Abstract
Objective
To synthesise evidence of the effectiveness of community based complex interventions, grouped according to their intervention components, to sustain independence for older people.
Design
Systematic review and network meta-analysis.
Data sources
Medline, Embase, CINAHL, PsycINFO, CENTRAL, clinicaltrials.gov, and International Clinical Trials Registry Platform from inception to 9 August 2021 and reference lists of included studies.
Eligibility criteria
Randomised controlled trials or cluster randomised controlled trials with ≥24 weeks’ follow-up studying community based complex interventions for sustaining independence in older people (mean age ≥65 years) living at home, with usual care, placebo, or another complex intervention as comparators.
Main outcomes
Living at home, activities of daily living (personal/instrumental), care home placement, and service/economic outcomes at 12 months.
Data synthesis
Interventions were grouped according to a specifically developed typology. Random effects network meta-analysis estimated comparative effects; Cochrane’s revised tool (RoB 2) structured risk of bias assessment. Grading of recommendations assessment, development and evaluation (GRADE) network meta-analysis structured certainty assessment.
Results
The review included 129 studies (74 946 participants). Nineteen intervention components, including “multifactorial action from individualised care planning” (a process of multidomain assessment and management leading to tailored actions), were identified in 63 combinations. For living at home, compared with no intervention/placebo, evidence favoured multifactorial action from individualised care planning including medication review and regular follow-ups (routine review) (odds ratio 1.22, 95% confidence interval 0.93 to 1.59; moderate certainty); multifactorial action from individualised care planning including medication review without regular follow-ups (2.55, 0.61 to 10.60; low certainty); combined cognitive training, medication review, nutritional support, and exercise (1.93, 0.79 to 4.77; low certainty); and combined activities of daily living training, nutritional support, and exercise (1.79, 0.67 to 4.76; low certainty). Risk screening or the addition of education and self-management strategies to multifactorial action from individualised care planning and routine review with medication review may reduce odds of living at home. For instrumental activities of daily living, evidence favoured multifactorial action from individualised care planning and routine review with medication review (standardised mean difference 0.11, 95% confidence interval 0.00 to 0.21; moderate certainty). Two interventions may reduce instrumental activities of daily living: combined activities of daily living training, aids, and exercise; and combined activities of daily living training, aids, education, exercise, and multifactorial action from individualised care planning and routine review with medication review and self-management strategies. For personal activities of daily living, evidence favoured combined exercise, multifactorial action from individualised care planning, and routine review with medication review and self-management strategies (0.16, −0.51 to 0.82; low certainty). For homecare recipients, evidence favoured addition of multifactorial action from individualised care planning and routine review with medication review (0.60, 0.32 to 0.88; low certainty). High risk of bias and imprecise estimates meant that most evidence was low or very low certainty. Few studies contributed to each comparison, impeding evaluation of inconsistency and frailty.
Conclusions
The intervention most likely to sustain independence is individualised care planning including medicines optimisation and regular follow-up reviews resulting in multifactorial action. Homecare recipients may particularly benefit from this intervention. Unexpectedly, some combinations may reduce independence. Further research is needed to investigate which combinations of interventions work best for different participants and contexts.
Registration
PROSPERO CRD42019162195.
Introduction
The global population aged over 65 years is expected to grow from 771 million people (10% of the population) in 2022 to 994 million by 2030 and 1.6 billion by 2050 (16%), necessitating change to healthcare systems.1 As the gap between life expectancy and healthy life expectancy grows, initiatives such as the World Health Organization’s Decade of Healthy Ageing seek to reverse this trend, maximising independence and social participation in later years as a shared global priority.2 3 4 This is important as an individual right, often diminished by ageism, but also to enable older people’s contribution to society and limit growing healthcare expenditure.2 5 6 7
Community based complex interventions to support healthy ageing are diverse and may target individuals, their environment, or both. Such interventions typically target factors that contribute to health and wellbeing in older adults, aiming to maximise independence and quality of life. They involve a combination of approaches, which may be tailored to the needs and circumstances of the individual.
The 2023 Chief Medical Officer’s Report on Health in an Ageing Society identifies maximising independence for older people as a policy priority for England.4 8 The report highlights an evidence gap regarding the effectiveness of complex interventions.4 Previous systematic reviews have indicated that, overall, such interventions probably have small but positive effects, despite some limitations in the underlying evidence.9 10 11 However, they have been unable to indicate which service models or components may be most effective. This field has seen further growth, and systematic review methods have developed strongly.12 13 14 Network meta-analysis extends traditional pairwise meta-analysis by comparing multiple interventions simultaneously in a single analysis, aiming to generate more precise results and rank them against each other to support policy and commissioning decisions.15 Network meta-analysis has not been used to evaluate community based complex interventions to sustain independence for older people. Therefore, we aimed to provide a rigorous, contemporary synthesis of trial evidence by using network meta-analysis to identify how interventions might best be configured to improve outcomes for older people and inform policy, commissioning, and delivery of evidence based services.
Methods
This was a prospectively registered systematic review and network meta-analysis (PROSPERO CRD42019162195) that used Grading of Recommendations Assessment, Development and Evaluation (GRADE) for network meta-analysis to assess certainty14 16 17 18 19 20 21 and followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 and network meta-analysis guidelines.22 23 We published the protocol before meta-analysis began.24 Only minor changes were made subsequently, detailed in appendix 1.
Objectives
Our objectives were to identify randomised controlled trials and cluster randomised controlled trials of community based complex interventions to sustain independence in older people; synthesise evidence of their effectiveness for key outcomes in a meta-analysis of study level data; identify key intervention components and study level frailty to inform groupings for network meta-analysis and meta-regression; compare effectiveness of different intervention configurations by using network meta-analysis; and investigate the impact of frailty and pre-frailty by using meta-regression.
Search strategy and selection criteria
Eligible studies were randomised controlled trials evaluating community based complex interventions to sustain independence in older people that met the criteria in table 1. DA searched the following databases and registers from inception between 9 and 11 August 2021: Cochrane Central Register of Controlled Trials (CENTRAL) (1992-); Medline (1946-); Embase and Embase Classic (1947-); CINAHL (1972-); PsycINFO (1806-); ClinicalTrials.gov (www.clinicaltrials.gov); and WHO International Clinical Trials Registry platform (https://trialsearch.who.int). Search strategies and their development are detailed in appendix 3. We also scanned reference lists of included reports (backward citation searches).
Table 1.
Eligibility criteria for studies
| Characteristic | Include | Exclude |
|---|---|---|
| Population | Older people (mean age ≥65 years) living at home at study entry | Participants living in residential care or nursing homes (care homes)25 |
| Intervention | Initiated and mainly provided in the community | Interventions delivered in other settings (eg, outpatient, day hospital, intermediate care) |
| Included two or more interacting components (intervention practices, structural elements, and contextual factors) | Interventions including only one discrete component (eg, exercise only) | |
| Targeted at the individual person, with provision of appropriate specialist care | Interventions not targeting the individual, such as general staff education or practice reorganisation | |
| Focused on sustaining (maintaining or improving) the person’s independence | Interventions not explicitly aimed at sustaining independence in activities of daily living | |
| Disease focused interventions (eg, for diabetes, depression) | ||
| Falls prevention interventions | ||
| Comparators | Usual care, “placebo,” or attention control or a different complex intervention that met criteria | Non-complex interventions |
| Outcomes | Outcome domains did not form part of eligibility criteria | Outcome data were measured only before 24 weeks |
| Study design | Randomised controlled trials or cluster randomised controlled trials including all variants such as crossover, waiting list control, and stepped wedge designs | Post-crossover data due to likelihood of carryover. Studies for which only one unit (ie, individual or cluster) was randomised to an arm |
| Report characteristics | All reports regardless of publication status, date, or language | - |
Duplicate records were removed with EndNote. Two reviewers independently used Rayyan (https://rayyan.ai/reviews) or Covidence (https://app.covidence.org/reviews) to evaluate eligibility of records (title and abstract) and, if potentially eligible, their reports (full text). We arranged translation as necessary. Disagreements were resolved by consensus, with guidance from the Project Management Group.
Data collection
Two reviewers independently extracted data in a custom built Microsoft Access database, with data finalised automatically in case of agreement or resolved by a third reviewer. The main outcomes were living at home, activities of daily living (instrumental/personal), hospital admission, care home placement, homecare services usage, costs, and cost effectiveness. Additional outcomes were health status, depression, loneliness, falls, and mortality.
Data were extracted (including treatment effect estimates) and categorised into three timeframes: short term (around six months): 24 weeks to 9 months; medium term (around 12 months): >9 months to 18 months; and long term (around 24 months): >18 months. Medium term was our main timeframe.
Other data items collected (including design and participant details) are listed in appendix 4. We did not routinely seek missing data but sought to clarify ambiguities.
Assessment of frailty
Two reviewers with extensive clinical-academic frailty expertise (AC and JGl) independently categorised study level frailty (robust, pre-frailty, frailty) on the basis of validated measures where available or participants’ characteristics and study inclusion criteria using the phenotype model as a framework.26
Intervention classification
We grouped all eligible interventions (including comparators) in preparation for network meta-analysis in a three stage process. Firstly, one reviewer (MJ, NL, RR, LM, IP, or EP) coded and summarised each intervention against the Template for Intervention Description and Replication items,27 28 and TC checked both coding and summaries, with disagreements resolved through discussion and involvement of the Project Management Group as necessary. Secondly, we generated categories of key intervention features through qualitative analysis, iteratively consolidating codes into categories. Thirdly, we grouped interventions on the basis of these categories, using a typology developed through discussion between reviewers, the Project Management Group, and experts including policy makers, commissioners, older people, and carers. The intervention groups became the network meta-analysis nodes.
Risk of bias
Two reviewers independently assessed risk of bias in each result of interest from each study, using the revised Cochrane risk of bias tool for randomised trials (RoB 2).12 29 Our effect of interest was assignment to the intervention (intention to treat). We rated risk of bias per domain and overall as low, some concerns, or high (serious or very serious concerns), through consensus between reviewers.
Data synthesis
We did separate meta-analyses for each timeframe for living at home (dichotomous), personal activities of daily living (continuous), instrumental activities of daily living (continuous), and care home placement (dichotomous) and in the medium term for hospital admission (dichotomous), health status (continuous), and depression (continuous). We narratively synthesised other outcomes owing to a lack of data suitable for meta-analysis. We preferred adjusted effect estimates but calculated effect estimates from extracted data where necessary and possible, applying cluster adjustment where applicable.
We meta-analysed the effect estimates by using Stata modules including metan, mvmeta, and network.30 We synthesised dichotomous outcomes as log transformed odds ratios.31 For continuous outcomes, we used Hedges’ g standardised mean difference. We did random effects meta-analyses.32
Initially, for each outcome and timeframe, we did a separate meta-analysis for each type of intervention versus control, to provide summary effectiveness results and forest plots based only on direct evidence. We then used network meta-analysis to compare relative effectiveness of all intervention types concurrently, combining direct evidence with indirect evidence, which is based on a network of intermediate comparisons between intervention types.15 We did network meta-analysis (for each outcome and timeframe separately) by using a multivariate random effects meta-analysis framework via the network module in Stata using restricted maximum likelihood estimation.30 We produced summary (pooled) effect estimates for each pair of treatments in the network, with 95% confidence intervals and network plots. On the basis of the results, we calculated the ranking of intervention groups by using re-sampling methods. To facilitate interpretation, we transformed each summary odds ratio to a summary risk ratio by using the median risk in the reference comparator arms and corresponding absolute intervention risks and risk differences by using the highest and lowest risk among reference comparator arms (n≥100) as the assumed comparator risks.33 We re-expressed standardised mean differences as the mean difference by using a pooled standard deviation for a common measure of the outcome.
