Abstract
[Purpose] The aim of this study was to examine whether the forward tilt of the sacrum, which can be measured using an inclinometer, correlates with pelvic tilt and is therefore suitable for therapeutic use as part of a postural assessment for treatment planning or for preventive screening. [Participants and Methods] In 121 athletes (22 females, 99 males), we measured the forward tilt of the sacrum in habitual stance using a digital inclinometer attached to the skin at the level of the posterior superior spinae. At the same time, the forward tilt of the pelvis was determined using videography. For this purpose, we determined the angle between two marker spheres placed on the posterior and anterior superior spinae and the horizontal using sagittal posture photographs. [Results] Taking age as a control variable, we found a significant correlation of moderate strength between pelvic tilt and sacral tilt in men. In women, there was a significant correlation with a strong effect. [Conclusion] The measurement of sacral tilt using an inclinometer positioned on the skin between the posterior superior spinae correlates statistically significantly with pelvic tilt and is therefore suitable as an easy-to-use diagnostic tool for therapeutic use in treatment planning and evaluation.
Keywords: Posture assessment, Sacral tilt, Pelvic tilt
INTRODUCTION
The shape of the spine is a decisive factor in the analysis and evaluation of human posture. The alignment of the pelvis in the sagittal plane plays an important role in posture and movement1), as the anchoring of the sacrum in the pelvic bones means that a forward tilt of the pelvis also biomechanically leads to a forward tilt of the sacrum2, 3). This results in an increased lordosis of the lumbar spine4,5,6), which in turn can lead to an increased thoracic kyphosis as compensation7). All in all, this often results in the medically relevant diagnosis of a hollow round back. Such postural deficits may be associated with incorrect loading of the lumbar facet joints and premature degeneration of vertebrae and intervertebral discs and can ultimately lead to complaints8, 9).
In physiotherapy, the correction of incorrect pelvic positions (usually tilting forward in the sagittal plane) is therefore an important starting point for creating a stable base for the spine10,11,12). To this end, it is important to measure meaningful parameters in order to carry out a baseline assessment that allows individual treatment planning or to measure an improvement in the parameters as a follow-up during treatment.
Reference ranges for pelvic forward tilt are known from the literature, which differ slightly between men and women due to differences in pelvic geometry1, 13). Examination of the pelvic alignment using X-ray methods provides a large number of well-studied parameters such as the sacral slope, the pelvic incidence angle, the pelvic angulation and the pelvic tilt14). The disadvantage of these methods, apart from the measuring technology involved, is above all the radiation exposure, which makes this method unsuitable for preventive examinations and screenings. A dependency on age was found for some of these parameters, although the results in the literature are not consistent15,16,17). For this reason, we used the age of the participants as a control variable for all correlation calculations.
Non-invasive, reliable and valid methods determine the position of the pelvis using externally visible anatomical landmarks18, 19). A relevant parameter here is the angle of the connecting line between the anterior superior iliac spine (ASIS) and the posterior superior iliac spine (PSIS) to the horizontal, which is also often referred to in the literature as the pelvic tilt16). For the clarity of nomenclature, we refer to this angle in this article as the external pelvic tilt (ePT) in contrast to the radiologically defined angle. This angle is determined after manual palpation of the spinae and measurement of the forward tilt either with an aid such as the Duometer Plus (OPIW, Opole, Poland) or photometrically using video analysis software (e.g. Dartfish Pro Suite, Fribourg, Switzerland). Both measurement methods are associated with higher costs for the measuring equipment or a higher time expenditure.
Due to the geometry of the pelvis, it can be assumed that the forward tilt of the sacrum correlates with the forward tilt of the pelvic bones5, 20, 21). The external sacral tilt (eST) can be determined very easily using an inclinometer placed on the skin, which makes it very suitable for practical use.
The aim of the present study was therefore to examine whether there is a correlation between external pelvic tilt and external sacral tilt, which would make it practicable to measure the latter in the context of therapeutic activity for diagnostic and follow-up purposes.
