Abstract
Objectives
To examine the incidence and trends in primary care, allied health, geriatric, pain and palliative care service use by permanent residential aged care (PRAC) residents and the older Australian population.
Methods
Repeated cross‐sectional analyses on PRAC residents (N = 318,484) and the older (≥65 years) Australian population (N ~ 3.5 million). Outcomes were Medicare Benefits Schedule (MBS) subsidised primary care, allied health, geriatric, pain and palliative services between 2012–13 and 2016–17. GEE Poisson models estimated incidence rates and incidence rate ratios (IRR).
Results
In 2016–17, PRAC residents had a median of 13 (interquartile range [IQR] 5–19) regular general medical practitioner (GP) attendances, 3 (IQR 1–6) after‐hours attendances and 5% saw a geriatrician. Highlights of utilisation changes from 2012–13 to 2016–17 include the following: GP attendances increased by 5%/year (IRR = 1.05, 95% confidence interval [CI] 1.05–1.05) for residents compared to 1%/year (IRR = 1.01, 95%CI 1.01–1.01) for the general population. GP after‐hours attendances increased by 15%/year (IRR = 1.15, 95%CI 1.14–1.15) for residents and 9%/year (IRR = 1.08, 95%CI 1.07–1.20) for the general population. GP management plans increased by 12%/year (IRR = 1.12, 95%CI 1.11–1.12) for residents and 10%/year (IRR = 1.10, 95%CI 1.09–1.11) for the general population. Geriatrician consultations increased by 28%/year (IRR = 1.28, 95%CI 1.27–1.29) for residents compared to 14%/year (IRR = 1.14, 95%CI 1.14–1.15) in the general population.
Conclusions
The utilisation of most examined services increased in both cohorts over time. Preventive and management care, by primary care and allied health care providers, was low and likely influences the utilisation of other attendances. PRAC residents' access to pain, palliative and geriatric medicine services is low and may not address the residents' needs.
Keywords: epidemiology, health services for the aged, palliative care, primary health care, residential facilities
Policy Impact
While access to general primary health care attendance is common by older people, access to preventive care remains underutilised while the access to specialised pain, palliative and geriatric services is very low. This comprehensive national evaluation has identified service access gaps by older people and can inform current primary health and aged care reforms in Australia.
Practice Impact
This study has identified several primary, allied health and specialist services that are underutilised by older Australians, particularly those in the residential aged care setting. Our findings support calls for better access to preventive and management care, as well as pain, palliative and geriatric services for older people.
1. INTRODUCTION
Primary care practitioners are uniquely positioned to coordinate and integrate the complex health care needs of older individuals, particularly those accessing aged care services. High levels of multimorbidity and frailty, often complicated by functional and cognitive impairment, are common in the 1.5 million people accessing aged care services in Australia yearly. 1 , 2 Not surprisingly, older individuals, particularly in residential aged care settings (~240,000 yearly), are heavily reliant on primary health care professionals, with 93% visiting a general practitioner (GP) approximately every fortnight (average of 25 times/year). 3
Primary care service utilisation in Australia has increased. 4 In 2020–21, GPs were the most‐visited health professionals by the general population (>80% saw a GP). 5 Coordinated and comprehensive primary health care has the potential to improve the overall health of older people and result in lower risk of hospitalisations and other health events. 6 , 7 Health assessments, GP management plans and team care arrangements for older people receiving home care packages or medication reviews for people living in permanent residential aged care (PRAC) have been found to be associated with lower mortality rates. 8 , 9
Despite the Australian Medical Association's 2018 Position Statement calling for a national evaluation of the access and effectiveness of primary care services in the care of older people to ensure their needs are being met, no such evaluation has occurred to date. 10 In addition, given the recent Australian Government investments in aged care 11 and primary health care reforms, 12 an understanding of the access and trends in the use of primary, allied health and specialist services by Australian aged care recipients is necessary for future reform evaluation.
This study examined the incidence and trends in the utilisation of Australian Government Medicare Benefits Schedule (MBS) subsidised primary care, allied health, geriatric and pain and palliative care services between 2012–13 and 2016–17 by PRAC residents and the older (≥65 years old) Australian general population.
2. METHODS
2.1. Study design, setting and data sources
Repeated yearly cross‐sectional analyses between 2012–13 and 2016–17 were conducted using data from the Registry of Senior Australians (ROSA) National Historical Cohort for PRAC residents 1 and publicly available MBS and Australian Bureau of Statistics (ABS) data for the general older (≥65 years old) population (which includes individuals in PRAC, approximately 5% of general older people). 13 , 14 Medicare is Australia's universal health care coverage, which covers the costs associated with health care services, and the MBS is the listing of subsidised services.
Registry of Senior Australians is a de‐identified linked data platform containing datasets from the National Aged Care Data Clearinghouse (NACDC), Australian Government MBS and Pharmaceutical Benefits Scheme (PBS), and state health authorities' hospitalisation records. 1 In this study, the following datasets from NACDC were used: Residential Aged Care Episodes, National Death Index, Aged Care Funding Instrument (entry into care assessment), and the Aged Care Assessment Program (aged care eligibility assessment).
For the analyses in the general population, publicly available aggregate MBS records for individuals were accessed from the Services Australia website 13 and population estimates from the ABS website. 14
This study was approved by the University of South Australia Committee (Ref: 200489) and Australian Institute of Health and Welfare (Ref: EO2018/1/418) Human Research Ethics Committees.
2.2. Study cohorts
The study cohort included non‐Aboriginal or Torres Strait Islander individuals aged ≥65 years old from the ROSA, who did not have a Department of Veterans' Affairs (DVA) card, and who were living in a PRAC facility in between 01/07/2012 and 30/06/2017. The resulting cohort included N = 318,484 individuals. DVA cardholders were not included as these individuals utilise Medicare‐subsidised health care services differently due to their entitlements.
The comparison cohort included Australians aged ≥65 years old from publicly available MBS and ABS data between 01/07/2012 and 30/06/2017 (3.3–3.8 million people/year).
