Abstract
Objectives
In 2015 and 2016, WHO issued guidelines on HIV testing services (HTS) highlighting recommendations for a strategic mix of differentiated HTS approaches. The policy review examines the uptake of differentiated HTS approaches recommendations in national policies.
Methods
Data were extracted from national policies published between January 2015 and June 2019. The WHO-recommended HTS approaches included facility-based testing, community-based testing, HIV self-testing and provider-assisted referral (or assisted partner notification). Other supportive recommendations include pre-test information, post-test counselling, lay provider testing and rapid testing. Descriptive analyses were conducted to examine inclusion of recommendations in national policies.
Results
Of 194 countries worldwide, 65 published policies were identified; 24 WHO Africa region (AFR) countries (51%, 24/47), 21 WHO European region (EUR) (40%, 21/53), 6 WHO Eastern Mediterranean region (EMR) (29%, 6/21), 5 Pan-American region (AMR) (14%, 5/35), 5 Western Pacific Region (WPR) (19%, 5/27) and 4 WHO South East Asia Region (SEAR) (36%, 4/11). Only five countries included all recommendations. 63 included a minimum of one. 85% (n=55) included facility-based testing for pregnant women, 75% (n=49) facility-based testing for key populations, 74% (n=48) community-based testing for key populations, 69% (n=45) rapid testing, 57% (n=37) post-test counselling, 45% (n=29) lay provider testing, 38% (n=25) HIV self-testing, 29% (n=19) pre-test information and 25% (n=16) provider-assisted referral. The proportion in each region that included at least one recommendation were: 100% AFR (24/47), 100% EMR (6/6), 100% AMR (5/5), 100% WPR (5/5), 100% SEAR (4/4) and 95% EUR (20/21). AFR followed by EMR included the highest number of reccomendations.
Conclusion
There was substantial variability in the uptake of the WHO-differentiated HTS recommendations. Those in EMR included the most WHO-differentiated HTS recommendation followed by AFR. Countries within AMR included the least number of recommendations. Ongoing advocacy and efforts are needed to support the uptake of the WHO-differentiated HTS recommendations in country policies as well as their implementation.
Keywords: HIV & AIDS, health policy, public health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
A comprehensive review of available HIV national policies, regardless of language, was conducted.
The WHO repository does not contain HIV policies for all countries worldwide, and some regions were more comprehensively represented than others.
The review was limited to the 2015 WHO-differentiated HIV testing services (HTS) recommendations due to the timeline in which it was written.
The 2019 WHO-introduced recommendations for social network-based approaches were published following the review period and were therefore not included due to timelines.
HTS policy uptake is often not reflective of implementation.
Introduction
HIV testing services (HTS) are essential in identifying individuals who are unaware of their HIV status, linking HIV-positive individuals to treatment and HIV-negative individuals to prevention services. In 2021, 85% of people living with HIV were aware of their HIV status.1 At least eight countries globally reported having reached the 90-90-90 targets in 2020, and in 2021 the Joint United Nations Programme on HIV and AIDS announced new targets of 95-95-95 by 2025.2–4
Testing uptake remains particularly low among key populations. Key populations are defined as men who have sex with men (MSM), sex workers, people who inject drugs (PWID), people in prisons and closed settings and transgender people. They make up nearly two-thirds (65%) of all new infections.3 5 6 Men and young people also have low uptake and access to services.7–12 In all populations with low uptake, particularly key populations, identified barriers to testing include stigma and discrimination. Structural barriers including accessibility of services, inconvenient clinic hours and opportunity costs for clients have also been identified among all populations.7–12
In 2015, WHO published the first consolidated guidelines on HTS, followed by supplementary guidance recommending HIV self-testing (HIVST) and provider-assisted referral (also referred to as ‘assisted partner notification’) in 2016.6 In 2019, WHO published updated consolidated guidelines for HTS which include a new recommendation on social network-based approaches for HIV testing and updated guidance on HIVST and counselling message.13 14 WHO guidelines encourage a strategic mix of differentiated HTS approaches with a focus on priority populations and people with HIV who do not know their status and areas with greatest gaps.6 13 Differentiated HTS approaches refer to tailored and ‘client-centred’ approaches and they address barriers individuals have in accessing HTS.15 The guidelines include recommendations for HTS approaches and HTS components taking into account the population, epidemic and context. See online supplemental file 1 for a summary of the 2015 and 2016 WHO guidelines on HTS.
bmjopen-2021-058098supp001.pdf (93.5KB, pdf)
It is important to monitor the uptake of these recommendations into country policies in order to promote the inclusion of WHO recommendations into those countries and prioritise support, thereby improving the uptake of HTS and achieving the global 95-95-95 goals. Global monitoring of WHO guidelines uptake in national policies is routinely undertaken as part of Global AIDS Monitoring system.16 However, an in-depth understanding of adoption of WHO HTS guidelines at national level and in varying epidemic contexts is lacking. Understanding this will enable a better knowledge of where gaps in service may exist, and where further support may be provided to countries. To this end, we reviewed national HTS policies to examine the uptake of 2015 WHO-differentiated HTS recommendations on differentiated testing services.
