Advance care planning (ACP) was initially narrowly defined as documentation of life-sustaining treatment (LST). One initial goal was to curb unwanted LSTs and costs.1 Yet, a focus solely on legal documentation of LST preferences has resulted in mixed data on goal-concordant care and healthcare utilization.2–4 Fortunately, the conceptualization of ACP continues to evolve, and is now widely recognized as a process of preparing patients (people) and surrogate decision-makers for communication and medical decision-making.5,6 This process involves a complex array of patient, surrogate, and clinician behaviors, health systems workflows, interventions, communities, and policy.
ACP is rooted in what quality of life means to people.4,5,7 However, antiquated narrow definitions of ACP as a one-time checkbox or code status persist, resulting in heterogeneous research, clinical, and policy initiatives.2,4 To address this heterogeneity, a modified Delphi panel defined ACP in 2017 as “a process that supports adults at any age or stage of health in understanding and sharing their personal values, life goals, and preferences regarding future medical care.”7 As the field has evolved, this definition focused on “future decisions” has proven to be too narrow as it does not include the preparation of patients and surrogates for decision-making over the life course or address public perceptions of ACP.8–10
The use of non-standardized and potentially inappropriate ACP outcomes in research also makes it difficult to evaluate ACP’s effectiveness.4,11 Goal-concordant care has been considered the “gold standard,” but there is a lack of validated or standardized measures.12–15 Because patient preferences may change, reliance on retrospective chart review to assess goal concordance may be inaccurate,13,14 and there is a growing consensus that surrogate outcomes should be one key focus of ACP research.6 Additionally, ACP is unlikely to affect some outcomes such as quality of life, which may be impacted by other factors such as symptom burden, available support, and so forth, or healthcare utilization, which is not patient-centered and affected by lack of healthcare access, systemic injustice, and other issues.12,16
Furthermore, the unique needs of historically marginalized populations are not well represented in prior definitions and outcomes identification. Rates of ACP are much lower (<20%) among racially or ethnically minoritized populations and those with limited health literacy.17–19 Disparities in ACP also persist for lesbian, gay, bisexual, transgender, queer, intersexual, asexual, homeless, and incarcerated populations.20,21 Reasons may include lack of access to healthcare, experiential discrimination, well-founded mistrust,22,23 and culturally diverse views on autonomy and decision-making,24,25 making it preferable for many to begin care planning discussions in their communities. Diverse communities, as well as interdisciplinary clinicians and community-based experts, have not been included in prior efforts to define ACP and ACP outcomes.
EVOLUTION OF ACP CLINICAL CARE TO CARE PLANNING
To evolve, we must reconceptualize ACP as a holistic process over the life course that includes both in-the-moment and advanced decisions at every life stage. We propose a new framework that reflects the updated focus on preparation for communication and medical decision-making and conceptualizes ACP as part of the continuum of care planning. Building on recent editorials and reviews from the healthcare and serious illness perspective and calls to rename ACP,3,11,26,27 Figure 1 illustrates a broad care planning framework from the perspective of patients, surrogates, caregivers, and the community across the life course.
FIGURE 1.
