Abstract
Recent research exploring the relationship between the gut and the brain suggests that the condition of the gut microbiota can influence cognitive health. A well-balanced gut microbiota may help reduce inflammation, which is linked to neurodegenerative conditions. Prebiotics, probiotics, and symbiotics are nutritional supplements and functional food components associated with gastrointestinal well-being. The bidirectional communication of the gut–brain axis is essential for maintaining homeostasis, with pre-, pro-, and symbiotics potentially affecting various cognitive functions such as attention, perception, and memory. Numerous studies have consistently shown that incorporating pre-, pro-, and symbiotics into a healthy diet can lead to improvements in cognitive functions and mood. Maintaining a healthy gut microbiota can support optimal cognitive function, which is crucial for disease prevention in our fast-paced, Westernized society. Our results indicate cognitive benefits in healthy older individuals with probiotic supplementation but not in healthy older individuals who have good and adequate levels of physical activity. Additionally, it appears that there are cognitive benefits in patients with mild cognitive impairment and Alzheimer’s disease, while mixed results seem to arise in younger and healthier individuals. However, it is important to acknowledge that individual responses may vary, and the use of these dietary supplements should be tailored to each individual’s unique health circumstances and needs.
Keywords: cognitive function, prebiotic, probiotic, symbiotic, dementia, randomized controlled trial
1. Introduction
The dietary habits and lifestyle of the Western civilized world have a significant impact on the gut microbiota, influencing cognitive functions [1,2,3]. Diets rich in added sugars and refined carbohydrates, with low fiber content and limited probiotic intake, can adversely affect the gut microbiota, potentially correlating with cognitive issues [1,4]. The prevalence of artificial additives, the consumption of pre-packaged, ultra-processed foods, and high-saturated fat diets can negatively influence both the gut microbiota and cognitive health and may be linked to cardiovascular problems as well [2]. The excessive use of antibiotics and other medications can harm beneficial gut bacteria, leading to long-term negative effects on cognitive functions [3]. Sedentary lifestyles, low levels of physical activity, and chronic stress can also detrimentally impact cognitive performance [5]. Therefore, maintaining and supporting a healthy gut microbiota can contribute to optimizing cognitive functions and play a crucial role in maintaining the balance between the brain and the gut.
As the aging of society poses significant challenges to healthcare systems and societies, it becomes increasingly important to recognize the interplay between gut health and cognitive well-being, especially in older populations. Estimates suggest that by 2030, one in six members of the global population will be aged 60 or older [6]. Furthermore, the number of individuals aged 60 and above is expected to double by 2050, potentially reaching 2.1 billion. Notably, the age group over 80 years old may triple between 2020 and 2050, reaching up to 426 million [6]. The World Health Organization (WHO) emphasizes several factors to preserve cognitive functions and support health in the elderly, including maintaining a balanced diet rich in vitamins, antioxidants, and nutrients; sustaining regular physical activity; avoiding smoking; limiting alcohol consumption; preventing social isolation; and maintaining social connections. All these factors are crucial for emotional and cognitive well-being [7].
The nourishment of the gut microbiota has long involved the use of probiotic products containing various beneficial strains, as well as fermented foods and strains that specifically stimulate proper brain function through gut–brain axis stimulation [8]. According to the WHO’s definition, probiotics are “live microorganisms which, when administered in adequate amounts, confer a health benefit on the host” [9]. Probiotic dairy products contain beneficial bacteria (mainly lactobacilli and bifidobacteria) in sufficient quantities, which can potentially create a less hospitable environment for pathogens in the colon lumen, thereby hypothetically supporting the integrity of the gut flora and the immune system [10]. Another nutritional factor is dietary fibers acting as prebiotics (food for probiotic bacterial strains), as the diverse consumption of dietary fibers also promotes microbiome diversity [11]. They stimulate the growth and activity of beneficial bacteria, promote a healthy balance of the gut flora, and support digestion. Concurrently intaking probiotics and prebiotics (symbiotics) can promote a healthy gut flora balance and have strengthening effects on the immune and digestive systems [12]. Increasing research results confirm that supporting the gut flora with probiotics and strengthening the gut–brain axis can offer a new treatment alternative for those with mental health issues such as major depression, anxiety disorders, chronic fatigue syndrome, attention deficit hyperactivity disorder (ADHD), depression caused by irritable bowel syndrome (IBS), mood disorders, and stress-induced harm [13,14]. Moreover, even in healthy individuals exposed to increased stress, their positive effects on the brain and psychological well-being are evident, suggesting that their use is safe and necessary for everyone, especially in the context of Western nutrition and modern urban lifestyles [15,16]. Therefore, the aim of our comprehensive review is to examine the publications of the last 5 years, with a particular focus on the administration of probiotics, prebiotics, and symbiotics and the cognitive outcomes derived from their use.
2. Methods
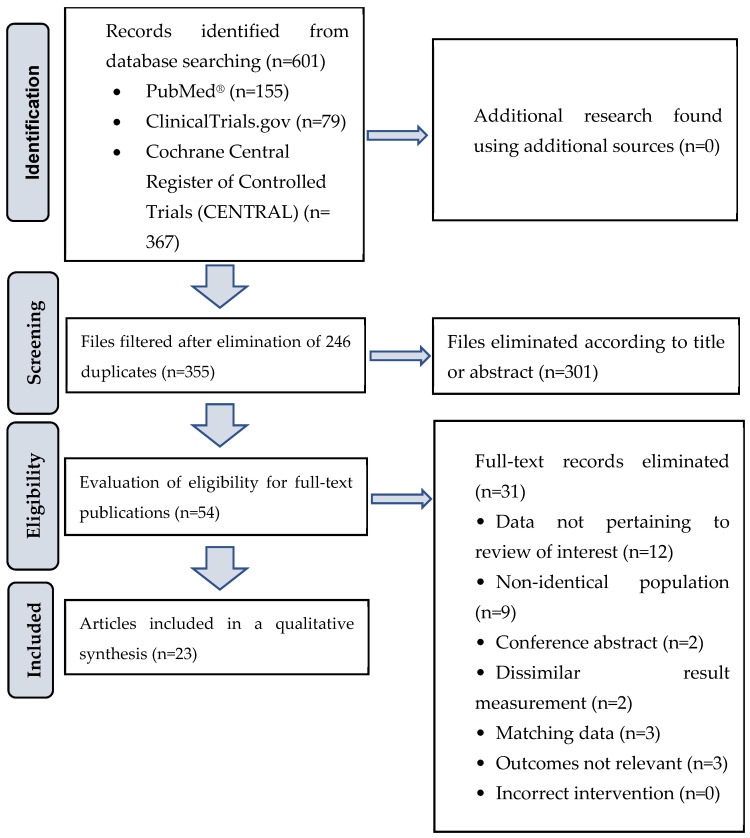
We conducted a comprehensive literature search using PubMed, ClinicalTrials.gov, and Cochrane Central Register of Controlled Trials (CENTRAL) databases from 31 January 2019 to 31 January 2024. Our focus was on randomized controlled trials (RCTs) and human clinical trials exploring dietary supplement interventions and their correlation with cognitive function. Specific and MESH keywords such as “probiotic”, “prebiotic”, “symbiotic”, “cognition”, “memory”, “executive function”, “dementia”, “mild cognitive impairment”, “Alzheimer’s disease”, “cognition disorder”, “randomized controlled trial”, and “controlled clinical trial” were used, without language restrictions. The search utilized conjunctions like “AND” or “OR” between keywords. After removing indexed duplicate articles, we screened titles and abstracts, excluding those that did not meet our inclusion criteria. The selected articles underwent careful evaluation based on their full texts. The goal of this review was to provide an up-to-date overview of the relationship between probiotics, prebiotics, symbiotics, and cognitive function, following the PICO (Population, Intervention, Comparison, and Outcomes) criteria. Table 1 outlines the inclusion and exclusion criteria, while Figure 1 illustrates a flowchart of the article selection process. In total, this review includes 23 articles, comprising 837 healthy individuals, 539 patients with mild cognitive impairment (MCI), and 299 patients with Alzheimer’s disease (AD). The current review article is a continuation of our previous study [17], which focused on specialized dietary supplements in the context of aging. Since probiotics/prebiotics are food components that can also be found in fermented foods such as live yogurt cultures, kefir, fermented soybean and probiotic fermented milk, our current summary study includes not only dietary supplement capsules.
Table 1.
Inclusion and exclusion criteria for studies in the review.
| Inclusion Criteria | Description |
|---|---|
| Study design | Randomized controlled trial or human clinical trial |
| Study population | Individuals in good health or patients admitted with a diagnosis of mild cognitive impairment or Alzheimer’s disease |
| Intervention | Prebiotic, probiotic, and symbiotic interventions |
| Language of publication | No limitations on language |
| Published articles | In the PubMed, ClinicalTrials.gov, and Cochrane Central Register of Controlled Trials (CENTRAL) databases |
| Output concepts | Score representing cognitive performance and various assessments of cognitive functions: attention, calculation, memory, verbal fluency, psychomotor speed, visual-constructional ability, neuropsychological function, reaction time, and psychocognitive tests. Various cognitive functions and their assessment tools include validated questionnaires like the Mini-Mental State Examination, Verbal Fluency Test, Repeatable Battery for the Assessment of Neuropsychological Status, Rapid Visual Information Processing, Wisconsin Card Sorting Test, Japanese version of Alzheimer’s Disease Assessment Scale, etc. |
| Exclusion Criteria | |
| In vitro studies | |
| Animal experiments | |
| Interventions targeting a range of health conditions, including but not limited to malignancies, post-traumatic stress disorder, depression, anxiety, stroke, multiple sclerosis, chronic cerebral ischemia, polycystic kidney disease, schizophrenia, bipolar disorder, autism spectrum disorder, attention deficit hyperactivity disorder, diabetes mellitus, fibromyalgia, hepatic encephalopathy, perioperative and postoperative conditions, Huntington’s disease, cirrhosis hepatis, allergic rhinitis, frailty syndrome, psychosis, mood disorders, bipolar disorder, epilepsy, portal hypertension, and a human immunodeficiency virus (HIV)-positive status | |
| Interventions tailored for various life stages and situations, including but not limited to premature, infancy, adolescence, pregnancy, and interventions designed for athletes | |
| Nutritional guidance, dietary recommendations, and food interventions | |
| Brief interventions lasting less than 4 weeks | |
| Weight loss support for overweight patients | |
Figure 1.
Flow diagram of article selection process.
3. Results
3.1. The Impact of Probiotic/Prebiotic/Symbiotic Supplementation on Cognitive Function in Individuals without Cognitive Impairment
Pro- and prebiotics, as well as symbiotics, influence the gut–brain axis, enhance the functioning of the central nervous system, and play a crucial role in the prevention and treatment of various conditions such as dementia, depression, attention deficit hyperactivity disorder, autism, chronic fatigue syndrome, etc. However, their impact is not limited to diseases; it is also noteworthy in healthy individuals. The supplementation of these products improves sleep quality through the modulation of the gut flora, plays a significant role in maintaining hormonal balance and the balanced functioning of the nervous system, and even contributes to shaping overall well-being and mood. In our review of the literature, we found that probiotic/prebiotic/symbiotic supplementation, administered for a minimum of 4 weeks (up to a maximum of 6 months), resulted in a significant improvement (p < 0.05) in cognitive performance among healthy aging individuals (over 60 years old) (see Table 2). This improvement was observed in various domains, including memory, attention, and visuospatial/constructional abilities [18,19,20,21,22,23,24,25,26]. However, one study [27] did not find a significant improvement in cognitive performance due to probiotic supplementation, specifically in seniors (average age 64.3 years) who were physically active and met recommended exercise guidelines. In healthy young individuals (under 30 years), cognitive performance did not change significantly after 8 weeks of pre–probiotic supplementation [28,29]. Although, a study with a low sample size (n = 26) involving healthy young adults (25–45 years), conducted by Cannavale CN et al. [30], reported a significant improvement in relational memory after the participants consumed a fermented probiotic beverage for 4 weeks (p < 0.05).
Table 2.
