Abstract
Aim
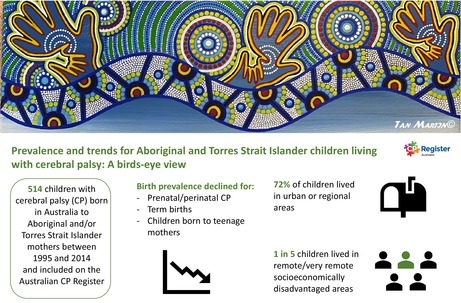
To provide a birds‐eye view of the trends of cerebral palsy (CP) for Australian Aboriginal and Torres Strait Islander children and young adults.
Method
Data were obtained for this population‐based observational study from the Australian Cerebral Palsy Register (ACPR), birth years 1995 to 2014. The Indigenous status of children was classified by maternal Aboriginal and Torres Strait Islander or non‐Indigenous status. Descriptive statistics were calculated for socio‐demographic and clinical characteristics. Prenatal/perinatal and post‐neonatal birth prevalence was calculated per 1000 live births and per 10 000 live births respectively, and Poisson regression used to assess trends.
Results
Data from the ACPR were available for 514 Aboriginal and Torres Strait Islander individuals with CP. Most children could walk independently (56%) and lived in urban or regional areas (72%). One in five children lived in socioeconomically disadvantaged remote/very remote areas. The birth prevalence of prenatal/perinatal CP declined after the mid‐2000s from a high of 4.8 (95% confidence interval 3.2–7.0) to 1.9 per 1000 live births (95% confidence interval 1.1–3.2) (2013–2014), with marked declines observed for term births and teenage mothers.
Interpretation
The birth prevalence of CP in Aboriginal and Torres Strait Islander children in Australia declined between the mid‐2000s and 2013 to 2014. This birds‐eye view provides key stakeholders with new knowledge to advocate for sustainable funding for accessible, culturally safe, antenatal and CP services.
What this paper adds
Birth prevalence of cerebral palsy (CP) is beginning to decline for Aboriginal and Torres Strait Islanders.
Recent CP birth prevalence for Aboriginal and Torres Strait Islanders is 1.9 per 1000 live births.
Most children with CP live in more populated areas rather than remote or very remote areas.
One in five Aboriginal and Torres Strait Islander children with CP live in socioeconomically disadvantaged remote areas.
What this paper adds
Birth prevalence of cerebral palsy (CP) is beginning to decline for Aboriginal and Torres Strait Islanders.
Recent CP birth prevalence for Aboriginal and Torres Strait Islanders is 1.9 per 1000 live births.
Most children with CP live in more populated areas rather than remote or very remote areas.
One in five Aboriginal and Torres Strait Islander children with CP live in socioeconomically disadvantaged remote areas.
This paper provides an overview of the prevalence and trends for Aboriginal and Torres Strait Islander children living with cerebral palsy (1995–2014).
This original article is commented on by Lynch on pages 1417–1418 of this issue.
There is a letter to the editor on this original article by Rowse on page 1530.
Abbreviations
- ACPR
Australian Cerebral Palsy Register
- ARIA
Accessibility Remoteness Index of Australia
- SEIFA
Socio‐Economic Indexes for Areas

Artwork: A Bird's‐Eye View of Aboriginal inclusion and knowledge sharing within the Australian Cerebral Palsy Register (ACPR) by first author Tanya Martin.
The ACPR Group would like to acknowledge the traditional owners of all the lands on which this work has been conducted. We pay our respects to the children, their families, and their elders past and present – for they are the ones that hold the memories, the stories, the traditions, and the cultures of Aboriginal and Torres Strait Islander people across the lands, that make up this continent.
Aboriginal and Torres Strait Islander peoples are a proud, linguistically, and culturally diverse population that represents 3.2% of the total Australian population. 1 The Aboriginal and Torres Strait Islander population is growing and predicted to grow by 136% by 2050. 2 One in five Aboriginal and Torres Strait Islander people live in remote and very remote settings, where they constitute up to 90% of residents. 3
However, because of the continuing legacy of colonization, dispossession of land, disruption, and censoring of language and cultural practices (a violation of international human rights [Mabo Decision 1992]), 4 Aboriginal and Torres Strait Islander people experience socioeconomic, criminal justice, health, and disability inequities compared with non‐Indigenous Australians. 2 , 5 , 6 For many generations, a deficit‐based research, service, and policy discourse has dominated the health and well‐being narratives of Aboriginal and Torres Strait Islander people. Inequities caused by policy based on these narratives have been further compounded by a shifting of blame for these inequities to Aboriginal and Torres Strait Islanders themselves. 7 , 8
Despite these injustices, 9 Aboriginal and Torres Strait Islander peoples remain resilient. 10 Contemporary epidemiological research must reflect this resilience and address these inequities. When led by Aboriginal and Torres Strait Islander people, it has the potential to simultaneously harness epidemiology's persuasive power in public health and policy to promote equity, while also critically challenging the legacy of colonialist misrepresentation of Indigenous health in population statistics and qualitative discourse. 11
There is a lack of epidemiological research into cerebral palsy (CP) for Australian Aboriginal and Torres Strait Islander children. CP is a lifelong condition and people with lived experience describe varying degrees of difficulty with muscle coordination, muscle control, muscle tone, reflexes, balance, and posture. In Australia, CP is seen across all socioeconomic groups; however, socioeconomic disadvantage is associated with more severe impairment and subsequently greater health‐service needs. 12 In the only other Australian epidemiological study, Blair et al. reported that Aboriginal and Torres Strait Islander children had a higher birth prevalence of CP (particularly post‐neonatally acquired) than non‐Indigenous children, which was based on birth years 1996 to 2005. 13 However, the research did not include an examination of socioeconomic status and area of residence in the context of service accessibility and did not report birth prevalence trends. In the intervening years, there has been a significant decline in the birth prevalence of CP in Australia. 14 , 15 It is yet to be determined whether CP birth prevalence has declined for Aboriginal and Torres Strait Islander children.
