Abstract
Background
Autistic adults experience more frequent suicidal thoughts and mental health difficulties than non‐autistic adults, but research has yet to explain how these experiences are connected. This study explored how anxiety and depression contribute to suicidal thoughts according to the Interpersonal Theory of Suicide for autistic and non‐autistic adults.
Methods
Participants (autistic adults n = 463, 61% female; non‐autistic n = 342, 64% female) completed online measures of anxiety, depression, thwarted belonging, and perceived burdensomeness. Network analysis explored whether: (i) being autistic is a risk marker for suicide; and (ii) pathways to suicidal thoughts are consistent for autistic and non‐autistic adults.
Results
Being autistic connected closely with feeling like an outsider, anxiety, and movement, which connected to suicidal thoughts through somatic experiences, low mood, and burdensomeness. Networks were largely consistent for autistic and non‐autistic people, but connections from mood symptoms to somatic and thwarted belonging experiences were absent for autistic adults.
Conclusion
Autistic people experience more life stressors than non‐autistic people leading to reduced coping, low mood, and suicidal thoughts. Promoting belonging, reducing anxiety, and understanding the role of movement could inform suicide prevention for autistic people. Research should accurately capture autistic lived experience when modeling suicide to ensure suicide prevention meets autistic needs.
Keywords: autism, interpersonal theory of suicide, network analysis
INTRODUCTION
Suicide accounts for the deaths of over 700,000 people each year (World Health Organization, 2021) and autistic people 1 —recently estimated to number at least 80 million worldwide (Lord et al., 2022)—are now recognized as over‐represented in those figures (Cassidy et al., 2022; Hirvikoski et al., 2016; Kirby et al., 2019; Kõlves et al., 2021). Autism is diagnosed by the observable presence of social communication, sensory differences, and restricted interests (American Psychiatric Association, 2013) and a recent UK study reported evidence of autism or possible autism in around 41% of those who died by suicide (Cassidy et al., 2022). Thus, there is an urgent need to understand and provide evidence‐based interventions for autistic people to meet global suicide prevention targets (Cassidy, Cogger‐Ward, et al., 2021; Cassidy, Robertson, et al., 2020). One limiting factor in guiding interventions is the absence of suicide theory and models that accurately describe the experiences of autistic people (Cassidy, Cogger‐Ward, et al., 2021). Our earlier research reported the Interpersonal Theory of Suicide (ITS) may be relevant for autistic adults (Pelton & Cassidy, 2017), but the model explains only one‐third of the variance in lifetime suicidal thoughts and behaviors for autistic adults compared with non‐autistic adults (Pelton et al., 2020b). One possibility is that mental health difficulties, such as anxiety and depression, could have a greater influence on suicidal thoughts and behaviors for autistic than non‐autistic adults. Mental health difficulties, such as anxiety and depression are reported by up to 80% of autistic adults (Lever & Geurts, 2016) and have been significantly associated with suicidal thoughts, behaviors, and death by suicide for autistic young people and adults (Jokiranta‐Olkoniemi et al., 2021; Kõlves et al., 2021; Zahid & Upthegrove, 2017), but we do not yet know how these experiences are connected. Reducing persistent distress caused by suicidal thoughts has been identified as a clinical priority for autistic adults (South et al., 2020) that could reduce future death by suicide (Large et al., 2021). Thus, in this study, we set out to explore the role of anxiety and depression in the development of suicidal desire according to the ITS and whether this differs for autistic and non‐autistic adults.
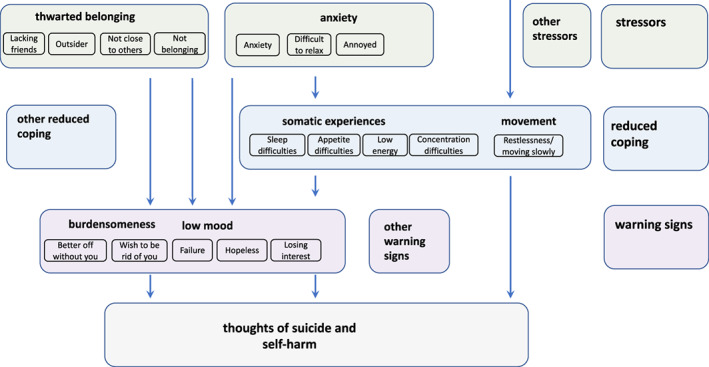
According to the ITS, in any population group, suicidal desire develops from the interaction of perceived burdensomeness (social worthlessness) with thwarted belonging (hopeless social isolation) (Joiner, 2005; Van Orden et al., 2010). As shown in Figure 1, mental health symptoms hypothetically contribute to suicidal desire because they increase the experience of these proximal risk markers (Davidson et al., 2011; Kleiman et al., 2014; Silva et al., 2015). Testing these pathways for autistic adults, however, requires a transdiagnostic approach to modeling mental health (Lombardo et al., 2019; Weiss, 2014). Higher rates of misdiagnosed and co‐occurring mental health difficulties (Camm‐Crosbie et al., 2019) are attributed to differences between autistic and non‐autistic people in the way that mental health—such as depression (Cassidy, Bradley, Bowen, et al., 2018; Cassidy, Bradley, Cogger‐Ward, et al., 2021), anxiety (Boulter et al., 2014; Rodgers et al., 2020; Rodgers & Ofield, 2018), thwarted belonging, and perceived burdensomeness (Pelton et al., 2020a)—are conceptualized and measured so comparisons based on scale total scores may not be accurate. One alternative is the network approach, which conceptualizes mental health difficulties as the interaction of their individual symptoms in contrast with the common cause or medical model (Borsboom, 2017; Borsboom & Cramer, 2013; Borsboom et al., 2021). Individual symptoms or experiences, such as hopelessness, feeling nervous, or like an outsider are nodes within the network while edges describe the strength of association between two nodes (Borsboom, 2017). Network analysis is particularly recommended for estimating and visualizing the complexity of suicidal thoughts (De Beurs, 2017) and specifically for (i) generating novel, putative theoretical pathways (Haslbeck et al., 2022) and (ii) understanding differences between patient groups (De Beurs, 2017). Thus, these are the aims of the current study.
FIGURE 1.
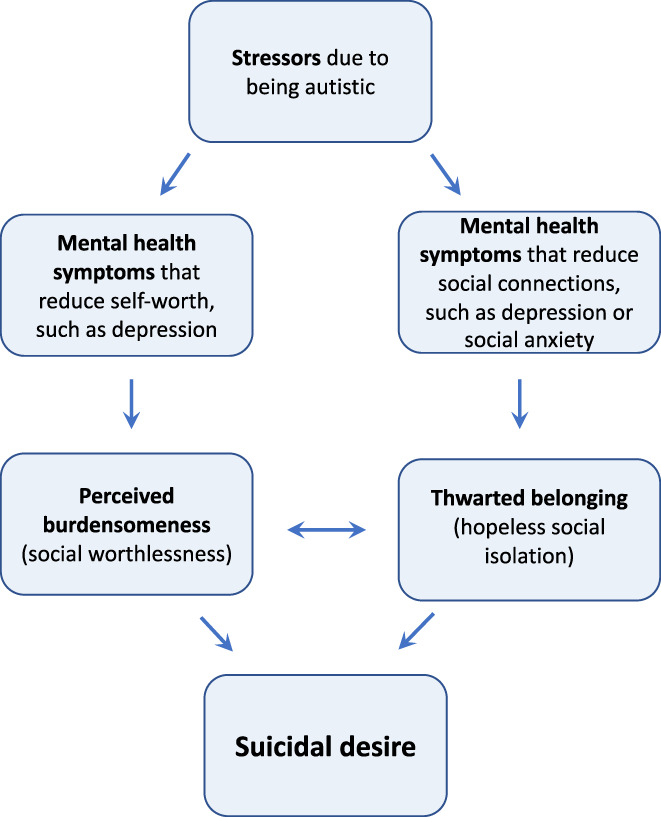
Hypothesized association between mental health difficulties, interpersonal theory of suicide proximal risk markers and suicidal thoughts showing possible influence of minority stress for autistic people.
One possibility is that being autistic represents a distal risk marker for suicide due to minority stress (Botha & Frost, 2020). As shown in Figure 1, being autistic could lead to multiple life stressors, making it more likely that an individual experiences anxiety and depression (Lever & Geurts, 2016), thwarted belonging, burdensomeness (Pelton et al., 2020b) and suicidal thoughts (Cassidy et al., 2014) than a non‐autistic person. Empirical research supports this: autistic traits are a unique risk marker for suicidal thoughts and behaviors in autistic and non‐autistic samples (Cassidy et al., 2022; Cassidy, Bradley, Shaw, et al., 2018; Pelton & Cassidy, 2017; Richards et al., 2019; Takara & Kondo, 2014; Upthegrove et al., 2018). Simple pathways have been described from (i) autistic traits through perceived burdensomeness and thwarted belonging (Pelton et al., 2020b); (ii) loneliness through depression (Hedley, Uljarević, Foley, et al., 2018); and (iii) social dissatisfaction and loneliness through perceived burdensomeness (Dow et al., 2021); to suicidal thoughts and behaviors for autistic adults. However, these modeling studies have included only simply linear relationships and have employed scale totals using measures designed for non‐autistic adults. Furthermore, network analysis has already extended our understanding of the interaction of these variables for non‐autistic people: perceived burdensomeness and low mood symptoms (such as feeling depressed or hopeless) are reported closely, directly connected to suicidal thoughts while thwarted belonging and anxiety are more distal or less strongly connected (Beard et al., 2016; De Beurs et al., 2019; Fried et al., 2016; Ordóñez‐Carrasco et al., 2021; Schönfelder et al., 2021; Suh et al., 2021), but studies, to date, have not included autistic samples. Thus, this study will use network analysis to visualize and estimate more complex interactions than traditional statistical analytic techniques to understand the role of, for example, restlessness or appetite preferences, without needing to attribute these to anxiety, depression, or autistic characteristics.
Finally, researchers propose that being autistic may moderate connections between risk markers (Lai et al., 2017; Pelton & Cassidy, 2017) and network analysis provides a range of tools to simultaneously test a range of propositions: first, autistic thinking styles, such as perseverative thinking (Arwert & Sizoo, 2020; Lai et al., 2017; South et al., 2020), may make it harder to switch away from negative thoughts and relatively hasten the development of suicidal thoughts compared with non‐autistic people. This is in line with the network approach which argues that connections between risk markers are stronger in vulnerable compared with less vulnerable groups (van Borkulo et al., 2015). Second, differences in emotional experience, such as alexithymia (difficulty identifying and expressing emotional states (Bird & Cook, 2013)) could mean that emotional symptoms are understated, attenuating connections between emotional risk markers, such as low mood or anxiety, with other risk markers (Costa et al., 2020; Pelton & Cassidy, 2017; Pelton et al., 2020b). Third, overlapping autistic characteristics and somatic depression symptoms (such as appetite or sleep differences) (Gotham et al., 2015) could suggest that somatic experiences are more influential in maintaining the symptom network for autistic compared with non‐autistic adults (Montazeri et al., 2020). However, to date, none of these propositions have been tested in a matched sample of autistic and non‐autistic adults. Thus, the current study will undertake exploratory analyses to explore whether and how connections between risk markers differ between autistic and non‐autistic adults.