2.3. Outcomes of interest
Medicare Benefits Schedule‐subsidised primary care, allied health, geriatric medicine, pain and palliative care service utilisation within the study period were the outcomes of interest (See Table S1 for coding). Primary care services included: general and urgent GP attendances by GPs, other medical practitioners and nurse practitioners; GP health assessments; and management plans attendances. Health assessments are GP consultations to identify long‐term health needs that could benefit from a health care plan, and in our study, for the general population, were restricted to people ≥75 years due to MBS subsidy criteria. A management plan, which includes a GP management plan and team care arrangements, is a service for people with chronic conditions or complex care needs to identify such needs and the services suitable to address them and coordinates multidisciplinary care with other providers. The allied health services examined included: optometrical, comprehensive medication reviews, dentistry and the allied health services part of GP management plans. Mental health services have been examined elsewhere and were not included. 15
2.4. Covariates
For PRAC residents, covariates included sex, age at study year start, number of health conditions at PRAC entry and facilities' states/major territory. Health conditions were ascertained using the Rx‐Risk‐V, a pharmaceutical‐based comorbidity index, based on medication dispensed in the 6 months prior to study entry. 1 For the general older people, sex and age were available as covariates.
2.5. Statistical analysis
Yearly use of services was examined using descriptive statistics. For the PRAC cohort, incidence rates (IR)/1000 people, incidence rate ratios (IRRs) and 95% confidence intervals (CI) were calculated using generalised estimating equation (GEE) Poisson models. All models were estimated with exchangeable correlation structure and robust standard errors. To estimate linear trends in utilisation, IRRs were calculated using GEE Poisson models. Complete case analysis was conducted, and missing data were negligible (PRAC cohort, N = 686, 0.002%).
For the general population cohort, age and sex direct standardised IRs/1000 people were calculated. The midterm population for each year was the denominator. Time‐series Poisson models with heteroskedasticity and autocorrelation consistent standard errors estimated IRRs.
Supplementary analyses (Tables S2 and S3) examined the IR/1000 resident‐days and service use incidence proportions by PRAC residents to determine whether trends were robust using different measures. GEE Poisson models were employed. No differences were observed.
All analyses were conducted using Stata MP 16.0 and R statistical software.
3. RESULTS
In 2012–13, there were 123,340 people in the PRAC cohort, the median age was 84 (IQR 80–89), and 67% (N = 82,467) were women. In 2016–17, there were 163,054 people in the PRAC cohort, the median age was 85 (IQR 80–90), and 66% (N = 107,195) were women (Table 1).
TABLE 1.
Demographic and clinical characteristics of permanent residential aged care residents by financial year (2012/13–2016/17).
| 2012–2013 (N = 123,340) | 2013–2014 (N = 135,957) | 2014–2015 (N = 143,564) | 2015–2016 (N = 153,542) | 2016–2017 (N = 163,054) | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Sex | |||||
| Women | 82,467 (67) | 90,871 (67) | 95,598 (67) | 101,823 (66) | 107,195 (66) |
| Men | 40,873 (33) | 45,086 (33) | 47,966 (33) | 51,719 (34) | 55,859 (34) |
| Age group, years | |||||
| <65 | 147 (<1) | 166 (<1) | 150 (<1) | 164 (<1) | 163 (<1) |
| 65–74 | 13,327 (11) | 14,359 (11) | 14,827 (10) | 15,576 (10) | 16,610 (10) |
| 75–84 | 48,484 (39) | 51,467 (38) | 52,299 (36) | 54,011 (35) | 55,863 (34) |
| 85+ | 61,382 (50) | 69,965 (52) | 76,288 (53) | 83,791 (55) | 90,418 (56) |
| Age (Median, IQR), years | 84 (80–89) | 85 (80–89) | 85 (80–89) | 85 (80–90) | 85 (80–90) |
| Health Conditions, RxRisk‐V (Median, IQR) | 5 (3–7) | 5 (3–7) | 5 (3–7) | 5 (3–7) | 5 (3–7) |
| Facility state/territory | |||||
| New South Wales | 41,397 (34) | 45,831 (34) | 47,950 (33) | 50,884 (33) | 54,110 (33) |
| Victoria | 32,668 (26) | 36,392 (27) | 38,764 (27) | 41,762 (27) | 44,261 (27) |
| Queensland | 21,711 (18) | 23,521 (17) | 25,191 (18) | 26,997 (18) | 29,114 (18) |
| South Australia | 12,137 (10) | 13,315 (10) | 13,927 (10) | 14,871 (10) | 15,522 (10) |
| Western Australia | 10,398 (8) | 11,534 (8) | 12,057 (8) | 12,836 (8) | 13,554 (8) |
| Tasmania | 3411 (3) | 3608 (3) | 3799 (3) | 3997 (3) | 4106 (2) |
| Australian Capital Territory | 1385 (1) | 1511 (1) | 1641 (1) | 1945 (1) | 2127 (1) |
| Northern Territory | 233 (<1) | 245 (<1) | 235 (<1) | 250 (<1) | 260 (<1) |
Abbreviation: IQR, interquartile range.
In the PRAC cohort, 95% had a GP/medical practitioner general attendance at least once/year between 2012–13 and 2016–17 and the median number of attendances increased from 11 (IQR 5–19) to 13 (IQR 6–22; Table 2).
TABLE 2.
Crude utilisation of Medicare Benefits Schedule subsidised primary care, allied health, geriatric, pain and palliative services among permanent residential aged care residents between 2012–2013 and 2016–2017.