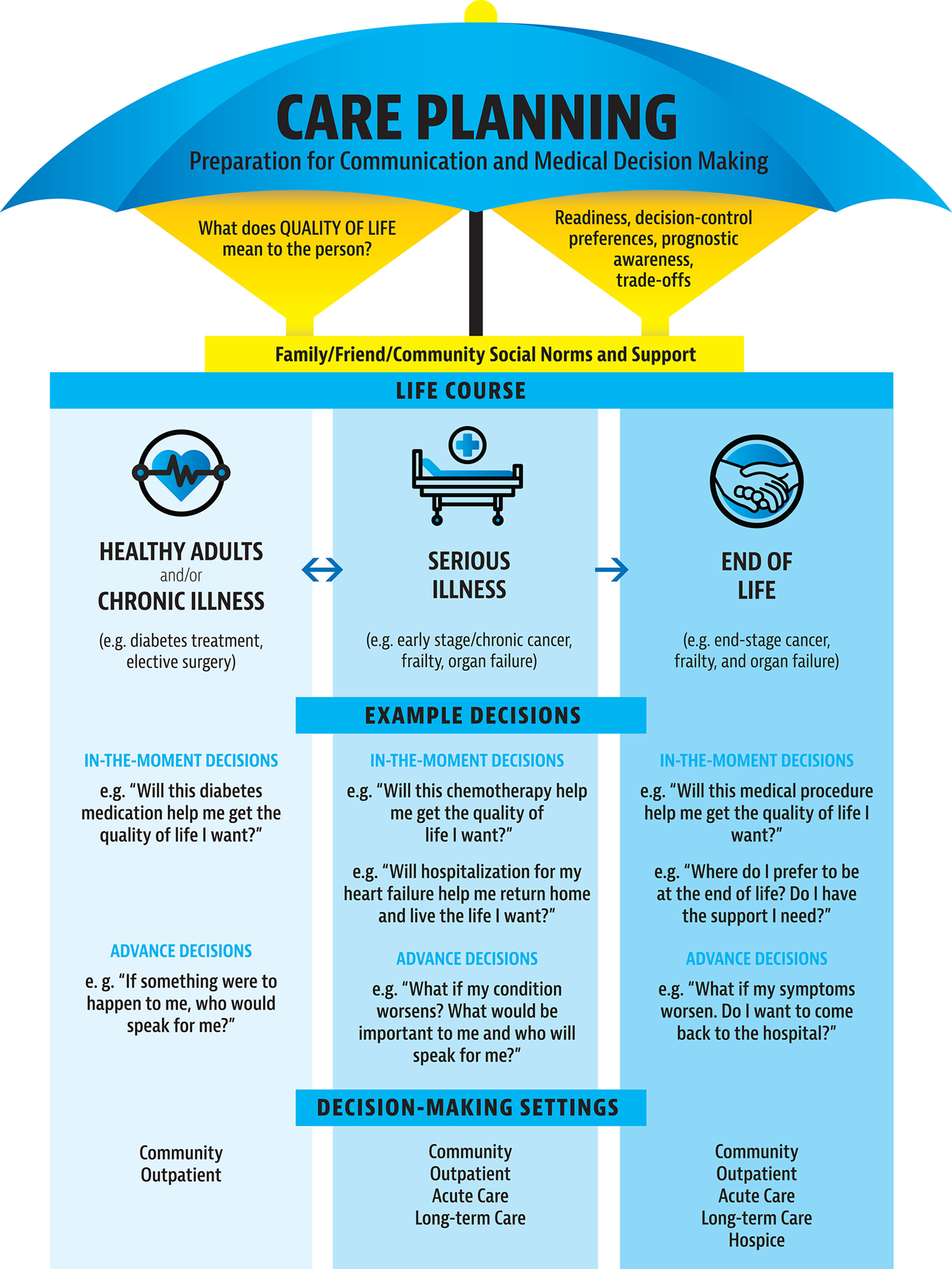
The care planning umbrella model.
We propose a new framework that reflects the updated focus on preparation for communication and medical decision-making and conceptualizes ACP as part of the continuum of care planning.
The overarching construct under the “Care Planning Umbrella” focuses on preparation for communication and medical decision-making,5 with quality of life and what brings meaning and purpose as the fundamental cornerstone. Underneath this broader umbrella are multiple steps, behaviors, people, clinical and community workflows, and decisions—some of which are in-the-moment and some in advance. Care planning is shaped by the person’s (or surrogate’s) perceptions of quality of life; understanding that these constructs are dynamic and evolve over time.28 It is also shaped by an individual’s readiness, preferences for control over decision-making, illness understanding, prognostic awareness, and views of acceptable/unacceptable tradeoffs.5 All care planning is also influenced by family and caregiver support, community social norms, accessible resources, and current policy.