Methods
Search strategy
A comprehensive search of national HTS policy documents was undertaken using the existing WHO national policy repository.17 The repository was first produced in 2015 and is routinely updated by WHO staff using a AIDSFree HTS policy database, country by country search of International Association of Physicians in AIDS Care (IAPAC)/HIV Policy Watch website and a broad Google search. The google search using the following keywords:
country name AND “HIV testing” AND policy;
country name AND “HIV testing” AND guideline;
country name AND PrEP AND policy;
country name AND PrEP AND guideline;
country name AND “pre-exposure prophylaxis” AND policy;
country name AND “pre-exposure prophylaxis” AND guideline The policy repository is maintained by WHO.
The repository includes national policies relating to HTS, HIV counselling services, prevention services, antiretroviral therapy (ART) as well as policies relating to prevention of mother-to-child transmission, HIV partner services, national HTS action/strategic plans and differentiated service delivery. In addition, national policies relating to sexual health and sexually transmitted infections were also included. All available national policies were used for data extraction.
For inclusion, national policies needed to include HTS and be published between January 2015, after the release of the 2015 WHO consolidated guidelines, and June 2019. The most recent available policy document containing information on HTS was used for extraction.
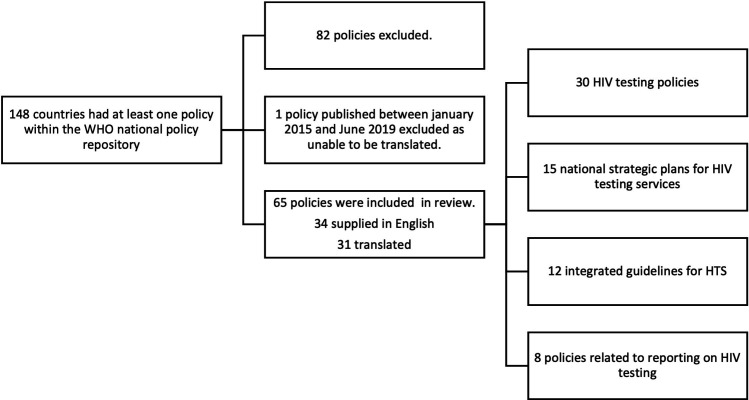
The national policies included were reviewed against WHO recommendations published in 2015/2016. Given the review end date of June 2019, the WHO 2019 guidelines were not included as they were published in December 2019. Policies in languages other than English were translated using Google translate. One country gave policy documents in formats that did not permit translation and was therefore excluded. Further details on the process to identify country policies including HTS recommendations is shown in figure 1.
Figure 1.
Process to identify country policies including recommendations on HIV testing services. 82 country policies were excluded as they were published before January 2015.
Data extraction
Data were extracted by one author (TK) into an Excel spreadsheet. The HTS approaches considered are: (1) facility-based testing for pregnant women (1a), adolescents (1b), infants and children (1c) and key populations (1c); (2) community-based testing, including community-based testing for specific populations; (3) HIV self-testing and (4) provider-assisted referral. Additional supportive HTS recommendatiosn considered were: (5) pre-test information, (6) post-test counselling, (7) lay provider testing and (8) rapid testing. In the 2015 guidelines, pre-test information was recommended instead of pre-test counselling, however data for pre-test counselling were extracted to better understand if countries were still recommending this component. The 2015 WHO consolidated guidelines and 2016 guidelines on HIV self-testing and partner notification were used.
