Abstract
Social support refers to the help someone receives emotionally or instrumentally from their social network. Poor social support in the perinatal period has been associated with increased risk for symptoms of common mental disorders, including depression and posttraumatic stress symptoms (PTS), which may impact parenting behavior. Whether social support impacts parenting behaviors, independent of mental health symptomatology, remains unclear. Among N=309 participants of the Scaling Up Maternal Mental healthcare by Increasing access to Treatment (SUMMIT Trial), a large perinatal depression and anxiety treatment trial, we explored the relations between perceived social support, perinatal depressive and PTS symptoms, and psychosocial stimulation provided by the parent in their home environment. Social support was measured at baseline using the Multidimensional Scale of Perceived Social Support (MSPSS). Perinatal depressive symptoms were measured by the Edinburgh Postnatal Depression Scale (EPDS) and PTS symptoms were measured by the Abbreviated PTSD Checklist (PCL-6) at baseline, 3-, and 6-months post-randomization. Psychosocial stimulation was assessed by the Home Observation Measurement of the Environment (HOME) when the infant was between 6 to 24 months. Using stepwise hierarchical regressions, we found: (1) perceived social support at baseline significantly predicted both depressive and PTS symptoms at 3-months post-randomization, even when controlling for baseline depressive and PTS symptoms; and (2) while neither depressive nor PTS symptoms were significantly associated with psychosocial stimulation, perceived social support at baseline was a significant predictor. Clinical implications regarding treatment of perinatal patients are discussed.
Keywords: perinatal depression, perinatal posttraumatic stress, infant development, perceived social support, psychosocial stimulation
Introduction
Depression and posttraumatic stress (PTS) are two common and comorbid mental health occurrences that can affect mothers during the perinatal (pregnancy and up to 1 year postpartum) period [1-3]. Symptoms include both general depressive symptoms (eg, feelings of worthlessness, sleep and concentration difficulties, psychomotor agitation) [4] and symptoms specific to the perinatal period (ie, difficulty bonding with the infant [5], feelings of inadequacy [6], and thoughts of harming the baby) [7]. PTS symptoms may manifest after a traumatic event and can include upsetting memories or dreams about the event, distress due to internal or external cues that remind someone of the event, self-destructive behavior, or negative cognitive or mood changes [4]. Pregnancy or childbirth can be a time when traumatic events occur due to a perceived threat to the health of mother and/or infant and memories of adverse childhood events during the perinatal period [8-10]. Memories of past traumas may be triggered by the psychological transition of pregnancy and motherhood, alongside biological changes, such as in stress signaling regulation, thereby exacerbating PTS symptoms [11]. This is consistent with the life course approach, which emphasizes the negative effect of cumulative adverse past events on current situations, including on the experience of pregnancy and postpartum [12-14]. These symptoms can be effectively treated with psychological and pharmacological interventions [15-18].
Depressive and PTS symptoms can significantly impact a mother’s functioning [1,2,10,11], with adverse effects on her child [8,9]. It is important to understand the underlying mechanisms that explain the relation between perinatal mental health symptoms and developmental outcomes to improve the identification of at-risk parent-child dyads and inform treatments [19]. One such mechanism may be the psychosocial stimulation a child receives in the home environment. Psychosocial stimulation refers to aspects of the environment that promote optimal child development, including language, cognitive, motor, and social development [20]. Parents have a major role in shaping the home environment to provide adequate psychosocial stimulation. Parental behaviors that support psychosocial stimulation include affection, warmth, responsivity, and cognitive stimulation via, for example, providing age-appropriate toys, books, and activities that encourage learning and language development [21-24]. Since psychosocial stimulation involves, in part, the behaviors and activities that a parent engages in with their child, psychosocial stimulation is likely impacted by perinatal mental health, whereby a mother experiencing depressive and posttraumatic symptoms may not have the same capacity to stimulate their child and engage with them [25,26]. Thus, researchers have widely acknowledged the importance of perinatal mental health for child development [27].
The relation between perinatal mental health symptoms and psychosocial stimulation may also be impacted by the broader social support environment in which the mother-child relationship exists. Social support—defined broadly as support that an individual receives from other people in their social network—is crucial, particularly during the perinatal period because: (1) perceived social support can buffer the negative effects of perinatal mental health symptoms on both mother and child [28-30]; (2) higher levels of perceived social support can reduce the risk of postpartum stress and depression symptoms, and/or reduce their severity [31-33]; and (3) parental social support also leads to more optimal home environments for their children [34,35]. For example, practical support can help a mother manage the demands of childcare (eg, babysitting, general care for the infant, help with household responsibilities); while emotional support can help a mother feel heard and less lonely, and emotionally process the demands of motherhood.
Relations between perceived social support, perinatal depressive and posttraumatic stress symptomatology, and psychosocial stimulation are unclear. The use of longitudinal data can assess not only whether relationships exist between perceived social support and depressive and posttraumatic stress symptoms but whether social support predicts these mental health symptoms. In addition, understanding whether perinatal mental health and social support are related to psychosocial stimulation is a less studied area and can contribute to a greater understanding of the role of maternal factors on a child’s environment and ultimately their development. Thus, the current study had two aims: 1) To examine the potential longitudinal relation between perceived social support and perinatal depressive and PTS symptoms; 2) To explore whether perinatal depressive symptoms, PTS symptoms, and perceived social support were associated with psychosocial stimulation of the home environment.
Method
This study was a secondary analysis within the Scaling Up of Maternal Mental healthcare by Increasing access to Treatment (SUMMIT) trial. The SUMMIT trial is a large, multi-site randomized controlled trial that uses a non-inferiority design for perinatal participants experiencing depressive and anxiety symptoms. The study, conducted in Canada (Toronto, ON) and the USA (Chapel Hill, NC and Evanston, IL), examined whether delivery of a brief, behavioral activation talk therapy by non-mental health providers (healthcare professionals without formal mental health care training or experience delivering psychotherapy, eg, nurses, midwives) is non-inferior to delivery by specialist providers (healthcare professionals who have formal training and experience in delivering psychological treatment, eg, psychiatrists, psychologists, social workers), and whether psychotherapy delivered via telemedicine is non-inferior to in-person treatment. All participants who were deemed eligible completed a baseline assessment and received the same 6-8 session Behavioral Activation (BA) treatment, but they were randomized to one of four different treatment arms: receiving treatment from either a non-mental health provider or specialist provider, either in-person or through telemedicine [36]. Measures were completed by participants at baseline, prior to randomization, and at 3-, 6-, and 12-months post-randomization. The participants were either pregnant or postpartum at the time they completed the baseline measures and postpartum by the time they completed the home visit. A home visit was conducted between 6 and 24 months postpartum to evaluate infant and child outcomes. Participants received a $20 e-gift card when assessments were completed and a $40 e-gift card when the home visit was completed. The detailed SUMMIT trial protocol has been published elsewhere [36].