We examined the consistency assumption (that direct and indirect evidence are consistent with each other) for each treatment comparison where possible and across the whole network.34 35 We summarised heterogeneity by the estimate of between study variance (τ), where possible.
We examined the effect of study level frailty on each intervention group effect where data allowed by using network meta-regression. We did sensitivity analyses excluding results rated as at very serious risk of bias. We examined funnel plots for small study effects if 10 or more studies were available.
We used the GRADE framework, adapted for network meta-analysis, to rate the certainty of the results of our network meta-analysis and presented summary of findings tables ordered by certainty and ranking.14 16 17 18 19 21 We used plain language terms “probably” and “may” to indicate moderate and low certainty respectively and qualified the size and direction of point estimates (see appendix 5).20 36 We followed the brief economic commentary framework to summarise and compare the principal economic findings reported by included studies.37
Patient and public involvement
This review benefited from the involvement of our established Patient and Public Involvement Frailty Oversight Group in the Bradford Institute for Health Research. The group has a structure that provides connections to the whole spectrum of older people, with a focus on those living with frailty to enable meaningful, public involvement in our research projects.38 We consulted our Frailty Oversight Group throughout the development of the protocol and discussed plans in detail at the group’s quarterly meetings and at our annual consumer research conference. Group members helped to draft and revise the plain language summary for our funding application. Other examples of patient and public involvement include the selection of important outcomes and their prioritisation as main and additional outcomes. Frailty Oversight Group members emphasised that a wide range of outcomes were important to older people, with a particular focus on independence in addition to wellbeing, alongside service orientated outcomes. We also spent time discussing the intervention components that we had identified with group members. Through this work, we developed and refined our descriptions of the components and thus the findings. The plain language summary of our findings, developed with Frailty Oversight Group members, is presented in appendix 2.
Results
Study selection
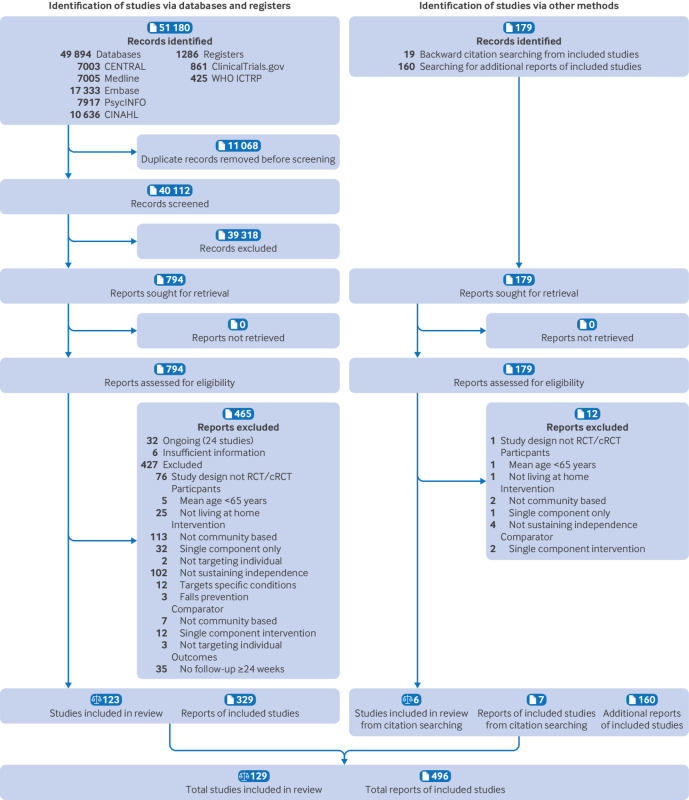
Figure 1 shows the study selection process. Our database and register searches identified 51 180 records. After de-duplication, we screened 40 112 records and then assessed 794 reports for eligibility. Subsequently, we assessed 179 reports identified through searching for additional reports of included studies and backward citation searches. We excluded 477 reports; reasons are listed in appendix 6. We included 129 studies with 266 eligible intervention arms presented in 496 reports39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 150 151 152 153 154 155 156 157 158 159 160 161 162 163 164 165 166 167; 90 studies contributed to network meta-analyses.
Fig 1.
PRISMA flow diagram showing identification, selection, and inclusion of studies from databases, registers, and other sources.23 ICTRP=International Clinical Trials Registry Platform
Included study characteristics
The 129 studies assigned 74 946 participants (reported by 126 studies; 61% (44 817/72 877) women and 39% (28 060/72 877) men, from 123 studies). Studies were predominantly conducted in developed countries, and most participants were described as white. Nevertheless, the overall population included a broad range of demographic characteristics. Study populations included all frailty levels. Study characteristics are summarised in appendix 7. We judged most results to be at high risk of bias, primarily owing to missing outcome data (appendix 8).
Intervention characteristics
We identified 19 separate components of included interventions (see box 1 and appendix 9), which were evaluated in 63 combinations including the absence of all these components, which we termed “available care.” “Homecare” was another common control group in populations in which all participants were receiving formal homecare. Homecare was one of 14 action components (further examples include education and exercise). Five other components primarily involved a tailoring process of ascertainment or assessment and planning with potential for subsequent multifactorial action, most often “multifactorial action” from care planning (a process of individualised multidomain assessment and management) with or without routine “review” (scheduled, regular follow-ups). Multifactorial action was further delineated according to the presence or absence of an embedded medication review and specific self-management strategies. Twenty six intervention groups (combinations) were evaluated in more than one study, and these are summarised in relation to Template for Intervention Description and Replication items in appendix 10.
Box 1. Nineteen identified components of community based complex interventions* intended to sustain independence in older people.
Action components
“Activities of daily living training”
Providing “aids” and adaptations
“Alternative medicine”
“Care voucher” provision
“Cognitive training”
Health “education”
Physical “exercise”
Formal “homecare”
Engagement in “meaningful activities”
“Nutrition”(al) support
Psychological (mood) therapy (“psychology”)
“Social skills” training
Technology for communication and engagement (“telecoms”)
“Welfare” rights advice.
Tailoring components
“Multifactorial action” from individualised care planning
Routine “review”
“Medication review”
“Monitoring”
Routine “risk screening”
*Text in quotation marks is short version of name used in results
Characteristics of network meta-analyses
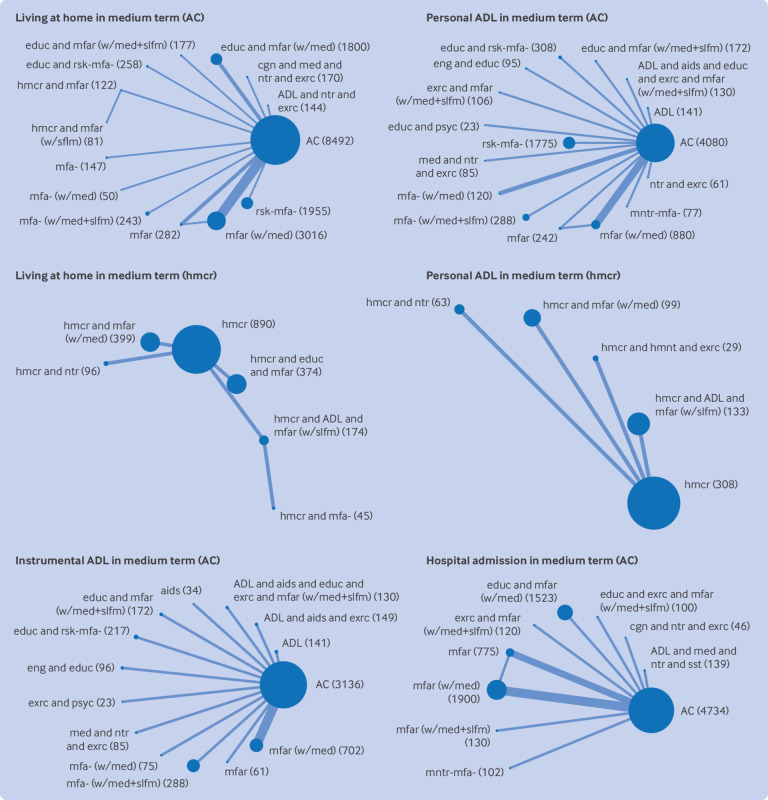
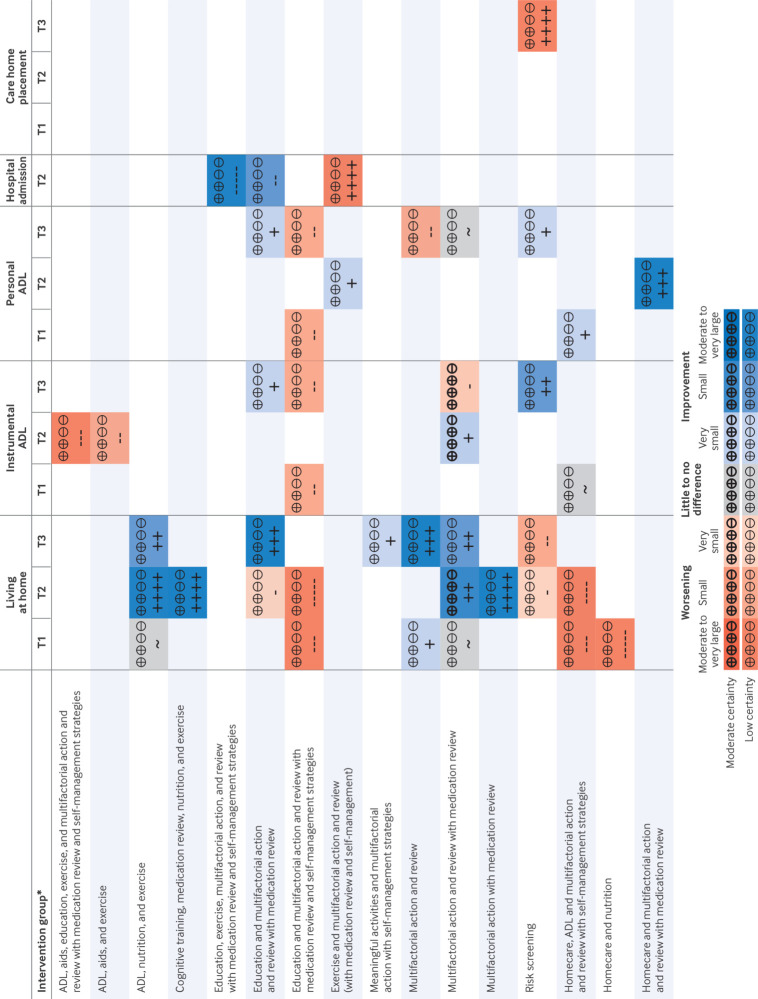
Most networks were small and sparse, with few included studies contributing to most networks (fig 2). We found little evidence of inconsistency or small study effects, but the power to detect this was usually low. All outcomes except mortality needed to be analysed in two separate network meta-analyses, as the networks were disconnected: one with available care as the reference comparator (“available care network”) and one with homecare as the reference comparator (“homecare network”). Estimates are reported here only in comparison with the reference comparator. Comparison with available care is the effect of adding the intervention for a population who are not all receiving any particular care; comparison with homecare is similarly an alternative intervention for a population already in receipt of homecare without associated reablement or multifactorial action from care planning. Most estimates were of low certainty or very low certainty owing to risk of bias, imprecision, or their combination, and we do not detail very low certainty estimates below. Full results are presented in appendix 11 and summarised in figure 3.
