Abstract
Background
There may be a higher risk of sexual dysfunction in the schizophrenia population. China has made significant contributions to the global community of patients with schizophrenia. Currently, there is no estimation of the prevalence of sexual dysfunction in Chinese patients with schizophrenia.
Aim
We conducted a meta-analysis to pool the evaluated prevalence of sexual dysfunction in Chinese patients with schizophrenia.
Methods
We systematically searched PubMed, Web of Science, Embase, PsycINFO, China National Knowledge Infrastructure, China Science and Technology Journal Database, Wanfang Medical Network, and Huayi Academic Literature Database from inception to September 2023. Meta-analysis was conducted with R version 4.3.1.
Outcomes
To examine the pooled prevalence of sexual dysfunctions among Chinese patients with schizophrenia.
Results
In our meta-analysis, we included 16 studies with 5417 participants, among whom 1727 experienced sexual dysfunction. The results of the meta-analysis reveal that the prevalence of sexual dysfunction in Chinese patients with schizophrenia is 50.43% (95% CI, 37.86%-62.95%). Subgroup analysis results indicate that various factors—including the specific type of dysfunction, duration of illness, assessment tools, mean ages, study region, gender, research setting, marital status, publication years, and type of antipsychotics—all have a particular impact on the occurrence rate of sexual dysfunction in Chinese patients with schizophrenia. Female patients had a slightly higher prevalence of sexual dysfunction than male patients (65.22% vs 54.84%).
Clinical Implications
The findings of this study can be used in high-quality nursing care for the schizophrenia population, particularly for the care of specific sexual dysfunction nursing.
Strengths and Limitations
This meta-analysis is the first to evaluate the prevalence of sexual dysfunction in China among patients with schizophrenia. The limited number of studies is the most important limitation.
Conclusions
The pooled prevalence of sexual dysfunction in Chinese patients with schizophrenia is relatively high, and the prevention and intervention of individual sexual dysfunctions in schizophrenia are advised.
Keywords: schizophrenia, sexual dysfunction, China, systematic review, meta-analysis
Introduction
Schizophrenia, a chronic severe mental disorder, is attributed to biological, genetic, and environmental factors.1 Notable symptoms include recurrent hallucinations, delusions, cognitive decline, social withdrawal, and emotional apathy, imposing significant distress on patients and a taxing burden on their families.2 A prevalent complication for patients with schizophrenia is sexual dysfunction, encompassing erectile dysfunction, decreased libido, or issues with ejaculation/orgasm—essentially, difficulties concerning sexual desire, behavior, and satisfaction.3 Previous research indicates that individuals with schizophrenia are 2 to 3 times more susceptible to sexual dysfunction than the general population.4
This correlation can be attributed to multiple causal factors.5 From a neurobiological perspective, patients with schizophrenia display abnormalities in intracranial structures such as the prefrontal cortex, insula, and thalamus—all vital structures for receiving, regulating, and transmitting sexual desire sensory signals.6 These abnormalities can consequently lead to sexual dysfunction.6 Another contributory factor is antipsychotic drug treatments: medications such as risperidone and olanzapine, commonly used in schizophrenia management, work by blocking dopamine D2 receptors and 5-HT2A receptors (5-hydroxytryptamine 2A).7 However, this process disrupts the normal regulation of sexual function.7 Additionally, social and psychological factors, such as unemployment and poor socioeconomic status, which frequently accompany schizophrenia, have been linked to occurrences of sexual dysfunction.8
The World Health Organization emphasizes the key role of sexual health in overall well-being for individuals, couples, and families and its broader impact on communities and nations’ socioeconomic development.9 While the sexual health of the general population has received widespread attention, the sexual health woes of patients with schizophrenia are largely overlooked by clinicians and society.10 Sexual dysfunction can significantly affect a patient’s self-esteem, quality of life, and relationship with spouse, and it can be a decisive factor in young patients discontinuing their treatment.11 Prior research illustrates that a healthy sexual lifestyle can boost self-esteem and sleep duration and mitigate negative emotions such as anxiety for patients with schizophrenia.12
China, the world’s most populous developing country, harbors approximately one-third of global patients with schizophrenia, equating to around 8 million individuals.13 Despite the prevalence, patients with schizophrenia do not typically express sexual dysfunction openly, due to the influence of Confucian cultural values in China, which leads to frequent missing of such evaluations.14,15 Additionally, the lack of established data regarding the incidence of sexual dysfunction in Chinese patients with schizophrenia has led to disparities in incidences, varying greatly from 4% to 78%.16,17 This uncertainty has resulted in many medical practitioners underestimating its significance.18
Therefore, it is imperative to conduct a systematic review and meta-analysis with existing studies to compile the prevalence of sexual dysfunction among Chinese patients with schizophrenia. This systematic review and meta-analysis extracted quantitative data from peer-reviewed research, providing an evidence-based framework for future investigations and encouraging conservative cultures to address the issue of sexual dysfunction in patients with schizophrenia.
Methods
We conducted this systematic review following the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-analyses). This protocol was registered and published on the PROSPERO platform (CRD42023469545).
This research was conducted in compliance with the Declaration of Helsinki and was exempted from institutional review board approval due to the nonutilization of confidential patient data.
Inclusion and exclusion criteria
Study type
This cross-sectional study examined the prevalence of sexual dysfunction in Chinese patients with schizophrenia in Chinese or English journals.
Study population
The sample was based on Chinese patients with schizophrenia.
Inclusion criteria
To be included, participants had to meet the diagnostic criteria for schizophrenia as outlined in the ICD-10,19DSM-IV,20 or Chinese Classification of Mental Disorders.21 In addition, study samples had to be representative, and outcome measures had to report the prevalence of sexual dysfunction among Chinese patients with schizophrenia.
Exclusion criteria
Articles were excluded if (1) samples were derived from non-Chinese patients with schizophrenia; (2) the study did not align with the research theme; (3) there was duplicate publication; and (4) studies had unavailable or incomplete data.