Data analysis and reporting
We estimated the number and proportion of countries in each WHO region that had a relevant policy in the period of review (76%: 148/194). This was done overall (worldwide) and stratified by WHO region and epidemic type defined by generalised (≥5% HIV prevalence) and concentrated (<5%) HIV prevalence) epidemics (now often referred to as high or low burden settings). This last stratification was included because some recommendations were epidemic type specific: in particular, routine facility-based testing for those with signs and symptoms, adults, adolescents and children apply only to concentrated epidemics and community-based testing for adolescents apply to both generalised epidemics. The 2015 WHO consolidated guidelines define a concentrated epidemic as ‘HIV has spread rapidly in a defined subpopulation (such as MSM, sex workers, transgender people, people who use drugs or people in prison or other closed settings) but is not well established in the general population’.6 A generalised is defined as ‘HIV is firmly established in the general population. Although subpopulations at high risk may contribute disproportionately to the spread of HIV, sexual networking in the general population is sufficient to sustain the epidemic’.18
Policies were categorised in three groups:
Included: policies that clearly and explicitly stated and included a specific recommendation.
Not included: policies that did not include a specific recommendation.
Unclear: policies in which it was unclear whether a WHO recommendation was included due to insufficient information.
Analyses were conducted in Microsoft Excel.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
Characteristics of included policies
Of the 194 WHO member states, 148 countries had at least one policy within the WHO national policy repository. Of these, 65 country policies were eligible to be included; 30 were HIV testing policies, 15 national strategic plans, 12 integrated guidelines for HTS, 8 were related polices reporting on HIV testing (1 HIV counselling policies, 1 ART policy, 1 integrated guidelines for sexually transmitted infections, 1 sexual health national strategic plan, 1 policy on HIV contact management, 1 global AIDS progress report, 1 differentiated testing guideline and 1 policy on community-based testing). Overall, 34 (52%) country policies were in English. 82 country policies were excluded because they were published before January 2015. Morocco’s latest policy documents (written in French) were in formats that did not permit translation. No other policies were available for Morocco in the timeframe of interest; therefore, we could not include Morocco.
Of the 65 country policies reviewed, 24 were from AFR (51% of 47 counteries), 21 from the WHO European region (EUR; 40% of 53 countries), 6 from the WHO Eastern Mediterranean region (EMR; 29% of 21 countries), 5 from the Pan-American region (AMR; 14% of 35 countries), 5 from the Western Pacific Region (WPR; 19% of 27 countries) and 4 from the WHO South East Asia Region (SEAR; 36% of 11 countries). Just over two-thirds (37%, 24/65) policies were from countries classified as having a concentrated epidemic, 34% (22/65) from a generalised epidemic.
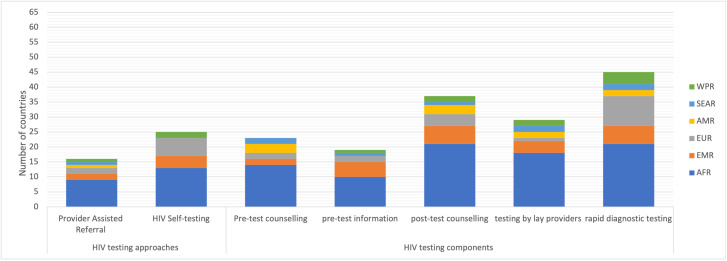
Overall uptake of the WHO-differentiated HTS recommendations in national policies
Only five country policies included all the relevant recommendations (figure 2). Among the recommendations on approaches, and components, applicable to all settings and populations (figure 3); 69% (45/65) included rapid testing, 45% (29/65) permitted lay provider testing, 38% (25/65) of countries supported HIVST, 35% (23/65) included pre-test counselling and did not specify the use of pre-test information, 35% included (37/65) post-test counselling, 29% (19/65) included pre-test information and 25% (16/65) supported provider-assisted referral.
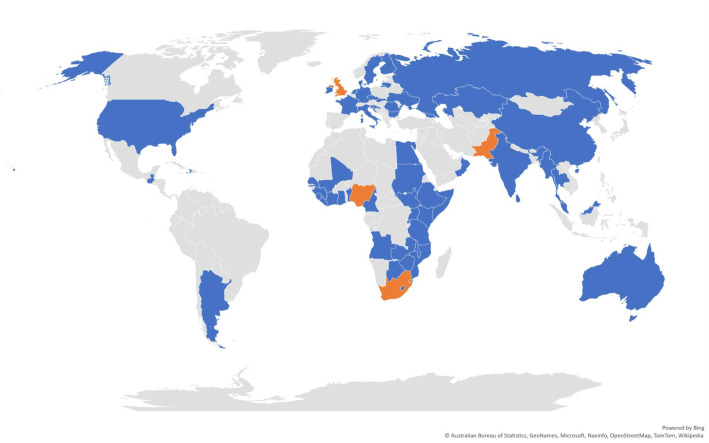
Figure 2.
Countries with a national policy identified between January 2015 and June 2019. A map of all 65 countries within this review (n=65). Countries highlighted in orange are those that included all recommendations relevant to their country setting (n=5).