Thus, the current study will undertake an item‐level network analysis to explore (i) whether and how being autistic represents a distal risk marker for suicide and (ii) whether and how risk markers interact differently for autistic compared with non‐autistic adults. We regard these analyses as exploratory due to an absence of previous research and are open to data‐driven results. Based on previous empirical research we expect to find autistic adults report more frequent experiences of anxiety, depression, thwarted belonging, perceived burdensomeness, and suicidal thoughts. In line with the network approach, there will be multiple interactions within and between items measuring distinct constructs.
MATERIALS AND METHODS
Participants and procedure
Data in this study are described elsewhere (Pelton et al., 2020a, 2020b). Participants were 805 complete records retained from an online survey of general population autistic (n = 463 [58% sample], 61% female) and non‐autistic (n = 342 [42%], 64% female) adults (Table 1). We recruited autistic adults via Cambridge Autism Research Database, West Midlands and UK autism organizations, including Autistica (UK‐based autism research charity), and non‐autistic adults via Cambridge Psychology Database, Coventry University psychology research participation scheme, suicide‐focussed websites, and social media.
TABLE 1.
Demographic information.
| Non‐autistic (n = 342) | Autistic (n = 463) | p | |
|---|---|---|---|
| Age (mean (SD)) | 41.31 (15.7) | 41.55 (13.9) | 0.82 |
| AQ‐S total (mean (SD)) | 60.92 (12.7) | 89.44 (12.0) | <0.01 |
| Gender (%) | |||
| Male | 118 (34.7) | 150 (32.5) | 0.01 |
| Female | 219 (64.4) | 282 (61.0) | |
| Not male or female | 2 (0.6) | 28 (6.1) | |
| Prefer not to say | 1 (0.3) | 2 (0.4) | |
| PHQ‐9 total (mean (SD)) | 7.64 (6.77) | 13.81 (7.43) | <0.01 |
| GAD‐7 total (mean (SD)) | 6.56 (5.39) | 12.02 (6.08) | <0.01 |
| INQ‐10 thwarted belonging (mean (SD)) | 16.55 (8.02) | 25.57 (6.77) | <0.01 |
| INQ‐10 burdensomeness (mean (SD)) | 8.70 (6.04) | 14.30 (7.92) | <0.01 |
| In full‐time employment (n (%)) | 144 (42.1) | 143 (30.9) | 0.01 |
| Highest academic qualification (n (%)) | |||
| GCSE/O‐Level/NVQ level 1 or 2 | 17 (5.0) | 45 (9.7) | <0.01 |
| A‐Level/Higher/NVQ level 3/BTEC/GNVQ | 43 (12.6) | 59 (12.8) | |
| Higher national diploma | 11 (3.2) | 26 (5.6) | |
| Undergraduate degree | 83 (24.4) | 137 (29.7) | |
| Postgraduate degree | 153 (45.0) | 156 (33.8) | |
| No school certificate or any qualifications | 5 (1.5) | 8 (1.7) | |
| Other | 28 (8.2) | 31 (6.7) | |
| Additional neurodevelopmental condition (n (%)) | |||
| Yes | 28 (8.2) | 127 (27.5) | <0.01 |
| No | 312 (91.5) | 332 (71.9) | |
| Prefer not to say | 1 (0.3) | 3 (0.6) | |
| Dyspraxia (%) | 2 (0.6) | 40 (8.6) | <0.01 |
| Learning disability (%) | 2 (0.6) | 13 (2.8) | 0.04 |
| Learning difficulty (%) | 2 (0.6) | 14 (3.0) | 0.03 |
| Dyscalculia (%) | 2 (0.6) | 14 (3.0) | 0.03 |
| Dyslexia (%) | 9 (2.6) | 45 (9.7) | <0.01 |
| Attention‐deficit hyperactivity (%) | 14 (4.1) | 64 (13.8) | <0.01 |
| Developmental delay (%) | 0 (0.0) | 8 (1.7) | 0.04 |
| Other (%) | 2 (0.6) | 19 (4.1) | <0.01 |
| Current mental health diagnosis (n, (%)) | |||
| Yes | 102 (30.0) | 298 (64.6) | <0.01 |
| No | 235 (69.1) | 162 (35.1) | |
| Prefer not to say | 3 (0.9) | 1 (0.2) | |
| Depression (%) | 76 (22.2) | 238 (51.4) | <0.01 |
| Anxiety (%) | 73 (21.3) | 248 (53.6) | <0.01 |
| OCD (%) | 7 (2.0) | 46 (9.9) | <0.01 |
| Bipolar (%) | 4 (1.2) | 30 (6.5) | <0.01 |
| Personality disorder (%) | 5 (1.5) | 46 (9.9) | <0.01 |
| Schizophrenia (%) | 2 (0.6) | 7 (1.5) | 0.37 |
| Anorexia (%) | 3 (0.9) | 33 (7.1) | <0.01 |
| Bulimia (%) | 1 (0.3) | 12 (2.6) | 0.02 |
| Epilepsy (%) | 9 (2.6) | 13 (2.8) | 1.0 |
| Chronic fatigue (%) | 11 (3.2) | 31 (6.7) | 0.04 |
| Tourette's (%) | 0 (0.0) | 8 (1.7) | 0.04 |
| Other (%) | 10 (2.9) | 59 (12.7) | <0.01 |
| Lifetime reported suicidal thoughts and behaviors (n (%)) | |||
| No past suicidal thoughts/ behaviors | 106 (31.7) | 24 (5.4) | <0.01 |
| Past suicidal ideation | 120 (35.9) | 79 (17.7) | |
| Past suicide plan | 73 (21.9) | 187 (41.8) | |
| Past suicide attempt | 35 (10.5) | 157 (35.1) | |
Participants gave informed consent via Qualtrics, were informed about question content in each section, prompted to take breaks, and given information about support services. Autistic adults (one male and one female) reviewed study materials, clarified instructions, advised on questionnaire selection, interpreted results, and developed the model. Coventry University Faculty of Health and Life Sciences Ethics Committee (ethics approval P61841, approved on 12.12.2018) and the Autism Research Centre, University of Cambridge approved the study.
Measures
Demographics: Participants' self‐reported age, gender, employment status, mental health difficulties, additional neurodevelopmental conditions, and autism diagnosis.
Thwarted belongingness and perceived burdensomeness were measured using The Interpersonal Needs Questionnaire 10 (INQ‐10), a 10‐item scale containing thwarted belonging and perceived burdensomeness subscales (Van Orden et al., 2012). We chose the INQ‐10 over the INQ‐15 to avoid frustration from similarly worded questions raised by our design group and given equivalent validity (Hill et al., 2015; Thwarted belonging α = 0.93, perceived burdensomeness α = 0.91 in this sample).
Depression was measured using 9‐item Patient Health Questionnaire (PHQ‐9) (Kroenke et al., 2001) which asks how frequently depression symptoms are experienced over the past 2 weeks with a four‐item ordinal scale: “not at all” (0), “several days” (1), “more than half the days” (2), and “nearly every day” (3). Item 9 measures thoughts of suicide and self‐harm and has been used here to measure current suicidal thoughts as in previous studies (de la Torre et al., 2021; Penfold et al., 2021; Quinlivan et al., 2017) (α = 0.92 in this sample).
Anxiety was measured using 7‐item Generalized Anxiety Disorder (GAD‐7) (Spitzer et al., 2006), which measures cognitive and emotional symptoms of anxiety on the same four‐item ordinal scale as the PHQ‐9. PHQ9 and GAD7 have been designed for non‐autistic population but used in research amongst autistic adults (Griffiths et al., 2019; Vasa & Mazurek, 2015; α = 0.92 in this sample).
Autistic characteristics were measured using the Autism Quotient Short Form (AQ‐S). The AQ‐S is a 28‐item subset of the AQ‐50 with a four‐item response scale from 1 “definitely agree” to 4 “definitely disagree” (Hoekstra et al., 2011). The AQ‐S demonstrates the same latent factors in autistic and non‐autistic adults (Murray et al., 2014; α = 0.88 non‐autistic, 0.87 autistic in this sample).
Self‐reported autism diagnosis shows up to 99.6% concordance with clinical diagnosis in validation studies (Allison et al., 2012; Daniels et al., 2012; Fombonne et al., 2022). Self‐reported diagnosis allows for larger samples for statistical modeling and online participation, which can increase disclosure of sensitive information, as in previous studies (Cassidy, Bradley, et al., 2020; Cassidy, Bradley, Shaw, et al., 2018). In this sample, total scores on the AQ‐S are above/below suggested cut‐off of 65 indicative of autism for autistic (mean = 89.44) and non‐autistic people (mean = 60.92) respectively (shown in Table 1; Hoekstra et al., 2011). We also included self‐diagnosed and possibly (awaiting diagnosis) autistic people because many autistic adults remain undiagnosed due to the historic development of diagnostic criteria (Lai & Baron‐Cohen, 2015; Russell et al., 2022). Bias in diagnostic tests and difficulties accessing services mean autism is less likely to be diagnosed in women and ethnic minority groups and, thus, these may represent high‐risk groups (Constantino et al., 2020; McCrossin, 2022; Roman‐Urrestarazu et al., 2021; Russell et al., 2022; Tromans et al., 2020).
Lifetime suicidal thoughts and behaviors are measured using item 1 of the Suicidal Behaviors Questionnaire revised (Osman et al., 2001), which demonstrates equivalent measurement properties in autistic and non‐autistic adults (Cassidy, Bradley, et al., 2020) and as in previous studies (Pelton & Cassidy, 2017). Total scores on the SBQ‐R are recommended not to be compared between autistic and non‐autistic people due to non‐invariance of items 3 and 4 (Cassidy, Bradley, et al., 2020).
Analytic approach
Network models or Gaussian graphical models
Gaussian graphical models (GGMs) are novel network estimation techniques for ordinal and continuous variables in between‐subject data. Edges connecting nodes represent partial correlations: the connection strength between two nodes while controlling for all others in the network. See Borsboom et al. (2021) for primer on the network approach. Analyses were conducted in R (v 4.0.5; R Core Team, 2021).