Search strategy
One researcher conducted computer-based searches in English databases such as PubMed, Web of Science, Embase, and PsycINFO, as well as in Chinese databases such as China National Knowledge Infrastructure, China Science and Technology Journal Database, Wanfang Medical Network, and Huayi Academic Literature Database, for cross-sectional studies on the sexual functioning of Chinese patients with schizophrenia until September 1, 2023. We supplemented the literature by manually searching for relevant references in the study. The search terms used in PubMed were as follows (MeSH or keywords):
[(schizophrenia OR schizoaffective OR “dementia praecox” OR “schizophrenic disorders” OR “dementia praecox” OR schizophr* OR psychotic OR psychosis) AND (“sexual dysfunction” OR “sexual adverse events” OR “sexual side effects” OR “sexual disorder” OR libido OR “hyper sex” OR orgasm OR orgasm* OR dyspareuni* OR penis dysfunction OR impotence)].
The detailed search strategy is reported in eIndex 1 in the supplement.
Study selection and data extraction
We identified 7649 articles after removing duplicates by reference management software EndNote X9. Three authors (L.Z., Y.C., Y.S.) independently read the titles and abstracts of studies; they collectively identified 113 articles that required a thorough full-text examination. Two primary authors (L.Z. and Y.C.) conducted a full-text assessment of these 113 articles, and 16 articles were included in the meta-analysis. The final articles underwent data extraction. In case of any disagreements, the 2 authors resolved them through discussion and, when necessary, sought consultation from the corresponding author (Y.Z.).
Quality assessment analysis of selected studies
Two researchers (Q.L. and Y.J.) utilized the cross-sectional study bias risk assessment tool recommended by the Agency for Healthcare Research and Quality to evaluate the methodological quality of the literature independently.22 There are 11 items, with responses categorized as yes, no, or unclear.
A yes response is scored 1 point, while all other responses are scored 0 points, resulting in a total score of 11. Articles with a score ≤3 were considered poor quality. In case of any disagreements, the 2 authors resolved them through discussion and, when necessary, sought consultation from the corresponding author.
Statistical analysis
We used R version 4.3.1 to pool the prevalence estimate of sexual dysfunction in Chinese patients with schizophrenia. We employed the logit transformation method to convert prevalence, providing its 95% CI.23 Heterogeneity among the studies was assessed through χ2 test analysis (with a significance level of α = .1), and quantitative judgment was made with the I2 value. If P ≤ .1 and I2 > 50%, heterogeneity was considered present, and a random effects model was used for the meta-analysis; if not, a fixed effects model was employed. Subgroup analysis and meta-regression were conducted to identify the sources of heterogeneity and explore differences in the prevalence of sexual dysfunction among subgroups of patients with schizophrenia. Sensitivity analysis was employed to investigate the stability of the study results, and the presence of publication bias was assessed with a funnel plot and Egger’s test. The significance level for the meta-analysis was set at α = .05.
Results
Study screening process and results
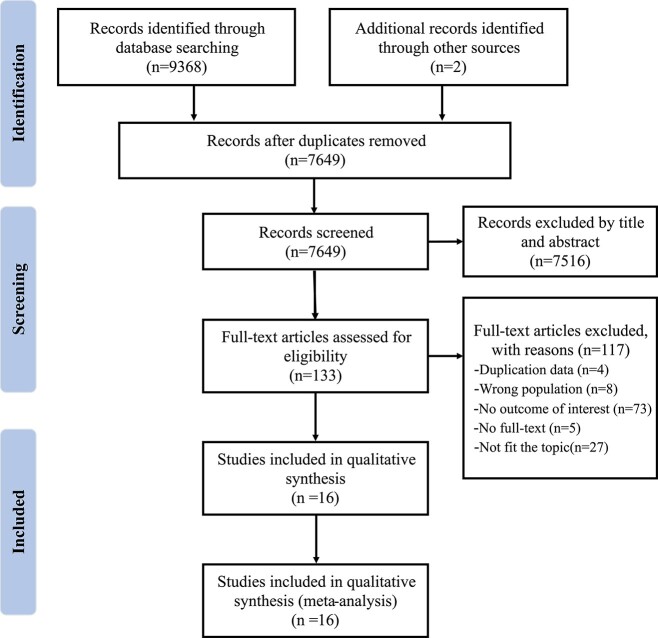
In the initial database search, 9368 relevant articles were identified, and an additional 2 articles were obtained through manual reference searches. After independent step-by-step screening, a final set of 16 cross-sectional studies was included (Figure 1).16,17,24–37 Among these, there were 8 articles in English16,17,24–29 and 8 articles in Chinese.30–37 These studies encompassed 5417 patients with schizophrenia, with 1727 of them experiencing sexual dysfunction.
Figure 1.
Flow diagram of literature search and selection.
Characteristics and quality assessment of studies
All the studies employed a cross-sectional design. Twelve studies were conducted in mainland China, 2 in the Hong Kong region, and 3 in Taiwan. The Xiang study conducted a review of samples from 2480 individuals globally, reporting data from Chinese samples. The study population sources included outpatient clinics, communities, and inpatient settings. In 4 studies, the samples consisted exclusively of male patients with schizophrenia. Six studies utilized the Arizona Sexual Experience Scale–Chinese Version as the assessment tool; 3 used the 5-item International Index of Erectile Function; 2 employed the Brief Sexual Dysfunction Self-rating Scale; 1 utilized the Psychotropic-Related Sexual Dysfunction Questionnaire; and 4 employed self-designed questionnaires. The study characteristics are presented in Table 1. The quality of the studies was rated good, with all receiving a quality score ≥3. The study quality assessment is reported in eIndex 2 in the supplement.
Table 1.