For this secondary analysis, only participants recruited in Canada (Toronto, ON) were included and only selected measures completed at baseline, 3-months post-randomization, 6-months post-randomization, and the home visit were analyzed. Ethical approval has been received from institutional review boards (IRBs) for all Toronto sites through Clinical Trials Ontario (1895). Additionally, ethical approval was received from Toronto Metropolitan University’s Research Ethics Board (2023-312), where the primary author is a student (TLK) and a co-author is a faculty member (MCM).
Participants
Participants were eligible for inclusion in the SUMMIT Trial if they were: either up to 36 weeks pregnant or 4-30 weeks postpartum; at least 18 years old; spoke and understood English; and scored at least 10 on the Edinburgh Postnatal Depression Scale (EPDS; indicating at least mild depressive symptomatology) [37] at the time of recruitment. Exclusion criteria included: active suicidal intent; active symptoms of psychosis or mania; a change in psychotropic medication within 2 weeks of enrollment or beginning treatment; had ongoing psychotherapy; active substance use or dependence; and reported severe fetal anomalies, stillbirth, or infant death at time of enrollment for index pregnancy [36]. Participants who were recruited from April 2020 to May 2023 from three academic hospitals in Toronto, Canada (Mount Sinai Hospital, Women’s College Hospital, and St. Michael’s Hospital) and who had completed all outcome measures relevant to the current study (see next section) were included in the current analysis.
Measures
Trial Baseline Questionnaire. Self-reported demographics were reported in a baseline questionnaire. This included participant age, ethnicity, education level, immigration status, marital status, and number of children.
Edinburgh Postnatal Depression Scale (EPDS). To assess depressive symptoms, participants completed the EPDS [34] at baseline, 3-, 6-, and 12-month post-randomization in the larger SUMMIT Trial; however, only the baseline, 3-, and 6-months post-randomization EPDS scores were included in the current study. The EPDS is a 10-item measure that screens for depressive symptoms. Participants rate how they have been feeling over the past 7 days and items are rated on a 4-point Likert scale from 0 (“No, not at all”) to 3 (“Yes, most of the time”). The EPDS item responses are then summed for a cumulative score, ranging from 0 to 30, with higher scores indicating more severe depressive symptoms. This measure was developed for use in assessing depression in perinatal populations [37]. It has been found to have good reliability, convergent validity, test-retest correlation, and sensitivity and specificity in studies with pregnant and postpartum women [38-40].
Post-Traumatic Checklist (PCL-6). To assess PTS symptoms, participants completed the PCL-6 [41] at baseline, 3-, 6-, and 12-month post-randomization in the SUMMIT Trial; however, only the baseline, 3-, and 6-months post-randomization PCL-6 scores were included in the current study. The PCL-6 uses a subset of questions from the original PCL-C [38], including two questions from each of the three symptom clusters related to cognitions, avoidance, and negative emotions. Example items include “feeling very upset when something reminded you of a stressful experience from the past” and “difficulty concentrating?” Respondents indicate their answer to each of the six items on a 5-point Likert scale, where each item is rated from 1 (“not at all”) to 5 (“extremely”). The PCL-6 yields a score between 6 and 30, with higher scores indicating more severe symptomatology. It is comprised of the items from the PCL-C that have the greatest correlation with the total score [41], thus, it is an efficient way of identifying individuals experiencing these symptoms. The PCL-6 has been used with perinatal populations previously [42,43], with acceptable reliability and validity [44-46].
Multidimensional Scale of Perceived Social Support (MSPSS). To assess perceived social support, participants completed the MSPSS [47] at baseline, 3-, 6-, and 12-month post-randomization in the larger SUMMIT Trial; however, only baseline MSPSS scores were used for the current study. The MSPSS is a 12-item scale where participants indicate their responses along a 7-point Likert scale from 1 (“very strongly disagree”) to 7 (“very strongly agree”). Items on this scale include “my friends really try to help me” and “I can talk about my problems with my family.” This scale yields a mean score between 1 and 12. A mean score between 1 and 2.9 indicates low social support; a score between 3 and 5 is considered moderate support; and a score between 5.1 and 7 suggests high support. The MSPSS has previously been used among perinatal populations [48-50]. It has also been used globally and found to be psychometrically sound with good reliability and validity [51-54].
Home Observation Measurement of the Environment (HOME). The HOME [55] was used to assess psychosocial stimulation. All participants were postpartum at the time this measure was completed. The HOME was completed by trained research assistants when the participant’s infant was between 6 and 24 months old. The HOME contains 45 items that are collected through a combination of observation and an interview with the parent, over an average of 15 minutes per participant, with research assistants typically visiting the participant and infant in their home environment. The HOME contains six sub-scales: 1) Emotional and verbal responsivity of the primary caregiver (eg, “Mother caresses or kisses child at least once during visit”); 2) Avoidance of restriction and punishment (eg, “Primary caregiver does not shout at child during visit”); 3) Organization of the physical and temporal environment (eg, “The child’s play environment appears safe and free of hazards”); 4) Provision of appropriate play materials (eg, “Provides equipment appropriate to age eg infant seat, infant rocker, playpen”); 5) Parental involvement with the child (eg, “Primary caregiver tends to keep child within visual range and looks at him/her often”); and 6) Opportunities for variety in daily stimulation (eg, “Family visits or receives visits from relatives approximately once a month”) [55]. All 45 items are coded as either a yes (1) or no (0), for a maximum total score of 45 [55]. The HOME has been found to be reliable and has acceptable concurrent and convergent validity for assessing the quality of the home environment [56-58].
Analytic Plan
We first analyzed descriptive variables to estimate means, SDs, and frequencies. A linear regression model was then conducted to investigate whether baseline EPDS and PCL-6 scores were significantly associated with MSPSS scores at baseline to establish whether the data supported a relation between perceived social support and depressive and posttraumatic stress symptoms, similar to past research [28,29]. The completed measures from the baseline timepoint were used for this analysis because we were not interested in assessing a temporal relationship at this stage. Our main analysis involved three hierarchical multiple regressions. We conducted stepwise regressions where independent variables were added one at a time to assess their unique contribution to the model. To determine whether social support at baseline impacted depressive and PTS symptoms at 3-months post-randomization, two hierarchical regressions were conducted. The 3-months post-randomization timepoint measures for PTS and depressive symptoms were used for this analysis because we were interested in the predictive relationship between social support and depressive and PTS symptoms.
The first regression included baseline MSPSS and baseline EPDS scores as independent variables, with EPDS scores at 3-months post-randomization as the outcome variable. The second regression included baseline MSPSS and baseline PCL-6 scores as independent variables, with PCL-6 scores at 3-months post-randomization as the outcome variable. Two covariates were included in both regressions: 1) “perinatal period” (whether participants were recruited while pregnant or postpartum); and 2) “treatment dosage” (how many treatment sessions the participant completed). These covariates were included to account for potential differences between participants who were recruited at different times during the perinatal period, and participants who received varying amounts of treatment. We conducted these same regressions but with the clinical measures (EPDS, PCL-6) from the 6-months post-randomization time point to determine if our findings would remain the same across time points.