Summary of the analyses
We explored data distribution and how the data split according to autism diagnosis (autistic, non‐autistic, and possibly autistic) and gender (female, male, not male or female) using the networktree package (Jones et al., 2020). Next, to avoid problems of multi‐collinearity between nodes we combined theoretical knowledge with the goldbricker function from the network tools package (Jones, 2020) to identify potential overlapping constructs and combine node scores using principal component analysis, similar to (Barthel et al., 2020; Lass et al., 2020). We estimated two networks using individual items of the INQ‐10, PHQ‐9, GAD‐7: first, in the whole sample network, we used all variables plus the categorical variable autism to estimate a network using mgm package (Haslbeck & Waldorp, 2020)to explore whether and how being autistic is connected to suicidal thoughts through network items. Second, we split the data and used the EstimateGroupNetwork package (Costantini et al., 2019) to estimate networks for autistic and non‐autistic people. We used the NetworkComparisonTest (van Borkulo et al., 2017) to test for differences between autistic and non‐autistic networks in (i) overall inter‐connectivity (“global density”: total sum of edges in each network); (ii) individual edge weights; and (iii) or relative inter‐connectedness of nodes (termed centrality estimates). We use expected influence (total sum of edge weights on a given node taking into account negative edge weights) as other centrality estimates are less reliable (Robinaugh et al., 2016). See Appendix S1 for technical details and r script.
RESULTS
Descriptive statistics
Table 2 shows mean individual item scores for autistic and non‐autistic people. Ninety‐five percent of autistic people (68% non‐autistic) reported past suicidal thoughts and behaviors, including 35% of autistic people (10% non‐autistic) who had previously attempted suicide. The mean total score of the 8 items on the PHQ‐9 was 12 for autistic people, which is above cutoff for possible clinical depression. The mean score on item 9 of the PHQ‐9 was 1 indicating that on average the autistic people in this sample had experienced suicidal thoughts for several days for the preceding 2 weeks. The mean score on each scale item was significantly higher for autistic than non‐autistic people.
TABLE 2.
Individual items included in the analyses.
| Not autistic (n = 342) (mean (SD)) | Autistic (n = 463) (mean (SD)) | p | Results of goldbricker/nodename | |
|---|---|---|---|---|
| GAD‐7 | ||||
| 1. Feeling nervous, anxious, or on edge | 1.18 (0.96) | 1.96 (1.04) | <0.01 | Anxiety |
| 2. Not being able to stop or control worrying | 0.95 (0.98) | 1.74 (1.09) | <0.01 | Anxiety |
| 3. Worrying too much about different things | 1.01 (0.99) | 1.82 (1.07) | <0.01 | Anxiety |
| 4. Trouble relaxing | 1.17 (1.04) | 1.98 (1.07) | <0.01 | Relax |
| 5. Being so restless that it is hard to sit still | 0.57 (0.85) | 1.36 (1.14) | <0.01 | Movement |
| 6. Being easily annoyed or irritable | 1.00 (0.90) | 1.66 (1.05) | <0.01 | Annoy |
| 7. Feeling afraid as if something awful might happen | 0.67 (0.90) | 1.49 (1.15) | <0.01 | Anxiety |
| PHQ‐9 | ||||
| 1. Little interest or pleasure in doing things | 0.79 (0.97) | 1.45 (1.05) | <0.01 | Interest |
| 2. Feeling down, depressed, or hopeless | 0.86 (0.98) | 1.56 (1.10) | <0.01 | Depressed |
| 3. Trouble falling or staying asleep or sleeping too much. | 1.30 (1.12) | 1.89 (1.13) | <0.01 | Sleep |
| 4. Feeling tired or having little energy | 1.34 (1.05) | 1.97 (1.03) | <0.01 | Tired |
| 5. Poor appetite or overeating | 0.99 (1.12) | 1.69 (1.18) | <0.01 | Appetite |
| 6. Feeling bad about yourself—or that you are a failure or have let yourself or your family down | 0.96 (1.09) | 1.76 (1.14) | <0.01 | Failure |
| 7. Trouble concentrating on things, such as reading the newspaper or watching television | 0.82 (0.98) | 1.64 (1.18) | <0.01 | Concentrate |
| 8. Moving or speaking so slowly that other people could have noticed? Or the opposite—being so fidgety or restless that you have been moving around a lot more than usual? | 0.25 (0.65) | 0.87 (1.05) | <0.01 | Movement |
| 9. Thoughts that you would be better off dead, or hurting yourself in some way | 0.33 (0.76) | 0.97 (1.09) | <0.01 | Dead |
| INQ‐10—Perceived burdensomeness | ||||
| 1. The people in my life would be better off if I were gone. | 1.73 (1.34) | 2.87 (1.83) | <0.01 | Better |
| 2. The people in my life would be happier without me. | 1.72 (1.33) | 2.78 (1.78) | <0.01 | Better |
| 3. I think my death would be a relief to the people in my life. | 1.48 (1.18) | 2.45 (1.79) | <0.01 | Rid |
| 4. I think the people in my life wish they could be rid of me. | 1.61 (1.28) | 2.50 (1.65) | <0.01 | Rid |
| 5. I think I make things worse for the people in my life. | 2.18 (1.67) | 3.7 (2.03) | <0.01 | Better |
| INQ‐10 Thwarted belonging | ||||
| 6. I feel like I belong. | 3.33 (1.95) | 5.15 (1.69) | <0.01 | Belong |
| 7. I am fortunate to have many caring and supportive friends. | 2.95 (1.92) | 4.53 (1.94) | <0.01 | Friends |
| 8. I feel disconnected from other people. | 3.39 (1.88) | 5.14 (1.69) | <0.01 | Belong |
| 9. I feel like an outsider at social gatherings. | 3.65 (1.89) | 5.86 (1.47) | <0.01 | Outsider |
| 10. I am close to other people. | 3.23 (1.86) | 4.90 (1.69) | <0.01 | Close |
Data splitting
As shown in Figure S1a, the data split primarily on autism diagnosis: the data differed significantly between those formally diagnosed, self‐diagnosed, and awaiting autism diagnosis (autistic) compared with those who had never considered they might be autistic (non‐autistic). The non‐autistic data then split significantly according to gender (male vs. non‐male), but there was no gender split in the autistic data. Thus, we proceeded with the analysis of autistic compared with non‐autistic people with combined gender groups.
Item selection
As shown in Table 2, we combined items as follows: the belief that life would improve for others in the event of your death (“better”), combined items 1, 2, and 5, INQ‐10. Believing others aspire for your death (“rid”) combined items 3 and 4, INQ‐10. Not belonging (“belong”) combined items 6 and 8, INQ‐10. Movement differences (“movement”) combined item 8 PHQ‐9 (restlessness and shutdown) and item 5, GAD‐7 (restlessness); (v) anxiety, including uncontrollable worry, feeling nervous and believing something terrible will happen, (“anxiety”) combined items 1, 2, 3 and 7, GAD‐7. Items representing sleep (PHQ‐9 item 3) and appetite difficulties (PHQ‐9 item 5) were flagged but we retained these as distinct constructs.
Is being autistic a distal risk marker for suicide? How does being autistic connect to other nodes to suggest pathways to suicidal thoughts?
Single network estimation
The network contained 138 edges between the 19 nodes. Eleven edges directly connected with thoughts of suicide and self‐harm. The strongest connections (shown in Figure 2) were with feeling depressed and hopeless (partial correlation, r = 0.19), believing others wish to be rid of you (r = 0.16), believing life would be better for others if you were gone (r = 0.16), feeling like a failure (r = 0.12) and movement differences (r = 0.14). Being autistic connected directly to feeling like an outsider, lacking caring and supportive friends, movement differences, and anxiety. Overall, this suggests that being autistic is a distal risk marker for suicide, which activates the network through anxiety, feeling like an outsider, lacking caring and supportive friends, and movement differences.
FIGURE 2.
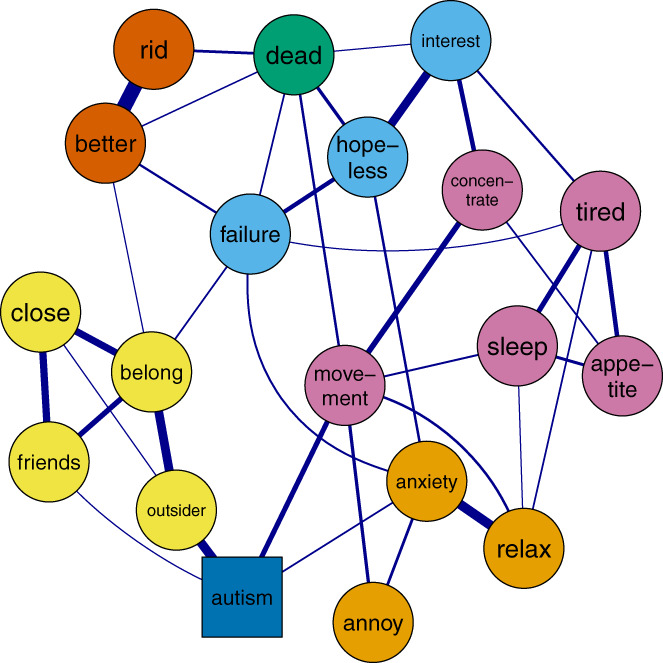
Whole sample network graph showing how being autistic connects with network nodes to thoughts of suicide and self‐harm. Note: Yellow = thwarted belongingness, light blue = low mood, green = thoughts of self‐harm or suicide, orange = anxiety, dark orange = perceived burdensomeness, pink = somatic experiences and dark blue = autism diagnosis. For full details and node names see Table 2. Graph minimum = 0.09, max = 0.14, cut = 0.09 for ease of interpretation. Theme = colorblind.
As shown in Figure 2, movement differences connected directly to thoughts of suicide and self‐harm. Feeling like an outsider and lacking caring and supportive friends connected to thoughts of suicide and self‐harm through feeling like you do not belong and feeling like a failure. Anxiety connected to thoughts of suicide and self‐harm through feeling depressed and hopeless. Overall, this suggests simultaneous pathways from autism diagnosis to thoughts of suicide and self‐harm through (i) movement differences; (ii) feeling like you do not belong, that others would be better off without you and feeling like a failure; (iii) anxiety and feeling depressed/ hopeless; and (iv) anxiety, somatic experiences, and low mood.
-
2
Are the network structure and global strength consistent for autistic and non‐autistic people? How do connections between risk markers differ for autistic compared with non‐autistic people?