The Care Planning Umbrella also spans the life course as people move between healthy/chronic illness, serious illness, and the end of life. They face different types of decisions (e.g., diabetes medication regimen for chronically ill, chemotherapy for seriously ill, hospice at end of life), and receive care in different settings (e.g., community, outpatient, acute care, long-term care, hospice).5,29 Care planning must be tailored to the individual’s life course, the decisions they are facing, and based on what quality of life means to the person at that time. For example, although surrogate designation and the integration of quality of life into medical decision-making is appropriate at every life stage, the appropriateness of integrating prognostic awareness and tradeoffs will vary (Figure 1).30,31 At all life stages, some decisions may be in-the-moment (e.g., diabetes treatment, chemotherapy, end-of-life procedures) and some may be in advance (e.g., designation of a surrogate, care setting preferences). Over the life course, the lines between in-the-moment and advanced decisions may be fluid.3,30,31
Furthermore, some people, even early in the life course, may have strong and enduring preferences about their future medical care based on personal experiences and beliefs. Those individuals should be given the opportunity to discuss and document those preferences while educating them and their surrogate decision-makers that their preferences may change over time and should be revisited.
EVOLUTION OF ACP RESEARCH TO INCLUDE IMPLEMENTATION SCIENCE AND HUMAN FACTORS ENGINEERING
The onus is on our field to disentangle the complexity of ACP (i.e., care planning) as patients and caregivers desire ACP and studies show ACP decreases surrogate distress.4 Based on recent consensus, more clinically meaningful outcomes from the patient and caregiver perspective may include surrogate burden and distress; feeling heard and understood; and satisfaction with care, communication, and decision-making.4,6 In addition, implementation science and human factors engineering can be used to help care planning achieve its next step in the evolutionary process.
Implementation science offers tools to understand complex processes, including determining the strategies and outcomes that meet the needs of culturally diverse patients and their families.32 System-level strategic approaches that consider organizational and community factors are preferred over examination of individual components (e.g., individual interventions or clinicians).2,4,33–35 The recently updated Consolidated Framework for Implementation Research (CFIR) is a well-established framework for implementing evidence-based interventions in real-world settings.36,37 CFIR provides a guide for systematically identifying implementation factors that determine whether ACP (i.e., care planning) programs or tools succeed or fail. CFIR also recognizes that barriers may arise at any level or setting and can be used to identify strategies to overcome barriers. CFIR consists of five, interrelated domains that can guide care planning research (see Table 1 and Supplemental figure [Appendix S1]): Outer Setting (e.g., cultural/social norms, systemic racism, policies and laws, health information exchanges, quality metrics, reimbursement, etc.); Inner Setting (e.g., healthcare system readiness and workflows, policies, incentives, EMR infrastructure); Individuals (e.g., disease trajectory; cultural backgrounds; experiential racism and mistrust influenced by Capacity, Opportunity, and Motivation (COM-B)38); Innovation (e.g., design for patients and caregivers: educational modalities; documentation; community navigators; community events, medical-legal partnerships, etc. and clinicians and staff: clinician training protocols; conversation guides; electronic medical record (EMR) templates, etc.); and Implementation Process39,40 (e.g., degree to which there is collaboration across leadership, multidisciplinary teams, settings; organizational champions; clinician buy-in; process to identify appropriate populations; messaging and marketing, and quality improvement, etc.).
TABLE 1.
Application of the Consolidated Framework for Implementation Science 2.0 to advance care planning.
