Abstract
Background
The high utilization of acute care services, particularly emergency departments (ED), continues to be a significant concern for healthcare providers. Numerous approaches have been studied to meet the care needs of patients who frequently seek care in the ED; however, there is no comprehensive review of the current literature base. As such, a current understanding of the interventions initiated within the ED to address the needs of frequent users is required. This mapping review had three objectives: identify the characteristics associated with the need to frequently seek care in the ED; identify interventions implemented to address the needs of this population; and identify gaps in the current evidence base.
Methods
A knowledge map was created by scoping the literature to identify characteristics associated with frequent ED use and interventions implemented to address frequent use. Then, a literature search was conducted to determine what has been implemented by EDs to reduce frequent ED use. The literature was searched from 2013 to January 2023. MeSH terms and keywords were used to identify relevant studies. Studies implementing an intervention for those with characteristics associated with frequent ED use and reporting on ED use were included.
Results
Twenty-three (23) controlled trials and 35 observational studies were included. The most common populations were older adults, those with chronic conditions, and generic “frequent users”. No studies assessed Indigenous Peoples or racial minorities, and few assessed patients with a disability or patients experiencing homelessness. The most common interventions were referrals, care plans, case management, care coordination, and follow-up phone calls. Most studies reported ED revisits, hospitalization, costs, length-of-stay, or outpatient utilization. Few assessed patient or staff perspectives. About one-third of studies (n = 24) reported significant reductions in ED revisits.
Conclusions
Similar interventions, mainly focused on care coordination and planning, have been implemented to address frequent use of the ED. There are still significant gaps in the populations that have been studied. Efforts now must be undertaken to study more diverse populations whose care needs are not being met elsewhere and thus frequent the ED often.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12873-024-00970-7.
Keywords: Emergency department, Frequent users, Knowledge map, Mapping review
Introduction
The high utilization of acute care services, particularly emergency department (ED) visits, continues to be a significant concern for healthcare providers and policymakers internationally. EDs play a crucial role in the healthcare system by providing immediate care to individuals with urgent medical needs 24 h a day, seven days a week. However, a substantial body of research demonstrates that much of the care provided in the ED is for issues that could be addressed outside the ED or in other healthcare settings [1–7].
There is a growing interest in patients who use the ED often. Some patient populations, such as those with chronic pain diagnoses, those with multiple chronic conditions, or older adults, are more likely to utilize EDs frequently [8]. Often people suffering from conditions such as those require highly complex care for health needs stemming from factors such as multimorbidity, psychiatric comorbidities, psychosocial issues, or a combination of these factors [9]. Patients who visit the ED often represent approximately 4.5–8% of ED patients but account for 21–28% of all ED visits [10]. While the definition of “often” varies with some studies suggesting a threshold of 3 or more annual individual patient visits while others employ 12 or more annual visits [11], the need to meet the care needs of patients with different interventions in the ED is commonly noted.
Numerous approaches have been studied over the years to meet the care needs of patients who frequently seek care in the ED. Many interventions have been implemented numerous times since the 1980s [12]. Some interventions are designed to transition patients away from the ED to other settings, such as an electronic medical record (EMR) flag, education, patient navigators, implementing phone lines, expanding primary care hours, and referring patients to relevant service centers that can address their concerns effectively [13–18]. Other interventions have targeted the structure or operation of the ED. These interventions include increased ED staffing, the implementation of care pathways based on risk assessment, the use of screening tools, nurse-led interventions, and integrated care case management within the ED [8, 10, 19]. These interventions also tend to be favoured by ED staff or hospital administrators wanting to reduce high utilization, as it is easier to adopt an intervention in one ED than it is to implement system-wide changes or community-based interventions. So while addressing the needs of those who frequently seek care in the ED will likely require comprehensive, society-wide changes, understanding what ED staff and administrators can do in the meantime is imperative.
Goals of this investigation
Despite a multitude of research on this topic existing, there is no comprehensive review of the current literature base. As such, a current understanding of the interventions initiated within the ED to reduce ED use in frequent users is required. The overall goal of this mapping review is to identify the characteristics associated with the need to seek care in the ED, identify interventions implemented to reduce unnecessary ED revisits, and to determine if there is any disconnect between who is seeking care and who is being targeted by primary studies.
Methods
To determine the state of the literature regarding ED-initiated interventions for frequent users, we conducted a mapping review to create an evidence and gap map (EGM). An EGM is a systematic way to identify and display the available evidence and the existing gaps relevant to a specific research question [20, 21]. This review followed the PRISMA reporting guidelines [22, 23].
Literature search strategy
To get a comprehensive understanding of the state of the literature, a search was conducted. Embase, MEDLINE, CINHAL, Cochrane CENTRAL, and the Cochrane Database of Systematic Reviews were searched for studies published from 2013 to January 18, 2023. This search updated a previously published systematic review conducted in 2013 to capture recently published interventions [24].
The strategies utilized a combination of MeSH terms (e.g., “Emergency Service”, Hospital”, “Patient Readmission”, “Evaluation Study”) and keywords (e.g., “emergency department”, “hotspot”, “intervention study”) to capture interventions of interest. Vocabulary and syntax were adjusted across the databases. The search was limited to English and French language studies. All study designs were retrieved. The search strategy was developed by a research librarian and a peer review of the electronic search strategy was conducted by another research librarian [25]. The full search strategy is available in Appendix A.
Grey literature searches were conducted through the Canadian Agency for Drug and Technologies in Health (CADTH) Grey Matters database, targeted Google searches, and preprint databases including medRixV and Research Square. Canadian provincial health websites were searched for relevant studies or reports. International agency websites including the National Institute for Health and Care Excellence (UK) and Europe PMC were also searched.
Records were downloaded and duplicates were removed using EndNote version 9.3.3 (Clarivate Analytics).
Study selection
A calibration exercise was conducted by four reviewers on a sample of the retrieved abstracts. After 100% agreement was reached among reviewers, the remaining abstracts were screened in duplicate by two teams of two independent reviewers.