To determine whether social support, depressive symptoms, and PTS symptoms impact psychosocial stimulation, the third hierarchical regression included baseline MSPSS score and 3-months post-randomization EPDS and PCL-6 scores as independent variables, with total HOME score as the outcome variable. Three covariates were included in this regression: 1) perinatal period; 2) treatment dosage; and 3) infant age at the time of the HOME assessment. Infant age at the HOME was added as a covariate to this model because this assessment was completed when the infant was anywhere between 6 and 24 months of age. Since the results of the HOME measure can be affected by infant age [58], potentially through differences in interactions the mother has with the child based on their child’s age, it was important to control for this factor. All analyses were conducted using R software version 4.3.1 [59].
Results
The study sample included N=309 participants. Participant characteristics are detailed in Table 1. Overall, participants were on average 34.96 years in age (range 21-54, SD = 4.42) with almost half of this sample self-identified as Black, Indigenous, and other People of Color (BIPOC), with most endorsing categories of Asian (18.77%), Black (9.06%), and multiracial (9.06%). For over half of participants, this was their first child. One-third of the sample was not born in Canada; the average number of years they have been living in Canada was 16 years. Almost 80% reported having an undergraduate or graduate university degree and over 90% of respondents self-reported that they were in a committed relationship (married, engaged, stable relationship).
Table 1. Demographic Characteristics (N=309).
| Variable | n | % |
| Participant Age (in years) (mean, SD) | 34.96 | SD=4.42 |
| Perinatal Period | ||
| Pregnant | 144 | 46.60 |
| Postpartum | 165 | 43.40 |
| Ethnicity | ||
| White | 157 | 50.80 |
| Asian | 58 | 18.77 |
| Black/African American | 28 | 9.06 |
| Multi-race | 28 | 9.06 |
| Hispanic | 19 | 6.15 |
| Middle Eastern | 8 | 2.59 |
| Hawaiian/Pacific Island | 2 | 0.64 |
| South-Asian | 2 | 0.64 |
| Persian | 1 | 0.32 |
| Prefer not to answer | 6 | 1.94 |
| Education Level | ||
| Graduate Degree | 140 | 45.31 |
| Undergraduate Degree | 107 | 34.63 |
| College/Trade | 43 | 13.92 |
| High-school | 17 | 5.50 |
| Elementary | 2 | 0.65 |
| Marital Status* | ||
| Married, engaged, or stable relationship | 285 | 92.23 |
| Dating, single, divorced, separated, widowed | 22 | 7.12 |
| Born in Canada | ||
| No | 102 | 33.01 |
| Years in Canada (mean, SD) | 16.03 | SD=11.06 |
| Parity | ||
| 0 | 172 | 55.66 |
| 1 | 99 | 32.04 |
| 2 | 31 | 10.03 |
| 3 | 7 | 2.27 |
* Data from 2 participants is missing
Sensitivity Analyses
During our analysis we explored various covariates that may have influenced our results. These included marital status, education level, and provider-type (specialist or non-specialist provider in the main SUMMIT trial study). None of these covariates significantly affected our results, so we did not include them in our final models.
Perceived Social Support and Perinatal Mental Health Symptoms
A linear regression to assess if EPDS and PCL-6 at baseline were associated with MSPSS at baseline was conducted. The model is reported in Table 2. The overall model was significant, F(2, 306)=16.06, p<.01, accounting for 9.5% of the variance in baseline MSPSS scores. PCL-6 (b=-0.06, t=-4.1, p<.01) was significantly associated with MSPSS at baseline; however, EPDS was not.
Table 2. Associations with MSPSS at Baseline.
| Independent Variable | Mean | SD | VIF | b | b 95% CI | p value | r |
| EPDS | 15.73 | 3.84 | 1.32 | -0.03 | [-0.06, 0.01] | 0.17 | -.21** |
| PCL-6 | 17.38 | 5.07 | 1.32 | -0.06*** | [-0.09, -0.03] | p<.0001 | -.30** |
|
R2= .095** 95% CI [.04, .16] |
Note: * indicates p <.05. ** indicates p <.01. *** indicates p <.001
The first hierarchical regression assessed predictors of EPDS scores at 3-months post-randomization. The model is reported in Table 3a. The overall model was significant, F(4, 303)=13.79, p<.01, accounting for 15.4% of the variance in EPDS at 3-months post-randomization. MSPSS at baseline (b=-0.71, t=-3.22, p<.01) and EPDS at baseline (b=0.37, t=5.47, p<.01) were significant predictors. We also conducted this regression model using EPDS scores from 6-months post-randomization as the outcome variable and the same overall results were found. This model is reported in Appendix A: Table S1a. The overall model was significant, F(4, 298)=10.36, p<.01, accounting for 12.2% of the variance in EPDS at 6-months post-randomization. MSPSS at baseline (b=-0.97, t=3.62, p<.01) and EPDS at baseline (b=-0.71, t=-4.43, p<.01) were both significant predictors.
Table 3a. Predicting EPDS at 3-months Post-randomization.
| Predictor | Mean | SD | VIF | b | b 95% CI | p value | r |
| MSPSS (baseline) | 5.37 | 1.18 | 1.05 | -0.71*** | [-1.17, -0.30] | 0.001 | -.24** |
| EPDS (baseline) | 15.73 | 3.84 | 1.05 | 0.37*** | [0.23, 0.50] | p<.0001 | .33** |
| Treatment dosage | 7.00 | 2.14 | 1.00 | -0.23* | [-0.48, -0.01] | 0.06 | -.10 |
| Perinatal Period | N/A Items were coded 1 or 2 based on pregnant or postpartum | N/A | 1.00 | -0.54 | [-1.61, 0.41] | 0.29 | -.07 |
|
R2= .154** 95% CI [.08, .22] |
The second hierarchical regression assessed predictors of PCL-6 scores at 3-months post-randomization. The model is reported in Table 3b. The overall model was significant, F(4, 303)=15.9, p<.01, accounting for 17.3% of the variance in PCL-6 at 3-months post-randomization. MSPSS at baseline (b=-0.65, t=-2.63, p<.01) and PCL-6 at baseline (b=0.36, t=6.29, p<.01) were both significant predictors. We also conducted this regression model using PCL-6 scores from 6-months post-randomization as the outcome variable and the same overall results were found. This model is reported in Appendix A: Table S1b. The overall model was significant, F(4, 297)=25.85, accounting for 25.8% of the variance in PCL-6 at 6-months post-randomization. MSPSS at baseline (b=-0.86, t=-3.49, p<.01) and PCL-6 at baseline (b=0.45, t=7.88, p<.01) were both significant predictors.