Figure 3.
Number of countries that included recommendations valid in all settings and populations from the 2015 WHO consolidated guidelines for HTS, by type of recommendation and WHO region. AFR, WHO Africa region; AMR, Pan-American region; EMR, WHO Eastern Mediterranean region; EUR, WHO European region; SEAR, WHO South East Asia Region; WPR: Western Pacific Region.
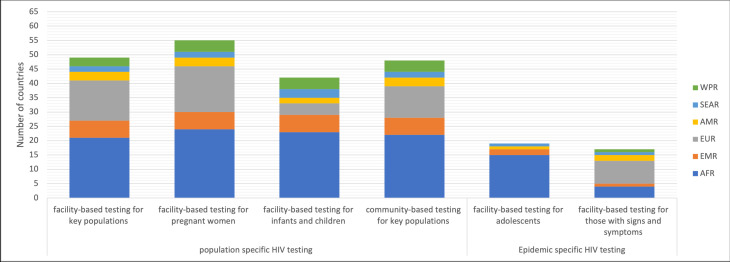
Regarding recommendation for specific subpopulations (figure 4 on the left), 85% (55/65) included recommendations for testing for pregnant women, 75% (49/65) recommended testing for key populations, 71% (17/24) recommended facility-based testing for all those presenting with signs and symptoms, 74% (48/65) recommended community-based testing for key populations and 65% (42/65) recommended facility-based testing for infants and children. Of countries with a concentrated epidemic (n=24), 71% (17/24) recommended facility-based testing for all those presenting with signs and symptoms. Of those with a generalised epidemic (n=22), 86% (19/22) recommended facility-based testing for adolescents.
Figure 4.
Number of countries included in the review that included population-specific or epidemic-specific recommendations from the 2015 WHO consolidated guidelines for HTS, by type of recommendation and WHO region. Facility-based testing for key popualtions here refers to provider-initiated testing and counselling; this is recommended in malnutrition clinics or sexually transmitted infections or hepatitis and tuberculosis services or health services for key populations in all settings. Facility-based testing for pregnant women, infants and children applies to all countries (n=65). Community-based testing for key populations applies to all countries (n=65). Facility-based testing for all those presenting with signs and symptoms is recommended only in countries with a concentrated epidemic (n=24); facility-based testing for adolescents only in countries with a generalised epidemics (n=22). AFR, WHO Africa region; AMR, Pan-American region; EMR, WHO Eastern Mediterranean region; EUR, WHO European region; SEAR, WHO South East Asia Region; WPR: Western Pacific Region.
Uptake of the WHO-recommended HTS approaches by WHO region
The uptake of recommendations varied across countries (see uptake of single recommendations for each country in online supplemental file 2) and regions. HIVST was recommended by 38% (25/65) of countries. The inclusion of HIVST ranged from EMR (67%; 4/6), AFR (54%; 13/24), WPR (40%; 2/5) and EUR (29%; 6/21). No included countries from SEAR and AMR supported HIVST at the time of review.
bmjopen-2021-058098supp002.pdf (86.8KB, pdf)
Only 25% (13/65) of countries included recommendations for provider-assisted referral: 38% of AFR (9/24) countries, 33% of EMR (2/6), 20% (1/5) of AMR, 10% (2/21) of EUR, 5% (1/4) of SEAR and in 5% (1/5) of WPR.
Pre-test information was included in 29% (19/65) of country policies. The inclusion of pre-test information ranged from EMR (83%; 5/6), followed by the AFR (42%; 10/24), WPR (20%; 1/5), SEAR (25%; 1/4) and EUR (10%; 2/21). No countries from AMR included this recommendation at the time of the review.
Overall, 57% (37/65) of country policies recommended post-test counselling, with variation across regions (100% EMR, 88% AFR, 40% WPR, 25% AMR, 25% SEAR and 19% EUR). While pre-test counselling is no longer recommended by WHO, it was still included by 35% (23/65) of countries: (60% AMR, 58% AFR, 50% SEAR, 33% EMR and 10% EUR) while no countries in the WPR included this recommendation.
Rapid testing was included in 69% (45/65) of country policies, with regional variation (100% EMR, 88% AFR, 80% WPR, 50% SEAR, 48% EUR and 40% AMR). Lay provider testing was permitted in 45% (29/65) of countries (75% AFR, 67% EMR, 50% SEAR, 40% WPR, 20% AMR and 5% EUR).