PARTICIPANTS AND METHODS
One hundred twenty one athletes (22 women, 99 men) from sports clubs took part in the study (see Table 1 for anthropometric data). The study was conducted in accordance with the Declaration of Helsinki and approved by the university’s ethics committee (reference no. RPTU 23-57). All participants gave their written informed consent; in the case of minors, the parents also gave their written consent. Exclusion criteria were acute orthopaedic or internal diseases, acute pain, past illnesses or operations in the hip-pelvic-lumbar region or acute dizziness.
Table 1. Anthropometric and pelvic data of the participants.
| Females (N=22) | Males (N=99) | |||
| MV ± SD | Min/Max | MV ± SD | Min/Max | |
| Age (years) | 21.14 ± 4.39 | 16/31 | 15.84 ± 1.56 | 13/19 |
| Height (cm) | 164.30 ± 5.61 | 149.5/170.5 | 174.55 ± 8.60 | 155/199 |
| Weight (kg) | 60.40 ± 5.46 | 47.5/68.3 | 66.06 ± 10.76 | 40.3/98.1 |
| ePT (°) | 9.90 ± 4.27 | 0.0/16.6 | 9.09 ± 4.64 | −3.2/24 |
| eST (°) | 12.30 ± 4.63 | 4.27/23.77 | 12.57 ± 5.76 | 1.09/27.73 |
MV: mean value; SD: standard deviation; ePT: external pelvic tilt; eST: external sacral tilt.
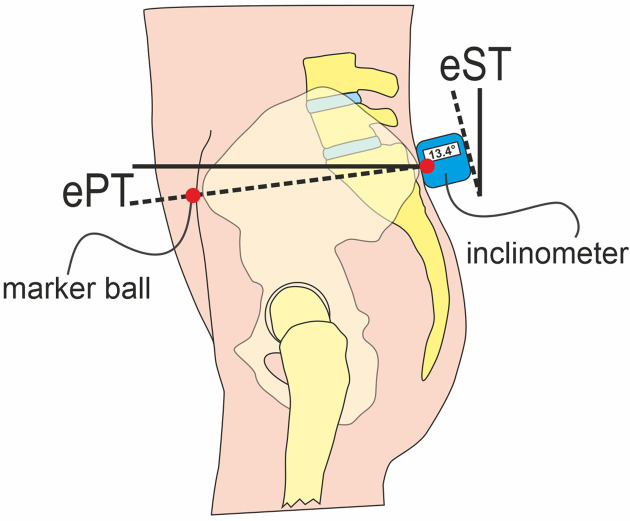
For the examination, the participants stood in underwear (men with bare upper body, women in sports bra) in a habitual position in front of a special measuring wall, with which the camera position was calibrated in the sagittal plane. On the left ASIS and PSIS, we fixed marker spheres (diameter 10 mm) to the skin with double-sided adhesive tape. With a digital camera (Panasonic HC-V777, full HD, Panasonic Corp., Kadoma, Osaka, Japan) mounted on a tripod at hip height we took a posture photo in the sagittal plane at a distance of approximately 2.50 meters. A digital inclinometer (Neoteck NTK033, angular resolution <0.1°, Neoteck Technology LTD., Hong Kong, China) was then positioned centrally between the PSIS on the skin above the sacrum so that the measuring side was flat on the skin, and the angular position was then read (Fig. 1). Care was taken to ensure that the pelvic position did not change by touching the skin.
Fig. 1.
Positioning of the marker spheres (red dots) and the inclinometer in the pelvic region.
ePT: external pelvic tilt; eST: external sacral tilt.
We analyzed the posture photos using the Dartfish ProSuite 6 software (Dartfish, Fribourg, Switzerland) and calculated the angle between the ASIS-PSIS connecting line and the horizontal (Fig. 1).
The statistical analysis was carried out using the IBM SPSS Statistics software (version 29.0, IBM Corp., Armonk, NY, USA). First, the data sets for men and women were tested separately for normal distribution using the Kolmogorov–Smirnov test. This was given in both cases (men ePT: p=0.200, eST: p=0.200; women ePT: p=0.673; eST: p=0.685). As the pelvic geometry may differ between the sexes and as the pelvic position can change with age, the Pearson correlation and the partial correlations were calculated separately for both sexes with age as a control variable.
