Abstract
Very little is known about the mechanisms underlying the development of personality pathology, hindering efforts to address early risk for these costly and stigmatized disorders. In this study, we examined associations between social and monetary reward processing, measured at the neurophysiological level, and personality pathology, operationalized through the Level of Personality Functioning (LPF), in a sample of early adolescent females (Mage=12.21 years old, SD=1.21). Female youth with (n=80) and without (n=30) a mental health history completed laboratory tasks assessing social and monetary reward responsiveness using electroencephalogram (EEG) and completed ratings of personality pathology. Commonly co-occurring psychopathology, including depression, anxiety, attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and conduct disorder (CD) were also assessed. At the bivariate level, significant associations did not emerge between psychopathology and reward processing variables. When covarying symptoms of depression, anxiety, ADHD, ODD, and CD, an enhanced reward positivity (RewP) component to social reward feedback (accounting for response to social rejection) was associated with higher levels of personality impairment. Results were specific to social rather than monetary reward processing. Depression, anxiety, and ODD also explained unique variance in LPF. These findings suggest that alterations in social reward processing may be a key marker for early emerging personality pathology. Future work examining the role of social reward processing on the development of LPF across adolescence may guide efforts to prevent the profound social dysfunction associated with personality pathology.
Keywords: personality pathology, event-related potentials, electroencephalogram, reward processing
Personality disorders are complex and debilitating disorders associated with profound social dysfunction, suicide, and costly and long-term mental health care (Bender et al., 2001; Bohus et al., 2021). Although traditionally diagnosed in adulthood, particularly among women (Goodman et al., 2010; Sansone & Sansone, 2011), early adolescence is a sensitive period in the development of personality pathology. Common childhood disorders, such as anxiety, depression, attention-deficit/hyperactivity disorder, and conduct problems, precede personality pathology, and remain comorbid across development (Sharp & Wall, 2018; Stepp et al., 2016), although personality pathology contributes to long-term dysfunction beyond the effects of these more commonly identified childhood mental health concerns (Wertz et al., 2019). Personality pathology can be reliably assessed in early adolescence, and predicts the development of personality disorders across the lifespan (Sharp et al., 2011, 2014; Shiner & Allen, 2013). Dimensional assessment offers notable advantages for identifying emerging personality pathology in early adolescents who may not yet meet full diagnostic criteria for a personality disorder (Sharp & Wall, 2021; Shiner & Allen, 2013). The level of personality functioning (LPF) is a dimensional assessment of personality included in the newly adopted criteria for the International Classification of Disorders, 11th Edition, and the DSM-5’s Alternative Model for Personality Disorders. LPF refers to dysfunction in self and interpersonal functioning, and represents the transdiagnostic core of all personality disorders (American Psychiatric Association, 2013; Sharp & Wall, 2021). LPF has demonstrated strong reliability and construct validity in adults and adolescents (Kerr et al., 2022; Weekers et al., 2021; Zimmermann et al., 2022). Yet, very little is known about the mechanisms underlying LPF, missing critical early opportunities to target youth at risk for some of the most stigmatized and costly conditions.
The NIMH RDoC Social Processes domain is highly relevant to probing mechanisms underlying LPF in youth (Hepp et al., 2023; Koudys et al., 2019). Difficulties processing social rejection and acceptance cues likely underlie difficulties developing and maintaining rewarding, flexible, and enduring relationships (Runions et al., 2020; Skabeikyte-Norkiene et al., 2022) among youth with personality pathology. However, extant research has relied primarily on self-report methodology to measure social processing (Runions et al., 2020), which is limited because youth with personality problems may lack insight into their difficulties, and social processing is posited to be a mostly automatic process (Crick & Dodge, 1994). Although sensitivity to rejection cues has long been considered relevant to the development and maintenance of personality pathology (Domsalla et al., 2014; Lazarus et al., 2014), similar deficits are also identified across other disorders (Gao et al., 2017), and it is not clear that sensitivity to rejection cues is a unique correlate of personality pathology. Instead, emerging fMRI studies show that personality pathology is uniquely associated with enhanced reactivity to inclusion feedback in the dorsomedial prefrontal cortex (Domsalla et al., 2014; Malejko et al., 2019), a region implicated in several cognitive functions, including emotional conflict monitoring and self-referential mentalizing about social knowledge. While this enhanced reactivity is speculated to reflect a conflict between the desire to be socially accepted and the internal belief of those with personality pathology that others will reject them (Malejko et al., 2019), fMRI methods lack temporal sensitivity, leaving questions about the specific nature of social acceptance processing deficits and how they unfold across time. Prominent models of social processing posit that social information is processed in a set of stages with early stages, including encoding and interpreting social cues, influencing later stages of social processing, such as selecting and enacting behavioral responses to social cues (e.g., Crick & Dodge, 1994). Event-related potentials (ERPs) derived from the electroencephalogram (EEG) provide excellent temporal resolution (Kappenman & Luck, 2016) and are ideal for assessing dysfunction in the most immediate stages of social processing that guide subsequent behavior (Crick & Dodge, 1994).
We have recently examined ERPs associated with processing social acceptance and rejection in an unselected sample of undergraduate students with borderline personality pathology, measured dimensionally (Babinski, Pegg, West, Arfer, & Kujawa, 2023). As borderline personality disorder is the only personality disorder that appears to represent the general factor common to all personality disorders (Clark et al., 2018; Sharp et al., 2015), it is likely relevant for examining social processing deficits related to LPF in youth. Young adult participants completed a laboratory-based interaction task which has been shown to reliably elicit ERPs sensitive to rejection and acceptance feedback (Kujawa et al., 2014a, 2017). In the task, participants play a game with simulated peers, in which they vote to reject and accept co-players, while also receiving rejection and acceptance feedback from peers. Borderline personality pathology was not associated with alterations in processing social rejection cues, although an enhanced reward positivity (RewP) component emerged for acceptance compared to rejection feedback among young adults with higher levels of personality pathology when considering depression and anxiety as covariates (Babinski et al., 2023). RewP is a frontocentral ERP component appearing approximately 300 ms after stimuli onset as a relative positivity to reward versus loss or neutral feedback that reflects reward-related brain activation (Proudfit, 2015). RewP has been correlated with self-report and behavioral measures of reward responsiveness (Bress & Hajcak, 2013) and may reflect individual differences in approach motivation and reward sensitivity.
As the RewP is reliably assessed across development (Ethridge & Weinberg, 2018), these findings showing altered neurophysiological processing of social reward in emerging adults may be relevant to emerging personality pathology in youth. However, reward dysfunction, considered part of the NIMH RDoC Positive Valence System and typically measured using monetary reward paradigms, has also been associated with personality pathology (Crowell & Kaufman, 2016; Stewart et al., 2019). Specifically, reduced responsiveness to monetary rewards, indicated by a blunted RewP as well as a lack of differentiation in RewP to monetary win versus loss, has been associated with personality pathology in later adolescents and adults (Endrass et al., 2016; Stewart et al., 2019). As similar dysfunction has been reported across other diagnoses (Zald & Treadway, 2017), it is important to determine the extent to which alterations in monetary reward processing are unique to emerging personality pathology and the extent to which examination of responses in the social reward domain offers unique information on mechanisms of personality pathology. Extant literature suggests that LPF may be differentially associated with alterations in social and monetary reward processing, but these two domains have not directly been compared in their relevance to LPF in youth.
The goal of this study was to examine associations between neurophysiological processing of social and monetary reward and LPF in a sample of early adolescent females. The focus was on female youth as personality disorders are disproportionately identified among female patients in mental health care (Goodman et al., 2010; Sansone & Sansone, 2011). As LPF commonly occurs with other symptoms, such as depression, anxiety, ADHD, ODD, and CD (Sharp & Wall, 2021; Kerr et al., 2022) and these co-occurring symptoms are also associated with altered reward processing (e.g., Babinski et al., 2019; Hill et al., 2023), associations between neural processing and LPF were tested accounting for these other symptoms. It is unclear why only some youth with these co-occuring psychiatric symptoms develop impairments in LPF, and it may be that additional variance in LPF can be accounted for by atypical neural processing of reward. It was hypothesized that an enhanced RewP to social acceptance would be associated with LPF, while a blunted RewP to monetary reward would be associated with LPF. Additionally, it was hypothesized that associations would persist when considering other psychopathology (i.e., depression, anxiety, ADHD, ODD, and CD) as covariates.