Baseline characteristics of studies.
| First author (year) | Diagnostic criteria | Age, y, mean (SD) | Location | Sample size | Male/female | Assessment tool | Research setting | Sexual dysfunction, % | Risk-of-bias score |
|---|---|---|---|---|---|---|---|---|---|
| Tsai (2011)30 | DSM-IV | 39.52 (8.81) | Taiwan | 161 | 84/77 | ASEX-CV | Outpatient | 70.2 | 9 |
| Gong (1992)31 | CCMD-2 | 38.3 (6.3) | Mainland | 50 | 50/0 | Self-designed | Outpatient | 64 | 5 |
| Hou (2016)17 | ICD-10 | 50.2 (9.7) | Mainland | 607 | 155/92 | ASEX-CV | Community | 78.5 | 8 |
| Huang (2019)24 | ICD-10 | 42.9 (12.3) | Mainland | 720 | 448/272 | ASEX-CV | Community | 71.3 | 7 |
| Liu (2021)25 | DSM-IV | 28.41 (7.61) | Mainland | 162 | 162/0 | ASEX-CV | Inpatient | 29.6 | 8 |
| Ma (2018)26 | DSM-IV | 47.71 (9.54) | Taiwan | 356 | 237/80 | ASEX-CV | Inpatient | 59.3 | 9 |
| Ng (2004)27 | ICD-10 | 38.3 (9.25) | Hong Kong | 70 | 70/0 | IIEF-5 | Outpatient | 41.4 | 5 |
| Shi (2003)32 | — | 44.3 (7.5) | Mainland | 50 | 50/0 | IIEF-5 | Community | 58 | 4 |
| Wang (2016)28 | ICD-10, DSM-IV | 38.3 (9.25) | Mainland | 179 | 86/93 | PRSexDQ | Inpatient | 53.2 | 6 |
| Xu (2009)33 | CCMD-3 | <48 | Mainland | 297 | 142/95 | BSDSRS | Inpatient, outpatient | 44.7 | 4 |
| Xiang (2011)16 | ICD-10, DSM-IV | 43.20 (13.74) | Taiwan/Hong Kong | 2480 | — | Self-designed | — | 6.2/18.6a | 6 |
| Yan (2014)34 | CCMD-3 | 34.5 (7.6) | Mainland | 412 | — | IIEF-5 | Inpatient | 37.9 | 4 |
| Zhang (1992)35 | CCMD-3 | 35.75 (8.52) | Mainland | 191 | 130/61 | Self-designed | Inpatient | 60.7 | 5 |
| Zou (1996)37 | DSM-IV, CCMD-1 | >24 | Mainland | 80 | — | Self-designed | Inpatient | 66.3 | 5 |
| Zhang (2001)36 | CCMD-2 | <55 | Mainland | 408 | 225/183 | BSDSRS | Inpatient, outpatient | 41.3 | 4 |
| Zhang (2018)29 | DSM-5 | 18-65b | Mainland | 118 | 55/63 | ASEX-CV | Inpatient | 51.7 | 7 |
Abbreviations: ASEX-CV, Arizona Sexual Experience Scale–Chinese Version; BSDSRS, Brief Sexual Dysfunction Self-rating Scale; CCMD, Chinese Classification of Mental Disorders; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, International Classification of Diseases; IIEF-5, 5-item International Index of Erectile Function; PRSexDQ, Psychotropic-Related Sexual Dysfunction Questionnaire.
6.2% is the prevalence of sexual dysfunction of Taiwan and 18.6% is HongKong.
Range.
Prevalence estimated of sexual dysfunction
The estimated pooled prevalence of sexual dysfunction in Chinese patients with schizophrenia was 50.43% (95% CI, 37.86%-62.95%) as presented in Figure 2. There was significant heterogeneity within the results for sexual dysfunction (I2 = 98.8%, P < .01). Sensitivity analysis results for the exclusion of individual studies are presented in eIndex 3 in the supplement. We observed that the pooled estimates fluctuated within the range of 48.27% to 55.75%, with no study having a significant impact on the meta-analysis results, indicating the robustness of the findings.
Figure 2.
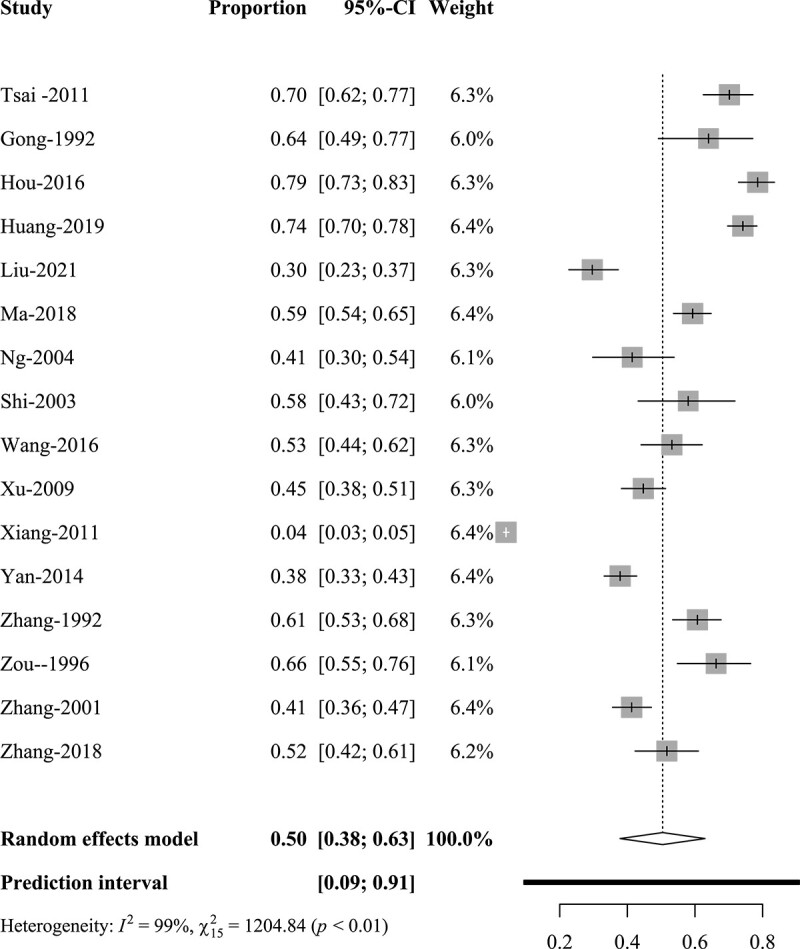
Forest plot for sexual dysfunction in Chinese patients with schizophrenia.
Subgroup and meta-regression analysis
To explore the sources of heterogeneity and potential confounding factors, we performed subgroup analysis and meta-regression based on specific type of dysfunction, duration of illness, assessment tools, mean ages, study region, gender, research setting, marital status, and publication year. The results of the subgroup analysis are presented in Table 2 and eIndex 5 in the supplement, while the meta-regression findings are available in eIndex 6 in the supplement.
Table 2.