| ADVANCE CARE PLANNING INNOVATION |
|---|
| ● Advance care planning (ACP) design: How assembled and presented For patients and caregivers: – Education modalities: written, video, online, group visits, narratives – Media, EMR patient portals, and other outreach materials and technologies – Legal forms, for example, advance directives & POLST – Healthcare and community-based navigators, dedicated ACP teams – Community events and engagement – Medical-legal partnerships For clinicians and staff: – Training materials and protocols – Conversation guides – Health record ACP templates ● Other important considerations: reliable source, evidence base, relative advantages, adaptability, trialability, complexity, cost |
| OUTER SETTING |
| ● Critical incidents: for example, pandemics ● Local attitudes: Community and cultural/societal norms about ACP; systemic and structural racism ● Local conditions: State politics and policies; available ACP EHR infrastructure; health information exchanges, emergency response systems ● Partnerships: Professional organizations, insurers, and health systems ● Policies and Laws: Legislation on AD/POLST, guidelines, accreditation ● Financing: CMS/insurance reimbursement, granting agencies ● Societal Pressure: Media campaigns, advocacy groups ● Market Pressure: Competing health systems to offer ACP ● Performance Measurement Pressure: Quality metrics |
| INNER SETTING |
| ● Structural characteristics ○ Physical space, staff, clinical time for ACP ○ EMR IT infrastructure for ACP documentation, storage, and retrieval ○ Defined ACP policies, workflows, roles/responsibilities ● Relational Connections/Communication ○ Between leadership, disciplines, clinical settings, the community ● Culture ○ Health system readiness to implement ACP ○ Support for patient-centered care ○ Anti-racism policies and practices ○ Learning-centeredness and use of data for ACP quality improvement ● Mission alignment with current workflows, systems, and priorities ● Available resources (e.g., ACP reimbursement rates, incentives, materials, training) |
| INDIVIDUALS |
| ● Leaders: Key decision-makers about ACP policies (e.g., executive leadership, supervisors) ● Opinion leaders and key informants (e.g., community, patient, caregiver advisory boards) ● Implementation Facilitators/Leads/Team Members (e.g., clinical champions, community collaborators) ● Innovation deliverer (e.g., interdisciplinary clinicians, setting, beliefs, attitudes, training) ● Innovation recipient (e.g., patients, caregivers, clinicians): Based on the Capability, Opportunity, Motivation (COM-B) Model for Behavior Change ○ Health literacy, language proficiency, digital literacy, cognitive impairment ○ Access to understandable health education materials and training ○ Patient and caregiver readiness to engage in ACP ○ Type of illness (e.g., cancer, frailty, organ failure) ○ Life and/or disease trajectory ○ Unique and differing cultural and family backgrounds and experiences ○ Experiential racism and justified mistrust in the health system |
| IMPLEMENTATION PROCESS |
| ● Teaming: Coordinating and collaborating with key individuals across disciplines and settings, securing resources, standardized workflows and roles and responsibilities to deliver the ACP innovation ● Assessing Needs: Collecting priorities, preferences of ACP innovation recipients and deliverers (e.g., patient/caregiver qualitative input, obtaining clinician buy-in, etc.) ● Assessing Context: Barriers and facilitators to ACP ● Tailoring Strategies: To address barriers and facilitators to ACP ● Engaging: Attract and encourage participation through appropriate ACP messaging and marketing ● Doing: Cycles of quality improvement and/or trials to optimize ACP delivery (e.g., creating processes to identify appropriate populations, etc.) ● Reflecting and Evaluating: Qualitative and quantitative information about the ACP innovation and implementation from patients, caregivers, clinicians ● Adapting: Modify the ACP innovation or the inner setting for optimal fit and integration of ACP innovation into workflows |
Human factors engineering methods are applied to understand how people engage in complex processes to improve system design and outcomes and can play a role in understanding and improving care planning.41 Process mapping can be used to visualize relevant care planning workflows and tasks of diverse parties (e.g., interdisciplinary clinicians, patients, surrogates, community members, faith leaders, attorneys, etc.) using multiple, iterative steps. Integrating process mapping and the CFIR model can ensure a complete understanding of the systems and processes involved. Care planning will likely require multiple process maps to fully reflect the complexity of diverse parties, settings, patients’ stage on the life course, and components and factors necessary for patient-centered care.
THE INCLUSION OF DIVERSE COMMUNITIES AND EXPERTS
Care planning implementation requires a broad range of community partners that extends well beyond the healthcare setting to where people live in their communities. As others have shown, community outreach and patient- or community-facing implementation strategies are needed, in addition to training clinicians for goals of care conversations.42 Future efforts to define care planning and appropriate outcomes will need to include representatives from diverse communities, interdisciplinary clinicians (e.g., nurses, social workers, chaplains, healthcare navigators) and other experts (e.g., community health workers, faith-based and community leaders, attorneys).