| Service group/financial year (total cohort) | 2012–2013 (N = 123,340) | 2013–2014 (N = 135,957) | 2014–2015 (N = 143,564) | 2015–2016 (N = 153,542) | 2016–2017 (N = 163,054) |
|---|---|---|---|---|---|
| Primary care | N (%) | N (%) | N (%) | N (%) | N (%) |
| General attendances | |||||
| GP/medical practitioner attendances | 117,643 (95) | 129,408 (95) | 137,439 (96) | 147,256 (96) | 155,932 (96) |
| Median (IQR) a | 11 (5–19) | 11 (6–20) | 12 (6–21) | 12 (6–21) | 13 (6–22) |
| Urgent GP attendance after‐hours | 38,307 (31) | 43,578 (32) | 47,406 (33) | 51,883 (34) | 51,183 (31) |
| Median (IQR) a | 1 (1–3) | 2 (1–3) | 2 (1–3) | 2 (1–3) | 1 (1–2) |
| GP/medical practitioner after‐hours attendances | 46,247 (38) | 54,320 (40) | 61,917 (43) | 71,495 (47) | 83,567 (51) |
| Median (IQR) a | 2 (1–5) | 2 (1–5) | 2 (1–6) | 2 (1–6) | 3 (1–6) |
| Nurse practitioners | 1574 (1) | 2902 (2) | 4303 (3) | 6110 (4) | 7508 (5) |
| Median (IQR) a | 3 (1–10) | 3 (1–8) | 3 (1–10) | 4 (1–12) | 4 (1–10) |
| Health assessments/management plans | |||||
| GP health assessments | 39,848 (32) | 46,888 (34) | 49,345 (34) | 53,778 (35) | 57,505 (35) |
| Median (IQR) a | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
| GP management plan attendances | 37,504 (30) | 46,840 (34) | 53,298 (37) | 62,086 (40) | 70,586 (43) |
| Median (IQR) a | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 2 (1–3) |
| GP attendance associated with PIP/non‐referred attendance associated with PIP | 975 (1) | 1208 (1) | 1419 (1) | 1469 (1) | 1586 (1) |
| Median (IQR) a | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
| Allied health services | |||||
| Optometrical services | 40,078 (32) | 45,639 (34) | 51,626 (36) | 56,257 (37) | 61,999 (38) |
| Median (IQR) a | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) |
| Comprehensive medication review | 42,764 (35) | 44,465 (33) | 37,472 (26) | 45,957 (30) | 46,334 (28) |
| Median (IQR) a | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
| Dentistry | 150 (<1) | 144 (<1) | 150 (<1) | 156 (<1) | 166 (<1) |
| Median (IQR) a | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
| Allied health service part of CDMP | 22,537 (18) | 30,747 (23) | 37,226 (26) | 43,527 (28) | 51,410 (32) |
| Median (IQR) a | 3 (2–5) | 3 (2–5) | 3 (2–5) | 3 (2–5) | 3 (2–5) |
| Podiatry | 20,026 (16) | 28,073 (21) | 34,784 (24) | 41,028 (27) | 48,535 (30) |
| Physiotherapy | 1644 (1) | 1731 (1) | 1630 (1) | 1802 (1) | 2385 (1) |
| Dietetics services | 932 (<1) | 992 (<1) | 814 (<1) | 790 (<1) | 800 (<1) |
| Exercise physiology | 461 (<1) | 585 (<1) | 422 (<1) | 489 (<1) | 362 (<1) |
| Speech pathology | 229 (<1) | 198 (<1) | 231 (<1) | 242 (<1) | 190 (<1) |
| Osteopathy | 30 (<1) | 25 (<1) | 28 (<1) | 33 (<1) | 28 (<1) |
| Occupational therapy | 29 (<1) | 52 (<1) | 66 (<1) | 63 (<1) | 65 (<1) |
| Chiropractic | 25 (<1) | 51 (<1) | 47 (<1) | 56 (<1) | 58 (<1) |
| Psychology | 12 (<1) | 64 (<1) | 75 (<1) | 49 (<1) | 30 (<1) |
| Mental Health Services b | 10 (<1) | 25 (<1) | 22 (<1) | 43 (<1) | 25 (<1) |
| Audiology | <5 | <5 | <5 | <5 | <5 |
| Geriatric, pain and palliative services | |||||
| Geriatric medicine | 2312 (2) | 3393 (2) | 4800 (3) | 6499 (4) | 8484 (5) |
| Median (IQR) a | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) |
| Pain and palliative medicine | 679 (<1) | 798 (<1) | 848 (<1) | 912 (<1) | 914 (<1) |
| Median (IQR) a | 1 (1–3) | 2 (1–3) | 1 (1–3) | 1 (1–3) | 1 (1–3) |
Abbreviations: CDMP, chronic disease management plan; GP, general practitioner; IQR, interquartile range; PIP, Practice Incentives Program.
Median and IQR among those that accessed services.
While any other mental health services were explicitly excluded from this analysis, this was included for completeness as these are accessed as part of a CDMP.
3.1. Utilisation rates and trends by PRAC residents
Between 2012–13 and 2016–17 GP and medical practitioner attendances, utilisation increased 5%/year (IRR = 1.05, 95%CI 1.05–1.05) from 12,175/1000 (95%CI 12,114–12,236) to 14,402/1000 (95%CI 14,339–14,464). GP and medical practitioner after‐hours attendances increased from 1583/1000 (95%CI 1559–1607) to 2692/1000 (95%CI 2662–2721) at a rate of 15%/year (IRR = 1.15, 95%CI 1.14–1.15). Nurse practitioner attendances increased from 83.6/1000 (95%CI 77.4–89.9) to 363/1000 (95%CI 351–375) at a rate of 42%/year (IRR = 1.42, 95%CI 1.39–1.44), and GP management plans attendances from 529/1000 (95%CI 523–535) to 812/1000 (95%CI 806–819) at a rate of 12%/year (IRR = 1.12, 95%CI 1.11–1.12). Of the allied health services examined, between 2012–13 and 2016–17, comprehensive medication review attendances decreased from 349/1000 (95%CI 347–352) to 287/1000 (95%CI 285–290) at a rate of 5%/year (IRR = 0.95, 95%CI 0.95–0.96), optometrical services attendances increased from 447/1000 (95%CI 442–451) to 502/1000 (95%CI 497–506) at a rate of 3%/year (IRR = 1.03, 95%CI 1.03–1.04), and the allied health attendances part of the GP management plan increased from 490/1000 (95%CI 482–498) to 950/1000 (95%CI 941–959) at an annual rate of 17% (IRR = 1.17, 95%CI 1.17–1.18). Between 2012–13 and 2016–17 geriatric medicine attendances increased from 25.7/1000 (95%CI 24.6–26.7) to 68.8/1000 (95%CI 67.3–70.4) and pain and palliative attendances increased from 15.7/1000 (95%CI 13.4–18.0) to 19.9/1000 (95%CI 17.8–21.9). See Figure 1 and Table 3 for IR and IRRs.
FIGURE 1.