Pooled and subgroup results for sexual dysfunction in Chinese patients with schizophrenia.
| Heterogeneity | Meta-analysis | ||||
|---|---|---|---|---|---|
| Item (No. of studies) | I 2 , % | P value | Effect model | Prevalence, % | 95% CI |
| Total prevalence (n = 16)16,17,24–37 | 98.8 | <.01 | Random | 50.43 | 37.86-62.95 |
| Specific type | |||||
| Orgasmic dysfunction | |||||
| Overall (n = 7)17,24,25,30,31,35,37 | 96.5 | <.01 | Random | 26.83 | 14.15-44.92 |
| Male (n = 6)17,24,25,30,31,35 | 94.3 | <.01 | Random | 23.03 | 10.79-42.55 |
| Female (n = 4)17,24,30,35 | 96.0 | <.01 | Random | 47.31 | 20.85-75.37 |
| Sexual desire disorders | |||||
| Overall (n = 4)30,31,35,37 | 81.5 | <.01 | Random | 57.15 | 47.13-66.62 |
| Male (n = 3)30,31,35 | 87.3 | <.01 | Random | 47.33 | 31.03-64.21 |
| Female (n = 2)30,35 | 0.0 | .67 | Fixed | 73.88 | 65.92-80.53 |
| Erectile dysfunction: male (n = 6)17,24,25,27,30,32 | 70.0 | <.01 | Random | 43.32 | 36.22-50.71 |
| Sexual pain: female (n = 3)30,35,37 | 0.0 | .85 | Fixed | 18.86 | 14.19-24.61 |
| Sexual dissatisfaction | |||||
| Overall (n = 6)17,24–26,30,37 | 96.5 | <.01 | Random | 50.89 | 36.89-64.75 |
| Male (n = 5)17,24–26,30 | 95.3 | <.01 | Random | 42.14 | 26.60-59.41 |
| Female (n = 4)17,24,26,30 | 94.3 | <.01 | Random | 43.32 | 26.19-62.20 |
| Duration of illness, y | |||||
| <10 (n = 3)25,31,34 | 88.8 | <.01 | Random | 42.70 | 24.91-69.60 |
| 10-20 (n = 3)24,32,35 | 85.7 | <.01 | Random | 65.64 | 54.43-75.18 |
| >20 (n = 1)17 | — | — | — | 78.54 | 72.98-83.22 |
| Assessment tools | |||||
| Self-designed (n = 4)16,31,35,37 | 99.5 | <.01 | Random | 40.73 | 9.91-81.11 |
| Validated tools (n = 12)17,24–30,32–34,36 | 95.6 | <.01 | Random | 53.89 | 44.41-63.09 |
| ASEX-CV (n = 6)17,24–26,29,30 | 89.9 | <.01 | Random | 61.6 | 57.94-75.15 |
| IIEF-5 (n = 3)27,32,34 | 72.6 | .03 | Random | 44.36 | 33.42-55.88 |
| PRSexDQ (n = 1)28 | — | — | — | 53.17 | 44.45-61.71 |
| BSDSRS (n = 2)33,36 | 0.0 | .42 | Fixed | 42.81 | 38.68-47.05 |
| Mean age, y | |||||
| ≤35 (n = 3)25,28,34 | 87.9 | <.01 | Random | 39.77 | 27.56-53.40 |
| >35, ≤40 (n = 7)27,29–31,33,35,36 | 88.9 | <.01 | Random | 52.86 | 43.39-62.13 |
| >40, ≤45(n = 3)24,33,36 | 99.6 | <.01 | Random | 37.03 | 8.88-78.01 |
| >45 (n = 2)17,26 | 95.6 | <.01 | Random | 69.66 | 48.22-84.99 |
| Study region | |||||
| Mainland (n = 12)17,24,25,28,29,31–37 | 95.3 | <.01 | Random | 55.31 | 46.05-64.22 |
| Taiwan (n = 3)16,26,30 | 99.5 | <.01 | Random | 37.84 | 6.35-84.54 |
| Hong Kong (n = 2)16,27 | 92.4 | <.01 | Random | 28.49 | 11.64-54.65 |
| Gender | |||||
| Male (n = 11)17,24,25,27,29–33,35,36 | 88.9 | <.01 | Random | 54.84 | 46.43-62.99 |
| Female (n = 7)17,24,29,30,35,36 | 96.2 | <.01 | Random | 65.22 | 45.28-80.96 |
| Research setting | |||||
| Outpatient (n = 3)27,30,31 | 87.9 | <.01 | Random | 59.14 | 41.24-74.91 |
| Community (n = 3)17,24,32 | 77.7 | .01 | Random | 71.93 | 60.43-81.12 |
| Inpatient (n = 7)25,26,28,29,34,35,37 | 50.4 | <.01 | Random | 50.94 | 41.00-60.80 |
| Marital status | |||||
| Married/sexual partner <50% (n = 7)25–27,29,30,35,37 | 91.1 | <.01 | Random | 54.35 | 43.25-65.03 |
| Married/sexual partner ≥50% (n = 8)17,24,28,31–34,36 | 96.3 | <.01 | Random | 56.99 | 45.35-67.91 |
| Publication years | |||||
| ≤2010 (n = 7)27,31–33,35–37 | 83.1 | <.01 | Random | 53.19 | 44.85-61.35 |
| >2010 (n = 9)16,17,24–26,28–30,34 | 99.3 | <.01 | Random | 47.99 | 27.55-69.72 |
| Taking antipsychotics | |||||
| FGAs (n = 4)17,24,31,34 | 95.8 | <.01 | Random | 66.96 | 41.43-85.31 |
| SGAs (n = 6)17,24,25,29,31,34 | 95.4 | <.01 | Random | 55.21 | 38.03-71.23 |
Abbreviations: ASEX-CV, Arizona Sexual Experience Scale–Chinese Version; BSDSRS, Brief Sexual Dysfunction Self-rating Scale; FGA, first-generation antipsychotic; IIEF-5, 5-item International Index of Erectile Function; PRSexDQ, Psychotropic-Related Sexual Dysfunction Questionnaire; SGA, second-generation antipsychotic.
Disorder type
The prevalence of different types of sexual dysfunction varied significantly. The prevalence for the various sexual function disorders was as follows: orgasmic dysfunction, 26.83% (95% CI, 14.15%-44.92%); sexual desire disorders, 57.15% (95% CI, 47.13%-66.62%); erectile dysfunction, 43.32% (95% CI, 36.22%-50.71%); dyspareunia, 18.86% (95% CI, 14.19%-24.61%); and sexual dissatisfaction, 50.89% (95% CI, 36.89%-64.75%).