The effects of probiotic/prebiotic/symbiotic supplementation on cognitive functions in healthy subjects.
| Study | Design | Mean Follow-Up | Country | Sample Size | Average Age (Year) | Sex Male/Female (%) |
Intervention | Main Results |
|---|---|---|---|---|---|---|---|---|
| Kim CS et al. [18] | RCT | 12 weeks | Republic of Korea | 63 | 71.5 ± 4.3 | 49.06/50.94 | The research participants were administered a probiotic supplement consisting of a total of 1 × 109 CFU of Bifidobacterium bifidum BGN4 and Bifidobacterium longum BORI, suspended in soybean oil. | At week 12, individuals in the probiotics group demonstrated a notable enhancement in mental flexibility compared to those in the placebo group (p < 0.05). Enhanced cognitive and mental capabilities following the administration of probiotic supplements. |
| Shi S et al. [19] | RCT | 8 weeks | China | 60 | 64.1 ± 3.4 | 57/43 | Participants were required to consume one sachet of probiotics (BB68S, 5 × 1010 CFU per sachet) or a placebo daily. | BB68S demonstrated a significant enhancement in participants’ cognitive functions, as evidenced by a notable 18.89-point increase in the total RBANS score post-intervention (p < 0.0001). This improvement was particularly prominent in the domains of immediate memory, visuospatial/constructional abilities, attention, and delayed memory. |
| Sakurai K et al. [20] | RCT | 12 weeks | Japan | 78 | 76.8 ± 4.6 | 46/54 | The participants received a 1 g packet containing Lactiplantibacillus plantarum OLL2712 cells in a quantity exceeding 5 × 109 daily. | The analysis results indicated that the intake of OLL2712 exerted a protective effect on memory function in the elderly (p < 0.05). |
| Czajeczny D et al. [21] | RCT | 6 weeks | Poland | 38 | 19–31 | 100% female | The individuals received a probiotic supplement containing Bifidobacterium lactis BS01 and Lactobacillus acidophilus LA02. | In the group supplemented with probiotics, there was a significant improvement in cognitive performance compared to the placebo group, as assessed by the Wisconsin Card Sorting Test (WCST) (p < 0.05). |
| M Ni [22] | RCT | 12 weeks | United Kingdom | 72 | >60 | 37/63 | The elderly subjects received a daily intake of one sachet of prebiotic dietary supplement. | In comparison to the placebo group, the prebiotic intervention arm exhibited an enhanced cognition factor score (0.482; 95% CI 0.823–0.141; p = 0.014). |
| Azuma N et al. [23] | RCT | 12 weeks | Japan | 80 | 64.6 ± 7.1 | 50/50 | During the 12-week study period, participants ingested test drinks containing 1 × 1010 CFU of GCL2505 per 100 g along with 2.0 g of inulin per 100 g. | Substantial enhancements were observed in the scores within the neurocognitive index domain (p = 0.027), evaluating overall cognitive function, as well as across the attention, cognitive flexibility, and executive function domains (p = 0.044). |
| Berding K et al. [24] | RCT | 4 weeks | Ireland | 18 | 26 ± 1.3 | 100% female | The female participants received 12.5 g of Litesse® Ultra (>90% polydextrose (PDX) polymer). | PDX demonstrated enhanced cognitive flexibility, indicated by a reduction in errors during the Intra–Extra Dimensional Set Shift (IED) task. Improved sustained attention was evident through a higher number of correct responses and rejections in the Rapid Visual Information Processing (RVP) task. |
| Sanborn V et al. [25] | RCT | 3 months | USA | 145 | 64.3 ± 5.5 | 40.7/59.3 | The intervention involved Culturelle Vegetarian Capsules which contained a blend of 10 billion CFUs of Lactobacillus rhamnosus GG for the experimental group. | Probiotic supplementation with Lactobacillus rhamnosus GG was linked to enhanced cognitive performance in middle-aged and older adults (p < 0.05). |
| Louzada ER et al. [26] | RCT | 6 months | Brazil | 49 | 77.2 ± 1.3 | 80/20 | The synbiotic group was administered two daily doses (6 g + 6 g) of a compound containing fructooligosaccharide (6 g), L. paracasei (109 CFU), L. rhamnosus (109 CFU), L. acidophilus (109 CFU), and B. lactis (109 CFU). | According to their results, the supplement exhibits modest effects on reducing depressive symptoms and more favorable effects on cognitive functions in elderly individuals (MMSE; p < 0.05). |
| Sanborn V et al. [27] | RCT | 8 weeks | USA | 127 | 64.3 ± 3.6 | 42/58 | The probiotic supplement for the subjects was Lactobacillus rhamnosus GG (2 × 1010 CFU/day). | The probiotic intervention did not influence cognitive performance. |
| Edebol Carlman HMT et al. [28] | RCT | 8 weeks | Sweden | 22 | 24.2 ± 3.4 | 27/73 | The subjects received a combination of three probiotic strains—Lactobacillus helveticus R0052 (CNCM-I-1722; 2 × 109 CFU), Lactiplantibacillus plantarum R1012 (CNCM-I-3736; 8 × 108 CFU), and Bifidobacterium longum R0175 (CNCM-I-3470; 7 × 107 CFU)—at a dosage of 3 g per day. | The probiotic intervention did not influence cognitive performance. |
| Ascone et al. [29] | RCT | 4 weeks | Germany | 59 | 27.1 ± 6.7 | 43/57 | The participants received a multi-strain probiotic (Vivomixx®) at a daily dosage of 4.4 g. | The administered multi-strain probiotic did not induce any effects on cognition or mental well-being in young, healthy adults. |
| Cannavale CN et al. [30] | RCT | 4 weeks | USA | 26 | 25–45 | 58/42 | Participants underwent testing before and after a 4-week consumption period, which included 8 oz of a dairy-based fermented beverage containing 25–30 billion CFUs of live and active kefir cultures. | The fermented dairy beverage led to enhanced performance in two aspects of relational memory: misplacement (p = 0.04) and object-location binding (p = 0.03). |
BB68S: Bifidobacterium longum BB68S; CFU: colony-forming unit; IED: Intra–Extra Dimensional; PDX: polydextrose; RCT: randomized controlled trial; RBANS: Repeatable Battery for the Assessment of Neuropsychological Status; RVP: Rapid Visual Information Processing; WCST: Wisconsin Card Sorting Test.
3.2. The Influence of Probiotic/Prebiotic/Symbiotic Supplementation on Cognitive Function in Individuals Diagnosed with Mild Cognitive Impairment
In our analysis, six RCTs [31,32,33,34,35,36] were carefully chosen, revealing a significant improvement in cognitive functions, including improvements in MMSE and Japanese version of Alzheimer’s Disease Assessment Scale (ADAS-Jcog) scores, in both male and female subjects (see Table 3). For mild cognitive impairment (MCI) patients aged over 60, a regimen of probiotics like Lactobacillus, Bifidobacterium, and a prebiotic (inulin) was administered for 2–6 months, once or twice a day, with a dosage of ×1010 CFU/day. Asaoka et al.’s study [32] highlighted that Bifidobacterium breve MCC1274 administration enhanced cognitive function in individuals with MCI, showing an improvement in scores on specific neuropsychological test subscales, especially ADAS-Jcog and MMSE. Additionally, the 24-week probiotic supplementation effectively slowed the progression of brain atrophy, evaluated through the voxel-based specific regional analysis system for Alzheimer’s disease (VSRAD) based on brain magnetic resonance imaging (MRI). Xiao J et al.’s [33] groundbreaking double-blind, placebo-controlled human trial demonstrated the cognitive enhancement benefits of Bifidobacterium breve A1 in suspected MCI individuals. Both primary (Repeatable Battery for the Assessment of Neuropsychological Status; RBANS) and secondary endpoints (Japanese version of the MCI Screen; JMCIS) were successfully achieved after 16 weeks of consistent consumption. The treatment demonstrated excellent tolerability, with no side effects being reported. The findings unveiled a significant enhancement in cognitive functions among participants receiving B. breve A1 compared to the placebo group. Notably, the RBANS score exhibited a remarkable 11.3-point improvement with B. breve A1 compared to the placebo (p < 0.0001). Improvements were also noted in RBANS domain scores, including immediate memory (p < 0.0001), visuospatial/constructional (p < 0.0001), and delayed memory (p < 0.0001). Fei Y et al.’s study [34] demonstrated the effectiveness of probiotic interventions in restoring various symptoms in MCI, indicating improvements in multiple neural behaviors, enhanced sleep quality, and the alleviation of recorded gastrointestinal symptoms through probiotic supplementation. Kobayashi et al. [35] observed positive outcomes after administering probiotics to elderly individuals with MCI for 24 weeks, showing that the intervention favorable effects on MMSE scores, suggesting an amelioration of cognitive impairment and a potential reduction in the risk of dementia. Hence, dietary supplementation with probiotics and prebiotics emerges as a novel, accessible therapeutic option for treating or preventing MCI without side effects.
Table 3.
The impacts of probiotic/prebiotic/symbiotic supplementation on cognitive functions in patients with mild cognitive impairment.
| Study | Design | Mean Follow-Up | Country | Sample Size | Average Age (Year) | Sex Male/Female (%) |
Intervention | Main Results |
|---|---|---|---|---|---|---|---|---|
| Aljumaah MR et al. [31] | RCT | 3 months | USA | 169 | 64.4 ± 5.5 | 38/48 | The LGG supplementation consisted of two capsules of Culturelle Vegetarian Capsules comprising a blend of 10 billion CFUs of Lactobacillus rhamnosus GG and 200 mg of prebiotic inulin derived from chicory root extract. | The reduction in the relative abundance of the Prevotella and Dehalobacterium genera following LGG supplementation in the MCI group showed a correlation with an enhanced cognitive score. |
| Asaoka D et al. [32] | RCT | 24 weeks | Japan | 130 | 77.2 ± 5.8 | 26/29 | The patients received a daily dosage of a probiotic (B. breve MCC1274, 2 × 1010 CFU/day). | The ADAS-Jcog subscale “orientation” showed significant improvement; MMSE subscales “orientation in time” and “writing” demonstrated significant improvement, specifically in the subgroup with lower baseline MMSE scores (p < 0.05). |
| Xiao J et al. [33] | RCT | 16 weeks | Japan | 79 | 61.3 ± 7.7 | 100% male | The patients received a daily dosage of a probiotic (B. breve A1, 2 × 1010 CFU/day). | The probiotic group exhibited a significant improvement in RBANS total score (p < 0.0001). Notably, there was a substantial enhancement in domain scores, including immediate memory, visuospatial/constructional, and delayed memory (p < 0.0001), observed in both intention-to-treat (ITT) analysis and per-protocol (PP) analysis. |
| Fei Y et al. [34] |
RCT | 12 weeks | China | 42 | 76.4 ± 9.6 | 90/10 | The group receiving the probiotic received a daily dosage of 2 g of a probiotic blend. | The probiotic group exhibited a notably higher MMSE score (24.75 ± 2.47), and there were significant improvements in attention and calculation (0.90 ± 0.79 vs. 0.65 ± 0.74, p < 0.001) and recall scores (1.95 ± 0.76 vs. 0.70 ± 0.47, p < 0.001) in comparison to the control group. |
| Kobayashi Y et al. [35] | RCT | 8 weeks | Japan | 19 | 82.5 ± 5.3 | 2/98 | The patients received B. breve A1 capsules, each containing more than 1 × 1010 CFU (2 × 1010 CFU/day). | MMSE scores showed a significant increase during the intervention (+1.7, p < 0.01). POMS2 and GSRS scores exhibited significant improvement during the intervention. |
| Hwang YH et al. [36] | RCT | 12 weeks | Korea | 100 | 69.2 ± 7.0 | 28/72 | Lactobacillus plantarum C29-fermented soybean (DW2009) 800 mg per day (1 × 1010 CFU/day). | The group receiving DW2009 exhibited more significant enhancements in overall cognitive functions (z = 2.36, p = 0.02), particularly in the attention domain (z = 2.34, p = 0.02). |
ADAS-Jcog: Japanese version of Alzheimer’s Disease Assessment Scale; CFU: colony-forming unit; DW2009: Lactobacillus plantarum C29-fermented soybean; GSRS: Gastrointestinal Symptom Rating Scale; ITT: intention-to-treat; LGG: Lactobacillus rhamnosus GG; MCI: mild cognitive impairment; MMSE: Mini-Mental State Examination; POMS2: Profile of Mood States 2nd Edition; RCT: randomized controlled trial; RBANS: Repeatable Battery for the Assessment of Neuropsychological Status.