To proceed to full-text review, abstracts had to report on an intervention implemented in the ED with the aim of reducing ED revisits or improving ED care. The columns of the knowledge map created in the previous step were used to determine the characteristics and interventions of interest. The population of interest was adults (18 or older) who were characterized by the authors as “frequent users”, or who had characteristics associated with frequent ED use, such as older adults or those with mental health conditions. Interventions of interest included any intervention that was initiated within the ED. Community-based, hospital-wide, or other interventions were only included if there was an intervention in the ED for these resources. All study designs were included, including qualitative studies that met the other inclusion criteria. Any comparator was considered. The outcome of interest was ED use. Abstracts were excluded if they failed to meet the inclusion criteria, or if they were published in other languages other than English or French. Abstracts selected for inclusion by either reviewer proceeded to full-text review. This initial screen was intentionally broad to ensure that all relevant literature was captured.
A similar calibration exercise was conducted by all reviewers on a sample of the retrieved full-text studies. After 100% agreement was reached among reviewers, full text review was conducted in duplicate by two independent reviewers. Any discrepancies between reviewers were resolved through discussion and consensus. If required, a third reviewer was consulted. Full texts were included if they met the inclusion criteria outlined above. Conference abstracts, case series, reviews, letters, and editorials were excluded.
Data extraction and analysis
For all included studies, year of publication, country, study design, number of participants, and healthcare practitioner involved in interventions were extracted by a single reviewer using standardized data extraction forms. A second reviewer verified the extracted data. Discrepancies between reviewers during data extraction were resolved through consensus. Additionally, the general population of interest and general intervention utilized were extracted. The data extraction form can be found in Appendix B.
Determining characteristics associated with frequent use and interventions studied in the literature
A knowledge map was created to determine the common characteristics associated with frequent ED use as well as the interventions commonly used to address these patients. Recent studies, systematic reviews, or scoping reviews on frequent ED use were assessed. The patient characteristics associated with frequent use were extracted. The search continued until saturation of characteristics was achieved. The most common characteristics comprised the columns of the knowledge map. A similar method was undertaken to identify interventions commonly used in the ED to address frequent users. The common interventions comprised the rows of the knowledge map.
The results of the literature review were placed within the knowledge map to identify gaps between the patient characteristics associated with frequent use and the populations studied in the literature. Any intervention or characteristic not identified on the knowledge map but identified in the literature was added.
Results
Results of the search
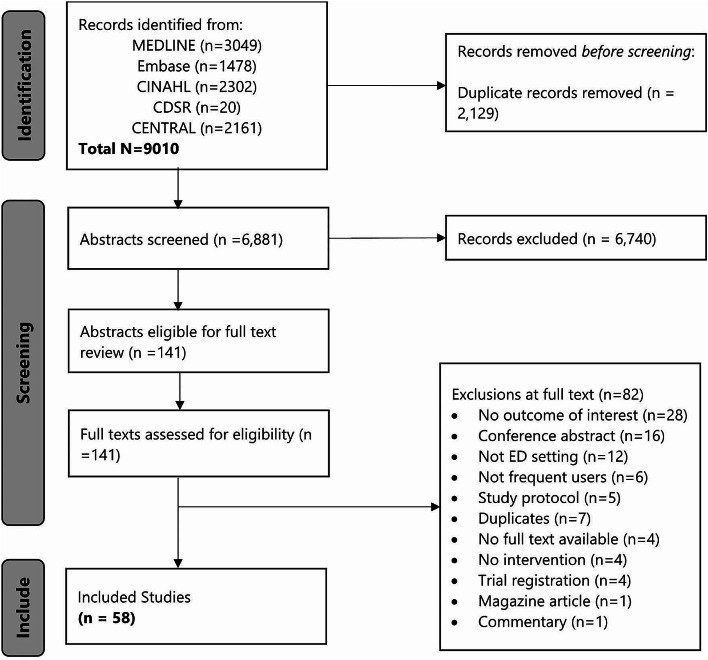
The search strategy yielded 6,881 unique citations, 6,740 of which were excluded after abstract review, Fig. 1. One hundred and forty-one studies proceeded to full-text review. Eighty-two studies were excluded for the following reasons: no outcome of interest (n = 26), conference abstract (n = 16), not ED setting (n = 12), not frequent users (n = 6), study protocol (n = 5), duplicates (n = 5), no full text (n = 4), no intervention (n = 4), trial registration (n = 4), magazine article (n = 1), commentary (n = 1), Fig. 1.
Fig. 1.
Flowchart of studies
Characteristics of included studies
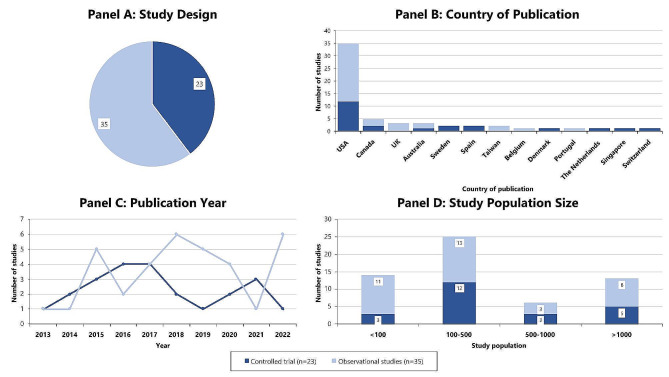
Overall, 58 full texts were included, including 23 controlled trials, one of which was reported in two publications, and 35 observational studies, Fig. 2. There were no qualitative studies identified. Thirty-five (35) were from the US [14, 16, 26–58], five were from Canada [59–63], three were from each of the UK [64–66] and Australia [67–69], two were from each of Sweden [15, 70], Taiwan [71, 72], and Spain [73, 74], and one was from each of Belgium [75], Denmark [76], Portugal [77], the Netherlands [18], Singapore [78], and Switzerland [79], Fig. 2.
Fig. 2.
Study characteristics
Thirty-six (36) studies used treatment-as-usual as the comparator group, 16 used self-comparator, and four used a control group. Study population size varied widely, ranging from seven participants to over 100,000. Fifteen studies had a study population of less than 100 [14, 26, 30, 34, 36, 41, 44, 47, 51, 57, 62, 65, 66, 68, 71], 24 had a study population of 100–500 [15, 16, 27, 28, 32, 33, 38, 40, 42, 43, 48–50, 53, 55, 58–61, 63, 67, 72, 77, 79], six had a study population of 500–1,000 [31, 45, 64, 74, 78, 80], and 13 had a study population of more than 1,000 [18, 29, 36, 37, 39, 46, 52, 54, 56, 69, 70, 75, 76], Fig. 2.