Methods
Participants were 110 female youth between the ages of 10 and 14 years old (Mage=12.21, SD=1.21) recruited from local clinics, mailing lists, and social media advertisements. Consent and assent were obtained before study participation. Most youth participated with their mothers (88.18%), while 9.10% participated with their fathers and 2.27% participated with their grandmothers. Youth were oversampled for mental health problems (n=80), based on parent-report on the computerized Kiddie Schedule for Affective Disorders and Schizophrenia (Townsend et al., 2020) or youth endorsement of suicidal thoughts or behaviors on the clinician-administered Self-Injurious Thoughts and Behaviors Interview (Nock et al., 2007). A smaller portion of the sample (n=30) was recruited without a history of mental health concerns. In the full sample, lifetime diagnoses were as follows: 11.82% mood disorder (i.e., major depressive disorder, persistent depressive disorder, and/or disruptive mood dysregulation disorder), 45.45% anxiety disorder (i.e., panic disorder, agoraphobia, separation anxiety, social anxiety disorder, generalized anxiety disorder, and/or obsessive-compulsive disorder), 11.82% ADHD, 26.36% ODD, and 6.36 CD; 33.64% of youth reported suicidal thoughts or behaviors. Youth were permitted to use psychiatric medication (14.55%) at the time of the laboratory visit. Twenty-four (21.82%) were attending therapy with a psychologist or therapist. Youth were required to have an IQ≥80, assessed by the Wechsler Abbreviated Scale of Intelligence, Second Edition (Wechsler, 2011). Intellectual, developmental, or psychotic disorders were exclusionary. The sample identified as White (87.27%), Black and/or African American (2.73%), Asian (1.82%), and other or more than one race (8.18%); 8.18% identified as Hispanic and/or Latino.
Measures
LPF.
Youth completed the Level of Personality Functioning Scale Brief Form 2.0 (LPF-BF 2.0; Weekers et al., 2018). The LPFS-BF 2.0 includes 12 items rated on a 4-point Likert scale from 1 (Completely untrue) to 4 (Completely true). Items reflect impairments in self-functioning, including identity disturbance (e.g., “I often do not know who I really am,”) and self-direction (e.g., “I have no sense of where I want to go in my life”), and interpersonal functioning, including empathy (e.g., “I often find it hard to stand when others have a different opinion”) and intimacy (e.g., “I often feel very vulnerable when relations become more personal”). A total score was computed with excellent internal consistency (Cronbach’s α = 0.907).
ADHD, ODD, and CD Symptoms.
The Disruptive Behavior Disorders Rating Scale is a caregiver-report questionnaire comprised of 45 items evaluating symptoms of ADHD, ODD, and CD corresponding to the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (Fosco et al., 2023). Each item is rated using a 4-point Likert scale that ranges from 0 (Not at all) to 3 (Very much). ADHD, ODD, and CD severity scores were calculated by averaging symptom items for each construct. The psychometric properties of the DBD are well supported (Fosco et al., 2023; Pelham et al., 1992). Internal consistency severity scores were excellent for ADHD (Cronbach’s α = .927) and ODD (Cronbach’s α = .900) and good for CD (Cronbach’s α = .811).
Depression.
The Short Mood and Feelings Questionnaire is a youth self-report questionnaire that consists of 13 items assessing depressive symptoms. The severity of symptoms for the past two weeks is rated on a 3-point scale from 0 (Not true) to 2 (True). This measure has strong psychometric properties to the longer measure (Messer et al., 1995). Internal consistency in the present sample (Cronbach’s α = .907) was excellent.
Anxiety.
The Screen for Child Anxiety Related Disorders is a 41-item self-report questionnaire (Birmaher et al., 1999) that assesses the severity of anxiety in the past three months. Items are rated on a Likert scale from 0 (Not true or hardly ever true) to 2 (True or often true) and totaled. In this sample, internal consistency (Cronbach’s α = .929) was excellent.
Social Reward Task.
The Island Getaway Task assessed neurophysiological responses to social acceptance and rejection cues (Kujawa, Kessel, Carroll, Arfer, & Klein, 2017; Kujawa et al., 2014a). This task reliably elicits a RewP in response to social acceptance cues. Participants were told they would be playing a game with 11 age-matched co-players in which they would be traveling in the Hawaiian Islands, and at each island they have to vote whether they wanted each peer to continue in the game and then receive feedback on how each peer voted for them. There were 11 co-players so that including the participant, the total number of players was even and 50% male/50% female. In the first round, participants created a profile with their photograph and background information, and reviewed profiles of computerized peers. In the subsequent five rounds, participants responded to a poll question (e.g., “If you could have a superpower, what would it be?”) and reviewed coplayer responses. Following a review of profiles and poll responses in each round, participants completed a voting and feedback phase. Participants were prompted to vote to accept (“Keep”) or reject (“Kick out”) each co-player, and after each vote, they saw feedback indicating whether that co-player had voted to accept or reject them. Acceptance feedback was indicated by a green “thumbs up” and rejection feedback was indicated by a red “thumbs down.” Each voting trial began with a peer profile presented until participants voted. To simulate variation in co-player response speed, a peer voting time was selected for each trial based on actual variability in participants’ voting speeds. If participants voted faster than the simulated voting time for that co-player, the message “Waiting for [co-player’s name] to vote…” was displayed. Lastly, a fixation “+” was presented for 1000 ms, followed by feedback displayed for 2000 ms. A blank screen was presented for 1500 ms before the start of the next trial. The task included a total of 51 feedback trials split evenly between acceptance and rejection, with the last trial type determined randomly. After each round, participants were informed that another player had been sent home, and after completing the sixth, participants were told that they made it to the “Big Island” and were in the winning group. A questionnaire was presented at the end of the task, including four items assessing positive affect and four items assessing negative affect during the task rated from 1 (Not at all) to 5 (Extremely).1
Monetary Reward Task.
In the monetary reward task (Bress & Hajcak, 2013; Kujawa et al., 2014b), participants were told they could win up to $5 and completed practice trials before beginning the task. This has task been shown to reliably elicit an enhanced RewP to win versus loss feedback (Bress & Hajcak, 2013; Kujawa et al., 2014b). The task consisted of 60 trials. At the beginning of each trial, participants were presented with an image of two doors and instructed to choose one door by clicking the left or right mouse button. The doors remained on the screen until the participant responded. Next, a fixation mark (+) appeared for 1000 ms, and feedback was presented on the screen for 1500 ms. Participants were told that they could either win $0.50 or lose $0.25 on each trial (for up to $5 total). A win was indicated by a green “↑,” and a loss was indicated by a red “↓.” Finally, a fixation mark appeared again and was followed by the message “Click for the next round,” which remained on the screen until the participant responded and the next trial began. Across the task, 30 win and 30 loss trials were presented in random order. Participants received $5 after completing the task. Participants were debriefed about the deception involved in both tasks at the end of the study visit.
EEG data acquisition
A 32-channel BrainProducts actiCHamp system (Munich, Germany) was used to collect continuous EEG data. Due to an administration error, social reward task EEG data was lost from one participant, but data from the monetary reward task was available for all 110 participants. Facial electrodes were attached 1 cm above and below the right eye and 1 cm on each outer corner of the eyes to measure electrooculogram. Bipolar electrodes were referenced to an electrode placed on the back of the neck of the participant, per the BrainProducts bipolar-to-auxiliary adapter design. The sampling rate was 1000 Hz, impedances were lowered below 30 kΩ, and online data acquisition was referenced to Cz. BrainVision Analyzer (Munich, Germany) was used to process collected data. A band-pass filter with cutoffs of 0.1 and 30 Hz was used, and data were re-referenced offline to linked mastoids TP9 and TP10.