Table 3b. Predicting PCL-6 at 3-months Post-randomization.
| Predictor | Mean | SD | VIF | b | b 95% CI | p value | r |
| MSPSS (baseline) | 5.37 | 1.18 | 1.10 | -0.65** | [-1.14, -0.16] | 0.009 | -.25** |
| PCL-6 (baseline) | 17.38 | 5.07 | 1.10 | 0.36*** | [0.25, 0.48] | p<.0001 | .39** |
| Treatment dosage | 7.00 | 2.14 | 1.00 | -0.09 | [-0.34, 0.17] | 0.49 | -.04 |
| Perinatal Period | N/A (items were coded 1 or 2 based on pregnant or postpartum) | N/A | 1.00 | -0.55 | [-1.65, 0.55] | 0.32 | -.04 |
|
R2= .173** 95% CI [.09, .24] |
Note: * indicates p <.05. ** indicates p <.01. *** indicates p <.001
Psychosocial Stimulation, Perceived Social Support, and Perinatal Mental Health Symptoms
To determine whether social support and clinical symptoms significantly impacted psychosocial stimulation in the child’s environment (as measured by the HOME) a hierarchical regression was conducted. In the first step, EPDS and PCL-6 scores at 3-months post-randomization were added to the model. Neither were significant independent variables. MSPSS at baseline was added in the next step. The covariates (treatment dosage, perinatal period, and infant age at HOME visit) were then added in the final step. The model is reported in Table 4. The model was significant, F(6, 301)=10.9, p<.01, accounting for 17.9% of the variance in total HOME score. MSPSS at baseline (b=0.42, t=2.87, p<.01) and infant age at HOME visit (b=0.21, t=6.67, p<.01) were both significant predictors, while EPDS and PCL-6 were not.
Table 4. Predicting Total HOME Score.
| Predictor | Mean | SD | VIF | b | b 95% CI | p value | r |
| EPDS (3-months) | 8.64 | 4.84 | 1.76 | 0.04 | [-0.05, 0.13] | 0.37 | -.02 |
| PCL-6 (3-months) | 14.26 | 5.34 | 1.74 | -0.06 | [-0.14, 0.03] | 0.18 | -.09 |
| MSPSS (baseline) | 5.37 | 1.18 | 1.09 | 0.42** | [0.13, 0.71] | 0.004 | .19** |
| Infant age at HOME visit | 13.25 | 5.31 | 1.03 | 0.21*** | [0.15, 0.28] | p<.0001 | .37** |
| Treatment dosage | 7.00 | 2.14 | 1.02 | 0.12 | [-0.03, 0.27] | 0.13 | .11* |
| Perinatal Period | N/A Items were coded 1 or 2 based on pregnant or postpartum | N/A | 1.01 | -0.49 | [-1.16, 0.17] | 0.14 | -.04 |
|
R2= .179** 95% CI [.09, .24] |
Note: * indicates p <.05. ** indicates p <.01. *** indicates p <.001
Discussion
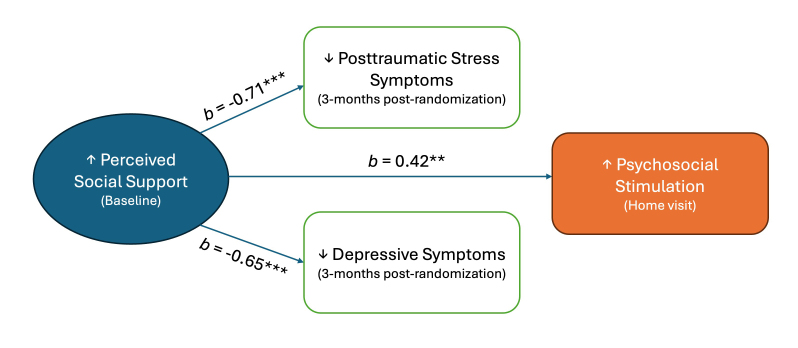
The overarching aim of the current study was to investigate the potential relations among perceived social support, common mental health symptoms (depressive and PTS symptoms), and psychosocial stimulation of the infant’s home environment. In addressing our first aim, we found that perceived social support at baseline was a significant predictor of both depressive and PTS symptoms at 3- and 6-months post-randomization, while controlling for baseline depressive and PTS symptoms. Specifically, lower perceived social support at baseline was associated with higher PTS and depressive symptomatology at 3-months and 6-months post-randomization. In addressing our second aim, we found that perceived social support at baseline was also a significant predictor of psychosocial stimulation of the home environment, while depressive and PTS symptoms at 3-months post-randomization were not, even when they were the only independent variables in the model. Specifically, higher perceived social support at baseline was associated with higher psychosocial stimulation. Figure 1 displays relations among perceived social support at baseline, depressive and PTS symptoms at 3-months post-randomization, and psychosocial stimulation at the home visit.
Figure 1.
Relations among perceived social support, perinatal mental health symptoms, and psychosocial stimulation. Standardized betas from hierarchical multiple regressions are presented. **p<.01, ***p<.001.
Our findings suggesting a negative relation between social support at baseline and 3-months post-randomization clinical symptoms are in line with previous research that has found relations between social support and perinatal mental health symptoms [60-65]. For example, Singla et al. (2019) implemented a psychosocial intervention for perinatal depression in India and Pakistan. They found that the effects of the intervention were mediated, in part, by the social support the mother received [65]. A cross-sectional study by Cho et al. (2022) in South Korea found that women with moderate or low social support were more likely to have postpartum depression [60]. Lastly, a systematic review and meta-analysis of 67 research articles on social support and mental health problems during pregnancy found that low social support is associated with depression during pregnancy [66].
Of note, significantly more past research has examined perinatal depressive symptoms than trauma-related symptoms. This study found similar correlations between perceived social support at baseline with both perinatal depressive symptoms and PTS symptoms at 3-months post-randomization. Additionally, our findings suggest that PTS symptoms at baseline were significantly associated with perceived social support at baseline while depressive symptoms were not. This highlights the need for more examination of perinatal trauma symptoms in research. Other researchers have also discussed how perinatal trauma remains understudied despite the potential long-term impact of these symptoms [67,68]. For example, Nillni et al. (2018) conducted a systematic review of 78 studies on treatment of perinatal depression, anxiety, and trauma-related disorders [67]. They found only five studies on anxiety or trauma-related disorders and highlighted the urgent need for more research on PTS during the perinatal period. PTS symptoms are likely overlooked compared to perinatal depressive and anxiety symptoms because posttraumatic stress symptoms are not screened for in research and clinical settings. Research has suggested that perinatal PTSD can be treated [69], highlighting the importance of screening for these symptoms in order to better help individuals suffering from posttraumatic stress symptoms during this period. Although past research has explored the impact of trauma on parenting behavior [70,71] and child outcomes [72,73], there is a paucity of research on the impact of trauma on the child’s home environment and, specifically, psychosocial stimulation. Our findings support the need for further research to understand the impact of posttraumatic stress symptoms in the perinatal period on the child’s environment.