Gender
The prevalence of sexual dysfunction among female patients with schizophrenia is notably higher than in their male counterparts, with a rate of 65.22% for females (95% CI, 45.28%-80.96%) as compared with 54.84% for males (95% CI, 46.43%-62.99%). This disparity becomes even more evident upon examination of specific types of sexual disorders. For instance, the rate of orgasmic disorders in females is 47.31% (95% CI, 20.85%-75.37%), while in males it is 23.03% (95% CI, 10.79%-42.55%). Similarly, sexual desire disorders are reported in 73.88% of females (95% CI, 65.92%-80.53%) in contrast to 47.33% of males (95% CI, 31.03%-64.21%). Furthermore, sexual dissatisfaction is observed in 43.32% of female patients (95% CI, 26.19%-62.20%) as compared with 42.14% of male patients (95% CI, 26.60%-59.41%).
Duration
The subgroup analysis results revealed a significant association between the duration of illness and the prevalence of sexual dysfunction in Chinese patients with schizophrenia. For patients with a duration of illness <10 years, the prevalence was 42.70% (95% CI, 24.91%-69.60%); from 10 to 20 years, it was 65.64% (95% CI, 54.43%-75.18%); exceeding 20 years, the rate was 78.54% (95% CI, 72.98%-83.22%).
Assessment tools
The overall incidence of sexual dysfunction in patients with schizophrenia, as measured by validated tools, was 53.89%. Studies that used the Arizona Sexual Experience Scale–Chinese Version as the assessment tool reported a significantly higher prevalence of 61.60% (95% CI, 57.94%-75.15%). For studies employing the 5-item International Index of Erectile Function, Psychotropic-Related Sexual Dysfunction Questionnaire, and Brief Sexual Dysfunction Self-rating Scale, the prevalence rates were 44.36% (95% CI, 33.42%–55.88%), 53.17% (95% CI, 44.45%–61.71%), and 42.81% (95% CI, 38.68%–47.05%), respectively. In contrast, studies with self-compiled questionnaires reported a significantly lower prevalence of 40.73% (95% CI, 9.91%–81.11%).
Risk-of-bias assessment
The funnel plot is presented in Figure 3, and the Egger’s test is presented in eIndex 4 in the supplement. Visual inspection and the Egger’s test indicate no significant publication bias (t = 1.34, P = .20).
Figure 3.
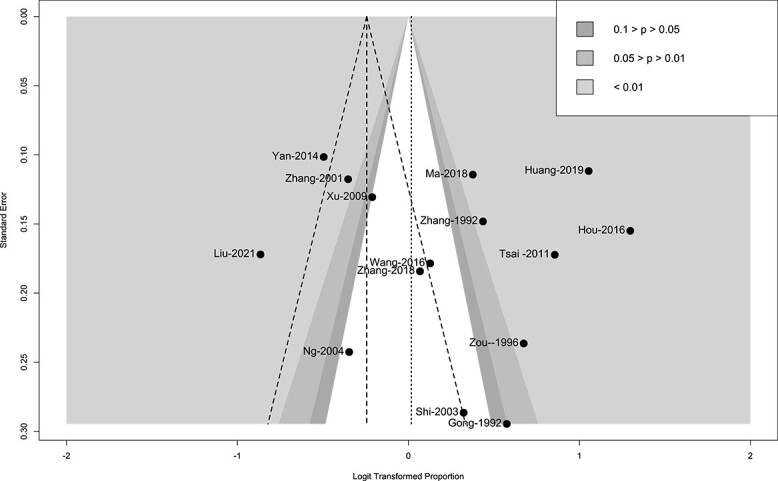
Funnel plot for sexual dysfunction in Chinese patients with schizophrenia.
Discussion
All 16 studies in our analysis reported the prevalence of sexual dysfunction in Chinese patients with schizophrenia. Our current research findings indicate that, as compared with the global prevalence of sexual dysfunction in patients with schizophrenia, which is 56.4%,4 the overall prevalence of sexual dysfunction in Chinese patients with schizophrenia is slightly lower at 50.43%. To mitigate the effects of unverified evaluation instruments on the outcomes, we reassessed the remaining 12 studies following the exclusion of the aforementioned. This reanalysis revealed a marginal increase in the incidence rate by 53.89%, which nevertheless remained below the worldwide prevalence of sexual dysfunction among individuals with schizophrenia. The reasons for this difference may be attributed to variations in diagnostic criteria and disease characteristics among countries and regions. Additionally, cultural and social factors might play a role, given China’s unique sociocultural background. When compared with Western countries, China tends to have a more conservative approach to discussing sexual topics, and clinical professionals may not routinely inquire about sexual dysfunction, resulting in an underestimation of its prevalence.38
Our research findings indicate that among specific types of sexual dysfunction, sexual desire disorders and erectile dysfunction are the most common among patients with schizophrenia, which is consistent with the results of a recent systematic review.39 This prevalence may be attributed to the fact that antipsychotic medications primarily function by inhibiting dopamine receptors, while dopamine is a crucial neurotransmitter regulating sexual desire and arousal.40 Therefore, individuals with schizophrenia are prone to experiencing sexual desire disorders (57.15%), erectile dysfunction (43.32%), and orgasmic dysfunction (26.83%). Our study also reports a prevalence of 50.89% for sexual dissatisfaction and 18.36% for sexual pain. The reasons for these findings may be related to the impact of schizophrenia on the reward circuitry of the brain. The reward circuitry is a neural network in the brain that regulates pleasure, motivation, and emotions.41 Individuals with schizophrenia often exhibit dysfunction in their reward circuitry, resulting in reduced responsiveness to positive stimuli (eg, sexual activities) and an increased responsiveness to negative stimuli (eg, pain). This can diminish their satisfaction with orgasms and lead to discomfort, stress, or pain during sexual intercourse rather than pleasure or satisfaction.