The purpose of this study was twofold: (1) to provide estimates of socio‐demographic and clinical profiles of Aboriginal and Torres Strait Islander children with CP; (2) to provide prevalence estimates and assess trends in birth prevalence of CP (term and preterm, and in teenage mothers) for Aboriginal and Torres Strait Islander peoples (birth years 1995–2014).
METHOD
In conducting this research, which was led by Aboriginal researchers, an Indigenous lens and a strengths‐based perspective was used. 7 , 16 The Community, Aboriginal and Torres Strait Islander Reference Group was developed to facilitate Aboriginal and Torres Strait Islander and non‐Indigenous consumer involvement in the use and reporting of Australian Cerebral Palsy Register (ACPR) data in research. Development of the study and interpretation of the findings were generated from a reciprocal balance between Aboriginal and Torres Strait Islander peoples', clinicians'/researchers', and people with CP and their families' experience and knowledge through yarning. Yarning is an important cultural form of communication for Aboriginal and Torres Strait Islander people; it refers to the sharing of information and stories, and it can set expectations and determine accountability. 17
Study cohort
In this population‐based observational study we used numerator data from the ACPR, which holds non‐identifiable data that are collected every 2 years from each of the eight Australian states and territories. These registers collect an agreed minimum data set for children with CP born in their jurisdiction. 18 Data are confirmed when the child is around 5 years of age either from their medical record (on the basis of clinical assessment) or from a clinical assessment undertaken by staff specifically for the CP register. 19 If a child passes away before their fifth birthday, and their CP diagnosis had been confirmed, their data are still included.
For all descriptive analyses, data from all state and territory CP registers were included (birth years 1995–2014). For the analysis of birth prevalence, numerator data for birth years 1995 to 2014 were included from three long‐standing registers (South Australia, Victoria, and Western Australia) where the researchers were confident that all or very nearly all children with CP were identified across the whole period at the time of data extraction (July 2020). 18
Study variables
Birth years were aggregated and reported by 10 2‐year epochs. Maternal Aboriginal and Torres Strait Islander status was described as Aboriginal and/or Torres Strait Islander (Aboriginal but not Torres Strait Islander, Torres Strait Islander but not Aboriginal, Aboriginal and Torres Strait Islander) and non‐Indigenous. 20
Neighbourhood socioeconomic status was estimated by taking birth postcode or, if unavailable, postcode at age 5 years and linking this to the related Socio‐Economic Indexes for Areas (SEIFA) Indices of Relative Socioeconomic Advantage and Disadvantage deciles published by the Australian Bureau of Statistics. 21 These SEIFA Indices deciles were then combined into quintiles, with quintile 1 being the most disadvantaged and quintile 5 being the most advantaged.
Residential postcode at birth (or at age 5 years if residential postcode at birth were missing) was used to determine accessibility and remoteness by applying the Accessibility Remoteness Index of Australia+2016 (ARIA+ 2016). ARIA+ 2016 data were sourced from the Hugo Centre for Population and Housing, University of Adelaide. 22 ARIA+ 2016 data were categorized by major city, inner regional, outer regional, remote, and very remote.
Maternal age was reported as younger than 20 years, 20 to 34 years, or 35 years or more. Sex was reported as male or female; gestational age as less than 28 weeks, 28 to 31 weeks, 32 to 36 weeks, and 37 weeks or more; and birthweight as less than 1000 g, 1000 g to 1499 g, 1500 g to 1999 g, 2000 g to 2499 g, 2500 g to 2999 g, or 3000 g or more. Small for gestational age was defined as birthweight below the 10th centile for gestational age, and sex using Australian birthweight centiles for singleton births. 23 Timing of brain injury or insult was described as prenatal/perinatal (occurring during pregnancy or up to 28 days after birth) or post‐neonatal (brain injury acquired more than 28 days after birth and before 2 years of age). The following variables were confirmed at 5 years of age by combined specialist assessments: predominant motor type (spastic unilateral [monoplegia, hemiplegia], spastic bilateral [diplegia, triplegia, quadriplegia], ataxic, dyskinetic, hypotonic), Gross Motor Function Classification System (levels I–II [independent mobility], levels III–V [mobility device required]), 24 intellectual impairment (no/borderline/mild, moderate–severe), speech (no/some impairment, non‐verbal), epilepsy (no active epilepsy, epilepsy), hearing (no/some impairment, deaf), and vision (no/mild impairment, functionally blind).