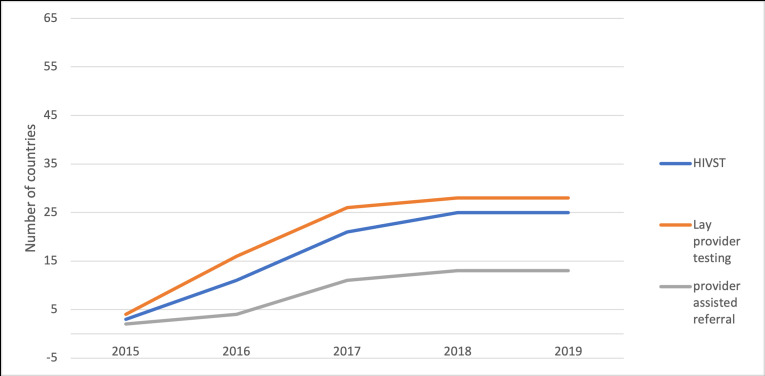
Lay provider testing was recommended for the first time by WHO in 2015 and provider-assisted referral and HIVST in 2016. Figure 5 shows the number of countries including the new recommendations in their policies in the years following their introduction. A steep increase in uptake can be observed with 16, 25 and 29 countries including recommendation on respectively provider-assisted referral, HIVST and lay provider testing by June 2019.
Figure 5.
Number of countries including the new recommendations, by year. HIVST, HIV self-testing.
Uptake of population-specific HTS approaches by WHO region
Facility-based testing for pregnant women was recommended by 85% (55/65) of countries, including all countries in EMR (100%; 6/6) and AFR (100%; 24/24) followed by WPR (80%; 4/5), EUR (76%; 16/21), AMR (60%; 3/5) and SEAR (50%; 2/4). Nearly two-thirds of countries (65%, 42/65) recommended facility-based testing for infants and children (100% EMR, 76% AFR, 80% WPR, 75% SEAR, 40% AMR and 19% EUR).
Facility-based testing for key populations is recommended in 49 countries (100% EMR, 88% AFR, 67% EUR, 60% AMR, 60% WPR and 50% SEAR). Of the countries that recommended facility-based testing for key populations, 69% (34/49) recommended targeted testing for MSM, 59% (29/49) for sex workers or those who engage in transactional sex, 57% (28/49) for PWID, 45% (22/49) for prisoners and 18% (9/49) for transgender people. Inclusion ranged with countries from the EMR starting from 100% (6/6) uptake, as well as AFR (88%; 21/24), the EUR (66%; 14/21) and WPR (60%; 3/5), while it was lower in the AMR (60%; 3/5) and the SEAR (50%; 2/4).
Nearly three-quarters (74%, 48/65) of countries recommended community-based testing for key populations. Uptake of community-based testing varied by region (100% EMR, 88% AFR, 80% WPR, 52% EUR, 50% SEAR and 20% AMR). Of the countries that included community-based testing for key populations; 44% (21/48) home-based/door-door testing, 38% (18/48) included outreach services, 35% (17/48) workplace testing, 35% (17/48) mobile testing, 23% (11/48) testing within educational establishments, 15% (7/48) testing in places of worship and 13% (6/48) recommended testing in community health centres.
Of the countries classified as having a concentrated epidemic, 37% (n=24) and 20% (5/24) were in the AFR, 46% (11/24) in EURO, 12% (3/24) in AMR, 8% (2/24) in SEAR, 8% (2/24) in WPR and 4% (1/24) in EMR. 72% (18/24) of these countries recommended facility-based testing for all those presenting with signs and symptoms of HIV. 34% (n=22) of countries were classified as having a generalised epidemic. Among the countries with a generalised epidemic, 100% (22/22) recommended routine facility-based testing for adolescents.
Discussion
As of 2019, 81% of all people with HIV are estimated to have been diagnosed globally.2 Differentiated testing approaches are critical for reaching the remaining people with HIV as standard testing services have not been successful in serving them. WHO recommends a strategic mix of HTS depending on the epidemiology, context and focus populations. The variations in uptake suggest that further research is required to understand why some countries did not include the WHO-differentiated HTS recommendations, and what support countries require to include recommendations. National policies often did not elaborate how various approaches will be used within a differentiated HTS plan to reach national goals and specific service delivery models and support tools. Moreover, inclusion of recommendations in policies does not always directly lead to implementation or scale up of effective practices. Further monitoring is needed to understand the implementation status of services as well as their scale and coverage.