CONCLUSION
ACP has evolved over the past several decades to a continuum of care planning focused on preparing people and their surrogate decision-makers for communication and medical decision-making, and it is still evolving. To get to the next level of ACP for clinical care and research, we must reconceptualize care planning as a holistic, ongoing process over the life course that includes both tailored in-the-moment and advanced decisions at every life stage. We suggest the need for a systems-level approach using evidenced-based methods of implementation science and human factors engineering and the inclusion of diverse communities and interdisciplinary experts to develop and evaluate processes to support the continuum of care planning in real-world settings.
Supplementary Material
ACKNOWLEDGMENTS
Thank you to graphic artist Kaylee Stewart for helping us communicate our ideas visually.
FUNDING INFORMATION
This work was unfunded. Dr. Sudore is funded in part by the National Institute on Aging, National Institutes of Health (K24AG054415). Dr. Savoy is supported by a Career Development Award from the National Institutes of Health (K01AG076971).
National Institute on Aging; National Institutes of Health, Grant/Award Numbers: K01AG076971, K24AG054415
Footnotes
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
Appendix S1. Application of the consolidated framework for implementation research to advance care planning.
SPONSOR’S ROLE
This work was unfunded and the content is solely the responsibility of the authors.
REFERENCES
- 1.Fagerlin A, Enough SCE. The failure of the living will. Hast Cent Rep 2004;34(2):30–42. [PubMed] [Google Scholar]
- 2.Jimenez G, Tan WS, Virk AK, Low CK, Car J, Ho AHY. Overview of systematic reviews of advance care planning: summary of evidence and global lessons. J Pain Symptom Manag 2018; 56(3):436–459 e425. [DOI] [PubMed] [Google Scholar]
- 3.Smith AK. Should we still believe in advance care planning? J Am Geriatr Soc 2022;70(5):1358–1360. [DOI] [PubMed] [Google Scholar]
- 4.McMahan RD, Tellez I, Sudore RL. Deconstructing the complexities of advance care planning outcomes: what do we know and where do we go? A scoping review. J Am Geriatr Soc 2021;69(1):234–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med 2010;153(4):256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried TR. Giving up on the objective of providing goal-concordant care: advance care planning for improving caregiver outcomes. J Am Geriatr Soc 2022;70(10):3006–3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sudore RL, Lum HD, You JJ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manag 2017;53(5):821–832 e821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McMahan RD, Knight SJ, Fried TR, Sudore RL. Advance care planning beyond advance directives: perspectives from patients and surrogates. J Pain Symptom Manag 2013;46(3):355–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morrison RS, Meier DE, Arnold RM. What’s wrong with advance care planning? JAMA 2021;326(16):1575–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant MS, Back AL, Dettmar NS. Public perceptions of advance care planning, palliative care, and hospice: a scoping review. J Palliat Med 2021;24(1):46–52. [DOI] [PubMed] [Google Scholar]
- 11.Rosa WE, Izumi S, Sullivan DR, et al. Advance care planning in serious illness: a narrative review. J Pain Symptom Manag 2022;65(1):E63–E78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sudore RL, Heyland DK, Lum HD, et al. Outcomes that define successful advance care planning: a Delphi panel consensus. J Pain Symptom Manag 2018;55(2):245–255 e248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanders JJ, Curtis JR, Tulsky JA. Achieving goal-concordant care: a conceptual model and approach to measuring serious illness communication and its impact. J Palliat Med 2018; 21(S2):S17–S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halpern SD. Goal-concordant care - searching for the holy grail. N Engl J Med 2019;381(17):1603–1606. [DOI] [PubMed] [Google Scholar]
- 15.Unroe KT, Hickman SE, Torke AM, Group ARCW. Care consistency with documented care preferences: methodologic considerations for implementing the “measuring what matters” quality indicator. J Pain Symptom Manag 2016;52(4):453–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perkins HS. Controlling death: the false promise of advance directives. Ann Intern Med 2007;147(1):51–57. [DOI] [PubMed] [Google Scholar]