Predictors of psychosocial stimulation of the home environment have not been studied widely, and there is limited research using the HOME measure, specifically. Consistent with our finding that perceived social support predicted HOME score, Pascoe and French (1993) conducted a prospective cohort study in the USA where women were recruited in their third trimester of pregnancy [74]. They found that women’s reports of their social support in their third trimester was a strong predictor of postnatal infant stimulation measured by the HOME when the infant was 4 months old. Pascoe and French (1993) found that third-trimester social support was a stronger predictor of psychosocial stimulation than other predictors, including depressive symptoms [74]. However, our findings that depressive and PTS symptoms did not predict total HOME score is inconsistent with other research. A study from Bangladesh by Nahar et al. (2015), which implemented food supplementation and psychosocial stimulation interventions for severely underweight children between the ages of 6 and 24 months, found a negative relation between depressive symptoms and HOME score [75]. This discrepancy in findings may be because our sample had a high average HOME score, which may have impeded our ability to find relations between depressive symptoms and psychosocial stimulation scores due to limited variance. Previous research has not examined the relation between perinatal posttraumatic stress symptoms and psychosocial stimulation of the infant; therefore, this is a novel contribution of the current study.
Although there is limited research using the HOME measure specifically, studies of parenting behavior more broadly often find a link between perinatal mental health symptoms and parenting behavior. For example, in a longitudinal study spanning infancy and childhood, Giallo et al. (2014) found that the relationship between maternal postnatal psychological distress and child emotional-behavioral outcomes at age 7 was mediated by hostile or irritable parenting behaviors [76]. Brookman et al. (2023) conducted a study of 48 mother-infant dyads in Australia and found that maternal depression moderated the relationship between maternal responsiveness and the infant’s vocabulary size [77]. This research is inconsistent with our findings, potentially due to psychosocial stimulation being less affected by perinatal mental health symptoms than specific parenting behaviors. Additionally, in the current sample, 285 participants (92%) reported that they were in a committed relationship or married. Thus, this finding may be partly explained by another parent or adult in the household providing psychosocial stimulation and therefore, buffering the relationship between perinatal mental health symptoms and psychosocial stimulation. Future studies would benefit from evaluating partners’ interactions with the child alongside the primary caregiver. It is also possible that because our sample was highly educated, the mothers were already more aware of the need to cognitively stimulate their child and thus this effect of mental health symptoms was not found.
Our findings highlight the importance of perceived social support when anticipating risk of perinatal mental health symptoms, delivering treatment intervention, and improving child-relevant outcomes. In the current study, perinatal women who had greater perceived social support had reduced clinical symptomatology at a later date. Perceived social support’s impact was not limited to perinatal mental health symptoms but it was also found to be significantly associated with aspects of a child’s home environment that have important implications for their development. Thus, if a mother has greater perceived social support, then the child is more likely to have a psychosocially stimulating home environment. It is important to note that the current sample had high levels of perceived social support overall. It is possible that the relations among perceived social support, perinatal mental health symptoms, and psychosocial stimulation might differ in a sample with lower social support.
Strengths and Limitations
Strengths of this study include a large and ethnically diverse sample. Almost half (47.23%) of the study participants self-identified as BIPOC, making these results potentially generalizable to a broader population. The current study also included several novel or under-researched elements, including the investigation of perinatal PTS symptoms, which are not as commonly researched as perinatal depression or anxiety despite their significant overlap (r=0.7) [3]. In addition, use of the HOME measure to explore the impact of a mother’s clinical symptoms on the child’s environment is an important contribution. The use of a longitudinal dataset with temporally distinct measurements allowed us to examine whether temporal relations between our variables of interest exist. Past research has examined the effect of maternal mental health symptoms on child outcomes (eg, internalizing and externalizing symptoms) but without probing the home environment as a potential mechanism by which these symptoms affect the child. The current study suggests that this is an important research avenue.
Despite the strengths of the current study, there were also several limitations. First, all participants were offered the same brief BA treatment for treatment of clinical symptoms, lacking comparison with participants who did not receive this treatment. To account for the role of treatment, models controlled for treatment dosage. In addition, the average total scores of the baseline MSPSS and HOME assessment were high, indicating that overall, our sample reported high perceived social support and demonstrated high psychosocial stimulation respectively. The lack of variance in psychosocial stimulation as an outcome measure in particular may have impacted our ability to find relations among our variables of interest. Future studies can explore the relations between perceived support, clinical symptomatology and child outcomes for participants with and without treatment.
Implications
Our findings speak to the active ingredient of social support in implementing mental healthcare treatments and the potential importance of including treatment components that enhance social support, including potentially incorporating significant others during treatment. The latter has been implemented in low- and middle-income countries [22-24,78-80] but minimally explored in high-income countries. Intervention can include both bolstering social support and also increasing appreciation for existing social support. Our findings can guide intervention delivery to include psychoeducation and facilitate social supports around providing psychosocial stimulation in the home. This also highlights the need for early intervention in order to mitigate the impact on the child. Identifying women during pregnancy who have low social support and working to enhance social support in psychological treatments are important areas of future research to improve the health and well-being of mother and child.
Glossary
- BA
Behavioral Activation
- BIPOC
Black, Indigenous, and other People of Color
- EPDS
Edinburgh Postnatal Depression Scale
- HOME
Home Observation Measurement of the Environment
- MSPSS
Multidimensional Scale of Perceived Social Support
- PCL-6
Abbreviated PTSD Checklist
- PTS
Posttraumatic stress
- PTSD
Post-traumatic stress disorder
- SUMMIT
Scaling Up Maternal Mental healthcare by Increasing access to Treatment
Appendix A.
Author Contributions
DRS and SNV are Study and Site PIs who, alongside NSM, oversee participant recruitment and data collection in their respective sites. TLK, MCM, and DRS conceptualized the study. TLK planned and analyzed the data, with input from all authors. All authors were involved in writing and editing the final manuscript. All authors provided final approval of the manuscript.
Funding Source
Research reported in this publication was supported by Patient-Centered Outcomes Research Institute (PCORI) under contract number PCS-2018C1-10621. The content is solely the responsibility of the authors and does not necessarily represent the official views of PCORI. SNV reports royalties from UpToDate Inc for authorship of materials on depression and pregnancy.