Characteristics associated with frequent ED use
Several characteristics associated with frequent ED use were identified by the process to create the knowledge map, Table 1. These were grouped into three main categories: demographic characteristics, patient health and disability status, and social factors. Demographic characteristics included older adults, Indigenous Persons, and racialized groups and ethnic minorities. Patient health and disability status included patients with chronic conditions, patients with mental health conditions, patients with a disability, and patients with a substance use disorder. Social factors included homelessness and social and material deprivation.
Table 1.
Completed knowledge map
| Interventions | Demographic characteristics | Patient health and disability status | Social factors | Unspecified frequent users | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Older adults | Indigenous peoples | Racialized groups and ethnic minorities | Chronic conditions | Mental health conditions | People with a disability | Substance use disorders | People experiencing homelessness | Social and material deprivation | |||
| Continuation of care | Case management | n = 2 | n = 1 | n = 1 | n = 6 | ||||||
| Care coordination | n = 1 | n = 1 | n = 2 | n = 4 | |||||||
| Care plan | n = 2 | n = 1 | n = 1 | n = 1 | n = 7 | ||||||
| Follow-up phone call | n = 4 | n = 1 | n = 1 | ||||||||
| Care transition intervention | n = 1 | ||||||||||
| Additional services | Early assessment and intervention | n = 1 | |||||||||
| ED physical therapy services | n = 2 | ||||||||||
| Specialist consult in ED | n = 1 | n = 1 | |||||||||
| ED counselling | n = 1 | ||||||||||
| Education | n = 2 | n = 2 | |||||||||
| Geriatric assessment | n = 4 | ||||||||||
| Medication review | n = 2 | ||||||||||
| Telepsychiatry | n = 1 | ||||||||||
| Warning systems | EMR flag | n = 1 | n = 1 | ||||||||
| Pain contract | n = 1 | ||||||||||
| Services outside the ED | Referral | n = 4 | n = 5 | n = 1 | n = 2 | n = 1 | n = 1 | n = 2 | |||
| SBIRT | n = 1 | ||||||||||
| Total | n = 25 | n = 0 | n = 0 | n = 14 | n = 4 | n = 1 | n = 7 | n = 1 | n = 3 | n = 19 | |
*Some interventions were multi-faceted and therefore are represented multiple times in the knowledge map
In the literature search, the only interventions developed based on patients’ demographic characteristics were interventions for older adults, of which there were 16 studies [18, 27, 29, 35, 36, 40, 45, 54, 56, 67, 69, 72, 74–76, 78]. For patient health and disability status, 12 studies were for those with chronic conditions such as diabetes, chronic pain, or epilepsy [31, 33, 34, 37, 38, 53, 58, 60–62, 66, 73], six for those with substance use disorders [26, 43, 48, 50, 52, 59], three for those with mental health conditions [30, 46, 63], and one for people with a disability [71]. Last, there were four studies developed based on patients’ social factors, three for those with social and material deprivation [32, 44, 51] and one for people experiencing homelessness [57], Table 1.
Additionally, 16 interventions were for “frequent users” as defined by the authors [14–16, 28, 39, 41, 42, 47, 49, 55, 64, 65, 68, 70, 77, 79]. The definition of “frequent user” varied; some authors used patients with a specified number of visits in the last 12 [16, 47, 49, 55, 77, 79] or six months [15, 39, 41, 70], the number of visits during multiple periods of time [14, 28, 42], or the most frequent users over a period [65, 68], such as the top 20 most frequent users in one quarter [68].
The literature search did not identify any interventions developed specifically for Indigenous Peoples, other racialized groups, or ethnic minorities, Table 1.
Interventions reported in the literature
Many different interventions were identified in the knowledge map, Table 1. These interventions can be broadly grouped into four categories: continuation of care, additional services in the ED, services outside the ED, and warning systems. Continuation of care consists of interventions that assist patients after their encounter in the ED. Additional services in the ED consist of interventions that provide patients with services not typically associated with the ED, such as specialist consultations, physical therapy services, education, or counselling. Services outside the ED included referring patients to services outside the ED, such as outpatient clinics or primary care providers. Last, warning systems consist of systems in place to identify patients as frequent users or limit the services they can receive in the ED, such as EMR flags or limits on opioid prescriptions.
Several interventions were utilized in the literature, and many studies reported multi-faceted interventions, Table 1. Overall, 36 studies reported on continuation of care interventions: 12 reported on care plans [15, 26, 28, 30, 38, 41, 42, 45, 49, 68, 70, 75], nine reported on case management [14, 15, 44, 47, 55, 63, 64, 72, 79], eight reported on care coordination [16, 39, 48, 50, 58, 65, 69, 77], six reported on follow-up phone calls [18, 30, 35, 36, 60, 67], and one reported on a care transition intervention [51]. Seventeen interventions reported on additional services in the ED: four each reported on education [34, 45, 61, 67] and geriatric assessment [72, 75, 76, 78], two each reported on physical therapy services [27, 29], specialist consultations [31, 76], and medication review [27, 74], and one each reported on early assessment and intervention [40], counselling [60], and telepsychiatry [46]. Seventeen reported on services outside the ED, with 16 reporting on referrals [16, 32, 37, 43, 45, 49, 53, 57, 59, 61, 62, 66, 67, 71, 75, 78] and one reporting on Screening, Brief Intervention and Referral to Treatment (SBIRT) [52]. Last, warning systems were reported in three studies, with EMR flags being reported in two studies [43, 53] and pain contracts being reported in one [33], Table 1.
Thirty-six (36) interventions included nurses, 28 included ED physicians, 15 included social workers, 10 included specialists, eight included family doctors or primary care practitioners, and 33 included other healthcare professionals, intervention staff, or volunteers. Other physicians included in interventions were cardiologists, endocrinologists, psychiatrists, geriatricians, and pulmonologists. Specialists included in interventions include physical therapists, pharmacists, and psychologists. Other staff involved include case managers, care coordinators, clinical directors, peer specialists, legal staff, representatives from local insurance organizations, and health navigators.