3.3. The Effect of Probiotic Supplementation on Cognitive Function in Individuals Afflicted by Alzheimer’s Disease
In our comprehensive research, we delved into four studies, including three RCTs and one clinical study, investigating the impact of probiotic supplementation on cognitive functions in elderly patients with Alzheimer’s disease. The average follow-up period across these studies was 12 weeks. One study involved patients receiving a probiotic fermented dairy beverage at a dosage of 2 mL/kg/day [37], while three other studies administered the probiotic in capsule form, with a dosage of twice 1015 CFU/day [37,38,39,40]. Additionally, one study included selenium supplementation at a dose of 200 μg/day [40]. The outcomes revealed a significant improvement in the measured cognitive functions, particularly in memory and attention, as evident in the MMSE test (see Table 4). Ton AMM et al.’s study [37] provided an initial assessment of the positive impacts of kefir supplementation over 90 days on cognitive function, along with the biomarkers associated with systemic oxidative stress, inflammation, and cell damage in elderly individuals with Alzheimer’s disease. Akhgarjand et al.’s trial [38], focusing on probiotic supplementation’s influence on cognitive status in patients with mild and moderate Alzheimer’s disease, demonstrated a noteworthy enhancement in MMSE total score. Moreover, improvements were observed in the categorical verbal fluency test (CFT), Activities of Daily Living (AD), and Generalized Anxiety Disorder (GAD-7) in response to probiotic supplementation. Kobayashi Y et al. [39] explored the effects of a 12-week supplementation with Bifidobacterium breve in elderly Japanese patients experiencing difficulties with their memory, reporting a significant increase in both Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) scores and MMSE total scores. Tamtaji et al.’s study [40] showcased that the co-supplementation of probiotics and selenium over a 12-week period in Alzheimer’s disease patients had positive effects on MMSE score; hs-CRP; serum total antioxidant capacity; total glutathione; markers of insulin metabolism; triglycerides; and VLDL-, LDL-, and total/HDL cholesterol ratios. However, it did not impact other biomarkers associated with inflammation and oxidative stress.
Table 4.
Impacts of probiotic/prebiotic/symbiotic supplementation on cognitive functions in patients with Alzheimer’s disease.
| Study | Design | Mean Follow-Up | Country | Sample Size | Average Age (Year) | Sex Male/Female (%) |
Intervention | Main Results |
|---|---|---|---|---|---|---|---|---|
| Ton AMM et al. [37] | Clinical Trial | 90 days | Brazil | 13 | 78.7 ± 3 | 15/85 | The participants received a probiotic fermented milk (4% kefir) supplement at a dosage of 2 mL/kg/day 1. | Most patients exhibited a notable improvement in memory, visual–spatial/abstraction abilities, and executive/language functions (p < 0.05). |
| Akhgarjand et al. [38] | RCT | 12 weeks | Iran | 90 | 67.9 ± 7.9 | 33/67 | They received probiotic capsules containing L. rhamnosus HA (each capsule with 1015 CFU probiotics) or probiotic capsules containing B. longum R0175 (1015 CFU probiotics per capsule) twice daily. | Cognition showed a significant improvement with MMSE (p < 0.0001). Post hoc comparisons revealed a notably greater enhancement in the B. longum intervention group (4.86, 95% CI: 3.91–5.81; p < 0.0001) compared to both the placebo and L. rhamnosus intervention groups (4.06, 95% CI: 3.11–5.01; p < 0.0001). |
| Kobayashi Y et al. [39] | RCT | 12 weeks | Japan | 117 | 61.5 ± 6.8 | 49/51 | The individuals took two capsules every day, each containing around more than 2.0 × 1010 CFU of B. breve A1. | In a stratified analysis, a notable distinction emerged between the B. breve A1 and placebo groups concerning the ‘immediate memory’ subscale of RBANS and the total MMSE score in participants with a low RBANS total score at the baseline. The scores on the ‘language’ and ‘attention’ subscales showed a significant increase. |
| Tamtaji et al. [40] | RCT | 12 weeks | Iran | 79 | 76.2 ± 8.1 | 50/50 | The patients received selenium (200 μg/day) plus a probiotic containing Lactobacillus acidophilus, Bifidobacterium bifidum, and Bifidobacterium longum (each at 2 × 109 CFU/day). | The combined use of the probiotic and selenium resulted in a significant improvement in the MMSE test (p < 0.001). Cognitive functions significantly improved. |
RCT: randomized controlled trial; CFU: colony-forming unit; MMSE: Mini-Mental State Examination; RBANS: Repeatable Battery for the Assessment of Neuropsychological Status; 1 Probiotic fermented milk containing Acetobacter aceti, Acetobacter spp., L. kefiranofaciens, L. delbrueckii, L. fructivorans, L. fermentum, Enterococcus faecium, Leuconostoc spp., Candida famata, and krusei.
4. Discussion
Probiotics, prebiotics, and symbiotics support the health of the digestive system and have gained increasing attention recently for their positive effects on cognitive functions and dementia prevention. Various studies [41,42,43] and our current review suggest that probiotics may help and slow down the decline in cognitive abilities in older age. Prebiotics can facilitate the growth and activity of probiotics, contributing to the health of the gut flora, which may play a role in the functioning of the immune and nervous systems [44]. Symbiotics may also offer additional benefits for both gut flora and cognitive health [45]. In conclusion, our review indicates that there is a close connection between the gut microbiome and cognitive aging. Through pursuing further investigations, we could realize the practical applications of theoretical findings. The more evidence we accumulate, the more likely targeted interventions will slow the decline in cognitive abilities in older age.
The microbiome–gut–brain axis is a complex system that describes interactions between the brain, the gut, and the microbiome [4,46,47,48]. There are numerous ways in which the microbiome and the brain interact, partially realized through direct neuronal, hormonal, and immune pathways [49,50]. During aging, the composition of the microbiome may change, influencing cognitive health [51,52]. As time progresses, microbiome diversity may decrease, potentially due to aging processes and cognitive decline [4,53,54]. Additionally, inflammatory processes may become more prevalent during aging [55], potentially harming brain structures and functions, indicating a bidirectional relationship. The question arises: how do probiotics exert their effects? Among several possible mechanisms, the production of neurotransmitters such as γ-aminobutyric acid (GABA), serotonin, catecholamines, and acetylcholine is a key consideration [56]. These compounds can directly impact neural activity, cognitive functions, mood, and emotional well-being. Another effect on neurological performance occurs through the stress response system, specifically via the inhibition of the hypothalamic–pituitary–adrenal (HPA) axis and cortisol synthesis. Researchers believe that irregular functioning of the HPA axis may underlie mood disorders and cognitive problems [57]. The third essential point is that gut microorganisms participate in regulating the immune system’s function [58]. Therefore, probiotics have anti-inflammatory effects, and inflammatory responses can influence the functioning of neurons in the brain and cognitive functions [59]. It is worth noting that gut microorganisms also contribute to the production of certain vitamins and minerals, which are crucial for the brain and cognitive functions [17,60].
According to numerous researchers, a close association can be observed between chronic inflammation, elevated levels of inflammatory mediators, factors supporting inflammation in the body, and the development of cognitive and/or mood disorders [61,62,63,64]. Susceptibility to inflammation in the body can be heightened by abdominal obesity (metabolically active adipose tissue) [65] and the phenomenon of Leaky Gut Syndrome [66], attributed to the impaired functioning of the intestinal mucosal barrier and its underlying microbiome. Disruption of the cohesive microbial layer ensuring the integrity and healthy functioning of the intestinal mucosa increases the vulnerability of the mucosa and enhances the risk of developing Leaky Gut Syndrome. The essence of this negative process involves the opening of junctional structures between intestinal mucosal cells, allowing protein fragments, bacteria, or bacterial-derived substances to enter the circulation. These circulating substances trigger an immune response, leading to sterile inflammation in tissues, enhancing the production of inflammatory factors (resulting in subclinical inflammation at the systemic level), and potentially serving as the basis for autoimmune processes [67]. It is likely that chronic low-grade sterile inflammation also plays a role in age-related alterations in the cerebral microcirculation, contributing to the pathogenesis of vascular cognitive impairment [68,69,70,71,72,73,74,75,76,77,78,79]. Probiotics play a crucial role in directly inhibiting inflammation threatening the nervous system and may prevent the circulation of substances that activate the immune system [42]. In summary, when consumed in the form of beneficial strains as probiotics, these microorganisms positively influence brain function, enhance cognitive functions, improve overall well-being, and contribute to a healthier life in terms of emotion and mood regulation for both healthy individuals and those suffering from cognitive disorders. Additionally, they enhance resilience against stress [14,18]. Studies indicate their positive effects on the brain and cognitive functions, even in fundamentally healthy individuals exposed to increased stress [80,81]. When applying probiotics, attention should be given to dosage and duration; ideally, they should be taken for a minimum of 4 weeks at a dosage of at least 10 billion CFUs per day [82].
In the case of MCI, cognitive, attentional, and memory functions are no longer as proficient as in healthy aging, but the decline has not yet reached the level of dementia. MCI can be considered a precursor to dementia, where solving complex tasks and understanding written information become challenging [83]. The prevalence of MCI is 6.7% at the age of 60–64 years, 8.4% at 65–69 years, 10.1% at 70–74 years, 14.8% at 75–79 years, and 25.2% at 80–84 years. The significance of this condition lies in the fact that within 2 years, dementia develops in 14.9% of individuals affected by MCI [84]. Currently, there is no known medication capable of preventing the progression of MCI into dementia. According to the guidelines of the American Academy of Neurology (AAN), physical activity and exercise are primarily encouraged in MCI cases, in contrast to pharmacological therapy [84]. Cognitive training, establishing proper sleep hygiene, managing potential depression, and improving quality of life are measures that can also alleviate MCI symptoms [84,85]. An important task is to identify other modifiable risk factors. Existing results suggest that probiotic treatment has a positive impact on cognitive abilities in individuals with MCI [86,87]. In our current study, the most commonly used bacterial strains were various types of Lactobacillus and Bifidobacterium breve. Patients received these probiotics for varying durations, ranging from 8 to 24 weeks. All six RCT studies showed significant results, indicating that individuals consuming probiotics achieved significantly better outcomes on tests such as the Mini-Mental State Examination. Overall, the consumption of probiotics had a positive effect on the cognitive abilities of individuals with MCI.
The development of Alzheimer’s disease [69,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107] and the mechanisms through which the microbiome can contribute to the progression of Alzheimer’s disease have been investigated [108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138]. Numerous studies are also available regarding treatments with probiotics [139,140,141,142]. In one study [143], it was observed that the consumption of a combined probiotic preparation (Lactobacillus acidophilus, Lactobacillus casei, Bifidobacterium bifidum, and Lactobacillus fermentum) for 12 weeks had a significantly positive impact on the cognitive abilities of the study participants in the Mini-Mental State Examination compared to the control group. Our current research reinforces these findings [38,39,40]. Results from a meta-analysis analyzing 12 published studies [144] suggest that adhering more closely to the Mediterranean diet is associated with a lower likelihood of dementia, Alzheimer’s disease, and overall cognitive decline. A more recent meta-analysis examining 34,168 participants [145] reached a similar conclusion: individuals following a plant-based Mediterranean diet have a 21% lower likelihood of developing cognitive impairments and a 40% lower likelihood of developing Alzheimer’s disease. This study also highlights positive changes in the gut microbiota among individuals following a plant-based diet, which can be attributed to a diet rich in probiotics and fiber. According to this study, at least one-third of individuals with Alzheimer’s disease may have developed the condition due to lifestyle-related factors [145]. Therefore, it will be crucial in the future to explore other lifestyle factors that may influence the state of the gut microbiota, for which we currently lack information, as well as to understand the specific mechanisms through which the gut microbiome affects cognitive functions.
While research studies on probiotics and neurodegenerative diseases are still ongoing and interest in them is increasing, another research topic has emerged in the literature, namely the concept of “para-probiotics” and “postbiotics”, which play an important role in understanding the benefits of fermented foods even after cooking [146]. This research topic focuses on the concept of “functional food”, which refers to foods that can provide additional health benefits beyond basic nutrition. Para-probiotics are microorganisms that mimic probiotic effects but do not survive in the gastrointestinal tract. These substances can function similarly to probiotics, as they can improve gut flora composition or support the immune system, but they do not remain present in the gut for as long as traditional probiotics. On the other hand, postbiotics are substances produced during digestion, such as short-chain fatty acids, which can also contribute to maintaining a healthy gut flora.