References
- Dozio E, Feldman M, Bizouerne C, Drain E, Laroche Joubert M, Mansouri M, et al. The transgenerational transmission of trauma: the effects of maternal PTSD in mother-infant interactions [Internet]. Front Psychiatry. 2020. Nov;11:480690. 10.3389/fpsyt.2020.480690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review [Internet]. Clin Psychol Rev. 2000. Aug;20(5):561–92. 10.1016/s0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- Clark HM, Hankin BL, Narayan AJ, Davis EP. Risk and resilience factors for psychopathology during pregnancy: an application of the Hierarchical Taxonomy of Psychopathology (HiTOP). Dev Psychopathol [Internet]. 2023. Feb 3:1-17. https://doi.org/ 10.1017/S0954579422001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . [APA]. (2022). Diagnostic and statistical manual of mental disorders 5th ed., text revised. https://doi.org/ 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Gilden J, Molenaar NM, Smit AK, Hoogendijk WJ, Rommel AS, Kamperman AM, et al. Mother-to-infant bonding in women with postpartum psychosis and severe postpartum depression: a clinical cohort study [Internet]. J Clin Med. 2020. Jul;9(7):2291. 10.3390/jcm9072291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson M, Benderix Y, Svensson I. Mothers’ and fathers’ lived experiences of postpartum depression and parental stress after childbirth: a qualitative study [Internet]. Int J Qual Stud Health Well-being. 2020. Dec;15(1):1722564. 10.1080/17482631.2020.1722564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review [Internet]. Infant Behav Dev. 2010. Feb;33(1):1–6. 10.1016/j.infbeh.2009.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myhre MC, Dyb GA, Wentzel-Larsen T, Grøgaard JB, Thoresen S. Maternal childhood abuse predicts externalizing behaviour in toddlers: a prospective cohort study [Internet]. Scand J Public Health. 2014. May;42(3):263–9. 10.1177/1403494813510983 [DOI] [PubMed] [Google Scholar]
- van de Ven MC, van den Heuvel MI, Bhogal A, Lewis T, Thomason ME. Impact of maternal childhood trauma on child behavioral problems: the role of child frontal alpha asymmetry [Internet]. Dev Psychobiol. 2020. Mar;62(2):154–69. 10.1002/dev.21900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalewski M, Cyranowski JM, Cheng Y, Swartz HA. Role of maternal childhood trauma on parenting among depressed mothers of psychiatrically ill children [Internet]. Depress Anxiety. 2013. Sep;30(9):792–9. 10.1002/da.22116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwenspoek MM, Kuehn A, Muller CP, Turner JD. The effects of early life adversity on the immune system. Psychoneuroendocrinology. 2017. Aug;82:140–54. 10.1016/j.psyneuen.2017.05.012 [DOI] [PubMed] [Google Scholar]
- Bublitz MH, Rodriguez D, Polly Gobin A, Waldemore M, Magee S, Stroud LR. Maternal history of adoption or foster care placement in childhood: a risk factor for preterm birth. Am J Obstet Gynecol. 2014;211(4), 397.e1 397.e3976. https://doi.org/ 10.1016/j.ajog.2014.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra GD, Cooper R, Kuh D. A life course approach to reproductive health: theory and methods. Maturitas. 2010. Feb;65(2):92–7. 10.1016/j.maturitas.2009.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swedo EA, D’Angelo DV, Fasula AM, Clayton HB, Ports KA. Associations of adverse childhood experiences with pregnancy and infant health. Am J Prev Med. 2023. Apr;64(4):512–24. 10.1016/j.amepre.2022.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Goodman SH, Sherwood NE, Simon GE, Ludman E, Gallop R, et al. A pragmatic randomized clinical trial of behavioral activation for depressed pregnant women. J Consult Clin Psychol. 2017. Jan;85(1):26–36. 10.1037/ccp0000151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EW, Denison FC, Hor K, Reynolds RM. Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC Pregnancy Childbirth. 2016. Feb;16(1):38. 10.1186/s12884-016-0831-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw RJ, Sweester CJ, St John N, Lilo E, Corcoran JB, Jo B, et al. Prevention of postpartum traumatic stress in mothers with preterm infants: manual development and evaluation. Issues Ment Health Nurs. 2013. Aug;34(8):578–86. 10.3109/01612840.2013.789943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinreb L, Wenz-Gross M, Upshur C. Postpartum outcomes of a pilot prenatal care-based psychosocial intervention for PTSD during pregnancy [Internet]. Arch Womens Ment Health. 2018. Jun;21(3):299–312. 10.1007/s00737-017-0794-x [DOI] [PubMed] [Google Scholar]
- Black MM, Walker SP, Fernald LC, Andersen CT, DiGirolamo AM, Lu C, et al. Lancet Early Childhood Development Series Steering Committee . Early childhood development coming of age: science through the life course. Lancet. 2017. Jan;389(10064):77–90. 10.1016/S0140-6736(16)31389-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha NA, Dos Santos Silva FP, Dos Santos MM, Dusing SC. Impact of mother-infant interaction on development during the first year of life: A systematic review [Internet]. J Child Health Care. 2020. Sep;24(3):365–85. 10.1177/1367493519864742 [DOI] [PubMed] [Google Scholar]
- Knauer HA, Ozer EJ, Dow WH, Fernald LC. Parenting quality at two developmental periods in early childhood and their association with child development. Early Child Res Q. 2019;47:396–404. 10.1016/j.ecresq.2018.08.009 [DOI] [Google Scholar]
- Nahar B, Hossain MI, Hamadani JD, Ahmed T, Grantham-McGregor S, Persson LA. Effects of psychosocial stimulation on improving home environment and child-rearing practices: results from a community-based trial among severely malnourished children in Bangladesh [Internet]. BMC Public Health. 2012. Aug;12(1):622. 10.1186/1471-2458-12-622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urke HB, Contreras M, Matanda DJ. The influence of maternal and household resources, and parental psychosocial child stimulation on early childhood development: a cross-sectional study of children 36–59 months in Honduras. Int J Environ Res Public Health. 2018. May;15(5):926. 10.3390/ijerph15050926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting intervention to address maternal psychological wellbeing and child development and growth in rural Uganda: a community-based, cluster randomised trial. Lancet Glob Health. 2015. Aug;3(8):e458–69. 10.1016/S2214-109X(15)00099-6 [DOI] [PubMed] [Google Scholar]
- Goodman SH, Muzik M, Simeonova DI, Kidd SA, Owen MT, Cooper B, et al. Maternal interaction with infants among women at elevated risk for postpartum depression [Internet]. Front Psychol. 2022. Mar;13:737513. 10.3389/fpsyg.2022.737513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludmer JA, Gonzalez A, Kennedy J, Masellis M, Meinz P, Atkinson L. Association between maternal childhood maltreatment and mother-infant attachment disorganization: moderation by maternal oxytocin receptor gene and cortisol secretion [Internet]. Horm Behav. 2018. Jun;102:23–33. 10.1016/j.yhbeh.2018.04.006 [DOI] [PubMed] [Google Scholar]
- Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA, Pollitt E, et al. International Child Development Steering Group . Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007. Jan;369(9556):145–57. 10.1016/S0140-6736(07)60076-2 [DOI] [PubMed] [Google Scholar]
- Manuel JI, Martinson ML, Bledsoe-Mansori SE, Bellamy JL. The influence of stress and social support on depressive symptoms in mothers with young children [Internet]. Soc Sci Med. 2012. Dec;75(11):2013–20. 10.1016/j.socscimed.2012.07.034 [DOI] [PubMed] [Google Scholar]
- Noyman-Veksler G, Herishanu-Gilutz S, Kofman O, Holchberg G, Shahar G. Post-natal psychopathology and bonding with the infant among first-time mothers undergoing a caesarian section and vaginal delivery: sense of coherence and social support as moderators [Internet]. Psychol Health. 2015;30(4):441–55. 10.1080/08870446.2014.977281 [DOI] [PubMed] [Google Scholar]
- Travis LA, Lyness JM, Shields CG, King DA, Cox C. Social support, depression, and functional disability in older adult primary-care patients [Internet]. Am J Geriatr Psychiatry. 2004;12(3):265–71. 10.1097/00019442-200405000-00005 [DOI] [PubMed] [Google Scholar]
- Xie RH, He G, Koszycki D, Walker M, Wen SW. Prenatal social support, postnatal social support, and postpartum depression. Ann Epidemiol. 2009. Sep;19(9):637–43. 10.1016/j.annepidem.2009.03.008 [DOI] [PubMed] [Google Scholar]
- Cho H, Lee K, Choi E, Cho HN, Park B, Suh M, et al. Association between social support and postpartum depression [Internet]. Sci Rep. 2022. Feb;12(1):3128. 10.21203/rs.3.rs-753172/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schury K, Zimmermann J, Umlauft M, Hulbert AL, Guendel H, Ziegenhain U, et al. Childhood maltreatment, postnatal distress and the protective role of social support [Internet]. Child Abuse Negl. 2017. May;67:228–39. 10.1016/j.chiabu.2017.02.021 [DOI] [PubMed] [Google Scholar]
- Armstrong MI, Birnie-Lefcovitch S, Ungar MT. Pathways between social support, family well being, quality of parenting, and child resilience: what we know [Internet]. J Child Fam Stud. 2005;14(2):269–81. 10.1007/s10826-005-5054-4 [DOI] [Google Scholar]
- Littlewood K, Swanke JR, Strozier A, Kondrat D. Measuring social support among kinship caregivers: validity and reliability of the Family Support Scale [Internet]. Child Welfare. 2012;91(6):59–78. [PubMed] [Google Scholar]
- Singla DR, Meltzer-Brody SE, Silver RK, Vigod SN, Kim JJ, La Porte LM, et al. Scaling Up Maternal Mental healthcare by Increasing access to Treatment (SUMMIT) through non-specialist providers and telemedicine: a study protocol for a non-inferiority randomized controlled trial [Internet]. Trials. 2021. Mar;22(1):186. 10.1186/s13063-021-05075-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale [Internet]. Br J Psychiatry. 1987. Jun;150(6):782–6. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Lydsdottir LB, Howard LM, Olafsdottir H, Thome M, Tyrfingsson P, Sigurdsson JF. The psychometric properties of the Icelandic version of the Edinburgh Postnatal Depression Scale (EPDS) when used prenatal [Internet]. Midwifery. 2019. Feb;69:45–51. 10.1016/j.midw.2018.10.009 [DOI] [PubMed] [Google Scholar]
- Kheirabadi GR, Maracy MR, Akbaripour S, Masaeli N. Psychometric properties and diagnostic accuracy of the edinburgh postnatal depression scale in a sample of Iranian women [Internet]. Iran J Med Sci. 2012. Mar;37(1):32–8. [PMC free article] [PubMed] [Google Scholar]
- Rubertsson C, Börjesson K, Berglund A, Josefsson A, Sydsjö G. The Swedish validation of Edinburgh Postnatal Depression Scale (EPDS) during pregnancy [Internet]. Nord J Psychiatry. 2011. Dec;65(6):414–8. 10.3109/08039488.2011.590606 [DOI] [PubMed] [Google Scholar]
- Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care [Internet]. Behav Res Ther. 2005. May;43(5):585–94. 10.1016/j.brat.2004.04.005 [DOI] [PubMed] [Google Scholar]
- Grekin R, Thomas EB, Miller ML, O’Hara MW. The role of prenatal posttraumatic stress symptoms among trauma exposed women in predicting postpartum depression [Internet]. Stress Health. 2022. Aug;38(3):610–4. 10.1002/smi.3100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Roch K, Lasater M, Woldeyes G, Solomon-Osborne A, Phan X, Bizouerne C, et al. Improving maternal mental health through postnatal services use for South Sudanese mothers and their babies living in Nguynyel refugee camp in Gambella, Ethiopia [Internet]. Eur Psychiatry. 2021;64 S1:S127. 10.1192/j.eurpsy.2021.356 [DOI] [Google Scholar]
- Han B, Wong EC, Mao Z, Meredith LS, Cassells A, Tobin JN. Validation of a brief PTSD screener for underserved patients in federally qualified health centers [Internet]. Gen Hosp Psychiatry. 2016;38:84–8. 10.1016/j.genhosppsych.2015.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, Wilkins K, Roy-Byrne PP, Golinelli D, Chavira D, Sherbourne C, et al. Abbreviated PTSD Checklist (PCL) as a guide to clinical response [Internet]. Gen Hosp Psychiatry. 2012;34(4):332–8. 10.1016/j.genhosppsych.2012.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudom K. Evaluation of three abbreviated versions of the PTSD Checklist in Canadian Armed Forces personnel. J Mil Veteran Fam Health. 2020;6(2):9–16. 10.3138/jmvfh-2019-0062 [DOI] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. Multidimensional Scale of Perceived Social Support. JPA [Internet]. 1988;52(1):30–41. 10.1037/t02380-000 [DOI] [Google Scholar]
- Hagaman A, LeMasters K, Zivich PN, Sikander S, Bates LM, Bhalotra S, et al. Longitudinal effects of perinatal social support on maternal depression: a marginal structural modelling approach [Internet]. J Epidemiol Community Health. 2021. Oct;75(10):936–43. 10.1136/jech-2020-215836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paddy A, Asamoah-Gyimah K, Nkyi A. Psychosocial determinants of postpartum depression and maternal well-being among postnatal women [Internet]. Open J Psychiatr. 2021;11(03):138–59. 10.4236/ojpsych.2021.113012 [DOI] [Google Scholar]
- Terada S, Kinjo K, Fukuda Y. The relationship between postpartum depression and social support during the COVID-19 pandemic: A cross-sectional study [Internet]. J Obstet Gynaecol Res. 2021. Oct;47(10):3524–31. 10.1111/jog.14929 [DOI] [PubMed] [Google Scholar]
- Aboud FE, Singla DR, Nahil MI, Borisova I. Effectiveness of a parenting program in Bangladesh to address early childhood health, growth and development [Internet]. Soc Sci Med. 2013. Nov;97:250–8. 10.1016/j.socscimed.2013.06.020 [DOI] [PubMed] [Google Scholar]
- Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: a confirmation study [Internet]. J Clin Psychol. 1991. Nov;47(6):756–61. [DOI] [PubMed] [Google Scholar]
- Osman A, Lamis DA, Freedenthal S, Gutierrez PM, McNaughton-Cassill M. The multidimensional scale of perceived social support: analyses of internal reliability, measurement invariance, and correlates across gender. J Pers Assess. 2014;96(1):103–12. 10.1080/00223891.2013.838170 [DOI] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support [Internet]. J Pers Assess. 1990;55(3-4):610–7. 10.1080/00223891.1990.9674095 [DOI] [PubMed] [Google Scholar]