Denominator data (live births born 1995–2014) were sourced from the National Perinatal Data Collection, Australian Institute of Health and Welfare. 25
Statistical analyses
Descriptive statistics (counts and percentages) were calculated for demographic and clinical characteristics of CP. If a state or territory had over 20% missing data for a variable, then that state or territory's data were excluded from the analysis for that variable. Prenatal/perinatal and post‐neonatal CP birth prevalences were calculated per 1000 live births and per 10 000 live births respectively, both with 95% confidence intervals. The numerators were the count of eligible children (Aboriginal and/or Torres Strait Islander or Non‐Aboriginal and/or Torres Strait Islander) with either prenatal/perinatal or post‐neonatally acquired CP (as described above) born in states with CP registers with total population ascertainment (South Australia, Victoria, and Western Australia), for each epoch and included in these registers. The denominator was a count of all live births born in these states during each 2‐year epoch. Birth prevalence for each epoch was calculated as the ratio of the numerator to denominator expressed as the number of cases per 1000 live births for prenatal/perinatal CP and the number of cases per 10 000 live births for post‐neonatally acquired CP. Two‐year moving averages were used for graphical representation of the data. Poisson regression was used to assess temporal trends, with the count as the outcome variable, including an offset term for the denominator to account for differences in denominators across state registers. Birth year was used as the predictor variable to assess whether there was a significant trend over time.
Ethics
Ethical oversite for the ACPR (2020/463) is held by The University of Sydney Human Research Ethics Committee and the Aboriginal Health and Medical Research Council (1388/18). Additional specific research approvals were received from the Aboriginal Health and Medical Research Council (1623/20) and individual State and Territories – Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health Research (2020–3612), Aboriginal Health Research Ethics Committee (South Australia) (04–20‐872), Western Australian Aboriginal Health Ethics Committee (975), and Women's and Children's Health Network Research and Ethics Committee (South Australia) (2020/GEM02413).
RESULTS
In the birth years 1995 to 2014 there were 514 Aboriginal and Torres Strait Islander children and young adults with CP included on the ACPR. Of these, 11% had CP resulting from a post‐neonatal injury. More than half of all children were male (55%) and two‐thirds of those with post‐neonatal CP were male. Ninety‐one per cent of children were born a singleton, with 9% a twin or triplet. Half of the children born a singleton were within the typical birthweight range, with 85% born at an appropriate weight for gestational age.
One‐third of all children had spastic unilateral CP and one‐half had spastic bilateral CP as their predominant motor type. Children with post‐neonatal CP only rarely had a non‐spastic predominant motor type. Most children and young people could walk without requiring aids (GMFCS levels I and II) (56%), had either no intellectual impairment or a mild intellectual impairment (72%), could talk (69%), did not have active epilepsy (59%), and had functional hearing (96%) and vision (91%) (Table 1).
TABLE 1.
Aboriginal and/or Torres Strait Islander children with cerebral palsy, birth years 1995–2014.
| All states and territories | Prenatal/perinatal, n (%) a | Post‐neonatal, n (%) a | All cerebral palsy, n (%) a |
|---|---|---|---|
| Total | 457 | 57 | 514 |
| Sex | |||
| Female | 208 (45.5) | 20 (35.1) | 228 (44.4) |
| Male | 249 (54.5) | 37 (64.9) | 286 (55.6) |
| Unknown | — | — | — |
| Plurality | |||
| Singletons | 379 (90.7) | 49 (90.7) | 428 (90.7) |
| Twins/triplets | 39 (9.3) | 5 (9.3) | 44 (9.3) |
| Unknown | 39 (8.5) | 3 (5.2) | 42 (8.2) |
| Gestational age | |||
| <28 weeks | 57 (13.5) | — | 57 (12.1) |
| 28–31 weeks | 61 (14.4) | b | 63 (13.3) |
| 32–36 weeks | 77 (18.2) | 10 (20.4) | 87 (18.4) |
| ≥37 weeks | 228 (53.9) | 37 (75.5) | 265 (56.1) |
| Unknown | 34 (7.4) | 8 (14.0) | 42 (8.2) |
| Birthweight (g) b | |||
| <1000 | 42 (14.0) | — | 42 (12.1) |
| 1000–1499 | 31 (10.3) | b | 32 (9.2) |
| 1500–1999 | 28 (9.3) | b | 30 (8.7) |
| 2000–2499 | 44 (14.6) | 7 (15.6) | 51 (14.7) |
| 2500–2999 | 54 (17.9) | 13 (28.9) | 67 (19.4) |
| ≥3000 c | 102 (33.9) | 22 (48.9) | 124 (35.8) |
| Unknown | 21 (6.5) | 5 (10.0) | 26 (7.0) |
| Small for gestational age (singletons only) b | |||
| <28 weeks | 6 (18.2) | — | 6 (18.2) |
| 28–31 weeks | 4 (11.1) | — | 4 (10.8) |
| 32–36 weeks | 7 (15.6) | — | 7 (13.7) |
| ≥37 c weeks | 46 (30.7) | 7 (15.9) | 53 (28.8) |
| Unknown | 11 (4.2) | 1 (2.2) | 12 (3.8) |
| Predominant motor type | |||
| Spastic unilateral | 141 (32.8) | 26 (49.1) | 167 (34.6) |
| Spastic bilateral | 227 (52.7) | 24 (45.4) | 251 (52.0) |
| Diplegia | 118 (27.4) | 7 (13.2) | 125 (25.9) |
| Tri/quadriplegia | 109 (25.3) | 17 (32.2) | 126 (26.1) |
| Ataxic | 14 (3.3) | — | 14 (2.9) |
| Dyskinetic | 31 (7.2) | 3 (5.7) | 34 (7.0) |
| Hypotonic | 17 (4.0) | — | 17 (3.5) |
| Unknown | 27 (6.0) | 4 (7.0) | 31 (6.0) |
| Gross Motor Function Classification System level c | |||
| I–II | 238 (56.9) | 30 (54.5) | 267 (56.7) |
| III–V | 180 (43.1) | 25 (45.4) | 205 (43.4) |
| Unknown | 27 (6.1) | 2 (3.6) | 29 (5.8) |
| Intellectual impairment | |||
| No, borderline, or mild impairment | 304 (72.7) | 32 (62.7) | 336 (71.6) |
| Moderate–severe impairment | 114 (27.3) | 19 (37.3) | 133 (28.4) |
| Unknown | 39 (8.5) | 6 (10.5) | 45 (8.8) |
| Speech c | |||
| No or mild impairment | 281 (69.6) | 33 (66.0) | 314 (69.2) |
| Non‐verbal | 123 (30.4) | 17 (34.0) | 140 (30.8) |
| Unknown | 41 (9.2) | 6 (10.7) | 47 (9.4) |
| Epilepsy c | |||
| No active epilepsy | 245 (60.0) | 27 (52.9) | 272 (59.3) |
| Epilepsy | 163 (40.0) | 24 (47.1) | 186 (40.7) |
| Unknown | 38 (8.5) | 5 (9.0) | 43 (8.6) |
| Hearing c | |||
| No or mild impairment | 373 (96.4) | 46 (93.9) | 419 (96.1) |
| Deaf | 14 (3.6) | b | 17 (3.9) |
| Unknown | 58 (13.0) | 7 (12.5) | 65 (13.0) |
| Vision c | |||
| No or mild impairment | 368 (92.2) | 43 (84.3) | 411 (91.3) |
| Functionally blind | 31 (7.8) | 8 (15.7) | 39 (8.7) |
| Unknown | 46 (10.3) | 5 (8.8) | 51 (9.2) |
Percentage calculated by n/total n minus unknown n.