Tempeh is a fermented soy product traditionally of Indonesian origin that is becoming increasingly popular worldwide among those following vegetarian and vegan diets. Tempeh can be considered a functional food because it is rich in protein, fiber, and other nutrients, as well as probiotics and bioactive compounds such as isoflavonoids. Research indicates that consuming tempeh may offer several health benefits, including reducing the risk of cardiovascular diseases, normalizing blood lipid levels, reducing the risk of diabetes, supporting bone health, and even reducing the risk of cancer. Furthermore, due to its high protein content, tempeh may be beneficial for individuals following vegetarian and vegan diets who need to ensure adequate protein intake. In terms of future prospects, further research is needed to better understand the relationship between tempeh and human health, as well as its effects on various health conditions and populations. Additionally, further developing tempeh and increasing its consumption could contribute to diversifying our diets and promoting healthier lifestyles [146].
In the context of preventing healthy aging and dementia, as well as preserving cognitive functions, several factors play a crucial role. Regular physical activity and maintaining a healthy diet and optimal weight are key elements in preserving healthy aging and cognitive functions [7]. In addition, maintaining social relationships and social interactions can contribute to brain health and the preservation of cognitive functions [147]. Engaging in mental challenges such as learning, solving puzzles, reading, creative activities, and intellectual stimulation can help to maintain and enhance cognitive functions [148]. Adequate sleep plays a significant role in brain regeneration and the maintenance of cognitive functions. Chronic sleep deprivation may increase the risk of dementia [149]. Optimal stress management and maintaining emotional well-being, along with maintaining a healthy cardiovascular system, are also important, as good blood circulation contributes to the brain receiving an adequate supply of oxygen [150]. Diabetes and high blood sugar levels are associated with the development of dementia [151], emphasizing the importance of monitoring blood sugar levels and adopting a balanced diet [152]. These factors collectively contribute to preserving health and cognitive functions in older age. However, it is important to note that each individual is unique, and genetic factors may also play a role in cognitive health and the development of dementia. Nevertheless, adopting a healthy lifestyle and preventive measures can offer a wide range of benefits.
Promoting healthy aging is a prioritized concern, given the rapidly aging population in Europe and the rest of the world [153]. Research areas focusing on the potential positive effects of this process on cognitive functions and the favorable regulatory impact on the gut microbiota, including the investigation of supplementation with vitamins, antioxidants, and omega-3 fatty acids, are of paramount importance [17,154]. This summary study provides substantial evidence supporting the use of probiotics as an alternative strategy for promoting cognitive health in aging. Daily supplementation with probiotics may have beneficial effects on cognitive functions such as memory and attention in both young and elderly individuals, whether healthy or ill [29,155]. This summary underscores the critical importance and urgency of using probiotics and advancing research related to cognitive aging. Ongoing studies aim to deepen our understanding of the interactions within the microbiome–gut–brain axis, particularly exploring mechanisms between the gastrointestinal tract and the nervous system [122,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171]. Future research should focus on more precise analyses and explorations of the composition of gut microbiota, identifying which strains are dominantly associated with conditions such as anxiety, depression, Parkinson’s disease, and other psychiatric and cognitive disorders, including Alzheimer’s disease [172,173,174,175,176,177,178,179,180,181,182,183,184]. Areas that remain less explored, such as the various negative associations of different bacterial strains, including inflammatory diseases, neuroinflammation, and metabolic disorders or postpartum depression, require further investigation for a deeper understanding. It is crucial to emphasize that probiotics are not miracle cures, and supporting healthy aging requires other fundamental factors, including a healthy diet, regular exercise, and an adequate quantity and quality of sleep, all of which contribute to overall health and well-being.
5. Limitations
Among the limitations, it is crucial to mention the small sample sizes in the studies (some less than 50 participants), which could have been a significant confounding factor in our research. Additionally, some studies only administered probiotics for a short duration (4 weeks). In the studies, the exclusion of the intake of other dietary supplements (e.g., vitamins, antioxidants, omega-3 supplements) was not addressed, nor was there any inquiry about antibiotic use. The studies did not exclude the application of various diets such as vegan, Mediterranean, Dietary Approaches to Stopping Hypertension (DASH Diet), Mediterranean–DASH Intervention for Neurodegenerative Delay (MIND diet), etc., which directly influence gut flora composition and may affect cognitive functions. Another essential confounding factor in cognitive performance is the level of physical activity, which was also not considered in the included studies, with one exception. Furthermore, the examined studies utilized different cognitive measurement scales, making a comparison between them impossible. They also did not exclude other mental activities or the use of herbs, coenzymes, micronutrients, etc., in their research. Although numerous research plans exist, few studies have been completed, and no precise dosage regimen has been defined for various types and stages of dementias with the identification of disease-specific probiotic strains; this needs to be determined in future research. In addition, future research should incorporate prospective studies to investigate whether the long-term use of probiotic supplements can contribute to preventing cognitive decline.
6. Conclusions
Based on our findings, it can be stated that the supplementation of probiotics, prebiotics, and symbiotics improves cognitive performance in both healthy individuals and those with cognitive disorders (e.g., MCI/AD), even after regular intake for just 1–2 months. However, for the confirmation of these results, further long-term clinical studies are necessary to gain a more precise understanding of the neuroprotective effects of these dietary supplements. It will also be crucial to determine how patients in different stages of various degenerative conditions respond to probiotic supplementation at different dosages during the progression of the disease. Therefore, additional long-term randomized controlled trials are required.
Abbreviations
AD: Alzheimer’s disease; ADAS-Jcog: Japanese version of Alzheimer’s Disease Assessment Scale; BB68S: Bifidobacterium longum BB68S; CENTRAL: Central Register of Controlled Trials; CFU: colony-forming unit; DW2009: Lactobacillus plantarum C29-fermented soybean; GSRS: Gastrointestinal Symptom Rating Scale; IED: Intra–Extra Dimensional; ITT: intention-to-treat; LGG: Lactobacillus rhamnosus GG; MCI: mild cognitive impairment; MMSE: Mini-Mental State Examination; PDX: polydextrose; POMS2: Profile of Mood States 2nd Edition; RBANS: Repeatable Battery for the Assessment of Neuropsychological Status; RCT: randomized controlled trial; RVP: Rapid Visual Information Processing; SO: soybean oil; VSRAD: voxel-based specific regional analysis system for Alzheimer’s disease; WCST: Wisconsin Card Sorting Test; WHO: World Health Organization.
Author Contributions
J.T.V., A.L., and M.F. designed the study and wrote and published the manuscript. S.T., V.F.-P., and T.C. supplemented and reviewed the manuscript. D.M., A.L. and Z.C. prepared the manuscript for publication. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Project: no. TKP2021-NKTA-47 was funded by the National Research, Development and Innovation Fund under the TKP2021-NKTA, with support from the Ministry of Innovation and Technology of Hungary. The project was funded by the Ministry of Innovation and Technology under the National Cardiovascular Laboratory Program (RRF-2.3.1-21-2022-00003) from the National Research, Development and Innovation Fund. This work was also supported by the European University for Well-Being (EUniWell) program (grant agreement number: 101004093/EUniWell/EAC-A02-2019/EAC-A02-2019-1) and the National Institute on Aging (NIA R03AG070479, NIA K01AG073614), the American Heart Association (AHA CDA941290), the NIA-supported Geroscience Training Program in Oklahoma (T32AG052363), the NIA-supported Oklahoma Nathan Shock Center, and the NIGMS-supported Center of Biomedical Research Excellence (CoBRE) (1P20GM125528-01A1). MF and MD were supported by the ÚNKP-23-4-I-SE-2 and ÚNKP-23-3-II-SE-14 New National Excellence Program of the Ministry for Innovation and Technology from the source of the National Research, Development and Innovation Fund, respectively. The funding sources played no role in the design of the study; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Clemente-Suárez V.J., Beltrán-Velasco A.I., Redondo-Flórez L., Martín-Rodríguez A., Tornero-Aguilera J.F. Global Impacts of Western Diet and Its Effects on Metabolism and Health: A Narrative Review. Nutrients. 2023;15:2749. doi: 10.3390/nu15122749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tristan Asensi M., Napoletano A., Sofi F., Dinu M. Low-Grade Inflammation and Ultra-Processed Foods Consumption: A Review. Nutrients. 2023;15:1546. doi: 10.3390/nu15061546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patangia D.V., Anthony Ryan C., Dempsey E., Paul Ross R., Stanton C. Impact of antibiotics on the human microbiome and consequences for host health. MicrobiologyOpen. 2022;11:e1260. doi: 10.1002/mbo3.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhari D.S., Jain S., Yata V.K., Mishra S.P., Kumar A., Fraser A., Kociolek J., Dangiolo M., Smith A., Golden A., et al. Unique trans-kingdom microbiome structural and functional signatures predict cognitive decline in older adults. Geroscience. 2023;45:2819–2834. doi: 10.1007/s11357-023-00799-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park J.H., Moon J.H., Kim H.J., Kong M.H., Oh Y.H. Sedentary lifestyle: Overview of updated evidence of potential health risks. Korean J. Fam. Med. 2020;41:365. doi: 10.4082/kjfm.20.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noto S. Perspectives on Aging and Quality of Life. Healthcare. 2023;11:2131. doi: 10.3390/healthcare11152131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dominguez L.J., Veronese N., Vernuccio L., Catanese G., Inzerillo F., Salemi G., Barbagallo M. Nutrition, physical activity, and other lifestyle factors in the prevention of cognitive decline and dementia. Nutrients. 2021;13:4080. doi: 10.3390/nu13114080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi L.H., Balakrishnan K., Thiagarajah K., Ismail N.I.M., Yin O.S. Beneficial properties of probiotics. Trop. Life Sci. Res. 2016;27:73. doi: 10.21315/tlsr2016.27.2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.FAO/WHO . Evaluation of Health and Nutritional Properties of Powder Milk and Live Lactic Acid Bacteria. Joint FAO/WHO Expert Consultation; Cordoba, Argentina: 2001. pp. 1–34. [Google Scholar]
- 10.Sartor R.B., LaMont T., Grover S. Probiotics for Gastrointestinal Diseases. Uptodate Feb 2013. [(accessed on 2 February 2024)]. Available online: https://www.uptodate.com/contents/probiotics-for-gastrointestinal-diseases.