Fig 2.
Network plots for analyses of main outcomes in medium term (~12 months) that yielded ≥1 finding of at least low certainty. AC indicates network including available care; hmcr indicates network including formal homecare. Each node is labelled with intervention group abbreviation and number of participants. Node size is proportionate to number of participants; edge thickness is proportionate to number of comparisons. Intervention and control group abbreviations are combination of: ADL=activities of daily living training; aids=provision of aids and adaptations; cgn=cognitive training; comm=technology for communication and engagement; educ=health education; eng=engagement in meaningful activities; exrc=physical exercise; hmcr=formal homecare; hmnt=alternative medicine; med=medication review; mfa=multifactorial action; mfar=multifactorial action and follow-on routine review; mntr-mfa=monitoring, which may trigger multifactorial action; ntr=nutritional support; psyc=psychological therapy; rsk-mfa=risk screening, which may trigger multifactorial action; sst=social skills training; vchr=care voucher provision; wlfr=welfare rights advice; w/med=with medication-review; w/slfm=with self-management strategies
Fig 3.
Summary of moderate and low certainty evidence for main outcomes synthesised with network meta-analysis. *In comparison with reference comparator. For intervention groups including homecare, reference comparator is homecare; for all other intervention groups, reference comparator is available care. Living at home (+ favoured); instrumental ADL (+ favoured); personal ADL (+ favoured); hospital admission (– favoured); care home placement (– favoured). ADL=activities of daily living; T1=short term timeframe (24 weeks to 9 months); T2=medium term timeframe (>9 months to 18 months; T3=long term timeframe (>18 months); +++++=very large increase; ++++=large increase; +++=moderate increase; ++= slight increase; +=very slight increase; ~=little to no difference; -=very slight reduction;--=slight reduction; ---=moderate reduction; ----=large reduction; -----=very large reduction. Blue shades indicate possible benefit; orange shades indicate possible harm; bold indicates moderate certainty evidence
Living at home
For living at home in the medium term, the available care network included 21 studies (n=16 937) with 14 intervention groups (fig 4). We found moderate certainty evidence that “multifactorial action and review with medication review” probably results in a slight increase in the odds of living at home (odds ratio 1.22, 95% confidence interval 0.93 to 1.59). We found low certainty evidence that “multifactorial action with medication review” (odds ratio 2.55 (large), 0.61 to 10.60), “cognitive training, medication review, nutrition, and exercise” (1.93 (large), 0.79 to 4.77), and “activities of daily living training, nutrition, and exercise” (1.79 (large), 0.67 to 4.76) may result in an increase in the odds of living at home and that “risk screening” (0.90 (very small), 0.66 to 1.23), “education and multifactorial action and review with medication review” (0.88 (very small), 0.60 to 1.29), and “education, multifactorial action, and review with medication review and self-management strategies” (0.41 (very large), 0.14 to 1.17) may each result in some reduction in the odds of living at home. Other comparisons were very low certainty.
Fig 4.

Living at home in medium term: comparisons with available care summary of findings table. Summary of findings table shows relative effects and anticipated absolute effects of each community based complex intervention type compared with available care (ac) for living at home outcome in medium term. Living at home is binary outcome, alternative outcome being either care home placement or death. Relative effects are odds ratio (OR) from network meta-analysis (NMA) and risk ratio (RR) calculated from odds ratio. OR>1 (or RR>1) favours listed community based complex intervention; OR<1 favours available care. Intervention types are ordered by certainty of evidence (high to very low) and ranking (highest to lowest). NMA included 21 studies, 14 nodes, and 16 937 participants in total. Follow-up ranged from 12 to 18 months. Heterogeneity was estimated as τ=8.56×10-2. Consistency assumption held. Mean rank of available care was 9.9 (95% CI 7 to 12). *Calculated from OR and assumed comparator risk of 0.935, median available care risk among these studies. †Serious concerns about imprecision as confidence interval (CI) crosses no effect line and includes substantial benefit. CI for absolute effect with high risk population also includes pre-specified definition of very small harm, but given that this was marginal and in light of small lower CI for RR (0.9955), this was not judged as very serious. Downgrade once. ‡Very serious concerns about imprecision as CI includes substantial benefit and substantial harm. Downgrade twice. §Very serious concerns about risk of bias owing to exclusion of participants in per protocol analysis and missing outcome data in indirect evidence via homecare and multifactorial action and review versus available care comparison. Downgrade twice. ¶Very serious concerns about imprecision as CI is very wide, no closed loop exists, and direct comparison is based on indirect evidence from 122 people in homecare and multifactorial action and review and 81 people in homecare and multifactorial action and review with self-management, which does not meet optimal information size. Already downgraded twice for risk of bias; downgrade once. **Very serious concerns about risk of bias owing to exclusion of participants in per protocol analysis and missing outcome data. Downgrade twice. ††Very serious concerns about imprecision as CI is very wide, no closed loop exists, and direct comparison is based on indirect evidence from 122 people in homecare and multifactorial action and review, which does not meet optimal information size. Already downgraded twice; downgrade once. ‡‡Serious concerns about risk of bias owing to missing outcome data. Downgrade once. §§Serious concerns about risk of bias owing to recruitment process of participants and missing outcome data in one study. Downgrade once. ¶¶Very serious concerns about risk of bias owing to randomisation process and missing outcome data. Already downgraded twice; downgrade once
In the short term and long term timeframes, results were low certainty at best. For “multifactorial action and review with medication review” and “activities of daily living traning, nutrition, and exercise,” estimates were similarly of small increases in the long term but of little to no difference in the short term. For “education, multifactorial action, and review with medication review and self-management strategies” and “risk screening,” we found similar results in other timeframes (may reduce living at home), but for “education and multifactorial action and review with medication review,” we found contrasting evidence of an increase in living at home.
The homecare network for living at home was smaller (five studies; n=1978 in the medium term). In the short and medium term timeframes we found low certainty evidence that “homecare, activities of daily living traing, and multifactorial action and review with self-management strategies” may result in reductions (short term, odds ratio 0.63 (moderate), 0.31 to 1.26; medium term, 0.76 (large), 0.40 to 1.45) in the odds of living at home compared with “homecare” alone. In the short term, “homecare and nutrition” may result in reductions in the odds of living at home compared with “homecare” (odds ratio 0.34 (very large), 0.12 to 0.95). Other comparisons were of very low certainty.
Instrumental activities of daily living
The medium term instrumental activities of daily living available care network included 16 studies (n=5309) with 14 intervention groups. We found moderate certainty evidence that “multifactorial action and review with medication review” was associated with very slightly increased independence in instrumental activities of daily living versus “available care” (standardised mean difference 0.11, 95% confidence interval 0.00 to 0.21). Two intervention groups may result in some reduction in instrumental activities of daily living: “activities of daily living training, aids, and exercise” and “activities of daily living training, aids, education, exercise, and multifactorial action and review with medication review and self-management strategies.” The findings for “multifactorial action and review with medication review” in the long term were contrasting, with moderate certainty evidence of a very slight reduction in instrumental activities of daily living (standardised mean difference −0.08, −0.21 to 0.05).
For the homecare network, we had one low certainty finding in the short term timeframe of little to no difference for “homecare, activities of daily living training and multifactorial action and review with self-management strategies,” with all other comparisons being of very low certainty.
Personal activities of daily living
For personal activities of daily living, 20 trials (n=8583 participants) with 16 intervention groups contributed to the medium term available care network. One comparison was low certainty: “exercise and multifactorial action and review with medication review and self-management startegies” may result in a very slight increase in personal activities of daily living (standardised mean difference 0.16, −0.51 to 0.82).
The homecare network included four trials (n=632 participants) in the medium term. Here too, only one comparison with “homecare” was low certainty: “homecare and multifactorial action and review with medication review” may result in an increase in personal activities of daily living (standardised mean difference 0.60 (moderate), 0.32 to 0.88).
Other main outcomes
For the service outcome of hospital admission, we found low certainty estimates of some reductions for “education, exercise, and multifactorial action and review with medication review and self-management strategies” and “education and multifactorial action and review with medication review” and of an increase for “exercise, multifactorial action, and review with medication review and self-management strategies.” For care home placement, all estimates were rated as very low certainty in the medium term. We found some evidence of both increases and decreases in use of homecare services with little pattern (not meta-analysed).
The summary of economic evidence included 39 studies (appendix 12). On the basis of the conclusions of 22 studies that did a full economic evaluation, five intervention groups seemed promising compared with a standard intervention or available care from an economic perspective: “activities of daily living training” (medium term time horizon); “homecare and multifactorial action and review with medication review and self-management strategies” (short term time horizon); “meaningful activities and education” (short and medium term time horizon); “multifactorial action and review with medication review” (short term but not medium or long term time horizon); and “exercise and multifactorial action with medication review” (long term time horizon).
Additional outcomes
Additional outcomes are summarised in appendix 13. We found little evidence of any effect on self-reported health status, only low certainty beneficial findings regarding depression, and very little evidence regarding loneliness; more complex interventions were associated with less falling than with more falling (12 v 4 studies). For mortality, we had a large network of 65 studies (n=38 351) and 41 intervention groups. We found low certainty evidence of reductions for two intervention groups and increases for five intervention groups.
Investigations of frailty and risk of bias
Across all outcomes, risk of bias sensitivity analyses produced very similar estimates to the main analyses. Funnel plots showed little evidence of asymmetry. Network meta-regressions were unable to estimate the effects of frailty for many comparisons, and those that were estimable had very wide confidence intervals.
Discussion
Principal findings
Our review has found evidence that “multifactorial action and review with medication review” probably improves the odds of living at home in the medium term timeframe (around 12 months). We also found that other complex interventions (“multifactorial action with medication review”; “cognitive training, medication review, nutrition, and exercise”; and “activities of daily living training, nutrition, and exercise”) may result in an increase in the odds of living at home in this timeframe. For 12 other intervention groups, we found low certainty evidence that they may improve or worsen at least one main outcome, but for other intervention groups evidence was either absent or very uncertain.
We identified moderate certainty evidence in three of our analyses of main outcomes, all related to “multifactorial action and review with medication review.” In comparison with “available care,” we found a probable slight increase in living at home in the medium term and a very slight increase in independence in instrumental activities of daily living in the medium term, but in contrast also a very slight reduction in instrumental activities of daily living in the long term (fig 3). The direct evidence for probable worsening came from studies that also contributed to the beneficial medium term finding (tables 28 and 32 and figures 8 and 14, appendix 11).49 131 For homecare recipients, the addition of “multifactorial action and review with medication review” was associated with low certainty evidence of a moderate increase in personal activities of daily living in the medium term (fig 3).