Excludes data for New South Wales/Australian Capital Territory.
Excludes South Australia children who had not received a follow‐up assessment at the time of data provision.
Fewer than five in the cell.
One in five Aboriginal and Torres Strait Islander children/young adults with CP were born or lived in the most socioeconomically advantaged areas (SEIFA quintiles 4 or 5) and two in five in the most socioeconomically disadvantaged areas (quintile 1). Overall, 72% of children lived in urban or regional areas, mostly on the eastern seaboard (Table 2 and Figure 1). Twenty‐eight per cent of children lived in remote and very remote areas, spread across the continent (Table 2 and Figure 1). The largest SEIFA/ARIA classification group, one in five children, was in the most socioeconomically disadvantaged group and lived in remote or very remote Australia. The next largest group comprised those in the most socioeconomically disadvantaged group who were living in major cities (Table 2).
TABLE 2.
Aboriginal and/or Torres Strait Islander children with cerebral palsy by Socio‐Economic Indexes for Areas (SEIFA) and Accessibility Remoteness Index Australia (ARIA) classifications, 1995–2014.
| SEIFA | ARIA | n (% of total) |
|---|---|---|
|
Quintile 1 40.1% |
Major Cities of Australia | 50 (10.2) |
| Inner Regional Australia | 26 (5.3) | |
| Outer Regional Australia | 27 (5.5) | |
| Remote Australia | 13 (2.6) | |
| Very Remote Australia | 81 (16.5) | |
|
Quintile 2 22.6% |
Major Cities of Australia | 29 (5.9) |
| Inner Regional Australia | 18 (3.7) | |
| Outer Regional Australia | 43 (8.8) | |
| Remote Australia | a | |
| Very Remote Australia | 19 (3.9) | |
|
Quintile 3 15.9% |
Major Cities of Australia | 32 (6.5) |
| Inner Regional Australia | 18 (3.7) | |
| Outer Regional Australia | 16 (3.3) | |
| Remote Australia | 6 (1.2) | |
| Very Remote Australia | 6 (1.2) | |
|
Quintile 4 12.2% |
Major Cities of Australia | 32 (6.5) |
| Inner Regional Australia | 11 (2.2) | |
| Outer Regional Australia | 6 (1.2) | |
| Remote Australia | 10 (2.0) | |
| Very Remote Australia | a | |
|
Quintile 5 9.2% |
Major Cities of Australia | 33 (6.7) |
| Inner Regional Australia | 0 | |
| Outer Regional Australia | 7 (1.4) | |
| Remote Australia | 0 | |
| Very Remote Australia | 5 (1.0) | |
| Total missing | 23 (4.5) | |
| Total | 491 (100) | |
Fewer than five in the cell.
FIGURE 1.
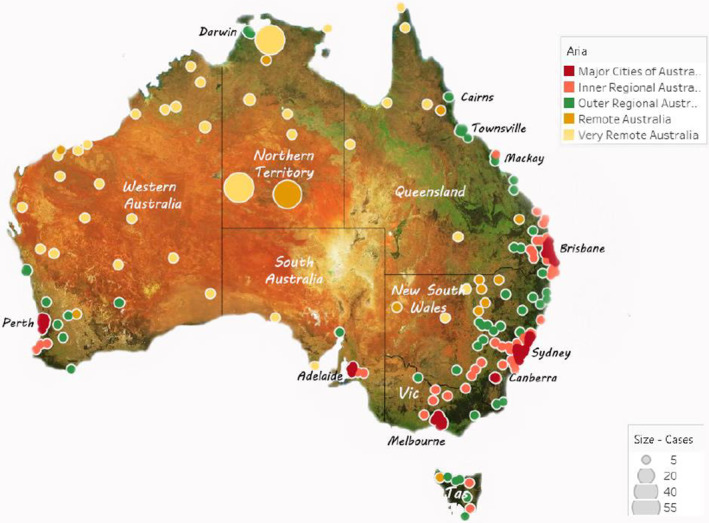
All Aboriginal and/or Torres Strait Islander children with cerebral palsy by Accessibility Remoteness Index Australia (ARIA), birth years 1995 to 2014.