- 11.Rosander A., Connolly E., Roos S. Removal of antibiotic resistance gene-carrying plasmids from Lactobacillus reuteri ATCC 55730 and characterization of the resulting daughter strain, L. reuteri DSM 17938. Appl. Environ. Microbiol. 2008;74:6032–6040. doi: 10.1128/AEM.00991-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Markowiak P., Śliżewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. 2017;9:1021. doi: 10.3390/nu9091021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jach M.E., Serefko A., Szopa A., Sajnaga E., Golczyk H., Santos L.S., Borowicz-Reutt K., Sieniawska E. The Role of Probiotics and Their Metabolites in the Treatment of Depression. Molecules. 2023;28:3213. doi: 10.3390/molecules28073213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mörkl S., Butler M.I., Holl A., Cryan J.F., Dinan T.G. Probiotics and the Microbiota-Gut-Brain Axis: Focus on Psychiatry. Curr. Nutr. Rep. 2020;9:171–182. doi: 10.1007/s13668-020-00313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Madison A., Kiecolt-Glaser J.K. Stress, depression, diet, and the gut microbiota: Human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr. Opin. Behav. Sci. 2019;28:105–110. doi: 10.1016/j.cobeha.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang X., Zhang P., Zhang X. Probiotics regulate gut microbiota: An effective method to improve immunity. Molecules. 2021;26:6076. doi: 10.3390/molecules26196076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fekete M., Lehoczki A., Tarantini S., Fazekas-Pongor V., Csípő T., Csizmadia Z., Varga J.T. Improving Cognitive Function with Nutritional Supplements in Aging: A Comprehensive Narrative Review of Clinical Studies Investigating the Effects of Vitamins, Minerals, Antioxidants, and Other Dietary Supplements. Nutrients. 2023;15:5116. doi: 10.3390/nu15245116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim C.S., Cha L., Sim M., Jung S., Chun W.Y., Baik H.W., Shin D.M. Probiotic Supplementation Improves Cognitive Function and Mood with Changes in Gut Microbiota in Community-Dwelling Older Adults: A Randomized, Double-Blind, Placebo-Controlled, Multicenter Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:32–40. doi: 10.1093/gerona/glaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi S., Zhang Q., Sang Y., Ge S., Wang Q., Wang R., He J. Probiotic Bifidobacterium longum BB68S Improves Cognitive Functions in Healthy Older Adults: A Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients. 2022;15:51. doi: 10.3390/nu15010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sakurai K., Toshimitsu T., Okada E., Anzai S., Shiraishi I., Inamura N., Kobayashi S., Sashihara T., Hisatsune T. Effects of Lactiplantibacillus plantarum OLL2712 on Memory Function in Older Adults with Declining Memory: A Randomized Placebo-Controlled Trial. Nutrients. 2022;14:4300. doi: 10.3390/nu14204300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Czajeczny D., Kabzińska K., Wójciak R.W. Effects of Bifidobacterium Lactis BS01 and Lactobacillus Acidophilus LA02 on cognitive functioning in healthy women. Appl. Neuropsychol. Adult. 2023;30:552–560. doi: 10.1080/23279095.2021.1967155. [DOI] [PubMed] [Google Scholar]
- 22.Lochlainn M.N., Bowyer R., Whelan K., Steves C.J. 66 The PROMOTe study: Prebiotic supplementation improves cognition versus placebo in healthy older twins. Age Ageing. 2023;52:afad156-006. doi: 10.1093/ageing/afad156.006. [DOI] [Google Scholar]
- 23.Azuma N., Mawatari T., Saito Y., Tsukamoto M., Sampei M., Iwama Y. Effect of Continuous Ingestion of Bifidobacteria and Dietary Fiber on Improvement in Cognitive Function: A Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients. 2023;15:4175. doi: 10.3390/nu15194175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berding K., Long-Smith C.M., Carbia C., Bastiaanssen T.F.S., van de Wouw M., Wiley N., Strain C.R., Fouhy F., Stanton C., Cryan J.F., et al. A specific dietary fibre supplementation improves cognitive performance—An exploratory randomised, placebo-controlled, crossover study. Psychopharmacology. 2021;238:149–163. doi: 10.1007/s00213-020-05665-y. [DOI] [PubMed] [Google Scholar]
- 25.Sanborn V., Azcarate-Peril M.A., Updegraff J., Manderino L., Gunstad J. Randomized Clinical Trial Examining the Impact of Lactobacillus rhamnosus GG Probiotic Supplementation on Cognitive Functioning in Middle-aged and Older Adults. Neuropsychiatr. Dis. Treat. 2020;16:2765–2777. doi: 10.2147/NDT.S270035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Louzada E.R., Ribeiro S.M.L. Synbiotic supplementation, systemic inflammation, and symptoms of brain disorders in elders: A secondary study from a randomized clinical trial. Nutr. Neurosci. 2020;23:93–100. doi: 10.1080/1028415X.2018.1477349. [DOI] [PubMed] [Google Scholar]
- 27.Sanborn V., Aljumaah M., Azcarate-Peril M.A., Gunstad J. Examining the cognitive benefits of probiotic supplementation in physically active older adults: A randomized clinical trial. Appl. Physiol. Nutr. Metab. 2022;47:871–882. doi: 10.1139/apnm-2021-0557. [DOI] [PubMed] [Google Scholar]
- 28.Edebol Carlman H.M.T., Rode J., König J., Repsilber D., Hutchinson A.N., Thunberg P., Persson J., Kiselev A., Pruessner J.C., Brummer R.J. Probiotic Mixture Containing Lactobacillus helveticus, Bifidobacterium longum and Lactiplantibacillus plantarum Affects Brain Responses to an Arithmetic Stress Task in Healthy Subjects: A Randomised Clinical Trial and Proof-of-Concept Study. Nutrients. 2022;14:1329. doi: 10.3390/nu14071329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ascone L., Forlim C.G., Gallinat J., Kühn S. Effects of a multi-strain probiotic on hippocampal structure and function, cognition, and emotional well-being in healthy individuals: A double-blind randomised-controlled trial. Psychol. Med. 2022;52:4197–4207. doi: 10.1017/S0033291722000988. [DOI] [PubMed] [Google Scholar]
- 30.Cannavale C.N., Mysonhimer A.R., Bailey M.A., Cohen N.J., Holscher H.D., Khan N.A. Consumption of a fermented dairy beverage improves hippocampal-dependent relational memory in a randomized, controlled cross-over trial. Nutr. Neurosci. 2023;26:265–274. doi: 10.1080/1028415X.2022.2046963. [DOI] [PubMed] [Google Scholar]
- 31.Aljumaah M.R., Bhatia U., Roach J., Gunstad J., Azcarate Peril M.A. The gut microbiome, mild cognitive impairment, and probiotics: A randomized clinical trial in middle-aged and older adults. Clin. Nutr. 2022;41:2565–2576. doi: 10.1016/j.clnu.2022.09.012. [DOI] [PubMed] [Google Scholar]
- 32.Asaoka D., Xiao J., Takeda T., Yanagisawa N., Yamazaki T., Matsubara Y., Sugiyama H., Endo N., Higa M., Kasanuki K., et al. Effect of Probiotic Bifidobacterium breve in Improving Cognitive Function and Preventing Brain Atrophy in Older Patients with Suspected Mild Cognitive Impairment: Results of a 24-Week Randomized, Double-Blind, Placebo-Controlled Trial. J. Alzheimers Dis. 2022;88:75–95. doi: 10.3233/JAD-220148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xiao J., Katsumata N., Bernier F., Ohno K., Yamauchi Y., Odamaki T., Yoshikawa K., Ito K., Kaneko T. Probiotic Bifidobacterium breve in Improving Cognitive Functions of Older Adults with Suspected Mild Cognitive Impairment: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Alzheimers Dis. 2020;77:139–147. doi: 10.3233/JAD-200488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fei Y., Wang R., Lu J., Peng S., Yang S., Wang Y., Zheng K., Li R., Lin L., Li M. Probiotic intervention benefits multiple neural behaviors in older adults with mild cognitive impairment. Geriatr. Nurs. 2023;51:167–175. doi: 10.1016/j.gerinurse.2023.03.006. [DOI] [PubMed] [Google Scholar]
- 35.Kobayashi Y., Kinoshita T., Matsumoto A., Yoshino K., Saito I., Xiao J.Z. Bifidobacterium Breve A1 Supplementation Improved Cognitive Decline in Older Adults with Mild Cognitive Impairment: An Open-Label, Single-Arm Study. J. Prev. Alzheimers Dis. 2019;6:70–75. doi: 10.14283/jpad.2018.32. [DOI] [PubMed] [Google Scholar]
- 36.Hwang Y.H., Park S., Paik J.W., Chae S.W., Kim D.H., Jeong D.G., Ha E., Kim M., Hong G., Park S.H., et al. Efficacy and Safety of Lactobacillus Plantarum C29-Fermented Soybean (DW2009) in Individuals with Mild Cognitive Impairment: A 12-Week, Multi-Center, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients. 2019;11:305. doi: 10.3390/nu11020305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ton A.M.M., Campagnaro B.P., Alves G.A., Aires R., Côco L.Z., Arpini C.M., Guerra E.O.T., Campos-Toimil M., Meyrelles S.S., Pereira T.M.C., et al. Oxidative Stress and Dementia in Alzheimer’s Patients: Effects of Synbiotic Supplementation. Oxid. Med. Cell Longev. 2020;2020:2638703. doi: 10.1155/2020/2638703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akhgarjand C., Vahabi Z., Shab-Bidar S., Etesam F., Djafarian K. Effects of probiotic supplements on cognition, anxiety, and physical activity in subjects with mild and moderate Alzheimer’s disease: A randomized, double-blind, and placebo-controlled study. Front. Aging Neurosci. 2022;14:1032494. doi: 10.3389/fnagi.2022.1032494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kobayashi Y., Kuhara T., Oki M., Xiao J.Z. Effects of Bifidobacterium breve A1 on the cognitive function of older adults with memory complaints: A randomised, double-blind, placebo-controlled trial. Benef. Microbes. 2019;10:511–520. doi: 10.3920/BM2018.0170. [DOI] [PubMed] [Google Scholar]
- 40.Tamtaji O.R., Heidari-Soureshjani R., Mirhosseini N., Kouchaki E., Bahmani F., Aghadavod E., Tajabadi-Ebrahimi M., Asemi Z. Probiotic and selenium co-supplementation, and the effects on clinical, metabolic and genetic status in Alzheimer’s disease: A randomized, double-blind, controlled trial. Clin. Nutr. 2019;38:2569–2575. doi: 10.1016/j.clnu.2018.11.034. [DOI] [PubMed] [Google Scholar]
- 41.Liu Y., Alookaran J.J., Rhoads J.M. Probiotics in autoimmune and inflammatory disorders. Nutrients. 2018;10:1537. doi: 10.3390/nu10101537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cristofori F., Dargenio V.N., Dargenio C., Miniello V.L., Barone M., Francavilla R. Anti-inflammatory and immunomodulatory effects of probiotics in gut inflammation: A door to the body. Front. Immunol. 2021;12:578386. doi: 10.3389/fimmu.2021.578386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fekete M., Szarvas Z., Fazekas-Pongor V., Fehér Á., Varga J.T. Az emberi szervezetben élő baktériumok klinikai jelentősége a gyakorlatban. Egészségfejlesztés. 2021;62:31–43. doi: 10.24365/ef.v62i4.6928. [DOI] [Google Scholar]
- 44.You S., Ma Y., Yan B., Pei W., Wu Q., Ding C., Huang C. The promotion mechanism of prebiotics for probiotics: A review. Front. Nutr. 2022;9:1000517. doi: 10.3389/fnut.2022.1000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roy S., Dhaneshwar S. Role of prebiotics, probiotics, and synbiotics in management of inflammatory bowel disease: Current perspectives. World J. Gastroenterol. 2023;29:2078. doi: 10.3748/wjg.v29.i14.2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carabotti M., Scirocco A., Maselli M.A., Severi C. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. Q. Publ. Hell. Soc. Gastroenterol. 2015;28:203. [PMC free article] [PubMed] [Google Scholar]
- 47.Tzemah-Shahar R., Turjeman S., Sharon E., Gamliel G., Hochner H., Koren O., Agmon M. Signs of aging in midlife: Physical function and sex differences in microbiota. Geroscience. 2024;46:1477–1488. doi: 10.1007/s11357-023-00905-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brunt V.E., LaRocca T.J., Bazzoni A.E., Sapinsley Z.J., Miyamoto-Ditmon J., Gioscia-Ryan R.A., Neilson A.P., Link C.D., Seals D.R. The gut microbiome-derived metabolite trimethylamine N-oxide modulates neuroinflammation and cognitive function with aging. Geroscience. 2021;43:377–394. doi: 10.1007/s11357-020-00257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Galland L. The gut microbiome and the brain. J. Med. Food. 2014;17:1261–1272. doi: 10.1089/jmf.2014.7000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Csipo T., Lipecz A., Fulop G.A., Hand R.A., Ngo B.-T.N., Dzialendzik M., Tarantini S., Balasubramanian P., Kiss T., Yabluchanska V. Age-related decline in peripheral vascular health predicts cognitive impairment. Geroscience. 2019;41:125–136. doi: 10.1007/s11357-019-00063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fekete M., Balazs P., Lehoczki A., Forrai J., Dosa N., Fazekas-Pongor V., Feher A., Madarasz B., Varga J.T. The role of gut microbiome and its modification while regulating the defence mechanisms, particularly in severe COVID-19 cases. Med. Int. Rev. 2023;30:154–166. [Google Scholar]