Strengths and limitations of review
We used rigorous methods to summarise the contemporary evidence on community based complex interventions for older people as an area of high strategic priority and global policy relevance. The evidence originated from a diverse population of older people, albeit mainly from high income regions. Population subgroups of various socioeconomic status, frailty levels, and ethnicity were included, and the ratio of women to men seemed typical for older populations.1 People with greater resource may be over-represented in many of these trials, given the voluntary nature of participation, which may have limited the effects of interventions and hence contributed to the small effect sizes presented here.
We developed a data driven grouping of interventions with expert guidance, so the groups were clearly specified to support practice, commissioning, and policy decisions. Our approach has resulted in a very clear typology of interventions, avoiding the historical problem of combining different interventions under unhelpful umbrella terms. We acknowledge that some clinical heterogeneity remains within intervention groups, particularly in the care available to different study populations. However, application of this typology led to the separation of evidence from populations in receipt of homecare and those that were not, reducing heterogeneity and improving the specificity of recommendations.
For consistency, we limited our review to interventions focused explicitly on independence in activities of daily living. Although this differs from preventing institutionalisation or activity limitation, multifactorial action interventions focused on each of these may work similarly. As such interventions can have multiple foci, differences may reflect intervention reporting rather than design. A less rigorous application of the criteria may have enabled us to pool similar evidence from more trials.168 169
Many of the trials seemed to be well conducted under challenging circumstances, and most declared non-commercial support, limiting the risks of funding bias. However, most results were at some risk of bias owing to missing outcome data. This was often inevitable given the combination of a frail population, long timelines, self-reported outcomes, community based research, and our stringent application of the RoB 2 tool. Many of the identified risks of within study bias were towards no effect or favouring the control group, meaning that true intervention effects may have been underestimated.
Owing to the scarcity of both direct and indirect evidence, the power to examine heterogeneity and inconsistency was low in most networks. However, the assessments we were able to do generally indicated little heterogeneity or inconsistency. We were also unable to effectively investigate the effect of population frailty on intervention effects, because of a lack of comparisons that contained different frailty populations.
We carefully assessed certainty in the findings by using GRADE for network meta-analysis guidance, providing clarity for the reader about the strength of the results. For many estimates, certainty was reduced because the confidence intervals included both improvement and worsening. Therefore, some low certainty findings may represent the play of chance around no effect.
Comparison with other studies
Whereas other reviews of similar literature have tended to identify positive effects, albeit small and with some limitations in the underlying evidence,9 10 11 this review has found evidence of both positive and negative effects, depending on the intervention type (fig 3). This difference is likely to reflect the broad pairwise pooling of comparisons in other reviews, with different combinations of intervention components, different comparators, and heterogeneous effects and time points. These other reviews also did not use GRADE to assess the certainty of the evidence or the RoB 2 tool to assess risk of bias and may therefore have been less likely to conclude that a statistically significant finding was nevertheless very uncertain.
Two recently published effectiveness trials have continued the trend of many previous studies in finding no significant difference in outcomes of interest.170 171 Given that many of the effects estimated in this review were relatively small, future definitive trials of similar interventions will likely need to be much larger than most of those included to provide sufficient power to identify plausible effects on independence.
Conclusions, policy implications, and future research
Overall, our best evidence of combinations associated with sustained independence are service models for older people that incorporate care planning leading to multifactorial action with embedded medication review. The strongest evidence also favoured services incorporating ongoing review of the older person. The combination of exercise and nutritional support was part of two additional favourable intervention groups. Given the overall evidence for their benefits, we recommend access to these interventions in services for older people.172 173
Unexpectedly, we found evidence that some intervention combinations may reduce independence. This finding was not one that we anticipated but is not one that should be dismissed entirely, despite uncertainty in the evidence. Plausible mechanisms depend on the intervention group details but include invoking disengagement with the person’s health or with services or encouraging an individual to take on more than they can effectively manage. It could also be the case that certain events, such as care home placement or hospital admission, may be part of the best care strategy for an individual. Even deterioration in activities of daily living may be in response to provision of assistance for tasks that someone finds difficult or painful and otherwise unrewarding and may therefore be an acceptable trade-off. We recommend that practitioners, commissioners, and policy makers remain mindful of these possibilities when designing systems of care.
Despite a very large amount of primary research (129 studies; 74 946 participants) a degree of uncertainty exists about the effects of many types of intervention, although this does not mean that they are ineffective. Although methodological improvements in the primary research could further enhance knowledge, consideration of the scale of effort that would be needed to begin to complete this network of interventions is worthwhile. Therefore, whether embarking on a programme of large scale randomised controlled trials to further examine all interventions would be an effective use of research resources is unclear. Value of information analysis, which aims to quantify the value of new research to examine existing uncertainties, may be a helpful next step to prioritise which interventions to take forward to new trial based evaluation.174 Additionally, conducting individual participant data meta-analysis and realist synthesis may be useful to better explore the factors that may relate to benefit.175
What is already known on this topic
Older people prioritise maintenance of independence
Previous systematic reviews have suggested that community based complex interventions may support independence for older people, but which are most effective is unclear
The lack of clear guidance about which services to implement has hampered translation of evidence into policy and practice
What this study adds
Individualised care planning with tailored actions, including medicines optimisation and regular follow-ups, probably helps people to stay living at home
Although some complex interventions may sustain independence, others may reduce independence
Further evidence is needed about who benefits most from which kinds of interventions, which may be provided by individual participant data meta-analysis
Acknowledgments
We are grateful to Nicola Harrison and Lesley Brown who coordinated and facilitated meetings with our Frailty Oversight Group; members of the Frailty Oversight Group, in particular Anne Grice and Marilyn Foster; members of the NIHR Applied Research Collaboration, Older People with Frailty Theme, Research Implementation Advisory Group; Zubair Arastu and Friederike Ziegler for their contributions to screening reference lists; Andy Mprah for his contribution to data collection; and Jasmin Manik for her support with testing the RoB 2 tool algorithms. We are particularly grateful to all of the authors of studies, both included and excluded, who responded to requests for information.
Web extra.
Extra material supplied by authors
Web appendix: Appendix 1-13
Contributors: AC, TC, JGl, and RRi conceived of the study. AC, TC, JE, AF, JGl, MJ, NL, EP, and RRi designed the study. DA, TC, and NL developed the search strategy. DA executed the database and trial register searches. TC, JGr, MJ, NL, JM, EP, RRa, and RW selected the studies. RB, CB, TC, JGr, MH, MJ, NL, JM, LM, EP, IP, RRa, OT, and RW extracted data. AC and JGl assessed frailty. AC, TC, AE, AF, JGl, MJ, and NL did intervention grouping. CB, TC, MJ, NL, and MP assessed risk of bias. MJ liaised with patient and public involvement groups. RB, MB, and JE prepared and analysed effectiveness data. JE and RRi supervised the meta-analyses. TC and NL assessed the certainty of the evidence. TC and NL did economic and narrative synthesis. AC, TC, JE, AF, JGl, NL, RRi, and OT interpreted the findings. TC wrote the first draft of the manuscript with input from AC, JE, AF, and JGl. All authors contributed to critically reviewing or revising the manuscript. CB, MB, RB, AC, TC, JE, JGl, JGr, MH, MJ, NL, JM, LM, EP, IP, MP, RRa, OT, and RW collectively accessed and verified the underlying data reported in the manuscript. JE and NL contributed equally. TC is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This project was funded by the National Institute for Health Research (NIHR) Health Technology Assessment programme (NIHR128862) and will be published in full in Health Technology Assessment.176 The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The grant applicants designed the overarching systematic review and network meta-analysis; the funders approved the protocol. The funders have not been involved in any aspect of the collection, analysis, or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at https://www.icmje.org/disclosure-of-interest/ and declare: AC, TC, JE, AF, JGl, MJ, NL, and RRi had financial support from the NIHR Health Technology Assessment Programme for the submitted work; MB had financial support from the PhD Graduate Teaching Fund at the University of Liverpool for the submitted work; DA declares payment made to her employer, University of Leeds Library, from the Academic Unit for Ageing and Stroke Research, Bradford Institute for Health Research, for services that included contributions to the submitted work; TC, AC, and AF received research funding from NIHR Programme Grants for Applied Research; AC and AF also received research funding from NIHR HSDR Programme; AC also received research funding from Health Data Research UK, NIHR ARC Yorkshire and Humber, NIHR Leeds BRC, and Dunhill Medical Trust; AF also declares NIHR Senior Investigator award, National Institute for Health (USA) payment for panel membership in 2021 and 2022, and University of Leeds Governor representative on the Governors Board of Bradford Teaching Hospitals NHS Foundation Trust; MB and MP received NIHR pre-doctoral fellowship funding; RB is supported by matched funding awarded to the NIHR Applied Research Collaboration (West Midlands) and is a member of the data monitoring committee for the Predict and Prevent AECOPD Trial and College of Experts, Versus Arthritis; AC is a member of NIHR HTA Commissioned Research Funding Committee and Dunhill Medical Trust Research Grants Committee; RRi received personal payments for training courses provided in-house to universities (Leeds, Aberdeen, Exeter, LSHTM) and other organisations (Roche), has received personal payments from the BMJ and BMJ Medicine as their statistical editor, is a co-convenor of the Cochrane Prognosis Methods Group and on the Editorial Board of Diagnostic and Prognostic Research, and Research Synthesis Methods, but receives no income for these roles, receives personal payment for being the external examiner of the MSc Medical Statistics, London School of Hygiene and Tropical Medicine, was previously an external examiner for the MSc Medical Statistics at University of Leicester, has written two textbooks for which he receives royalties from sales (Prognosis Research in Healthcare, and Individual Participant Data Meta-analysis), is a lead editor on an upcoming book (Cochrane Handbook for Prognosis Reviews, Wiley, 2025), for which he will receive royalties from sales, has received consulting fees for a training course on IPD meta-analysis from Roche in 2018, the NIHR HTA grant paid for travel to Leeds for one meeting, and is a member of the NIHR Doctoral Research Fellowships grant panel, and a member of the MRC Better Methods Better Research grant panel—for the latter, he receives an attendance fee; MH declares NIHR Academic Clinical Fellowship; OT declares NIHR Academic Clinical Lectureship and Dunhill Medical Trust Doctoral Research Fellowship RTF107/0117; no other relationships or activities that could appear to have influenced the submitted work.
Transparency: The lead author (the manuscript's guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: To ensure that we clearly communicate our findings with patients and member of the public, we spent time discussing the intervention components we had identified with Frailty Oversight Group members. Through this work, we developed and refined our descriptions of the components. Frailty Oversight Group members helped to draft and revise the plain language summary of our findings (see appendix 2). This will be included in the final report to be published in Health Technology Assessment,176 as well as on our website. We have produced short video presentations of our work that are also available. Our findings will be publicised on social media and at our regular research engagement events in the local community. As this systematic review was secondary research using aggregated, anonymised data, we do not have any contact details for the participants in the primary research to enable us to share the findings directly with them.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
Ethics approval was not sought as this systematic review was secondary research using aggregated, anonymised data available in the public domain.
Data availability statement
The data associated with this paper will be openly available indefinitely upon publication under a Creative Commons attribution license from the University of Leeds Data Repository. Summary effect estimates and findings from network meta-analyses: https://doi.org/10.5518/1377; risk of bias judgments: https://doi.org/10.5518/1386.