Joint network estimation
There were consistent edges in the autistic (n = 160) and non‐autistic (n = 162) between 18 nodes with strongest connections shown in Figure 3. In both networks, nine nodes connected to thoughts of suicide and self‐harm and in both groups the strongest edges were with feeling hopeless (autistic r = 0.21, non‐autistic r = 0.13) and believing others would be better off if you were gone (autistic r = 0.12, non‐autistic r = 0.14). In the autistic group, strongest edges also included feeling like a failure (r = 0.15), and in the non‐autistic group, believing others wish to be rid of you (r = 0.22).
FIGURE 3.
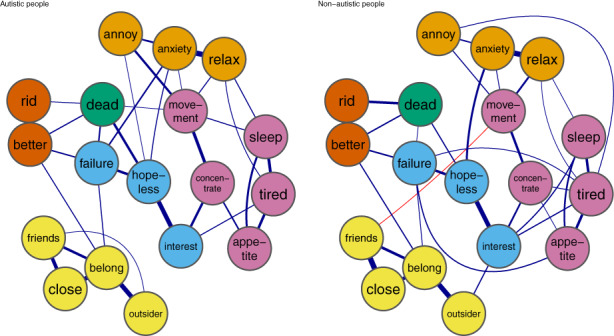
Network graphs for autistic (left) and non‐autistic (right) adults. Note: Yellow = thwarted belongingness, light blue = low mood, green = thoughts of self‐harm or suicide, orange = anxiety, dark orange = perceived burdensomeness, pink = somatic experiences. For full details and node names, see Table 2. Graph minimum = 0.08, max = 0.95, cut = 0.08 for ease of interpretation.Theme = colorblind. We use the averagelayout function to provide a consistent layout for networks.
Network comparisons
The Network Comparison Test (NCT) reported that global density was greater in the non‐autistic network (global density = 8.47) than in the autistic network (global density = 8.30), but this was not statistically significant (p = 0.30).
Eight edge strengths differed significantly between autistic and non‐autistic networks. First, four edges connected mood symptoms with somatic experiences for the non‐autistic network but were absent in the autistic network. These edges connected: (i) losing interest and sleep difficulties (autistic network r = 0, non‐autistic network r = 0.36, p = 0.02), (ii) feeling annoyed and feeling tired (autistic network r = 0, non‐autistic network r = 0.10, p < 0.01), (iii) feeling like a failure and appetite difficulties (autistic network r = 0, non‐autistic network r = 0.23, p = 0.02), and (iv) sleep difficulties and thoughts of self‐harm and ending life (autistic network r = 0, non‐autistic network r = 0.04, p = 0.01). Overall, this suggests mood symptoms are associated with somatic experiences for non‐autistic people but are independent for autistic people.
Second, three edges connected thwarted belonging experiences with mood symptoms or burdensomeness for non‐autistic people but were absent for autistic people. These were edges between: (i) feeling like an outsider with (a) feeling annoyed (autistic network = 0, non‐autistic network = 0.07, p = 0.05) and (b) losing interest (autistic network = 0, non‐autistic network = 0.04, p = 0.03); (ii) lacking caring and supportive friends and believing other would be better off if you were gone (autistic network = 0, non‐autistic network = 0.04, p = 0.02). Furthermore, (iii) not feeling close to other people was negatively connected to having difficulty relaxing (autistic network = −0.02, non‐autistic = 0, p = 0.04) in autistic people but unconnected in non‐autistic people. Overall, this suggests that thwarted belonging is independent of, or differently connected to affective symptoms or burdensomeness for autistic compared with non‐autistic people.
As shown in Figure 4, similar nodes were most influential in each group; the 75th percentile expected influence nodes in both groups were as follows: (1) feeling like you do not belong, (2) feeling depressed, (3) believing others wish you were gone, (4) feeling anxious, and (5) having difficulty relaxing (autistic network) and feeling tired (non‐autistic network). Unstandardized expected influence is reported in Figure S1b. Expected Influence was similar in each network, however, two nodes were significantly more inter‐connected in the non‐autistic than autistic networks. Feeling like an outsider (total sum of edges on this node in autistic network = 0.60, non‐autistic network = 0.78, p = 0.01) and feeling tired (autistic network = 0.88, non‐autistic network = 1.03, p = 0.05) had significantly greater expected influence in the non‐autistic than autistic networks.
FIGURE 4.
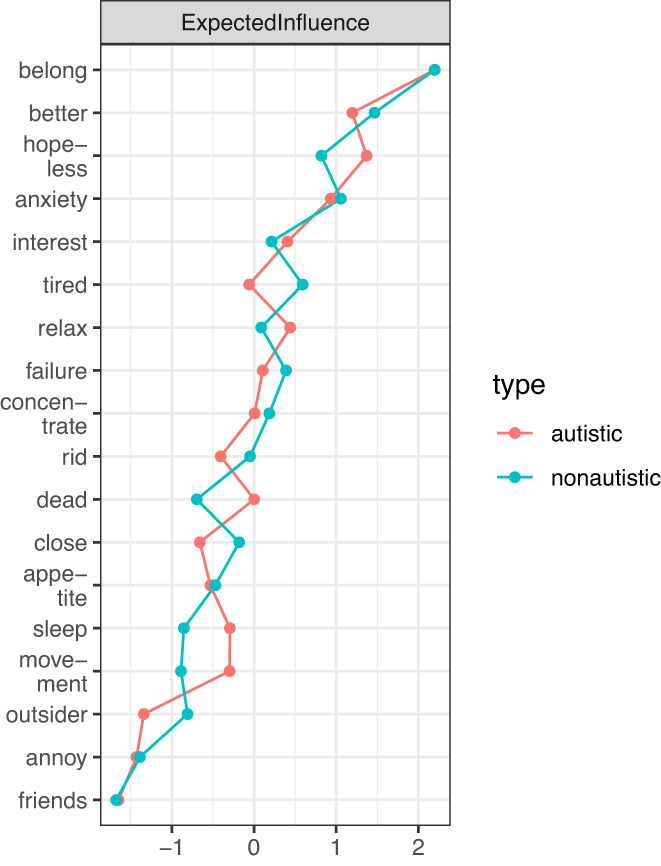
Standardized relative expected influence of nodes within autistic and non‐autistic networks.
Network stability
As shown in Figures S2–S7, the edge weights were accurately measured. The centrality stability coefficient was 0.52 in the non‐autistic network and 0.75 in the autistic network suggesting that expected influence scores were stable.
DISCUSSION
For the first time, we used network analysis to extend our theoretical understanding of how anxiety and depression contribute to suicidal thoughts for autistic and non‐autistic adults. In line with our expectations, autistic adults reported more frequent suicidal thoughts, anxiety, depression, thwarted belonging, and perceived burdensomeness than non‐autistic adults. Exploratory analyses reported that being autistic connected directly to feeling like an outsider, lacking caring and supportive friends, anxiety, and movement (such as restlessness). These experiences connected to suicidal thoughts through feelings of low mood (hopelessness or failure) and burdensomeness (believing others wish you were gone), except movement, which connected directly to suicidal thoughts. Group difference tests reported that overall inter‐connectedness was consistent for autistic and non‐autistic networks. In the non‐autistic network, mood symptoms connected to thwarted belonging and somatic experiences, but these were independent in the autistic network. Feeling tired and like an outsider were less inter‐connected for autistic than for non‐autistic adults.
In line with previous research, autistic adults reported more frequent suicidal thoughts (Cassidy et al., 2014), burdensomeness (Camm‐Crosbie et al., 2019; Pelton et al., 2020b), unmet need for belonging (Milton & Sims, 2016), anxiety and depression (Lever & Geurts, 2016) than non‐autistic adults. In line with the network approach, there were multiple interactions within and between items designed to measure distinct constructs (Borsboom, 2017; Borsboom & Cramer, 2013; Cramer et al., 2010) and more experiences connected to suicidal thoughts than epidemiology studies suggest (De Beurs, 2017; De Beurs et al., 2017, 2021). Overall, this suggests network analysis is a helpful transdiagnostic alternative to research boundaried by non‐autistic categories (Lombardo et al., 2019; Weiss, 2014) to extend our understanding of the development of suicidal thoughts and behaviors.
Our results describe, for the first time, how being autistic may be a distal risk marker for suicide. As described in conceptual model Figure 5, being autistic is connected directly to daily stressors, feeling like an outsider, lacking friends, and anxiety in line with research describing that autistic adults report loneliness (Causton‐Theoharis et al., 2009; Hedley, Uljarević, Wilmot, et al., 2018), feeling “othered” (being treated as intrinsically different or inhuman) (Cage et al., 2019; Michael, 2021) and experience significant daily anxiety (Uljarević et al., 2020), which negatively impacts quality of life (Mason et al., 2018). In line with previous research, there was no connection between anxiety and thwarted belonging (Rath et al., 2019). Anxiety is connected with somatic experiences, such as sleep difficulties, which is a particular concern for autistic people in the development of suicidal thoughts and behaviors (Cassidy, Cogger‐Ward, et al., 2021). In our network, sleep was strongly inter‐connected with tiredness and appetite, suggesting inter‐dependency, and linked with movement and concentration difficulties. This could suggest anxiety erodes somatic coping mechanisms to decrease mood. Thwarted belonging connected to feelings of burdensomeness as in previous network analyses (De Beurs et al., 2019) and to feeling like a failure: a more nuanced description of how thwarted belonging contributes to depression (Kleiman et al., 2014), resonating with “failed social struggle” described by the Integrated Motivational Volitional model of suicide (O'Connor, 2011). Both burdensomeness items (believing others are better off without you/wish to be rid of you), feeling like a failure, hopeless, and losing interest in life connected closely and directly to suicidal thoughts, suggesting these are potent warning signs of those most at risk. Thus, in sum, as shown in Figure 5, our results suggest a progression from daily stressful or traumatic experiences through reduced coping and warning signs to suicidal thoughts.
FIGURE 5.
Conceptual model of progression from environmental stressors, reduced coping, and warning signs to suicidal thoughts.
The connection between being autistic and movement reflects the long‐standing role of repetitive behaviors as a diagnostic criterion. More surprising is the direct connection from movement to suicidal thoughts though one study reported agitation as a unique risk marker for suicide attempts in individuals with high autistic traits (Takara & Kondo, 2014). One possibility is that other experiences, such as sensory overload, may be coped with through movement and/or other warning signs that mediate the relationship with suicidal thoughts. However, “stimming” (self‐stimulation) is important for autistic people to regulate uncontainable emotions (Kapp et al., 2019; Pearson & Rose, 2021) so future partnership research could explore the meaning of our findings and how stimming and movement regulate emotional distress.