Birth prevalence
Using data from Western Australia, South Australia, and Victoria (n = 161), we observed that birth prevalence of prenatally/perinatally acquired CP for Aboriginal and Torres Strait Islander children fluctuated, peaking in the mid‐2000s and decreasing to a low of 1.9 per 1000 live births in the most recent birth years (Figure 2a). The trend was not statistically significant (p = 0.09) but since the peak in the mid‐2000s has followed a similar pattern to the decline seen for non‐Indigenous children with CP.
FIGURE 2.

Aboriginal and/or Torres Strait Islander cerebral palsy birth prevalence by 1000 live births, with 2 year moving averages, South Australia, Victoria, and Western Australia combined, 1995 to 2014: (a) prenatal/perinatal cerebral palsy; (b) prenatal/perinatal cerebral palsy, children born <37 weeks; (c) prenatal/perinatal cerebral palsy, children born ≥37 weeks.
The birth prevalence of CP fluctuated for Aboriginal and Torres Strait Islander children born preterm (n = 37) (Figure 2b). There was no trend (p = 0.97) and birth prevalence estimates in the most recent birth years (8.9 per 1000 live births) were similar to those of the earliest estimates in the mid‐1990s (8.8 per 1000 live births). Birth prevalence of CP in term‐born infants (n = 88) fluctuated (p = 0.58) since the early 2000s to a very low point (0.5 per 1000 live births) in the most recent birth years (2013 to 2014) (Figure 2c).
Birth prevalence of CP for Aboriginal and Torres Strait lslander teenage mothers (n = 46) declined from 4 per 1000 live births in the mid‐1990s to a low of 1.8 per 1000 live births (most recent birth years), also a non‐significant trend (p = 0.81) likely owing to small numbers (Table S1).
There were 26 Aboriginal and Torres Strait Islander children with post‐neonatally acquired CP born in the three states used for the trends analysis. Large fluctuations in prevalence were observed with no trends identified (Table S2).
DISCUSSION
Aboriginal and Torres Strait Islander peoples are leaders in the concept of inclusion. The centrality of Indigenous culture overshadows impairments such that there is not a word to describe disability in Aboriginal or Torres Strait Islander languages and culture. 5 Disability is not about personal limitations, but societal responses to these, including the provision of equitable, culturally appropriate services. 5 However, until now there has been a dearth of evidence on the epidemiology of CP for Aboriginal and Torres Strait Islander people to guide this service provision.
This paper provides a birds‐eye view of CP in Aboriginal and Torres Strait lslander children, young people, and young adults in Australia. The study identified three key results warranting further discussion: (1) one in five Aboriginal and Torres Strait Islander children/young adults lived in socioeconomically disadvantaged remote and very remote areas of Australia; (2) most (72%) of Aboriginal and Torres Strait Islander individuals with CP lived in urban or regional areas; and (3) CP birth prevalence started to decline in the mid‐2000s to a current low of 1.9 per 1000 live births, especially for infants born at term and to teenage mothers.
In Australia, 19% of all Aboriginal and Torres Strait Islander people live in remote or very remote areas compared with 2% of non‐Indigenous people. 3 Similarly, in this study 20% of Aboriginal and Torres Strait lslander children/young adults with CP lived in remote or very remote areas and were in the lowest SEIFA quintile (our first key result). In our previous research looking at all Australian children with CP and their families there was no difference in SEIFA quintiles compared with the Australian population, 12 but this is not the case for Aboriginal and Torres Strait lslander children with CP.
It has also been identified that, in general, Australian families do not move house to access services when they have a child with CP, preferring to stay in their own community. 26 Aboriginal and Torres Strait Islander people are connected to country, and the desire to live on country is strong and is a human right. As such it is essential that children with CP who are living in remote and very remote areas have culturally safe CP‐specific intervention services that are accessible in their place of residence, and additional resourcing for this will be required (as agreed by the National Disability Insurance Scheme Rural and Remote Strategy). 27 For the 72% of children and young people who are spread widely through urban and regional centres of Australia (our second key result), it is vital that the health and disability workforce are trained in cultural competency and evidence‐based practice, to ensure safe, quality services are experienced by all.
The issue of accessibility of culturally safe services also exists for infants and children who are at risk of neurodevelopmental disability. International guidelines highlight the importance of early detection and intervention for infants with a high risk of CP. 28 , 29 Ninety per cent of motor development is reached between the age of 3 and 5 years; therefore early detection and intervention is essential to maximize motor function. 30 As these guidelines are being implemented in Australia and internationally, it is important that Aboriginal and Torres Strait Islander children, including those living in rural and remote regions, also benefit from this shift in practice. After early identification, access to culturally safe, responsive evidence‐based early intervention that is CP specific, alongside health and well‐being services for children and families, is required. This should be available to all in a wealthy country such as Australia.