Ocular correction was completed using Gratton’s algorithm (Gratton et al., 1983). In most cases, facial EOG electrodes were used for ocular correction; however in some cases, noisy EOG data required use of scalp electrodes instead.2 Semiautomatic artifact rejection was completed with a voltage step greater than 50 μV/ms between sample points, maximum voltage difference of 175 μV within 400 ms intervals, a minimal allowed amplitude of −200 μV and maximal allowed amplitude of 200 μV, and lowest allowed activity of 0.5 μV within 100 ms intervals. Data were visually inspected to remove any remaining artifacts. Single electrodes with faulty recordings were interpolated using the signal from surrounding electrodes. For three participants (one in the social reward task, two in the monetary reward task) with poor data from one of the mastoid electrodes (TP9/TP10), data were interpolated at one or both mastoids before mastoid re-reference2. Data were averaged by type of feedback (acceptance and rejection, or win and loss), and baseline corrected −200 to 0 ms before feedback onset. Participants had on average 24.88 (SD = 1.42) trials for the acceptance condition and 24.81 (SD = 1.36) for the rejection condition, and 29.69 (SD = 0.70) trials in the win and 29.72 (SD = 0.80) trials in the loss conditions at Cz following artifact rejection. Consistent with prior work showing a later peak for the social RewP (Kujawa et al., 2017) relative to the monetary RewP (Kujawa et al., 2018) as well as visual inspection of the grand averages in this study for the full sample (Figure 1), RewP was scored 275–375 ms after feedback onset at Cz in the social reward task (e.g., Hill et al., 2023; Kujawa et al., 2017) and 250–350 ms after feedback onset at Cz in the monetary reward task (Dickey et al., 2023; Pegg et al., 2020).3 Spearman-Brown coefficients for split-half reliability for RewP to acceptance and rejection feedback were 0.80 and 0.83, respectively, and 0.86 for both RewP to win and loss feedback.
Figure 1.
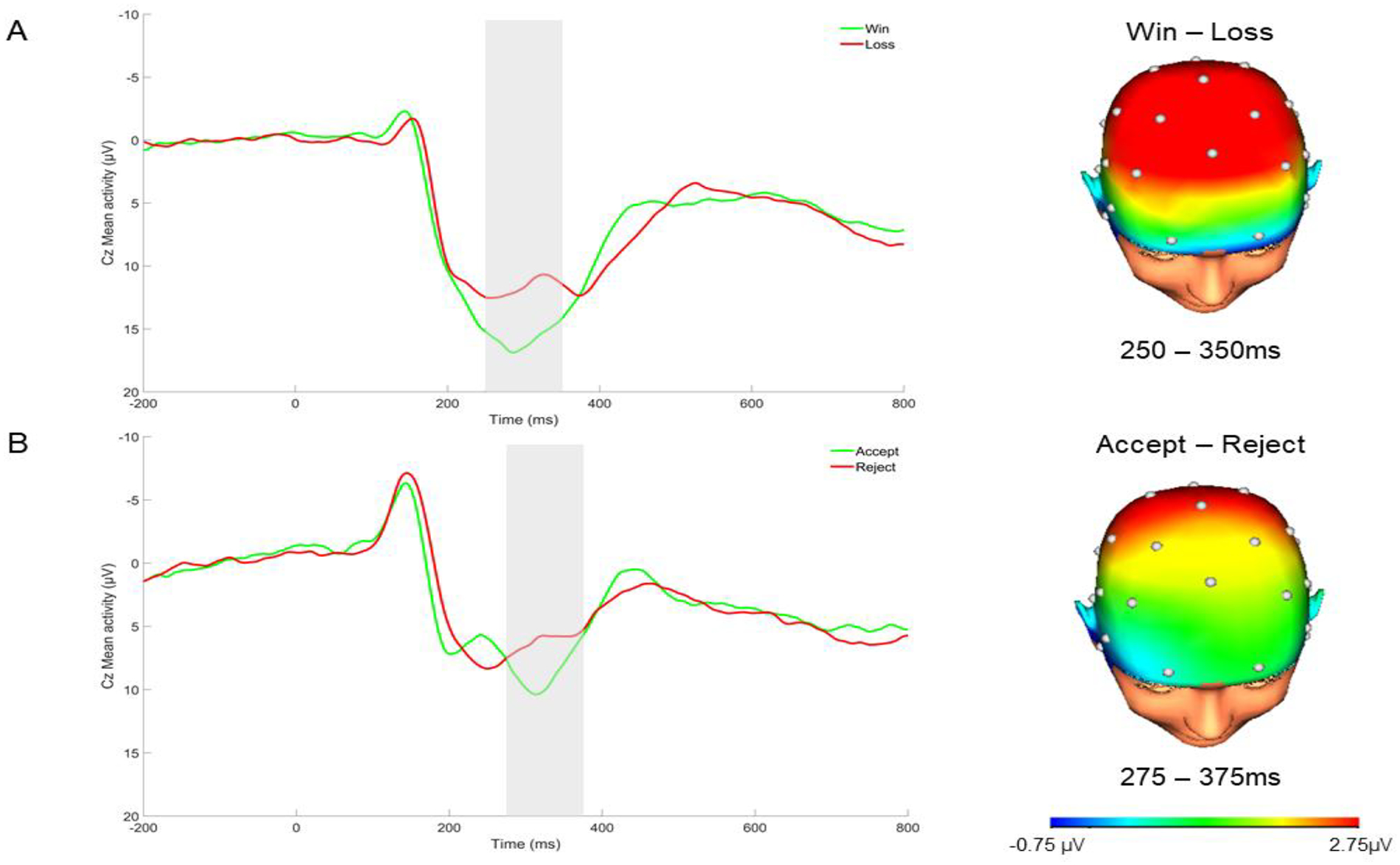
ERP Waveform and Scalp Distributions Depicting Neural Responses to Monetary (A) and Social (B) Feedback in the Full Sample
Note. ERP waveform is at Cz. The 250–350 ms time window is highlighted in the ERP waveform representing the RewP in the monetary reward task (A), while the 275–375 time window is highlighted in the ERP waveform representing the RewP in the social reward task (B). Negative values are plotted up. Scalp distributions reference the respective RewP time window identified for each task.
Data Analytic Plan
First, bivariate correlations were computed to examine associations between LPF, depression, anxiety, ADHD, ODD, CD, and reward processing variables. Specifically, RewP to acceptance, RewP to rejection, RewP to win, and RewP to loss were considered. Additionally, to isolate the variance in the ERP wave attributed to social and monetary reward, unstandardized residual scores for RewP to acceptance and RewP to win were computed by partialing out the variance associated with RewP for the rejection and loss conditions, respectively (Meyer et al., 2017), and these residual scores were used to test bivariate associations with psychopathology. Second, to examine the unique effects of neural variables on LPF, accounting for co-occurring psychopathology, a regression model was computed. Depression, anxiety, ADHD, ODD, and CD, as well as RewP to acceptance, rejection, monetary loss, and monetary win were included as independent variables in the model and LPF was the dependent variable. Standardized regression coefficients are presented as an estimate of effect size to demonstrate the relative strength of associations and their practical meaning (Nieminen et al., 2013), with 0.10, 0.30, and 0.50 consistent with small, medium, and large effects, respectively (Cohen, 1988).
Results
At the bivariate level (Table 1), LPF was associated with depression, anxiety, ADHD, ODD, and CD. Significant correlations did not emerge between RewP in any of the monetary or social feedback conditions and LPF. Positive and significant associations emerged between RewP to social acceptance, rejection, monetary loss, and monetary win.
Table 1.
Bivariate Correlations between Study Variables
| M(SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. RewP to social reward | 8.71 (8.78) | -- | |||||||||||
| 2. RewP to social rejection | 6.13 (8.80) | .797** | -- | ||||||||||
| 3. Social RewP residual | 0.00 (5.30) | .604** | .000 | -- | |||||||||
| 4. RewP to monetary reward | 15.79 (8.02) | .626** | .578** | .274** | -- | ||||||||
| 5. RewP to monetary loss | 11.65 (8.06) | .668** | .673** | .218* | .828** | -- | |||||||
| 6. Monetary RewP residual | 0.00 (4.49) | .130 | .037 | .166+ | .560** | .000 | -- | ||||||
| 7. LPF | 20.84 (7.23) | −.013 | −.110 | .123 | −.100 | −.090 | −.046 | -- | |||||
| 8. Depression | 6.18 (5.64) | −.092 | −.134 | .024 | −.155 | −.164+ | −.034 | .799** | -- | ||||
| 9. Anxiety | 29.69 (14.59) | −.105 | −.128 | −.004 | −.161+ | −.153 | −.061 | .767** | .716** | -- | |||
| 10. ADHD | 0.59 (0.56) | .010 | −.004 | .023 | −.109 | −.060 | −.105 | .217** | .382** | .181+ | -- | ||
| 11. ODD | 0.65 (0.60) | .037 | .043 | .005 | −.088 | −.059 | −.070 | .191* | .264** | .066 | .692** | -- | |
| 12. CD | 0.08 (0.17) | .076 | .009 | .114 | −.064 | .002 | −.117 | .230** | .323** | .249** | .590** | .661** | -- |
Note.
p < .01,
p < .05,
p<.10 level (2-tailed).
Unstandardized social RewP residual was calculated adjusting for RewP to rejection. Unstandardized monetary RewP residual was calculated adjusting for RewP to monetary loss.