References
- 1.United Nations Department of Economic and Social Affairs. Population Division. World Population Prospects 2022: Summary of Results. 2022. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/wpp2022_summary_of_results.pdf.
- 2.World Health Organization. Decade of Healthy Ageing: 2020-2030. https://www.who.int/ageing/decade-of-healthy-ageing.
- 3.World Health Organization. Global Health Estimates: Life expectancy and leading causes of death and disability. 2023. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-life-expectancy-and-healthy-life-expectancy.
- 4.Whitty CJM. Chief medical officer’s annual report 2023: Health in an ageing society. 2023. https://www.gov.uk/government/publications/chief-medical-officers-annual-report-2023-health-in-an-ageing-society.
- 5. Han L, Clegg A, Doran T, Fraser L. The impact of frailty on healthcare resource use: a longitudinal analysis using the Clinical Practice Research Datalink in England. Age Ageing 2019;48:665-71. 10.1093/ageing/afz088 [DOI] [PubMed] [Google Scholar]
- 6. de Meijer C, Wouterse B, Polder J, Koopmanschap M. The effect of population aging on health expenditure growth: a critical review. Eur J Ageing 2013;10:353-61. 10.1007/s10433-013-0280-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pot AM, Rabheru K, Chew M. Person-centred long-term care for older persons: a new Lancet Commission. Lancet 2023;401:1754-5. 10.1016/S0140-6736(23)00920-0 [DOI] [PubMed] [Google Scholar]
- 8. Mahase E. Generalist skills are vital to serve ageing population, says England’s CMO. BMJ 2023;383:2640. 10.1136/bmj.p2640 [DOI] [PubMed] [Google Scholar]
- 9. Beswick AD, Rees K, Dieppe P, et al. Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet 2008;371:725-35. 10.1016/S0140-6736(08)60342-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Luker JA, Worley A, Stanley M, Uy J, Watt AM, Hillier SL. The evidence for services to avoid or delay residential aged care admission: a systematic review. BMC Geriatr 2019;19:217. 10.1186/s12877-019-1210-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Whitehead PJ, Worthington EJ, Parry RH, Walker MF, Drummond AER. Interventions to reduce dependency in personal activities of daily living in community dwelling adults who use homecare services: a systematic review. Clin Rehabil 2015;29:1064-76. 10.1177/0269215514564894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 13. Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. John Wiley & Sons, 2019. 10.1002/9781119536604 . [DOI] [Google Scholar]
- 14. Brignardello-Petersen R, Bonner A, Alexander PE, et al. GRADE Working Group . Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol 2018;93:36-44. 10.1016/j.jclinepi.2017.10.005 [DOI] [PubMed] [Google Scholar]
- 15. Riley RD, Jackson D, Salanti G, et al. Multivariate and network meta-analysis of multiple outcomes and multiple treatments: rationale, concepts, and examples. BMJ 2017;358:j3932. 10.1136/bmj.j3932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brignardello-Petersen R, Guyatt GH, Mustafa RA, et al. GRADE guidelines 33: Addressing imprecision in a network meta-analysis. J Clin Epidemiol 2021;139:49-56. 10.1016/j.jclinepi.2021.07.011 [DOI] [PubMed] [Google Scholar]
- 17. Brignardello-Petersen R, Murad MH, Walter SD, et al. GRADE Working Group . GRADE approach to rate the certainty from a network meta-analysis: avoiding spurious judgments of imprecision in sparse networks. J Clin Epidemiol 2019;105:60-7. 10.1016/j.jclinepi.2018.08.022 [DOI] [PubMed] [Google Scholar]
- 18. Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 2011;64:380-2. 10.1016/j.jclinepi.2010.09.011 [DOI] [PubMed] [Google Scholar]
- 19. Puhan MA, Schünemann HJ, Murad MH, et al. GRADE Working Group . A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014;349:g5630. 10.1136/bmj.g5630 [DOI] [PubMed] [Google Scholar]
- 20. Santesso N, Glenton C, Dahm P, et al. GRADE Working Group . GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol 2020;119:126-35. 10.1016/j.jclinepi.2019.10.014 [DOI] [PubMed] [Google Scholar]
- 21. Yepes-Nuñez JJ, Li S-A, Guyatt G, et al. Development of the summary of findings table for network meta-analysis. J Clin Epidemiol 2019;115:1-13. 10.1016/j.jclinepi.2019.04.018 [DOI] [PubMed] [Google Scholar]
- 22. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777-84. 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- 23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Crocker TF, Clegg A, Riley RD, et al. Community-based complex interventions to sustain independence in older people, stratified by frailty: a protocol for a systematic review and network meta-analysis. BMJ Open 2021;11:e045637. 10.1136/bmjopen-2020-045637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Crocker T, Forster A, Young J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev 2013;(2):CD004294. 10.1002/14651858.CD004294.pub3 [DOI] [PubMed] [Google Scholar]
- 26. Fried LP, Tangen CM, Walston J, et al. Cardiovascular Health Study Collaborative Research Group . Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146-56. 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 27. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 28. Hoffmann TC, Oxman AD, Ioannidis JPA, et al. Enhancing the usability of systematic reviews by improving the consideration and description of interventions. BMJ 2017;358:j2998. 10.1136/bmj.j2998 [DOI] [PubMed] [Google Scholar]
- 29. Crocker TF, Lam N, Jordão M, et al. Risk-of-bias assessment using Cochrane’s revised tool for randomized trials (RoB 2) was useful but challenging and resource-intensive: observations from a systematic review. J Clin Epidemiol 2023;161:39-45. 10.1016/j.jclinepi.2023.06.015 [DOI] [PubMed] [Google Scholar]
- 30. White IR. Network meta-analysis. Stata J 2015;15:951-85 10.1177/1536867X1501500403 . [DOI] [Google Scholar]
- 31. Doi SA, Furuya-Kanamori L, Xu C, et al. The Odds Ratio is “portable” across baseline risk but not the Relative Risk: Time to do away with the log link in binomial regression. J Clin Epidemiol 2022;142:288-93. 10.1016/j.jclinepi.2021.08.003 [DOI] [PubMed] [Google Scholar]
- 32. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342:d549. 10.1136/bmj.d549 [DOI] [PubMed] [Google Scholar]
- 33. Schünemann H, Higgins J, Vist G, et al. Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins J, Thomas J, Chandler J, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. [Google Scholar]
- 34. Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making 2013;33:641-56. 10.1177/0272989X12455847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G. Evaluation of inconsistency in networks of interventions. Int J Epidemiol 2013;42:332-45. 10.1093/ije/dys222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Glenton C, Santesso N, Rosenbaum S, et al. Presenting the results of Cochrane Systematic Reviews to a consumer audience: a qualitative study. Med Decis Making 2010;30:566-77. 10.1177/0272989X10375853 [DOI] [PubMed] [Google Scholar]
- 37. Aluko P, Graybill E, Craig D, et al. Economic evidence. In: Higgins J, Thomas J, Chandler J, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. [Google Scholar]
- 38. Heaven A, Brown L, Foster M, Clegg A. Keeping it credible in cohort multiple Randomised Controlled Trials: the Community Ageing Research 75+ (CARE 75+) study model of patient and public involvement and engagement. Res Involv Engagem 2016;2:30. 10.1186/s40900-016-0044-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Alegría M, Frontera W, Cruz-Gonzalez M, et al. Effectiveness of a Disability Preventive Intervention for Minority and Immigrant Elders: The Positive Minds-Strong Bodies Randomized Clinical Trial. Am J Geriatr Psychiatry 2019;27:1299-313. 10.1016/j.jagp.2019.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Arthanat S. Promoting information communication technology adoption and acceptance for aging-in-place: A randomized controlled trial. J Appl Gerontol 2021;40:471-80. 10.1177/0733464819891045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Auvinen K, Voutilainen A, Jyrkkä J, Lönnroos E, Mäntyselkä P. Interprofessional medication assessment among home care patients: any impact on functioning? Results from a randomised controlled trial. BMC Geriatr 2020;20:390. 10.1186/s12877-020-01796-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Balaban DJ, Goldfarb NI, Perkel RL, Carlson BL. Follow-up study of an urban family medicine home visit program. J Fam Pract 1988;26:307-12. [PubMed] [Google Scholar]
- 43. Barenfeld E, Dahlin-Ivanoff S, Wallin L, Gustafsson S. Promoting aging migrants’ capabilities: A randomized controlled trial concerning activities of daily living and self-rated health. AIMS Public Health 2018;5:173-88. 10.3934/publichealth.2018.2.173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bernabei R, Landi F, Gambassi G, et al. Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ 1998;316:1348-51. 10.1136/bmj.316.7141.1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bleijenberg N, Drubbel I, Schuurmans MJ, et al. Effectiveness of a proactive primary care program on preserving daily functioning of older people: a cluster randomized controlled trial. J Am Geriatr Soc 2016;64:1779-88. 10.1111/jgs.14325 [DOI] [PubMed] [Google Scholar]
- 46. Blom J, den Elzen W, van Houwelingen AH, et al. Effectiveness and cost-effectiveness of a proactive, goal-oriented, integrated care model in general practice for older people. A cluster randomised controlled trial: Integrated Systematic Care for older People--the ISCOPE study. Age Ageing 2016;45:30-41. 10.1093/ageing/afv174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Borrows A, Holland R. Independent living centre occupational therapy (OT) versus routine community OT. Int J Ther Rehabil 2013;20:187-94 10.12968/ijtr.2013.20.4.187 . [DOI] [Google Scholar]
- 48.Botjes E. Methodebeschrijving EigenKrachtWijzer. Databank Effectieve sociale interventies Movisie, 2013.
