (UNI-Astiss) and Città di Asti for the “Benessere in Gioco” project. ML and FB were supported for the Multimove for Kids project by the Flemish Government. IE was supported by the Generalitat Valenciana, Conselleria de Innovación, Universidades, Ciencia y Sociedad Digital (project APE/2021/013). AES and LKW were supported by NIH NICHD R21HD095035; Gulf States-HPC from the NIHMD NIH (U54MD0086 02), P30DK072476, U54GM104940, and the LSU Biomedical Collaborative Research Program. LER was partially supported by the National Institutes of Health under the National Heart, Lung, and Blood Institute (1R01HL132979). AO, PC, and RJ were supported by The Australian Data from New South Wales, using funding from the National Health and Medical Research Council of Australia (APP1062433). LMB accessed data from The Melbourne INFANT Program follow-ups that were funded by a National Health and Medical Research Council Project Grant (GNT1008879). PRB was supported by the Scholarship Program for Productivity in Research and Stimulus to Interiorization and Technological Innovation—BPI (04–2022).
Footnotes
Conflicts of Interest/Competing Interests All the authors declare no funding, employment, financial or non-financial conflicts of interest.
Declarations
Ethics Approval This study was performed in line with the principles of the Declaration of Helsinki. Institutional review board/ethics committee approval was obtained by each collaborator’s institutional review board and is presented in Table 1 of the ESM.
Consent to Participate Not applicable.
Consent for Publication Not applicable.
Code Availability Not applicable.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s40279-023-01929-7.
Availability of Data and Material
Data generated or analyzed during this study are included in the article as tables, figures, and/or the ESM, and are available from the corresponding author on reasonable request.
References
- 1.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO fact-sheet: obesity and overweight. Geneva: World Health Organization; 2020. [Google Scholar]
- 3.Jabakhanji SB, Boland F, Ward M, Biesma R. Body mass index changes in early childhood. J Pediatr. 2018;202:106–14. [DOI] [PubMed] [Google Scholar]
- 4.Stuart B, Panico L. Early-childhood BMI trajectories: evidence from a prospective, nationally representative British cohort study. Nutr Diabetes. 2016;6(3): e198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nader PR, O’Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594–601. [DOI] [PubMed] [Google Scholar]
- 6.Stodden DF, Goodway JD, Langendorfer SJ, Roberton MA, Rudisill ME, Garcia C, et al. A developmental perspective on the role of motor skill competence in physical activity: an emergent relationship. Quest. 2008;60(2):290–306. [Google Scholar]
- 7.D’Hondt E, Deforche B, Gentier I, De Bourdeaudhuij I, Vaeyens R, Philippaerts R, et al. A longitudinal analysis of gross motor coordination in overweight and obese children versus normal-weight peers. Int J Obesity. 2013;37(1):61–7. [DOI] [PubMed] [Google Scholar]
- 8.Cattuzzo MT, Dos Santos HR, Re AH, de Oliveira IS, Melo BM, de Sousa MM, et al. Motor competence and health related physical fitness in youth: a systematic review. J Sci Med Sport. 2016;19(2):123–9. [DOI] [PubMed] [Google Scholar]
- 9.Utesch T, Bardid F, Büsch D, Strauss B. The relationship between motor competence and physical fitness from early childhood to early adulthood: a meta-analysis. Sports Med. 2019;49(4):541–51. [DOI] [PubMed] [Google Scholar]
- 10.van der Fels IM, Te Wierike SC, Hartman E, Elferink-Gemser MT, Smith J, Visscher C. The relationship between motor skills and cognitive skills in 4–16 year old typically developing children: a systematic review. J Sci Med Sport. 2015;18(6):697–703. [DOI] [PubMed] [Google Scholar]
- 11.O’Hagan AD, Behan S, Peers C, Belton S, O’Connor N, Issartel J. Do our movement skills impact our cognitive skills? Exploring the relationship between cognitive function and fundamental movement skills in primary school children. J Sci Med Sport. 2022;25(11):871–7. [DOI] [PubMed] [Google Scholar]
- 12.Jones D, Innerd A, Giles EL, Azevedo LB. Association between fundamental motor skills and physical activity in the early years: a systematic review and meta-analysis. J Sport Health Sci. 2020;9(6):542–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lubans DR, Morgan PJ, Cliff DP, Barnett LM, Okely AD. Fundamental movement skills in children and adolescents: review of associated health benefits. Sports Med. 2010;40(12):1019–35. [DOI] [PubMed] [Google Scholar]
- 14.Barnett LM, Webster EK, Hulteen RM, De Meester A, Valentini NC, Lenoir M, et al. Through the looking glass: a systematic review of longitudinal evidence, providing new insight for motor competence and health. Sports Med. 2022;52(4):875–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Black MM, Walker SP, Fernald LC, Andersen CT, DiGirolamo AM, Lu C, et al. Advancing early childhood development: from science to scale 1: early childhood development coming of age: science through the life course. Lancet. 2017;389(10064):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engle PL, Black MM, Behrman JR, Cabral de Mello M, Gertler PJ, Kapiriri L, et al. Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. Lancet. 2007;369(9557):229–42. [DOI] [PubMed] [Google Scholar]
- 17.Klingberg B, Schranz N, Barnett LM, Booth V, Ferrar K. The feasibility of fundamental movement skill assessments for preschool aged children. J Sports Sci. 2019;37(4):378–86. [DOI] [PubMed] [Google Scholar]
- 18.Hulteen RM, Barnett LM, True L, Lander NJ, del Pozo CB, Lonsdale C. Validity and reliability evidence for motor competence assessments in children and adolescents: a systematic review. J Sports Sci. 2020;38(15):1717–98. [DOI] [PubMed] [Google Scholar]
- 19.Alison G, Rachel T, Prue EM, Alicia JS. Psychometric properties of gross motor assessment tools for children: a systematic review. BMJ Open. 2018;8(10): e021734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The World Bank. DataBank. https://databank.worldbank.org/databases. Accessed 14 Mar 2023.