RESULTS
Table 1 shows the values for ePT and eST found in females and males. There was a significant correlation between external sacral tilt and age in women (r=−0.432, p=0.022) of moderate strength according to Cohen22), but not between external pelvic tilt and age (p=0.064). The same was found for men (eST −age: r=−0.246, p=0.013; ePT −age: r=−0.097, p=0.337).
Considering age as a control variable, there was a significant correlation of r=0.395 (p<0.001) with moderate strength between external pelvic tilt (ePT) and external sacral tilt (eST) in men. In women, there was a significant correlation of r=0.549 (p=0.005) indicating a strong effect.
DISCUSSION
The values for ePT and eST found in females and males are within the range of reference values described by other authors1, 13, 23), so we can assume that there were no particular anomalies here. We found moderate to strong correlations between the investigated pelvic parameters external pelvic tilt and external sacral tilt. This initially shows that, in addition to the ePT, which has been well studied in the literature and reproducibly describes the position of the pelvis in the sagittal plane18, 22, 24), the forward tilt of the sacral region also appears to be a suitable parameter for assessing the pelvic position. The slight age dependency of the parameters must be taken into account, as it is known that the pelvic geometry changes in the course of adolescent development in the sense of a decrease in forward tilt. Mac-Thiong et al.15) found no age dependency of pelvic incidence in asymptomatic adults, neither in women nor in men, but a weak correlation of pelvic tilt with age. In contrast, Merrill et al.16), who also studied adults, found a statistically significant increase in pelvic tilt and pelvic incidence with increasing age. In children and adolescents, the parameters thoracic kyphosis, lumbar lordosis, pelvic tilt and pelvic incidence were found to be weakly correlated with age due to growth effects17). This is in partial accordance with our results, which indicate a significant but only moderate correlation between external sacral tilt and age in both genders, but not between external pelvic tilt and age. However, these age effects are irrelevant for the clinical application of our results.
It must also be kept in mind that there are different pelvic geometries, meaning that the inclination of the sacrum cannot be directly inferred from the forward inclination of the pelvic blade. The parameters measured on the body surface do not correlate directly with radiologically determined parameters, as other studies have shown25). Nevertheless, they can be a valuable tool for assessing the pelvic position.
Our study is subject to some limitations. The measurement of the forward inclination of the sacral region is, like any measurement on a person, subject to errors. The position of the inclinometer does not exactly reflect the position of the sacrum, as skin and fatty tissue lie over the sacrum and the bony structure of the crista sacralis mediana is not homogeneous. Therefore, an inclinometer in the sacral region does not always lie flat on the skin. We have tried to reduce this error by positioning the center of the inclinometer in a reproducible way in the middle between the PSIS. The study was also only conducted with young athletes, whereby the proportion of female participants was significantly lower, but the age of our female participants was higher. Therefore, transferability to other target and age groups must initially be viewed with caution.
The advantage of the inclinometer measurement is that it can be carried out in a few seconds with an inexpensive electronic device and does not require any complex or expensive equipment.
The measurement of sacral forward tilt using a digital inclinometer positioned on the skin between the PSIS correlates statistically significantly with pelvic forward tilt and is therefore suitable as a diagnostic tool for therapeutic use in treatment planning and evaluation.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the individuals who participated in the study.