- Elardo R, Bradley RH. The home observation for measurement of the environment (HOME) scale: a review of research [Internet]. Dev Rev. 1981;1(2):113–45. 10.1016/0273-2297(81)90012-5 [DOI] [Google Scholar]
- Burston A, Puckering C, Kearney E. At HOME in Scotland: validation of the home observation for measurement of the environment inventory [Internet]. Child Care Health Dev. 2005. Sep;31(5):533–8. 10.1111/j.1365-2214.2005.00546.x [DOI] [PubMed] [Google Scholar]
- Jones PC, Pendergast LL, Schaefer BA, Rasheed M, Svensen E, Scharf R, et al. MAL-ED Network Investigators . Measuring home environments across cultures: invariance of the HOME scale across eight international sites from the MAL-ED study [Internet]. J Sch Psychol. 2017. Oct;64:109–27. 10.1016/j.jsp.2017.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Totsika V, Sylva K. The Home Observation for Measurement of the Environment Revisited [Internet]. Child Adolesc Ment Health. 2004. Feb;9(1):25–35. 10.1046/j.1475-357x.2003.00073.x [DOI] [PubMed] [Google Scholar]
- R Core Team . R: A language and environment for statistical computing [Internet]Vienna, Austria: R Foundation for Statistical Computing; 2022.[November 2023]. [Google Scholar]
- Cho H, Lee K, Choi E, Cho HN, Park B, Suh M, et al. Association between social support and postpartum depression [Internet]. Sci Rep. 2022. Feb;12(1):3128. 10.1038/s41598-022-07248-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Zhang L, Guo N, Jiang H. Postpartum depression and postpartum post-traumatic stress disorder: prevalence and associated factors [Internet]. BMC Psychiatry. 2021. Oct;21(1):487. 10.1186/s12888-021-03432-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid KM, Taylor MG. Social support, stress, and maternal postpartum depression: A comparison of supportive relationships [Internet]. Soc Sci Res. 2015. Nov;54:246–62. 10.1016/j.ssresearch.2015.08.009 [DOI] [PubMed] [Google Scholar]
- Sufredini F, Catling C, Zugai J, Chang S. The effects of social support on depression and anxiety in the perinatal period: A mixed-methods systematic review [Internet]. J Affect Disord. 2022. Dec;319:119–41. 10.1016/j.jad.2022.09.005 [DOI] [PubMed] [Google Scholar]
- van Heumen MA, Hollander MH, van Pampus MG, van Dillen J, Stramrood CA. Psychosocial predictors of postpartum posttraumatic stress disorder in women with a traumatic childbirth experience [Internet]. Front Psychiatry. 2018. Jul;9:348. 10.3389/fpsyt.2018.00348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla DR, MacKinnon DP, Fuhr DC, Sikander S, Rahman A, Patel V. Multiple mediation analysis of the peer-delivered Thinking Healthy Programme for perinatal depression: findings from two parallel, randomised controlled trials. Br J Psychiatry. 2021. Mar;218(3):143–50. 10.1192/bjp.2019.184 [DOI] [PubMed] [Google Scholar]
- Bedaso A, Adams J, Peng W, Sibbritt D. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis [Internet]. Reprod Health. 2021. Jul;18(1):162. 10.1186/s12978-021-01209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nillni YI, Mehralizade A, Mayer L, Milanovic S. Treatment of depression, anxiety, and trauma-related disorders during the perinatal period: A systematic review [Internet]. Clin Psychol Rev. 2018. Dec;66:136–48. 10.1016/j.cpr.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera E, Chou S, Cousins N, Mota N, Reynolds K. Women’s experiences of trauma, the psychosocial impact and health service needs during the perinatal period [Internet]. BMC Pregnancy Childbirth. 2023. Mar;23(1):197. 10.1186/s12884-023-05509-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw RJ, St John N, Lilo EA, Jo B, Benitz W, Stevenson DK, et al. Prevention of traumatic stress in mothers with preterm infants: a randomized controlled trial. Pediatrics. 2013. Oct;132(4):e886–94. 10.1542/peds.2013-1331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie H, Hamilton-Giachritsis C, Alves-Costa F, Tomlinson M, Halligan SL. The impact of parental posttraumatic stress disorder on parenting: a systematic review. Eur J Psychotraumatol. 2019. Jan;10(1):1550345. 10.1080/20008198.2018.1550345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvara BJ, Mills-Koonce R, Cox M. Maternal childhood sexual trauma, child directed aggression, parenting behavior, and the moderating role of child sex [Internet]. J Fam Violence. 2017. Feb;32(2):219–29. 10.1007/s10896-016-9839-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenerci RL, DePrince AP. Intergenerational transmission of trauma: maternal trauma related cognitions and toddler symptoms [Internet]. Child Maltreat. 2018. May;23(2):126–36. 10.1177/1077559517737376 [DOI] [PubMed] [Google Scholar]
- Iyengar U, Kim S, Martinez S, Fonagy P, Strathearn L. Unresolved trauma in mothers: intergenerational effects and the role of reorganization [Internet]. Front Psychol. 2014. Sep;5:966. 10.3389/fpsyg.2014.00966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe JM, French J. Third-trimester maternal psychosocial factors and infants’ home stimulation. A prospective study. Arch Fam Med. 1993. Jun;2(6):624–7. 10.1001/archfami.2.6.624 [DOI] [PubMed] [Google Scholar]
- Nahar B, Hossain I, Hamadani JD, Ahmed T, Grantham-McGregor S, Persson LA. Effect of a food supplementation and psychosocial stimulation trial for severely malnourished children on the level of maternal depressive symptoms in Bangladesh [Internet]. Child Care Health Dev. 2015. May;41(3):483–93. 10.1111/cch.12176 [DOI] [PubMed] [Google Scholar]
- Giallo R, Cooklin A, Wade C, D’Esposito F, Nicholson JM. Maternal postnatal mental health and later emotional-behavioural development of children: the mediating role of parenting behaviour [Internet]. Child Care Health Dev. 2014. May;40(3):327–36. 10.1111/cch.12028 [DOI] [PubMed] [Google Scholar]
- Brookman R, Kalashnikova M, Levickis P, Conti J, Xu Rattanasone N, Grant KA, et al. Effects of maternal depression on maternal responsiveness and infants’ expressive language abilities [Internet]. PLoS One. 2023. Jan;18(1):e0277762. 10.1371/journal.pone.0277762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuhr DC, Weobong B, Lazarus A, Vanobberghen F, Weiss HA, Singla DR, et al. Delivering the Thinking Healthy Programme for perinatal depression through peers: an individually randomised controlled trial in India [Internet]. Lancet Psychiatry. 2019. Feb;6(2):115–27. 10.1016/s2215-0366(18)30466-8 [DOI] [PubMed] [Google Scholar]
- Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low- and middle-income countries [Internet]. Annu Rev Clin Psychol. 2017. May;13(1):149–81. 10.1146/annurev-clinpsy-032816-045217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atif N, Krishna RN, Sikander S, Lazarus A, Nisar A, Ahmad I, et al. Mother-to-mother therapy in India and Pakistan: adaptation and feasibility evaluation of the peer-delivered Thinking Healthy Programme [Internet]. BMC Psychiatry. 2017. Feb;17(1):79. 10.1186/s12888-017-1244-z [DOI] [PMC free article] [PubMed] [Google Scholar]