Regression analysis complied with the assumptions of linearity, homoscedasticity, normality, and independence. The distribution of standardized LPF regression residuals is presented in Figure 2. The Durbin-Watson statistics (1.90) indicated that the residuals were independent. Variable inflation factor (VIF) scores were below 4.0 for all independent variables.
Figure 2.
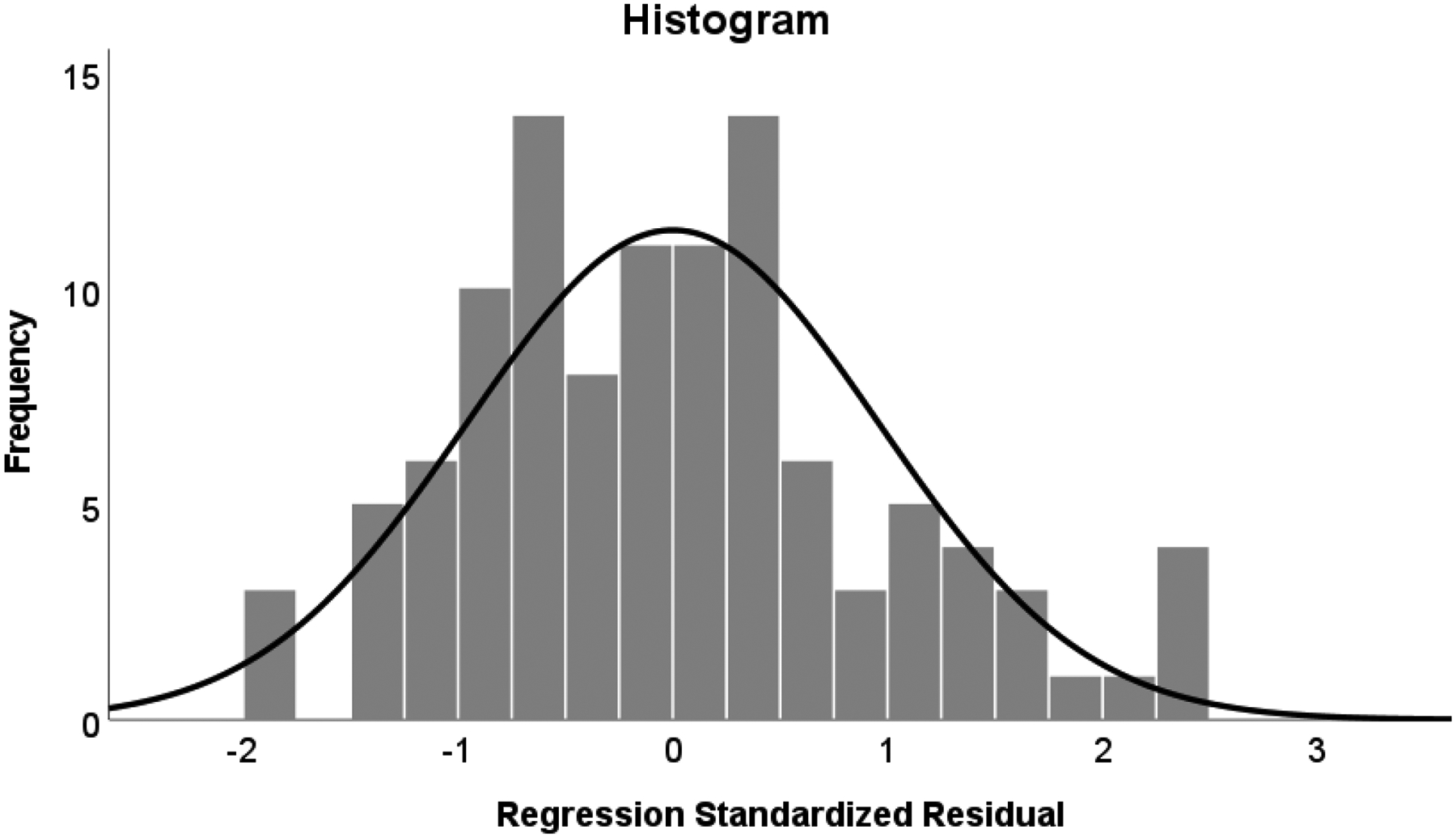
Distribution of standardized LPF regression residuals
The omnibus test for the regression analysis (Table 2) was significant, F(9,108)=32.620, p<.001, R2=.748. Significant associations with LPF persisted for ODD, depression, and anxiety. Additionally, RewP in both social conditions was associated with LPF. Specifically, an enhanced RewP to social acceptance feedback was associated with greater LPF, as was a more negative RewP to social rejection feedback. This pattern of results indicates greater differentiation in neural responses to social acceptance versus rejection feedback in LPF (Figure 3). A scatterplot of the association between residual RewP to social acceptance and residual LPF is depicted in Figure 4. Exploratory regression analyses also including age and use of psychotropic medication were considered, but the same pattern of significant effects persisted.
Table 2.
Regression Analyses Testing Unique Associations between RewP to Social and Monetary Feedback and LPF (dependent variable) considering co-ocurring psychopathology
| Variables | B | SE B | St. β | p |
|---|---|---|---|---|
| ADHD | −1.832 | .973 | −.142 | .063 |
| ODD | 2.42 | .965 | .203 | .014 |
| CD | −4.866 | 3.078 | −.115 | .117 |
| Anxiety | .212 | .037 | .427 | <.001 |
| Depression | .680 | .100 | .531 | <.001 |
| RewP to win | −.053 | .083 | −.059 | .526 |
| RewP to loss | .102 | .090 | .114 | .262 |
| RewP to acceptance | .161 | .074 | .196 | .032 |
| RewP to rejection | −.157 | .074 | −.191 | .036 |
Figure 3.
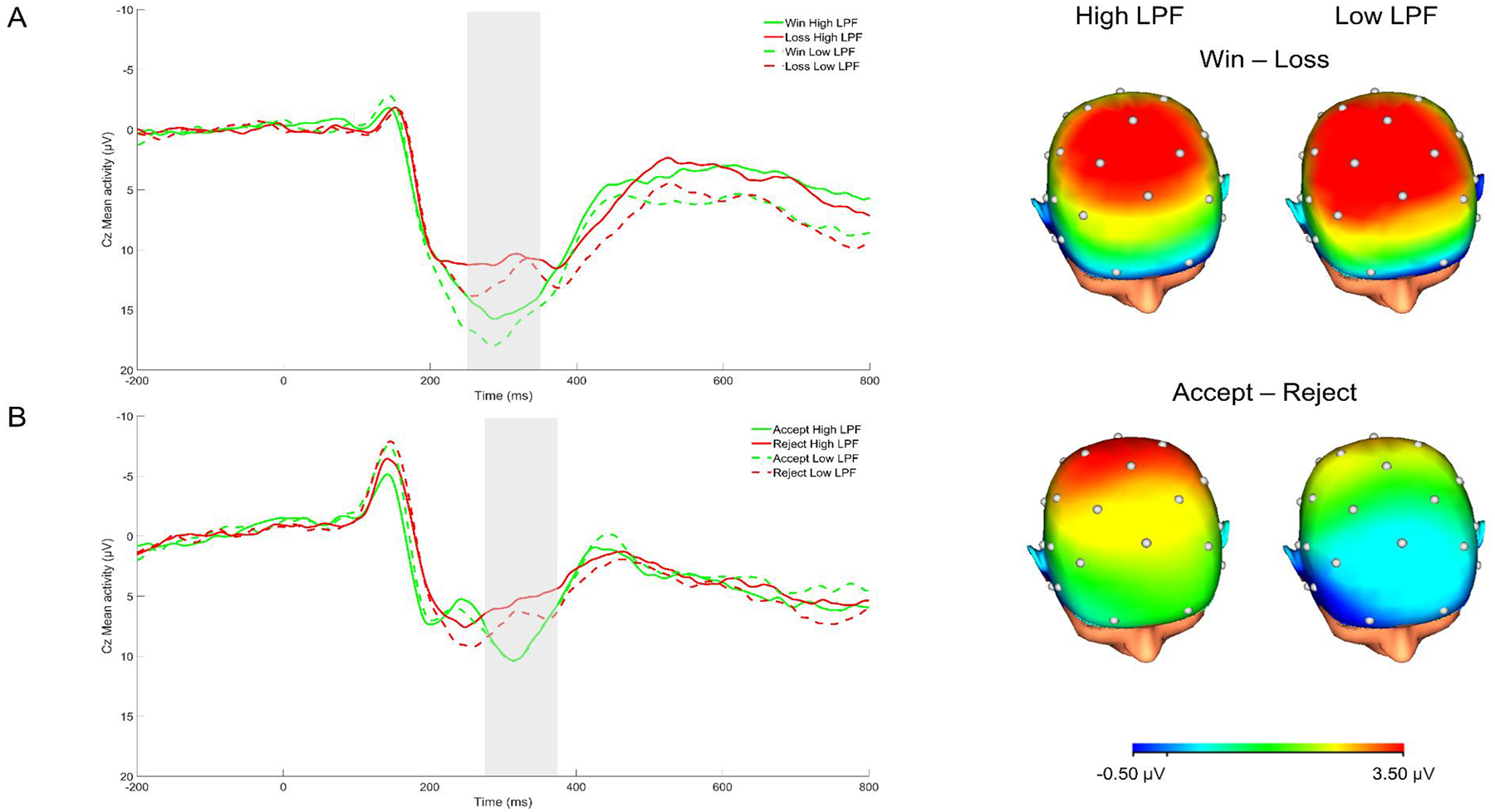
ERP Waveform and Scalp Distributions Depicting Neural Responses to Monetary (A) and Social (B) Feedback for Low and High LPF
Note. ERP waveform is at Cz. The 250–350 ms time window is highlighted in the ERP waveform representing the RewP in the monetary reward task (A), while the 275–375 time window is highlighted in the ERP waveform representing the RewP in the social reward task (B). Negative values are plotted up. Scalp distributions reference the respective RewP time window identified for each task. A median split was computed for illustrative purposes to present findings for youth with low and high LPF.