Our model allows interventions to be identified at each level; for example, understanding and reducing anxiety (Parr et al., 2020), promoting belonging (Milton & Sims, 2016) and autism acceptance (Cage et al., 2018) could reduce the extent to which the network is activated. Maintaining relationships (Hedley, Uljarević, Foley, et al., 2018; Hedley, Uljarević, Wilmot, et al., 2018), peer relationships (Cage et al., 2022), enabling a healthy lifestyle, and meeting support needs (Cassidy, Bradley, Shaw, et al., 2018) could prevent the progression from stressors to warning signs. Identifying hopelessness, burdensomeness, loss of interest in life and failure could be incorporated into safety planning/risk assessments to improve crisis care (Schwartzman et al., 2021). Our model extends the ITS suggesting that, in addition to burdensomeness, low mood is proximal and significant in the development of suicidal thoughts. The distal role of thwarted belonging reflects previous network analyses (De Beurs et al., 2019; Ordóñez‐Carrasco et al., 2021) and the protective role of connectedness outlined in the 3Step theory (Klonsky & May, 2015). Our results emphasize the role of burdensomeness as a proximal risk marker, but failure and hopelessness also resonate with broader emotional pain proposed by the Three‐step Theory (3ST) (Klonsky & May, 2015). Caution should be exercised that our model includes only a subset of risk markers and those at greatest risk of suicide are likely to experience a wide range of risk markers (Cassidy et al., 2022).
However, before pursuing future research, we should consider the comparison between autistic and non‐autistic networks. Overall connectedness was consistent between autistic and non‐autistic networks, but connections from mood symptoms with somatic and thwarted belonging experiences were absent for autistic adults, and feeling tired and like an outsider were significantly less inter‐connected in the autistic than non‐autistic network. These results suggest that somatic experiences described in the PHQ‐9 and GAD‐7 are not the most pertinent to capture emotional change for autistic people. New tools to measure depression and anxiety have identified more precise somatic indicators for autistic adults, such as a change in fatigue, rather than the presence of fatigue (Cassidy, Bradley, Cogger‐Ward, et al., 2021) and anxiety indicators, such as feeling shaky (Rodgers et al., 2016, 2020). Similarly, feeling like an outsider has already been identified as a less meaningful indicator of thwarted belonging for autistic than for non‐autistic adults (Pelton et al., 2020a). Thus, our model takes an important first step in demonstrating how autistic adults experience general population risk markers but, may not yet capture unique risk markers for autistic adults. Additional stressors could include uncertainty (Boulter et al., 2014), pressures contributing to autistic burnout (Higgins et al., 2021; Mantzalas et al., 2022; Raymaker et al., 2020), and research could explore how the experience of those stressors is influenced by age (Stewart et al., 2022) or gender (Kõlves et al., 2021) for autistic people to contribute to unique risk.
Our study highlights methodological challenges in comparing suicidal thoughts and behaviors for autistic and non‐autistic adults. First, drawing on non‐clinical samples, autistic adults report shockingly more frequent experiences of depression, suicidal thoughts, and behaviors than non‐autistic adults; researchers should carefully consider recruitment and statistical methods for accurate comparison. Second, our findings suggest we may be reaching the limits of what we can infer about suicidal thoughts and behaviors for autistic adults using constructs and measurement tools designed for non‐autistic adults. Commentary argues that research should focus on relevant experiences for autistic people rather than statistically valid non‐autistic measurement tools (Jones, 2022) reflecting more general concerns about precise construct definition and accurate measurement for suicide and psychological theory (Bringmann et al., 2022; Lawson & Robins, 2021; Millner et al., 2020). Overall, this could suggest that future theory development take autistic lived experience as its starting point and articulate a model independent of non‐autistic experience.
This study has several strengths: this is the first study to apply network analysis to explore suicide theory in autistic people responding to calls to go beyond single risk factor studies and apply novel, rigorous methods in a transdiagnostic approach (Franklin et al., 2017; Lombardo et al., 2019; Millner et al., 2020). The development of support, interventions, risk assessments, and crisis services for autistic adults (Cassidy, Cogger‐Ward, et al., 2021; Jager‐Hyman et al., 2020) is essential to meet global suicide prevention goals. This study is limited by an absence of valid measurement tools to explore suicidal thoughts and behaviors for autistic people at the time of design. Researchers should consider using the recently published Suicidal Behaviours Questionnaire‐Revised (Autism Spectrum Condition) (SBQ‐ASC) (Cassidy, Bradley, Cogger‐Ward, & Rodgers, 2021) or the Suicidal Ideation Attributes Scale‐Modified (SIDAS‐M) (Hedley et al., 2022). This study used self‐report autism diagnosis, which falls short of “gold standard” confirmation of autism but allows for wider participation. The sample size is relatively small (see van Borkulo et al., 2022 for discussion on appropriate sample size) for group comparison network analyses); thus, future research could employ cohort, population studies, or simulation studies to replicate and extend our findings. Furthermore, our cross‐sectional design cannot infer causality; thus, findings should be considered strictly exploratory, and taking a time‐series or longitudinal approach should confirm intervention targets (Rath et al., 2019). Future network analyses could, thus, apply temporal analyses (Haslbeck & Waldorp, 2015) drawing on ecological momentary assessment (Rath et al., 2019), moderation analysis to explore how autistic characteristics (such as difficulty switching attention) moderate connections between risk markers (Haslbeck, Borsboom, et al., 2021) or cluster analysis to accurately define and measure constructs (Forkmann et al., 2018; Golino & Epskamp, 2017).
CONCLUSION
This study reports that being autistic represents a unique distal risk marker for suicidal thoughts and behaviors through feeling like an outsider, anxiety, and movement differences. Research should extend these exploratory findings using longitudinal study designs in partnership with autistic people, ensuring constructs are meaningfully defined to produce suicide theory that accurately reflects lived experience of autistic people. This will be vital to ensure tailored suicide prevention for autistic adults.
Supporting information
Appendix S1
Figure S1
Figures S2–S7
ACKNOWLEDGMENTS
We would like to extend gratitude to everyone who took part in this research. We thank Sharon Gardner and other members of the Coventry Design group for their support in conceptualizing the study, selecting and devising the study materials, providing well‐being guidance, discussing and interpreting results, and developing the model. This study acknowledges the kind support of Carrie Allison and Paula Smith at the Autism Research Centre, University of Cambridge for assisting with contacting participants registered in the Cambridge Autism Research Database and of Autistica for advertising our study via their Discover network. We are grateful to Sacha Epskamp, Adela Isvoranu, Jonas Haslbeck, and Julian Berger at the University of Amsterdam Network Analysis Winter school 2020. This study forms part of a component of PhD study with financial support from Coventry University. Mirabel Pelton is grateful for the generous support of grants from Funds for Women Graduates [Ref: GA‐00109], Coventry City of Culture, PsyPAG, Centre for Global Engagement, Coventry University, and Coventry University Students Union. Sarah Cassidy was supported by the Economic and Social Research Council [grant number: ES/N000501/2], Autistica, the International Society for Autism Research, and the Slifka‐Ritvo Foundation. Hayley Crawford is supported by the National Institute for Health Research (NIHR) Applied Research Centre West Midlands. The views expressed are those of the author(s) and not necessarily those of the NHS, NIHR, or Department of Health and Social Care. Simon Baron‐Cohen received funding from the Wellcome Trust 214322\Z\18\Z. For the purpose of Open Access, the author has applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission. Simon Baron‐Cohen also received funding from the Autism Centre of Excellence, SFARI, the Templeton World Charitable Fund, the MRC, and the NIHR Cambridge Biomedical Research Centre. The research was supported by the NIHR Applied Research Collaboration East of England. Any views expressed are those of the author(s) and not necessarily those of the funder.
Pelton, M. K. , Crawford, H. , Bul, K. , Robertson, A. E. , Adams, J. , de Beurs, D. , Rodgers, J. , Baron‐Cohen, S. , & Cassidy, S. (2023). The role of anxiety and depression in suicidal thoughts for autistic and non‐autistic people: A theory‐driven network analysis. Suicide and Life‐Threatening Behavior, 53, 426–442. 10.1111/sltb.12954
Endnote
We refer to ‘autistic people’ (termed ‘identity‐first language’) to reflect the published preference of the majority of autistic people that autism is an integral component of identity (Kenny et al., 2016). We avoid the use of ‘person‐first language’ (such as ‘person with autism’), which has been associated with stigma and dehumanization (Botha et al., 2021). For guidance on language choices in autism research see (Bottema‐Beutel et al., 2021).
Contributor Information
Mirabel K. Pelton, MSc, Email: peltonm@coventry.ac.uk.
Sarah Cassidy, Email: sarah.cassidy@nottingham.ac.uk.