Our final key result was that the prevalence of CP had started to decline. This is positive, and there are opportunities to continue monitoring and to build on this momentum. Fifty per cent of Aboriginal and Torres Strait Islander children with CP were born preterm and there was no decline in the birth prevalence of CP for infants born preterm. This lends support to the argument to prioritize Birthing on Country programmes. One programme undertaken in urban Brisbane 31 reduced preterm births by 40%; if scaled up, to include rural, remote, and very remote areas, this has the potential for huge impact. 32
There has been a long‐term trend to reduce the number of maternity units (often in rural and remote areas) in many countries. 33 , 34 In Australia, this results in pregnant females having to leave home and family weeks before their birth due date, potentially to culturally unsafe maternal and neonatal intensive‐care providers. 35 Birthing should not be a highly stressful experience; however, rural and remote service delivery favouring policies of centralization of obstetric services has ensured that this is the case for many Aboriginal and Torres Strait Islander people living in rural and remote areas. It is likely that the proportion of families living far away from maternity units will grow, so it is imperative to continually monitor the impact of centralization of obstetric services, while advocating for alternative options for females to deliver their babies in their communities, such as Birthing on Country programmes. 34 , 36
Culturally sensitive health promotion programmes focused on healthy pregnancies, such as Mums and Bubs, have been implemented into clinical practice, and are acknowledged as best practice, although they are still yet to be fully funded and provided at scale across the country. Promisingly, there has been an increase in Aboriginal and Torres Strait lslander mothers attending antenatal care in the first trimester (up to 65%) and a decrease in smoking during pregnancy (from 49% to 44% over 10 years). 37 , 38 The largest declines in smoking have been among 18‐ to 24‐year‐olds in recent years (2014–2019) in urban areas. 39 The prevalence of CP among teenage Aboriginal and Torres Strait Islanders seems to be declining. This mirrors the general trend where teenage pregnancy rates have decreased significantly from 70 births per 1000 Indigenous in 2006 to 46 per 1000 in 2017. 40 Engaging young Aboriginal and Torres Strait Islander people as youth health workers to lead sexual health programmes will help. 41 , 42 Opportunities therefore exist to further improve smoking rates and teenage pregnancy, by expanding evidence‐based programmes, particularly into remote areas.
There were some limitations to this study. At the time of data extraction, states with the highest proportions of Aboriginal and Torres Strait Islander people had incomplete ascertainment for their CP registers. It is a priority of the CP registers in these states to become complete, so that trend analyses can be Australia‐wide. The ACPR has historically collected maternal Indigenous status, and only recently started collecting the child's Indigenous status. Consequently, this study may have under‐reported the frequency of CP in Aboriginal and Torres Strait Islander children. We were unable to report ‘age at diagnosis’, as the proportion of missing data was too great. There may also be underestimates of intellectual, speech, and visual impairment in regions where culturally safe services do not currently exist.
The strengths of this study include the fact that it was led by Aboriginal researchers; best practice methodologies were used including a strength‐based perspective and consultation with the ACPR's Community, Aboriginal and Torres Strait Islander Reference Group to gain community input into the development and interpretation of the findings of this study. To date, to our knowledge this is the largest population‐based study of Aboriginal and Torres Strait lslander children with CP conducted in Australia and of First Nations children with CP across the globe.
It is anticipated that key stakeholders such as Aboriginal Community Controlled Health Organisations, the National Disability Insurance Scheme, and health and disability service providers will use this information to advocate for, and allocate appropriate resources to, the expansion of evidence‐based Aboriginal and Torres Strait Islander‐led antenatal care programmes, and services for the health and well‐being needs of children and young adults with CP and their families.
Much work in epidemiology and public health focuses on the presence (or absence) of disease, as we have done here with CP in Aboriginal and Torres Strait Islander peoples. However, to have effective public health in Australia we need to shift these parameters to the Aboriginal and Torres Strait Islander concepts of health: mental, physical, cultural, and spiritual, with land essential to well‐being. 6 In future research the ACPR group hopes to expand its work with Aboriginal and Torres Strait Islander people to map whether culturally appropriate services are accessible for children with CP, and to determine which health and well‐being outcomes are important and how they should be reported.
FUNDING INFORMATION
The Cerebral Palsy Alliance Research Foundation through an Early Career Grant for the first author. The Australian Capital Territory, New South Wales and Australian Cerebral Palsy Registers are funded by the Cerebral Palsy Alliance Research Foundation. The Northern Territory Cerebral Palsy Register is funded by Women, Children and Youth, Royal Darwin Hospital. The Queensland Cerebral Palsy Register is funded by Choice, Passion, Life. The South Australian Cerebral Palsy Register is funded by the Women's and Children's Health Network with additional support provided by Novita. The Tasmanian Cerebral Palsy Register is supported by St Giles and the Tasmanian Department of Health. The Victorian Cerebral Palsy Register received funding from the Lorenzo and Pamela Galli Research Trust, the Victorian Department of Health and Human Services, and the Royal Children's Hospital Foundation, and infrastructure support was provided by the Victorian Government's Operational Infrastructure Support Program. The Western Australian Register of Developmental Anomalies ‐ Cerebral Palsy is funded by Department of Health Western Australia. HSS received salary support through a National Health and Medical Research Council of Australia Early Career Fellowship (1144566) and Australasian Cerebral Palsy Clinical Trials Network.