Across all country policies reviewed, only five countries (in three AFR, one EMR and one EUR) included all the WHO-differentiated HTS recommendations (relevant to their country setting) with gaps in uptake remaining. 63 counteries included at least one recommendation. The uptake of recommendation in some country policies, although varied, does however suggests that it is feasible to adapt latest policies within a short timeframe. We found high uptake of recommendations for community-based testing, first recommended in 2013.19 Mobile testing, outreach testing, self-testing and provider-assisted referral were the approaches with the lowest uptake. As mentioned, the first two were more recently recommended so they might partly explain the lower uptake. For the latter two (mobile testing and outreach testing), the lower uptake might reflect the fact that they require more resources to introduce them and that they are more difficult to integrate. Population-specific facility-based testing recommendations were generally taken up for pregnant women and, infants and children and key populations. Among countries with generalised and concentrated epidemics, there was high uptake of community-based testing for key populations; while, only half of countries recommended mobile testing explicitly, and just over two-fifths recommended outreach testing.
These methods are likely to increase the uptake of HIV testing for key populations, by reducing barriers to access to HTS. For example, the 2016 WHO guidelines on HIVST and partner notification pointed out that these two approaches were perceived to reduce stigma among MSM and female sex workers.20 Stigma and discrimination have been found to be associated with never testing.21 22 In particular, studies have shown people might fear to be perceived as promiscuous, to be sexually rejected, socially distanced or even rejected by friends and family members if found to be living with HIV.23 24 Stigma has also been associated with feelings of worthlessness and shame.24 Women with greater perceived stigma have been shown to be less likely to test with gender inequality being associated with stigmatising attitudes, and in some studies healthcare workers identify stigma as a barrier to testing.25 26
Both HIVST and provider-assisted referral have been found to be acceptable and feasible to implement, and in reaching people who would not otherwise have tested for HIV.27 28 A steady increase in the number of countries adopting these recommendations within national policies has been observed. According to latest Global AIDS Monitoring, as of 2021 94 countries globally report inclusion of HIVST in national policies and 48 of them are routinely implementing HIVST.2
Since 2015, WHO has recommended a brief pre-test information when offering HTS instead of detailed pre-test counselling. Evidence and programmatic experiences suggest lengthy pre-test counselling is no longer needed and may in fact deter some testers from seeking HTS, such as repeat testers. Our review shows many countries may still be continuing to include traditional pre-test counselling within their national policies. Traditional pre-test counselling reduces the efficiency of HTS and does not represent the best use of scarce human and financial resources.6 Anecdotal evidence suggests many countries provide post-test counselling that includes outdated information. For example, many programmes had not adapted counselling messages to include information of prevention benefits of treatment and achieving viral suppression for partners (undetectable=untransmissible), availability of effective prevention options such as pre-exposure prophylaxis and messages on optimal testing frequency based on risk and epidemiology. Countries need to review and revise their policies to adopt latest WHO recommendation on pre-test information and post-test counselling.
Over two-thirds of countries included in this review support the use of rapid HIV testing, which can provide same day diagnosis, facilitating rapid initiation of ART. WHO recommends the use of trained lay providers and peers for delivering HTS using Rapid diagnostic tests (RDTs). However, of the countries that included RDT in their policies, few included the use of lay providers. Lay providers can affect expansion of services by enabling testing at places accessible and convenient to populations or groups most affected with HIV. This includes the introduction and scale up of community-based testing. Countries need to review their policies to address legal barriers to use of trained lay providers and develop standard operating procedures and training material and supervision activities for this cadre of providers.
Our review found variations in policy uptake by region. Overall, countries in EMR showed the highest uptake followed by AFR countries, while uptake in other regions remained comparatively low. For AFR, these findings are expected as well as encouraging as this region represents the highest burden of HIV infection.2 We also had a greater coverage of policies included (51% of all countries in the region) better representation of countries compared with other regions. WHO and other international agencies and donors make concerted efforts to support the HIV response in AFR which may be reflected in greater uptake of WHO recommendations. Typically, countries in this region also rely on WHO guidelines to inform national policies in contrast to some other regions such as AMR, EUR and WPR, which are more likely policy-based decisions on national guidance. These findings need to be interpreted with caution for regions other than AFR, partly due to low coverage of policies included (ranging 14%–40%), thus may not be representative of the country approaches. The epidemic context also varies in other regions, epidemics focused among key populations may face the presence of stigma and discrimination and varied implementation should also be considered. Further efforts focused on these regions and engagement with countries may be needed to improve uptake.