- 52.Fekete M., Szarvas Z., Fazekas-Pongor V., Feher A., Csipo T., Forrai J., Dosa N., Peterfi A., Lehoczki A., Tarantini S. Nutrition strategies promoting healthy aging: From improvement of cardiovascular and brain health to prevention of age-associated diseases. Nutrients. 2022;15:47. doi: 10.3390/nu15010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Coradduzza D., Sedda S., Cruciani S., De Miglio M.R., Ventura C., Nivoli A., Maioli M. Age-Related Cognitive Decline, Focus on Microbiome: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023;24:13680. doi: 10.3390/ijms241813680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shintani T., Shintani H., Sato M., Ashida H. Calorie restriction mimetic drugs could favorably influence gut microbiota leading to lifespan extension. Geroscience. 2023;45:3475–3490. doi: 10.1007/s11357-023-00851-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sanada F., Taniyama Y., Muratsu J., Otsu R., Shimizu H., Rakugi H., Morishita R. Source of chronic inflammation in aging. Front. Cardiovasc. Med. 2018;5:12. doi: 10.3389/fcvm.2018.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wall R., Cryan J.F., Ross R.P., Fitzgerald G.F., Dinan T.G., Stanton C. Bacterial neuroactive compounds produced by psychobiotics. Adv. Exp. Med. Biol. 2014;817:221–239. doi: 10.1007/978-1-4939-0897-4_10. [DOI] [PubMed] [Google Scholar]
- 57.Watson S., Mackin P. HPA axis function in mood disorders. Psychiatry. 2006;5:166–170. doi: 10.1383/psyt.2006.5.5.166. [DOI] [Google Scholar]
- 58.Wu H.-J., Wu E. The role of gut microbiota in immune homeostasis and autoimmunity. Gut Microbes. 2012;3:4–14. doi: 10.4161/gmic.19320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nandwana V., Nandwana N.K., Das Y., Saito M., Panda T., Das S., Almaguel F., Hosmane N.S., Das B.C. The role of microbiome in brain development and neurodegenerative diseases. Molecules. 2022;27:3402. doi: 10.3390/molecules27113402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hossain K.S., Amarasena S., Mayengbam S. B vitamins and their roles in gut health. Microorganisms. 2022;10:1168. doi: 10.3390/microorganisms10061168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Petra A.I., Panagiotidou S., Hatziagelaki E., Stewart J.M., Conti P., Theoharides T.C. Gut-Microbiota-Brain Axis and Its Effect on Neuropsychiatric Disorders with Suspected Immune Dysregulation. Clin. Ther. 2015;37:984–995. doi: 10.1016/j.clinthera.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee C.-H., Giuliani F. The role of inflammation in depression and fatigue. Front. Immunol. 2019;10:1696. doi: 10.3389/fimmu.2019.01696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sartori A.C., Vance D.E., Slater L.Z., Crowe M. The impact of inflammation on cognitive function in older adults: Implications for health care practice and research. J. Neurosci. Nurs. 2012;44:206. doi: 10.1097/JNN.0b013e3182527690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jin R., Chan A.K.Y., Wu J., Lee T.M.C. Relationships between inflammation and age-related neurocognitive changes. Int. J. Mol. Sci. 2022;23:12573. doi: 10.3390/ijms232012573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kawai T., Autieri M.V., Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol.-Cell Physiol. 2021;320:C375–C391. doi: 10.1152/ajpcell.00379.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Camilleri M. Leaky gut: Mechanisms, measurement and clinical implications in humans. Gut. 2019;68:1516–1526. doi: 10.1136/gutjnl-2019-318427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ma J., Piao X., Mahfuz S., Long S., Wang J. The interaction among gut microbes, the intestinal barrier and short chain fatty acids. Anim. Nutr. 2022;9:159–174. doi: 10.1016/j.aninu.2021.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gulej R., Nyul-Toth A., Csik B., Petersen B., Faakye J., Negri S., Chandragiri S.S., Mukli P., Yabluchanskiy A., Conley S., et al. Rejuvenation of cerebromicrovascular function in aged mice through heterochronic parabiosis: Insights into neurovascular coupling and the impact of young blood factors. Geroscience. 2024;46:327–347. doi: 10.1007/s11357-023-01039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ting K.K., Coleman P., Kim H.J., Zhao Y., Mulangala J., Cheng N.C., Li W., Gunatilake D., Johnstone D.M., Loo L., et al. Vascular senescence and leak are features of the early breakdown of the blood-brain barrier in Alzheimer’s disease models. Geroscience. 2023;45:3307–3331. doi: 10.1007/s11357-023-00927-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lineback C.M., Stamm B., Sorond F., Caprio F.Z. Carotid disease, cognition, and aging: Time to redefine asymptomatic disease? Geroscience. 2023;45:719–725. doi: 10.1007/s11357-022-00688-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang H., Roman R.J., Fan F. Hippocampus is more susceptible to hypoxic injury: Has the Rosetta Stone of regional variation in neurovascular coupling been deciphered? Geroscience. 2022;44:127–130. doi: 10.1007/s11357-021-00449-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vestergaard M.B., Lindberg U., Knudsen M.H., Urdanibia-Centelles O., Bakhtiari A., Mortensen E.L., Osler M., Fagerlund B., Benedek K., Lauritzen M., et al. Subclinical cognitive deficits are associated with reduced cerebrovascular response to visual stimulation in mid-sixties men. Geroscience. 2022;44:1905–1923. doi: 10.1007/s11357-022-00596-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Toth L., Czigler A., Hegedus E., Komaromy H., Amrein K., Czeiter E., Yabluchanskiy A., Koller A., Orsi G., Perlaki G., et al. Age-related decline in circulating IGF-1 associates with impaired neurovascular coupling responses in older adults. Geroscience. 2022;44:2771–2783. doi: 10.1007/s11357-022-00623-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Montagne A., Barnes S.R., Nation D.A., Kisler K., Toga A.W., Zlokovic B.V. Imaging subtle leaks in the blood-brain barrier in the aging human brain: Potential pitfalls, challenges, and possible solutions. Geroscience. 2022;44:1339–1351. doi: 10.1007/s11357-022-00571-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tarantini S., Balasubramanian P., Delfavero J., Csipo T., Yabluchanskiy A., Kiss T., Nyul-Toth A., Mukli P., Toth P., Ahire C., et al. Treatment with the BCL-2/BCL-xL inhibitor senolytic drug ABT263/Navitoclax improves functional hyperemia in aged mice. Geroscience. 2021;43:2427–2440. doi: 10.1007/s11357-021-00440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sabayan B., Westendorp R.G.J. Neurovascular-glymphatic dysfunction and white matter lesions. Geroscience. 2021;43:1635–1642. doi: 10.1007/s11357-021-00361-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Faakye J., Nyul-Toth A., Muranyi M., Gulej R., Csik B., Shanmugarama S., Tarantini S., Negri S., Prodan C., Mukli P., et al. Preventing spontaneous cerebral microhemorrhages in aging mice: A novel approach targeting cellular senescence with ABT263/navitoclax. Geroscience. 2024;46:21–37. doi: 10.1007/s11357-023-01024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kiss T., Nyul-Toth A., Balasubramanian P., Tarantini S., Ahire C., DelFavero J., Yabluchanskiy A., Csipo T., Farkas E., Wiley G., et al. Single-cell RNA sequencing identifies senescent cerebromicrovascular endothelial cells in the aged mouse brain. Geroscience. 2020;42:429–444. doi: 10.1007/s11357-020-00177-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Czakó C., Kovács T., Ungvari Z., Csiszar A., Yabluchanskiy A., Conley S., Csipo T., Lipecz A., Horváth H., Sándor G.L., et al. Retinal biomarkers for Alzheimer’s disease and vascular cognitive impairment and dementia (VCID): Implication for early diagnosis and prognosis. Geroscience. 2020;42:1499–1525. doi: 10.1007/s11357-020-00252-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Papalini S., Michels F., Kohn N., Wegman J., van Hemert S., Roelofs K., Arias-Vasquez A., Aarts E. Stress matters: Randomized controlled trial on the effect of probiotics on neurocognition. Neurobiol. Stress. 2019;10:100141. doi: 10.1016/j.ynstr.2018.100141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chaiyasut C., Sivamaruthi B.S. Influence of probiotic supplementation on brain function: Involvement of gut microbiome, inflammation, and stress pathway. Gut Microbiota-Brain Axis. 2018:20–33. doi: 10.5772/intechopen.79511. [DOI] [Google Scholar]
- 82.National Institutes of Health Probiotics: Fact Sheet for Health Professionals. [(accessed on 12 February 2024)];2020 Available online: https://ods.od.nih.gov/factsheets/Probiotics-HealthProfessional/
- 83.Lee J. Mild cognitive impairment in relation to Alzheimer’s disease: An investigation of principles, classifications, ethics, and problems. Neuroethics. 2023;16:16. doi: 10.1007/s12152-023-09522-5. [DOI] [Google Scholar]
- 84.Petersen R.C., Lopez O., Armstrong M.J., Getchius T.S., Ganguli M., Gloss D., Gronseth G.S., Marson D., Pringsheim T., Day G.S. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90:126–135. doi: 10.1212/WNL.0000000000004826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Levy S.-A., Smith G., De Wit L., DeFeis B., Ying G., Amofa P., Locke D., Shandera-Ochsner A., McAlister C., Phatak V. Behavioral interventions in mild cognitive impairment (MCI): Lessons from a multicomponent program. Neurotherapeutics. 2023;19:117–131. doi: 10.1007/s13311-022-01225-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhu G., Zhao J., Zhang H., Chen W., Wang G. Probiotics for mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. Foods. 2021;10:1672. doi: 10.3390/foods10071672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Li X., Lv C., Song J., Li J. Effect of probiotic supplementation on cognitive function and metabolic status in mild cognitive impairment and alzheimer’s disease: A meta-analysis. Front. Nutr. 2021;8:757673. doi: 10.3389/fnut.2021.757673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang Q., Fan C., Wang L., Li T., Wang M., Han Y., Jiang J., and for the Alzheimer’s Disease Neuroimaging Initiative Glucose metabolism in posterior cingulate cortex has supplementary value to predict the progression of cognitively unimpaired to dementia due to Alzheimer’s disease: An exploratory study of (18)F-FDG-PET. Geroscience. 2024;46:1407–1420. doi: 10.1007/s11357-023-00897-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zadka L., Sochocka M., Hachiya N., Chojdak-Lukasiewicz J., Dziegiel P., Piasecki E., Leszek J. Endocytosis and Alzheimer’s disease. Geroscience. 2024;46:71–85. doi: 10.1007/s11357-023-00923-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wortha S.M., Schulz J., Hanna J., Schwarz C., Stubbe B., Frenzel S., Bulow R., Friedrich N., Nauck M., Volzke H., et al. Association of spermidine blood levels with microstructure of sleep-implications from a population-based study. Geroscience. 2024;46:1319–1330. doi: 10.1007/s11357-023-00886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Williamson J., James S.A., Mukli P., Yabluchanskiy A., Wu D.H., Sonntag W., Alzheimer’s Disease Neuroimaging Initiative C., Yang Y. Sex difference in brain functional connectivity of hippocampus in Alzheimer’s disease. Geroscience. 2024;46:563–572. doi: 10.1007/s11357-023-00943-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang Z., Liu A., Yu J., Wang P., Bi Y., Xue S., Zhang J., Guo H., Zhang W. The effect of aperiodic components in distinguishing Alzheimer’s disease from frontotemporal dementia. Geroscience. 2024;46:751–768. doi: 10.1007/s11357-023-01041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang Q., Qi L., He C., Feng H., Xie C., Depression Imaging R.C. Age- and gender-related dispersion of brain networks across the lifespan. Geroscience. 2024;46:1303–1318. doi: 10.1007/s11357-023-00900-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.van Gennip A.C.E., Satizabal C.L., Tracy R.P., Sigurdsson S., Gudnason V., Launer L.J., van Sloten T.T. Associations of plasma NfL, GFAP, and t-tau with cerebral small vessel disease and incident dementia: Longitudinal data of the AGES-Reykjavik Study. Geroscience. 2024;46:505–516. doi: 10.1007/s11357-023-00888-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Salwierz P., Thapa S., Taghdiri F., Vasilevskaya A., Anastassiadis C., Tang-Wai D.F., Golas A.C., Tartaglia M.C. Investigating the association between a history of depression and biomarkers of Alzheimer’s disease, cerebrovascular disease, and neurodegeneration in patients with dementia. Geroscience. 