- 21.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Van-denbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. [DOI] [PubMed] [Google Scholar]
- 22.Ulrich D. Test of gross development: examiner’s manual. Austin: Pro-Ed; 2000. [Google Scholar]
- 23.Ulrich DA. TGMD-3: test of gross motor development. Austin: Pro-Ed; 2018. [Google Scholar]
- 24.Ulrich B, Ulrich D. The role of balancing ability in performance of fundamental motor skills in 3-, 4-, and 5-year-old children. In: Motor development: current selected research. Princeton, NJ: Princeton Book Company; 1985; p. 87–97. [Google Scholar]
- 25.Bardid F, Huyben F, Lenoir M, Seghers J, De Martelaer K, Goodway JD, et al. Assessing fundamental motor skills in Belgian children aged 3–8 years highlights differences to US reference sample. Acta Paediatr. 2016;105(6):e281–90. [DOI] [PubMed] [Google Scholar]
- 26.Estevan I, Clark C, Molina-García J, Menescardi C, Barton V, Queralt A. Longitudinal association of movement behaviour and motor competence in childhood: a structural equation model, compositional, and isotemporal substitution analysis. J Sci Med Sport. 2022;25(8):661–6. [DOI] [PubMed] [Google Scholar]
- 27.Magistro D, Piumatti G, Carlevaro F, Sherar LB, Esliger DW, Bardaglio G, et al. Psychometric proprieties of the Test of Gross Motor Development-Third Edition in a large sample of Italian children. J Sci Med Sport. 2020;23(9):860–5. [DOI] [PubMed] [Google Scholar]
- 28.Mota JG, Clark CCT, Bezerra TA, Lemos LFG, Reuter CP, Mota J, et al. Twenty-four-hour movement behaviours and fundamental movement skills in preschool children: a compositional and isotemporal substitution analysis. J Sports Sci. 2020;38(18):2071–9. [DOI] [PubMed] [Google Scholar]
- 29.Valentini N. Validity and reliability of the TGMD-2 for Brazilian children. J Mot Behav. 2012;44(4):275–80. [DOI] [PubMed] [Google Scholar]
- 30.Valentini NC, Zanella LW, Webster EK. Test of Gross Motor Development-Third Edition: establishing content and construct validity for Brazilian children. J Motor Learn Dev. 2017;5(1):15–28. [Google Scholar]
- 31.Salami S, Bandeira PFR, Gomes CMA, Dehkordi PS. The Test of Gross Motor Development-Third Edition: a bifactor model, dimensionality, and measurement invariance. J Motor Learn Dev. 2021;10(1):116–31. [Google Scholar]
- 32.Bandeira PFR, Duncan M, Pessoa ML, Soares Í, da Silva L, Mota J, et al. TGMD-2 Short Version: evidence of validity and associations with sex, age, and BMI in preschool Children. J Motor Learn Dev. 2020;8(3):528–43. [Google Scholar]
- 33.Garn AC, Webster EK. Bifactor structure and model reliability of the Test of Gross Motor Development-3rd edition. J Sci Med Sport. 2021;24(1):67–73. [DOI] [PubMed] [Google Scholar]
- 34.Barnett LM, Salmon J, Hesketh KD. More active pre-school children have better motor competence at school starting age: an observational cohort study. BMC Public Health. 2016;16(1):1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. WHO child growth standards: length/ height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization; 2006. [Google Scholar]
- 36.Md Onis, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cohen J. The effect size index: d. Statistical power analysis for the behavioral sciences. Abingdon-on-Thames: Routledge Academic; 1988. [Google Scholar]
- 38.Firpo S, Fortin NM, Lemieux T. Unconditional quantile regressions. Econometrica. 2009;77(3):953–73. [Google Scholar]
- 39.Gebregziabher M, Lynch CP, Mueller M, Gilbert GE, Echols C, Zhao Y, et al. Using quantile regression to investigate racial disparities in medication non-adherence. BMC Med Res Methodol. 2011;11:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Koenker R, Bassett G Jr. Regression quantiles. Econometrica. 1978;33–50. [Google Scholar]
- 41.Péneau S, Giudici KV, Gusto G, Goxe D, Lantieri O, Hercberg S, et al. Growth trajectories of body mass index during childhood: associated factors and health outcome at adulthood. J Pediatr. 2017;186:64–71.e1. [DOI] [PubMed] [Google Scholar]