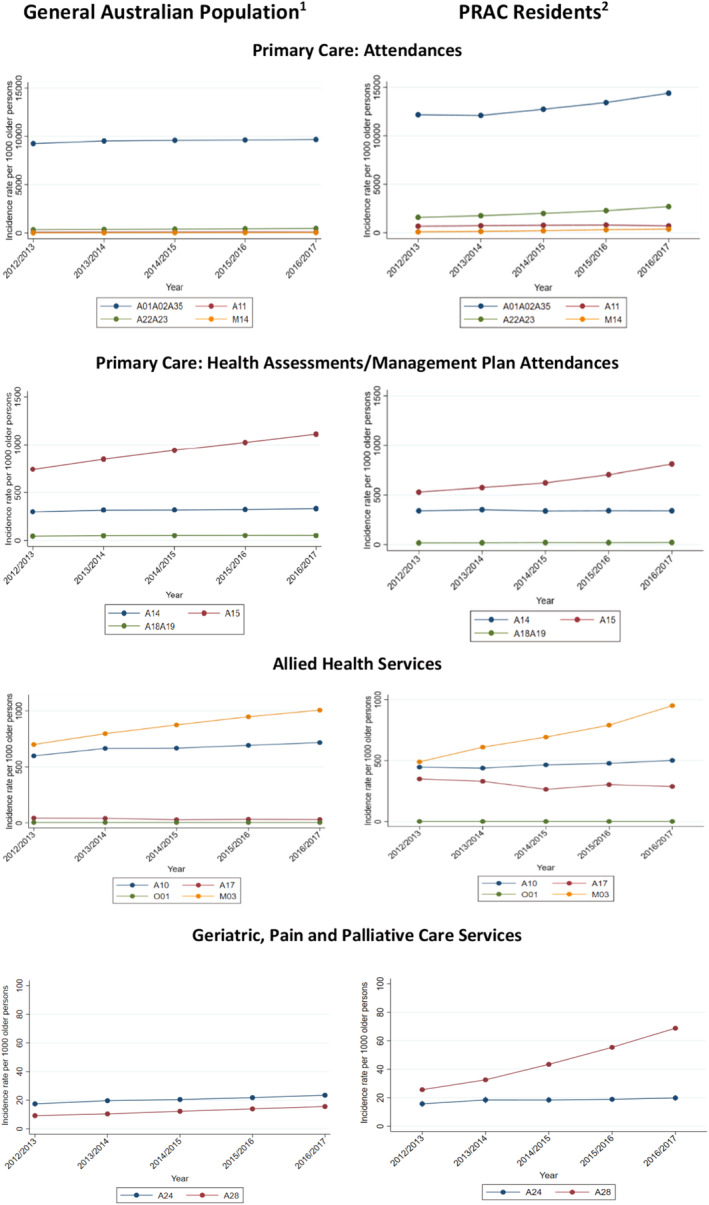
Adjusted incidence rates (per 1000 people) of Medicare Benefits Schedule subsidised primary care (general attendances, health assessments/management plans), allied health, geriatric, pain and palliative services among the general Australian population (left) and permanent residential aged care residents (right) per financial year, 2012/13–2016/17. A01, GP attendances; A02, non‐referred attendance to medical practitioner; A10, optometrical services; A11, urgent GP attendance after‐hours; A14, GP health assessments; A15, GP management plans/team care arrangements and multidisciplinary care plans attendances; A17, comprehensive medication reviews; A18, GP attendance associated with PIP; A19, non‐referred attendance associated with PIP; A22, GP after‐hours attendance; A23, non‐referred after‐hours attendance with medical practitioners; A24, pain and palliative medicine; A28, geriatric medicine; A35, medical services at residential aged care facilities; M03, allied health service part of chronic disease management plan; M14, nurse practitioners; O01, dentistry; PRAC, Permanent Residential Aged Care. 1. Standardised by sex and age. 2. Adjusted for sex, age category, number of comorbid conditions and state of residence.
TABLE 3.
Adjusted a incidence rate (per 1000 people) of Medicare Benefits Schedule subsidised primary care, allied health, geriatric, pain and palliative services among permanent residential aged care residents and incidence rate ratio, 2012–2013 to 2016–2017.
| Service group/financial year | 2012–2013 IR [95% CI] | 2013–2014 IR [95% CI] | 2014–2015 IR [95% CI] | 2015–2016 IR [95% CI] | 2016–2017 IR [95% CI] | Trend IRR [95% CI] |
|---|---|---|---|---|---|---|
| Primary care | ||||||
| General attendances | ||||||
| GP/medical practitioner attendances | 12,175 (12,114–12,236) | 12,103 (12,045–12,161) | 12,742 (12,685–12,800) | 13,432 (13,372–13,492) | 14,402 (14,339–14,464) | 1.05 (1.05–1.05) |
| Urgent GP attendance after‐hours | 670 (662–678) | 721 (713–729) | 766 (757–774) | 797 (789–805) | 698 (691–705) | 1.02 (1.01–1.02) |
| GP/medical practitioner after‐hours attendances | 1583 (1559–1607) | 1753 (1729–1777) | 1991 (1966–2016) | 2273 (2247–2299) | 2692 (2663–2722) | 1.15 (1.14–1.15) |
| Nurse practitioners | 83.6 (77.4–89.9) | 129 (122–137) | 203 (194–212) | 305 (294–317) | 363 (351–376) | 1.42 (1.39–1.44) |
| Health assessments/management plans | ||||||
| GP health assessments | 340 (338–343) | 352 (350–354) | 338 (336–341) | 342 (339–344) | 341 (338–343) | 1.00 (0.99–1.00) |
| GP management plan attendances | 529 (523–535) | 574 (569–580) | 622 (617–628) | 705 (698–711) | 812 (806–819) | 1.12 (1.11–1.12) |
| GP attendance associated with PIP/non‐referred attendance associated with PIP | 16.5 (15.2–17.8) | 17.5 (16.2–18.7) | 19.7 (18.4–20.9) | 19.2 (18.0–20.4) | 20.5 (19.3–21.7) | 1.05 (1.03–1.08) |
| Allied health services | ||||||
| Optometrical services | 447 (442–451) | 438 (434–443) | 465 (461–469) | 477 (473–482) | 502 (497–506) | 1.03 (1.03–1.04) |
| Comprehensive medication review | 349 (347–352) | 330 (328–333) | 264 (262–267) | 302 (301–305) | 288 (285–290) | 0.95 (0.95–0.96) |
| Dentistry | 1.4 (1.1–1.7) | 1.2 (1.0–1.4) | 1.2 (1.0–1.4) | 1.2 (1.0–1.4) | 1.2 (1.0–1.4) | 0.97 (0.92–1.03) |
| Allied health service part of CDMP | 490 (482–498) | 610 (602–618) | 693 (685–700) | 791 (782–799) | 950 (942–959) | 1.17 (1.17–1.18) |
| Geriatric, pain and palliative services | ||||||
| Geriatric medicine | 25.7 (24.6–26.7) | 32.6 (31.4–33.7) | 43.4 (42.2–44.7) | 55.4 (54.0–56.8) | 68.8 (67.3–70.4) | 1.28 (1.27–1.29) |
| Pain and palliative medicine | 15.7 (13.4–18.0) | 18.4 (16.1–20.8) | 18.4 (16.3–20.6) | 18.9 (17.0–20.8) | 19.9 (17.8–21.9) | 1.05 (1.01–1.09) |
| Pain | 2.6 (1.6–3.7) | 2.3 (1.5–3.2) | 2.5 (1.9–3.0) | 2.6 (2.0–3.2) | 2.6 (2.0–3.3) | 1.01 (0.88–1.16) |
| Palliative | 13.1 (11.0–15.1) | 16.0 (13.8–18.3) | 15.7 (13.7–17.8) | 16.0 (14.1–17.8) | 16.8 (14.9–18.7) | 1.05 (1.01–1.09) |
Abbreviations: CDMP, chronic disease management plan; CI, confidence interval; GP, general practitioner; IQR, interquartile range; IR, incidence rate; IRR, incidence rate ratio; PIP, Practice Incentives Program.