Outcomes reported in the literature
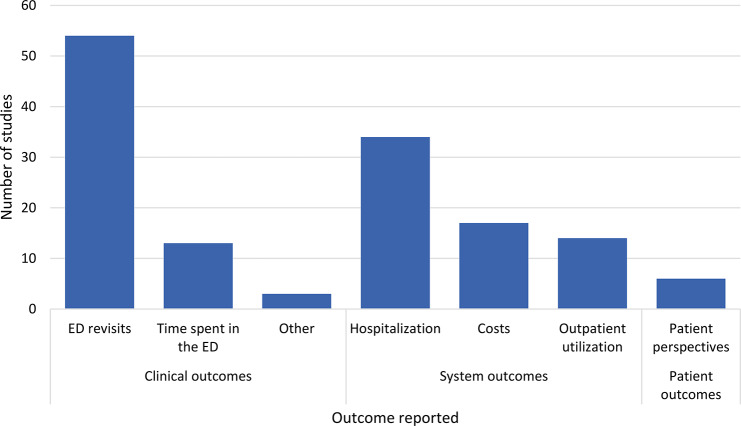
Outcomes reported in this literature can be broadly categorized as system outcomes, clinical outcomes, and patient-reported outcomes, Fig. 3. For clinical outcomes, 54 studies reported ED revisits, 13 reported time spent in the ED, and one each reported the number of diagnostic tests conducted [57], number of referrals provided by ED staff [61], and opioid prescriptions provided by ED staff [50]. Importantly, no studies reported on whether patients’ conditions were improved or worsened. For system outcomes, 34 studies reported on hospitalizations, 17 reported costs, and 14 reported on outpatient utilization. Six studies reported on patient perspectives, though none of these were qualitative. Overall, 24 studies reported significant reductions in ED revisits, 12 reported significant reductions in hospitalization, five reported significant reductions in time spent in the ED, four reported significant increases in outpatient utilization, three reported significant reductions in costs, and one reported significant improvement in patient perspectives.
Fig. 3.
Outcomes reported in the literature
Six studies reported results by sex and/or gender [15, 18, 26, 41, 47, 72], Fig. 4. Of these, three were for those who frequently seek care in the ED [15, 41, 47], two were for older adults [18, 72], and one was for those with a substance use disorder [26]. Two were controlled trials [15, 18] and four were observational studies [26, 41, 47, 72]. Two were multi-faceted interventions, assessing case management and care plans [15] and geriatric assessment and case management [72]. The other interventions assessed care plans [26, 41], case management [47], and follow-up telephone calls [18]. Two studies identified significant differences between men and women, with women consistently having higher ED revisit rates and hospital admissions [26, 72]. No other differences were reported. The remaining four studies found no significant differences between men and women. Additionally, no study distinguished between sex and gender and often it was not clear which concept was being assessed.
Fig. 4.
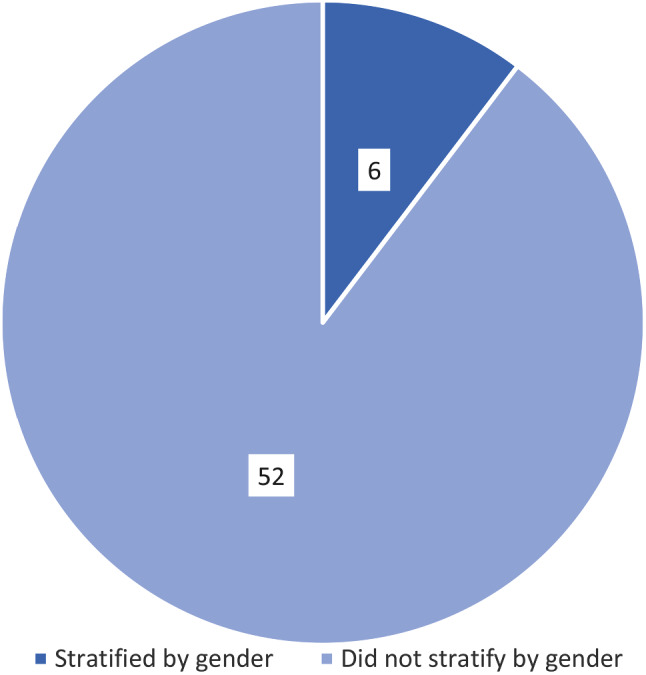
Stratification by gender
Discussion
Overall, 58 studies were identified, including 23 controlled trials and 35 observational studies. Most studies included interventions targeted frequent users as defined by the authors, older adults, and those with chronic conditions. Very few interventions were for marginalized populations, with only a handful for those with mental health conditions, people with a disability, and people experiencing homelessness, and none for Indigenous Peoples and other racialized persons. The types of interventions ranged, with the most popular being referrals, care plans, care coordination, and case management.
There is clearly a disconnect between the populations studied in this literature and the characteristics typically associated with frequent ED use. There were very few interventions for those with mental health conditions and those with social and material deprivation, despite these factors being associated with frequent ED use [24, 81, 82]. In contrast, the most commonly identified characteristics were older adults and those with chronic conditions; while these characteristics are associated with increase ED use, they typically comprise a smaller percentage of ED visits. Further, there were no studies implemented specifically for non-white patients, particularly Indigenous Persons and racialized minorities. It appears, therefore, that those who are at the highest risk of needing to rely on the ED are not typically the focus of ED-initiated interventions. It is likely that interventions for these patients have been implemented outside the ED; however, these patients make up a relatively large portion of ED patients and should be a focus in ED-initiated interventions. Future directions should focus on the gaps identified by this review. Interventions should be developed for the populations missing, particularly Indigenous Peoples, racialized or marginalized patients, patients experiencing homelessness, or patients with a disability or mental illness. Additionally, the interventions that have been trialed should be implemented for these populations and adapted to fit their specific needs. There is a plethora of research demonstrating the need for culturally appropriate and safe care that is tailored to the specific needs of patients, particularly Black and Indigenous patients [83–86]. For example, case management that is developed specifically for Indigenous patients would likely be more successful at meeting patients’ needs than using generic case management strategies. Ultimately, the needs of the patients being cared for should be prioritized.
One major gap in the literature is the types of interventions tried. The most implemented interventions are very similar. For example, care coordination, case management, and care plans all center around ensuring patients’ care is consistent and patients are being supported. Perhaps the literature suggests that these interventions are not as effective as previously suspected, and that while these interventions may have benefits not explored by this literature, other measures are needed to fully address ED frequent use. Further, many of the interventions assessed did not attempt to address the underlying causes of frequent ED use. Some interventions did—many educational interventions focused on self-management and referrals typically referred patients to outpatient centers to learn about their condition—and there were some interventions tailored to very specific populations that attempted to address the underlying needs of patients, such as one intervention for people experiencing homelessness that referred patients to a housing service. Overall, however, most of the interventions were fairly generic and did not attempt to address the barriers faced by patients. Additionally, the characteristics of frequent users can vary based on location [81, 87, 88], so interventions that work in one location may not be appropriate for another. Perhaps more specific, tailored interventions are needed to truly help patients and reduce frequent ED use.