2024;46:783–793. doi: 10.1007/s11357-023-01030-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fernandez A., Cuesta P., Marcos A., Montenegro-Pena M., Yus M., Rodriguez-Rojo I.C., Bruna R., Maestu F., Lopez M.E. Sex differences in the progression to Alzheimer’s disease: A combination of functional and structural markers. Geroscience. 2024;46:2619–2640. doi: 10.1007/s11357-023-01020-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ercolano E., Bencivenga L., Palaia M.E., Carbone G., Scognamiglio F., Rengo G., Femminella G.D. Intricate relationship between obstructive sleep apnea and dementia in older adults. Geroscience. 2024;46:99–111. doi: 10.1007/s11357-023-00958-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.DeVries S.A., Conner B., Dimovasili C., Moore T.L., Medalla M., Mortazavi F., Rosene D.L. Immune proteins C1q and CD47 may contribute to aberrant microglia-mediated synapse loss in the aging monkey brain that is associated with cognitive impairment. Geroscience. 2024;46:2503–2519. doi: 10.1007/s11357-023-01014-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.da Silva S.P., de Castro C.C.M., Rabelo L.N., Engelberth R.C., Fernandez-Calvo B., Fiuza F.P. Neuropathological and sociodemographic factors associated with the cortical amyloid load in aging and Alzheimer’s disease. Geroscience. 2024;46:621–643. doi: 10.1007/s11357-023-00982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chen Y., Zhang Y., Yang H., Li H., Zhou L., Zhang M., Wang Y. Associations of sugar-sweetened, artificially sweetened, and naturally sweet juices with Alzheimer’s disease: A prospective cohort study. Geroscience. 2024;46:1229–1240. doi: 10.1007/s11357-023-00889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Weijs R.W.J., Oudegeest-Sander M.H., Vloet J.I.A., Hopman M.T.E., Claassen J., Thijssen D.H.J. A decade of aging in healthy older adults: Longitudinal findings on cerebrovascular and cognitive health. Geroscience. 2023;45:2629–2641. doi: 10.1007/s11357-023-00790-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Waigi E.W., Webb R.C., Moss M.A., Uline M.J., McCarthy C.G., Wenceslau C.F. Soluble and insoluble protein aggregates, endoplasmic reticulum stress, and vascular dysfunction in Alzheimer’s disease and cardiovascular diseases. Geroscience. 2023;45:1411–1438. doi: 10.1007/s11357-023-00748-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Van Skike C.E., DeRosa N., Galvan V., Hussong S.A. Rapamycin restores peripheral blood flow in aged mice and in mouse models of atherosclerosis and Alzheimer’s disease. Geroscience. 2023;45:1987–1996. doi: 10.1007/s11357-023-00786-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Seman A., Chandra P.K., Byrum S.D., Mackintosh S.G., Gies A.J., Busija D.W., Rutkai I. Targeting mitochondria in the aged cerebral vasculature with SS-31, a proteomic study of brain microvessels. Geroscience. 2023;45:2951–2965. doi: 10.1007/s11357-023-00845-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dorigatti A.O., Riordan R., Yu Z., Ross G., Wang R., Reynolds-Lallement N., Magnusson K., Galvan V., Perez V.I. Brain cellular senescence in mouse models of Alzheimer’s disease. Geroscience. 2022;44:1157–1168. doi: 10.1007/s11357-022-00531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Custodero C., Ciavarella A., Panza F., Gnocchi D., Lenato G.M., Lee J., Mazzocca A., Sabba C., Solfrizzi V. Role of inflammatory markers in the diagnosis of vascular contributions to cognitive impairment and dementia: A systematic review and meta-analysis. Geroscience. 2022;44:1373–1392. doi: 10.1007/s11357-022-00556-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bagi Z., Kroenke C.D., Fopiano K.A., Tian Y., Filosa J.A., Sherman L.S., Larson E.B., Keene C.D., Degener O’Brien K., Adeniyi P.A., et al. Association of cerebral microvascular dysfunction and white matter injury in Alzheimer’s disease. Geroscience. 2022;44:1–14. doi: 10.1007/s11357-022-00585-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jiang C., Li G., Huang P., Liu Z., Zhao B. The gut microbiota and Alzheimer’s disease. J. Alzheimer’s Dis. 2017;58:1–15. doi: 10.3233/JAD-161141. [DOI] [PubMed] [Google Scholar]
- 109.Ferreiro A.L., Choi J., Ryou J., Newcomer E.P., Thompson R., Bollinger R.M., Hall-Moore C., Ndao I.M., Sax L., Benzinger T.L.S., et al. Gut microbiome composition may be an indicator of preclinical Alzheimer’s disease. Sci. Transl. Med. 2023;15:eabo2984. doi: 10.1126/scitranslmed.abo2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Vogt N.M., Kerby R.L., Dill-McFarland K.A., Harding S.J., Merluzzi A.P., Johnson S.C., Carlsson C.M., Asthana S., Zetterberg H., Blennow K., et al. Gut microbiome alterations in Alzheimer’s disease. Sci. Rep. 2017;7:13537. doi: 10.1038/s41598-017-13601-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cammann D., Lu Y., Cummings M.J., Zhang M.L., Cue J.M., Do J., Ebersole J., Chen X., Oh E.C., Cummings J.L., et al. Genetic correlations between Alzheimer’s disease and gut microbiome genera. Sci. Rep. 2023;13:5258. doi: 10.1038/s41598-023-31730-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jemimah S., Chabib C.M.M., Hadjileontiadis L., AlShehhi A. Gut microbiome dysbiosis in Alzheimer’s disease and mild cognitive impairment: A systematic review and meta-analysis. PLoS ONE. 2023;18:e0285346. doi: 10.1371/journal.pone.0285346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bhattacharjee N., Sarkar P., Sarkar T. Beyond the acute illness: Exploring long COVID and its impact on multiple organ systems. Physiol. Int. 2023;110:291–310. doi: 10.1556/2060.2023.00256. [DOI] [PubMed] [Google Scholar]
- 114.Moreno-Arribas M.V., Bartolome B., Penalvo J.L., Perez-Matute P., Motilva M.J. Relationship between Wine Consumption, Diet and Microbiome Modulation in Alzheimer’s Disease. Nutrients. 2020;12:3082. doi: 10.3390/nu12103082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lamichhane G., Liu J., Lee S.J., Lee D.Y., Zhang G., Kim Y. Curcumin Mitigates the High-Fat High-Sugar Diet-Induced Impairment of Spatial Memory, Hepatic Metabolism, and the Alteration of the Gut Microbiome in Alzheimer’s Disease-Induced (3xTg-AD) Mice. Nutrients. 2024;16:240. doi: 10.3390/nu16020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Giridharan V.V., Catumbela C.S.G., Catalao C.H.R., Lee J., Ganesh B.P., Petronilho F., Dal-Pizzol F., Morales R., Barichello T. Sepsis exacerbates Alzheimer’s disease pathophysiology, modulates the gut microbiome, increases neuroinflammation and amyloid burden. Mol. Psychiatry. 2023;28:4463–4473. doi: 10.1038/s41380-023-02172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mansell V., Hall Dykgraaf S., Kidd M., Goodyear-Smith F. Long COVID and older people. Lancet Healthy Longev. 2022;3:e849–e854. doi: 10.1016/S2666-7568(22)00245-8. [DOI] [PubMed] [Google Scholar]
- 118.Prajapati S.K., Shah R., Alford N., Mishra S.P., Jain S., Hansen B., Sanberg P., Molina A.J.A., Yadav H. The Triple Alliance: Microbiome, Mitochondria, and Metabolites in the Context of Age-Related Cognitive Decline and Alzheimer’s Disease. J. Gerontol. A Biol. Sci. Med. Sci. 2023;78:2187–2202. doi: 10.1093/gerona/glad226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhao Y., Jaber V., Lukiw W.J. Gastrointestinal Tract Microbiome-Derived Pro-inflammatory Neurotoxins in Alzheimer’s Disease. J. Aging Sci. 2021;9:002. [PMC free article] [PubMed] [Google Scholar]
- 120.Li X.Y., Qin H.Y., Li T.T. Advances in the study of the relationship between Alzheimer’s disease and the gastrointestinal microbiome. Ibrain. 2022;8:465–475. doi: 10.1002/ibra.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang T., Gao G., Kwok L.Y., Sun Z. Gut microbiome-targeted therapies for Alzheimer’s disease. Gut Microbes. 2023;15:2271613. doi: 10.1080/19490976.2023.2271613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhan Y., Al-Nusaif M., Ding C., Zhao L., Dong C. The potential of the gut microbiome for identifying Alzheimer’s disease diagnostic biomarkers and future therapies. Front. Neurosci. 2023;17:1130730. doi: 10.3389/fnins.2023.1130730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Laske C., Muller S., Preische O., Ruschil V., Munk M.H.J., Honold I., Peter S., Schoppmeier U., Willmann M. Signature of Alzheimer’s Disease in Intestinal Microbiome: Results from the AlzBiom Study. Front. Neurosci. 2022;16:792996. doi: 10.3389/fnins.2022.792996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bello-Corral L., Sanchez-Valdeon L., Casado-Verdejo I., Seco-Calvo J.A., Antonio Fernandez-Fernandez J., Nelida Fernandez-Martinez M. The Influence of Nutrition in Alzheimer’s Disease: Neuroinflammation and the Microbiome vs. Transmissible Prion. Front. Neurosci. 2021;15:677777. doi: 10.3389/fnins.2021.677777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hill J.M., Bhattacharjee S., Pogue A.I., Lukiw W.J. The gastrointestinal tract microbiome and potential link to Alzheimer’s disease. Front. Neurol. 2014;5:43. doi: 10.3389/fneur.2014.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mone Y., Earl J.P., Krol J.E., Ahmed A., Sen B., Ehrlich G.D., Lapides J.R. Evidence supportive of a bacterial component in the etiology for Alzheimer’s disease and for a temporal-spatial development of a pathogenic microbiome in the brain. Front. Cell Infect. Microbiol. 2023;13:1123228. doi: 10.3389/fcimb.2023.1123228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Arora K., Green M., Prakash S. The Microbiome and Alzheimer’s Disease: Potential and Limitations of Prebiotic, Synbiotic, and Probiotic Formulations. Front. Bioeng. Biotechnol. 2020;8:537847. doi: 10.3389/fbioe.2020.537847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lee E.H., Kim G.H., Park H.K., Kang H.J., Park Y.K., Lee H.A., Hong C.H., Moon S.Y., Kang W., Oh H.S., et al. Effects of the multidomain intervention with nutritional supplements on cognition and gut microbiome in early symptomatic Alzheimer’s disease: A randomized controlled trial. Front. Aging Neurosci. 2023;15:1266955. doi: 10.3389/fnagi.2023.1266955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hill J.M., Clement C., Pogue A.I., Bhattacharjee S., Zhao Y., Lukiw W.J. Pathogenic microbes, the microbiome, and Alzheimer’s disease (AD) Front. Aging Neurosci. 2014;6:127. doi: 10.3389/fnagi.2014.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Seo D.O., Holtzman D.M. Current understanding of the Alzheimer’s disease-associated microbiome and therapeutic strategies. Exp. Mol. Med. 2024;56:86–94. doi: 10.1038/s12276-023-01146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Abraham D., Feher J., Scuderi G.L., Szabo D., Dobolyi A., Cservenak M., Juhasz J., Ligeti B., Pongor S., Gomez-Cabrera M.C., et al. Exercise and probiotics attenuate the development of Alzheimer’s disease in transgenic mice: Role of microbiome. Exp. Gerontol. 2019;115:122–131. doi: 10.1016/j.exger.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 132.Chen G., Zhou X., Zhu Y., Shi W., Kong L. Gut microbiome characteristics in subjective cognitive decline, mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. Eur. J. Neurol. 2023;30:3568–3580. doi: 10.1111/ene.15961. [DOI] [PubMed] [Google Scholar]
- 133.Kohler C.A., Maes M., Slyepchenko A., Berk M., Solmi M., Lanctot K.L., Carvalho A.F. The Gut-Brain Axis, Including the Microbiome, Leaky Gut and Bacterial Translocation: Mechanisms and Pathophysiological Role in Alzheimer’s Disease. Curr. Pharm. Des. 2016;22:6152–6166. doi: 10.2174/1381612822666160907093807. [DOI] [PubMed] [Google Scholar]
- 134.Bou Zerdan M., Hebbo E., Hijazi A., El Gemayel M., Nasr J., Nasr D., Yaghi M., Bouferraa Y., Nagarajan A. The Gut Microbiome and Alzheimer’s Disease: A Growing Relationship. Curr. Alzheimer Res. 2022;19:808–818. doi: 10.2174/1567205020666221227090125. [DOI] [PubMed] [Google Scholar]
- 135.Kaur H., Nookala S., Singh S., Mukundan S., Nagamoto-Combs K., Combs C.K. Sex-Dependent Effects of Intestinal Microbiome Manipulation in a Mouse Model of Alzheimer’s Disease. Cells. 2021;10:2370. doi: 10.3390/cells10092370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Dilmore A.H., Martino C., Neth B.J., West K.A., Zemlin J., Rahman G., Panitchpakdi M., Meehan M.J., Weldon K.C., Blach C., et al. Effects of a ketogenic and low-fat diet on the human metabolome, microbiome, and foodome in adults at risk for Alzheimer’s disease. Alzheimers Dement. 2023;19:4805–4816. doi: 10.1002/alz.13007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nagarajan A., Srivastava H., Morrow C.D., Sun L.Y. Characterizing the gut microbiome changes with aging in a novel Alzheimer’s disease rat model. Aging. 2023;15:459–471. doi: 10.18632/aging.204484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Guo X., Zhang X., Tang P., Chong L., Li R. Integration of genome-wide association studies (GWAS) and microbiome data highlights the impact of sulfate-reducing bacteria on Alzheimer’s disease. Age Ageing. 2023;52:afad112. doi: 10.1093/ageing/afad112. [DOI] [PubMed] [Google Scholar]