- 49. Bouman A, van Rossum E, Ambergen T, Kempen G, Knipschild P. Effects of a home visiting program for older people with poor health status: a randomized, clinical trial in The Netherlands. J Am Geriatr Soc 2008;56:397-404. 10.1111/j.1532-5415.2007.01565.x [DOI] [PubMed] [Google Scholar]
- 50. Brettschneider C, Luck T, Fleischer S, et al. Cost-utility analysis of a preventive home visit program for older adults in Germany. BMC Health Serv Res 2015;15:141. 10.1186/s12913-015-0817-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cameron ID, Fairhall N, Langron C, et al. A multifactorial interdisciplinary intervention reduces frailty in older people: randomized trial. BMC Med 2013;11:65. 10.1186/1741-7015-11-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Carpenter GI, Demopoulos GR. Screening the elderly in the community: controlled trial of dependency surveillance using a questionnaire administered by volunteers. BMJ 1990;300:1253-6. 10.1136/bmj.300.6734.1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Cesari M, Demougeot L, Boccalon H, Guyonnet S, Vellas B, Andrieu S. The Multidomain Intervention to preveNt disability in ElDers (MINDED) project: rationale and study design of a pilot study. Contemp Clin Trials 2014;38:145-54. 10.1016/j.cct.2014.04.006 [DOI] [PubMed] [Google Scholar]
- 54. Challis D, Clarkson P, Williamson J, et al. The value of specialist clinical assessment of older people prior to entry to care homes. Age Ageing 2004;33:25-34. 10.1093/ageing/afh007 [DOI] [PubMed] [Google Scholar]
- 55. Clark F, Azen SP, Zemke R, et al. Occupational therapy for independent-living older adults. A randomized controlled trial. JAMA 1997;278:1321-6. 10.1001/jama.1997.03550160041036 [DOI] [PubMed] [Google Scholar]
- 56. Clark F, Jackson J, Carlson M, et al. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: results of the Well Elderly 2 Randomised Controlled Trial. J Epidemiol Community Health 2012;66:782-90. 10.1136/jech.2009.099754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Coleman EA, Grothaus LC, Sandhu N, Wagner EH. Chronic care clinics: a randomized controlled trial of a new model of primary care for frail older adults. J Am Geriatr Soc 1999;47:775-83. 10.1111/j.1532-5415.1999.tb03832.x [DOI] [PubMed] [Google Scholar]
- 58. Counsell SR, Callahan CM, Clark DO, et al. Geriatric care management for low-income seniors: a randomized controlled trial. JAMA 2007;298:2623-33. 10.1001/jama.298.22.2623 [DOI] [PubMed] [Google Scholar]
- 59. Cutchin MP, Coppola S, Talley V, Svihula J, Catellier D, Shank KH. Feasibility and effects of preventive home visits for at-risk older people: design of a randomized controlled trial. BMC Geriatr 2009;9:54. 10.1186/1471-2318-9-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Dalby DM, Sellors JW, Fraser FD, Fraser C, van Ineveld C, Howard M. Effect of preventive home visits by a nurse on the outcomes of frail elderly people in the community: a randomized controlled trial. CMAJ 2000;162:497-500. [PMC free article] [PubMed] [Google Scholar]
- 61. de Craen AJ, Gussekloo J, Blauw GJ, Willems CG, Westendorp RG. Randomised controlled trial of unsolicited occupational therapy in community-dwelling elderly people: the LOTIS trial. PLoS Clin Trials 2006;1:e2. 10.1371/journal.pctr.0010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Dorresteijn TA, Zijlstra GA, Ambergen AW, Delbaere K, Vlaeyen JW, Kempen GI. Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: results of a randomized controlled trial. BMC Geriatr 2016;16:2. 10.1186/s12877-015-0177-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Dupuy L, Froger C, Consel C, Sauzéon H. Everyday functioning benefits from an assisted living platform amongst frail older adults and their caregivers. Front Aging Neurosci 2017;9:302. 10.3389/fnagi.2017.00302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, Rubenstein LZ. An in-home preventive assessment program for independent older adults: a randomized controlled trial. J Am Geriatr Soc 1994;42:630-8. 10.1111/j.1532-5415.1994.tb06862.x [DOI] [PubMed] [Google Scholar]
- 65. Fairhall N, Kurrle SE, Sherrington C, et al. Effectiveness of a multifactorial intervention on preventing development of frailty in pre-frail older people: study protocol for a randomised controlled trial. BMJ Open 2015;5:e007091. 10.1136/bmjopen-2014-007091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Faul AC, Yankeelov PA, Rowan NL, et al. Impact of geriatric assessment and self-management support on community-dwelling older adults with chronic illnesses. J Gerontol Soc Work 2009;52:230-49. 10.1080/01634370802609288 [DOI] [PubMed] [Google Scholar]
- 67. Fernández-Barrés S, García-Barco M, Basora J, Martínez T, Pedret R, Arija V, Project ATDOM-NUT group . The efficacy of a nutrition education intervention to prevent risk of malnutrition for dependent elderly patients receiving Home Care: A randomized controlled trial. Int J Nurs Stud 2017;70:131-41. 10.1016/j.ijnurstu.2017.02.020 [DOI] [PubMed] [Google Scholar]
- 68.Fischer G, Sandholzer H, Perschke-Hartmann C. Final report of the scientific support of “Getting Healthy Elderly (GÄW)”. A prevention project of the AOK Lower Saxony.)[German] (Abschlussbericht der wissenschaftlichen Begleitung von “Gesund Älter Werden (GÄW)“). AOK Niedersachsen, 2009.
- 69. Ford AB, Katz S, Downs TD, Adams M. Results of long-term home nursing: the influence of disability. J Chronic Dis 1971;24:591-6. 10.1016/0021-9681(71)90047-6 [DOI] [PubMed] [Google Scholar]
- 70. Fox PJ, Breuer W, Wright JA. Effects of a health promotion program on sustaining health behaviors in older adults. Am J Prev Med 1997;13:257-64. 10.1016/S0749-3797(18)30172-7 [DOI] [PubMed] [Google Scholar]
- 71. Fristedt S, Nystedt P, Skogar Ö. Mobile geriatric teams - a cost-effective way of improving patient safety and reducing traditional healthcare utilization among the frail elderly? A randomized controlled trial. Clin Interv Aging 2019;14:1911-24. 10.2147/CIA.S208388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Gené Huguet L, Navarro González M, Kostov B, et al. Pre Frail 80: Multifactorial intervention to prevent progression of pre-frailty to frailty in the elderly. J Nutr Health Aging 2018;22:1266-74. 10.1007/s12603-018-1089-2 [DOI] [PubMed] [Google Scholar]
- 73. Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Byers A. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med 2002;347:1068-74. 10.1056/NEJMoa020423 [DOI] [PubMed] [Google Scholar]
- 74. Giné-Garriga M, Sansano-Nadal O, Tully MA, et al. Accelerometer-measured sedentary and physical activity time and their correlates in European older adults: The SITLESS study. J Gerontol A Biol Sci Med Sci 2020;75:1754-62. 10.1093/gerona/glaa016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc 2006;54:809-16. 10.1111/j.1532-5415.2006.00703.x [DOI] [PubMed] [Google Scholar]
- 76. Grimmer K, Luker J, Beaton K, Kumar S, Crockett A, Price K. TRialing individualized interventions to prevent functional decline in at-risk older adults (TRIIFL): study protocol for a randomized controlled trial nested in a longitudinal observational study. Trials 2013;14:266. 10.1186/1745-6215-14-266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Gustafson DH, Sr, Kornfield R, Mares M-L, et al. Effect of an eHealth intervention on older adults’ quality of life and health-related outcomes: a randomized clinical trial. J Gen Intern Med 2022;37:521-30. 10.1007/s11606-021-06888-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Gustafsson S, Eklund K, Wilhelmson K, et al. Long-term outcome for ADL following the health-promoting RCT--elderly persons in the risk zone. Gerontologist 2013;53:654-63. 10.1093/geront/gns121 [DOI] [PubMed] [Google Scholar]
- 79. Hall N, De Beck P, Johnson D, Mackinnon K, Gutman G, Glick N. Randomized trial of a health promotion program for frail elders. Can J Aging 1992;11:72-91 10.1017/S0714980800014537 . [DOI] [Google Scholar]
- 80. Harari D, Iliffe S, Kharicha K, et al. Promotion of health in older people: a randomised controlled trial of health risk appraisal in British general practice. Age Ageing 2008;37:565-71. 10.1093/ageing/afn150 [DOI] [PubMed] [Google Scholar]
- 81. Hattori S, Yoshida T, Okumura Y, Kondo K. Effects of reablement on the independence of community-dwelling older adults with mild disability: A randomized controlled trial. Int J Environ Res Public Health 2019;16:3954. 10.3390/ijerph16203954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Hay WI, van Ineveld C, Browne G, et al. Prospective care of elderly patients in family practice. Is screening effective? Can Fam Physician 1998;44:2677-87. [PMC free article] [PubMed] [Google Scholar]
- 83. Hébert R, Robichaud L, Roy PM, Bravo G, Voyer L. Efficacy of a nurse-led multidimensional preventive programme for older people at risk of functional decline. A randomized controlled trial. Age Ageing 2001;30:147-53. 10.1093/ageing/30.2.147 [DOI] [PubMed] [Google Scholar]
- 84.Henderson MJ. In-home preventive health assessment and telephone case management for over 75s living alone in independent living units: A cluster randomized controlled trial [PhD thesis]. Queensland University of Technology, 2005. [Google Scholar]
- 85. Hendriksen C, Lund E, Strømgård E. Consequences of assessment and intervention among elderly people: a three year randomised controlled trial. Br Med J (Clin Res Ed) 1984;289:1522-4. 10.1136/bmj.289.6457.1522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Hogg W, Lemelin J, Dahrouge S, et al. Randomized controlled trial of anticipatory and preventive multidisciplinary team care: for complex patients in a community-based primary care setting. Can Fam Physician 2009;55:e76-85. [PMC free article] [PubMed] [Google Scholar]
- 87. Holland SK, Greenberg J, Tidwell L, Malone J, Mullan J, Newcomer R. Community-based health coaching, exercise, and health service utilization. J Aging Health 2005;17:697-716. 10.1177/0898264305277959 [DOI] [PubMed] [Google Scholar]
- 88. Howel D, Moffatt S, Haighton C, et al. Does domiciliary welfare rights advice improve health-related quality of life in independent-living, socio-economically disadvantaged people aged ≥60 years? Randomised controlled trial, economic and process evaluations in the North East of England. PLoS One 2019;14:e0209560. 10.1371/journal.pone.0209560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Imhof L, Naef R, Wallhagen MI, Schwarz J, Mahrer-Imhof R. Effects of an advanced practice nurse in-home health consultation program for community-dwelling persons aged 80 and older. J Am Geriatr Soc 2012;60:2223-31. 10.1111/jgs.12026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Jing L, Jin Y, Zhang X, Wang F, Song Y, Xing F. The effect of Baduanjin qigong combined with CBT on physical fitness and psychological health of elderly housebound. Medicine (Baltimore) 2018;97:e13654. 10.1097/MD.0000000000013654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Jitapunkul S. A randomised controlled trial of regular surveillance in Thai elderly using a simple questionnaire administered by non-professional personnel. J Med Assoc Thai 1998;81:352-6. [PubMed] [Google Scholar]
- 92. Kerse N, McLean C, Moyes SA, et al. The cluster-randomized BRIGHT trial: Proactive case finding for community-dwelling older adults. Ann Fam Med 2014;12:514-24. 10.1370/afm.1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. King AII, Parsons M, Robinson E, Jörgensen D. Assessing the impact of a restorative home care service in New Zealand: a cluster randomised controlled trial. Health Soc Care Community 2012;20:365-74. 10.1111/j.1365-2524.2011.01039.x [DOI] [PubMed] [Google Scholar]