There were some limitations to this review. The first is that community-based or system-wide interventions were excluded. There have likely been interventions developed for the missing populations that were excluded from this review because they were community-based, which would not provide a totally accurate depiction of the interventions trialed to reduce frequent ED use and the populations that have been considered. Additionally, this review only included studies that reported on ED use as an outcome. Though other outcomes were reported, this focus on ED use as an outcome would have limited the number of studies included in the review. There also was not a focus on patient perspectives; qualitative studies would have been included had they reported on ED use as well, but none were identified. Patient perspectives on ED care is important: patients may feel supported by the interventions or may feel they are more in control of their health, which could have other benefits. However, it is important to understand what has been attempted in the ED to understand where further work is needed and understand how EDs can support the patients that do come to the ED.
Conclusion
There is a wide range of interventions that have been implemented to address several populations associated with frequent use of the ED. Despite the wealth of literature, however, there are still significant gaps in the populations that have been assessed and the interventions that have been utilized across multiple populations. Future work should focus on implementing specific interventions created for marginalized patients, particularly Black and Indigenous patients, and interventions that meet the needs of the patients attending the ED. Additionally, new, innovative interventions should be tried, given the homogeneity of interventions identified in the literature and the lack of standout interventions.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
There are not acknowledgements.
Author contributions
BRH, EL, SK, and FC conceived the study. NE and FC designed the review and supervised the conduct of the review and data collection. AM, BA, MK, and NE reviewed the articles. AM and MK extracted the data and conducted quality assessment. AM managed the data. AM drafted the manuscript, and all authors contributed substantially to its revision. FC takes responsibility for the paper as a whole.
Funding
There was no specific funding for this project.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no financial or non-financial competing interests. The Health Technology Assessment Unit is supported by a general grant from Alberta Health (the ministry of health in the province of Alberta) to undertake a wide range of evidence syntheses as part of the Health Evidence Review process.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Moe J, Kirkland SW, Rawe E, et al. Effectiveness of interventions to decrease Emergency Department visits by adult frequent users: a systematic review. Acad Emerg Med. 2017;24(1):40–52. doi: 10.1111/acem.13060. [DOI] [PubMed] [Google Scholar]
- 2.Shumway M, Boccellari A, O’Brien K, Okin RL. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial. Am J Emerg Med. 2008;26(2):155–64. doi: 10.1016/j.ajem.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Spillane LL, Lumb EW, Cobaugh DJ, Wilcox SR, Clark JS, Schneider SM. Frequent users of the emergency department: can we intervene? Acad Emerg Med. 1997;4(6):574–80. doi: 10.1111/j.1553-2712.1997.tb03581.x. [DOI] [PubMed] [Google Scholar]
- 4.Alnasser S, Alharbi M. Analysis of Emergency Department Use by Non-urgent patients and their visit characteristics at an academic Center. Int J Gen Med. 2023;16:221–32. doi: 10.2147/IJGM.S391126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Cathain A, Connell J, Long J, Coster J. Clinically unnecessary’ use of emergency and urgent care: a realist review of patients’ decision making. Health Expect. 2020;23(1):19–40. doi: 10.1111/hex.12995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson LD, Hwang U. Access to care: a review of the emergency medicine literature. Acad Emerg Med. 2001;8(11):1030–6. doi: 10.1111/j.1553-2712.2001.tb01111.x. [DOI] [PubMed] [Google Scholar]
- 7.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Deciding to visit the emergency department for non-urgent conditions: a systematic review of the literature. Am J Manag Care. 2013;19(1):47. [PMC free article] [PubMed] [Google Scholar]
- 8.Kimmel HJ, Brice YN, Trikalinos TA, Sarkar IN, Ranney ML. Real-time Emergency Department Electronic notifications regarding high-risk patients: a systematic review. Telemed J E Health. 2019;25(7):604–18. doi: 10.1089/tmj.2018.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hudon C, Courteau J, Krieg C, Vanasse A. Factors associated with chronic frequent emergency department utilization in a population with diabetes living in metropolitan areas: a population-based retrospective cohort study. BMC Health Serv Res. 2017;17(1):525. doi: 10.1186/s12913-017-2453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med. 2013;44(3):717–29. doi: 10.1016/j.jemermed.2012.08.035. [DOI] [PubMed] [Google Scholar]
- 11.Chiu YM, Vanasse A, Courteau J, et al. Persistent frequent emergency department users with chronic conditions: a population-based cohort study. PLoS ONE. 2020;15(2):e0229022. doi: 10.1371/journal.pone.0229022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flores-Mateo G, Violan-Fors C, Carrillo-Santisteve P, Peiro S, Argimon JM. Effectiveness of organizational interventions to reduce emergency department utilization: a systematic review. PLoS ONE. 2012;7(5):e35903. doi: 10.1371/journal.pone.0035903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tricco A, Jesmin Anto NM, Ivers HM, Ashoor PA, Khan H, Chen. Lianne Kark Ezer, Sharon E. Straus. Effectiveness of quality improvement strategies for coordination of care to reduce use of health care services: a systematic review and meta-analysis. CMAJ Open 2014;186(15). [DOI] [PMC free article] [PubMed]
- 14.Lin MP, Blanchfield BB, Kakoza RM, et al. editors. -based care coordination reduces costs for frequent ED users. Am J Manag Care 2017;23(12):762–766. [PubMed]