Adjusted for sex, age, number of health conditions and facility state.
3.2. Utilisation rates and trends by the general population
Between 2012–13 and 2016–17, there was an 1%/year (IRR = 1.01, 95%CI 1.01–1.01) increase in GP and medical practitioner attendances from 9248/1000 (95%CI 9245–9252) to 9668/1000 (95%CI 9665–9671), a 8%/year (IRR = 1.08, 95%CI 1.07–1.10) increase in after‐hours attendances from 329/1000 (95%CI 328–329) to 465/1000 people (95%CI 464–465), and a 35%/year (IRR = 1.35, 95%CI 1.23–1.47) increase in the use of nurse practitioner attendances from 12.5/1000 (95%CI 12.3–12.6) to 42.5/1000 (95%CI 42.3–42.8). The use of GP management plans' attendances increased 10%/year (IRR = 1.10, 95%CI 1.08–1.10) from 745/1000 (95%CI 744–746) to 1110/1000 (95%CI 1109–1111), and the use of health assessments increased 2%/year (IRR = 1.02, 95%CI 1.02–1.03) from 301/1000 (95%CI 300–302) to 335/1000 (95%CI 334–336). Within the allied health services, the use of services as part of the chronic disease management plans increased the most at 10%/year (IRR = 1.10, 95%CI 1.08–1.12) from 700/1000 (95%CI 699–701) to 1007/1000 (95%CI 1006–1008). An 8%/year (IRR = 1.08, 95%CI 1.07–1.09) increase in the utilisation of pain and palliative medicine attendances and 8%/year (IRR = 1.08, 95%CI 1.07–1.10) increase for geriatric medicine attendances was observed. See Figure 1 and Table 4 for IR and IRRs.
TABLE 4.
Standardised a incidence rates (per 1000 people) of Medicare Benefits Schedule subsidised primary care, allied health, geriatric, pain and palliative services among the Australian population aged ≥65 years old and incidence rate ratio, 2012–2013 to 2016–2017.
| Service group/financial year | 2012–2013 IR [95% CI] | 2013–2014 IR [95% CI] | 2014–2015 IR [95% CI] | 2015–2016 IR [95% CI] | 2016–2017 IR [95% CI] | Trend IRR [95% CI] |
|---|---|---|---|---|---|---|
| Primary care | ||||||
| General attendances | ||||||
| GP/medical practitioner attendances | 9248 (9245–9252) | 9518 (9515–9522) | 9586 (9583–9590) | 9617 (9614–9620) | 9668 (9665–9671) | 1.01 (1.01–1.01) |
| Urgent GP attendance after‐hours | 82.9 (82.6–83.2) | 90.4 (90.1–90.8) | 98.0 (97.6–98.3) | 104 (104–105) | 91.0 (90.7–91.3) | 1.00 (0.97–1.04) |
| GP/medical practitioner after‐hours attendances | 329 (328–329) | 367 (366–367) | 395 (394–395) | 433 (432–434) | 465 (464–465) | 1.08 (1.07–1.10) |
| Nurse practitioners | 12.5 (12.3–12.6) | 19.7 (19.5–19.8) | 27.4 (27.2–27.5) | 35.7 (35.5–35.9) | 42.5 (42.3–42.8) | 1.35 (1.23–1.47) |
| Health assessments/management plans | ||||||
| GP health assessments b | 301 (300–302) | 320 (318–320) | 322 (320–322) | 326 (325–326) | 335 (334–336) | 1.02 (1.02–1.03) |
| GP management plan attendances | 745 (744–746) | 850 (849–851) | 942 (941–943) | 1025 (1024–1026) | 1110 (1109–1111) | 1.10 (1.08–1.11) |
| GP attendance associated with PIP/non‐referred attendance associated with PIP | 43.7 (43.5–44.0) | 49.1 (48.9–49.4) | 50.9 (50.7–51.2) | 51.6 (51.4–51.9) | 51.5 (51.2–51.7) | 1.04 (1.02–1.06) |
| Allied health services | ||||||
| Optometrical services | 598 (597–599) | 665 (664–666) | 668 (668–669) | 692 (691–693) | 717 (716–718) | 1.04 (1.04–1.05) |
| Comprehensive medication review | 43.2 (43.0–43.4) | 40.4 (40.2–40.6) | 28.6 (28.5–28.8) | 32.1 (31.9–32.3) | 30.2 (30.0–30.4) | 0.99 (0.97–1.01) |
| Dentistry | 4.1 (4.1–4.2) | 3.9 (3.8–3.9) | 3.9 (3.8–3.9) | 3.7 (3.7–3.8) | 3.6 (3.5–3.7) | 0.98 (0.98–0.98) |
| Allied health service part of CDMP | 700 (699–701) | 797 (796–798) | 875 (874–876) | 948 (947–949) | 1007 (1006–1008) | 1.10 (1.08–1.12) |
| Geriatric, pain and palliative services | ||||||
| Geriatric medicine | 9.2 (9.1–9.3) | 10.4 (10.3–10.5) | 12.3 (12.1–12.4) | 13.9 (13.8–14.1) | 15.6 (15.5–15.7) | 1.14 (1.14–1.15) |
| Pain and palliative medicine | 19.5 (19.3–19.6) | 22.0 (21.9–22.2) | 23.2 (23.0–23.3) | 25.0 (24.8–25.1) | 27.0 (26.8–27.1) | 1.08 (1.07–1.09) |
| Pain | 6.4 (6.3–6.5) | 7.5 (7.4–7.6) | 8.6 (8.5–8.7) | 10.1 (10.0–10.2) | 11.2 (11.1–11.3) | 1.15 (1.14–1.16) |
| Palliative | 13.1 (13.0–13.2) | 14.5 (14.4–14.7) | 14.6 (14.4–14.7) | 14.9 (14.8–15.1) | 15.8 (15.7–15.9) | 1.04 (1.03–1.05) |
Abbreviations: CDMP, chronic disease management plan; CI, confidence interval; GP, general practitioner; IQR, interquartile range; IR, incidence rate; IRR, incidence rate ratio; PIP, Practice Incentives Program.