Figure 4.
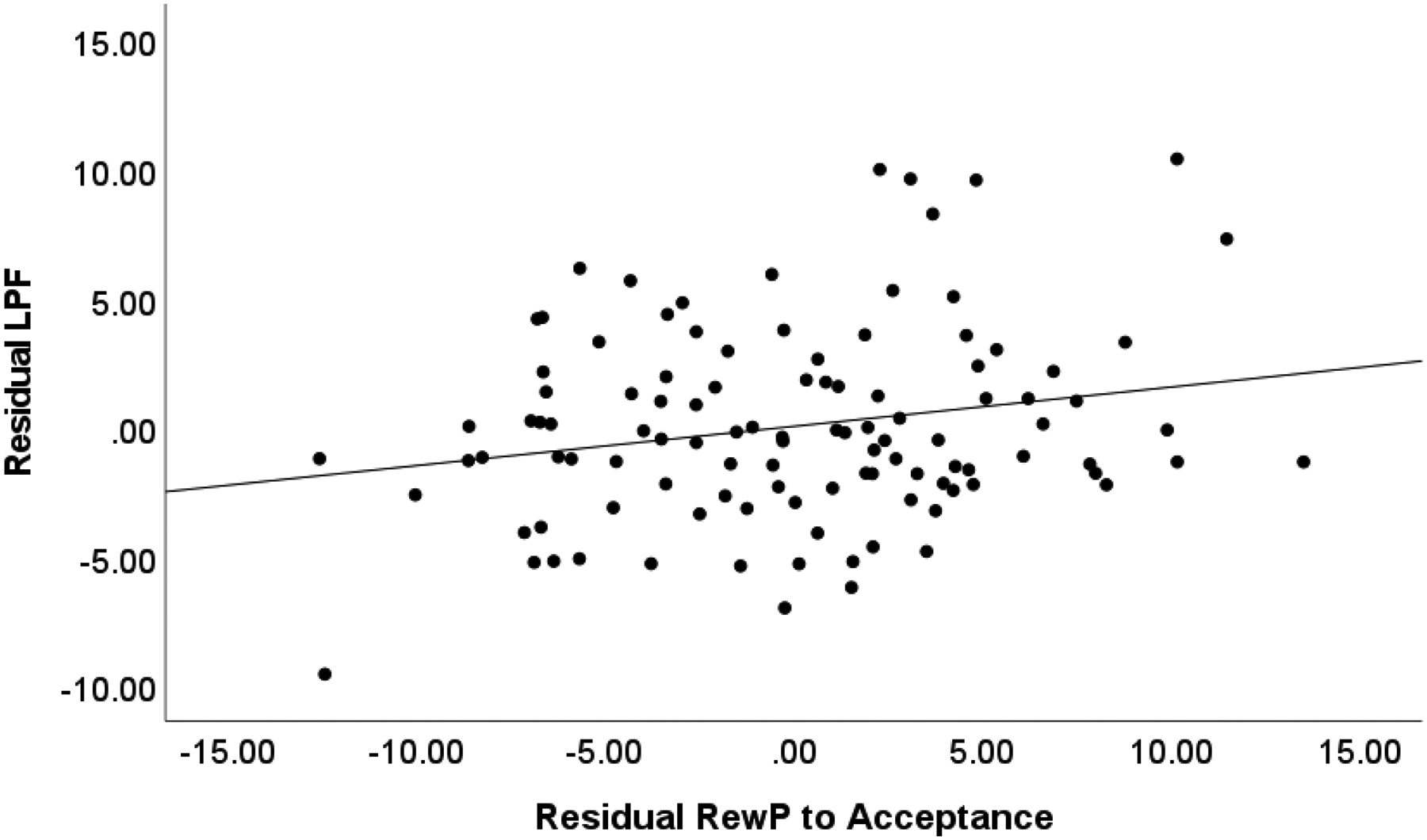
Scatterplot Depicting the Association between Residual RewP to Acceptance and Residual LPF
Note. Unstandardized residual RewP to acceptance was adjusted for RewP to rejection. Unstandardized residual LPF was adjusted for depression, anxiety, ADHD, ODD, CD, and RewP to win and loss conditions.
Discussion
To our knowledge, this is the first study examining neural correlates of LPF in youth. As expected, LPF was associated with all forms of psychopathology. When controlling for co-occurring symptoms, LPF was associated with heightened processing of social acceptance versus rejection feedback as indicated by the RewP. Effects were specific to social, rather than monetary reward processing and did not emerge at the bivariate level. These findings point to the relevance of social reward functioning, rather than general reward dysfunction, in LPF.
At the bivariate level, youth-reported depression and anxiety were associated with LPF. This is consistent with considerable work showing high rates of comorbidity among these diagnostic categories in later adolescence and adulthood (Watson & Clark, 2023; Zimmerman et al., 2005). Significant associations between parent-reported ADHD, ODD, and CD with LPF also emerged. While these externalizing disorders have long been identified as precursors to antisocial personality disorder (Keenan et al., 1999), only recently have they been considered among other personality disorders, such as borderline personality disorder (Stepp et al., 2012; Storebo & Simonsen, 2014). When considering all of these diagnostic factors together in the regression model, depression, anxiety, and ODD continued to explain significant variance in LPF. These effects may be due to the overlapping interpersonal and identity concerns that are central to depression, anxiety, ODD, and LPF. While some criteria of ADHD (e.g., interrupts or intrudes on others) and CD (e.g., bullies, threatens or intimidates others) are relevant to interpersonal impairment, these features are not required for diagnosis, and social dysfunction may better represent a correlate or consequence of ADHD and CD rather than a core diagnostic feature (McQuade & Hoza, 2014). It is also possible that the relatively larger associations between depression, anxiety, and LPF may reflect method bias, as youth report was collected for depression, anxiety, and LPF, while parent report was used to assess ODD. However, the decision to use different informants for these constructs was based on theoretical and empirical grounds that suggest that youth report of the largely internal experiences of depression, anxiety, and personality pathology in early adolescence may be more valid than parent report (Viana et al., 2008), whereas parent report rather than youth report is central to the assessment of externalizing disorders such as ADHD, ODD, and CD (Pelham, Fabiano, 2005).