- 15.Reinius P, Johansson M, Fjellner A, Werr J, Ohlen G, Edgren G. A telephone-based case-management intervention reduces healthcare utilization for frequent emergency department visitors. Eur J Emerg Med. 2013;20(5):327–34. doi: 10.1097/MEJ.0b013e328358bf5a. [DOI] [PubMed] [Google Scholar]
- 16.Seaberg D, Elseroad S, Dumas M, et al. Patient Navigation for Patients Frequently Visiting the Emergency Department: a Randomized, Controlled Trial. Acad Emerg Med. 2017;24(11):1327–33. doi: 10.1111/acem.13280. [DOI] [PubMed] [Google Scholar]
- 17.Van den Heede K, Van de Voorde C. Interventions to reduce emergency department utilisation: a review of reviews. Health Policy. 2016;120(12):1337–49. doi: 10.1016/j.healthpol.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 18.van Loon-van Gaalen M, van der Linden MC, Gussekloo J, van der Mast RC. Telephone follow-up to reduce unplanned hospital returns for older emergency department patients: a randomized trial. J Am Geriatr Soc. 2021;69(11):3157–66. doi: 10.1111/jgs.17336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karam G, Radden Z, Berall LE, Cheng C, Gruneir A. Efficacy of emergency department-based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic review. Geriatr Gerontol Int. 2015;15(9):1107–17. doi: 10.1111/ggi.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White H, Albers B, Gaarder M, et al. Guidance for producing a Campbell evidence and gap map. Campbell Syst Rev. 2020;16(4):e1125. doi: 10.1002/cl2.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campbell F, Tricco AC, Munn Z, et al. Mapping reviews, scoping reviews, and evidence and gap maps (EGMs): the same but different- the big picture review family. Syst Rev. 2023;12(1):45. doi: 10.1186/s13643-023-02178-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol (Engl Ed) 2021;74(9):790–9. doi: 10.1016/j.recesp.2021.06.016. [DOI] [PubMed] [Google Scholar]
- 23.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 24.Soril LJ, Leggett LE, Lorenzetti DL, Noseworthy TW, Clement FM. Characteristics of frequent users of the emergency department in the general adult population: a systematic review of international healthcare systems. Health Policy. 2016;120(5):452–61. doi: 10.1016/j.healthpol.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 25.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 26.Fiesseler F, Riggs R, Salo D, Klemm R, Flannery A, Shih R. Care plans reduce ED visits in those with drug-seeking behavior. Am J Emerg Med. 2015;33(12):1799–801. doi: 10.1016/j.ajem.2015.08.038. [DOI] [PubMed] [Google Scholar]
- 27.Goldberg EM, Marks SJ, Resnik LJ, Long S, Mellott H, Merchant RC. Can an Emergency Department-Initiated Intervention Prevent Subsequent Falls and Health Care Use in older adults? A Randomized Controlled Trial. Ann Emerg Med. 2020;76(6):739–50. doi: 10.1016/j.annemergmed.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grover CA, Sughair J, Stoopes S, et al. Case Management reduces length of stay, charges, and testing in Emergency Department frequent users. West J Emerg Med. 2018;19(2):238–44. doi: 10.5811/westjem.2017.9.34710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lesser A, Israni J, Kent T, Ko KJ. Association between Physical Therapy in the Emergency Department and Emergency Department revisits for older adult fallers: a nationally Representative Analysis. J Am Geriatr Soc. 2018;66(11):2205–12. doi: 10.1111/jgs.15469. [DOI] [PubMed] [Google Scholar]
- 30.Stanley B, Brown GK, Currier GW, Lyons C, Chesin M, Knox KL. Brief intervention and Follow-Up for suicidal patients with repeat Emergency Department visits enhances Treatment Engagement. Am J Public Health. 2015;105(8):1570–2. doi: 10.2105/AJPH.2015.302656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tabit CE, Coplan MJ, Spencer KT, et al. Cardiology Consultation in the Emergency Department reduces re-hospitalizations for low-socioeconomic patients with Acute Decompensated Heart failure. Am J Med. 2017;130(9):1112. doi: 10.1016/j.amjmed.2017.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wexler R, Hefner JL, Sieck C, et al. Connecting Emergency Department patients to Primary Care. J Am Board Fam Med. 2015;28(6):722–32. doi: 10.3122/jabfm.2015.06.150044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alburaih A, Witting MD. Effectiveness of a Rural Emergency Department (ED)-Based Pain contract on ED visits among ED frequent users. J Emerg Med. 2018;55(3):327–e332321. doi: 10.1016/j.jemermed.2018.04.056. [DOI] [PubMed] [Google Scholar]
- 34.Asthana V, Sundararajan M, Ackah RL, et al. Heart failure education in the emergency department markedly reduces readmissions in un- and under-insured patients. Am J Emerg Med. 2018;36(12):2166–71. doi: 10.1016/j.ajem.2018.03.057. [DOI] [PubMed] [Google Scholar]
- 35.Biese K, Lamantia M, Shofer F, et al. A randomized trial exploring the effect of a telephone call follow-up on care plan compliance among older adults discharged home from the emergency department. Acad Emerg Med. 2014;21(2):188–95. doi: 10.1111/acem.12308. [DOI] [PubMed] [Google Scholar]
- 36.Biese KJ, Busby-Whitehead J, Cai J, et al. Telephone Follow-Up for older adults discharged to home from the Emergency Department: a pragmatic randomized controlled trial. J Am Geriatr Soc. 2018;66(3):452–8. doi: 10.1111/jgs.15142. [DOI] [PubMed] [Google Scholar]
- 37.Blair RA, Palermo NE, Modzelewski KL, et al. Reduced Impact of Diabetes Clinic Referral on high-frequency Emergency Department users. Endocr Pract. 2018;24(12):1043–50. doi: 10.4158/EP-2018-0161. [DOI] [PubMed] [Google Scholar]
- 38.Blind F, Melton J, Karp J, et al. Evaluation of the use of individualized patient care plans in frequent emergency department visitors with pain complaints. Int J Emerg Med. 2022;15(1):37. doi: 10.1186/s12245-022-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Capp R, Misky GJ, Lindrooth RC, et al. Coordination program reduced Acute Care Use and increased primary care visits among frequent emergency care users. Health Aff (Millwood) 2017;36(10):1705–11. doi: 10.1377/hlthaff.2017.0612. [DOI] [PubMed] [Google Scholar]