Standardised by sex and age.
Denominator restricted to population ≥75 years old, due to MBS subsidy eligibility criteria.
4. DISCUSSION
Between 2012–13 and 2016–17, the utilisation of most MBS‐subsidised primary health care, allied health, geriatric, pain and palliative care attendances increased in PRAC residents and the general older people. However, use of comprehensive medication reviews and dentistry services has declined and GP health assessments of PRAC residents have remained stable. The service use increase has been similar in PRAC and the general population, but the magnitude of service utilisation varies greatly—with PRAC residents accessing more primary care attendances, but less allied health, pain and palliative care.
The utilisation of primary care attendances in 2016–17 by PRAC residents was 1.5 times higher than the older Australian population. Even greater differences were the utilisation of urgent after‐hours services (7.7 times higher in 2016–17), general after‐hours attendances (5.8 times higher) and nurse practitioner attendances (8.5 times higher) by those in PRAC compared to the general population. Given the high burden of health conditions, frailty and care needs of PRAC residents, more general primary care attendances by PRAC residents are expected and have already been reported. 1 , 3 The increase in after‐hours services use in PRAC settings has been previously reported 1 and investigated by an MBS Task Force, 16 which concluded that this was likely due to a ‘corporate model of advertising on the basis of convenience’ and not individuals' needs. While after‐hours care may facilitate GP access at potentially critical times and reduce reliance on hospital attendance, the use of urgent after‐hours services could be the result of, or lead to, unmet care needs. For example, more after‐hours attendances have been reported to be associated with higher antibiotic use. 17 The increasing trend of general health attendances by PRAC residents and reliance on after‐hours care identifies a need for more efficient care delivery models to address residents' health care demands.
The utilisation of health assessments by PRAC residents (in 2016–17, 341/1000) and the general population (335/1000) was low but comparable. This underutilisation of health assessments has been reported in the general population (1999–2009) 18 and in PRAC (2006–2015). 1 Given health assessments' role in the identification of conditions in need of treatment, optimisation of care plans and therapeutic management, this long‐standing suboptimal utilisation indicates access and structural barriers to and with their use. 6 , 8 GP management plans, while increasing in use by both PRAC residents and general population, concordant with a previous study, 19 are also underutilised. Management plans aim to reduce ad hoc GP attendances by helping plan, manage and coordinate individuals' conditions and facilitate access to referral‐only allied health services. Given the health care complexities of PRAC residents, 1 which have translated into a high and increasing use of other health attendances, improving accessibility and utility of health assessments and GP management plans could improve PRAC residents' care.
Medicare‐subsidised allied health services examined were less used by PRAC residents than the general population, except for comprehensive medication reviews, which were used almost 10 times more in PRAC (e.g. 30.2/1000 general population compared to 287/1000 PRAC, 2016–17). While medication reviews' utilisation was higher in PRAC residents, their rates have decreased due to funding and eligibility criteria changes. 20 We have also found that PRAC residents and the general population have low but increasing use of eye health services (3%–4%/year) and the allied health services part of GP management plans (10%–17%/year). 21 However, 90% of services obtained under GP management plans' referrals are podiatry, which agrees with previous figures for older Australians. 22 It should be noted that while 70% of people aged ≥80 years old access Medicare‐subsidised services, most allied health services accessed are subsidised by private health insurers. 4 However, only 43% of Australian women and 47% of men aged ≥85 year old have health insurance, which does not always include allied health coverage. 23 Furthermore, not all PRAC facilities offer allied health services, with a survey of 331 facilities reporting that only 29% have these services and most focus on physiotherapy and lifestyle officers. 24 Therefore, the observed limited access to allied health care is not just due to the low use of Medicare‐subsidised services but is pervasive in PRAC settings. The barriers to allied health care access (e.g. funding models, limited number of subsidised services and workforce) are well‐recognised, and the impacts were highlighted in the 2021 Royal Commission into Aged Care Quality and Safety's investigations. 25 As a result of these investigations, recommendations were made to improve access to allied health in PRAC facilities (recommendation #38), establish a funding mechanism for dental care (recommendation #60) and amend the Quality of Care Principles to ensure that allied health, mental health, oral and dental care are included within the role and responsibilities of providers (recommendation #69). 25 Several Australian Government aged care reforms underway may affect allied health services in PRAC, including implementation of a new funding model; new care‐minutes reporting requirements that include allied health; and development of an allied health model of care for PRAC and sector workforce planning. 26 Other reforms that affect allied health services include $345.7 million investment in on‐site pharmacists; and COVID‐19 temporary allied health services subsidies. 27 Of note, no government actions to improve dental and oral health care for PRAC residents to date (2023) have been announced, a neglected area in PRAC settings. 25
Access to geriatric medicine and pain and palliative Medicare‐subsidised attendances by PRAC residents and the general Australian population are low but have increased over time. Geriatric medicine attendances, while low in use despite a high prevalence of dementia and frailty in PRAC, 1 is 2.5 times higher in PRAC residents than in the general population. The increase in individuals' need, the increasing number of geriatricians nationally and recognition of the significant contributions that geriatric medicine can offer, have likely contributed to this observation. 28 , 29 Palliative care attendances alone were similar between those in PRAC and the general population while pain attendances by those in PRAC were lower. In addition to MBS‐subsidised palliative care attendances, PRAC residents can also access palliative care services from aged care providers or through in‐patient services, but very few do, despite this cohort's higher mortality rate. This low utilisation of palliative care combined with prior reports of low access to other palliative services suggests unmet needs for these individuals. 30 Similarly, this cohort has a high pain prevalence and opioid use but low access to pain specialists, indicating potential pain management needs. 1 , 30
This study has limitations. Our analyses examined government‐subsidised health services, so the utilisation of certain services is underestimated. Allied health care services, which could be accessed privately or through aged care, are likely to be the most affected. We have minimised the impact of concessional entitlements on the utilisation of services (e.g. DVA) by excluding them from our cohort. We also underestimated medication reviews and geriatric medicine services, as only MBS‐subsidised services were included. We are unable to discern whether the after‐hours attendances were provided by individuals' usual GP or by others, which affects an individual's continuity of care and can have implications to their care. 17 We examined the types of attendances that are most often accessed by older people and recognised that other subsidised attendances were not included, including telehealth consultations, which were not commonly used during the study period. Other limitations are the inclusion of the PRAC residents and Aboriginal individuals in the general population analyses. Datasets used in this study were de‐identified and the analyses conducted independently; therefore, it was not possible to remove the individuals in PRAC from the general population analyses. While the proportion of PRAC residents in the general population cohort is approximately 5% (e.g. in 2016–17 163,054 out of 3.5 million people) the impact is likely a slight attenuation of the general population utilisation estimates. Similarly, the Aboriginal population could not be disaggregated from the aggregate Medicare utilisation; however, since they represent <1% of the population older than 65 years, this probably has minimal impact on our estimates. 14 We also cannot make inferences about appropriateness of care in this study and did not examine other contributors to service utilisation, including hospitalisations and other aged care service use.