At the bivariate level, no significant associations emerged between psychopathology and reward processing variables. Cross-sectional associations between psychopathology and RewP are generally modest and do not always emerge at the bivariate level (Babinski et al., 2019; Pegg et al., 2021). However, as expected, enhanced processing of social acceptance cues, indicated by an enhanced RewP component, was associated with LPF when considering co-occurring psychopathology as well as RewP to rejection, and RewP in monetary win and loss conditions. Comorbid internalizing and externalizing symptoms may mask the effects of social RewP on LPF. While the association between RewP to acceptance and LPF was modest in size, it is nonetheless notable considering that other forms of psychopathology, which often co-occurr with LPF, such as depression and ADHD, have been associated with a blunted RewP in response to social acceptance (Babinski et al., 2019; Kujawa et al., 2014a). The association between enhanced RewP to acceptance and LPF identified herein is consistent with our previous work using this social interaction task among emerging adults with borderline personality features (Babinski et al., 2023), as well as extant adult EEG (Gutz et al., 2015; Weinbrecht et al., 2018) and fMRI (Domsalla et al., 2014; Malejko et al., 2019) studies. This heightened processing of social acceptance may reflect abnormalities in social reward responsiveness and social approach motivation, as combined ERP-fMRI studies have linked RewP to activation in reward-related brain regions including the ventral striatum, ventromedial prefrontal cortex, midcingulate, and anterior cingulate (Becker et al., 2014; Carlson et al., 2011). Future work examining how this enhanced RewP to social acceptance is associated with self-reported experiences of social acceptance and behavioral responses to social acceptance is needed. It may be that the enhanced RewP identified in the current study is suggestive of impairments in modulating responses to acceptance, which may underlie some of the most pervasive features of personality impairment, including dependency and frantic efforts to avoid being alone (Choi-Kain et al., 2010).
An opposite effect emerged showing a blunted RewP to social rejection was associated with LPF. Although not directly related to study hypotheses, this effect in the opposite direction to RewP to acceptance suggests that there is greater differentiation between these feedback conditions for youth with elevated LPF. The amplitude of the RewP is associated with the degree of positive reward error (i.e., receiving better than expected outcomes; Baker & Holroyd, 2011; Cavanagh, 2015). Thus, while the enhanced RewP to acceptance associated with LPF may signify that the experience of acceptance is relatively unexpected for youth, who have often experienced persistent social rejection and invalidation (Crowell et al., 2009; Runions et al., 2020), the more blunted RewP to rejection may reflect that experience of being rejected is relatively more aligned with their social expectations (e.g., Weinbrecht et al., 2018).
Counter to hypotheses, neural responses to monetary loss and win were not significantly associated with LPF. Although several studies spanning adolescence through adulthood suggest that individuals with borderline personality pathology demonstrate less differentiation in neural responses to monetary reward and loss compared to those without personality pathology (Endrass et al., 2016; Stewart et al., 2019), these finding may be related to disinhibition that is part of the categorical diagnosis of borderline personality disorder rather than interpersonal and identity impairment. Indeed, a similar lack of differentiation in RewP to monetary win and loss has been identified in other disorders characterized by disinhibition, such as ADHD (van Meel et al., 2011). Monetary reward dysfunction may represent a general liability for psychopathology (Zald & Treadway, 2017), while the altered social reward processing identified herein may specifically reflect emerging personality pathology or more severe psychopathology that has significantly and negatively impacted social functioning (Sharp & Wall, 2018). Indeed, prominent models of personality pathology development highlight child vulnerabilities, particularly impulsivity, as some of the earliest precursors to personality pathology (Crowell et al., 2009; Sharp & Wall, 2018). However, it is through negative transactions with parents and peers, leading to the development of psychopathology, such as ADHD, ODD, CD, depression, and anxiety, and subsequent social processing deficits that beget impairments in LPF.
Several limitations of this study must be highlighted. First, in this cross-sectional study, we cannot test the directionality of effects and explore the developmental cascade through which these psychopathology and reward processing variables give rise to LPF. Relatedly, as internalizing and externalizing pathology are theortized to contribute to the development of LPF, LPF was selected as the dependent variable in regression analysis, but it may also be that LPF and reward processing variables worsen internalizing and externalizing pathology. Second, self-reported LPF was considered, but other measures of personality dysfunction, such as maladaptive traits may also be worth considering. Interview-based measures of personality pathology (e.g., Weekers et al., 2021) may also sidestep the known limitations of assessing personality pathology through self-report (Waugh et al., 2017). Third, the real-world, clinical significance of the association between enhanced RewP to social acceptance and LPF was not tested. Fourth, only female youth were included, but personality pathology is also highly relevant to males and the high rates of detection among women may represent diagnostic bias (Skodol & Bender, 2003). Fifth, effects, while significant, were modest, which is common given the large sample size and lack of shared method variance (Patrick et al., 2013). Large effects in clinical neuroscience may be due, at least in part, to overestimates of effect sizes in studies with small samples (Button et al., 2013). Studies integrating multiple measures and levels of analysis are essential to clarify the clinical significance of findings.
Despite these limitations, this study provides one of the first studies examining early adolescent neural predictors of personality pathology using a conceptually grounded and developmentally sensitive measure of personality pathology consistent with Section II of the DSM-5. Although internalizing and externalizing pathology is associated with risk for personality pathology, it is currently unclear why only some youth with these psychiatric concerns develop personality pathology. The current study indicates that additional variance in LPF can be accounted for by enhanced neural responses to social reward. Thus, social reward dysfunction may represent an early marker of emergent personality pathology. Future research is needed to extend these novel findings to understand the developmental progression from social reward dysfunction to personality disorder across development. Although psychosocial treatment for personality disorders, namely borderline personality disorder, has focused on coping with negative social experiences (Lynch et al., 2007), the results of this study suggest that clinical attention to addressing adaptive responses to positive social feedback is also worthwhile in treating and preventing personality disorders.
Acknowledgements
This work was supported by R21-MH125052, F31-MH127817-01, and T32-MH18921.
Footnotes
Conflicts of Interest
All authors declare that they have no conflicts of interests to declare with respect to the current study.
Participant votes to accept and reject co-players were not significantly associated with LPF (ps>.75). Positive (M=3.53, SD=0.93) and negative (M=1.52, SD=0.67) affect were not significantly associated with RewP to acceptance or rejection (ps <.21).
Analyses were conducted excluding participants with data interpolated at one or both mastoids prior to mastoid re-reference and considering ocular correction procedures. No substantive changes were observed.
Data exported using a 250–350ms window were also considered for social RewP and results were similar.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5). [Google Scholar]
- Babinski DE, Kujawa A, Kessel EM, Arfer KB, & Klein DN (2019). Sensitivity to peer feedback in young adolescents with symptoms of ADHD: Examination of neurophysiological and self-report measures. Journal of Abnormal Child Psychology, 47(4), 605–617. 10.1007/s10802-018-0470-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babinski DE, Pegg S, West M, Arfer KB, & Kujawa A (2023). Borderline personality features and altered social feedback processing in emerging adults: An EEG study. Progress in NeuroPsychopharmacology and Biological Psychiatry, 120, 110648. 10.1016/j.pnpbp.2022.110648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TE, & Holroyd CB (2011). Dissociated roles of the anterior cingulate cortex in reward and conflict processing as revealed by the feedback error-related negativity and N200. Biological Psychology, 87(1), 25–34. 10.1016/j.biopsycho.2011.01.010 [DOI] [PubMed] [Google Scholar]