- 40.Cassarino M, Robinson K, Trepel D, et al. Impact of assessment and intervention by a health and social care professional team in the emergency department on the quality, safety, and clinical effectiveness of care for older adults: a randomised controlled trial. PLoS Med. 2021;18(7):e1003711. doi: 10.1371/journal.pmed.1003711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Flowers A, Shade K. Evaluation of a Multidisciplinary Care Coordination Program for frequent users of the Emergency Department. Prof Case Manag. 2019;24(5):230–9. doi: 10.1097/NCM.0000000000000368. [DOI] [PubMed] [Google Scholar]
- 42.Grover CA, Crawford E, Close RJ. The efficacy of Case Management on Emergency Department frequent users: an eight-year observational study. J Emerg Med. 2016;51(5):595–604. doi: 10.1016/j.jemermed.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 43.Kahler ZP, Musey PI, Schaffer JT, Johnson AN, Strachan CC, Shufflebarger CM. Effect of a no superuser opioid prescription policy on ED visits and statewide opioid prescription. West J Emerg Med. 2017;18(5):894–902. doi: 10.5811/westjem.2017.6.33414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kelley L, Capp R, Carmona JF, et al. Patient Navigation To Reduce Emergency Department (ED) utilization among Medicaid Insured, frequent ED users: a Randomized Controlled Trial. J Emerg Med. 2020;58(6):967–77. doi: 10.1016/j.jemermed.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 45.Liberman T, Roofeh R, Sohn N, et al. The GAP-ED project: improving Care for Elderly patients presenting to the Emergency Department. J Emerg Med. 2020;58(2):191–7. doi: 10.1016/j.jemermed.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 46.Maeng D, Richman JH, Lee HB, Hasselberg MJ. Impact of integrating psychiatric assessment officers via telepsychiatry on rural hospitals’ emergency revisit rates. J Psychosom Res. 2020;133:109997. doi: 10.1016/j.jpsychores.2020.109997. [DOI] [PubMed] [Google Scholar]
- 47.McCarty RL, Zarn J, Fenn R, Collins RD. Frequent ED utilizers: a case management program to address patient needs. Nurs Manage. 2015;46(9):24–31. doi: 10.1097/01.NUMA.0000470771.17731.3d. [DOI] [PubMed] [Google Scholar]
- 48.Murphy SM, Howell D, McPherson S, Grohs R, Roll J, Neven D. A randomized controlled trial of a Citywide Emergency Department Care-Coordination Program to reduce prescription opioid-related visits: an economic evaluation. J Emerg Med. 2017;53(2):186–94. doi: 10.1016/j.jemermed.2017.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murphy SM, Neven D. Cost-effective: emergency department care coordination with a regional hospital information system. J Emerg Med. 2014;47(2):223–31. doi: 10.1016/j.jemermed.2013.11.073. [DOI] [PubMed] [Google Scholar]
- 50.Neven D, Paulozzi L, Howell D, et al. A randomized controlled trial of a Citywide Emergency Department Care Coordination Program to reduce prescription opioid related Emergency Department visits. J Emerg Med. 2016;51(5):498–507. doi: 10.1016/j.jemermed.2016.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nossel IR, Lee RJ, Isaacs A, Herman DB, Marcus SM, Essock SM. Use of peer staff in a critical time intervention for frequent users of a Psychiatric Emergency Room. Psychiatr Serv. 2016;67(5):479–81. doi: 10.1176/appi.ps.201500503. [DOI] [PubMed] [Google Scholar]
- 52.Pringle JL, Kelley DK, Kearney SM, et al. Screening, brief intervention, and referral to treatment in the Emergency Department: an examination of Health Care utilization and costs. Med Care. 2018;56(2):146–52. doi: 10.1097/MLR.0000000000000859. [DOI] [PubMed] [Google Scholar]
- 53.Ringwalt C, Shanahan M, Wodarski S, et al. A randomized controlled trial of an Emergency Department Intervention for Patients with chronic Noncancer Pain. J Emerg Med. 2015;49(6):974–83. doi: 10.1016/j.jemermed.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schumacher JR, Lutz BJ, Hall AG, et al. Impact of an Emergency Department-to-Home Transitional Care Intervention on Health Service Use in Medicare beneficiaries: a mixed methods study. Med Care. 2021;59(1):29–37. doi: 10.1097/MLR.0000000000001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shankar KN, Dugas JN, Flacks J, et al. High touch, high trust: using community health advocates and lawyers to address ED high utilizers. Am J Emerg Med. 2022;60:171–6. doi: 10.1016/j.ajem.2022.07.049. [DOI] [PubMed] [Google Scholar]
- 56.Shaw PB, Delate T, Lyman A, Jr, et al. Impact of a clinical pharmacy specialist in an Emergency Department for seniors. Ann Emerg Med. 2016;67(2):177–88. doi: 10.1016/j.annemergmed.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 57.Smith MA, Moyer D. A Quality Improvement Project to examine outcomes of a Partnership to improve the Health of Emergency Department frequent users. J Nurs Care Qual. 2020;36(4):376–81. doi: 10.1097/NCQ.0000000000000534. [DOI] [PubMed] [Google Scholar]
- 58.Zafar MA, Loftus TM, Palmer JP, et al. COPD Care Bundle in Emergency Department Observation Unit Reduces Emergency Department revisits. Respir Care. 2020;65(1):1–10. doi: 10.4187/respcare.07088. [DOI] [PubMed] [Google Scholar]
- 59.Corace K, Willows M, Schubert N, et al. Alcohol Medical Intervention Clinic: a Rapid Access Addiction Medicine Model reduces Emergency Department visits. J Addict Med. 2020;14(2):163–71. doi: 10.1097/ADM.0000000000000559. [DOI] [PubMed] [Google Scholar]
- 60.Cossette S, Vadeboncoeur A, Frasure-Smith N, McCusker J, Perreault D, Guertin MC. Randomized controlled trial of a nursing intervention to reduce emergency department revisits. CJEM. 2015;17(1):13–20. doi: 10.2310/8000.2013.131291. [DOI] [PubMed] [Google Scholar]
- 61.Gao Y, Xu C, Yang A, et al. How Outpatient Diabetes Education Programs can support local hospitals to reduce Emergency Department visits for adults with diabetes. Can J Diabetes. 2022;46(8):797–803. doi: 10.1016/j.jcjd.2022.05.006. [DOI] [PubMed] [Google Scholar]
- 62.Rash JA, Poulin PA, Shergill Y, et al. Chronic Pain in the Emergency Department: a Pilot Interdisciplinary Program demonstrates improvements in disability, psychosocial function, and Healthcare utilization. Pain Res Manag. 2018;2018:1875967. doi: 10.1155/2018/1875967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stergiopoulos V, Gozdzik A, Cohen A, et al. The effect of brief case management on emergency department use of frequent users in mental health: findings of a randomized controlled trial. PLoS ONE. 2017;12(8):e0182157. doi: 10.1371/journal.pone.0182157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Elston J, Gradinger FP, Streeter AJ, Macey S, Martin S. Effectiveness of a targeted telephone-based case management service on activity in an Emergency Department in the UK: a pragmatic difference-in-differences evaluation. BMC Health Serv Res. 2022;22(1):1038. doi: 10.1186/s12913-022-08415-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ng A, Nadarajan V, McIver S, Reid C, Schofield E, Sachar A. Frequent attendances to a London emergency department: a service improvement project embedding mental health into the team. Lond J Prim Care. 2015;7(4):70–7. doi: 10.1080/17571472.2015.11493438. [DOI] [Google Scholar]