Supporting information
Table S1: Aboriginal and/or Torres Strait Islander pre/perinatal cerebral palsy birth prevalence by 1000 live births
Table S2: Aboriginal and/or Torres Strait Islander post‐neonatally acquired cerebral palsy birth prevalence by 10 000 live births
ACKNOWLEDGMENTS
The members of the ACPR Birds‐Eye View Group are as follows: ACPR/Australian Capital Territory/New South Wales (Shona Goldsmith, Nadia Badawi, Anne Masi, Emma Stanton, Isabelle Balde, Katarina Ostojic); Northern Territory (Fiona Kay, Cassie Goldsworthy); Queensland (Megan Auld, Jacinta Quartermain); South Australia (Catherine Gibson, Heather Scott); Tasmania (Nadine Davies, Clare Wiltshire); Victoria (Gina Hinwood); Western Australia (Dylan Gration). Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
We thank all the children and young people with CP and their families. We are grateful to the Australian Institute of Health and Welfare for data from the National Perinatal Data Collection and the Consultative Council on Obstetric and Paediatric Mortality and Morbidity for providing access to data used for this project and for the assistance of the staff at Safer Care Victoria. We also thank the register staff, collaborators, and the organizations that support the work of the Cerebral Palsy Registers. We acknowledge the ACPR Community, Aboriginal and Torres Strait Islander Reference Group for sharing their wisdom and knowledge throughout this study. We sincerely thank the Aboriginal Health and Medical Research Council for their guidance and review in conjunction with their ethical oversight.
Martin T, McIntyre S, Waight E, Baynam G, Watson L, Langdon K, et al. ACPR Birds‐Eye View Group. Prevalence and trends for Aboriginal and Torres Strait Islander children living with cerebral palsy: A birds‐eye view. Dev Med Child Neurol. 2023;65:1475–1485. 10.1111/dmcn.15617
DATA AVAILABILITY STATEMENT
Research data are not shared.
REFERENCES
- 1. ABS . Aboriginal and Torres Strait Islander people: Census, 2021. 2022 [Available from: https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/aboriginal‐and‐torres‐strait‐islander‐people‐census/latest‐release.
- 2. Taylor A, Wilson T, Temple J, Kelaher M, Eades S. The future growth and spatial shift of Australia's Aboriginal and Torres Strait Islander population, 2016–2051. Population space and place. 2021;27(4):n/a. [Google Scholar]
- 3. Australian Institute of Health and Welfare . Rural and remote health. AIHW, Australian Government; 2019. [Google Scholar]
- 4. Mabo v Queensland (No 2). Australian High Court; 1992.
- 5. Avery S. Culture is inclusion: a narrative of Aboriginal and Torres Strait Islander people with disability. Sydney: First Peoples Disability Network; 2018. [Google Scholar]
- 6. Salmon M, Doery K, Dance P, Chapman J, Gilbert R, Williams R, et al. Defining the indefinable: Descriptors of Aboriginal and Torres Strait Islander peoples' cultures and their links to health and wellbeing. 2018.
- 7. Thurber KA, Thandrayen J, Banks E, Doery K, Sedgwick M, Lovett R. Strengths‐based approaches for quantitative data analysis: A case study using the australian Longitudinal Study of Indigenous Children. SSM ‐ population health. 2020;12:100637‐. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bond CJ, Singh D, Tyson S. Black bodies and Bioethics: Debunking Mythologies of Benevolence and Beneficence in Contemporary Indigenous Health Research in Colonial Australia. Journal of bioethical inquiry. 2021;18(1):83–92. [DOI] [PubMed] [Google Scholar]
- 9. Griffiths K, Coleman C, Lee V, Madden R. How colonisation determines social justice and Indigenous health—a review of the literature. Journal of population research (Canberra, ACT). 2016;33(1):9–30. [Google Scholar]
- 10. Cronin D, D'arcy J, Murphy L. Indigenous Resilience Project Report. Homebush, NSW: Edmund Rice Centre; 2019. [Google Scholar]
- 11. Prussing E. Through a Critical Lens: Expertise in Epidemiology for and by Indigenous Peoples. Science, technology, & human values. 2020;45(6):1142–67. [Google Scholar]
- 12. Woolfenden S, Galea C, Smithers‐Sheedy H, Blair E, McIntyre S, Reid S, et al. Impact of social disadvantage on cerebral palsy severity. Developmental medicine and child neurology. 2019;61(5):586–92. [DOI] [PubMed] [Google Scholar]
- 13. Blair E, Watson L, O'Kearney E, D'Antoine H, Delacy MJ. Comparing risks of cerebral palsy in births between Australian Indigenous and non‐Indigenous mothers. Developmental medicine and child neurology. 2016;58 Suppl 2:36–42. [DOI] [PubMed] [Google Scholar]
- 14. Galea C, McIntyre S, Smithers‐Sheedy H, Reid SM, Gibson C, Delacy M, et al. Cerebral palsy trends in Australia (1995–2009): a population‐based observational study. Developmental medicine and child neurology. 2019;61(2):186–93. [DOI] [PubMed] [Google Scholar]
- 15. Smithers‐Sheedy H, Waight E, Goldsmith S, Reid S, Gibson C, Watson L, et al. Declining trends in birth prevalence and severity of singletons with cerebral palsy of prenatal or perinatal origin in Australia: A population‐based observational study. Developmental medicine and child neurology. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fogarty W, Lovell M, Langenberg J, Heron M‐J. Deficit Discourse and Strengths‐based Approaches: Changing the narrative of Aboriginal and Torres Strait Islander health and wellbeing. Melbourne: The Lowitja Institute. [Google Scholar]
- 17. Walker M, Fredericks B, Mills K, Anderson D. "Yarning" as a Method for Community‐Based Health Research With Indigenous Women: The Indigenous Women's Wellness Research Program. Health care for women international. 2014;35(10):1216–26. [DOI] [PubMed] [Google Scholar]
- 18. ACPR . Australian Cerebral Palsy Register Report. 2016.