- 94. Kono A, Izumi K, Yoshiyuki N, Kanaya Y, Rubenstein LZ. Effects of an updated preventive home visit program based on a systematic structured assessment of care needs for ambulatory frail older adults in Japan: A randomized controlled trial. J Gerontol A Biol Sci Med Sci 2016;71:1631-7. 10.1093/gerona/glw068 [DOI] [PubMed] [Google Scholar]
- 95. Kono A, Kai I, Sakato C, Harker JO, Rubenstein LZ. Effect of preventive home visits for ambulatory housebound elders in Japan: a pilot study. Aging Clin Exp Res 2004;16:293-9. 10.1007/BF03324554 [DOI] [PubMed] [Google Scholar]
- 96. Kono A, Kanaya Y, Fujita T, et al. Effects of a preventive home visit program in ambulatory frail older people: a randomized controlled trial. J Gerontol A Biol Sci Med Sci 2012;67:302-9. 10.1093/gerona/glr176 [DOI] [PubMed] [Google Scholar]
- 97. Kukkonen-Harjula K, Karmeniemi P, Suikkanen S, et al. Long-term home-based physiotherapy for older people with signs of frailty-RCT (NCT02305433) [P-229]. Eur Geriatr Med 2017;8:S105. [Google Scholar]
- 98. Lambotte D, De Donder L, De Roeck EE, et al. Randomized controlled trial to evaluate a prevention program for frail community-dwelling older adults: a D-SCOPE protocol. BMC Geriatr 2018;18:194. 10.1186/s12877-018-0875-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Leung AC, Liu C, Chow NW, Chi I. Cost-Benefit Analysis of a Case Management Project for the Community-Dwelling Frail Elderly in Hong Kong. J Appl Gerontol 2004;23:70-85 10.1177/0733464804263088 . [DOI] [Google Scholar]
- 100. Leveille SG, Wagner EH, Davis C, et al. Preventing disability and managing chronic illness in frail older adults: a randomized trial of a community-based partnership with primary care. J Am Geriatr Soc 1998;46:1191-8. 10.1111/j.1532-5415.1998.tb04533.x [DOI] [PubMed] [Google Scholar]
- 101. Lewin G, De San Miguel K, Knuiman M, et al. A randomised controlled trial of the Home Independence Program, an Australian restorative home-care programme for older adults. Health Soc Care Community 2013;21:69-78. 10.1111/j.1365-2524.2012.01088.x [DOI] [PubMed] [Google Scholar]
- 102. Liddle J, March L, Carfrae B, et al. Can occupational therapy intervention play a part in maintaining independence and quality of life in older people? A randomised controlled trial. Aust N Z J Public Health 1996;20:574-8. 10.1111/j.1467-842X.1996.tb01068.x [DOI] [PubMed] [Google Scholar]
- 103. Liimatta H, Lampela P, Laitinen-Parkkonen P, Pitkala KH. Effects of preventive home visits on health-related quality-of-life and mortality in home-dwelling older adults. Scand J Prim Health Care 2019;37:90-7. 10.1080/02813432.2019.1569372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Loh DA, Hairi NN, Choo WY, et al. MultiComponent Exercise and theRApeutic lifeStyle (CERgAS) intervention to improve physical performance and maintain independent living among urban poor older people--a cluster randomised controlled trial. BMC Geriatr 2015;15:8. 10.1186/s12877-015-0002-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Lood Q, Gustafsson S, Dahlin Ivanoff S. Bridging barriers to health promotion: a feasibility pilot study of the ‘Promoting Aging Migrants’ Capabilities study’. J Eval Clin Pract 2015;21:604-13. 10.1111/jep.12345 [DOI] [PubMed] [Google Scholar]
- 106. Mann J, Thompson F, McDermott R, Esterman A, Strivens E. Impact of an integrated community-based model of care for older people with complex conditions on hospital emergency presentations and admissions: a step-wedged cluster randomized trial. BMC Health Serv Res 2021;21:701. 10.1186/s12913-021-06668-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Mann WC, Ottenbacher KJ, Fraas L, Tomita M, Granger CV. Effectiveness of assistive technology and environmental interventions in maintaining independence and reducing home care costs for the frail elderly. A randomized controlled trial. Arch Fam Med 1999;8:210-7. 10.1001/archfami.8.3.210 [DOI] [PubMed] [Google Scholar]
- 108. Markle-Reid M, Weir R, Browne G, Roberts J, Gafni A, Henderson S. Health promotion for frail older home care clients. J Adv Nurs 2006;54:381-95. 10.1111/j.1365-2648.2006.03817.x [DOI] [PubMed] [Google Scholar]
- 109. Melis RJ, van Eijken MI, Teerenstra S, et al. A randomized study of a multidisciplinary program to intervene on geriatric syndromes in vulnerable older people who live at home (Dutch EASYcare Study). J Gerontol A Biol Sci Med Sci 2008;63:283-90. 10.1093/gerona/63.3.283 [DOI] [PubMed] [Google Scholar]
- 110. Meng H, Friedman B, Wamsley BR, Mukamel D, Eggert GM. Effect of a consumer-directed voucher and a disease-management-health-promotion nurse intervention on home care use. Gerontologist 2005;45:167-76. 10.1093/geront/45.2.167 [DOI] [PubMed] [Google Scholar]
- 111.Messens L, Quinn S, Saez I, Cuidad Mas MJ, Squillace P, Laura AG. Health monitoring and sOcial integration environMent for Supporting WidE ExTension of independent life at HOME (Home Sweet Home): Final Trial Evaluation Report. Zorgbedrijf Antwerpen, 2014.
- 112. Metzelthin SF, van Rossum E, de Witte LP, et al. Effectiveness of interdisciplinary primary care approach to reduce disability in community dwelling frail older people: cluster randomised controlled trial. BMJ 2013;347:f5264. 10.1136/bmj.f5264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Moll van Charante EP, Richard E, Eurelings LS, et al. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): a cluster-randomised controlled trial. Lancet 2016;388:797-805. 10.1016/S0140-6736(16)30950-3 [DOI] [PubMed] [Google Scholar]
- 114. Monteserín Nadal R, Altimir Losada S, Brotons Cuixart C, et al. [Randomized clinical trial on the efficacy of global geriatric assessment in primary care] [Spanish]. Rev Esp Geriatr Gerontol 2008;43:5-12. [DOI] [PubMed] [Google Scholar]
- 115. Morey MC, Ekelund C, Pearson M, et al. Project LIFE: a partnership to increase physical activity in elders with multiple chronic illnesses. J Aging Phys Act 2006;14:324-43. 10.1123/japa.14.3.324 [DOI] [PubMed] [Google Scholar]
- 116. Morey MC, Peterson MJ, Pieper CF, et al. The Veterans Learning to Improve Fitness and Function in Elders Study: a randomized trial of primary care-based physical activity counseling for older men. J Am Geriatr Soc 2009;57:1166-74. 10.1111/j.1532-5415.2009.02301.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Morgan GS, Haase AM, Campbell RM, Ben-Shlomo Y. A pilot randomised controlled trial of physical activity facilitation for older adults: feasibility study findings. Pilot Feasibility Stud 2019;5:40. 10.1186/s40814-019-0414-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Newbury JW, Marley JE, Beilby JJ. A randomised controlled trial of the outcome of health assessment of people aged 75 years and over. Med J Aust 2001;175:104-7. 10.5694/j.1326-5377.2001.tb143541.x [DOI] [PubMed] [Google Scholar]
- 119. Newcomer R, Maravilla V, Faculjak P, Graves MT. Outcomes of preventive case management among high-risk elderly in three medical groups: a randomized clinical trial. Eval Health Prof 2004;27:323-48. 10.1177/0163278704270011 [DOI] [PubMed] [Google Scholar]
- 120. Ng TP, Feng L, Nyunt MS, et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: A randomized controlled trial. Am J Med 2015;128:1225-1236.e1. 10.1016/j.amjmed.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 121. Parsons J, Rouse P, Robinson EM, Sheridan N, Connolly MJ. Goal setting as a feature of homecare services for older people: does it make a difference? Age Ageing 2012;41:24-9. 10.1093/ageing/afr118 [DOI] [PubMed] [Google Scholar]
- 122. Parsons M, Senior H, Kerse N, Chen MH, Jacobs S, Anderson C. Randomised trial of restorative home care for frail older people in New Zealand. Nurs Older People 2017;29:27-33. 10.7748/nop.2017.e897 [DOI] [PubMed] [Google Scholar]
- 123. Parsons M, Senior H, Kerse N, et al. Should care managers for older adults be located in primary care? A randomized controlled trial. J Am Geriatr Soc 2012;60:86-92. 10.1111/j.1532-5415.2011.03763.x [DOI] [PubMed] [Google Scholar]
- 124. Pathy MS, Bayer A, Harding K, Dibble A. Randomised trial of case finding and surveillance of elderly people at home. Lancet 1992;340:890-3. 10.1016/0140-6736(92)93294-W [DOI] [PubMed] [Google Scholar]
- 125. Phelan EA, Balderson B, Levine M, et al. Delivering effective primary care to older adults: a randomized, controlled trial of the senior resource team at group health cooperative. J Am Geriatr Soc 2007;55:1748-56. 10.1111/j.1532-5415.2007.01416.x [DOI] [PubMed] [Google Scholar]
- 126. Ploeg J, Brazil K, Hutchison B, et al. Effect of preventive primary care outreach on health related quality of life among older adults at risk of functional decline: randomised controlled trial. BMJ 2010;340:c1480. 10.1136/bmj.c1480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Pröfener F, Anders J, Dapp U, Minder CE, Golgert S, von Renteln-Kruse W. [Acceptance of preventive home visits among frail elderly persons : Participants an non-participants in a Follow-up after 2 and 4 years within the LUCAS longitudinal study] [German]. Z Gerontol Geriatr 2016;49:596-605. [DOI] [PubMed] [Google Scholar]
- 128. Rockwood K, Stadnyk K, Carver D, et al. A clinimetric evaluation of specialized geriatric care for rural dwelling, frail older people. J Am Geriatr Soc 2000;48:1080-5. 10.1111/j.1532-5415.2000.tb04783.x [DOI] [PubMed] [Google Scholar]
- 129. Romera-Liebana L, Orfila F, Segura JM, et al. Effects of a primary care-based multifactorial intervention on physical and cognitive function in frail, elderly individuals: A randomized controlled trial. J Gerontol A Biol Sci Med Sci 2018;73:1688-1674. 10.1093/gerona/glx259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Rooijackers TH, Kempen GIJM, Zijlstra GAR, et al. Effectiveness of a reablement training program for homecare staff on older adults’ sedentary behavior: A cluster randomized controlled trial. J Am Geriatr Soc 2021;69:2566-78. 10.1111/jgs.17286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Rubenstein LZ, Alessi CA, Josephson KR, Trinidad Hoyl M, Harker JO, Pietruszka FM. A randomized trial of a screening, case finding, and referral system for older veterans in primary care. J Am Geriatr Soc 2007;55:166-74. 10.1111/j.1532-5415.2007.01044.x [DOI] [PubMed] [Google Scholar]
- 132. Ryvicker M, Feldman PH, Rosati RJ, Sobolewski S, Maduro GA, Jr, Schwartz T. Improving functional outcomes in home care patients: impact and challenges of disseminating a quality improvement initiative. J Healthc Qual 2011;33:28-36. 10.1111/j.1945-1474.2011.00156.x [DOI] [PubMed] [Google Scholar]
- 133. Serra-Prat M, Sist X, Domenich R, et al. Effectiveness of an intervention to prevent frailty in pre-frail community-dwelling older people consulting in primary care: a randomised controlled trial. Age Ageing 2017;46:401-7. 10.1093/ageing/afw242 [DOI] [PubMed] [Google Scholar]
- 134. Shapiro A, Taylor M. Effects of a community-based early intervention program on the subjective well-being, institutionalization, and mortality of low-income elders. Gerontologist 2002;42:334-41. 10.1093/geront/42.3.334 [DOI] [PubMed] [Google Scholar]