In examining the prevalence of sexual dysfunction among genders, we found that female patients with schizophrenia (65.22%) experience a higher incidence than their male counterparts (54.84%). This disparity may be attributed to the additional reproductive health-related stressors that women face, such as concerns over pregnancy, childbirth, and contraception.42 Furthermore, our analysis of specific sexual dysfunctions, namely sexual desire disorder and orgasmic dysfunction, revealed that these conditions were significantly more prevalent in female patients. The rates for women were nearly double those for men, with sexual desire disorder affecting 73.88% of women vs 47.33% of men, with orgasmic dysfunction mirroring these percentages. These findings underscore the need for heightened awareness and targeted management of sexual dysfunction in female patients with schizophrenia within clinical settings.
Furthermore, subgroup analysis revealed that the longer the duration of illness in Chinese individuals with schizophrenia, the higher the prevalence of sexual dysfunction, consistent with other research findings.5 Regarding the assessment tools used in this meta-analysis, 5 tools were employed, all of which demonstrated variations in their rates of detecting sexual dysfunction in individuals with schizophrenia. Presently, the Arizona Sexual Experience Scale developed by McGahuey et al43 in 2000 is widely used internationally and aligns with the systematic review results by Korchia et al4 in 2023. Our study results also indicate that the prevalence of sexual dysfunction in individuals with schizophrenia increases with age. Therefore, we must not overlook issues related to sexual function in middle-aged and older patients.
Contrasting patients with schizophrenia taking first-generation antipsychotic drugs, those taking the second generation have less incidence of sexual dysfunction. This observation aligns with the results of various studies. It may be attributable to their heightened antagonism of 5-HT2A:D2 receptors and diminished risk of prolactin-related sexual side effects.44 However, one recent study suggests that by excluding the transient effects evident in short-term quetiapine trials, no second-generation antipsychotic truly outperforms the first-generation antipsychotic treatment.45 Therefore, additional future research is warranted.
As compared with patients in Taiwan and Hong Kong, those in mainland China exhibited a higher prevalence of sexual dysfunction. This may be associated with the polymorphism of the 5-HTTLPR gene and its relevance to the sexual function of Han Chinese individuals.46 Additionally, our subgroup analysis revealed that the differences in the prevalence of sexual dysfunction among individuals with schizophrenia were not significant when based on gender, research setting, marital status, and publication years, with high within-group heterogeneity.
Our findings indicate that patients with schizophrenia have a very high incidence of sexual dysfunction. It reminds clinicians of the need to be aware of sexual health issues in this population. Sexual dysfunction is affected by multiple factors, such as the disease itself, antipsychotic drugs, and psychosocial factors.5 In clinical work, we need to separate from excessive attention to the symptoms of mental illness and increase attention to patients’ sexual health needs to better improve their quality of life. In view of the adverse side effects of antipsychotic drugs, we must choose drugs that have less impact on sexual function according to the patient’s specific conditions as much as possible or even explore alternative drug treatments.47 Additionally, nonpharmacologic interventions, such as targeted psychotherapy and cognitive therapy, can be incorporated into treatment regimens to mitigate the adverse effects of antipsychotic-induced sexual dysfunction.47,48
Furthermore, given China’s sociocultural caution regarding sexual health discussions, it is crucial to address communication barriers between clinicians and patients.49 A culturally sensitive approach should be taken to encourage open dialogue about sexual dysfunction.50 Educational initiatives for health care providers and patients may play a key role in this regard.50 For example, physician training programs could emphasize the importance of incorporating sexual health assessment into routine psychiatric evaluations.51 At the same time, patient education materials can make the topic more accessible and empower people with schizophrenia to proactively seek help for their sexual health issues.51 These may be critical in closing gaps in the understanding and management of sexual dysfunction in this group. It also requires the joint efforts of a multidisciplinary team including psychiatrists, sexual health experts, and psychologists.
We acknowledge the following limitations in this study. First, all studies were cross-sectional, and the meta-analysis results may be subject to certain biases due to limitations in study design, sample selection, data analysis, and processing. Second, the studies used different assessment tools, and these scales exhibited variations in sensitivity and specificity, potentially leading to significant heterogeneity. Third, subgroup analyses considered multiple factors; however, heterogeneity remained high, and some subgroup analyses included a limited number of studies. Fourth, most of the combined studies were region specific, lacking research from nationwide studies. Finally, currently, there is a limited number of studies on the prevalence rates of sexual dysfunction in patients with schizophrenia in the Chinese context. Thus, the results of this meta-analysis await further validation through high-quality, large-sample studies.
Conclusion
Our research indicates that the prevalence of sexual dysfunction is relatively high among Chinese patients with schizophrenia. This finding may contribute to an increased focus on the issue of sexual dysfunction in schizophrenia, promoting early identification and targeted interventions for individuals with various types of sexual dysfunction. However, it is important to note that our systematic review included a limited number of studies with varying quality. In the future, there is a need for large-scale, multicenter, or region-specific original research. Systematic reviews similar to ours are necessary to elucidate the impact of sexual dysfunction on individuals with schizophrenia and to emphasize the importance of targeted interventions.
Author contributions
L.Z. and Y.C. contributed equally to the manuscript. Y.C. is the co–first author.
L.Z. AND Y.C.: Conceptualization, Methodology, Formal Analysis, Data Curation, Writing – Original Draft, Writing – Review & Editing; Y.J.: Methodology, Formal Analysis, Resources, Writing – Review & Editing, Supervision, Funding Acquisition; Y.Z.: Formal Analysis, Writing – Review & Editing, Supervision, Project Administration; Q.L. AND Y.J.: Conceptualization, Methodology, Resources, Writing – Review & Editing.
Funding
This work was supported by the National Natural Science Foundation of China (grants 72074063 and 72304076). The funder was not involved in study design, analysis, or interpretation. It also had no part in manuscript preparation, review, or approval and did not influence the decision to publish.
Conflict of interests
The authors disclose no financial or personal conflicts that may have influenced the research presented in this article.
Supplementary Material
Contributor Information
Linghui Zhang, Department of Nursing, Harbin Medical University, Harbin, 150081, China.
Yubin Chen, Department of Nursing, Harbin Medical University, Harbin, 150081, China.
Yujing Sun, Department of Nursing, Harbin Medical University, Harbin, 150081, China.
Yuqiu Zhou, Department of Medical, Huzhou University, Huzhou, Zhejiang 313000, China.