- 17.Harrison KL, Adrion ER, Ritchie CS, Sudore RL, Smith AK. Low completion and disparities in advance care planning activities among older Medicare beneficiaries. JAMA Intern Med 2016;176(12):1872–1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudore RL, Landefeld CS, Barnes DE, et al. An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Couns 2007;69(1–3):165–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rao JK, Anderson LA, Lin FC, Laux JP. Completion of advance directives among U.S. consumers. Am J Prev Med 2014;46(1): 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes M, Cartwright C. Lesbian, gay, bisexual and transgender people’s attitudes to end-of-life decision-making and advance care planning. Australas J Ageing 2015;34(Suppl 2): 39–43. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan LM, Sudore RL, Arellano Cuervo I, Bainto D, Olsen P, Kushel M. Barriers and solutions to advance care planning among homeless-experienced older adults. J Palliat Med 2020; 23(10):1300–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Welch LC, Teno JM, Mor V. End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc 2005;53(7):1145–1153. [DOI] [PubMed] [Google Scholar]
- 23.Rhodes R, Teno JM. What’s race got to do with it? J Clin Oncol 2009;27(33):5496–5498. [DOI] [PubMed] [Google Scholar]
- 24.Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist 2005;45(5):634–641. [DOI] [PubMed] [Google Scholar]
- 25.Singh JA, Sloan JA, Atherton PJ, et al. Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the control preferences scale. Am J Manag Care 2010;16(9):688–696. [PMC free article] [PubMed] [Google Scholar]
- 26.Heyland DK. Advance care planning (ACP) vs. advance serious illness preparations and planning (ASIPP). Healthcare (Basel) 2020;8(3):218. doi: 10.3390/healthcare8030218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacobsen J, Bernacki R, Paladino J. Shifting to serious illness communication. JAMA 2022;327(4):321–322. [DOI] [PubMed] [Google Scholar]
- 28.Auriemma CL, Nguyen CA, Bronheim R, et al. Stability of end-of-life preferences: a systematic review of the evidence. JAMA Intern Med 2014;174(7):1085–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tinetti ME, Naik AD, Dodson JA. Moving from disease-centered to patient goals-directed Care for Patients with Multiple Chronic Conditions: patient value-based care. JAMA Cardiol 2016;1(1):9–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sinuff T, Dodek P, You JJ, et al. Improving end-of-life communication and decision making: the development of a conceptual framework and quality indicators. J Pain Symptom Manag 2015;49(6):1070–1080. [DOI] [PubMed] [Google Scholar]
- 31.Tinetti ME, Costello DM, Naik AD, et al. Outcome goals and health care preferences of older adults with multiple chronic conditions. JAMA Netw Open 2021;4(3):e211271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: unifying the discipline to improve the public health. Clin Psychol Sci 2014;2(1):22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Auret K, Sinclair C, Averill B, Evans S. Advance care planning and end-of-life care in a network of rural Western Australian hospitals. Aust J Rural Health 2015;23(4):195–200. [DOI] [PubMed] [Google Scholar]
- 34.Fassbender K, Biondo P, Holroyd-Leduc J, et al. Identification and operationalisation of indicators to monitor successful uptake of advance care planning policies: a modified Delphi study. BMJ Support Palliat Care 2021;12:e329–e336. [DOI] [PubMed] [Google Scholar]
- 35.Palmer JA, Parker VA, Mor V, et al. Barriers and facilitators to implementing a pragmatic trial to improve advance care planning in the nursing home setting. BMC Health Serv Res 2019;19(1):527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci 2022;17:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 23(6):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013;56(11): 1669–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Powell BJ, McMillen JC, Proctor EK, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev 2012;69(2):123–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci 2015;10(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Biondo PD, King S, Minhas B, et al. How to increase public participation in advance care planning: findings from a world cafe to elicit community group perspectives. BMC Public Health 2019;19(1):679. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