- 135. Sherman H, Söderhielm-Blid S, Forsberg C, Karp A, Törnkvist L. Effects of preventive home visits by district nurses on self-reported health of 75-year-olds. Prim Health Care Res Dev 2016;17:56-71. 10.1017/S1463423614000565 [DOI] [PubMed] [Google Scholar]
- 136. Siemonsma PC, Blom JW, Hofstetter H, et al. The effectiveness of functional task exercise and physical therapy as prevention of functional decline in community dwelling older people with complex health problems. BMC Geriatr 2018;18:164. 10.1186/s12877-018-0859-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Stewart S, Harvey I, Poland F, Lloyd-Smith W, Mugford M, Flood C. Are occupational therapists more effective than social workers when assessing frail older people? Results of CAMELOT, a randomised controlled trial. Age Ageing 2005;34:41-6. 10.1093/ageing/afh230 [DOI] [PubMed] [Google Scholar]
- 138. Stuck AE, Aronow HU, Steiner A, et al. A trial of annual in-home comprehensive geriatric assessments for elderly people living in the community. N Engl J Med 1995;333:1184-9. 10.1056/NEJM199511023331805 [DOI] [PubMed] [Google Scholar]
- 139. Stuck AE, Minder CE, Peter-Wüest I, et al. A randomized trial of in-home visits for disability prevention in community-dwelling older people at low and high risk for nursing home admission. Arch Intern Med 2000;160:977-86. 10.1001/archinte.160.7.977 [DOI] [PubMed] [Google Scholar]
- 140. Stuck AE, Moser A, Morf U, et al. Effect of health risk assessment and counselling on health behaviour and survival in older people: a pragmatic randomised trial. PLoS Med 2015;12:e1001889. 10.1371/journal.pmed.1001889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Suijker JJ, van Rijn M, Buurman BM, Ter Riet G, Moll van Charante EP, de Rooij SE. Effects of nurse-led multifactorial care to prevent disability in community-living older people: Cluster randomized trial. PLoS One 2016;11:e0158714. 10.1371/journal.pone.0158714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Szanton SL, Thorpe RJ, Boyd C, et al. Community aging in place, advancing better living for elders: a bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled older adults. J Am Geriatr Soc 2011;59:2314-20. 10.1111/j.1532-5415.2011.03698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Szanton SL, Xue QL, Leff B, et al. Effect of a biobehavioral environmental approach on disability among low-income older adults: A randomized clinical trial. JAMA Intern Med 2019;179:204-11. 10.1001/jamainternmed.2018.6026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Takahashi PY, Pecina JL, Upatising B, et al. A randomized controlled trial of telemonitoring in older adults with multiple health issues to prevent hospitalizations and emergency department visits. Arch Intern Med 2012;172:773-9. 10.1001/archinternmed.2012.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Teut M, Schnabel K, Baur R, et al. Effects and feasibility of an Integrative Medicine program for geriatric patients-a cluster-randomized pilot study. Clin Interv Aging 2013;8:953-61. 10.2147/CIA.S45242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Thiel C, Braun T, Grüneberg C. [Physical training as core component of multimodal treatment of older frail people-study protocol of a randomized controlled pilot study]. Z Gerontol Geriatr 2019;52:45-60. 10.1007/s00391-018-1443-3 [DOI] [PubMed] [Google Scholar]
- 147. Thomas R, Worrall G, Elgar F, Knight J. Can they keep going on their own? A four-year randomized trial of functional assessments of community residents. Can J Aging 2007;26:379-90. 10.3138/cja.26.4.379 [DOI] [PubMed] [Google Scholar]
- 148. Tomita MR, Mann WC, Stanton K, Tomita AD, Sundar V. Use of currently available smart home technology by frail elders: process and outcomes. Top Geriatr Rehabil 2007;23:24-34 10.1097/00013614-200701000-00005 . [DOI] [Google Scholar]
- 149. Tulloch AJ, Moore V. A randomized controlled trial of geriatric screening and surveillance in general practice. J R Coll Gen Pract 1979;29:733-40. [PMC free article] [PubMed] [Google Scholar]
- 150. Tuntland H, Aaslund MK, Espehaug B, Førland O, Kjeken I. Reablement in community-dwelling older adults: a randomised controlled trial. BMC Geriatr 2015;15:145. 10.1186/s12877-015-0142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. van der Pols-Vijlbrief R, Wijnhoven HAH, Bosmans JE, Twisk JWR, Visser M. Targeting the underlying causes of undernutrition. Cost-effectiveness of a multifactorial personalized intervention in community-dwelling older adults: A randomized controlled trial. Clin Nutr 2017;36:1498-508. 10.1016/j.clnu.2016.09.030 [DOI] [PubMed] [Google Scholar]
- 152. van Dongen EJI, Haveman-Nies A, Doets EL, Dorhout BG, de Groot LCPGM. Effectiveness of a diet and resistance exercise intervention on muscle health in older adults: ProMuscle in Practice. J Am Med Dir Assoc 2020;21:1065-1072.e3. 10.1016/j.jamda.2019.11.026 [DOI] [PubMed] [Google Scholar]
- 153. van Heuvelen MJ, Hochstenbach JB, Brouwer WH, et al. Differences between participants and non-participants in an RCT on physical activity and psychological interventions for older persons. Aging Clin Exp Res 2005;17:236-45. 10.1007/BF03324603 [DOI] [PubMed] [Google Scholar]
- 154. van Hout HP, Jansen AP, van Marwijk HW, Pronk M, Frijters DF, Nijpels G. Prevention of adverse health trajectories in a vulnerable elderly population through nurse home visits: a randomized controlled trial [ISRCTN05358495]. J Gerontol A Biol Sci Med Sci 2010;65:734-42. 10.1093/gerona/glq037 [DOI] [PubMed] [Google Scholar]
- 155. van Leeuwen KM, Bosmans JE, Jansen AP, et al. Cost-effectiveness of a chronic care model for frail older adults in primary care: Economic evaluation alongside a stepped-wedge cluster-randomized trial. J Am Geriatr Soc 2015;63:2494-504. 10.1111/jgs.13834 [DOI] [PubMed] [Google Scholar]
- 156. van Lieshout MRJ, Bleijenberg N, Schuurmans MJ, de Wit NJ. The effectiveness of a PRoactive multicomponent intervention program on disability in independently living older people: A randomized controlled trial. J Nutr Health Aging 2018;22:1051-9. 10.1007/s12603-018-1101-x [DOI] [PubMed] [Google Scholar]
- 157. van Rossum E, Frederiks CM, Philipsen H, Portengen K, Wiskerke J, Knipschild P. Effects of preventive home visits to elderly people. BMJ 1993;307:27-32. 10.1136/bmj.307.6895.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Vass M, Avlund K, Lauridsen J, Hendriksen C. Feasible model for prevention of functional decline in older people: municipality-randomized, controlled trial. J Am Geriatr Soc 2005;53:563-8. 10.1111/j.1532-5415.2005.53201.x [DOI] [PubMed] [Google Scholar]
- 159. Vetter NJ, Jones DA, Victor CR. Effect of health visitors working with elderly patients in general practice: a randomised controlled trial. Br Med J (Clin Res Ed) 1984;288:369-72. 10.1136/bmj.288.6414.369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. von Bonsdorff MB, Leinonen R, Kujala UM, et al. Effect of physical activity counseling on disability in older people: a 2-year randomized controlled trial. J Am Geriatr Soc 2008;56:2188-94. 10.1111/j.1532-5415.2008.02000.x [DOI] [PubMed] [Google Scholar]
- 161. Wallace JI, Buchner DM, Grothaus L, et al. Implementation and effectiveness of a community-based health promotion program for older adults. J Gerontol A Biol Sci Med Sci 1998;53:M301-6. 10.1093/gerona/53A.4.M301 [DOI] [PubMed] [Google Scholar]
- 162. Walters K, Frost R, Kharicha K, et al. Home-based health promotion for older people with mild frailty: the HomeHealth intervention development and feasibility RCT. Health Technol Assess 2017;21:1-128. 10.3310/hta21730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Whitehead PJ, Walker MF, Parry RH, Latif Z, McGeorge ID, Drummond AE. Occupational Therapy in HomEcare Re-ablement Services (OTHERS): results of a feasibility randomised controlled trial. BMJ Open 2016;6:e011868. 10.1136/bmjopen-2016-011868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Williams EI, Greenwell J, Groom LM. The care of people over 75 years old after discharge from hospital: an evaluation of timetabled visiting by Health Visitor Assistants. J Public Health Med 1992;14:138-44. [PubMed] [Google Scholar]
- 165. Wolter A, Stolle C, Roth G, Rothgang H. [Does the resident care assessment instrument improve long-term home care? - results of a nation-wide study in Germany] [German]. Gesundheitswesen 2013;75:29-32. [DOI] [PubMed] [Google Scholar]
- 166. Wong AKC, Wong FKY, Chang K. Effectiveness of a community-based self-care promoting program for community-dwelling older adults: a randomized controlled trial. Age Ageing 2019;48:852-8. 10.1093/ageing/afz095 [DOI] [PubMed] [Google Scholar]
- 167. Yamada Y, Ikegami N. Preventive home visits for community- dwelling frail elderly people based on minimum data set-home care: randomized controlled trial. Geriatr Gerontol Int 2003;3:236-42 10.1111/j.1444-1586.2003.00103.x . [DOI] [Google Scholar]
- 168. Di Pollina L, Guessous I, Petoud V, et al. Integrated care at home reduces unnecessary hospitalizations of community-dwelling frail older adults: a prospective controlled trial. BMC Geriatr 2017;17:53. 10.1186/s12877-017-0449-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Byles JE, Tavener M, O’Connell RL, et al. Randomised controlled trial of health assessments for older Australian veterans and war widows. Med J Aust 2004;181:186-90. 10.5694/j.1326-5377.2004.tb06233.x [DOI] [PubMed] [Google Scholar]
- 170. Bloomfield K, Wu Z, Broad JB, et al. Learning from a multidisciplinary randomized controlled intervention in retirement village residents. J Am Geriatr Soc 2022;70:743-53. 10.1111/jgs.17533 [DOI] [PubMed] [Google Scholar]
- 171. Teh R, Barnett D, Edlin R, et al. Effectiveness of a complex intervention of group-based nutrition and physical activity to prevent frailty in pre-frail older adults (SUPER): a randomised controlled trial. Lancet Healthy Longev 2022;3:e519-30. 10.1016/S2666-7568(22)00124-6 [DOI] [PubMed] [Google Scholar]
- 172. Shlisky J, Bloom DE, Beaudreault AR, et al. Nutritional Considerations for Healthy Aging and Reduction in Age-Related Chronic Disease. Adv Nutr 2017;8:17-26. 10.3945/an.116.013474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.UK Chief Medical Officers. UK Chief Medical Officers' physical activity guidelines. 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf.
- 174. Tuffaha HW, Gordon LG, Scuffham PA. Value of information analysis in healthcare: a review of principles and applications. J Med Econ 2014;17:377-83. 10.3111/13696998.2014.907170 [DOI] [PubMed] [Google Scholar]
- 175. Clegg A, Bandeen-Roche K, Farrin A, et al. New horizons in evidence-based care for older people: individual participant data meta-analysis. Age Ageing 2022;51:afac090. 10.1093/ageing/afac090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Crocker TF, Lam N, Ensor J, et al. Community-based complex interventions to sustain independence in older people, stratified by frailty: a systematic review and network meta-analysis. Health Technol Assess [forthcoming]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Appendix 1-13
Data Availability Statement
The data associated with this paper will be openly available indefinitely upon publication under a Creative Commons attribution license from the University of Leeds Data Repository. Summary effect estimates and findings from network meta-analyses: https://doi.org/10.5518/1377; risk of bias judgments: https://doi.org/10.5518/1386.