- 19. Delacy MJ, Reid SM, the Australian cerebral palsy register g . Profile of associated impairments at age 5 years in Australia by cerebral palsy subtype and Gross Motor Function Classification System level for birth years 1996 to 2005. Developmental Medicine & Child Neurology. 2016;58:50–6. [DOI] [PubMed] [Google Scholar]
- 20. Australian Institute of Health and Welfare Metadata Online Registry . Person—Indigenous status, code N ‐ Identifying and definitional attributes: Australian Institute of health and Welfare; 2022. [Available from: https://meteor.aihw.gov.au/content/602543?technical = True.
- 21. ABS . Census of Population and Housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2011. Australian Bureau of Statistics; http://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 accessed September 2014. 2011. [Google Scholar]
- 22. Accessibility/Remoteness Index of Australia Plus 2016. (ARIA+2016). Adelaide, South Australia: Hugo Centre for Migration and Population Research, The University of Adelaide. 2018. [Google Scholar]
- 23. Joseph FA, Hyett JA, Schluter PJ, McLennan A, Gordon A, Chambers GM, et al. New Australian birthweight centiles. Medical journal of Australia. 2020;213(2):79–85. [DOI] [PubMed] [Google Scholar]
- 24. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology. 1997;39(4):214–23. [DOI] [PubMed] [Google Scholar]
- 25. Australian Institute of Health and Welfare (AIHW) . National Perinatal Data Collection (NPDC). [Internet]. 2019. [cited August, 2021]. Available from: https://www.aihw.gov.au/about‐our‐data/our‐data‐collections/national‐perinatal‐data‐collection.
- 26. DeLacy MJ, Louca C, Smithers‐Sheedy H, McIntyre S. Change in residential remoteness during the first 5 years of life in an Australian cerebral palsy cohort. Developmental medicine and child neurology. 2016;58:60–5. [DOI] [PubMed] [Google Scholar]
- 27. National Disability Insurance Agency Rural and Remote Strategy 2016‐2019 2016 [Available from: https://www.ndis.gov.au/about‐us/strategies/rural‐and‐remote‐strategy.
- 28. Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom‐Hernandez J, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA pediatrics. 2017;171(9):897–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Morgan C, Fetters L, Adde L, Badawi N, Bancale A, Boyd RN, et al. Early Intervention for Children Aged 0 to 2 Years With or at High Risk of Cerebral Palsy: International Clinical Practice Guideline Based on Systematic Reviews. JAMA Pediatrics. 2021;175(8):846–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rosenbaum PL, Walter SD, Hanna SE, Palisano RJ, Russell DJ, Raina P, et al. Prognosis for Gross Motor Function in Cerebral Palsy: Creation of Motor Development Curves. JAMA: the journal of the American Medical Association. 2002;288(11):1357–63. [DOI] [PubMed] [Google Scholar]
- 31. Kildea S, Gao Y, Hickey S, Kruske S, Nelson C, Blackman R, et al. Reducing preterm birth amongst Aboriginal and Torres Strait Islander babies: A prospective cohort study, Brisbane, Australia. EClinicalMedicine. 2019;12:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Birthing on Country: Rise Safely [Available from: https://www.birthingoncountry.com/rise‐safely.
- 33. Kildea S, McGhie AC, Gao Y, Rumbold A, Rolfe M. Babies born before arrival to hospital and maternity unit closures in Queensland and Australia. Women Birth. 2015;28(3):236–45. [DOI] [PubMed] [Google Scholar]
- 34. Blondel B, Drewniak N, Pilkington H, Zeitlin J. Out‐of‐hospital births and the supply of maternity units in France. Health Place. 2011;17(5):1170–3. [DOI] [PubMed] [Google Scholar]
- 35. Kildea S, Tracy S, Sherwood J, Magick‐Dennis F, Barclay L. Improving maternity services for Indigenous women in Australia: moving from policy to practice. Medical journal of Australia. 2016;205(8):374–9. [DOI] [PubMed] [Google Scholar]
- 36. Huotari T, Rusanen J, Keistinen T, Lähderanta T, Ruha L, Sillanpää MJ, et al. Effect of centralization on geographic accessibility of maternity hospitals in Finland. BMC health services research. 2020;20(1):337‐. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Australian Institute of Health and Welfare 2019 . Australia's mothers and babies 2017—in brief. Perinatal statistics series no. 35. Cat. no. PER 100. Canberra: AIHW; 2019. [Google Scholar]
- 38. Closing the Gap Report 2020 . Commonwealth of Australia, Department of the Prime Minister and Cabinet.; 2020. [Google Scholar]
- 39. Maddox R, Thurber KA, Calma T, Banks E, Lovett R. Deadly news: the downward trend continues in Aboriginal and Torres Strait Islander smoking 2004–2019. Australian and New Zealand journal of public health. 2020;44(6):449–50. [DOI] [PubMed] [Google Scholar]
- 40. Australian Institute of Health and Welfare . Australia's Children. Canberra: AIHW; 2020. [Google Scholar]
- 41. Bell S, Aggleton P, Ward J, Murray W, Silver B, Lockyer A, et al. Young Aboriginal people's engagement with STI testing in the Northern Territory, Australia. BMC public health. 2020;20(1):459‐. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Marino JL, Lewis LN, Bateson D, Hickey M, Skinner S. Teenage mothers. Australian family physician. 2016;45(10):712–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Aboriginal and/or Torres Strait Islander pre/perinatal cerebral palsy birth prevalence by 1000 live births
Table S2: Aboriginal and/or Torres Strait Islander post‐neonatally acquired cerebral palsy birth prevalence by 10 000 live births
Data Availability Statement
Research data are not shared.