Qi Li, Department of Nursing, Harbin Medical University, Harbin, 150081, China.
Yannan Jia, Department of Nursing, Harbin Medical University, Harbin, 150081, China.
References
- 1. Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388(10039):86–97. 10.1016/S0140-6736(15)01121-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McCutcheon RA, Reis Marques T, Howes OD. Schizophrenia—an overview. JAMA Psychiatry. 2020;77(2):201–210. 10.1001/jamapsychiatry.2019.3360 [DOI] [PubMed] [Google Scholar]
- 3. Acuña MJ, Martín JC, Graciani M, Cruces A, Gotor F. A comparative study of the sexual function of institutionalized patients with schizophrenia. J Sex Med. 2010;7(10):3414–3423. 10.1111/j.1743-6109.2010.01832.x [DOI] [PubMed] [Google Scholar]
- 4. Korchia T, Achour V, Faugere M, et al. Sexual dysfunction in schizophrenia: a systematic review and meta-analysis. JAMA Psychiatry. 2023;80(11):1110. 10.1001/jamapsychiatry.2023.2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhao S, Wang X, Qiang X, et al. Is there an association between schizophrenia and sexual dysfunction in both sexes? A systematic review and meta-analysis. J Sex Med. 2020;17(8):1476–1488. 10.1016/j.jsxm.2020.03.005 [DOI] [PubMed] [Google Scholar]
- 6. Edinoff AN, Nix CA, Fort JM, et al. Sexual dysfunction in schizophrenia: a narrative review of the mechanisms and clinical considerations. Psychiatry International. 2022;3(1):29–42. 10.3390/psychiatryint3010003 [DOI] [Google Scholar]
- 7. Just MJ. The influence of atypical antipsychotic drugs on sexual function. Neuropsychiatr Dis Treat. 2015;11:1655–1661. 10.2147/NDT.S84528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Aker T, Erkoç Ş, Üçok A, İncesu C. Sexual dysfunction in patients with schizophrenia on antipsychotic medication. Eur Psychiatry. 2007;22(5):328–333. 10.1016/j.eurpsy.2007.01.001 [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization. Sexual health: health topics . 2023. Accessed October 31, 2023. https://www.who.int/health-topics/sexual-health#tab=tab_3
- 10. Simiyon M, Chandra PS, Desai G. Sexual dysfunction among women with schizophrenia—a cross sectional study from India. Asian J Psychiatr. 2016;24:93–98. 10.1016/j.ajp.2016.08.022 [DOI] [PubMed] [Google Scholar]
- 11. de Boer MK, Castelein S, Wiersma D, Schoevers RA, Knegtering H. The facts about sexual (dys)function in schizophrenia: an overview of clinically relevant findings. Schizophr Bull. 2015;41(3):674–686. 10.1093/schbul/sbv001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Montejo AL, Majadas S, Montejo-Egido L. EPA-1591—sexual and relational dysfunctions in people wit schizophrenia. Eur Psychiatry. 2014;29(S1):1. 10.1016/S0924-9338(14)78746-224119631 [DOI] [Google Scholar]
- 13. Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. 10.1016/S2215-0366(18)30511-X [DOI] [PubMed] [Google Scholar]
- 14. Chen J, Zhai H, Jin H, Li X, Zhang P, Chen R. Sexual experiences of postmenopausal women in China: a qualitative study. Sex Med. 2023;11(6):11. 10.1093/sexmed/qfad062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yang J-W, Yu K, Wang X-Q, et al. Sexual needs of people with schizophrenia: a descriptive phenomenological study. BMC Psychiatry. 2023;23(1):147. 10.1186/s12888-023-04640-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Xiang YT, Wang CY, Si TM, et al. The low frequency of reported sexual dysfunction in Asian patients with schizophrenia (2001-2009): low occurrence or ignored side effect? Hum Psychopharmacol. 2011;26(4-5):352–357. 10.1002/hup.1213 [DOI] [PubMed] [Google Scholar]
- 17. Hou CL, Zang Y, Rosen RC, et al. Sexual dysfunction and its impact on quality of life in Chinese patients with schizophrenia treated in primary care. Compr Psychiatry. 2016;65:116–121. 10.1016/j.comppsych.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 18. Greenhalgh T. Uncertainty and clinical method. In: Sommers LS, Launer J eds. Clinical Uncertainty in Primary Care: The Challenge of Collaborative Engagement. Springer; 2013: 23–45. [Google Scholar]
- 19. World Health Organization . International Statistical Classification of Diseases and Related Health Problems : Tenth Revision. World Health Organization; 2010. [PubMed] [Google Scholar]
- 20. Bell CC. DSM-IV: diagnostic and statistical manual of mental disorders. JAMA. 1994;272(10):828–829. 10.1001/jama.1994.03520100096046 [DOI] [Google Scholar]
- 21. Chen Y-F. Chinese Classification of Mental Disorders (CCMD-3): towards integration in international classification. Psychopathology. 2002;35(2-3):171–175. 10.1159/000065140 [DOI] [PubMed] [Google Scholar]
- 22. Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8(1):2–10. 10.1111/jebm.12141 [DOI] [PubMed] [Google Scholar]
- 23. Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67(11):974–978. 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 24. Huang YH, Hou CL, Ng CH, et al. Sexual dysfunction in Chinese rural patients with schizophrenia. BMC Psychiatry. 2019;19(1):218. 10.1186/s12888-019-2205-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu D, Liu S, Xiu M, et al. Sexual dysfunction in chronically medicated male inpatients with schizophrenia: prevalence, risk factors, clinical manifestations, and response to sexual arousal. Front Psychiatry. 2021;12:761598. 10.3389/fpsyt.2021.761598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ma MC, Chao JK, Hung JY, Sung SC, Chao IC. Sexual activity, sexual dysfunction, and sexual life quality among psychiatric hospital inpatients with schizophrenia. J Sex Med. 2018;15(3):324–333. 10.1016/j.jsxm.2018.01.008 [DOI] [PubMed] [Google Scholar]
- 27. Ng ML, Ho R. Erectile function of Chinese men with schizophrenia in psychiatric out-patient clinics and their attitude towards treatment. Sex Health. 2004;1(1):35–38. 10.1071/SH03020 [DOI] [PubMed] [Google Scholar]