- 42.Robinson LE, Stodden DF, Barnett LM, Lopes VP, Logan SW, Rodrigues LP, et al. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015;45(9):1273–84. [DOI] [PubMed] [Google Scholar]
- 43.Cheng J, East P, Blanco E, Kang Sim E, Castillo M, Lozoff B, et al. Obesity leads to declines in motor skills across childhood. Child Care Health Dev. 2016;42(3):343–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bruininks RH, Bruininks BD. The Bruininks-Oseretsky test of motor proficiency, 2nd Edn. MN: AGS Publishing Circle Pines; 2005. [Google Scholar]
- 45.Barros WMA, da Silva KG, Silva RKP, Souza A, da Silva ABJ, Silva MRM, et al. Effects of overweight/obesity on motor performance in children: a systematic review. Front Endocrinol (Lausanne). 2021;12: 759165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haapala EA, Väistö J, Lintu N, Tompuri T, Brage S, Westgate K, et al. Adiposity, physical activity and neuromuscular performance in children. J Sports Sci. 2016;34(18):1699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lima RA, Bugge A, Ersbøll AK, Stodden DF, Andersen LB. The longitudinal relationship between motor competence and measures of fatness and fitness from childhood into adolescence. J Pediatr (Rio J). 2019;95:482–8. [DOI] [PubMed] [Google Scholar]
- 48.Chagas DdV, Mohebbi M, Barnett ML. How important is motor competence for healthy weight status across adolescence? Childh Obes. 2021;17(3):220–7. [DOI] [PubMed] [Google Scholar]
- 49.Cools W, De Martelaer K, Samaey C, Andries C. Movement skill assessment of typically developing preschool children: a review of seven movement skill assessment tools. J Sports Sci Med. 2009;8(2):154. [PMC free article] [PubMed] [Google Scholar]
- 50.Slaton A, Kowalski AJ, Zemanick A, Pulling Kuhn A, Hager ER, Black MM. Motor competence and attainment of global physical activity guidelines among a statewide sample of preschoolers. Int J Environ Res Public Health. 2020;17(22):8546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morgan PJ, Barnett LM, Cliff DP, Okely AD, Scott HA, Cohen KE, et al. Fundamental movement skill interventions in youth: a systematic review and meta-analysis. Pediatrics. 2013;132(5):e1361–83. [DOI] [PubMed] [Google Scholar]
- 52.Barnett L, Van Beurden E, Morgan PJ, Brooks LO, Beard JR. Childhood motor skill proficiency as a predictor of adolescent physical activity. J Adoles Health. 2009;44(3):252–9. [DOI] [PubMed] [Google Scholar]
- 53.Lister NB, Baur LA, Felix JF, Hill AJ, Marcus C, Reinehr T, et al. Child and adolescent obesity. Nat Rev Disease Primers. 2023;9(1):24. [DOI] [PubMed] [Google Scholar]
- 54.Jebeile H, Kelly AS, O’Malley G, Baur LA. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022;10(5):351–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Aubert S, Brazo-Sayavera J, González SA, Janssen I, Manyanga T, Oyeyemi AL, et al. Global prevalence of physical activity for children and adolescents; inconsistencies, research gaps, and recommendations: a narrative review. Int J Behav Nutr Phys Activity. 2021;18:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Draper CE, Barnett LM, Cook CJ, Cuartas JA, Howard SJ, McCoy DC, et al. Publishing child development research from around the world: an unfair playing field resulting in most of the world’s child population under-represented in research. Infant Child Dev. e2375. 10.1002/icd.2375. [DOI] [Google Scholar]
- 57.Rodriguez RN, Yao Y. Five things you should know about quantile regression. Proceedings of the SAS Global Forum 2017; 2017; p. 2–5; Orlando (FL). [Google Scholar]
- 58.Hulteen RM, True L, Kroc E. Trust the “process”? When fundamental motor skill scores are reliably unreliable. Measurement in physical education and exercise science. 2023. p. 1–12. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data generated or analyzed during this study are included in the article as tables, figures, and/or the ESM, and are available from the corresponding author on reasonable request.