REFERENCES
- 1.Bibrowicz K, Szurmik T, Lipowicz A, et al. : Tilt and mobility of the hip girdle in the sagittal and frontal planes in healthy subjects aged 19–30 years. J Back Musculoskeletal Rehabil, 2022, 35: 1203–1210. [DOI] [PubMed] [Google Scholar]
- 2.Levine D, Whittle MW: The effects of pelvic movement on lumbar lordosis in the standing position. J Orthop Sports Phys Ther, 1996, 24: 130–135. [DOI] [PubMed] [Google Scholar]
- 3.Fujiwara K, Kiyota N, Toyama H, et al. : Three-dimensional analysis of gender differences in spinal curvature change with pelvic tilt for young adults. Health Behav Sci, 2020, 19: 17–23. [Google Scholar]
- 4.Jackson RP, Kanemura T, Kawakami N, et al. : Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine, 2000, 25: 575–586. [DOI] [PubMed] [Google Scholar]
- 5.Le Huec JC, Aunoble S, Philippe L, et al. : Pelvic parameters: origin and significance. Eur Spine J, 2011, 20: 564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Day JW, Smidt GL, Lehmann T: Effect of pelvic tilt on standing posture. Phys Ther, 1984, 64: 510–516. [DOI] [PubMed] [Google Scholar]
- 7.Czaprowski D, Stoliński Ł, Tyrakowski M, et al. : Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord, 2018, 13: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jentzsch T, Geiger J, Bouaicha S, et al. : Increased pelvic incidence may lead to arthritis and sagittal orientation of the facet joints at the lower lumbar spine. BMC Med Imaging, 2013, 13: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roussouly P, Pinheiro-Franco JL: Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J, 2011, 20: 609–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klee A, Jöllenbeck T, Wiemann K: Correlation between muscular function and posture-lowering the degree of pelvic inclination with exercise. ISBS-Conference Proceedings, 2000. [Google Scholar]
- 11.Ludwig O, Fröhlich M, Schmitt E: Therapy of poor posture in adolescents: sensorimotor training increases the effectiveness of strength training to reduce increased anterior pelvic tilt. Cogent Med, 2016, 3: 1262094. [Google Scholar]
- 12.Kim D, Cho M, Park Y, et al. : Effect of an exercise program for posture correction on musculoskeletal pain. J Phys Ther Sci, 2015, 27: 1791–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herrington L: Assessment of the degree of pelvic tilt within a normal asymptomatic population. Man Ther, 2011, 16: 646–648. [DOI] [PubMed] [Google Scholar]
- 14.Decker S, Müller CW, Omar M, et al. : Sagittal balance of the spine-clinical importance and radiographic assessment. Z Orthop Unfall, 2016, 154: 128–133 (in German). [DOI] [PubMed] [Google Scholar]
- 15.Mac-Thiong JM, Roussouly P, Berthonnaud E, et al. : Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J, 2011, 20: 572–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merrill RK, Kim JS, Leven DM, et al. : Differences in fundamental sagittal pelvic parameters based on age, sex, and race. Clin Spine Surg, 2018, 31: E109–E114. [DOI] [PubMed] [Google Scholar]
- 17.Mac-Thiong JM, Berthonnaud E, Dimar JR, 2nd, et al. : Sagittal alignment of the spine and pelvis during growth. Spine, 2004, 29: 1642–1647. [DOI] [PubMed] [Google Scholar]
- 18.Fourchet F, Materne O, Rajeb A, et al. : Pelvic tilt: reliability of measuring the standing position and range of motion in adolescent athletes. Br J Sports Med, 2014, 48: 594. [Google Scholar]
- 19.Gajdosik R, Simpson R, Smith R, et al. : Pelvic tilt. Intratester reliability of measuring the standing position and range of motion. Phys Ther, 1985, 65: 169–174. [DOI] [PubMed] [Google Scholar]
- 20.Lewis CL, Laudicina NM, Khuu A, et al. : The human pelvis: variation in structure and function during gait. Anat Rec (Hoboken), 2017, 300: 633–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeSilva JM, Rosenberg KR: Anatomy, development, and function of the human pelvis. Anat Rec (Hoboken), 2017, 300: 628–632. [DOI] [PubMed] [Google Scholar]
- 22.Cohen J: Statistical power analysis for the behavioral sciences, revised edition. London: Academic Press, 2013. [Google Scholar]
- 23.Stolinski L, Kozinoga M, Czaprowski D, et al. : Two-dimensional digital photography for child body posture evaluation: standardized technique, reliable parameters and normative data for age 7–10 years. Scoliosis Spinal Disord, 2017, 12: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iunes D, Bevilaqua-Grossi D, Oliveira A, et al. : Comparative analysis between visual and computerized photogrammetry postural assessment. Braz J Phys Ther, 2009, 13: 308–315. [Google Scholar]
- 25.Gilliam J, Brunt D, MacMillan M, et al. : Relationship of the pelvic angle to the sacral angle: measurement of clinical reliability and validity. J Orthop Sports Phys Ther, 1994, 20: 193–199. [DOI] [PubMed] [Google Scholar]