- 28. Wang YX, Zhang P, Xin LM, et al. Chinese version of the Psychotropic-Related Sexual Dysfunction Questionnaire (PRSexDQ-SALSEX): validity and reliability for schizophrenic patients taking antipsychotics. Psychiatry Res. 2016;246:303–307. 10.1016/j.psychres.2016.05.063 [DOI] [PubMed] [Google Scholar]
- 29. Zhang Y, Tang Z, Ruan Y, et al. Prolactin and thyroid stimulating hormone (TSH) levels and sexual dysfunction in patients with schizophrenia treated with conventional antipsychotic medication: a cross-sectional study. Med Sci Monit. 2018;24:9136–9143. 10.12659/MSM.913759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tsai H-Y, Lee C-S, Wen J-K. An empirical evaluation of the Arizona sexual experience scale for assessing antipsychotic-related sexual dysfunction in outpatients with schizophrenia and schizoaffective disorder. Schizophr Res. 2011;81(2–3):51–63. [DOI] [PubMed] [Google Scholar]
- 31. Gong G, Shu L. 50 Cases of research on the sexual activities of male patients with schizophrenia in the recovery period and their correlation with antipsychotic medications. Article in Chinese. Chinese Journal of Nervous and Mental Diseases. 1992;18(6):357–359. [Google Scholar]
- 32. Shi Y, Wang J. Investigation on the sexual function of patients with community schizophrenia. Article in Chinese. J Clin Psychiatry. 2003;13(6):362–362. [Google Scholar]
- 33. Xu J, Wang H, Gao Z. Sexual dysfunction in the patients with schizophrenics. Article in Chinese. Hainan Medical Journal. 2009;20(7):136–138. [Google Scholar]
- 34. Yan Y, Sui A. Effects on sexual function of different antipsychotic drugs in male patients with schizophrenia. Article in Chinese. Zhejiang Medical Journal. 2014;36(14):1252–1254. [Google Scholar]
- 35. Zhang B, Liu E, Lu L, Liu X, Jiang T, Zhang B. Research on sexual issues related to schizophrenia patients. Article in Chinese. Chinese Journal of Nervous and Mental Diseases. 1992;18(4):206–209,255. [Google Scholar]
- 36. Zhang B, Wang C, Li Z, Cai C. Sexual dysfunction of 298 schizophrenics. Article in Chinese. Chin Ment Health J. 2001;15(3):190–192. [Google Scholar]
- 37. Zou K, Liao Y. Sexual adaptation of patients with schizophrenia. Article in Chinese. China. J Health Psychol. 1996;4(2):85–87. [Google Scholar]
- 38. Colonnello E, Jannini EA. Impact of Chinese traditional culture and related social norms on current Chinese sexuality and on the future of Chinese sexual medicine. In: Cultural Differences and the Practice of Sexual Medicine: A Guide for Sexual Health Practitioners. Springer; 2020:95–113.
- 39. Dumontaud M, Korchia T, Khouani J, et al. Sexual dysfunctions in schizophrenia: beyond antipsychotics: a systematic review. Prog Neuropsychopharmacol Biol Psychiatry. 2020;98:109804. 10.1016/j.pnpbp.2019.109804 [DOI] [PubMed] [Google Scholar]
- 40. Stępnicki P, Kondej M, Kaczor AA. Current concepts and treatments of schizophrenia. Molecules. 2018;23(8):2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Robison A, Thakkar KN, Diwadkar VA. Cognition and reward circuits in schizophrenia: synergistic, not separate. Biol Psychiatry. 2020;87(3):204–214. 10.1016/j.biopsych.2019.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Khalid NN, Jamani NA, Abd Aziz KH, Draman N. The prevalence of sexual dysfunction among postpartum women on the East Coast of Malaysia. J Taibah Univ Med Sci. 2020;15(6):515–521. 10.1016/j.jtumed.2020.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McGahuey CA, Gelenberg AJ, Laukes CA, et al. The Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther. 2000;26(1):25–40. 10.1080/009262300278623 [DOI] [PubMed] [Google Scholar]
- 44. Downing L, Kim DD, Procyshyn RM, Tibbo P. Management of sexual adverse effects induced by atypical antipsychotic medication. J Psychiatry Neurosci. 2019;44(4):287–288. 10.1503/jpn.190053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bobes J, Garc A-Portilla MP, Rejas J, et al. Frequency of sexual dysfunction and other reproductive side-effects in patients with schizophrenia treated with risperidone, olanzapine, quetiapine, or haloperidol: the results of the EIRE study. J Sex Marital Ther. 2003;29(2):125–147. 10.1080/713847170 [DOI] [PubMed] [Google Scholar]
- 46. Luo S, Wang F, Xie Z, Huang X, Lu Y. Study on the correlation of the 5-HTTLPR polymorphism with premature ejaculation in Han Chinese population. Article in Chinese. Beijing Da Xue Xue Bao. 2011;43(4):514–518. [PubMed] [Google Scholar]
- 47. Montejo AL, Montejo L, Baldwin DS. The impact of severe mental disorders and psychotropic medications on sexual health and its implications for clinical management. World Psychiatry. 2018;17(1):3–11. 10.1002/wps.20509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Silva C, Rebelo M, Chendo I. Managing antipsychotic-related sexual dysfunction in patients with schizophrenia. Expert Rev Neurother. 2023;23(12):1147–1155. 10.1080/14737175.2023.2281399 [DOI] [PubMed] [Google Scholar]
- 49. Zhao X. Challenges and barriers in intercultural communication between patients with immigration backgrounds and health professionals: a systematic literature review. Health Commun. 2023;38(4):824–833. 10.1080/10410236.2021.1980188 [DOI] [PubMed] [Google Scholar]
- 50. Atallah S, Redón AM. Relevant (sexual) aspects of cultural differences. In: Geuens S, Polona Mivšek A, Gianotten WL, eds. Midwifery and Sexuality. Springer International Publishing; 2023:271–281. 10.1007/978-3-031-18432-1_23. [DOI] [Google Scholar]
- 51. Lukoff D, Gioia-Hasick D, Sullivan G, Golden JS, Nuechterlein KH. Sex education and rehabilitation with schizophrenic male outpatients. Schizophr Bull. 1986;12(4):669–677. 10.1093/schbul/12.4.669 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.