- Becker MP, Nitsch AM, Miltner WH, & Straube T (2014). A single-trial estimation of the feedback-related negativity and its relation to BOLD responses in a time-estimation task. Journal of Neuroscience, 34(8), 3005–3012. doi: 10.1523/JNEUROSCI.3684-13.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Shea MT, Zanarini MC, Oldham JM, & Gunderson JG (2001). Treatment utilization by patients with personality disorders. American Journal of Psychiatry, 158(2), 295–302. 10.1176/appi.ajp.158.2.295 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry, 38(10), 1230–1236. 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, & Lieb K (2021). Borderline personality disorder. The Lancet, 398(10310), 1528–1540. 10.1016/S0140-6736(21)00476-1 [DOI] [PubMed] [Google Scholar]
- Bress JN, & Hajcak G (2013). Self-report and behavioral measures of reward sensitivity predict the feedback negativity. Psychophysiology, 50(7), 610–616. 10.1111/psyp.12053 [DOI] [PubMed] [Google Scholar]
- Button KS, Ioannidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ, & Munafò MR (2013). Power failure: why small sample size undermines the reliability of neuroscience. Nature Reviews Neuroscience, 14(5), 365–376. 10.1038/nrn3475 [DOI] [PubMed] [Google Scholar]
- Carlson JM, Foti D, Mujica-Parodi LR, Harmon-Jones E, & Hajcak G (2011). Ventral striatal and medial prefrontal BOLD activation is correlated with reward-related electrocortical activity: A combined ERP and fMRI study. NeuroImage, 57(4), 1608–1616. 10.1016/j.neuroimage.2011.05.037 [DOI] [PubMed] [Google Scholar]
- Cavanagh JF (2015). Cortical delta activity reflects reward prediction error and related behavioral adjustments, but at different times. NeuroImage, 110, 205–216. 10.1016/j.neuroimage.2015.02.007 [DOI] [PubMed] [Google Scholar]
- Choi-Kain LW, Zanarini MC, Frankenburg FR, Fitzmaurice GM, & Bradford Reich D (2010). A longitudinal study of the 10-year course of interpersonal features in borderline personality disorder. Journal of Personality Disorders, 24(3), 365–376. 10.1521/pedi.2010.24.3.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Nuzum H, & Ro E (2018). Manifestations of personality impairment severity: comorbidity, course/prognosis, psychosocial dysfunction, and ‘borderline’ personality features. Current Opinion in Psychology, 21, 117–121. 10.1016/j.copsyc.2017.12.004 [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale: Erlbaum [Google Scholar]
- Crick NR, & Dodge KA (1994). A Review and reformulation of social information-processing mechanisms in children’s social adjustment. Psychological Bulletin, 115(1), 74–101. 10.1037/0033-2909.115.1.74 [DOI] [Google Scholar]
- Crowell SE, Beauchaine TP, & Linehan MM (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135(3), 495–510. 10.1037/a0015616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, & Kaufman EA (2016). Borderline personality disorder and the emerging field of developmental neuroscience. Personality Disorders: Theory, Research, and Treatment, 7(4), 324–333. 10.1037/per0000204 [DOI] [PubMed] [Google Scholar]
- Dickey L, Pegg S, Cárdenas EF, Green H, Dao A, Waxmonsky J, Pérez-Edgar K, & Kujawa A (2023). Neural predictors of improvement with cognitive behavioral therapy for adolescent depression: An examination of reward responsiveness and emotion regulation. Research on Child and Adolescent Psychopathology, 0123456789. 10.1007/s10802-023-01054-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domsalla M, Koppe G, Niedtfeld I, Vollstädt-Klein S, Schmahl C, Bohus M, & Lis S (2014). Cerebral processing of social rejection in patients with borderline personality disorder. Social Cognitive and Affective Neuroscience, 9(11), 1789–1797. 10.1093/scan/nst176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endrass T, Schuermann B, Roepke S, Kessler-Scheil S, & Kathmann N (2016). Reduced risk avoidance and altered neural correlates of feedback processing in patients with borderline personality disorder. Psychiatry Research, 243, 14–22. 10.1016/j.psychres.2016.06.016 [DOI] [PubMed] [Google Scholar]
- Ethridge P, & Weinberg A (2018). Psychometric properties of neural responses to monetary and social rewards across development. International Journal of Psychophysiology, 132, 311–322. 10.1016/j.ijpsycho.2018.01.011 [DOI] [PubMed] [Google Scholar]
- Fosco WD, Babinski DE, & Waschbusch DA (2023). The Disruptive Behavior Disorders Rating Scale: Updated factor structure, measurement invariance, and national caregiver norms. Journal of Pediatric Psychology, 1–11. 10.1093/jpepsy/jsad006 [DOI] [PubMed] [Google Scholar]
- Gao S, Assink M, Cipriani A, & Lin K (2017). Associations between rejection sensitivity and mental health outcomes: A meta-analytic review. Clinical Psychology Review, 57, 59–74. 10.1016/j.cpr.2017.08.007 [DOI] [PubMed] [Google Scholar]
- Goodman M, Patil U, Steffel L, Avedon J, Sasso S, Triebwasser J, & Stanley B (2010). Treatment utilization by gender in patients with borderline personality disorder. Journal of Psychiatric Practice, 16(3), 155–163. 10.1097/01.pra.0000375711.47337.27 [DOI] [PubMed] [Google Scholar]
- Gratton G, Coles MGH, & Donchin E (1983). A new method for off-line removal of ocular artifact. Electroencephalography and Clinical Neurophysiology, 55(4), 468–484. 10.1016/0013-4694(83)90135-9 [DOI] [PubMed] [Google Scholar]
- Gutz L, Renneberg B, Roepke S, & Niedeggen M (2015). Neural processing of social participation in borderline personality disorder and social anxiety disorder. Journal of Abnormal Psychology, 124(2), 421–431. 10.1037/a0038614 [DOI] [PubMed] [Google Scholar]
- Hepp J, Niedtfeld I, & Schulze L (2023). Experimental paradigms in personality disorder research: A review of covered RDoC constructs, methodological issues, and future directions. Personality Disorders: Theory, Research, and Treatment, 14(1), 50–61. 10.1037/per0000588 [DOI] [PubMed] [Google Scholar]
- Hill KE, Dickey L, Pegg S, Dao A, Arfer KB, & Kujawa A (2023). Associations between parental conflict and social and monetary reward responsiveness in adolescents with clinical depression. Research on Child and Adolescent Psychopathology, 51(1), 119–131. 10.1007/s10802-022-00949-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kappenman ES, & Luck SJ (2016). Best practices for event-related potential research in clinical populations. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 1(2), 110–115. 10.1016/j.bpsc.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Loeber R, & Green S (1999). Conduct disorder in girls: a review of the literature. Clinical Child and Family Psychology Review, 2(1), 3–19. 10.1023/A:1021811307364 [DOI] [PubMed] [Google Scholar]
- Kerr S, McLaren V, Cano K, Vanwoerden S, Goth K, & Sharp C (2022). Levels of Personality Functioning Questionnaire 12–18 (LoPF-Q 12–18): Factor structure, validity, and vlinical cut-Offs. Assessment. 10.1177/10731911221124340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koudys JW, Traynor JM, Rodrigo AH, Carcone D, & Ruocco AC (2019). The NIMH Research Domain Criteria (RDoC) initiative and its implications for research on personality disorder. Current Psychiatry Reports, 21(6). 10.1007/s11920-019-1023-2 [DOI] [PubMed] [Google Scholar]
- Kujawa A, Kessel EM, Carroll A, Arfer KB, & Klein DN (2017). Social processing in early adolescence: Associations between neurophysiological, self-report, and behavioral measures. Biological Psychology, 128, 55–62. 10.1016/j.biopsycho.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa A, Arfer KB, Klein DN, & Proudfit GH (2014a). Electrocortical reactivity to social feedback in youth: A pilot study of the Island Getaway task. Developmental Cognitive Neuroscience, 10, 140–147. 10.1016/j.dcn.2014.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa A, Carroll A, Mumper E, Mukherjee D, Kessel EM, Olino T, … & Klein DN (2018). A longitudinal examination of event-related potentials sensitive to monetary reward and loss feedback from late childhood to middle adolescence. International Journal of Psychophysiology, 132, 323–330. 10.1016/j.ijpsycho.2017.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa A, Proudfit GH, & Klein DN (2014b). Neural reactivity to rewards and losses in offspring of mothers and fathers with histories of depressive and anxiety disorders. Journal of Abnormal Psychology, 123, 287–297. 10.1037/a0036285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus SA, Cheavens JS, Festa F, & Zachary Rosenthal M (2014). Interpersonal functioning in borderline personality disorder: A systematic review of behavioral and laboratory-based assessments. Clinical Psychology Review, 34(3), 193–205. 10.1016/j.cpr.2014.01.007 [DOI] [PubMed] [Google Scholar]
- Lynch TR, Trost WT, Salsman N, & Linehan MM (2007). Dialectical behavior therapy for borderline personality disorder. Annual Review of Clinical Psychology, 3, 181–205. 10.1146/annurev.clinpsy.2.022305.095229 [DOI] [PubMed] [Google Scholar]
- Malejko K, Neff D, Brown RC, Plener PL, Bonenberger M, Abler B, & Graf H (2019). Neural signatures of social inclusion in borderline personality disorder versus non-suicidal self-injury. Brain Topography, 32(5), 753–761. 10.1007/s10548-019-00712-0 [DOI] [PubMed] [Google Scholar]