Study strengths include the evaluation of nationally representative cohorts, such as the entire older Australian population and most PRAC residents. We have examined comprehensively the utilisation of primary care attendances, allied health care services, pain and palliative and geriatric services access over 5 years. Our side‐by‐side highlights common trends and major differences and provides baseline estimates for future care access evaluation when national reforms and activities to improve care integration for PRAC residents are implemented.
5. CONCLUSIONS
Access to health care services to maintain and manage older people's complex health profiles is required in PRAC and is a significant contributor to the quality and safety of care individuals' experience. While a moderate increase in the use of GP management plans and geriatric medicine services by older people has been observed in PRAC between 2012–13 and 2016–17, their use was still only accessed by seven in 20 and one out of 20 residents, respectively. The lack of active preventive and management care, by primary care providers and allied health care providers, likely influences the increasing utilisation of after‐hours services in PRAC, which is more much more common in this setting than in the general population. Similarly, access to Medicare‐subsidised pain, palliative care and geriatric medicine services by PRAC residents is still low and likely does not address the residents' needs, highlighting areas in significant need of improvement.
FUNDING INFORMATION
This work is supported by funding from a MRFF Primary Health Care Research Grant (MRFF1200056). Prof Maria Inacio is supported by The Hospital Research Foundation Mid‐Career Fellowship (MCF‐27‐2019) and National Health and Medical Research Council (NHMRC) Investigator Grant (GNT119378). JKS is supported by an NHMRC Early Career Fellowship (GNT1156439).
CONFLICT OF INTEREST STATEMENT
Dr Janet K Sluggett is a pharmacist who is accredited to perform comprehensive medicine review. All other authors have no conflict of interest to declare.
Supporting information
Table S1–S3
ACKNOWLEDGEMENTS
We would like to acknowledge the Registry of Senior Australians’ (ROSA) Steering Committee and the ROSA South Australian Health and Medical Research Institute (SAHMRI) Research Team for ensuring the success of the ROSA and support with this study. We also acknowledge the South Australian Government Department for Innovation and Skills (2017–2021) who provided us with support to establish ROSA, the Australian Government Medical Research Future Fund (2021–2024, PHRDI000009), and ROSA collaborating partners (SAHMRI, ECH Inc, Silver Chain, Life Care) for its ongoing support, and the Australian Institute of Health and Welfare for the linkage and construction of input data. Open access publishing facilitated by University of South Australia, as part of the Wiley ‐ University of South Australia agreement via the Council of Australian University Librarians.
Inacio MC, Collier L, Air T, et al. Primary, allied health, geriatric, pain and palliative healthcare service utilisation by aged care residents, 2012–2017. Australas J Ageing. 2023;42:564‐576. doi: 10.1111/ajag.13199
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from Australian Institute of Health and Welfare. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the author(s) with the permission of Australian Institute of Health and Welfare.