REFERENCES
- Allison, C. , Auyeung, B. , & Baron‐Cohen, S. (2012). Toward brief “red flags” for autism screening: The short autism spectrum quotient and the short quantitative checklist in 1,000 cases and 3,000 controls. Journal of the American Academy of Child & Adolescent Psychiatry, 51(2), 202–212. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (DSM‐5®). American Psychiatric Pub. [Google Scholar]
- Arwert, T. G. , & Sizoo, B. B. (2020). Self‐reported suicidality in male and female adults with autism spectrum disorders: Rumination and self‐esteem. Journal of Autism and Developmental Disorders, 50(10), 3598–3605. [DOI] [PubMed] [Google Scholar]
- Barthel, A. L. , Pinaire, M. A. , Curtiss, J. E. , Baker, A. W. , Brown, M. L. , Hoeppner, S. S. , Bui, E. , Simon, N. M. , & Hofmann, S. G. (2020). Anhedonia is central for the association between quality of life, metacognition, sleep, and affective symptoms in generalized anxiety disorder: A complex network analysis. Journal of Affective Disorders, 277, 1013–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard, C. , Millner, A. J. , Forgeard, M. J. , Fried, E. I. , Hsu, K. J. , Treadway, M. T. , Leonard, C. V. , Kertz, S. J. , & Björgvinsson, T. (2016). Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Medicine, 46(16), 3359–3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird, G. , & Cook, R. (2013). Mixed emotions: the contribution of alexithymia to the emotional symptoms of autism. Translational Psychiatry, 3(7), e285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D. , & Cramer, A. O. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Borsboom, D. , Deserno, M. K. , Rhemtulla, M. , Epskamp, S. , Fried, E. I. , McNally, R. J. , Robinaugh, D. J. , Perugini, M. , Dalege, J. , & Costantini, G. (2021). Network analysis of multivariate data in psychological science. Nature Reviews Methods Primers, 1(1), 1–18. [Google Scholar]
- Botha, M. , & Frost, D. M. (2020). Extending the minority stress model to understand mental health problems experienced by the autistic population. Society and Mental Health, 10(1), 20–34. [Google Scholar]
- Botha, M. , Hanlon, J. , & Williams, G. L. (2021). Does language matter? Identity‐first versus person‐first language use in autism research: A response to Vivanti. Journal of Autism and Developmental Disorders, 53(2), 870–878. 10.1007/s10803-020-04858-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottema‐Beutel, K. , Kapp, S. K. , Lester, J. N. , Sasson, N. J. , & Hand, B. N. (2021). Avoiding ableist language: Suggestions for autism researchers. Autism in Adulthood, 3(1), 18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulter, C. , Freeston, M. , South, M. , & Rodgers, J. (2014). Intolerance of uncertainty as a framework for understanding anxiety in children and adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44(6), 1391–1402. [DOI] [PubMed] [Google Scholar]
- Bringmann, L. F. , Elmer, T. , & Eronen, M. I. (2022). Back to basics: The importance of conceptual clarification in psychological science. Current Directions in Psychological Science, 31(4), 340–346. 10.1177/09637214221096485 [DOI] [Google Scholar]
- Cage, E. , Cranney, R. , & Botha, M. (2022). Brief report: Does autistic community connectedness moderate the relationship between masking and wellbeing? Autism in Adulthood, 4(3), 247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cage, E. , Di Monaco, J. , & Newell, V. (2018). Experiences of autism acceptance and mental health in autistic adults. Journal of Autism and Developmental Disorders, 48(2), 473–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cage, E. , Di Monaco, J. , & Newell, V. (2019). Understanding, attitudes and dehumanisation towards autistic people. Autism, 23(6), 1373–1383. [DOI] [PubMed] [Google Scholar]
- Camm‐Crosbie, L. , Bradley, L. , Shaw, R. , Baron‐Cohen, S. , & Cassidy, S. (2019). ‘People like me don't get support’: Autistic adults' experiences of support and treatment for mental health difficulties, self‐injury and suicidality. Autism, 23(6), 1431–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy, S. , Au‐Yeung, S. , Robertson, A. , Cogger‐Ward, H. , Richards, G. , Allison, C. , Bradley, L. , Kenny, R. , O'Connor, R. , & Mosse, D. (2022). Autism and autistic traits in those who died by suicide in England. The British Journal of Psychiatry, 221, 1–9. [DOI] [PubMed] [Google Scholar]
- Cassidy, S. , Bradley, L. , Bowen, E. , Wigham, S. , & Rodgers, J. (2018). Measurement properties of tools used to assess depression in adults with and without autism spectrum conditions: A systematic review. Autism Research, 11(5), 738–754. 10.1002/aur.1922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy, S. , Bradley, L. , Cogger‐Ward, H. , Graham, J. , & Rodgers, J. (2021). Development and validation of the Autistic Depression Assessment Tool–Adult (ADAT‐A) in autistic adults .
- Cassidy, S. , Bradley, L. , Shaw, R. , & Baron‐Cohen, S. (2018). Risk markers for suicidality in autistic adults. Molecular Autism, 9(1), 42. 10.1186/s13229-018-0226-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy, S. , Cogger‐Ward, H. , Robertson, A. E. , Goodwin, J. , & Rodgers, J. (2021). Autism community priorities for suicide prevention. An International Society for Autism Research Policy Brief. [Google Scholar]
- Cassidy, S. A. , Bradley, L. , Cogger‐Ward, H. , & Rodgers, J. (2021). Development and validation of the suicidal behaviours questionnaire‐autism spectrum conditions in a community sample of autistic, possibly autistic and non‐autistic adults. Molecular Autism, 12(1), 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy, S. A. , Bradley, L. , Cogger‐Ward, H. , Shaw, R. , Bowen, E. , Glod, M. , Baron‐Cohen, S. , & Rodgers, J. (2020). Measurement properties of the suicidal behaviour questionnaire‐revised in autistic adults. Journal of Autism and Developmental Disorders, 50(10), 3477–3488. 10.1007/s10803-020-04431-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy, S. A. , Bradley, P. , Robinson, J. , Allison, C. , McHugh, M. , & Baron‐Cohen, S. (2014). Suicidal ideation and suicide plans or attempts in adults with Asperger's syndrome attending a specialist diagnostic clinic: A clinical cohort study. The Lancet Psychiatry, 1(2), 142–147. [DOI] [PubMed] [Google Scholar]
- Cassidy, S. A. , Robertson, A. , Townsend, E. , O'Connor, R. C. , & Rodgers, J. (2020). Advancing our understanding of self‐harm, suicidal thoughts and Behaviours in autism. Journal of Autism and Developmental Disorders, 50(10), 3445–3449. 10.1007/s10803-020-04643-9 [DOI] [PubMed] [Google Scholar]
- Causton‐Theoharis, J. , Ashby, C. , & Cosier, M. (2009). Islands of loneliness: Exploring social interaction through the autobiographies of individuals with autism. Intellectual and Developmental Disabilities, 47(2), 84–96. 10.1352/1934-9556-47.2.84 [DOI] [PubMed] [Google Scholar]
- Costantini, G. , Richetin, J. , Preti, E. , Casini, E. , Epskamp, S. , & Perugini, M. (2019). Stability and variability of personality networks. A tutorial on recent developments in network psychometrics. Personality and Individual Differences, 136, 68–78. [Google Scholar]
- Constantino, J. N. , Abbacchi, A. M. , Saulnier, C. , Klaiman, C. , Mandell, D. S. , Zhang, Y. , Hawks, Z. , Bates, J. , Klin, A. , & Shattuck, P. (2020). Timing of the diagnosis of autism in African American children. Pediatrics, 146(3), e20193629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa, A. P. , Loor, C. , & Steffgen, G. (2020). Suicidality in adults with autism spectrum disorder: The role of depressive symptomatology, alexithymia, and antidepressants. Journal of Autism and Developmental Disorders, 50(10), 3585–3597. [DOI] [PubMed] [Google Scholar]
- Cramer, A. O. , Waldorp, L. J. , Van Der Maas, H. L. , & Borsboom, D. (2010). Comorbidity: A network perspective. Behavioral and Brain Sciences, 33(2–3), 137–150. [DOI] [PubMed] [Google Scholar]
- Daniels, A. M. , Rosenberg, R. E. , Anderson, C. , Law, J. K. , Marvin, A. R. , & Law, P. A. (2012). Verification of parent‐report of child autism spectrum disorder diagnosis to a web‐based autism registry. Journal of Autism and Developmental Disorders, 42(2), 257–265. [DOI] [PubMed] [Google Scholar]
- Davidson, C. , Wingate, L. , Grant, D. , Judah, M. , & Mills, A. (2011). Interpersonal suicide risk and ideation: The influence of depression and social anxiety. Journal of Social and Clinical Psychology, 30(8), 842–855. [Google Scholar]
- De Beurs, D. (2017). Network analysis: A novel approach to understand suicidal behaviour. International Journal of Environmental Research and Public Health, 14(3), 219. [Google Scholar]
- De Beurs, D. , Bockting, C. , Kerkhof, A. , Scheepers, F. , O'Connor, R. , Penninx, B. , & van de Leemput, I. (2021). A network perspective on suicidal behavior: Understanding suicidality as a complex system. Suicide and Life‐threatening Behavior, 51(1), 115–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Beurs, D. , Fried, E. I. , Wetherall, K. , Cleare, S. , O'Connor, D. B. , Ferguson, E. , O'Carroll, R. E. , & O'Connor, R. C. (2019). Exploring the psychology of suicidal ideation: A theory driven network analysis. Behaviour Research and Therapy, 120, 103419. [DOI] [PubMed] [Google Scholar]
- De Beurs, D. P. , Van Borkulo, C. D. , & O'Connor, R. C. (2017). Association between suicidal symptoms and repeat suicidal behaviour within a sample of hospital‐treated suicide attempters. British Journal of Psychiatry Open, 3(3), 120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Torre, J. A. , Ronaldson, A. , Vilagut, G. , Serrano‐Blanco, A. , Molina, A. J. , Martín, V. , Valderas, J. M. , Dutta, R. , Dregan, A. , & Alonso, J. (2021). Improving suicide surveillance systems through the use of the patient health Questionnaire‐9. Journal of Affective Disorders, 293, 71–72. [DOI] [PubMed] [Google Scholar]
- Dow, D. , Morgan, L. , Hooker, J. L. , Michaels, M. S. , Joiner, T. E. , Woods, J. , & Wetherby, A. M. (2021). Anxiety, depression, and the Interpersonal Theory of Suicide in a community sample of adults with autism spectrum disorder. Archives of Suicide Research, 25(2), 297–314. [DOI] [PubMed] [Google Scholar]
- Fombonne, E. , Coppola, L. , Mastel, S. , & O’Roak, B. J. (2022). Validation of autism diagnosis and clinical data in the SPARK cohort. Journal of Autism and Developmental Disorders, 52(8), 3383–3398. 10.1007/s10803-021-05218-y [DOI] [PubMed] [Google Scholar]
- Forkmann, T. , Teismann, T. , Stenzel, J. , Glaesmer, H. , & De Beurs, D. (2018). Defeat and entrapment: More than meets the eye? Applying network analysis to estimate dimensions of highly correlated constructs. BMC Medical Research Methodology, 18(1), 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin, J. C. , Ribeiro, J. D. , Fox, K. R. , Bentley, K. H. , Kleiman, E. M. , Huang, X. , Musacchio, K. M. , Jaroszewski, A. C. , Chang, B. P. , & Nock, M. K. (2017). Risk factors for suicidal thoughts and behaviors: A meta‐analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Fried, E. I. , Epskamp, S. , Nesse, R. M. , Tuerlinckx, F. , & Borsboom, D. (2016). What are ‘good’ depression symptoms? Comparing the centrality of DSM and non‐DSM symptoms of depression in a network analysis. Journal of Affective Disorders, 189, 314–320. [DOI] [PubMed] [Google Scholar]
- Golino, H. F. , & Epskamp, S. (2017). Exploratory graph analysis: A new approach for estimating the number of dimensions in psychological research. PLoS One, 12(6), e0174035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham, K. , Unruh, K. , & Lord, C. (2015). Depression and its measurement in verbal adolescents and adults with autism spectrum disorder. Autism, 19(4), 491–504. 10.1177/1362361314536625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths, S. , Allison, C. , Kenny, R. , Holt, R. , Smith, P. , & Baron‐Cohen, S. (2019). The vulnerability experiences quotient (VEQ): A study of vulnerability, mental health and life satisfaction in autistic adults. Autism Research, 12(10), 1516–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck, J. , Ryan, O. , Robinaugh, D. J. , Waldorp, L. J. , & Borsboom, D. (2022). Modeling psychopathology: From data models to formal theories. Psychological Methods, 27, 930–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck, J. , & Waldorp, L. J. (2015). mgm: Estimating time‐varying mixed graphical models in high‐dimensional data. arXiv Preprint arXiv:1510.06871 .