- McQuade JD, & Hoza B (2014). Peer relationships of children with ADHD. In In Barkley RA (Ed.), Attention-deficit/hyperactivity disorder: a handbook for diagnosis and treatment (pp. 210–222). [Google Scholar]
- Messer SC, Angold A, Costello J, Loeber R, Van Kämmen W, & Stouthamer-Loeber M (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: factor composition and structure across development. International Journal of Methods in Psychiatric Research, 5(4), 251–262. [Google Scholar]
- Meyer A, Lerner MD, De Los Reyes A, Laird RD, & Hajcak G (2017). Considering ERP difference scores as individual difference measures: Issues with subtraction and alternative approaches. Psychophysiology, 54(1), 114–122. 10.1111/psyp.12664 [DOI] [PubMed] [Google Scholar]
- Nieminen P, Lehtiniemi H, Vähäkangas K, Huusko A, & Rautio A (2013). Standardised regression coefficient as an effect size index in summarising findings in epidemiological studies. Epidemiology Biostatistics and Public Health, 10(4). 10.2427/8854 [DOI] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-injurious thoughts and behaviors interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. 10.1037/1040-3590.19.3.309 [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Venables NC, Yancey JR, Hicks BM, Nelson LD, & Kramer MD (2013). A construct-network approach to bridging diagnostic and physiological domains: application to assessment of externalizing psychopathology. Journal of Abnormal Psychology, 122(3), 902–916. 10.1037/a0032807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pegg S, Dickey L, Green H, & Kujawa A (2020). Differentiating clinically depressed adolescents with and without active suicidality: An examination of neurophysiological and self-report measures of reward responsiveness. Depression and Anxiety, 37(9), 876–884. 10.1002/da.23012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE Jr, Fabiano GA, & Massetti GM (2005). Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 34(3), 449–476. 10.1207/s15374424jccp3403_5 [DOI] [PubMed] [Google Scholar]
- Proudfit GH (2015). The reward positivity: From basic research on reward to a biomarker for depression. Psychophysiology, 52(4), 449–459. 10.1111/psyp.12370 [DOI] [PubMed] [Google Scholar]
- Runions KC, Wong J, Pace G, & Salmin I (2020). Borderline personality disorder and peers: A scoping review of friendship, victimization and aggression studies. Adolescent Research Review, 6(4), 359–389. 10.1007/s40894-020-00137-y [DOI] [Google Scholar]
- Sansone RA, & Sansone LA (2011). Gendered patterns in borderline personality disorder. Innovations in Clinical Neuroscience, 8(5), 16–20. [PMC free article] [PubMed] [Google Scholar]
- Sharp C, Wright AG, Fowler J, Frueh B, Allen J, Oldham J, & Clark L (2015). The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? Journal of Abnormal Psychology, 124(2), 387–398. 10.1037/abn0000033 [DOI] [PubMed] [Google Scholar]
- Sharp C, Mosko O, Chang B, & Ha C (2011). The cross-informant concordance and concurrent validity of the Borderline Personality Features Scale for Children in a community sample of boys. Clinical Child Psychology and Psychiatry, 16(3), 335–349. 10.1177/1359104510366279 [DOI] [PubMed] [Google Scholar]
- Sharp C, & Wall K (2018). Personality pathology grows up: Adolescence as a sensitive period. Current Opinion in Psychology, 21, 111–116. 10.1016/j.copsyc.2017.11.010 [DOI] [PubMed] [Google Scholar]
- Sharp C, & Wall K (2021). DSM-5 Level of Personality Functioning: Refocusing personality disorder on what it means to be human. Annual Review of Clinical Psychology, 17, 313–337. 10.1146/annurev-clinpsy-081219-105402 [DOI] [PubMed] [Google Scholar]
- Shiner RL, & Allen TA (2013). Assessing personality disorders in adolescents: Seven guiding principles. Clinical Psychology: Science and Practice, 20(4), 361–377. 10.1111/cpsp.12047 [DOI] [Google Scholar]
- Skabeikyte-Norkiene G, Sharp C, Kulesz PA, & Barkauskiene R (2022). Personality pathology in adolescence: relationship quality with parents and peers as predictors of the level of personality functioning. Borderline Personality Disorder and Emotion Dysregulation, 9(1), 1–11. 10.1186/s40479-022-00202-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, & Bender DS (2003). Why are women diagnosed borderline more than men? Psychiatric Quarterly, 74(4), 349–360. 10.1023/A:1026087410516 [DOI] [PubMed] [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, & Loeber R (2012). Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. Journal of Abnormal Child Psychology, 40(1), 7–20. 10.1007/s10802-011-9530-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Lazarus SA, & Byrd AL (2016). A systematic review of risk factors prospectively associated with borderline personality disorder: Taking stock and moving forward. Personality Disorders: Theory, Research, and Treatment, 7(4) 316–323. 10.1037/per0000186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JG, Singleton P, Benau EM, Foti D, Allchurch H, Kaplan CS, Aguirre B, & Auerbach RP (2019). Neurophysiological activity following rewards and losses among female adolescents and young adults with borderline personality disorder. Journal of Abnormal Psychology, 128(6), 610–621. 10.1037/abn0000439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storebo OJ, & Simonsen E (2014). Is ADHD an early stage in the development of borderline personality disorder? Nordic Journal of Psychiatry, 68(5), 289–295. 10.3109/08039488.2013.841992 [DOI] [PubMed] [Google Scholar]
- Townsend L, Kobak K, Kearney C, Milham M, Andreotti C, Escalera J, … & Kaufman J (2020). Development of three web-based computerized versions of the kiddie schedule for affective disorders and schizophrenia child psychiatric diagnostic interview: preliminary validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 59(2), 309–325. 10.1016/j.jaac.2019.05.009 [DOI] [PubMed] [Google Scholar]
- van Meel CS, Heslenfeld DJ, Oosterlaan J, Luman M, & Sergeant JA (2011). ERPs associated with monitoring and evaluation of monetary reward and punishment in children with ADHD. Journal of Child Psychology and Psychiatry, 52(9), 942–953. 10.1111/j.1469-7610.2010.02352.x [DOI] [PubMed] [Google Scholar]
- Viana AG, Rabian B, & Beidel DC (2008). Self-report measures in the study of comorbidity in children and adolescents with social phobia: Research and clinical utility. Journal of Anxiety Disorders, 22(5), 781–792. 10.1016/j.janxdis.2007.08.005 [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (2023). Comorbidity and heterogeneity: Two challenges for personality pathology research. Personality Disorders, 14(1), 39–49. 10.1037/per0000586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waugh MH, Hopwood CJ, Krueger RF, Morey LC, Pincus AL, & Wright AGC (2017). Psychological assessment with the DSM-5 alternative model for personality disorders: Tradition and innovation. Professional Psychology: Research and Practice, 48(2), 79–89. 10.1037/pro0000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (2011). WASI-II: Wechsler abbreviated scale of intelligence.
- Weekers LC, Hutsebaut J, & Kamphuis JH (2018). The Level of Personality Functioning Scale-Brief Form 2.0: Update on a brief instrument for assessing level of personality functioning. Personality and Mental Health, 13, 3–14. 10.1002/pmh.1434 [DOI] [PubMed] [Google Scholar]
- Weekers LC, Verhoeff SCE, Kamphuis JH, & Hutsebaut J (2021). Assessing criterion A in adolescents using the Semistructured Interview for Personality Functioning DSM-5. Personality Disorders: Theory, Research, and Treatment, 12(4), 312–319. 10.1037/per0000454 [DOI] [PubMed] [Google Scholar]
- Weinbrecht A, Niedeggen M, Roepke S, & Renneberg B (2018). Feeling excluded no matter what? Bias in the processing of social participation in borderline personality disorder. NeuroImage: Clinical, 19, 343–350. 10.1016/j.nicl.2018.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wertz J, Caspi A, Ambler A, Arseneault L, Belsky DW, Danese A, Fisher HL, Matthews T, Richmond-Rakerd L, & Moffitt TE (2019). Borderline symptoms at age 12 signal risk for poor outcomes during the transition to adulthood: Findings from a genetically sensitive longitudinal cohort study. Journal of the American Academy of Child & Adolescent Psychiatry. 10.1016/j.jaac.2019.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zald DH, & Treadway MT (2017). Reward processing, neuroeconomics, and psychopathology. Annual Review of Clinical Psychology, 13, 471–495. 10.1146/annurev-clinpsy-032816-044957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, Rothschild L, & Chelminski I (2005). The prevalence of DSM-IV personality disorders in psychiatric outpatients. American Journal of Psychiatry, 162, A56–1992. 10.1016/s0084-3970(08)70470-5 [DOI] [PubMed] [Google Scholar]
- Zimmermann R, Steppan M, Zimmermann J, Oeltjen L, Birkhölzer M, Schmeck K, & Goth K (2022). A DSM-5 AMPD and ICD-11 compatible measure for an early identification of personality disorders in adolescence-LoPF-Q 12–18 latent structure and short form. PloS One, 17(9), e0269327. 10.1371/journal.pone.0269327 [DOI] [PMC free article] [PubMed] [Google Scholar]