REFERENCES
- 1. Inacio MC, Lang C, Bray SCE, et al. Health status and healthcare trends of individuals accessing Australian aged care programmes over a decade: the registry of senior Australians historical cohort. Intern Med J. 2021;51(5):712‐724. doi: 10.1111/imj.14871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Australian Government. Department of Health . 2020–21 Report on the Operation of the Aged Care Act 1997. Accessed March 23, 2023. https://www.gen‐agedcaredata.gov.au/www_aihwgen/media/ROACA/21520‐Health_Report‐on‐the‐Operation‐of‐the‐Aged‐Care‐Act‐2020%e2%80%932021.pdf
- 3. Australian Government . Australian Institute of Health and Welfare. Interfaces between the aged care and health systems in Australia—GP use by people living in permanent residential aged care 2012–13 to 2016–17. Accessed March 23, 2023. https://www.aihw.gov.au/reports/aged‐care/gp‐use‐by‐people‐in‐permanent‐residential‐care/contents/summary
- 4. Australian Institute of Health and Welfare . Medicare‐subsidised GP, allied health and specialist health care across local areas: 2013–14 to 2018–19. Accessed March 23, 2023. https://www.aihw.gov.au/reports/primary‐health‐care/medicare‐subsidised‐health‐local‐areas‐2019/contents/introduction
- 5. Australian Bureau of Statistics . Patient experiences in Australia: summary of findings. Accessed March 23, 2023. https://www.abs.gov.au/statistics/health/health‐services/patient‐experiences‐australia‐summary‐findings/latest‐release
- 6. Dolja‐Gore X, Byles JE, Tavener MA, et al. Estimating the effect of health assessments on mortality, physical functioning and health care utilisation for women aged 75 years and older. PLoS One. 2021;16(4):e0249207. doi: 10.1371/journal.pone.0249207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dyer SM, Suen J, Williams H, et al. Impact of relational continuity of primary care in aged care: a systematic review. BMC Geriatr. 2022;22(1):579. doi: 10.1186/s12877-022-03131-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Visvanathan R, Amare AT, Wesselingh S, Inacio MC. General practitioner conduct of clinical services representing comprehensive geriatric assessment is associated with lower risk of mortality in older Australians receiving home care packages. Age Ageing. 2021;50(4):1243‐1251. doi: 10.1093/ageing/afaa272 [DOI] [PubMed] [Google Scholar]
- 9. Sluggett JK, Caughey GE, Air T, et al. Provision of a comprehensive medicines review is associated with lower mortality risk for residents of aged care facilities: a retrospective cohort study. Age Ageing. 2022;51(7):afac149. doi: 10.1093/ageing/afac149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Australian Medical Association . Position Statement: Health and care of older people – 2018. Accessed March 23, 2023. https://www.ama.com.au/position‐statement/health‐and‐care‐older‐people‐%E2%80%93‐2018
- 11. Australian Government Department of Health . Five pillars over 5 years. Accessed December 14, 2022. https://www.health.gov.au/resources/publications/five‐pillars‐over‐5‐years
- 12. Australian Government Department of Health . Primary Health Reform Steering Group established. Accessed March 23, 2023. https://www.health.gov.au/ministers/the‐hon‐greg‐hunt‐mp/media/primary‐health‐reform‐steering‐group‐established
- 13. Australian Government Services Australia . Medicare item reports. Accessed March 23, 2023. http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp
- 14. Australian Bureau of Statistics . National, state and territory population. Accessed March 23, 2023. https://www.abs.gov.au/statistics/people/population/national‐state‐and‐territory‐population/latest‐release#data‐downloads‐data‐cubes
- 15. Cations M, Collier LR, Caughey G, et al. Government‐subsidised mental health services are underused in Australian residential aged care facilities. Aust Health Rev. 2022;46(4):432‐441. doi: 10.1071/AH22049 [DOI] [PubMed] [Google Scholar]
- 16. Australian Government Department of Health . Questions and answers – new MBS urgent after‐hours Items starting on 1 March 2018. Accessed March 23, 2023. http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/news‐2018‐03‐01‐new‐urgent‐afterhours‐items
- 17. Sluggett JK, Moldovan M, Lang C, et al. Contribution of facility level factors to variation in antibiotic use in long‐term care facilities: a national cohort study. J Antimicrob Chemother. 2021;76(5):1339‐1348. doi: 10.1093/jac/dkab007 [DOI] [PubMed] [Google Scholar]
- 18. Hamirudin AH, Ghosh A, Charlton K, Bonney A, Walton K. Trends in uptake of the 75+ health assessment in Australia: a decade of evaluation. Aust J Prim Health. 2015;21(4):423‐428. doi: 10.1071/PY14074 [DOI] [PubMed] [Google Scholar]
- 19. Welberry H, Barr ML, Comino EJ, Harris‐Roxas BF, Harris E, Harris MF. Increasing use of general practice management and team care arrangements over time in New South Wales, Australia. Aust J Prim Health. 2019;25(2):168‐175. doi: 10.1071/PY18113 [DOI] [PubMed] [Google Scholar]
- 20. Sluggett JK, Collier LR, Bartholomaeus JD, Inacio MC, Wesselingh SL, Caughey GE. National trends and policy impacts on provision of home medicines reviews and residential medication management reviews in older Australians, 2009–2019. Int J Environ Res Public Health. 2021;18(18):9898. doi: 10.3390/ijerph18189898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Australian Government Department of Health . Chronic disease management individual allied health services under Medicare. Accessed November 9, 2022. https://www1.health.gov.au/internet/main/publishing.nsf/Content/74EB0CF19603E7B7CA257BF0001FA204/$File/Fact%20Sheet%20‐%20CDM%20‐%20Individual%20Allied%20Health%20Services%20‐%20Patient%20Info.pdf
- 22. Barr ML, Welberry H, Comino EJ, et al. Understanding the use and impact of allied health services for people with chronic health conditions in central and eastern Sydney, Australia: a five‐year longitudinal analysis. Prim Health Care Res Dev. 2019;20:e141. doi: 10.1017/S146342361900077X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Australian Government . Australian institute of health and welfare. Australia's health snapshots 2020. Accessed June 30, 2022. https://www.aihw.gov.au/getmedia/128856d0‐19a0‐4841‐b5ce‐f708fcd62c8c/aihw‐aus‐234‐Australias‐health‐snapshots‐2020.pdf
- 24. StewartBrown . Allied health deep dive survey. 2020. Accessed March 23, 2023. https://www.stewartbrown.com.au/images/documents/StewartBrown_Allied_Health_Deep_Dive_Survey__Feb_2021.pdf
- 25. Royal Commission into Aged Care Quality and Safety . Final report: care, dignity and respect. Accessed March 23, 2023. https://agedcare.royalcommission.gov.au/sites/default/files/2021‐03/final‐report‐volume‐1_0.pdf
- 26. Australian Government Department of Health . How allied health care is supported under AN‐ACC. Accessed March 23, 2023. https://www.health.gov.au/sites/default/files/documents/2022/06/how‐allied‐health‐care‐is‐supported‐under‐an‐acc‐what‐impact‐will‐an‐acc‐have‐on‐allied‐health‐services.pdf
- 27. Australian Government. Department of Health . COVID‐19 temporary MBS allied health services for residents of aged care facilities. Accessed March 23, 2023. http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Factsheet‐RACK‐AH
- 28. Flicker L. Advances in research, education and practice in geriatric medicine, 1982–2012. Australas J Ageing. 2013;32(Suppl 2):35‐39. doi: 10.1111/ajag.12074 [DOI] [PubMed] [Google Scholar]
- 29. Ellis G, Gardner M, Tsiachristas A, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:CD006211. doi: 10.1002/14651858.CD006211.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Australian Government. Australian institute of health and welfare . Palliative care services in Australia. Accessed March 23, 2023. https://www.aihw.gov.au/reports/palliative‐care‐services/palliative‐care‐services‐in‐australia/contents/medicare‐subsidised‐palliative‐medicine‐services
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1–S3
Data Availability Statement
The data that support the findings of this study are available from Australian Institute of Health and Welfare. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the author(s) with the permission of Australian Institute of Health and Welfare.