- 66.Ridsdale L, McCrone P, Morgan M, Goldstein L, Seed P, Noble A. Can an epilepsy nurse specialist-led self-management intervention reduce attendance at emergency departments and promote well-being for people with severe epilepsy? A non-randomised trial with a nested qualitative phase. Health Serv Delivery Res 2013;1(9). [PubMed]
- 67.Arendts G, Bullow K, Etherton-Beer C, et al. A randomized-controlled trial of a patient-centred intervention in high-risk discharged older patients. Eur J Emerg Med. 2018;25(4):237–41. doi: 10.1097/MEJ.0000000000000444. [DOI] [PubMed] [Google Scholar]
- 68.Gerdtz MF, Kapp S, Michael E, Prematunga R, Virtue E, Knott J. An evaluation of the use of management care plans for people who frequently attend the emergency department. Australas Emerg Care. 2019;22(4):229–35. doi: 10.1016/j.auec.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 69.Shrapnel S, Dent E, Nicholson C. A nurse-led model of care within an emergency department reduces representation rates for frail aged care residents. Aging Clin Exp Res. 2019;31(11):1695–8. doi: 10.1007/s40520-018-1101-z. [DOI] [PubMed] [Google Scholar]
- 70.Edgren G, Anderson J, Dolk A, et al. A case management intervention targeted to reduce healthcare consumption for frequent Emergency Department visitors: results from an adaptive randomized trial. Eur J Emerg Med. 2016;23(5):344–50. doi: 10.1097/MEJ.0000000000000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hsu SL, Tsai KT, Tan TH, et al. Interdisciplinary collaboration and computer-assisted home healthcare referral in the emergency department: a retrospective cohort study. Aging Clin Exp Res. 2022;34(8):1939–46. doi: 10.1007/s40520-022-02109-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin CF, Lin PC, Hu SY et al. Comprehensive Geriatric Assessment and Clinical outcomes in the older people at the Emergency Department. Int J Environ Res Public Health 2021;18(11). [DOI] [PMC free article] [PubMed]
- 73.Juanes A, Ruiz J, Puig M et al. The Effect of the drug-related problems Prevention Bundle on early readmissions in patients from the Emergency Department: a Randomized Clinical Trial. Ann Pharmacother 2022:10600280221143237. [DOI] [PubMed]
- 74.Santolaya-Perrin R, Calderon-Hernanz B, Jimenez-Diaz G, et al. The efficacy of a medication review programme conducted in an emergency department. Int J Clin Pharm. 2019;41(3):757–66. doi: 10.1007/s11096-019-00836-0. [DOI] [PubMed] [Google Scholar]
- 75.Heeren P, Devriendt E, Fieuws S, et al. Unplanned readmission prevention by a geriatric emergency network for transitional care (URGENT): a prospective before-after study. BMC Geriatr. 2019;19(1):215. doi: 10.1186/s12877-019-1233-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pedersen LH, Gregersen M, Barat I, Damsgaard EM. Early geriatric follow-up after discharge reduces readmissions a quasi-randomised controlled trial. Eur Geriatr Med. 2016;7(5):443–8. doi: 10.1016/j.eurger.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 77.Goncalves S, von Hafe F, Martins F, et al. Case management intervention of high users of the emergency department of a Portuguese hospital: a before-after design analysis. BMC Emerg Med. 2022;22(1):159. doi: 10.1186/s12873-022-00716-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Foo CL, Siu VW, Ang H, Phuah MW, Ooi CK. Risk stratification and rapid geriatric screening in an emergency department - a quasi-randomised controlled trial. BMC Geriatr. 2014;14:98. doi: 10.1186/1471-2318-14-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bodenmann P, Velonaki VS, Griffin JL, et al. Case Management may reduce Emergency Department frequent use in a Universal Health Coverage System: a Randomized Controlled Trial. J Gen Intern Med. 2017;32(5):508–15. doi: 10.1007/s11606-016-3789-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Juanes A, Ruiz J, Puig M, et al. The Effect of the drug-related problems Prevention Bundle on early readmissions in patients from the Emergency Department: a Randomized Clinical Trial. Ann Pharmacother. 2023;57(9):1025–35. doi: 10.1177/10600280221143237. [DOI] [PubMed] [Google Scholar]
- 81.Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48(1):1–8. doi: 10.1016/j.annemergmed.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 82.Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department’s frequent users. Acad Emerg Med. 2000;7(6):637–46. doi: 10.1111/j.1553-2712.2000.tb02037.x. [DOI] [PubMed] [Google Scholar]
- 83.Beverley M, Holson DA, Hewlett D., Jr Patient engagement and cultural sensitivity as a strategy to improve health inequities: the solutions are as simple as they are complex. J Natl Med Assoc. 2022;114(6):578–83. doi: 10.1016/j.jnma.2022.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cuevas AG, O’Brien K, Saha S. What is the key to culturally competent care: reducing bias or cultural tailoring? Psychol Health. 2017;32(4):493–507. doi: 10.1080/08870446.2017.1284221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health. 2019;18(1):174. doi: 10.1186/s12939-019-1082-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.O’Sullivan B. Considering culture in Aboriginal care. CMAJ. 2013;185(1):E27–28. doi: 10.1503/cmaj.109-4376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cho ED, Kim B, Kim DH, Lee SG, Jang SY, Kim TH. Factors related to the frequent use of emergency department services in Korea. BMC Emerg Med. 2023;23(1):73. doi: 10.1186/s12873-023-00808-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Saef SH, Carr CM, Bush JS, et al. A comprehensive view of frequent Emergency Department users based on data from a Regional HIE. South Med J. 2016;109(7):434–9. doi: 10.14423/SMJ.0000000000000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.