Overall, our review findings suggest that regular monitoring and better understanding of country uptake of WHO recommendations is needed to address country support needs to address such gaps. It is important to consider that inclusion of recommendations in national policies does not necessarily reflect that they are implemented and often there is a gap between policy uptake and implementation. Efforts are needed to enhance country policy uptake and minimise the lag in implementation. It is also important to note that while this review focuses on the inclusion of recommendation from the 2015 WHO consolidated guidelines, national HTS policies were already in existence before this date. All stakeholders including international organisations, implementing partners and donors need to support the governments and national programmes in updating national policies and translating these into implementation. Community groups and civil society need to advocate for availability of latest and evidence-based recommendations and interventions in their countries. Further support may be needed in operationalisation and scale up of such policies, and strategies focusing on key populations are required in some settings. Regular monitoring of country policy uptake and implementation status is needed to identify country support gaps for appropriate action.
This review has several limitations. National HTS policies were available only for 65 countries published between January 2015 and June 2019. There may be policies published in this period that we have not identified. For eight countries information was extracted from policy documents that were not directly related to HTS and may not have information with the required level of detail. For the EMR, SEAR and WPR, national policies were available from only a small number of countries and thus they may not be representative of the situaiton in the whole regions. In 2019, WHO published updated consolidated guidelines for HTS which include a new recommendation on social network-based approaches for HIV testing and updated guidance on HIVST and counselling messages,14 20 these were not included within this review due to timelines.
Conclusion
This review found that the uptake of all WHO’s 2015 and 2016 HTS recommendations varied substantially. Five countries included all the recommendations relevant to their country setting, and 63 included at least one. Uptake was particularly low for HIV self-testing, provider-assisted referral and lay provider testing, key interventions for reaching undiagnosed populations and for expanding access to HTS. Encouragingly, the inclusion of recommendations in the AFR and EMR was high compared with other regions. Differentiated HTS are essential for reaching people with HIV who do not know their status and others at high ongoing risk to facilitate linkage to prevention, treatment and care. Ongoing advocacy and efforts are needed to support the uptake of the WHO-differentiated testing recommendations in country policies as well as their implementation. The variations in the inclusion of the WHO-differentiated reccomendations suggest that further research is required to understand why some countries did not include the WHO-differentiated testing recommendations, and the support countries require to include recommendations.
Supplementary Material
Footnotes
Twitter: @ccasejohn
Contributors: TK took overall responsibility for the review of the policies. MS, CJ and MD were responsible for creating the WHO’s global policy repository and keeping it up to date. TK, CJ, VC, RB were involved in the development of the protocol and of the data extraction tool and in designing the analysis. TK screened the policies, extracted the data, conducted the analysis and produced the first draft of the manuscript. All authors reviewed the manuscript, provided inputs and approved the final version of the manuscript. CJ contributed to the writing, coordination and research for the WHO Consolidated Guidelines for HIV Testing Services.
Funding: This work was supported by the Bill & Melinda Gates Foundation, grant number INV-024432.
Disclaimer: The author is a staff member of the World Health Organization. The author alone is responsible for the views expressed in this publication and they do not necessarily represent the views, decisions or policies of the World Health Organization.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Extra data can be accessed via the Dryad data repository at http://datadryad.org/withthedoi:10.5061/dryad.fj6q57406.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. UNAIDS . Fact sheet 2022. UNAIDS, 2022. [Google Scholar]
- 2. UNAIDS . 2021 global AIDS update: confronting inequalities. 2021. Available: https://www.unaids.org/sites/default/files/media_asset/2021-global-aids-update_en.pdf
- 3. UNAIDS . Aids targets: putting people living with HIV and communities at risk at the centre 2021. 2025. Available: https://aidstargets2025.unaids.org/ [Accessed 23 Feb 2022].