- Haslbeck, J. M. , Borsboom, D. , & Waldorp, L. J. (2021). Moderated network models. Multivariate Behavioral Research, 56(2), 256–287. [DOI] [PubMed] [Google Scholar]
- Haslbeck, J. M. B. , & Waldorp, L. J. (2020). mgm : Estimating time‐varying mixed graphical models in high‐dimensional data. Journal of Statistical Software, 93(8), 1–46. 10.18637/jss.v093.i08 [DOI] [Google Scholar]
- Hedley, D. , Batterham, P. J. , Bury, S. M. , Clapperton, A. , Denney, K. , Dissanayake, C. , Fox, P. , Frazier, T. W. , Gallagher, E. , Hayward, S. M. , Robinson, J. , Sahin, E. , Trollor, J. , Uljarević, M. , & Stokes, M. A. (2022). The suicidal ideation attributes scale‐modified (SIDAS‐M): Development and preliminary validation of a new scale for the measurement of suicidal ideation in autistic adults. Autism: The International Journal of Research & Practice. 10.1177/13623613221131234 [DOI] [PubMed] [Google Scholar]
- Hedley, D. , Uljarević, M. , Foley, K. , Richdale, A. , & Trollor, J. (2018). Risk and protective factors underlying depression and suicidal ideation in autism spectrum disorder. Depression and Anxiety, 35(7), 648–657. [DOI] [PubMed] [Google Scholar]
- Hedley, D. , Uljarević, M. , Wilmot, M. , Richdale, A. , & Dissanayake, C. (2018). Understanding depression and thoughts of self‐harm in autism: A potential mechanism involving loneliness. Research in Autism Spectrum Disorders, 46, 1–7. 10.1016/j.rasd.2017.11.003 [DOI] [Google Scholar]
- Higgins, J. M. , Arnold, S. R. , Weise, J. , Pellicano, E. , & Trollor, J. N. (2021). Defining autistic burnout through experts by lived experience: Grounded Delphi method investigating# AutisticBurnout. Autism, 25(8), 2356–2369. [DOI] [PubMed] [Google Scholar]
- Hill, R. M. , Rey, Y. , Marin, C. E. , Sharp, C. , Green, K. L. , & Pettit, J. W. (2015). Evaluating the interpersonal needs questionnaire: Comparison of the reliability, factor structure, and predictive validity across five versions. Suicide and Life‐threatening Behavior, 45(3), 302–314. 10.1111/sltb.12129 [DOI] [PubMed] [Google Scholar]
- Hirvikoski, T. , Mittendorfer‐Rutz, E. , Boman, M. , Larsson, H. , Lichtenstein, P. , & Bolte, S. (2016). Premature mortality in autism spectrum disorder. The British Journal of Psychiatry: The Journal of Mental Science, 208(3), 232–238. [DOI] [PubMed] [Google Scholar]
- Hoekstra, R. A. , Vinkhuyzen, A. A. , Wheelwright, S. , Bartels, M. , Boomsma, D. I. , Baron‐Cohen, S. , Posthuma, D. , & van der Sluis, S. (2011). The construction and validation of an abridged version of the autism‐spectrum quotient (AQ‐Short). Journal of Autism and Developmental Disorders, 41(5), 589–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager‐Hyman, S. , Maddox, B. B. , Crabbe, S. R. , & Mandell, D. S. (2020). Mental health clinicians’ screening and intervention practices to reduce suicide risk in autistic adolescents and adults. Journal of Autism and Developmental Disorders, 50(10), 3450–3461. [DOI] [PubMed] [Google Scholar]
- Joiner, T. E. (2005). Why people die by suicide. Harvard University Press. [Google Scholar]
- Jokiranta‐Olkoniemi, E. , Gyllenberg, D. , Sucksdorff, D. , Suominen, A. , Kronström, K. , Chudal, R. , & Sourander, A. (2021). Risk for premature mortality and intentional self‐harm in autism spectrum disorders. Journal of Autism and Developmental Disorders, 51(9), 3098–3108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, P. (2020). networktools: Tools for Identifying Important Nodes in Networks. R package version 1.2.3. https://CRAN.Rproject.org/package=networkstools
- Jones, P. J. , Mair, P. , Simon, T. , & Zeileis, A. (2020). Network trees: A method for recursively partitioning covariance structures. Psychometrika, 85(4), 926–945. [DOI] [PubMed] [Google Scholar]
- Jones, S. C. (2022). Measuring the wrong thing the right way? Time to rethink autism research tools. Autism in Adulthood, 4, 104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapp, S. K. , Steward, R. , Crane, L. , Elliott, D. , Elphick, C. , Pellicano, E. , & Russell, G. (2019). ‘People should be allowed to do what they like’: Autistic adults' views and experiences of stimming. Autism, 23(7), 1782–1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny, L. , Hattersley, C. , Molins, B. , Buckley, C. , Povey, C. , & Pellicano, E. (2016). Which terms should be used to describe autism? Perspectives from the UK autism community. Autism, 20(4), 442–462. [DOI] [PubMed] [Google Scholar]
- Kirby, A. V. , Bakian, A. V. , Zhang, Y. , Bilder, D. A. , Keeshin, B. R. , & Coon, H. (2019). A 20‐year study of suicide death in a statewide autism population. Autism Research, 12(4), 658–666. 10.1002/aur.2076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman, E. M. , Liu, R. T. , & Riskind, J. H. (2014). Integrating the interpersonal psychological theory of suicide into the depression/suicidal ideation relationship: A short‐term prospective study. Behavior Therapy, 45(2), 212–221. 10.1016/j.beth.2013.10.007 [DOI] [PubMed] [Google Scholar]
- Klonsky, E. D. , & May, A. M. (2015). The three‐step theory (3ST): A new theory of suicide rooted in the ‘ideation‐to‐action’ framework. International Journal of Cognitive Therapy, 8(2), 114–129. 10.1521/ijct.2015.8.2.114 [DOI] [Google Scholar]
- Kõlves, K. , Fitzgerald, C. , Nordentoft, M. , Wood, S. J. , & Erlangsen, A. (2021). Assessment of suicidal behaviors among individuals with autism spectrum disorder in Denmark. JAMA Network Open, 4(1), e2033565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Rhee, E. , & Nicholas, D. (2017). Suicidality in autism spectrum disorder: A commentary. Advances in Neurodevelopmental Disorders, 1(3), 190–195. 10.1007/s41252-017-0018-4 [DOI] [Google Scholar]
- Lai, M. , & Baron‐Cohen, S. (2015). Identifying the lost generation of adults with autism spectrum conditions. The Lancet Psychiatry, 2(11), 1013–1027. [DOI] [PubMed] [Google Scholar]
- Large, M. , Corderoy, A. , & McHugh, C. (2021). Is suicidal behaviour a stronger predictor of later suicide than suicidal ideation? A systematic review and meta‐analysis. Australian and New Zealand Journal of Psychiatry, 55(3), 254–267. 10.1177/0004867420931161 [DOI] [PubMed] [Google Scholar]
- Lass, A. N. , Winer, E. S. , Collins, A. C. , & Rokke, P. D. (2020). The associations among distress tolerance, unhelpful coping behaviors, and symptoms of depression: A network analysis. Cognitive Therapy and Research, 44(6), 1077–1090. [Google Scholar]
- Lawson, K. M. , & Robins, R. W. (2021). Sibling constructs: What are they, why do they matter, and how should you handle them? Personality and Social Psychology Review, 25(4), 344–366. 10.1177/10888683211047101 [DOI] [PubMed] [Google Scholar]
- Lever, A. G. , & Geurts, H. M. (2016). Psychiatric co‐occurring symptoms and disorders in young, middle‐aged, and older adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(6), 1916–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardo, M. V. , Lai, M. , & Baron‐Cohen, S. (2019). Big data approaches to decomposing heterogeneity across the autism spectrum. Molecular Psychiatry, 24(10), 1435–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord, C. , Charman, T. , Havdahl, A. , Carbone, P. , Anagnostou, E. , Boyd, B. , Carr, T. , De Vries, P. J. , Dissanayake, C. , & Divan, G. (2022). The lancet commission on the future of care and clinical research in autism. The Lancet, 399(10321), 271–334. [DOI] [PubMed] [Google Scholar]
- Mantzalas, J. , Richdale, A. L. , Adikari, A. , Lowe, J. , & Dissanayake, C. (2022). What is autistic burnout? A thematic analysis of posts on two online platforms. Autism in Adulthood, 4(1), 52–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason, D. , McConachie, H. , Garland, D. , Petrou, A. , Rodgers, J. , & Parr, J. R. (2018). Predictors of quality of life for autistic adults. Autism Research, 11(8), 1138–1147. 10.1002/aur.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrossin, R. (2022). Finding the true number of females with autistic Spectrum disorder by estimating the biases in initial recognition and clinical diagnosis. Children, 9(2), 272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael, C. (2021). Is being othered a co‐occurring condition of autism? Autism in Adulthood, 3(2), 118–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millner, A. J. , Robinaugh, D. J. , & Nock, M. K. (2020). Advancing the understanding of suicide: The need for formal theory and rigorous descriptive research. Trends in Cognitive Sciences, 24(9), 704–716. 10.1016/j.tics.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milton, D. , & Sims, T. (2016). How is a sense of well‐being and belonging constructed in the accounts of autistic adults? Disability & Society, 31(4), 520–534. [Google Scholar]
- Montazeri, F. , de Bildt, A. , Dekker, V. , & Anderson, G. M. (2020). Network analysis of behaviors in the depression and autism realms: Inter‐relationships and clinical implications. Journal of Autism and Developmental Disorders, 50(5), 1580–1595. [DOI] [PubMed] [Google Scholar]
- Murray, A. L. , Booth, T. , McKenzie, K. , Kuenssberg, R. , & O'Donnell, M. (2014). Are autistic traits measured equivalently in individuals with and without an autism spectrum disorder? An invariance analysis of the autism Spectrum quotient short form. Journal of Autism and Developmental Disorders, 44(1), 55–64. [DOI] [PubMed] [Google Scholar]
- O'Connor, R. C. (2011). The integrated motivational‐volitional model of suicidal behavior. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 32(6), 295–298. 10.1027/0227-5910/a000120 [DOI] [PubMed] [Google Scholar]
- Ordóñez‐Carrasco, J. L. , Sayans‐Jiménez, P. , & Rojas‐Tejada, A. J. (2021). Ideation‐to‐action framework variables involved in the development of suicidal ideation: A network analysis. Current Psychology, 1–12. [Google Scholar]
- Osman, A. , Bagge, C. L. , Gutierrez, P. M. , Konick, L. C. , Kopper, B. A. , & Barrios, F. X. (2001). The suicidal behaviors questionnaire‐revised (SBQ‐R): Validation with clinical and nonclinical samples. Assessment, 8(4), 443–454. [DOI] [PubMed] [Google Scholar]