- 139.Stavropoulou E., Bezirtzoglou E. Probiotics in Medicine: A Long Debate. Front Immunol. 2020;11:2192. doi: 10.3389/fimmu.2020.02192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lekchand Dasriya V., Samtiya M., Dhewa T., Puniya M., Kumar S., Ranveer S., Chaudhary V., Vij S., Behare P., Singh N. Etiology and management of Alzheimer’s disease: Potential role of gut microbiota modulation with probiotics supplementation. J. Food Biochem. 2022;46:e14043. doi: 10.1111/jfbc.14043. [DOI] [PubMed] [Google Scholar]
- 141.Murai T., Matsuda S. Therapeutic implications of probiotics in the gut microbe-modulated neuroinflammation and progression of Alzheimer’s disease. Life. 2023;13:1466. doi: 10.3390/life13071466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Islam S.U. Clinical Uses of Probiotics. Medicine. 2016;95:e2658. doi: 10.1097/MD.0000000000002658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Akbari E., Asemi Z., Daneshvar Kakhaki R., Bahmani F., Kouchaki E., Tamtaji O.R., Hamidi G.A., Salami M. Effect of probiotic supplementation on cognitive function and metabolic status in Alzheimer’s disease: A randomized, double-blind and controlled trial. Front. Aging Neurosci. 2016;8:256. doi: 10.3389/fnagi.2016.00256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lourida I., Soni M., Thompson-Coon J., Purandare N., Lang I.A., Ukoumunne O.C., Llewellyn D.J. Mediterranean diet, cognitive function, and dementia: A systematic review. Epidemiology. 2013;24:479–489. doi: 10.1097/EDE.0b013e3182944410. [DOI] [PubMed] [Google Scholar]
- 145.Jennings A., Cunnane S.C., Minihane A.M. Can nutrition support healthy cognitive ageing and reduce dementia risk? Bmj. 2020;369:m2269. doi: 10.1136/bmj.m2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Rizzo G. Soy-Based Tempeh as a Functional Food: Evidence for Human Health and Future Perspective. Front. Biosci.-Elite. 2024;16:3. doi: 10.31083/j.fbe1601003. [DOI] [PubMed] [Google Scholar]
- 147.Miceli S., Maniscalco L., Matranga D. Social networks and social activities promote cognitive functioning in both concurrent and prospective time: Evidence from the SHARE survey. Eur. J. Ageing. 2019;16:145–154. doi: 10.1007/s10433-018-0486-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Jensen E. Teaching with the Brain in Mind. ASCD; Alexandria, VA, USA: 2005. [Google Scholar]
- 149.Qi X., Pei Y., Malone S.K., Wu B. Social Isolation, sleep disturbance, and cognitive functioning (HRS): A Longitudinal Mediation Study. J. Gerontol. Ser. A. 2023;78:1826–1833. doi: 10.1093/gerona/glad004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Trivieri L., Jr., Association A.H.M. The American Holistic Medical Association Guide to Holistic Health: Healing Therapies for Optimal Wellness. John Wiley & Sons; Hoboken, NJ, USA: 2001. [Google Scholar]
- 151.Crane P.K., Walker R., Hubbard R.A., Li G., Nathan D.M., Zheng H., Haneuse S., Craft S., Montine T.J., Kahn S.E. Glucose levels and risk of dementia. N. Engl. J. Med. 2013;369:540–548. doi: 10.1056/NEJMoa1215740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Biessels G.J., Despa F. Cognitive decline and dementia in diabetes mellitus: Mechanisms and clinical implications. Nat. Rev. Endocrinol. 2018;14:591–604. doi: 10.1038/s41574-018-0048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Organization W.H. Decade of Healthy Ageing: Baseline Report. World Health Organization; Geneva, Switzerland: 2021. [Google Scholar]
- 154.Fekete M., Csípő T., Fazekas-Pongor V., Fehér Á., Szarvas Z., Kaposvári C., Horváth K., Lehoczki A., Tarantini S., Varga J.T. The Effectiveness of Supplementation with Key Vitamins, Minerals, Antioxidants and Specific Nutritional Supplements in COPD-A Review. Nutrients. 2023;15:2741. doi: 10.3390/nu15122741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Baldi S., Mundula T., Nannini G., Amedei A. Microbiota shaping—The effects of probiotics, prebiotics, and fecal microbiota transplant on cognitive functions: A systematic review. World J. Gastroenterol. 2021;27:6715. doi: 10.3748/wjg.v27.i39.6715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhou M., Chen S., Chen Y., Wang C., Chen C. Causal associations between gut microbiota and regional cortical structure: A Mendelian randomization study. Front. Neurosci. 2023;17:1296145. doi: 10.3389/fnins.2023.1296145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yu G., Chen Q., Chen J., Liao X., Xie H., Zhao Y., Liu J., Sun J., Chen S. Gut microbiota alterations are associated with functional outcomes in patients of acute ischemic stroke with non-alcoholic fatty liver disease. Front. Neurosci. 2023;17:1327499. doi: 10.3389/fnins.2023.1327499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ullah H., Arbab S., Tian Y., Liu C.Q., Chen Y., Qijie L., Khan M.I.U., Hassan I.U., Li K. The gut microbiota-brain axis in neurological disorder. Front. Neurosci. 2023;17:1225875. doi: 10.3389/fnins.2023.1225875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Turroni S., Provensi G. Editorial: Gut biodiversity and its influence in brain health. Front. Neurosci. 2023;17:1221543. doi: 10.3389/fnins.2023.1221543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Thomasi B., Valdetaro L., Ricciardi M.C., Goncalves de Carvalho M., Fialho Tavares I., Tavares-Gomes A.L. Enteric glia as a player of gut-brain interactions during Parkinson’s disease. Front. Neurosci. 2023;17:1281710. doi: 10.3389/fnins.2023.1281710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Tan H.E. The microbiota-gut-brain axis in stress and depression. Front. Neurosci. 2023;17:1151478. doi: 10.3389/fnins.2023.1151478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Shi J., Zhang X., Chen J., Shen R., Cui H., Wu H. Acupuncture and moxibustion therapy for cognitive impairment: The microbiome-gut-brain axis and its role. Front. Neurosci. 2023;17:1275860. doi: 10.3389/fnins.2023.1275860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Riehl L., Furst J., Kress M., Rykalo N. The importance of the gut microbiome and its signals for a healthy nervous system and the multifaceted mechanisms of neuropsychiatric disorders. Front. Neurosci. 2023;17:1302957. doi: 10.3389/fnins.2023.1302957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Plummer A.M., Matos Y.L., Lin H.C., Ryman S.G., Birg A., Quinn D.K., Parada A.N., Vakhtin A.A. Gut-brain pathogenesis of post-acute COVID-19 neurocognitive symptoms. Front. Neurosci. 2023;17:1232480. doi: 10.3389/fnins.2023.1232480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Liang J., Liu B., Dong X., Wang Y., Cai W., Zhang N., Zhang H. Decoding the role of gut microbiota in Alzheimer’s pathogenesis and envisioning future therapeutic avenues. Front. Neurosci. 2023;17:1242254. doi: 10.3389/fnins.2023.1242254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Klepinowski T., Skonieczna-Zydecka K., Pala B., Stachowska E., Sagan L. Gut microbiome in intracranial aneurysm growth, subarachnoid hemorrhage, and cerebral vasospasm: A systematic review with a narrative synthesis. Front. Neurosci. 2023;17:1247151. doi: 10.3389/fnins.2023.1247151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hayer S.S., Hwang S., Clayton J.B. Antibiotic-induced gut dysbiosis and cognitive, emotional, and behavioral changes in rodents: A systematic review and meta-analysis. Front. Neurosci. 2023;17:1237177. doi: 10.3389/fnins.2023.1237177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Denman C.R., Park S.M., Jo J. Gut-brain axis: Gut dysbiosis and psychiatric disorders in Alzheimer’s and Parkinson’s disease. Front. Neurosci. 2023;17:1268419. doi: 10.3389/fnins.2023.1268419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Corley C., McElroy T., Sridharan B., Trujillo M., Simmons P., Kandel S., Sykes D.J., Robeson M.S., 2nd, Allen A.R. Physiological and cognitive changes after treatments of cyclophosphamide, methotrexate, and fluorouracil: Implications of the gut microbiome and depressive-like behavior. Front. Neurosci. 2023;17:1212791. doi: 10.3389/fnins.2023.1212791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Boem F., Greslehner G.P., Konsman J.P., Chiu L. Minding the gut: Extending embodied cognition and perception to the gut complex. Front. Neurosci. 2023;17:1172783. doi: 10.3389/fnins.2023.1172783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Barton J.R., Londregan A.K., Alexander T.D., Entezari A.A., Covarrubias M., Waldman S.A. Enteroendocrine cell regulation of the gut-brain axis. Front. Neurosci. 2023;17:1272955. doi: 10.3389/fnins.2023.1272955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Zhou S.Y., Guo Z.N., Yang Y., Qu Y., Jin H. Gut-brain axis: Mechanisms and potential therapeutic strategies for ischemic stroke through immune functions. Front. Neurosci. 2023;17:1081347. doi: 10.3389/fnins.2023.1081347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zhang Q., Jin K., Chen B., Liu R., Cheng S., Zhang Y., Lu J. Overnutrition Induced Cognitive Impairment: Insulin Resistance, Gut-Brain Axis, and Neuroinflammation. Front. Neurosci. 2022;16:884579. doi: 10.3389/fnins.2022.884579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yan C., Diao Q., Zhao Y., Zhang C., He X., Huang R., Li Y. Fusobacterium nucleatum infection-induced neurodegeneration and abnormal gut microbiota composition in Alzheimer’s disease-like rats. Front. Neurosci. 2022;16:884543. doi: 10.3389/fnins.2022.884543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wang Y., Hang C., Hu J., Li C., Zhan C., Pan J., Yuan T. Role of gut-brain axis in neurodevelopmental impairment of necrotizing enterocolitis. Front. Neurosci. 2023;17:1059552. doi: 10.3389/fnins.2023.1059552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sun X., Xue L., Wang Z., Xie A. Update to the Treatment of Parkinson’s Disease Based on the Gut-Brain Axis Mechanism. Front. Neurosci. 2022;16:878239. doi: 10.3389/fnins.2022.878239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Salami M., Soheili M. The microbiota-gut- hippocampus axis. Front. Neurosci. 2022;16:1065995. doi: 10.3389/fnins.2022.1065995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Li Z., Zhou J., Liang H., Ye L., Lan L., Lu F., Wang Q., Lei T., Yang X., Cui P., et al. Differences in Alpha Diversity of Gut Microbiota in Neurological Diseases. Front. Neurosci. 2022;16:879318. doi: 10.3389/fnins.2022.879318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Krakovski M.A., Arora N., Jain S., Glover J., Dombrowski K., Hernandez B., Yadav H., Sarma A.K. Diet-microbiome-gut-brain nexus in acute and chronic brain injury. Front. Neurosci. 2022;16:1002266. doi: 10.3389/fnins.2022.1002266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hao X., Ding N., Zhang Y., Yang Y., Zhao Y., Zhao J., Li Y., Li Z. Benign regulation of the gut microbiota: The possible mechanism through which the beneficial effects of manual acupuncture on cognitive ability and intestinal mucosal barrier function occur in APP/PS1 mice. Front. Neurosci. 2022;16:960026. doi: 10.3389/fnins.2022.960026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Han W., Wang N., Han M., Ban M., Sun T., Xu J. Reviewing the role of gut microbiota in the pathogenesis of depression and exploring new therapeutic options. Front. Neurosci. 2022;16:1029495. doi: 10.3389/fnins.2022.1029495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Freijy T.M., Cribb L., Oliver G., Metri N.J., Opie R.S., Jacka F.N., Hawrelak J.A., Rucklidge J.J., Ng C.H., Sarris J. Effects of a high-prebiotic diet versus probiotic supplements versus synbiotics on adult mental health: The “Gut Feelings” randomised controlled trial. Front. Neurosci. 2022;16:1097278. doi: 10.3389/fnins.2022.1097278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Eltokhi A., Sommer I.E. A Reciprocal Link Between Gut Microbiota, Inflammation and Depression: A Place for Probiotics? Front. Neurosci. 2022;16:852506. doi: 10.3389/fnins.2022.852506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Bashir Y., Khan A.U. The interplay between the gut-brain axis and the microbiome: A perspective on psychiatric and neurodegenerative disorders. Front. Neurosci. 2022;16:1030694. doi: 10.3389/fnins.2022.1030694. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.