- 4. UNAIDS . Fast-track strategy to end the AIDS epidemic by 2030. UNAIDS, 2014. [Google Scholar]
- 5. WHO . Progress report on HIV, viral hepatitis and sexually transmitted infections, 2019 accountability for the global health sector strategies, 2016–2021. Geneva, Switzerland: WHO, 2019. [Google Scholar]
- 6. WHO . Consolidated guidelines on HIV testing services. Geneva: WHO, 2015: 1–188. [Google Scholar]
- 7. Qiao S, Zhang Y, Li X, et al. Facilitators and barriers for HIV-testing in Zambia: a systematic review of multi-level factors. PLoS ONE 2018;13:e0192327. 10.1371/journal.pone.0192327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thi Thanh Huong N, Thi Hau N, Van Chau N, et al. Perceived barriers and Facilitators to uptake of HIV testing services among people who inject drugs in Vietnam. J Subst Use 2018;23:551–6. 10.1080/14659891.2018.1448473 [DOI] [Google Scholar]
- 9. Surratt HL, O’Grady CL, Kurtz SP, et al. HIV testing and engagement in care among highly vulnerable female sex workers: implications for treatment as prevention models. J Health Care Poor Underserved 2014;25:1360–78. 10.1353/hpu.2014.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Staveteig S, Wang S, Head SK, et al. Demographic patterns of HIV testing uptake in Sub-Saharan Africa. DHS Comparative Reports. Calverton, Maryland, USA: ICF International, 2013. [Google Scholar]
- 11. Traversy GP, Austin T, Ha S, et al. An overview of recent evidence on barriers and facilitators to HIV testing. Can Commun Dis Rep 2015;41:302–21. 10.14745/ccdr.v41i12a02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Loos J, Manirankunda L, Hendrickx K, et al. HIV testing in primary care: feasibility and acceptability of provider initiated HIV testing and counseling for sub-Saharan African migrants. AIDS Educ Prev 2014;26:81–93. 10.1521/aeap.2014.26.1.81 [DOI] [PubMed] [Google Scholar]
- 13. WHO . Consolidated guidelines on HIV testing services for a changing epidemic. Geneva, Switzerland: WHO, 2019: 1–12. [Google Scholar]
- 14. WHO . WHO recommends social-network based HIV testing approaches for key populations as part of partner services package. Geneva, Switzerland: WHO, 2019. [Google Scholar]
- 15. IAS . Differentiated service delivery for HIV: a decision framework for HIV testing services. It’s time to test differently. Geneva, Switzerland: International Aids Society, 2018: 1–68. [Google Scholar]
- 16. UNAIDS . Global AIDS Monitoring 2020: indicators for monitoring the 2016 political declaration on ending AIDS. Global AIDS Monitoring. Geneva, Switzerland: UNAIDS, 2020. [Google Scholar]
- 17. WHO . WHO national policy repository. 2015 ed. Dropbox: WHO, 2020. [Google Scholar]
- 18. Buse K, Hawkes S. Health post-2015: evidence and power. Lancet 2014;383:678–9. 10.1016/S0140-6736(13)61945-5 [DOI] [PubMed] [Google Scholar]
- 19. WHO . Consolidated ARV guidelines. Geneva, Switzerland: WHO, 2013. [Google Scholar]
- 20. WHO . Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services. Geneva, Switzerland: WHO, 2016. [PubMed] [Google Scholar]
- 21. Pitpitan EV, Kalichman SC, Eaton LA, et al. AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape town, South Africa. Ann Behav Med 2012;43:362–71. 10.1007/s12160-012-9346-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Conway DP, Holt M, Couldwell DL, et al. Barriers to HIV testing and characteristics associated with never testing among gay and Bisexual men attending sexual health clinics in Sydney. J Int AIDS Soc 2015;18:20221. doi:20221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Iott BE, Loveluck J, Benton A, et al. The impact of stigma on HIV testing decisions for gay, bisexual, queer and other men who have sex with men: a qualitative study. BMC Public Health 2022;22:471. 10.1186/s12889-022-12761-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Akatukwasa C, Getahun M, El Ayadi AM, et al. Dimensions of HIV-related stigma in rural communities in Kenya and Uganda at the start of a large HIV ‘test and treat’ trial. PLoS ONE 2021;16:e0249462. 10.1371/journal.pone.0249462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sullivan MC, Rosen AO, Allen A, et al. Falling short of the first 90: HIV stigma and HIV testing research in the 90–90–90 era. AIDS Behav 2020;24:357–62. 10.1007/s10461-019-02771-7 [DOI] [PubMed] [Google Scholar]
- 26. Thapa S, Hannes K, Cargo M, et al. Stigma reduction in relation to HIV test uptake in Low- and middle-income countries: a realist review. BMC Public Health 2018;18:1277. 10.1186/s12889-018-6156-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang C, Li X, Brecht M-L, et al. Can self-testing increase HIV testing among men who have sex with men: a systematic review and meta-analysis. PLoS ONE 2017;12:e0188890. 10.1371/journal.pone.0188890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Qin Y, Han L, Babbitt A, et al. Experiences using and organizing HIV self-testing. AIDS 2018;32:371–81. 10.1097/QAD.0000000000001705 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058098supp001.pdf (93.5KB, pdf)
bmjopen-2021-058098supp002.pdf (86.8KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Extra data can be accessed via the Dryad data repository at http://datadryad.org/withthedoi:10.5061/dryad.fj6q57406.