- Parr, J. R. , Brice, S. , Welsh, P. , Ingham, B. , Le Couteur, A. , Evans, G. , Monaco, A. , Freeston, M. , & Rodgers, J. (2020). Treating anxiety in autistic adults: study protocol for the Personalised Anxiety Treatment–Autism (PAT‐A©) pilot randomised controlled feasibility trial. Trials, 21(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson, A. , & Rose, K. (2021). A conceptual analysis of autistic masking: Understanding the narrative of stigma and the illusion of choice. Autism in Adulthood, 3(1), 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelton, M. K. , & Cassidy, S. A. (2017). Are autistic traits associated with suicidality? A test of the interpersonal‐psychological theory of suicide in a non‐clinical young adult sample. Autism Research, 10(11), 1891–1904. 10.1002/aur.1828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelton, M. K. , Crawford, H. , Robertson, A. E. , Rodgers, J. , Baron‐Cohen, S. , & Cassidy, S. (2020a). A measurement invariance analysis of the interpersonal needs questionnaire and acquired capability for suicide scale in autistic and non‐autistic adults. Autism in Adulthood, 2(3), 193–203. 10.1089/aut.2019.0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelton, M. K. , Crawford, H. , Robertson, A. E. , Rodgers, J. , Baron‐Cohen, S. , & Cassidy, S. (2020b). Understanding suicide risk in autistic adults: Comparing the interpersonal theory of suicide in autistic and non‐autistic samples. Journal of Autism and Developmental Disorders, 50(10), 3620–3637. [DOI] [PubMed] [Google Scholar]
- Penfold, R. B. , Whiteside, U. , Johnson, E. E. , Stewart, C. C. , Oliver, M. M. , Shortreed, S. M. , Beck, A. , Coleman, K. J. , Rossom, R. C. , & Lawrence, J. M. (2021). Utility of item 9 of the patient health questionnaire in the prospective identification of adolescents at risk of suicide attempt. Suicide and Life‐threatening Behavior, 51(5), 854–863. [DOI] [PubMed] [Google Scholar]
- Quinlivan, E. B. , Gaynes, B. N. , Lee, J. S. , Heine, A. D. , Shirey, K. , Edwards, M. , Modi, R. , Willig, J. , & Pence, B. W. (2017). Suicidal ideation is associated with limited engagement in HIV care. AIDS and Behavior, 21(6), 1699–1708. [DOI] [PubMed] [Google Scholar]
- Rath, D. , De Beurs, D. , Hallensleben, N. , Spangenberg, L. , Glaesmer, H. , & Forkmann, T. (2019). Modelling suicide ideation from beep to beep: Application of network analysis to ecological momentary assessment data. Internet Interventions, 18. 10.1016/j.invent.2019.100292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2021). R: A language and environment for statistical computing (version 4.0.5). R Foundation for Statistical Computing; https://www.R‐project.org/ [Google Scholar]
- Raymaker, D. M. , Teo, A. R. , Steckler, N. A. , Lentz, B. , Scharer, M. , Delos Santos, A. , Kapp, S. K. , Hunter, M. , Joyce, A. , & Nicolaidis, C. (2020). “Having all of your internal resources exhausted beyond measure and being left with no clean‐up crew”: Defining autistic burnout. Autism in Adulthood, 2, 132–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, G. , Kenny, R. , Griffiths, S. , Allison, C. , Mosse, D. , Holt, R. , O'Connor, R. C. , Cassidy, S. , & Baron‐Cohen, S. (2019). Autistic traits in adults who have attempted suicide. Molecular Autism, 10(1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh, D. J. , Millner, A. J. , & McNally, R. J. (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, J. , Farquhar, K. , Mason, D. , Brice, S. , Wigham, S. , Ingham, B. , Freeston, M. , & Parr, J. R. (2020). Development and initial evaluation of the anxiety scale for autism‐adults. Autism in Adulthood, 2(1), 24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, J. , & Ofield, A. (2018). Understanding, recognising and treating co‐occurring anxiety in autism. Current Developmental Disorders Reports, 5(1), 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, J. , Wigham, S. , McConachie, H. , Freeston, M. , Honey, E. , & Parr, J. R. (2016). Development of the anxiety scale for children with autism spectrum disorder (ASC‐ASD). Autism Research, 9(11), 1205–1215. [DOI] [PubMed] [Google Scholar]
- Roman‐Urrestarazu, A. , van Kessel, R. , Allison, C. , Matthews, F. E. , Brayne, C. , & Baron‐Cohen, S. (2021). Association of race/ethnicity and social disadvantage with autism prevalence in 7 million school children in England. JAMA Pediatrics, 175(6), e210054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, G. , Stapley, S. , Newlove‐Delgado, T. , Salmon, A. , White, R. , Warren, F. , Pearson, A. , & Ford, T. (2022). Time trends in autism diagnosis over 20 years: A UK population‐based cohort study. Journal of Child Psychology and Psychiatry, 63(6), 674–682. 10.1111/jcpp.13505 [DOI] [PubMed] [Google Scholar]
- Schönfelder, A. , Rath, D. , Forkmann, T. , Paashaus, L. , Lucht, L. , Teismann, T. , Stengler, K. , Juckel, G. , & Glaesmer, H. (2021). Child abuse and suicidality in the context of the interpersonal psychological theory of suicide: A network analysis. British Journal of Clinical Psychology, 60(4), 425–442. [DOI] [PubMed] [Google Scholar]
- Schwartzman, J. M. , Smith, J. R. , & Bettis, A. H. (2021). Safety planning for suicidality in autism: Obstacles, potential solutions, and future directions. Pediatrics, 148(6), e2021052958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva, C. , Ribeiro, J. D. , & Joiner, T. E. (2015). Mental disorders and thwarted belongingness, perceived burdensomeness, and acquired capability for suicide. Psychiatry Research, 226(1), 316–327. 10.1016/j.psychres.2015.01.008 [DOI] [PubMed] [Google Scholar]
- South, M. , Beck, J. S. , Lundwall, R. , Christensen, M. , Cutrer, E. A. , Gabrielsen, T. P. , Cox, J. C. , & Lundwall, R. A. (2020). Unrelenting depression and suicidality in women with autistic traits. Journal of Autism and Developmental Disorders, 50(10), 3606–3619. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD‐7. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Stewart, G. R. , Corbett, A. , Ballard, C. , Creese, B. , Aarsland, D. , Hampshire, A. , Charlton, R. A. , & Happé, F. (2022). Self‐harm and suicidality experiences of middle‐age and older adults with vs. without high autistic traits. Journal of Autism and Developmental Disorders, 51(6), 1049–1051. 10.1007/s10803-022-05595-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh, W. Y. , Lee, J. , Yun, J. , Sim, J. , & Yun, Y. H. (2021). A network analysis of suicidal ideation, depressive symptoms, and subjective well‐being in a community population. Journal of Psychiatric Research, 142, 263–271. [DOI] [PubMed] [Google Scholar]
- Takara, K. , & Kondo, T. (2014). Comorbid atypical autistic traits as a potential risk factor for suicide attempts among adult depressed patients: A case‐control study. Annals of General Psychiatry, 13(1), 1–8. 10.1186/s12991-014-0033-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tromans, S. , Chester, V. , Gemegah, E. , Roberts, K. , Morgan, Z. , Yao, G. L. , & Brugha, T. (2020). Autism identification across ethnic groups: A narrative review. Advances in Autism, 7, 241–255. [Google Scholar]
- Uljarević, M. , Hedley, D. , Rose‐Foley, K. , Magiati, I. , Cai, R. Y. , Dissanayake, C. , Richdale, A. , & Trollor, J. (2020). Anxiety and depression from adolescence to old age in autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(9), 3155–3165. [DOI] [PubMed] [Google Scholar]
- Upthegrove, R. , Abu‐Akel, A. , Chisholm, K. , Lin, A. , Zahid, S. , Pelton, M. , Apperly, I. , Hansen, P. C. , & Wood, S. J. (2018). Autism and psychosis: Clinical implications for depression and suicide. Schizophrenia Research, 195, 80–85. 10.1016/j.schres.2017.08.028 [DOI] [PubMed] [Google Scholar]
- van Borkulo, C. , Boschloo, L. , Borsboom, D. , Penninx, B. W. , Waldorp, L. J. , & Schoevers, R. A. (2015). Association of symptom network structure with the course of depression. JAMA Psychiatry, 72(12), 1219–1226. [DOI] [PubMed] [Google Scholar]
- van Borkulo, C. , Boschloo, L. , Kossakowski, J. J. , Tio, P. , Schoevers, R. , Borsboom, D. , & Waldorp, L. (2017). Comparing network structures on three aspects: A permutation test. 2017. http://www.researchgate.net/Publication/314750838 [DOI] [PubMed]
- van Borkulo, C. D. (2017). Symptom network models in depression research. From methodological exploration to clinical application . (Doctoral Dissertation).
- van Borkulo, C. D. , van Bork, R. , Boschloo, L. , Kossakowski, J. J. , Tio, P. , Schoevers, R. A. , Borsboom, D. , & Waldorp, L. J. (2022). Comparing network structures on three aspects: A permutation test. Psychological Methods. 10.1037/met0000476. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Van Orden, K. A. , Cukrowicz, K. C. , Witte, T. K. , & Joiner, T. E., Jr. (2012). Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the interpersonal needs questionnaire. Psychological Assessment, 24(1), 197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden, K. A. , Witte, T. K. , Cukrowicz, K. C. , Braithwaite, S. R. , Selby, E. A. , & Joiner, T. E., Jr. (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasa, R. A. , & Mazurek, M. O. (2015). An update on anxiety in youth with autism spectrum disorders. Current Opinion in Psychiatry, 28(2), 83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss, J. A. (2014). Transdiagnostic case conceptualization of emotional problems in youth with ASD: An emotion regulation approach. Clinical Psychology: Science and Practice, 21(4), 331–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2021). Suicide worldwide in 2019: global health estimates. World Health Organization. [Google Scholar]
- Zahid, S. , & Upthegrove, R. (2017). Suicidality in autistic Spectrum disorders. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 38(4), 237–246. 10.1027/0227-5910/a000458 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Figure S1
Figures S2–S7


